Abstract
Background:
Localized gingival recession can be treated successfully via coronally positioned flap (CPF) and additional use of root surface demineralization agents. The purpose of this study was to evaluate the effects of additional use of ethylene diamine tetraacetic acid (EDTA) and citric acid as a root conditioner in association with CPF to cover localized buccal gingival recessions.
Materials and Methods:
Twenty-seven patients with 66 Miller class I buccal gingival recession ≥ 2 mm on single-rooted teeth were studied. Patients were randomly assigned: CPF with EDTA gel (test 1) and CPF with saturated citric acid (test 2) or CPF alone (control). Clinical parameters were measured at baseline and 1, 2, 3 and 6 months after surgery; assessment included recession depth (RD), clinical attachment level (CAL), probing depth (PD) and height of keratinized gingiva (HKG). SPSS version-20 was used to perform all statistical analyses. Data was reported as Mean ± SD. Age, RD, CAL, PD, and HKG before treatment and after 6 months among study groups were compared by one-way ANOVA followed by the Tukey test. The level of significance was considered to be less than 0.05.
Results:
At 6 months, all treatment modalities showed significant root coverage and gain in CAL. RD was reduced from 2.86 ± 0.76 mm to 0.55±0.53 mm in the EDTA group and from 2.37±0.57 mm to 1.03±0.43 mm in the acid group and from 2.37±0.54 mm to 0.85±0.49 mm in the control group. The average percentage of root coverage for the EDTA, acid, and control groups were 80.73%, 52.16%, and 64.50%, respectively. At 6 months, there was a significant difference (P < 0.05) in all parameters for the EDTA group (except HKG that did not vary among the groups).
Conclusion:
Root preparation with EDTA was an effective procedure to cover localized gingival recessions and significantly improved the amount of root coverage obtained.
Keywords: Citric acid, EDTA, gingival recession, periodontal plastic surgery, root coverage
INTRODUCTION
Marginal gingival recession is not an uncommon feature in almost all populations regardless of oral hygiene.[1,2,3,4,5] Covering exposed root surfaces are indicated mainly in subjects with esthetic demands, root sensitivity, and cervical caries.[1] An important and integral part of periodontal plastic surgery is root coverage procedures. There are two main groups of surgical procedures: Free graft and pedicle flap. All free-graft procedures require a donor site and result in an additional wound site and discomfort for the patient while pedicle flaps without tissue grafts do not require harvesting the graft from a donor site and have been used for root coverage successfully.[6] One of the predictable techniques for recession coverage is the coronally positioned flap (CPF). It is a relatively easy procedure for the clinician and patient, with satisfactory esthetic results without the need for a second surgical site.[1,7,8] Despite the positive results reported by all root coverage procedures, surgical techniques using particular subepithelialized connective tissue graft and matrix graft should be considered as the first and second choice procedures, respectively, when complete root coverage is the desired outcome.[9] The reported range of root coverage with CPF is 70-99% with a mean of 83%.[1] The additional use of demineralized agents of varying PH as an adjunct to root coverage procedures has been recommended in order to remove the smear layer and bacterial toxins,[10] to expose collagen fibers on the dentin surface,[11] facilitate cell migration and retard epithelial downgrowth.[12,13]
Several controlled clinical trials comparing the effects of different surgical techniques with and without use of citric acid did not show any beneficial clinical effect from the use of citric acid.[14,15,16] Some studies comparing the effects of etching agents operating at neutral PH (PH = 7) such as ethylene diamine tetraacetic acid (EDTA) and agents operating at low PH such as citric acid (PH = 1) demonstrated improved healing following etching with EDTA in comparison to controls with no etching or citric acid etching.[10,11,16] EDTA root treatment may facilitate the formation and adherence of the blood clot to the root surface, whilst maintaining the vitality of the surrounding periodontium.[10,11,16] In contrast, low PH agents may dissolve and alter the collagenous fibrillar surface resulting in a granulated rather than fibrous dentin surface.[12,17,18,19,20]
The aim of the present study was to compare the clinical efficacy of CPF procedure with and without the additional use of root surface demineralization agents of varying PH (EDTA, 24%, PH = 7and citric acid PH = 1) in treatment of recession type defects.
