Abstract
This study tested a novel extension of Schnurr and Green’s (2004) model of the relationships between trauma symptoms and health outcomes, with the specific application to HIV-positive men. A diverse sample of 167 HIV-positive men recruited from San Francisco Bay Area HIV Clinics completed demographic, medical, trauma history and symptom questionnaires. Mediation analyses were conducted using the method proposed by Baron and Kenny (1986). Regression analyses found sexual revictimization (SR) significantly mediated the relationship between child sexual abuse (CSA) and peritraumatic dissociation (PD) and PD mediated the relationship between SR and current posttraumatic stress (PTS) symptom severity. PTS symptoms partially mediated the relationship between SR and current HIV symptom severity. The findings indicate that among HIV-positive men, sexually revictimized men constitute a vulnerable group that is prone to peritraumatic dissociation, which places them at risk for posttraumatic stress disorder and worsened HIV-related health. Furthermore, traumatic stress symptoms were associated with worse HIV-related symptoms, suggesting that PTS symptoms mediate the link between trauma and health outcomes. This study highlights the need for future research to identify the bio-behavioral mediators of the PTSD-health relationship in HIV-positive individuals.
Keywords: HIV, Sexual Abuse of Males, Child Sexual Abuse, Revictimization, Dissociation, Posttraumatic Stress Disorder
Since the beginning of the HIV/AIDS epidemic in the United States, men have been disproportionately affected by HIV infection, with recent estimates of HIV prevalence estimating that men account for approximately 73% of new cases (Centers for Disease Control and Prevention [CDC], 2008). Research also suggests that HIV-positive individuals in general are disproportionately affected by traumatic events. One recent study found that more than 90% of HIV-positive men and women reported at least one severe traumatic event in their lifetime (Pence et al., 2007). Estimates of the prevalence of child physical or sexual abuse among HIV-positive individuals typically exceed 50% (Allers & Benjack, 1991; Whetten et al., 2006), a rate significantly higher than in community populations, where reported rates of childhood abuse are closer to 20–33% (Briere & Elliot, 2003). One reason for the increased rates of child and adult trauma among people living with HIV (PLH) is that traumatic events are related to greater HIV risk behavior. In the general population, child sexual abuse (CSA) has been associated with substance abuse, many sexual partners, sexual impulsivity, sex work, and infrequent condom use (Zurbriggen & Freyd, 2004). Specifically among men who have sex with men, a history of CSA is associated with HIV risk behavior and subsequent HIV infection (Lloyd & Operario, 2012). Furthermore, history of CSA has been associated with worse HIV-related medical treatment engagement and medication adherence (Meade et al., 2009). Given these high rates of trauma among PLH, and the high proportion of men affected by HIV, it is important to determine both the psychological sequelae of trauma exposure among adult men living with HIV and the ways in which these sequelae relate to HIV-related health status.
Survivors of CSA who later experience sexual violence in adulthood are said to have been sexually revictimized (Classen, Palesh, & Aggarwal, 2005). Although research on sexual revictimization (SR) among HIV-positive men has been limited, studies have found that men at risk for HIV report greater revictimization rates compared to the general population. In an epidemiological study, 2% of males recruited through a national telephone survey reported CSA and 1% reported adult sexual abuse in the general population (Desai, Arias, Thompson, & Basile, 2002). In contrast, a study among gay and bisexual men at risk for HIV (at risk due to the fact that anal intercourse is a more potent vector of HIV transmission than vaginal sex) found that 22% reported a history of CSA, 20% reported a history of adult sexual trauma, and 7% reported SR (Kalichman et al., 2001). Given the high incidence rates of CSA and SR among HIV-positive men and those at risk for contracting HIV, research addressing potential mechanisms by which CSA and SR may impact the psychological and physical health of HIV-positive men is needed.
PLH who have been sexually revictimized may be particularly vulnerable to more severe psychiatric and behavioral problems. Although no studies have examined this phenomenon among male samples, research on women has found that those reporting SR report greater severity of PTSD and dissociative symptoms (Classen et al., 2005). Dissociative symptoms are among the most common reactions to traumatic stress, and include detachment and emotional numbing (Ross, Joshi, & Currie, 1990). Dissociation has been fundamentally linked to CSA in both the general population (Mulder, Beautrais, Joyce, & Fergusson, 1998) and in a sample of HIV-positive men (Kamen, Bergstrom, Koopman, Lee, & Gore-Felton, 2012). While some research has focused on investigating dissociation (e.g., during sexual activity) as a mediator between CSA and SR (Hansen, Brown, Tsatkin, Zelgowski, & Nightingale, 2012), other research has proposed that SR may be linked to the etiology of peritraumatic dissociation (i.e., dissociation occurring during and in the immediate aftermath of trauma exposure) in response to subsequent traumatic events (Cloitre, Scarvalone, & Difede, 1997; Shearer, 1994; Zlotnick et al., 1996). Sensitization theory provides an explanation for these findings, which states that repeated exposure to a stimulus (i.e., sexual trauma) leads to increased behavioral and physiological responsiveness (i.e., avoidance, hyperarousal) during subsequent exposures (Charney, Deutch, Southwick, & Krystal, 1995). Evidence supporting sensitization theory has been found in studies of rape victims (Resnick et al., 1995). The similarity of adult sexual assault to CSA experiences may trigger PD through respondent conditioning to the characteristics of sexual encounters, which further entrenches a dissociative response. Further investigation of the impact of SR on PD among PLH in needed.
