Abstract
Background
Oncoplastic breast reduction in women with medium to large breasts has reportedly benefitted them both oncologically and cosmetically. We present our experience with an oncoplastic breast reduction technique using a vertical scar superior-medial pedicle pattern for immediate partial breast reconstruction.
Methods
All patients with breast tumours who underwent vertical scar superior-medial pedicle reduction pattern oncoplastic surgery at our centre between September 2006 and June 2010 were retrospectively studied. Follow-up continued from 12 months to 6 years.
Results
Twenty women (age 28–72 yr) were enrolled: 16 with invasive carcinoma and 4 with benign tumours. They all had tumour-free surgical margins, and no further oncological operations were required. The patients expressed a high degree of satisfaction from the surgical outcome in terms of improved quality of life and a good cosmetic result.
Conclusion
The vertical scar superior-medial pedicle reduction pattern is a versatile oncoplastic technique that allows breast tissue rearrangement for various tumour locations. It is oncologically beneficial and is associated with high patient satisfaction.
Abstract
Contexte
Chez des femmes qui avaient une poitrine de moyenne à volumineuse, la réduction mammaire oncoplastique aurait exercé des bienfaits, tant au plan oncologique que cosmétique. Nous présentons notre expérience d’une technique de réduction mammaire oncoplastique à cicatrice verticale et pédicule supéromédian pour une reconstruction mammaire partielle immédiate.
Méthodes
Tous les cas de tumeurs mammaires soumis à la réduction à cicatrice verticale et pédicule supéromédian en chirurgie oncoplastique dans notre centre entre septembre 2006 et juin 2010 ont été passés en revue rétrospectivement. Le suivi s’est échelonné sur 1 à 6 ans.
Résultats
Vingt femmes (âgées de 28 à 72 ans) ont été inscrites : 16 étaient atteintes d’un cancer envahissant et 4 de tumeurs bénignes. Elles présentaient toutes des marges chirurgicales libres de tumeur et aucune autre intervention oncologique n’a été nécessaire. Les patientes ont exprimé un degré élevé de satisfaction à l’endroit des résultats de la chirurgie pour ce qui est de l’amélioration de leur qualité de vie et de l’effet cosmétique positif.
Conclusion
La technique de réduction à cicatrice verticale et pédicule supéromédian est une technique oncoplastique flexible qui permet un réarrangement des tissus mammaires en fonction de la localisation des tumeurs. Au plan oncologique, elle est bénéfique et associée à un degré élevé de satisfaction chez les patientes.
Breast cancer is the most common malignancy affecting women in the western world.1,2 The surgical treatment for breast cancer has continuously undergone profound changes over the past 3 decades, and the medical community currently endorses breast-conserving therapy (BCT) as the gold standard approach for most women with early-stage breast cancer.1,2 The combination of partial mastectomy and postsurgical radiation therapy has sometimes resulted in poor cosmetic results, characterized by deformation and noticeable asymmetry of the shape and size of the operated breast.3–7
This occurs more often when the tumour:breast size ratio is high. Several studies have shown a direct correlation between the magnitude of parenchymal and cutaneous excision and cosmetic outcome.3–7 Improvements in diagnostic technology and mammographic screening as well as increased use of preoperative local or systemic therapies have extended the indications for BCT.1,2 Several oncoplastic breast surgery techniques have been introduced in an attempt to optimize the balance between the risk of local recurrence and the cosmetic outcome of BCT.3–14 The combined plastic surgery techniques of tissue replacement or rearrangement provide a wider local excision while achieving better breast shape and symmetry.3–23
Although macromastia has been considered a contraindication for BCT owing to difficulties in administering radiation therapy at the surgical site, it has become standard procedure for a select group of patients with both breast cancer and breast hypertrophy.15–23 The combination of a tumour resection in a reduction pattern with a contralateral breast reduction was first developed in the late 1980s and has been reported by many authors.15–23 An increasing number of reports have stated that bilateral breast reduction in conjunction with tumour-directed breast-conserving therapy is a surgical technique that can potentially improve the effectiveness of radiation therapy, alleviate neuropathic symptoms that may accompany macromastia and enhance the patients’ perceptions of their bodies after surgery.15–23 Numerous surgical techniques for oncologic breast reduction have been described in the literature, and many of them have variably overlapping technical details, all of which can cause some confusion when evaluating and comparing the published results.15–23
Our objective was to describe our experience with the vertical scar superior-medial pedicle reduction pattern approach for immediate oncoplastic reconstruction surgery on BCT deformities. The indications, advantages and limitations of the technique are discussed, and the simplicity of a single reduction technique for accommodating the different breast tumour regions is emphasized.