MATERIALS AND METHODS
This randomized controlled trial was performed on 27 systemically healthy and non–smoking patients who were referred to the Department of Periodontology, School of Dentistry, Tehran Azad University, for treatment of buccal recession type defects. Patients of any age in both gender were eligible if they had at least one Miller class I[21] buccal gingival recession ≥ 2 mm, single-rooted teeth, at least 2-mm keratinized tissues, a good occlusal relationship, and no caries or cervical restorations. Exclusion criteria included sites with probing depths (PDs) > 3 mm, poor oral hygiene (O’leary plaque index ≥ 20%),[22] systemic illness, compromised immune systems, pregnancy, taking any drug known to cause gingival enlargement. Also, patients allergic or sensitive to any medication or those who had contraindications for periodontal surgery were excluded from the study. The present study was assessed and approved by the Ethical Committee of the Islamic Azad University of Tehran, and written informed consent was obtained from all patients.
Twenty-seven eligible patients with 66 gingival recessions fulfilled the 6-month examination. Following selection, all patients received plaque control instruction and professional tooth cleansing on all tooth surfaces. In each patient, tooth or teeth with areas of gingival recession was randomly assigned into three groups (group I and II) of test and control, using random-maker software “Random Allocation.” Two test groups received surgical treatment modalities consisted of recession coverage by CPF technique with additional application of demineralization agents either EDTA gel or citric acid on the denuded root surfaces. The control (group III) teeth were treated similarly but without additional application of any root conditioner.
After local anesthesia, an intrasulcular incision was made with a-15C surgical blade on the buccal aspect of the involved tooth. The adjacent papillae were only partially involved to preserve soft tissue and to leave the buccal gingival margin of the adjacent teeth intact. A frenum pull (when present) was eliminated before surgery. Two oblique releasing incisions were made from the mesial and distal extremities of the intrasulcular buccal incision beyond the mucogingival junction. The interdental papillae were preserved as much as possible (facial portion was de-epithelialized to create a connective tissue bed). The full-thickness trapezoidal flap exposed the marginal bone of the dehiscence on the root surface ≥ 3 mm [Figures 1a-c].
Figure 1.
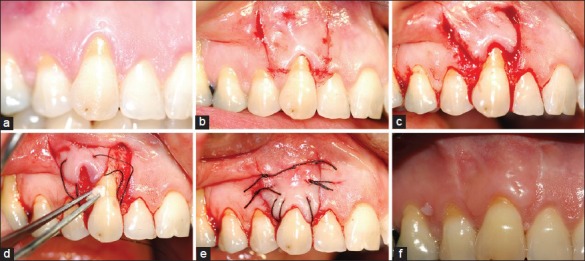
(a) Right maxillary cuspid treated with the EDTA gel (preoperative view); (b) Oblique incisions; (c) Raising a trapezoidal full-thickness flap; (d) EDTA application to the exposed root; (e) The flap sutured in the new coronal position; (f) Healing 6 months post-surgery
The exposed root surface was planned using hand instruments. A horizontal releasing incision was made in the periosteum at the base of the flap to allow for a tension – free coronal flap. The root surface in the EDTA group was conditioned with EDTA gel (24% PH = 7)[23] with rubbing technique[23,24] using a cotton pellet for 3 min. The cotton pellet was changed approximately every 30 s followed by copious irrigation with sterile saline [Figure 1d].
In the acid group, the roots were treated with citric acid using a cotton pellet soaked in aqueous solution of citric acid (PH = 1 supersaturated) for 20 s[10] and followed by copious irrigation with sterile saline [Figure 2a].
Figure 2.
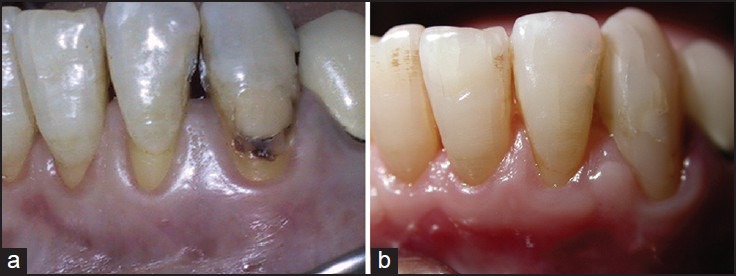
(a) Left mandibular lateral incisor treated with the citric acid (preoperative view); (b) The 6-month result
The coronally advanced flap was secured at the level of the cementoenamel junction (CEJ) by suturing to the de-epithelialized papillae using 4-0 silk sutures and a single-sling suturing technique. Interrupted sutures were then used for releasing incisions [Figure 1e]. The same surgical procedure was performed for recessions in controls with the exception of not applying any root conditioner on the root surfaces [Figure 3a].