PD has been found to predict later development of posttraumatic stress disorder (PTSD; Lendsvelt-Mulders et al., 2008). PD leads to detachment from the traumatic experience, which impairs the cognitive and affective processing of the event in its aftermath, promoting the development of PTSD (Spiegel & Cardena, 1991). While most research on PD as a risk factor for developing PTSD has been conducted on combat veterans and survivors of accidents, research on survivors of SR are lacking (Lendsvelt-Mulders et al., 2008). PLH who report a history of SR may be more likely to experience PD, and therefore be more vulnerable to developing PTSD.
Exposure to trauma is of interest in the context of men living with HIV, as it has been linked to physical health detriments in diverse populations (Schnurr & Jankowski, 1999). Research suggests that PTSD serves as a mediator between trauma exposure and poor health status, a relationship that forms the backbone of an integrative model of trauma exposure, PTSD, and health (Schnurr & Green, 2004). Empirical studies of PLH have supported this model, which have found that PTSD symptoms are associated with greater pain and fatigue severity, functional impairment, poorer health-related quality of life, increased health care utilization, and HIV disease progression (Barroso et al., 2010; Leserman et al., 2005; O’Cleirigh, Skeer, Mayer, & Safren, 2009; Smith, Egert, Winkel, & Jacobson, 2002). The Schnurr and Green (2004) model proposes that trauma exposure results in PTSD, which in turn leads to alterations in psychological (e.g., depression, anxiety, and dissociation), biological (e.g., hypothalamic-pituitary-adrenal axis dysregulation), attentional (e.g., altered symptom perception), and behavioral (e.g., substance abuse, unprotected sex) factors that mediate poorer health outcomes. In this model, dissociation is conceptualized as a psychological symptom of PTSD. Yet considering the research suggesting that PD is a risk factor for developing PTSD, the prevalence of multiple sexual trauma exposures among PLH, and the possible etiological connection between SR and PD, it appears likely that PD is a mediator of the sexual revictimization-PTSD relationship.
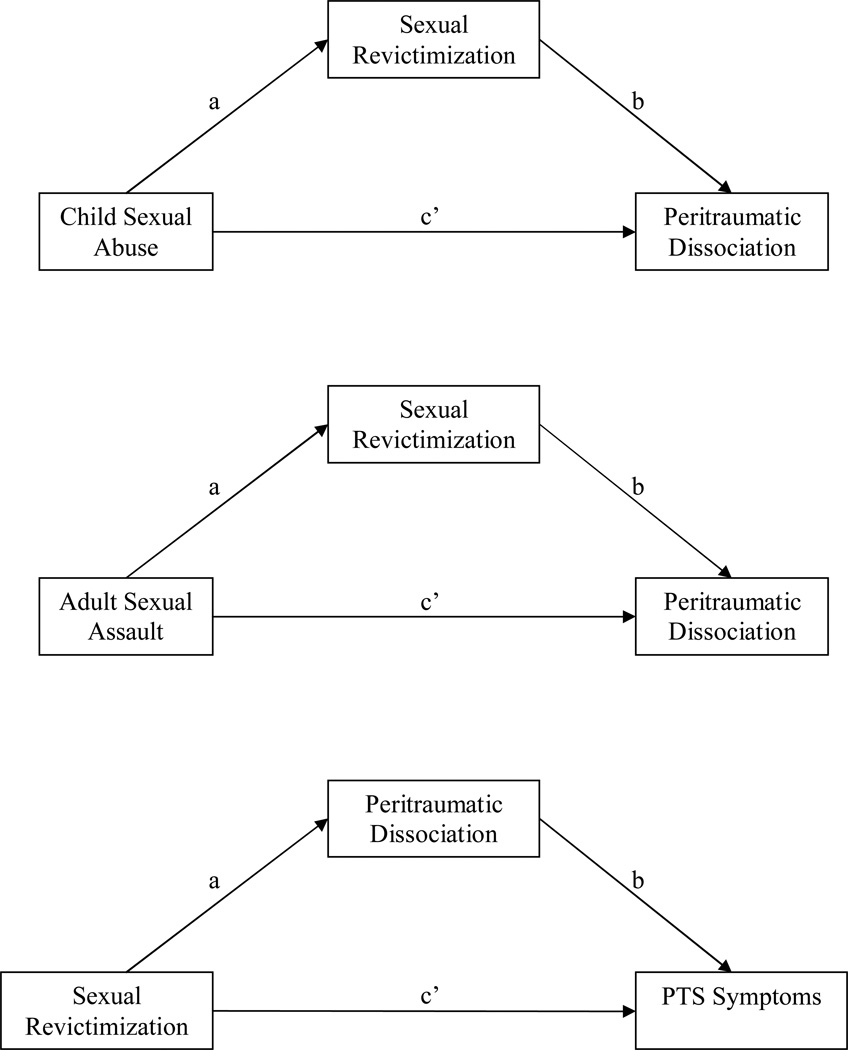
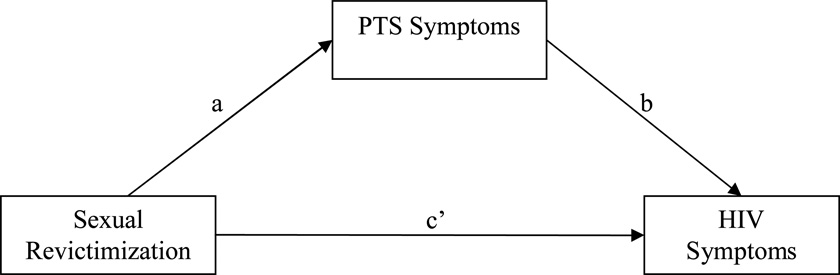
Consequently, in the current study we propose a revision of Schnurr and Green’s (2004) model where PD is a primary mediator between sexual trauma exposure and posttraumatic stress (PTS) symptoms. We examined three key mediators in this model among a sample of HIV-positive men (see Figure 1). We hypothesized that: (a) SR would significantly mediate the relationship between CSA and PD, (b) SR would mediate the relationship between ASA and PD, (c) PD would mediate the relationship between SR and PTS symptoms, (d) and PTS symptom severity would mediate the relationship between SR and HIV symptom severity.
