Abstract
Background
More than 320 000 hip fractures occur annually in North America. An estimated 30% of this population have cognitive impairment. We sought to determine the extent to which patients with cognitive impairment or dementia have been included in randomized controlled trials (RCTs) assessing hip fracture management.
Methods
We conducted a systematic search of 3 electronic journal databases of articles published between January 2000 and June 2010. Studies were screened in duplicate to collect English-language RCTs assessing operative interventions for femoral head, neck or intertrochanteric fractures. We systematically collected descriptive data and used the χ2 test for comparison between groups as appropriate.
Results
We screened 1201 abstracts, 72 of which were eligible for inclusion in our review. Femoral neck and intertrochanteric fractures were equally represented. Thirty-three (46%) studies did not report the inclusion or exclusion of patients with cognitive impairment. Nineteen (26%) studies explicitly included cognitively impaired patients, whereas 20 (28%) excluded them. Only 2 trials (3%) reported outcomes specific to cognitively impaired patients. Fourteen trials (19.4%) reported the use of a validated cognitive assessment tool. None of the trials that reported inclusion of cognitively impaired patients were from North American centres.
Conclusion
One in 3 patients with hip fractures have concomitant cognitive impairment, yet 8 of 10 hip fracture trials excluded or ignored this population. The ambiguity or exclusion of these patients misses an opportunity to study outcomes and identify factors associated with improved prognosis.
Abstract
Contexte
On dénombre plus de 320 000 fractures de la hanche chaque année en Amérique du Nord et on estime que 30 % de ces personnes ont une atteinte cognitive. Nous avons voulu déterminer dans quelle mesure les patients qui souffrent d’une atteinte cognitive ou de démence ont été inclus dans les essais randomisés et contrôlés (ERC) portant sur la prise en charge de la fracture de la hanche.
Méthodes
Nous avons procédé à une interrogation systématique de 3 bases de don-nées de journaux électroniques pour recenser les articles publiés entre janvier 2000 et juin 2010. Les études ont été passées en revue en parallèle pour dégager les ERC de langue anglaise ayant évalué des interventions chirurgicales pour fractures de la tête ou du col du fémur ou fractures intertrochantériennes. Nous avons recueilli les don-nées descriptives de manière systématique et utilisé le test du χ2 pour comparer des groupes entre eux, selon le cas.
Résultats
Nous avons passé en revue 1201 résumés, dont 72 répondaient à nos critères d’admissibilité. Les fractures du col du fémur et intertrochantériennes étaient représentées en proportions égales. Trente-trois études (46 %) ne faisaient aucune mention de l’inclusion ou de l’exclusion des patients souffrant d’atteinte cognitive. Dix-neuf (26 %) études incluaient expressément des patients souffrant d’atteinte cognitive, tandis que 20 (28 %) les excluaient. Seulement 2 essais (3 %) ont fait état de résultats spécifiques aux patients souffrant d’atteinte cognitive. Quatorze essais (19,4 %) ont déclaré utiliser un outil d’évaluation cognitive validé. Aucun des essais ayant mentionné l’inclusion de patients souffrant d’atteinte cognitive ne provenait de centres nord-américains.
Conclusion
Un patient victime d’une fracture de la hanche sur 3 souffrait concomi-tamment d’une atteinte cognitive et pourtant, 8 essais sur 10 portant sur la fracture de la hanche ont exclus ou ignoré cette population. L’ambiguïté vis-à-vis de ces patients ou leur exclusion est une occasion manquée d’étudier les paramètres et de relever les facteurs associés à un pronostic plus favorable.