Figure 3.
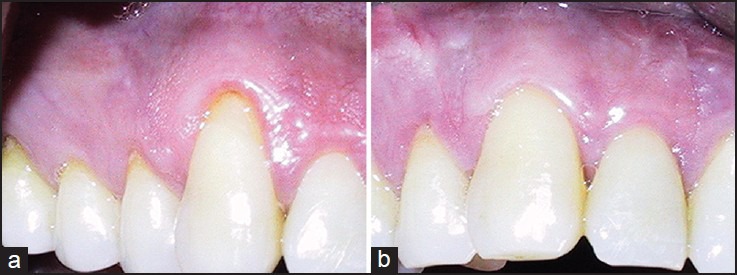
(a) Right maxillary cuspid as control case (preoperative view); (b) The 6-month result
Patients were instructed to discontinue tooth brushing for 1 week and flossing for the first 4 weeks in the treated areas to avoid trauma around the surgical site, to rinse twice daily with 0.2% chlorhexidine digluconate solution (for 45 s), and to use modified Stillman brush technique. Sutures were removed 10 days following surgery. All patients were seen at 1, 2, 3, and 6 months post-surgery to monitor their oral hygiene condition. At these visits, all measurements and clinical photographs were obtained and oral hygiene instructions were reviewed by a single examiner who was different from the surgeon and, if needed, prophylaxis were performed [Figures 1f, 2b, and 3b]. Surgeon, clinical examiner, and patients were unaware of the group conditions of each patient.
All measurements and photographs were done by a single examiner. Patients were called for measurement and photographic documentation pre-surgically and 1, 2, 3, and 6 months post-operatively. Measurements were made using a periodontal probe and rounded off to the nearest millimeter. At baseline and 1, 2, 3, and 6 months after surgical treatment, the following parameters were recorded: Recession depth (RD) was measured at the point of the deepest recession from the CEJ to the gingival margin.[25] PD was the distance to which an ad hoc instrument (probe) penetrates into the pocket.[25] Clinical attachment level (CAL) was the distance from the CEJ to the base of the pocket and was calculated by combining PD and RD measurements.[25] Height of keratinized gingiva (HKG) was measured from the gingival margin to the mucogingival junction at the same point as the RD.[25] Plaque score was recorded using the plaque control record (PCR) (O’leary plaque index).[22] The surgical treatment for each patient was done only when the PCR reached was below 20% [Figure 4].
Figure 4.
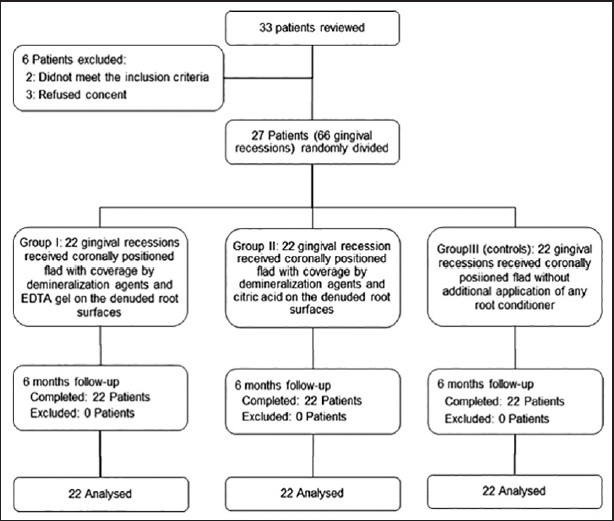
Trail flowchart
SPSS version-20 (Statistical Package for the Social Sciences, SPSS Inc., Chicago, IL, USA) was used to perform all statistical analyses. Data are reported as Mean ± SD and number (percent) as appropriated. Age, RD, CAL, PD, and HKG before treatment and after 6 months among study groups were compared by one-way ANOVA followed by the Tukey test. The level of significance was considered to be less than 0.05.