Methods
All patients who underwent BCT and immediate reconstruction using the vertical scar superior-medial pedicle reduction pattern oncoplastic surgery at the Tel-Aviv Sourasky Medical Center and a private clinic between September 2006 and June 2010 were included in this series. We retrospectively collected and evaluated data on their demographic characteristics, oncologic findings, hospital admissions and postoperative outcomes. Oncologic information included tumour type, size and location; axillary lymph-node surgery; and adjuvant chemo- and radiotherapy. All breast specimens had been marked and weighed, and surgical margins were assessed by pathology to determine if the tumour had been fully excised and whether the margins were tumour-free.
Each patient was closely followed postoperatively by her plastic and general surgeons as well as by her oncologist. Cosmetic outcome was determined based on patient satisfaction and by grading from 5 independent reviewers, all of whom were plastic surgeons. Categories for evaluation included breast shape, nipple position and breast/nipple symmetry. Each were given a score on a scale of 1 to 4 (1 = poor, 2 = satisfactory, 3 = good, 4 = very good). The patients graded their satisfaction on a scale of 1 to 4 (1 = regret the decision, 2 = disappointed, 3 = satisfied, 4 = very satisfied). Data were collected retrospectively from outpatient charts.
Surgical technique
The patients were seen preoperatively by a multidisciplinary breast surgery team, and a plastic surgeon was consulted because of large breast volume, ptosis or tumour size and location. Patients with macromastia and tumours not located in the superior-medial pole of the breast were considered candidates for an oncoplastic breast reduction technique using the vertical scar superior-medial pedicle pattern for immediate reconstruction. Tumour size and location, surgical scars, resection area and axillary dissection were planned and discussed among the participating specialists after reviewing all relevant breast imaging.
Tumour location was marked on the breast skin. Nipple location was spotted 1–2 cm below the inframammary fold on the central meridian of the breast. A mosque pattern was marked around the new nipple location, and the medial and lateral margins of the skin resection were patterned using the Lassus manoeuvre.24–26 The superior-medial pedicle was marked with a width of 6–8 cm, depending on the volume of the breast and planned tissue resection. The base width of the pedicle included 5 cm of the medial pillar on the vertical limb 1–3 cm from the medial part of the mosque. The pedicle was oriented more medially than superiorly when the distance between the new and old nipple was shorter. Tumour resection was achieved through the skin resection markings of both the general surgeon and the plastic surgeon. Skin undermining beside the tumour bed was performed in order to permit wide glandular resection. After resection, tissue extensions were taken from all tumour bed dimensions, and the tumour bed margins were marked by surgical clips to facilitate locating the original tumour bed for the expected radiation boost. The tumour specimens were marked and weighed. Axillary dissection, when needed, was performed through a separate axillary incision.
Once the tumour had been removed, its location dictated the reduction pattern, resection and insetting. For tumour defects located in the inferior pole of the breast, the remaining skin and glandular tissue were resected according to the previous reduction pattern markings, and the pedicle was rotated superiorly to its new position. The medial and lateral pillars were then shaped and plicated. For tumours that were located in the lateral pole of the breast, the pedicle was harvested with additional glandular tissue from the inferior pole that filled the defect in the lateral area once the pedicle had been rotated superiorly (Fig. 1). Centrally located tumours that required resection of the nipple/areola complex (NAC) were marked by an inverted “V” instead of the mosque design, positioning the tip of the “V” at the planned new nipple position. The pedicle stub (resected NAC) was harvested with additional glandular tissue from the inferior-medial pole, which was rotated to the central area of the breast for better breast projection (Fig. 2). Lateral fullness was addressed by thorough undermining and emptying of the lower-lateral triangles during the procedure. No lateral liposuction was performed.