More than 320 000 hip fractures occur annually in North America.1,2 As hip fracture is a condition most common among elderly individuals, its societal burden is expected to grow as the North American population continues to age. By 2040, the number of individuals older than 65 is forecasted to increase from 34.8 million to 77.2 million, resulting in an annual hip fracture incidence of greater than 580 000.1 Dementia — a chronic form of cognitive impairment — is prevalent in the elderly population as well, and co-occurrence of this condition with hip fracture is not infrequent. By some estimates, 30% of patients who sustain a hip fracture also have cognitive impairment or dementia.3–5
There is early evidence to suggest that patients with dementia typically experience poorer functional outcomes and increased morbidity and mortality following a hip fracture.6–15 Identifying strategies to optimize outcomes in hip fracture patients with dementia is therefore critically important; however, the extent to which this issue is addressed in orthopedic surgery randomized controlled trials (RCTs) has not been well-elucidated. Exclusion of patients with dementia from surgical RCTs could potentially undermine the applicability of trial results to this sizeable subgroup.
We conducted a systematic review to analyze the inclusion of patients with cognitive impairment and dementia in hip fracture RCTs conducted over the course of the past decade. This information will provide an important consideration to both clinicians managing hip fracture patients with dementia and researchers designing future hip fracture RCTs.
Methods
We performed a systematic review of RCTs involving hip fracture operative treatments to determine the extent to which patients with cognitive impairment or dementia were included. We used applicable components of the PRISMA 2009 checklist as a framework for this review.
Eligibility criteria and study selection
Criteria for inclusion in this review were established a priori, and all studies satisfied the following parameters: RCT study design; assessment of an operative intervention for femoral head, femoral neck, or intertrochanteric fractures; publication in English; original publication; and publication date between January 2000 and June 2010.
We used a 2-step review process to screen and select eligible trials. The first step entailed a review of all titles and abstracts yielded by our search strategy. Studies meeting the inclusion criteria and those with equivocal eligibility were retrieved for full-text review and data retrieval.
Search strategy
We performed a systematic search of the medical literature to identify all relevant RCTs published between January 2000 and June 2010. Two investigators searched 3 electronic medical databases (Medline, Embase, PubMed) using the following search terms: “hip fracture*” OR “femoral neck fracture*” OR “femoral head fracture*” OR “intertrochanteric fracture*” OR “subcapital fracture*” alongside appropriate database subject headings (i.e., MeSH, Emtree). Given the eligibility criteria outlined, we placed the following limits on the searches: publication in the English language, RCT and publication in January 2000 or later. We included a systematic PubMed search as a supplementary query to ensure no pertinent trials were overlooked. This search was done with limits to predetermined journals that were judged to be high-yield: The Journal of Bone & Joint Surgery (American and British volumes), Clinical Orthopaedic and Related Research, Acta Orthopaedica and The Journal of Orthopaedic Trauma.
Data extraction
Standardized data extraction forms were developed a priori. For each study, characteristics of the trial, including geographical location, sample size, number of centres, mean patient population age and sex ratios, were recorded. Furthermore, we documented the fracture type and operative interventions assessed, as well as the significance of the results of the primary outcome measure.
For each trial, we evaluated whether patients with dementia or other forms of cognitive impairment were explicitly included or explicitly excluded. We also recorded the cognitive assessment tool used to make a diagnosis for inclusion or exclusion. If inclusion status could not be ascertained based on the published manuscript or if no mention was made regarding the strategy for cognitive assessment, then we considered it “not reported.” Finally, for studies including patients with dementia, we determined whether a subgroup analysis was performed and assessed the results of such analyses. For studies excluding patients with dementia, we recorded if a rationale for exclusion was provided, and if so, we noted the reason provided.
All data extraction was done in duplicate, and any discrepancies were resolved by consensus among the reviewers.
Statistical analysis
We systematically collected descriptive data and used the χ2 statistical test for comparison between groups as appropriate. Our primary variable of interest was the number of studies that included patients with dementia compared with those that excluded patients with dementia.