Figure 1.
Hypothesized mediation models being tested (“a” and “b” are hypothesized indirect pathways, and c’ are hypothesized direct pathways).
Method
Participants
A sample of 167 HIV-positive adult men were recruited as part of a larger, randomized clinical trial examining the efficacy of an HIV prevention and stress reduction intervention on reducing HIV transmission risk behavior (Project RISE). Project RISE was approved by the Institutional Review Board at Stanford University. All participants gave written informed consent prior to participating in the study. Participants were recruited from clinics and community based organizations in the San Francisco Bay Area. This study used data from baseline assessments completed before the men were randomized into intervention or wait-list control groups.
The inclusion criteria for the current study were as follows: (a) 18 years or older; (b) HIV-positive; (c) reported engaging in unprotected anal or vaginal sex, sharing needles, or contracting a sexually transmitted infection) in the past 3 months; (d) reported experiencing a traumatic stressor that meets Criterion A1 in the DSM-IV for posttraumatic stress disorder and reported experiencing one or more trauma-related symptoms (i.e., re-experiencing, hyperarousal, or avoidance) in the past 3 months; and (e) could speak/understand English.
Measures
Demographics
The Demographics Questionnaire is a self-report measure that assesses a number of sociodemographic variables, including age, gender, education, income, employment, sexual orientation, relationship history and status.
Child Sexual Abuse
The Trauma History Questionnaire (THQ) assesses participants’ lifetime history of experiencing trauma in the following domains: (a) physical abuse, (b) sexual abuse, (c) domestic violence, (d) natural disasters, (e) sexual assault, and (f) crime victimization (Green, 1996). Each domain includes items asking whether the participant has experienced the event, whether the event occurred repeatedly, and the participant’s age when the event first and most recently happened. The test-retest reliability is fairly high over a several week period (r = 0.6 to 1.0; Green, 1996). In the current study we defined child sexual abuse as experiencing either forced oral/anal intercourse (THQ item 18), unwanted/forced touching of one’s own private parts or of the perpetrator (THQ item 19), or any other unwanted sexual contact (THQ item 20) prior to the age of 16, in keeping with previous research (Wurr & Partridge, 1996). This variable was coded dichotomously (yes/no), where participants who endorsed at least one of items 18, 19, or 20 were coded as “yes.”
Adult Sexual Assault
Adult sexual assault (ASA) is measured by the same items as CSA (THQ items 18, 19, and 20) identified as occurring at age 16 or thereafter. This variable was coded dichotomously (yes/no), where participants who endorsed at least one of items 18, 19, or 20 were coded as “yes.”
Sexual Revictimization
Sexual revictimization (SR) is measured by the THQ and is defined as experiencing both CSA (endorsing THQ items 18, 19, or 20 occurring before age 16) and ASA (endorsing THQ items 18, 19, or 20 occurring at age 16 or thereafter). Thus to meet criteria for SR, a participant would need to meet criteria for both CSA and ASA, as described above.
Peritraumatic Dissociation
The RAND Peritraumatic Dissociative Experiences Questionnaire (PDEQ; Marmar, Weiss, & Metzler, 1997; Marshall et al., 2002) is an 8-item self-report measure of peritraumatic dissociative symptoms experienced during the worst traumatic event previously encountered. Symptoms include depersonalization, derealization, symptoms of amnesia, emotional numbing, reduced awareness, detachment, altered sense of time, and out-of-body experiences. The revised 8-item version was validated in a sample with diverse sociocultural and economic backgrounds (Marshall et al., 2002). Each item measures symptom severity on a Likert-type scale where 1 = “Not at all true,” 2 = “Slightly true,” 3 = “Somewhat true,” 4 = “Very true,” and 5 = “Extremely true.” The PDEQ total score is the mean of the sum of the scores on the 8 items. In the current study, the measure demonstrated strong internal consistency (Cronbach’s alpha = .91).
PTS Symptoms
The Impact of Event Scale – Revised (IES-R; Weiss & Marmar, 1997) is a self-report measure of posttraumatic stress symptom severity experienced in the past one month. The IES-R has re-experiencing, hyperarousal, and avoidance subscales. Each item measures symptom severity on a 5-point, Likert-type scale where 0 = “Not at all,” 1 = “A little bit,” 2 = “Moderately,” 3 = “Quite a bit,” and 4 = “Extremely.” In previous research, the highest power for diagnosing PTSD (.88) was achieved by using a cutoff score of 33 on the IES-R in a recent report of the measure’s psychometrics (Creamer, Bell, & Failla, 2003). This same study also indicated that the IES-R might best be utilized as a total score, summing all 22 items. In the current study, internal consistency for the total scale (Cronbach’s α = .96) was strong.