RESULTS
Figure 4 shows flowchart of study. Of 33 reviewed patients, 6 were not eligible (2 did not meet inclusion criteria and 4 patients refused informed consent) and did not enter the study. Finally, 27 patients with 66 gingival recessions in 3 groups completed the study and analyzed. The mean age of the studied patients was 35.3 ± 11 years. Fourteen patients (51.8%) were male and thirteen (48.2%) were female.
Comparison of means of RD among study groups before and 6 months after intervention are summarized in Table 1. As shown, the difference among study groups at baseline was not significant. Six months later, no significant differences were noted between controls with test groups, but in group I RD was significantly lower than group II. RD changes were statistically different between group I and two other groups but RD change was not statistically different between group II and control group. Percentage of root coverage in group I was significantly higher than in groups II and III, but there was no significant difference between groups II and III. The clinical results of a representative case are shown in Figures 1e, 2b, and 3b.
Table 1.
Recession depth during trial period in studied groups
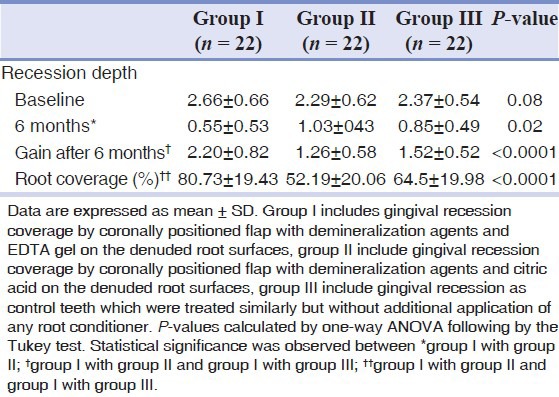
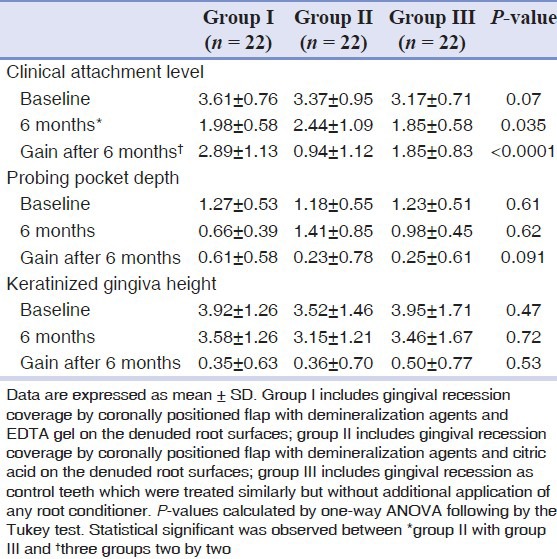
Table 2 shows the clinical variables at baseline and 6 months after treatment. Differences in the mean of CAL, PPD, and HKG among study groups at baseline were not statistically significant. CAL 6 months after treatment and gain after 6 months among the three groups was significant. PPD and HKG among the study groups 6 months after treatment and gain after 6 months were not statistically significant.
Table 2.
Clinical variables at baseline and at postoperative intervals after coronally positioned flap in studied groups
DISCUSSION
The results of the present study showed that all treatment modalities (EDTA + CPF, citric acid + CPF, and CPF alone) can produce significant improvements in the studied clinical parameters with respect to baseline. Also, our results demonstrated that there was a significant difference for RD between the EDTA and acid group and also between the EDTA and control group.
Several studies have compared the effect of Emdogain (EMD) and EDTA gel and CPF for covering exposed root surfaces; controversial results have been reported. Pilloni et al.[26] and Castellanous et al.[27] showed that topical application of EMD and EDTA are beneficial in augmenting the effects of the CPF in terms of the amount of root coverage gained. Hagewald et al.[6] and Modica et al.[28] reported that additional use of EMD and EDTA, together with CPF technique for recession coverage showed no significant difference in overall clinical outcome. Several possible reasons may explain these controversies such as differences in methodology, duration of the study, and also data variability.
In the present study, the relative values for root coverage expressed as a percentage after 6 months in the EDTA group showed it to be superior. Hagewald et al.[6] reported that the mean values for treatment success in the two treatment groups were 80% for experimental sites and 79% for control sites.