Results
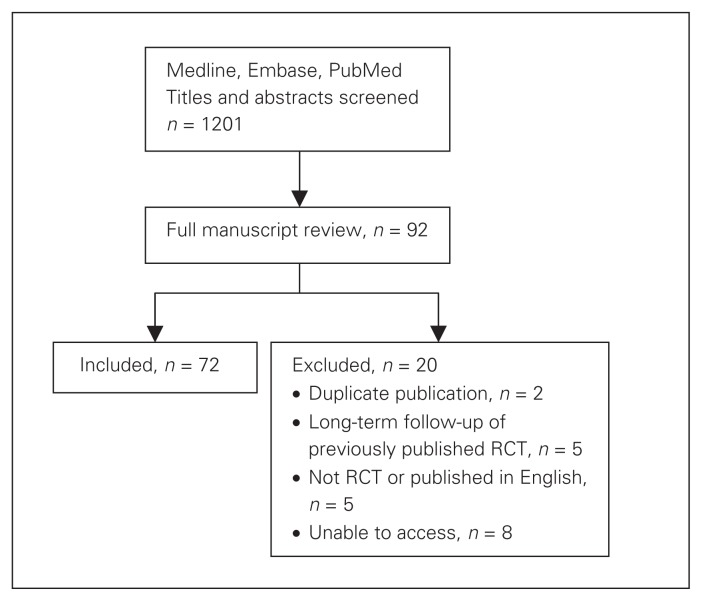
Our search identified a total of 1201 studies published between January 2000 and June 2010 for screening of titles and abstracts. Of the 1201 studies, 92 trials were deemed potentially eligible and retrieved for full text review. Of these studies, 72 were included for final review (Fig. 1).
Fig. 1.
Systematic search strategy for article inclusion. RCT = randomized controlled trial.
Study characteristics
The majority of studies were conducted in Europe (79%) and involved a single centre (65%). Sample sizes ranged from 19 to 569 patients. An equivalent number of studies assessed the management of femoral neck fractures (n = 36) and intertrochanteric fractures (n = 36). More than half (51%) of the studies compared methods of internal fixation, 22% compared methods of arthroplasty, and 15% compared arthroplasty to internal fixation. Studies reported significant findings 18% of the time (Table 1).
Table 1.
Characteristics of RCTs
| Characteristic | Studies, no. (%) |
|---|---|
| Geographical location | |
| Europe | 57 (79) |
| North America | 5 (7) |
| East Asia | 5 (7) |
| South Asia | 3 (4) |
| Other | 2 (3) |
| No. of centres | |
| Single centre | 47 (65) |
| Multicentre | 16 (22) |
| Not reported | 9 (13) |
| Sample size | |
| < 50 | 10 (14) |
| 50–100 | 21 (29) |
| 100–150 | 19 (26) |
| > 150 | 22 (31) |
| Type of fracture | |
| Femoral head | 0 |
| Femoral neck | 36 (50) |
| Intertrochanteric | 36 (50) |
| Type of treatment | |
| IF v. IF | 37 (51) |
| Arthroplasty | 16 (22) |
| HA v. HA | 11 (15) |
| THA v. HA | 3 (4) |
| THA v. THA | 2 (3) |
| Arthroplasty v. IF | 11 (15) |
| Other | 8 (11) |
| Significance of results | |
| Significant | 13 (18) |
| Not significant | 14 (19) |
| Mixed | 45 (63) |
HA = hip arthroplasty; IF = internal fixation; RCT = randomized controlled trial; THA = total hip arthroplasty.
Inclusion of patients with dementia
Among the 72 RCTs included in this review, 19 studies included both cognitively intact and impaired patients, and 1 of these studies reported dementia or cognitive impairment as the focus of the paper.