HIV Symptoms
Total severity of HIV-related symptoms was measured with the HIV Symptom Checklist (Folkman, Chesney, Pollack, & Coates, 1993). The 20-item self-report questionnaire assessed HIV-related symptoms that include pain, fatigue, unintentional weight loss, cold or flu-like symptoms, and neuropathy. Each item measures symptom severity on a 5-point, Likert-type scale where 0 = “Not present,” 1 = “Mild,” 2 = “Moderate,” 3 = “Severe,” and 4 = “Very severe,” and the sum of each item was used to obtain a total score. The HIV Symptom Checklist demonstrated good consistency in the current study (Cronbach’s alpha = .87).
Data Analysis
Data were analyzed using SPSS version 17.0. Univariate statistical analyses were conducted on demographic variables, history of traumatic experiences, and the key study variables of child sexual abuse, sexual revictimization, PD symptoms, PTS symptoms, and HIV symptoms. Bivariate correlations were calculated to identify significant relationships between history of traumatic experiences, peritraumatic dissociation, traumatic stress, and HIV symptoms.
Regression analyses were conducted to test three mediation hypotheses within a conceptual model explaining the relationship between childhood and adult sexual trauma history (CSA and ASA), PD, PTS symptom severity, and HIV-related symptom severity in the past three months. We used the approach described by Baron and Kenny (1986) to test our four mediation hypotheses. First, we examined the potential mediating role of SR in the relationship between CSA/ASA and PD. Since SR was calculated as a composite of the CSA and ASA variables, we conducted separate regression analyses to test whether SR is a mediator of the relationship between (a) CSA and peritraumatic dissociation, and (b) ASA and peritraumatic dissociation. Second, we examined the potential mediating role of PD in the relationship between SR and PTS symptoms. Finally, we examined the potential mediating role of PTS symptoms in the relationship between SR and HIV symptom severity. The Sobel test was used to confirm the significance of all models.
Results
The sample had a mean age of 45 years, ranging from 23 to 67 (SD = 8 years). The majority self-identified as Caucasian (38%), followed by African-American (30%), and Hispanic/Latino (23%). The vast majority of the sample reported being unemployed (83%) and having an annual income of less than $20,000 during the past year (71%). Approximately one-quarter of the sample reported completing high school/GED, 14% reported obtaining an AA degree, and another quarter reported obtaining a college degree. More than half of the sample reported having never been married (64%). Approximately three-fourths of the men reported having sex with men (62% gay, 15% bisexual), and 23% identified as heterosexual. When comparing the demographics of participants reporting CSA, ASA, and SR, it was found that those reporting SR were slightly more likely to be unemployed (chi square = 6.41, p < .05). No other demographics differences were found between the CSA, ASA, and SR groups.
Table 1 summarizes trauma exposure and trauma-related symptom severity measures for the sample. Participants reported experiencing an average of eight (SD = 5) traumatic experiences in their lifetimes, ranging from 0–24 traumas. One-third of the sample reported experiencing any CSA, 11% reported experiencing any adult sexual assault, and 7% reported SR. 82% of people who experienced CSA did not experience ASA, and 63% of people who experienced ASA did not experience CSA. Most (87%) of the sample reported some HIV-related symptoms and 13% reported being completely asymptomatic. 56% of participants scored a 33 or above on the IES-R total score, the recommended cutoff value for a likely diagnosis of PTSD.
Table 1.
Traumatic Stress Experiences and independent variables
| Independent Variable | n | M (SD) | % |
|---|---|---|---|
| Trauma History Questionnaire (total score) Child Sexual Abuse (<16 years old) |
7.90 (4.72) | ||
| Forced vaginal/oral/anal intercourse | 39 | 23.4 | |
| Touched your privates/forced you to touch theirs | 38 | 22.8 | |
| Other unwanted/forced sexual contact | 19 | 11.4 | |
| Any Childhood Sexual Abuse | 57 | 34.1 | |
| Adult Sexual Assault (occurring ≥ 16 years old) | |||
| Forced vaginal/oral/anal intercourse | 19 | 11.4 | |
| Touched your privates/forced you to touch theirs | 11 | 6.6 | |
| Other unwanted/forced sexual contact | 15 | 9.0 | |
| Any Adult Sexual Assault | 32 | 11.2 | |
| Sexual Revictimization | 12 | 7.2 | |
| Peritraumatic Dissociative Experiences Questionnaire (total score) | 2.02 (1.06) | ||
| Impact of Events Scale – Revised (total score) | 35.23 (18.82) | ||
| HIV Symptom Checklist (total score) | 11.70 (9.81) |
Table 2 summarizes bivariate correlations between CSA, ASA, PD, PTS symptom severity, and HIV symptom severity. CSA was not significantly correlated with ASA. Both CSA and ASA were significantly associated with both PD and PTS symptom severity. HIV symptom severity was significantly correlated with ASA, SR, PD, and PTS symptom severity, but not with CSA. PTS symptom severity was significantly correlated with HIV symptom severity (r = .43, p < .01).
Table 2.