In this study, while there was a significant difference between the EDTA and acid group for gingival recession coverage (80.13% vs. 52.6%), no statistically significant differences for gingival recession coverage were found between the acid and control group. The relative values expressed as a percentage after 6 months for the acid and control group were 52.16% and 64.5%, respectively, and the absolute values of the change expressed in millimeter were also similar. Thus, there is no additional benefit for citric acid application on root surfaces for root coverage. This is in accordance with some other studies[14,15] and suggests that, low PH etching agents such as citric acid exerts an immediate (within 20 s) necrotizing effect on both mucosal flaps and periodontal tissue. This is in sharp contrast to EDTA gel which operates at neutral PH. EDTA gel did not induce any detectable necrosis during the experimental period.[10,11] Thus, the superficial necrotizing effect on exposed periodontal tissues by citric acid in the present study may have restricted the healing potential of these tissues while etching at neutral PH (EDTA gel) may be argued to enhanced periodontal healing by inducing less adverse effects and consequently making full use of the healing potential of surrounding periodontal tissues.[11,16]
The CAL was improved by reduction of RD and PPD in the EDTA and control group after 6 months. This is in accordance with other studies[10,29,30] and suggests that recession coverage by CPF procedure does not result in pocket formation but in tissue attachment on the previously exposed root surface; to facilitate this tissue attachment it has been advocated to condition the root surfaces with agents with a neutral PH. These agents such as EDTA gel 24% may be able to produce a biocompatible surface more conductive to periodontal membrane cell colonization after removal of root surface smear without compromising the vitality of the surrounding periodontium.[10,11,13]
On the other hand, acidic etching agents such as citric acid (PH = 1) was able to dissolves the mineral component of the roots and erodes the collagenous matrix[23] and may not only be unable to produce additional new attachment[16] but may also exert an immediate necrotizing effect on the periodontium.[10,11]
The clinical significance of attached gingival width is questionable, as the dimensions of the keratinized tissue are not related to the health and stability of the gingival tissues.[31,32,33] Wennstrom and Zucchelli suggested that tooth brushing habits may be of greater importance for maintenance of the surgically established position of the gingival margin.[8]
Short follow-up duration was one of the limitations of the present study. Long-term clinical studies are needed to evaluate the long-term clinical effects of the application of EDTA gel 24% and the stability of the results achieved. Another limitation was lack of a histological evaluation. From a histologic point of view, one cannot draw conclusions regarding the type of attachment that was gained based on clinical measurements.
CONCLUSION
In conclusion, our results demonstrated that root preparation with EDTA is an effective procedure to cover localized gingival recessions; use of EDTA significantly improved the amount of root coverage obtained; Long-term clinical studies are needed to evaluate the long-term clinical effects and stability of the results achieved.
Footnotes
Source of Support: Nil
Conflict of Interest: Nil
REFERENCES
- 1.Wennstrom JL, Zucchelli G, Pini Prato GP. Mucogingival therapy — Periodontal plastic surgery. In: Lang NP, Lindhe J, editors. Clinical Periodontology and Implant Dentistry. 5th ed. Oxford: Blackwell Munksgaard; 2008. pp. 958–71. [Google Scholar]