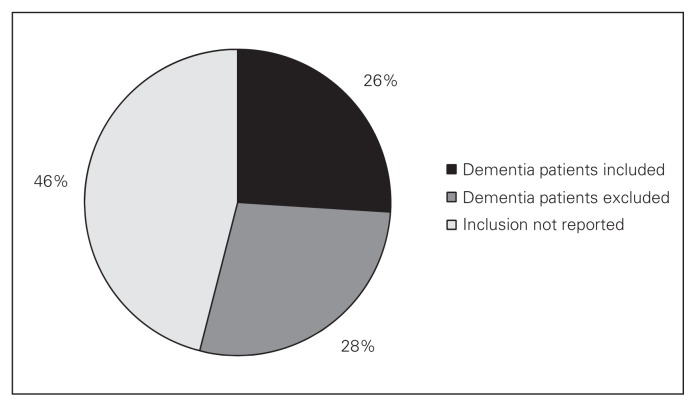
Nineteen studies (26%) explicitly included patients with cognitive impairment and 20 studies (28%) explicitly excluded such patients, as stated in their methodology or as evident in the paper. None of the RCTs that reported inclusion of cognitively impaired patients were from North American centres. There were no significant differences between RCTs that included or excluded these patients in terms of patient age, number of centres, or operative procedures compared. Of the 19 studies that included this patient population, 10 specified dementia as the form of cognitive impairment, whereas the remaining 9 did not. Thirty-three studies (46%) failed to report the inclusion or exclusion of patients with cognitive impairment from their trials (Fig. 2 and Table 2).
Fig. 2.
Proportion of studies including, excluding, and not reporting patients with cognitive impairment or dementia.
Table 2.
Inclusion and exclusion by study characteristics
| Characteristic | Group; no. | p value | ||
|---|---|---|---|---|
| Dementia patients included | Dementia patients excluded | Not reported | ||
| Geographical location | ||||
| Europe | 19 | 15 | 23 | 0.020 |
| North America | 0 | 4 | 1 | 0.040 |
| East Asia | 0 | 1 | 4 | 0.32 |
| South Asia | 0 | 0 | 3 | > 0.99 |
| Other | 0 | 0 | 2 | > 0.99 |
| Type of fracture | ||||
| Neck | 10 | 14 | 12 | 0.27 |
| Intertrochanteric | 9 | 6 | 21 | 0.27 |
| Operative intervention | ||||
| IF v. IF | 11 | 6 | 20 | 0.08 |
| Arthroplasty v. arthroplasty | 2 | 6 | 8 | 0.13 |
| Arthroplasty v. IF | 5 | 5 | 1 | 0.93 |
| Other | 1 | 3 | 4 | 0.32 |
| Results | ||||
| Significant | 5 | 4 | 4 | 0.64 |
| Not significant | 4 | 3 | 7 | 0.62 |
| Mixed | 10 | 13 | 22 | 0.43 |
IF = internal fixation.
Fourteen of 72 trials (19.4%) reported the use of a validated cognitive assessment tool. This included formal tests, such as the Mini-Mental State Exam (MMSE). A single additional trial used a cognitive assessment tool that was not validated.
Of the 19 studies including patients with cognitive impairment, only 2 studies highlighted outcomes of this population. The first study tested surgical interventions in cognitively impaired patients only, while the second conducted a subgroup analysis on this population. With respect to the 20 studies excluding patients with cognitive impairment, only 6 (30%) attempted to provide a rationale within the published manuscript for the exclusion of such patients. Reasons were the patients’ inability to provide informed consent (1 study) and the aim of evaluating outcomes in an active or a mentally competent subpopulation (5 studies).
Discussion
Our systematic review evaluated 72 RCTs in an attempt to delineate the degree to which patients with cognitive impairment and dementia are being incorporated into orthopedic trials on hip fracture management. Our results indicate that patients with cognitive impairment are seldom included (26%) and are rarely the focus (1%) of RCTs evaluating operative hip fracture management. Furthermore, validated screening tools for cognitive impairment are rarely used in those studies that purport to explicitly include or exclude these patients. Finally, we were able to identify only 2 trials that evaluated interventions specifically for patients with cognitive impairment. One of these studies included only patients with cognitive impairment, while another conducted a subgroup analysis for this patient population.10,16
Previous literature has provided contrasting results. In a systematic review of 17 RCTs conducted over a period of 20 years, Herbert-Davies17 and colleagues found that 13 (76%) RCTs explicitly included patients with dementia, while 4 (24%) explicitly excluded this patient population. A possible explanation for this discrepancy is that the authors evaluated only RCTs that reported sufficient data on the number of patients with dementia. Studies offering a quantitative description of patients with dementia are certainly more likely to include such patients. Our review was more comprehensive to the extent that our analysis was based solely upon reporting of inclusion and exclusion status, irrespective of further quantitative reporting.