Bivariate correlations between traumatic experiences, dissociation, and trauma and HIV symptoms (N = 167)
| 1. | 2 | 3. | 4. | 5. | |
| 1. Child Sexual Abuse | 1 | ||||
| 2. Adult Sexual Assault | .04 | 1 | |||
| 3. Sexual Revictimization | .78** | .65*** | 1 | ||
| 4. Peritraumatic Dissociation | .22** | .22** | .30** | 1 | |
| 5. PTSD Symptoms | .16* | .17* | .23** | .65** | 1 |
| 6. HIV Symptoms | .12 | .23** | .24** | .30** | .43** |
Note:
p < .05;
p < .01
The results of the mediation analyses are summarized in Tables 3–6. In the first analysis, SR was found to mediate the relationship between CSA and PD symptom severity (Beta = .34, p < .05; Sobel test = 2.82, p < .01), and also mediated the relationship between ASA and PD symptom severity (Beta = .28, p < .05; Sobel test = 2.75, p < .01). In the second mediation analysis, PD was found to mediate the relationship between SR and PTS symptom severity (Beta = .63, p <.05; Sobel test = 2.91, p < .01). In the third mediation analysis, PTS symptom severity partially mediated the relationship between SR and HIV symptom severity (Beta = .40, p < .05; Sobel test = 2.77, p < .01), yet SR remained significant in the final regression model (Beta = .15, p < .05).
Table 3.
Regression analyses testing if sexual revictimization (SR) mediates the relationship between child sexual abuse (CSA) and peritraumatic dissociation (PD; N = 167)
| Step | β | R-squared | |
|---|---|---|---|
| 1 | CSA predicting PD | .22* | .05 |
| 2 | CSA predicting SR | .78* | .61 |
| 3 | CSA predicting PD | −.05 | .09 |
| SR predicting PD | .34* |
Note.
p < .05
Table 6.
Regression analyses testing if posttraumatic stress symptoms (PTS symptoms) mediate the relationship between sexual revictimization (SR) and HIV symptoms (N = 167)
| Step | β | R-squared | |
|---|---|---|---|
| 1 | SR predicting HIV symptoms | .24* | .06 |
| 2 | SR predicting PTS symptoms | .23* | .05 |
| 3 | SR predicting HIV symptoms | .15* | .20 |
| PTS symptoms predicting HIV symptoms | 40* |
Note.
p < .05
Discussion
Overall, our statistical analyses supported our study hypotheses. SR was found to mediate the relationship between CSA and PD, and also mediated the relationship between ASA and PD. This suggests that repeated sexual trauma in childhood and adulthood is significantly more associated with the development of PD than either CSA or ASA alone. This supports the theory that SR is related to the etiology of PD. Factors related to this relationship include physiological and respondent learning processes, as proposed by sensitization theory.
We did not expect to find that CSA was not significantly correlated with ASA, as this suggests that childhood trauma was not related to increased likelihood of adult victimization, which is inconsistent with previous research (Classen et al., 2005). This finding may be a result of the way we calculated CSA and ASA. Since we calculated ASA and CSA from the same three variables on the THQ (and differentiated childhood versus adult trauma from the reported age when it occurred), it is possible that participants may not have reported all of the ages when they experienced sexual trauma (i.e., childhood, adult, and/or both).
We did not find that SR was directly associated with PTS symptomatology in our mediation analyses. Interestingly, we did find that PD mediated the relationship between SR and PTS symptom severity. This finding supports the theory that PD is a potent risk factor for the development of PTSD. A history of repeated sexual trauma exposure in childhood and adulthood may represent one of the primary factors associated with the development of a dissociative response to stress, which in turn is associated with subsequent PTSD.
Our finding that PTS symptom severity was strongly associated with HIV symptomatology contributes to the extant literature by demonstrating the mediating role of posttraumatic stress in the trauma-health relationship in an HIV-positive sample. Significant traumatic stress symptoms might worsen HIV-related health through poor health behavior (e.g., poor medication adherence, substance abuse, avoidance of needed medical treatment, etc; Gore-Felton & Koopman, 2008; Keuroghlian et al., 2011). There might also be a physiological explanation such that trauma-related symptoms (i.e., hyperarousal) might increase disease progression through sympathetic nervous system activation (Cole, 2008).
Interestingly, SR remained significantly associated with HIV symptom severity in the final regression model, after the addition of PTS symptom severity. This suggests that PTS symptomatology does not fully mediate the effect of SR on HIV symptom severity. The Schnurr & Green (2004) model suggests a number of possible variables that could account for this finding. These variables could include alterations in attentional processes (e.g., altered symptom perception and mislabeling). Alternatively, there are psychological sequelae of sexual trauma exposure that were not assessed by our measure of PTS symptom severity, such as shame and guilt, that may be associated with worse HIV-related health (Ginzburg et al., 2009). Lastly, SR may lead to physiological changes beyond those associated with PTS severity that contribute to worse HIV-related health.
Limitations
There are a few important limitations to this study. Since the data is cross-sectional, conclusions about causal relationships between PD, PTS symptoms, and HIV symptoms are not possible. Also, because PTS symptoms were measured using a self-report questionnaire rather than using a clinician-administered diagnostic interview, we cannot determine with certainty how many men in this sample actually met DSM-IV criteria for the PTSD diagnosis. Self-report methodologies, in general, have a number of shortcomings; for instance, self-report is subjected to social desirability bias and recall bias (e.g., forgetting). Lastly, the sample only included men and those with recent trauma exposure with resulting stress symptoms, which limits our ability to generalize the findings to women and those without a recent history of traumatic stress.