Fig. 1.
A 45-year-old patient with infiltrating ductal carcinoma (IDC) of her left breast located at the lateral pole (A, B). She previously underwent left lumpectomy with a periareolar incision twice, with involved tumour margins on both occasions. She underwent left relumpectomy with vertical scar superior-medial pedicle reduction pattern oncoplastic surgery and right breast reduction. Postoperative pictures (C, D) 1.5 years after surgery and radiation therapy to the left breast.
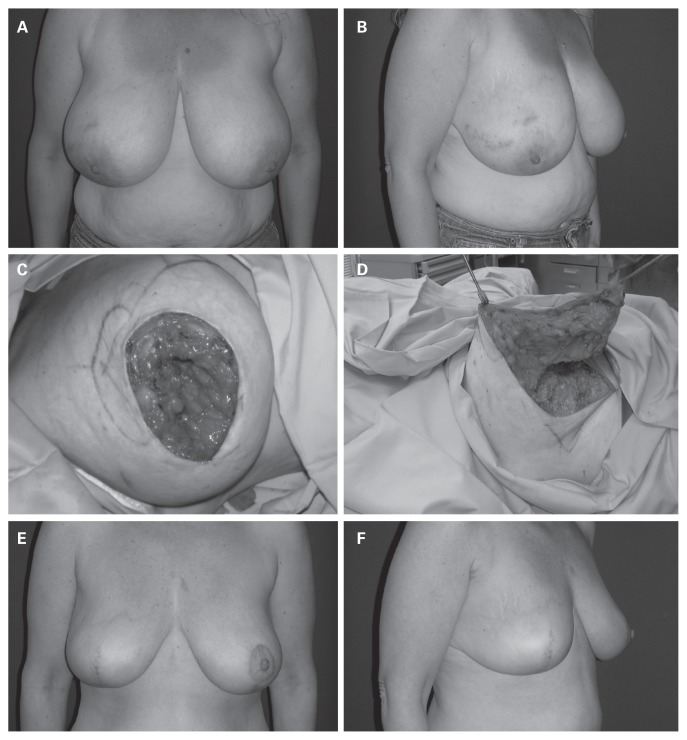
Fig. 2.
A 46-year-old patient with infiltrating ductal carcinoma (IDC) of her right breast located under the nipple/areola complex (NAC) (A, B). The patient underwent right lumpectomy, including the NAC, leaving a large central defect (C). Glandular tissue from the inferior-medial pole based medially was rotated to the central area of the breast to fill in the defect (D). The left breast was reduced simultaneously. Postoperative pictures (E, F) 1 year after surgery and radiation therapy to the right breast.
The resected breast tissue was added to the weight of the tumour specimen for determining total tissue removal. The contralateral breast underwent reduction in the superior-medial pattern. We usually tried to reduce the normal breast by 10% more than the affected breast in order to achieve better symmetry after radiation therapy.
The patient was then positioned upright for final assessment of symmetry, flap moulding and breast shape. Three drains were inserted (1 in each breast and 1 in the axilla after dissection) and the incisions were sutured. The surgical scars were protected with gauze pads, and a sports bra was fitted comfortably over the entire surgical field.