- 2.Serino G, Wennstrom JL, Lindhe J, Eneroth L. The prevalence and distribution of gingival recession in subjects with high standard of oral hygiene. J Clin Periodontol. 1994;21:57–63. doi: 10.1111/j.1600-051x.1994.tb00278.x. [DOI] [PubMed] [Google Scholar]
- 3.Kallestal C, Matsson L, Holm A-K. Periodontal conditions in a group of Swedish adolescents. I. A descriptive epidemiologic study. J Clin Periodontol. 1990;17:601–8. [PubMed] [Google Scholar]
- 4.Baelum V, Fejerskov O, Karring T. Oral hygiene, gingivitis and periodontal breakdown in adult Tanzanians. J Periodont Res. 1986;21:221–32. doi: 10.1111/j.1600-0765.1986.tb01454.x. [DOI] [PubMed] [Google Scholar]
- 5.Yoneyama T, Okamoto H, Lindhe J, Socransky SS, Haffajee AD. Probing depth, attachment loss and gingival recession. Findings from a clinical examination in Ushiko, Japan. J Clin Periodontol. 1988;15:581–91. doi: 10.1111/j.1600-051x.1988.tb02133.x. [DOI] [PubMed] [Google Scholar]
- 6.Hagewald S, Spahr A, Rompola E, Haller B, Heijl L, Bernimoulin JP. Comparative study of Emdogain and coronally advanced flap technique in the treatment of human gingival recessions. A prospective controlled clinical study. J Clin Periodontol. 2002;29:35–41. doi: 10.1034/j.1600-051x.2002.290106.x. [DOI] [PubMed] [Google Scholar]
- 7.Matter J. Free gingival graft and coronally repositioned flap. A 2-year follow-up report. J Clin Periodontol. 1979;6:437–42. doi: 10.1111/j.1600-051x.1979.tb01942.x. [DOI] [PubMed] [Google Scholar]
- 8.Wennstrom J, Zucchelli G. Increased gingival dimensions. A significant factor for successful outcome of root coverage procedures? A 2-year prospective clinical study. J Clin Periodontol. 1996;23:770–7. doi: 10.1111/j.1600-051x.1996.tb00608.x. [DOI] [PubMed] [Google Scholar]
- 9.Leandro Chambrone, Claudio Mendes Pannuti, Yu-Kang Tu, Luiz Armando Chambrone. Evidence-based periodontal plastic surgery II. An individual data analysis for evaluating factors in achieving complete root coverage. J Periodontol. 2012;83:477–90. doi: 10.1902/jop.2011.110382. [DOI] [PubMed] [Google Scholar]
- 10.Blomlof J, Jansson, Blomlof L, Lindskog S. Long-time etching at low PH jeopardizes periodontal healing. J Clin Periodontol. 1995;22:459–63. doi: 10.1111/j.1600-051x.1995.tb00177.x. [DOI] [PubMed] [Google Scholar]
- 11.Blomlof J, Lindskog S. Periodontal tissue-vitality after different etching modalities. J Clin Periodontol. 1995;22:464–8. [PubMed] [Google Scholar]
- 12.Polson AM, Proye MP. Effect of root surface alteration on periodontal healing. II. Citric acid treatment of the denuded root. J Clin Periodontol. 1982;9:441–54. doi: 10.1111/j.1600-051x.1982.tb02105.x. [DOI] [PubMed] [Google Scholar]
- 13.Blomlof J. Root cementum appearance in healthy monkeys and periodontitis-prone patients after different etching modalities. J Clin Periodontol. 1996;23:12–18. doi: 10.1111/j.1600-051x.1996.tb00498.x. [DOI] [PubMed] [Google Scholar]
- 14.Liu WJ-L, Solt CH. A surgical procedure for the treatment of localized gingival recession in conjunction with root surface citric acid conditioning. J Periodontol. 1980;51:505–9. doi: 10.1902/jop.1980.51.9.505. [DOI] [PubMed] [Google Scholar]
- 15.Ibbott CG, Oles RD, Laverty WH. Effects of citric acid treatment on autogenous free graft coverage of localized recession. J Periodontol. 1985;56:662–5. doi: 10.1902/jop.1985.56.11.662. [DOI] [PubMed] [Google Scholar]
- 16.Blomlof J, Jansson L, Blomlof L, Lingdskog S. Root surface etching at neutral PH promotes periodontal healing. J Clin Periodontol. 1996;23:50–5. doi: 10.1111/j.1600-051x.1996.tb00504.x. [DOI] [PubMed] [Google Scholar]
- 17.Blomlof J, Blomlof L, Lindskog S. Smear layer formed by different root planing modalities and its removal by an ethylenediaminetetraacetic acid gel preparation. Int J Periodontics Restorative Dent. 1997;17:243–9. [PubMed] [Google Scholar]