Although the study had limitations, there were several strengths which included the following: a large number of participants, the ethnically-diverse sample, the inclusion of heterosexual, gay, and bisexual men, and the inclusion of heterogeneous trauma experiences. Each of these strengths increases the robustness of the findings, suggesting the results may be generalizable to a diverse population of HIV-positive men.
Directions for future research and clinical implications
Further research that examines PD and its association to later development of PTSD and poor health outcomes will contribute to improving our understanding of traumatic stress and enhance trauma-focused interventions. In addition, since sexual trauma has been associated with the etiology of dissociation, further research on dissociation in general and PD (e.g., neurobiological factors, impact on behavior and cognition) will facilitate an elucidation of the relationships between sexual trauma and its psychosocial sequelae. Future research should also examine the mediators of the PTSD-health relationship (e.g., sympathetic nervous system activation, CD4+ cell count).
There are a number of important clinical implications of this study. First, considering that over half of the sample met or exceeded the IES-R cutoff score for probable PTSD diagnosis, an important component of health care for people living with HIV is stress management. Stress reduction will assist in emotion regulation, which is associated with psychological well-being (Moore, Zoellner, & Mollenholt, 2008). Second, one-third of the sample reported experiencing some type of CSA and reported substantial lifetime traumas including SR. This demonstrates a need for clinical interventions to target traumatic revictimization (Davies & Frawley, 1994). Also, it will be important to understand the ways in which psychotherapy for sexually abused men might differ from that aimed at women (e.g., accounting for differing socio-cultural factors, gender issues, greater depressive responses among women). Future clinical research should develop treatment models that are tailored to the unique socio-cultural aspects of men and their reactions to CSA (Spiegel, 2003). Finally, considering the role of PD as a mediator between SR and PTS symptoms, clinical interventions that reduce dissociative symptoms are likely to result in significant reduction in traumatic stress symptoms for HIV-positive men who report SR.
Table 4.
Regression analyses testing if sexual revictimization (SR) mediates the relationship between adult sexual assault (ASA) and peritraumatic dissociation (PD; N = 167)
| Step | β | R-squared | |
|---|---|---|---|
| 1 | ASA predicting PD | .22* | .05 |
| 2 | ASA predicting SR | .65* | .43 |
| 3 | ASA predicting PD | .04 | .09 |
| SR predicting PD | .28* |
Note.
p < .05
Table 5.
Regression analyses testing if peritraumatic dissociation (PD) mediates the relationship between sexual revictimization (SR) and posttraumatic stress symptoms (PTS symptoms; N = 167)
| Step | β | R-squared | |
|---|---|---|---|
| 1 | SR predicting PTS symptoms | .23* | .05 |
| 2 | SR predicting PD | .30* | .09 |
| 3 | SR predicting PTS symptoms | .04 | .42 |
| PD predicting PTS symptoms | .36* |
Note.
p < .05
Acknowledgments
This research was funded by the National Institute of Mental Health (NIMH; PI: Gore-Felton, R01MH072386).
References
- Allers CT, Benjack KJ. Connection between childhood abuse and HIV infection. Journal of Counseling and Development. 1991;70(2):309–313. Retrieved from http://www.counseling.org/Default_poppy.aspx?ReturnUrl=http://www.counseling.org/Publications/TP/JCDInfo/CT2.aspx. [Google Scholar]
- Baron R, Kenny D. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Barroso J, Hammill BG, Leserman J, Salahuddin N, Harmon JL, Pence BW. Physiological and psychosocial factors that predict HIV-related fatigue. AIDS and behavior. 2010;14(6):1415–1427. doi: 10.1007/s10461-010-9691-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briere J, Elliott DM. Prevalence and psychosocial sequelae of self-reported childhood physical and sexual abuse in a general population sample of men and women. Child Abuse & Neglect. 2003;27(10):1205–1222. doi: 10.1016/j.chiabu.2003.09.008. [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. Subpopulation Estimates from the HIV Incidence Surveillance System - United States, 2006. Morbidity and Mortality Weekly Report. 2008;57(36):985–989. Retrieved from http://www.cdc.gov/mmwr/preview/mmwrhtml/mm5736a1.htm. [PubMed] [Google Scholar]
- Charney DS, Deutch AY, Southwick SM, Krystal JH. Neural circuits and mechanisms of post-traumatic stress disorder. In: Friedman MJ, Charney DS, Deutch AY, editors. Neurobiological and clinical consequences of stress: From normal adaptation to PTSD. Philadelphia, PA: Lippincott-Raven Publishers; 1995. pp. 271–287. [Google Scholar]