Results
A total of 20 women with breast tumours underwent surgery by means of the vertical scar superior-medial pedicle reduction pattern oncoplastic surgery technique. Their mean age was 46.6 (range 28–72) years. Reconstructions were done immediately by the plastic surgeon after tumour removal by the general surgeon. The participants’ demographic and clinical characteristics are summarized in Table 1. Sixteen patients (80%) had invasive carcinomas and the other 4 patients (20%) had benign breast tumours (2 fibroadenoma, 1 cystosarcoma phylloides and 1 lipoma). Eighteen patients (90%) underwent unilateral oncoplastic reconstruction and 2 patients had bilateral oncoplastic reconstruction. Contralateral breast surgery (n = 18) included 16 with reduction/mastopexy, 1 with contralateral mastectomy and immediate tissue expander reconstruction and 1 with no surgery, yielding a total of 39 operated breasts. The tumour locations are displayed in Figure 3. One patient had unilateral NAC resection because of tumour location. Duration of surgery averaged 3 hours and 30 minutes (range 2.5–5.5 h), and hospital stay averaged 3.5 (range 2–8) days.
Table 1.
Patient characteristics
| Characteristic | No. (%) or mean [range] |
|---|---|
| Age, yr | 46.6 [28–72] |
| Comorbidities | |
| Hyperlipidemia | 3 (15) |
| Hypertension | 2 (10) |
| Asthma | 1 (5) |
| Body mass index | 29 [22–36] |
| Smoker | 2 (10) |
| Premenopausal | 15 (75) |
| Previous breast surgery | 1 (5) |
Fig. 3.

Schematic illustration of patients’ breast tumour locations (22 tumours in 20 patients).
The oncological data are summarized in Table 2. Eleven of the 16 patients with malignant disease underwent axillary lymph node dissection, and 5 patients underwent sentinel lymph node biopsy that was negative for metastasis, both performed from a separate axillary incision. Five patients had chemotherapy before surgery (Table 2) and 8 had it after surgery. All patients with malignant tumours received postoperative radiation therapy. Radiotherapy was administered after chemotherapy and included daily fractionated doses up to a total of 45–50 Gy and an additional boost of 10 Gy to the primary tumour bed.
Table 2.
Oncological data
| Factor | No. (%) or mean [range] |
|---|---|
| Tumour type, n = 22 | |
| Malignant IDC | 18 (82) |
| Nonmalignant | 4 (18) |
| Tumour location, n = 22 | |
| Inferior pole | 13 (59) |
| Lateral pole | 8 (36) |
| Nipple/areola complex | 1 (5) |
| Tumour size, cm; n = 22 | 3.5 [1–12] |
| Tumour specimen weight mean, g | 255 [50–600] |
| Total tumour + reduction resection, g | 534 [50–1265] |
| Total contralateral breast reduction, g; n = 16 | 642 [50–1146] |
| Neoadjuvant chemotherapy, n = 16 | 5 (31) |
| Adjuvant chemotherapy, n = 16 | 8 (50) |
| Malignant tumour staging, n = 16 | |
| T1, < 2 cm | 8 (50) |
| T2, 2–5 cm | 6 (37.5) |
| T3, > 5 cm | 2 (12.5) |
| Tumour receptors, n = 16 | |
| Estrogen positive | 10 |
| HER2-positive | 5 |
HER2 = human epidermal growth factor receptor 2; IDC = infiltrating ductal carcinoma.
All patients had tumour-free surgical margins, and no further oncological operations were required. One patient had invasive ductal carcinoma that reached 0.5 cm from the surgical margin; extension biopsies taken from that area during surgery were negative. No residual tumour was seen on the pathological specimens of 2 patients after they had undergone preoperative neoadjuvant chemotherapy (complete pathological response).
The postoperative follow-up period averaged 34.7 (range 12–72) months. One patient was lost to long-term follow-up because she lived abroad. Postoperative complications included dehiscence of the upper vertical scar and lateral fat necrosis in 1 patient, who was successfully treated conservatively. There were no surgical complications in the contralateral healthy breast. Two patients underwent revision surgery unrelated to radiation therapy: 1 for improved areolar symmetry and the other for re-reduction of the oncoplastic breast owing to asymmetry of the implant-reconstructed contralateral breast (Fig. 4).
Fig. 4.