An assumption that outcomes are similar in patients with and without cognitive impairment is not supported by the evidence. For instance, Panula and colleagues11 reviewed the charts of 428 hip fracture patients in a Finnish hospital registry and correlated these to the official cause of death statistics in Finland. The investigators found that patients with dementia who sustained hip fractures had a more than 3-fold increased risk of death than those with dementia in the general population. Similarly, in a chart review of 495 hip fracture patients in the United States, Bentler and colleagues18 demonstrated that patients with dementia were 45% more likely to die postinjury than patients without dementia.
Some early evidence indicates that patients with cognitive impairment may actually have different intervention-specific outcomes as well. An RCT performed by Johannson and colleagues10 comparing total hip arthroplasty to internal fixation for hip fracture demonstrated an inversion of outcomes among hip fracture patients with cognitive impairment. Specifically, the investigators found a 5% reoperation rate with internal fixation and a 32% dislocation rate after arthroplasty in patients with cognitive impairment. This pattern was reversed in cognitively intact patients, who experienced a 60% reoperation rate after internal fixation and a 12% dislocation rate after arthroplasty.10 Purposly studying patients with cognitive impairment would help identify such differences, thereby better informing orthopedic practice.
Limitations
Our study has several strengths. As mentioned, we used a systematic search strategy to identify eligible studies and applied this search across 3 medical databases to collect a large sample of 72 RCTs. Two reviewers extracted all data independently and in duplicate. We were able to capture a broad range of studies with respect to geographic location, type of hip fracture and operative intervention. Unfortunately, our study did have the limitation of excluding 8 potentially relevant articles owing to inaccessibility. Given our large sample size and the findings of our study, it is unlikely that the inclusion of such studies would have substantially altered our results.
Conclusion
The ambiguity and outright exclusion of patients with cognitive impairment in RCTs challenges the apparent external validity of these trials. The selection of certain primary outcomes, such as patient-reported questionnaires, may necessarily preclude inclusion of patients with cognitive impairment in an RCT. However, given the size of this subpopulation, we believe that exclusion without explanation is no longer acceptable. We propose a “call for inclusion” of patients with cognitive dysfunction to identify interventions that improve survival and function in this patient population.
Footnotes
Poster presented at the Canadian Orthopaedic Residents Association annual meeting, the Canadian Orthopaedic Association annual meeting and the Orthopaedic Trauma Association (OTA) annual meeting.
Competing interests: None declared.
Contributors: All authors designed the study. S. Mundi and H. Chaudhry acquired the data, which all authors analyzed, S. Mundi and H. Chaudhry wrote the article, which M. Bhandari reviewed. All authors approved the final version for publication.
References
- 1.Schemitsch E, Bhandari M. Femoral neck fractures: controversies and evidence. J Orthop Trauma. 2009;23:385. doi: 10.1097/BOT.0b013e3181acc51f. [DOI] [PubMed] [Google Scholar]
- 2.Cooper C, Campion G, Melton LJ. Hip fractures in the elderly: a world-wide projection. Osteoporos Int. 1992;2:285–9. doi: 10.1007/BF01623184. [DOI] [PubMed] [Google Scholar]