- Classen CC, Palesh O, Aggarwal R. Sexual revictimization: A review of the empirical literature. Trauma, Violence, & Abuse. 2005;6(2):10–109. doi: 10.1177/1524838005275087. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Scarvalone P, Difede J. Posttraumatic stress disorder, self- and interpersonal dysfunction among sexually retraumatized women. Journal of Traumatic Stress. 1997;10:437–452. doi: 10.1023/a:1024893305226. [DOI] [PubMed] [Google Scholar]
- Cole SW. Psychosocial influences on HIV-1 disease progression: Neural, endocrine, and virologic mechanisms. Psychosomatic Medicine. 2008;70(5):562–568. doi: 10.1097/PSY.0b013e3181773bbd. [DOI] [PubMed] [Google Scholar]
- Creamer M, Bell R, Failla S. Psychometric properties of the Impact of Event Scale-Revised. Behaviour Research and Therapy. 2003;41(12):1489–1496. doi: 10.1016/j.brat.2003.07.010. [DOI] [PubMed] [Google Scholar]
- Davies JM, Frawley MG. Treating the adult survivor of childhood sexual abuse: A psychoanalytic perspective. New York, NY: Basic Books; 1994. [Google Scholar]
- Desai S, Arias I, Thompson MP, Basile KC. Childhood victimization and subsequent revictimization assessed in a nationally representative sample of women and men. Violence and Victims. 2002;17(6):639–653. doi: 10.1891/vivi.17.6.639.33725. Retrieved from http://www.ingentaconnect.com/content/springer/vav. [DOI] [PubMed] [Google Scholar]
- Folkman S, Chesney MA, Pollack L, Coates TJ. Stress, control, coping and depressive mood in human immunodeficiency virus-positive and -negative gay men in San Francisco. Journal of Nervous and Mental Disease. 1993;181(7):409–416. doi: 10.1097/00005053-199307000-00002. [DOI] [PubMed] [Google Scholar]
- Ginzburg K, Butler LD, Giese-Davis J, Cavanaugh CE, Neri E, Koopman C, Classen CC, Spiegel D. Shame, guilt, and posttraumatic stress disorder in adult survivors of childhood sexual abuse at risk for human immunodeficiency virus: outcomes of a randomized clinical trial of group psychotherapy treatment. The Journal of Nervous and Mental Disease. 2009;197(7):536–542. doi: 10.1097/NMD.0b013e3181ab2ebd. [DOI] [PubMed] [Google Scholar]
- Gore-Felton C, Koopman C. Behavioral mediation of the relationship between psychosocial factors and HIV disease progression. Psychosomatic Medicine. 2008;70(5):569–574. doi: 10.1097/PSY.0b013e318177353e. [DOI] [PubMed] [Google Scholar]
- Green BL. Psychometric review of the Trauma History Questionnaire. In: Stamm BH, editor. Measurement of stress, trauma, and adaptation. Lutherville, MD: Sidran Press; 1996. pp. 366–369. [Google Scholar]
- Hansen NB, Brown LJ, Tsatkin E, Zelgowski B, Nightingale V. Dissociative experiences during sexual behavior among a sample of adults living with HIV infection and a history of childhood sexual abuse. Journal of Trauma & Dissociation. 2012;13(2):345–360. doi: 10.1080/15299732.2011.641710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Benotsch E, Rompa D, Gore-Felton C, Austin J, Luke W, DiFonzo K, Buckles J, Kyomugisha F, Simpson D. Unwanted sexual experiences, and sexual risks, in gay and bisexual, men: Associations among revictimization, substance use, and psychiatric symptoms. The Journal of Sex Research. 2001;38(1):1–9. Retrieved from http://www.tandf.co.uk/journals/titles/00224499.asp. [Google Scholar]
- Kamen C, Bergstrom J, Koopman C, Lee S, Gore-Felton C. Relationships among childhood trauma, posttraumatic stress disorder and dissociation in men living with HIV/AIDS. Journal of Trauma & Dissociation. 2012;13(1):102–114. doi: 10.1080/15299732.2011.608629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keuroghlian AS, Kamen CS, Neri E, Lee S, Liu R, Gore-Felton C. Trauma, dissociation, and antiretroviral adherence among persons living with HIV/AIDS. Journal of Psychiatric Research. 2011;45(7):942–948. doi: 10.1016/j.jpsychires.2011.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lensvelt-Mulders G, van der Hart O, van Ochten JM, van Son MJM, Steele K, Breeman L. Relations among peritraumatic dissociation and posttraumatic stress: A meta-analysis. Clinical Psychology Review. 2008;28:1138–1151. doi: 10.1016/j.cpr.2008.03.006. [DOI] [PubMed] [Google Scholar]
- Leserman J, Whetten K, Lowe K, Stangl D, Swartz MS, Thielman N. How do trauma, recent stressful events, and PTSD affect functional health status and health utilization among HIV-positive in the deep South. Psychosomatic Medicine. 2005;6:500–507. doi: 10.1097/01.psy.0000160459.78182.d9. [DOI] [PubMed] [Google Scholar]
- Leserman J. Role of depression, stress, and trauma in HIV disease progression. Psychosomatic Medicine. 2008;70(5):539–545. doi: 10.1097/PSY.0b013e3181777a5f. [DOI] [PubMed] [Google Scholar]
- Lloyd S, Operario D. HIV risk among men who have sex with men who have experienced childhood sexual abuse: systematic review and meta-analysis. AIDS Education and Prevention. 2012;24(3):228–41. doi: 10.1521/aeap.2012.24.3.228. [DOI] [PubMed] [Google Scholar]
- Marmar CR, Weiss DS, Metzler TJ. The Peritraumatic Dissociative Experiences Questionnaire. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD. New York, NY: Guilford Press; 1997. pp. 412–428. [Google Scholar]