A 56-year-old patient with a history of left breast cancer and current diagnosis of bilateral breast cancer (A). She underwent left mastectomy and immediate reconstruction with implant and right lumpectomy with vertical scar superior-medial pedicle reduction pattern oncoplastic surgery (B). She underwent right revision surgery owing to breast asymmetry and nipple position (C).
The patients reported a high degree of satisfaction with the surgical outcome in terms of improved breast shape, volume and position, all of which were retained after radiation therapy. Eighteen patients were either very satisfied or satisfied with their results, while 2 patients were disappointed (1 owing to breast asymmetry between the oncoplastic-reduced breast and an implant-reconstructed contralateral breast [Fig. 4] and 1 owing to hypertrophic scarring on the healthy breast). None of the 18 women regretted having undergone the surgery. The independent observers’ evaluation of the 19 patients who completed follow-up was that most of the patients had a very good to good surgical outcome regarding breast shape, NAC position and breast symmetry (Table 3). Figure 5 shows a patient who was considered to have a good to satisfactory outcome based on the evaluation by the independent observers.
Table 3.
Outcome evaluation by independent observers*
| Outcome parameter; score range | No. of patients | Mean (range) |
|---|---|---|
| Breast shape | 3.1 (2.3–3.8) | |
| Very good (n = 4) to good (n = 3) | 14 | |
| Good (n = 3) to satisfactory (n = 2) | 5 | |
| Satisfactory (n = 2) to poor (n = 1) | 0 | |
| Nipple/areola complex position | 3.1 (2.4–3.6) | |
| Very good (n = 4) to good (n = 3) | 15 | |
| Good (n = 3) to satisfactory (n = 2) | 4 | |
| Satisfactory (n = 2) to poor (n = 1) | 0 | |
| Breast symmetry | 2.9 (2.0–3.8) | |
| Very good (n = 4) to good (n = 3) | 14 | |
| Good (n = 3) to satisfactory (n = 2) | 4 | |
| Satisfactory (n = 2) to poor (n = 1) | 1 |
5 observers.
Fig. 5.
A 39-year-old patient with infiltrating ductal carcinoma (IDC) of her right breast located at the upper-lateral pole (A). She underwent right lumpectomy with vertical scar superior-medial pedicle reduction pattern oncoplastic surgery and left breast reduction. Postoperative picture (B) 1 year after surgery and radiation therapy to the right breast.
Discussion
Breast conservative surgery in combination with postoperative radiation therapy has become the gold standard for early-stage breast cancer.1,2 In select patients, the lumpectomy defect and adjuvant radiation therapy can cause substantial breast deformity in shape, size and NAC position. Poor cosmetic results of BCT have been reported in 5%–40% of patients.10–14 The management of secondary breast deformities from partial mastectomies can be challenging, particularly when operating in a radiated field, and increasing attention is being paid to long-term cosmetic results. Immediate breast repair before adjuvant radiotherapy has been shown by many studies to be oncologically safe and esthetically beneficial.3–7,10,14 The breast reduction pattern technique has been described in various series as having a high success rate and good patient satisfaction, especially for those with macromastia and carcinoma of the breast.15–23
The oncoplastic breast reduction technique for partial mastectomy reportedly has numerous advantages: it permits wider resection margins with a higher probability of negative tumour margins; breast tissue rearrangement is done using local tissue, with no other donor sites or foreign body materials, obliterating the lumpectomy tissue dead-space; the reduced breast has better radiation-field efficiency and less radiation fibrosis during radiation therapy compared with larger breasts; and long-term breast surveillance imaging is technically easier and more precise in reduced breasts.10–23 Furthermore, removal of additional breast tissue through reduction techniques allows examination of contralateral breast tissue for occult breast lesions and theoretically makes sense in terms of reducing the risk of breast cancer.