- 3.Stenvall M, Berggren M, Lundstrom M, et al. A multidisciplinary intervention program improved the outcome after hip fracture for people with dementia — subgroup analyses of a randomized controlled trial. Arch Gerontol Geriatr. 2012;54:e284–9. doi: 10.1016/j.archger.2011.08.013. [DOI] [PubMed] [Google Scholar]
- 4.Lundström M, Olofsson B, Stenvall M, et al. Postoperative delirium in old patients with femoral neck fracture: a randomized intervention study. Aging Clin Exp Res. 2007;19:178–86. doi: 10.1007/BF03324687. [DOI] [PubMed] [Google Scholar]
- 5.Juliebø V, Krogseth M, Skovlund E, et al. Delirium is not associated with mortality in elderly hip fracture patients. Dement Geriatr Cogn Disord. 2010;30:112–20. doi: 10.1159/000318819. [DOI] [PubMed] [Google Scholar]
- 6.Samuelsson B, Hedstrom MI, Ponzer S, et al. Gender difference and cognitive aspects on functional outcome after hip fracture — a 2 years’ follow up of 2,134 patients. Age Ageing. 2009;38:686–92. doi: 10.1093/ageing/afp169. [DOI] [PubMed] [Google Scholar]
- 7.Givens JL, Sanft TB, Marcantonio ER. Functional recovery after hip fracture: the combined effects of depressive symptoms, cognitive impairment, and delirium. J Am Geriatr Soc. 2008;56:1075–9. doi: 10.1111/j.1532-5415.2008.01711.x. [DOI] [PubMed] [Google Scholar]
- 8.Rogmark C, Johnell O. Primary arthroplasty is better than internal fixation of displaced femoral neck fractures: a meta-analysis of 14 randomized studies with 2,289 patients. Acta Orthop. 2006;77:359–67. doi: 10.1080/17453670610046262. [DOI] [PubMed] [Google Scholar]
- 9.Clayer MT, Bauze RJ. Morbidity and mortality following fractures of the femoral neck and trochanteric region: analysis of risk factors. J Trauma. 1989;29:1673–8. doi: 10.1097/00005373-198912000-00016. [DOI] [PubMed] [Google Scholar]
- 10.Johansson T, Jacobsson SA, Ivarsson I, et al. Internal fixation versus total hip arthroplasty in the treatment of displaced femoral neck fractures. Acta Orthop Scand. 2000;71:597–602. doi: 10.1080/000164700317362235. [DOI] [PubMed] [Google Scholar]
- 11.Panula J, Pihlajamaki H, Mattila VM, et al. Mortality and cause of death in hip fracture patients ages 65 or older — a population-based study. BMC Musculoskelet Disord. 2011;12:105. doi: 10.1186/1471-2474-12-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Huusko TM, Karppi P, Avikainen V, et al. Randomised, clinically controlled trial of intensive geriatric rehabilitation in patients with hip fracture: subgroup analysis of patients with dementia. BMJ. 2000;321:1107–11. doi: 10.1136/bmj.321.7269.1107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kyo T, Takaoka K, Ono K. Femoral neck fracture. Factors related to ambulation and prognosis. Clin Orthop Relat Res. 1993;(292):215–22. [PubMed] [Google Scholar]
- 14.Lieberman D, Fried V, Castel H, et al. Factors related to successful rehabilitation after hip fracture: a casecontrol study. Disabil Rehabil. 1996;18:224–30. doi: 10.3109/09638289609166305. [DOI] [PubMed] [Google Scholar]
- 15.Nightingale S, Holmes J, Mason J, et al. Psychiatric illness and mortality after hip fracture. Lancet. 2001;357:1264–5. doi: 10.1016/S0140-6736(00)04421-4. [DOI] [PubMed] [Google Scholar]
- 16.Blomfeldt R, Tornkvist H, Ponzer S, et al. Internal fixation versus hemiarthroplasty for displaced fractures of the femoral neck in elderly patients with severe cognitive impairment. J Bone Joint Surg Br. 2005;87:523–9. doi: 10.1302/0301-620X.87B4.15764. [DOI] [PubMed] [Google Scholar]
- 17.Hebert-Davies J, Laflamme GY, Rouleau D, et al. Bias towards dementia: Are hip fracture trials excluding to many patients? A systematic review. Injury. 2012;43:1978–84. doi: 10.1016/j.injury.2012.08.061. [DOI] [PubMed] [Google Scholar]
- 18.Bentler SE, Liu L, Obrizan M, et al. The aftermath of hip fracture: discharge placement, functional status change, and mortality. Am J Epidemiol. 2009;170:1290–9. doi: 10.1093/aje/kwp266. [DOI] [PMC free article] [PubMed] [Google Scholar]