- Marshall GN, Orlando M, Jaycox LH, Foy DW, Belzberg H. Development and validation of a modified version of the Peritraumatic Dissociative Experiences Questionnaire. Psychological Assessment. 2002;14(2):123–134. doi: 10.1037//1040-3590.14.2.123. [DOI] [PubMed] [Google Scholar]
- Meade CS, Hansen NB, Kochman A, Sikkema K. Utilization of medical treatments and adherence to antiretroviral therapy among HIV-positive adults with histories of childhood sexual abuse. AIDS Patient Care and STDs. 2009;23(4):259–266. doi: 10.1089/apc.2008.0210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moore SA, Zoellner LA, Mollenholt N. Are expressive suppression and cognitive reappraisal associated with stress-related symptoms? Behaviour Research and Therapy. 2008;46(9):993–1000. doi: 10.1016/j.brat.2008.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mulder RT, Beautrais AL, Joyce PR, Fergusson DM. Relationship between dissociation, childhood sexual abuse, childhood physical abuse, and mental illness in a general population sample. American Journal of Psychiatry. 1998;155(6):806–811. doi: 10.1176/ajp.155.6.806. Retrieved from http://ajp.psychiatryonline.org/journal.aspx?journalid=13. [DOI] [PubMed] [Google Scholar]
- O’Cleirigh C, Skeer M, Mayer KH, Safren SA. Functional impairment and health care utilization among HIV-infected men who have sex with men: the relationship with depression and post-traumatic stress. Journal of Behavioral Medicine. 2009;32:466–477. doi: 10.1007/s10865-009-9217-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pence BW, Reif S, Whetten K, Leserman J, Stangl D, Swartz M, Thielman N, Mugavero MJ. Minorities, the poor, and survivors of abuse: HIV-infected patients in the US Deep South. Southern Medical Journal. 2007;100(11):1114–1122. doi: 10.1097/01.smj.0000286756.54607.9f. Retrieved from http://journals.lww.com/smajournalonline/pages/default.aspx. [DOI] [PubMed] [Google Scholar]
- Resnick HS, Yehuda R, Pitman RK, Foy DW. Effective of previous trauma on acute plasma cortisol level following rape. American Journal of Psychiatry. 1995;152:1675–1677. doi: 10.1176/ajp.152.11.1675. [DOI] [PubMed] [Google Scholar]
- Ross CA, Joshi S, Currie R. Dissociative experiences in the general population. American Journal of Psychiatry. 1990;147:1547–1552. doi: 10.1176/ajp.147.11.1547. [DOI] [PubMed] [Google Scholar]
- Schnurr PP, Green BL. Understanding relationships between trauma, posttraumatic stress disorder, and health outcomes. In: Schnurr PP, Green BL, editors. Trauma and health: Physical health consequences of exposure to extreme stress. Washington, DC: American Psychological Association; 2004. pp. 247–275. [Google Scholar]
- Schnurr PP, Jankowski MK. Physical health and post-traumatic stress disorder: Review and synthesis. Seminars in Clinical Neuropsychiatry. 1999;4(4):295–304. doi: 10.153/SCNP00400295. [DOI] [PubMed] [Google Scholar]
- Shearer S. Dissociative phenomena in women with borderline personality disorder. American Journal of Psychiatry. 1994;151:1324–1328. doi: 10.1176/ajp.151.9.1324. [DOI] [PubMed] [Google Scholar]
- Smith MY, Egert J, Winkel G, Jacobson J. The impact of PTSD on pain experience in persons with HIV/AIDS. Pain. 2002;98:9–17. doi: 10.1016/s0304-3959(01)00431-6. [DOI] [PubMed] [Google Scholar]
- Spiegel D, Cardeña E. Disintegrated experience: The dissociative disorders revisited. Journal of Abnormal Psychology. 1991;100(3):366–378. doi: 10.1037//0021-843x.100.3.366. Retrieved from http://www.apa.org/pubs/journals/abn/index.aspx. [DOI] [PubMed] [Google Scholar]
- Spiegel J. Sexual abuse of males: The SAM Model of theory and practice. New York: Routledge; 2003. [Google Scholar]
- Weiss DS, Marmar CR. The Impact of Event Scale – Revised. In: Wilson JP, Keane TM, editors. Assessing psychological trauma and PTSD: A practitioner’s handbook. New York, NY: Guilford Press; 1997. pp. 399–411. [Google Scholar]
- Whetten K, Leserman J, Lowe K, Stangl D, Thielman N, Swartz M, Hanisch L, Van Scoyoc L. Prevalence of childhood sexual abuse and physical trauma in an HIV-positive sample from the Deep South. American Journal of Public Health. 2006;96(6):1028–1030. doi: 10.2105/AJPH.2005.063263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wurr CJ, Partridge IM. The prevalence of a history of childhood sexual abuse in an acute adult inpatient population. Child Abuse & Neglect. 1996;20(9):867–872. doi: 10.1016/0145-2134(96)00074-9. [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Zakriski AL, Shea MT, Costello E, Begin A, Pearlstein T, Simpson E. The long-term sequelae of sexual abuse: Support for a complex posttraumatic stress disorder. Journal of Traumatic Stress. 1996;9:195–205. doi: 10.1007/BF02110655. [DOI] [PubMed] [Google Scholar]
- Zurbriggen EL, Freyd JJ. The link between child sexual abuse and risky sexual behavior: The role of dissociative tendencies, information processing effects, and consensual sex decision mechanisms. In: Koenig LJ, Doll LS, O’Leary A, Pequenat W, editors. From Child Sexual Abuse to Adult Sexual Risk: Trauma, Revictimization, and Intervention. Washington, D.C: American Psychological Association; 2004. pp. 135–158. [Google Scholar]