The reduction of the normal contralateral breast in parallel with the oncoplastic reduction pattern reconstruction results in smaller-sized breasts that are aesthetically more pleasing, have better symmetry and provide relief from back and neck pain for patients with large, heavy and pendulous breasts.10–23 There are various management algorithms and approaches for reduction pattern oncoplastic surgery, including different skin reduction patterns, NAC pedicles and breast tissue rearrangement.15–23 Our experience with the vertical scar superior-medial pedicle reduction pattern approach to oncoplastic breast surgery was highly rewarding. This technique is based on the Hall-Findlay vertical reduction mammaplasty24 and has several advantages over other reduction pattern oncoplastic techniques. It is relatively simple and has a short learning curve. It involves a straightforward glandular resection and shorter skin incisions, resulting in a shorter duration of surgery.24 Furthermore, the superior-medial pedicle offers a reliable NAC for different breast sizes as well as versatility for different tumour locations and tissue rearrangement.24–26 The tumour location in this series was in the inferior and lateral poles of the breast, with 1 patient having a tumour under the NAC (Fig. 1). The vertical scar we used has low skin vascular compromise, sparing the long inframammary horizontal scar of the traditional wise pattern. Long-term follow-up findings demonstrated high patient satisfaction as well as high scoring for breast shape, NAC position and breast symmetry by independent observers (Table 3).
Local recurrence is an important consideration in oncoplastic surgery. In our series, the average tumour specimen weighed 255 g, compared with institutional norms of about 40–50 g with the nononcoplastic approach, thus reducing the risk for local recurrence.4 All our patients had tumour-free surgical margins; there was no need to widen the margins in any of them. However, in the event that there had been positive margins, they could have been managed either by completion mastectomy and reconstruction or re-excision, depending on a variety of patient- and surgeon-related factors and preferences as well as pathological findings. There is minimal downside to conversion to mastectomy and reconstruction. The skin is spared and immediate reconstruction is performed.
Early postoperative complications were limited to partial dehiscence of the vertical scar and lateral fat necrosis in 1 patient that was successfully treated conservatively. The vertical scar was closed secondarily before radiation therapy was initiated. There was no incidence in which adjuvant treatment was delayed due to surgical complications. Two patients underwent revision surgery: 1 for periareolar scars and another for rereduction of the oncoplastic breast. No revision surgery was needed as a consequence of postoperative radiation therapy or owing to breast shape (e.g., fat necrosis, breast fibrosis) or symmetry. Because the shape of the breast is generally preserved, cases of postradiation asymmetry can be treated with minor adjustments to the contralateral nonradiated breast rather than by reconstructing a deformity in the radiated breast.
Limitations
There are several limitations associated with the vertical scar superior-medial pedicle reduction pattern technique. Tumours located in the superior and medial poles require modifying the NAC pedicle to an inferiorly or laterally based pedicle. Furthermore, the vertical scar limits skin resection in the vertical aspect, leaving skin puckers, rippling and a mid-inferior dog-ear that can potentially cause scar dehiscence and takes weeks to straighten out and improve. Breast tissue rearrangement can cause internal scar tissue and fat necrosis that sometimes require tissue sampling to rule out recurrent cancer. However, overall we found the technique to be safe and effective without significantly affecting postoperative cancer surveillance.15
Conclusion
Our experience was that the vertical scar superior-medial pedicle reduction pattern was a simple, reliable and highly versatile technique with the other recognized benefits of reduction pattern oncoplastic surgery. It was associated with tumour-free oncological margins, high patient satisfaction and pleasing aesthetic results. Judicious patient selection, coordinated planning and meticulous intraoperative management are the keys to favourable surgical outcome. We encourage the education of patients and physicians about the benefits of oncoplastic surgery for BCT.
Acknowledgements
We thank Esther Eshkol for editorial assistance.
Footnotes
Competing interests: None declared.
Contributors: Y. Barnea, D. Barsuk, T. Menes, A. Zaretski, D. Leshem, J. Weiss, S. Schneebaum and E. Gur designed the study. Y. Barnea and A. Inbal acquired the data, which Y. Barnea analyzed. Y. Barnea and A. Inbal wrote the article, which all authors reviewed and approved for publication.