- 18.Mayfield L, Soderholm G, Norderyd O, Attstrom R. Root conditioning using EDTA gel as an adjunct to surgical therapy for the treatment of intraosseous periodontal defects. J Clin Periodontol. 1998;25:707–14. doi: 10.1111/j.1600-051x.1998.tb02511.x. [DOI] [PubMed] [Google Scholar]
- 19.Khoshkhoo Nejad AA, Shariatmadar Ahmadi R, Jannatt B. A comparative study on EDTA and coronally advanced flap technique in the treatment of human gingival recessions. jdm. 2003;16:5–13. [Google Scholar]
- 20.Shariatmadar Ahmadi R, Ghasemi Z, Mani Kashani KH, Gheyratian R. Comparative study of coronally advanced flap technique with and without use of EDTA gel in the treatment of human gingival recession (in Iran) The Journal of Islamic Dental Association of IRAN (JIDA) 2005;17:75–82. [Google Scholar]
- 21.Miller PD. A classification of marginal tissue recession. Int J Periodontics Restorative Dent. 1985;2:9–14. [PubMed] [Google Scholar]
- 22.O’Leary TJ, Drake RB, Naylor JE. The plaque control record. J Periodontol. 1972;43:38. doi: 10.1902/jop.1972.43.1.38. [DOI] [PubMed] [Google Scholar]
- 23.Blomlof J, Blomlof L, Lindskog S. Effect of different concentration of EDTA on smear removal and collagen exposure in periodontitis affected root surfaces. J Clin Periodontol. 1997;24:534–7. doi: 10.1111/j.1600-051x.1997.tb00225.x. [DOI] [PubMed] [Google Scholar]
- 24.Blomlof J, Lindskog S. Root surface texture and early cell and tissue colonization after different etching modalities. Eur J Oral Sci. 1995;103:17–24. doi: 10.1111/j.1600-0722.1995.tb00005.x. [DOI] [PubMed] [Google Scholar]
- 25.Carranza FA, Takei HH. Clinical diagnosis. In: Carranza FA, Newman MG, Takei HH, Klokkevold PR, editors. Carranza's Clinical Periodontology. 11th ed. Philadelphia: Saunders; 2011. pp. 352–3. [Google Scholar]
- 26.Pilloni A, Paolantonio M, Camargo PM. Root coverage with a coronally positional flap used in combination with enamel matrix derivative: 18-month clinical evaluation. J Periodontol. 2006;77:2031–9. doi: 10.1902/jop.2006.050390. [DOI] [PubMed] [Google Scholar]
- 27.Castellanos AT, Del Rasa RM, Del Garza M, Cafesse RG. Enamel matrix derivative and coronal flaps to cover marginal tissue recessions. J Periodontol. 2006;77:7–14. doi: 10.1902/jop.2006.77.1.7. [DOI] [PubMed] [Google Scholar]
- 28.Modica F, Del Pizzo M, Roccuzo M, Romagnoli R. Coronally advanced flap for the treatment of buccal gingival recession with and without enamel matrix derivative. A split-mouth study. J Periodontol. 2000;71:1693–8. doi: 10.1902/jop.2000.71.11.1693. [DOI] [PubMed] [Google Scholar]
- 29.Borghetti A, Gardella JP. Thick gingival autograft for the coverage of gingival recession: a clinical evaluation. Int J Periodontics Restorative Dent. 1990;10:216–29. [PubMed] [Google Scholar]
- 30.Baldi C, Pininprato G, Pagliaro U, Nieri M, Saletta D, Muzzi L, et al. Coronally advanced flap procedure for root coverage. Is flap thickness a relevant predictor to achieve root coverage?A 19-case series. J Periodontol. 1999;70:1077–84. doi: 10.1902/jop.1999.70.9.1077. [DOI] [PubMed] [Google Scholar]
- 31.Miyasato M, Crigger M, Egelberg J. Gingival condition in area of minimal and appreciable width of keratinized gingival. J Clin Periodontol. 1977;4:200–9. doi: 10.1111/j.1600-051x.1977.tb02273.x. [DOI] [PubMed] [Google Scholar]
- 32.Dorfman HS, Kennedy JE, Bird WC. Longitudinal evaluation of free gingival grafts. A four year report. J Periodontol. 1982;53:349–52. doi: 10.1902/jop.1982.53.6.349. [DOI] [PubMed] [Google Scholar]
- 33.Wennstrom JL. Lack of association between width of attached gingiva and development of gingival recession. A 5-year longitudinal study. J Clin Periodontol. 1987;14:181–4. doi: 10.1111/j.1600-051x.1987.tb00964.x. [DOI] [PubMed] [Google Scholar]