References
- 1.Fisher B, Anderson S, Bryant J, et al. Twenty-year follow-up of a randomized trial comparing total mastectomy, lumpectomy, and lumpectomy plus irradiation for the treatment of invasive breast cancer. N Engl J Med. 2002;347:1233–41. doi: 10.1056/NEJMoa022152. [DOI] [PubMed] [Google Scholar]
- 2.Veronesi U, Cascinelli N, Mariani L, et al. Twenty-year follow-up of a randomized study comparing breast conserving surgery with radical mastectomy for early breast cancer. N Engl J Med. 2002;347:1227–32. doi: 10.1056/NEJMoa020989. [DOI] [PubMed] [Google Scholar]
- 3.Baildam AD. Oncoplastic surgery of the breast. Br J Surg. 2002;89:532–3. doi: 10.1046/j.1365-2168.2002.02077.x. [DOI] [PubMed] [Google Scholar]
- 4.Masetti R, Di Leone A, Franceschini G, et al. Oncoplastic techniques in the conservative surgical treatment of breast cancer: an overview. Breast J. 2006;12(Suppl 2):S174–80. doi: 10.1111/j.1075-122X.2006.00331.x. [DOI] [PubMed] [Google Scholar]
- 5.Giacalone PL, Roger P, Dubon O, et al. Comparative study of the accuracy of breast resection in oncoplastic surgery and quadrantectomy in breast cancer. Ann Surg Oncol. 2007;14:605–14. doi: 10.1245/s10434-006-9098-5. [DOI] [PubMed] [Google Scholar]
- 6.Kaur N, Petit JY, Rietjens M, et al. Comparative study of surgical margins in oncoplastic surgery and quadrantectomy in breast cancer. Ann Surg Oncol. 2005;12:539–45. doi: 10.1245/ASO.2005.12.046. [DOI] [PubMed] [Google Scholar]
- 7.Asgeirsson KS, Rasheed T, McCulley SJ, et al. Oncological and cosmetic outcomes of oncoplastic breast conserving surgery. Eur J Surg Oncol. 2005;31:817–23. doi: 10.1016/j.ejso.2005.05.010. [DOI] [PubMed] [Google Scholar]
- 8.Losken A, Hamdi M. Partial breast reconstruction: current perspectives. Plast Reconstr Surg. 2009;124:722–36. doi: 10.1097/PRS.0b013e3181b179d2. [DOI] [PubMed] [Google Scholar]
- 9.Kronowitz SJ, Kuerer HM, Buchholz TA, et al. A management algorithm and practical oncoplastic surgical techniques for repairing partial mastectomy defects. Plast Reconstr Surg. 2008;122:1631–47. doi: 10.1097/PRS.0b013e31818cbf1b. [DOI] [PubMed] [Google Scholar]
- 10.Clough KB, Lewis JS, Couturaud B, et al. Oncoplastic techniques allow extensive resections for breast-conserving therapy of breast carcinomas. Ann Surg. 2003;237:26–34. doi: 10.1097/00000658-200301000-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kronowitz SJ, Feledy JA, Hunt KK, et al. Determining the optimal approach to breast reconstruction after partial mastectomy. Plast Reconstr Surg. 2006;117:1–11. doi: 10.1097/01.prs.0000194899.01875.d6. [DOI] [PubMed] [Google Scholar]
- 12.Anderson BO, Masetti R, Silverstein MJ. Oncoplastic approaches to partial mastectomy: an overview of volume-displacement techniques. Lancet Oncol. 2005;6:145–57. doi: 10.1016/S1470-2045(05)01765-1. [DOI] [PubMed] [Google Scholar]
- 13.Huemer GM, Schrenk P, Moser F, et al. Oncoplastic techniques allow breast-conserving treatment in centrally located breast cancers. Plast Reconstr Surg. 2007;120:390–8. doi: 10.1097/01.prs.0000267328.09246.02. [DOI] [PubMed] [Google Scholar]
- 14.Rietjens M, Urban CA, Rey PC, et al. Long-term oncological results of breast conservative treatment with oncoplastic surgery. Breast. 2007;16:387–95. doi: 10.1016/j.breast.2007.01.008. [DOI] [PubMed] [Google Scholar]
- 15.Losken A, Schaefer TG, Newell M, et al. The impact of partial breast reconstruction using reduction techniques on postoperative cancer surveillance. Plast Reconstr Surg. 2009;124:9–17. doi: 10.1097/PRS.0b013e3181ab10e5. [DOI] [PubMed] [Google Scholar]
- 16.Losken A, Styblo TM, Carlson GW, et al. Management algorithm and outcome evaluation of partial mastectomy defects treated using reduction or mastopexy techniques. Ann Plast Surg. 2007;59:235–42. doi: 10.1097/SAP.0b013e31802ec6d1. [DOI] [PubMed] [Google Scholar]
- 17.Kronowitz SJ, Hunt KK, Kuerer HM, et al. Practical guidelines for repair of partial mastectomy defects using the breast reduction technique in patients undergoing breast conservation therapy. Plast Reconstr Surg. 2007;120:1755–68. doi: 10.1097/01.prs.0000287130.77835.f6. [DOI] [PubMed] [Google Scholar]
- 18.Losken A, Elwood ET, Styblo TM, et al. The role of reduction mammaplasty in reconstructing partial mastectomy defects. Plast Reconstr Surg. 2002;109:968–75. doi: 10.1097/00006534-200203000-00025. [DOI] [PubMed] [Google Scholar]
- 19.Shestak KC, Johnson RR, Greco RJ, et al. Partial mastectomy and breast reduction as a valuable treatment option for patients with macromastia and carcinoma of the breast. Surg Gynecol Obstet. 1993;177:54–6. [PubMed] [Google Scholar]
- 20.Newman LA, Kuerer HM, McNeese MD, et al. Reduction mammoplasty improves breast conservation therapy in patients with macromastia. Am J Surg. 2001;181:215–20. doi: 10.1016/s0002-9610(01)00563-3. [DOI] [PubMed] [Google Scholar]
- 21.Spear SL, Pelletiere CV, Wolfe AJ, et al. Experience with reduction mammaplasty combined with breast conservation therapy in the treatment of breast cancer. Plast Reconstr Surg. 2003;111:1102–9. doi: 10.1097/01.PRS.0000046491.87997.40. [DOI] [PubMed] [Google Scholar]
- 22.Jones JA, Pu LL. Oncoplastic approach to early breast cancer in women with macromastia. Ann Plast Surg. 2007;58:34–8. doi: 10.1097/01.sap.0000250754.73886.0c. [DOI] [PubMed] [Google Scholar]
- 23.Munhoz AM, Montag E, Arruda EG, et al. Critical analysis of reduction mammaplasty techniques in combination with conservative breast surgery for early breast cancer treatment. Plast Reconstr Surg. 2006;117:1091–103. doi: 10.1097/01.prs.0000202121.84583.0d. [DOI] [PubMed] [Google Scholar]
- 24.Hall-Findlay EJ. A simplified vertical reduction mammaplasty: shortening the learning curve. Plast Reconstr Surg. 1999;104:748–59. [PubMed] [Google Scholar]
- 25.Orlando JC, Guthrie RH., Jr The superomedial dermal pedicle for nipple transposition. Br J Plast Surg. 1975;28:42–5. doi: 10.1016/s0007-1226(75)90149-6. [DOI] [PubMed] [Google Scholar]
- 26.Munhoz AM, Montag E, Arruda EG, et al. Superior-medial dermo-glandular pedicle reduction mammaplasty for immediate conservative breast surgery reconstruction: technical aspects and outcome. Ann Plast Surg. 2006;57:502–8. doi: 10.1097/01.sap.0000233969.25031.cb. [DOI] [PubMed] [Google Scholar]