Abstract
Purpose
Few studies have compared acute use of alcohol in suicide decedents with that in a nonsuicide group. This study provides the first national analysis of acute use of alcohol prior to suicide compared with an estimate of acute use of alcohol in a living sample.
Methods
Pooled 2003-2011 National Violent Death Reporting System data were used to estimate the prevalence of postmortem blood alcohol content positivity (BAC >0.0 g/dl) and intoxication (BAC ≥ 0.08 g/dl). Population estimates of comparable use of alcohol (within the past 48 hours) were based on the National Epidemiologic Survey on Alcohol and Related Conditions.
Results
Compared to the living sample, male and female suicide decedents showed, respectively, a 1.83- (95% confidence interval [CI], 1.73-1.93) and 2.40-fold (95% CI, 2.24-2.57) increased risk of alcohol ingestion prior to their death after age, race/ethnicity, and chronic alcohol problems were controlled. Furthermore, male and female decedents exhibited, respectively, a 6.18- (95% CI, 5.57-6.86) and a 10.04-fold (95% CI, 8.67-11.64) increased risk of being intoxicated prior to their death after confounders were considered.
Conclusions
The findings underscore the crucial need to include among the essential components of suicide prevention policies programs that minimize use of alcohol, particularly drinking to intoxication.
Keywords: Suicide, Toxicology, Alcohol Drinking, and Epidemiology
Suicide continues to be an urgent global public health problem [1]. In the United States, 38,364 people died by suicide in 2010, representing the 10th leading overall cause of death and fifth leading cause of years of potential life lost (YPLL). Men across the age span, but particularly in older age, have a higher suicide rate than do women at any age [2].
Alcohol plays a key role in suicide [3-6]. According to the U.S. Centers for Disease Control and Prevention (CDC), on average, 7,266 suicides (23%) and 243,516 YPLL (36%) were attributable to alcohol annually in 2001–05 [7]. There have been several uncontrolled, descriptive studies of the association of acute use of alcohol and suicide [6], including several reports of national U.S. data by our investigative team [8-10]. This literature confirms that alcohol is commonly consumed prior to suicide; for example, our group recently reported that 37% of male and 29% of female suicide decedents in a U.S. national sample had positive blood alcohol levels [8]. These data further showed that individuals who drank prior to suicide tended to consume high levels of alcohol; we recorded estimates of mean blood alcohol concentrations (BACs) of 0.15 g/dl and 0.13 g/dl in male and female suicide decedents, respectively, who used alcohol prior to suicide [10], levels that far exceed the 0.08 g/dl legal limit for drinking and driving in the United States.
What is missing from such data is the ability to compare drinking in suicide decedents with that in a nonsuicide comparison group, a procedure that would allow for estimation of the degree of risk for suicide associated with drinking occasions and heavy drinking occasions, respectively. Indeed, to our knowledge there has been only one study that systematically compared acute use of alcohol in suicide decedents with that in a nonsuicide comparison group [11]. Using a case-control study of 149 firearm suicides, Branas et al. [11] found acute alcohol intoxication to increase firearm suicide risk. Although the report by Branas and colleagues is informative, its generalizability to suicides nationally or to suicides using other methods is unclear. Its small sample size also does not allow for estimates of risk in men versus women (i.e., n < 20 female suicides) or in specific age groups, a key limitation in light of dramatic differences in drinking (and heavy drinking) in the general population as a function of age and gender [12].
The primary purpose of the current study was to provide the first estimates based on U.S. national data of relative risk of suicide associated with a) drinking occasions and b) heavy drinking occasions. We hypothesized that suicide decedents had higher drinking rates and levels prior to death than a living sample. This study addressed these issues using the National Violent Death Reporting System (NVDRS), a large, well-characterized database with unrivaled toxicology information. The primary aim of the study was to compare acute alcohol use among suicide decedents with drinking patterns of a living population. The results can be used to facilitate the development of more effective clinical practices, treatment programs, and public policies to reduce the incidence of alcohol-associated suicides.
Method
This study used restricted pooled data for decedents from the 2003–2011 NVDRS [13]. Supported by the CDC, the NVDRS is a state-based active surveillance system that provides a detailed account of violent deaths in the participating states. Although a smaller cohort of states participated in 2003 and 2004, in 2005–2011 16 states (Alaska, Colorado, Georgia, Kentucky, Maryland, Massachusetts, New Jersey, New Mexico, North Carolina, Oklahoma, Oregon, Rhode Island, South Carolina, Utah, Virginia, and Wisconsin) contributed data to the NVDRS. In 2010, Ohio joined the NVDRS.
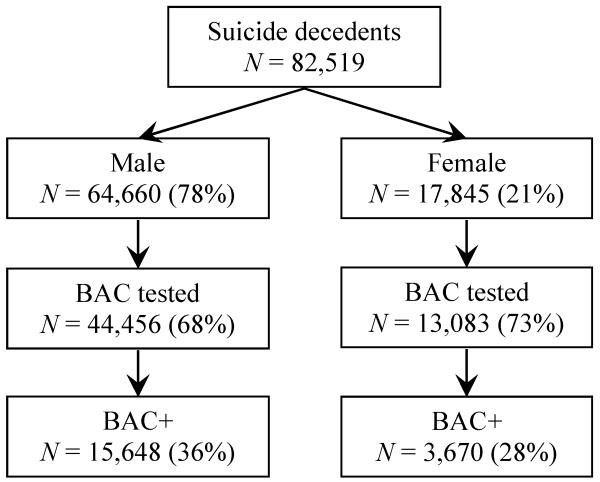
The data were gathered from coroner/medical examiner (C/ME) records; police reports; death certificates; toxicology laboratories; crime laboratories; and Bureau of Alcohol, Tobacco, Firearms and Explosives (ATF) firearm trace reports. Information on acute alcohol use was based on toxicological analyses of decedents as part of the C/ME investigation. Suicide decedents were identified using the International Classification of Diseases, 10th Revision codes X60–X84 or Y87.0 [14]. Pooled 2003–2011 NVDRS data yielded 82,519 suicide decedents (Figure 1). A detailed description of the sample characteristics appears elsewhere [8, 9, 15]. The Human Subjects Review Committee at Portland State University approved this study.
Fig. 1.
Study population in the National Violent Death Reporting System (NVDRS), 2003–2011 BAC = blood alcohol concentration; BAC+ = BAC positivity (BAC > 0.0 g/dl)
As shown in Figure 1, 68% of male (n = 44,456) and 73% of female (n = 13,083) suicide decedents were tested for blood alcohol concentration. BAC positivity (BAC+) refers to the presence of alcohol versus its absence (BAC negative). The BAC was first coded as a continuous measure in terms of weight by volume and then classified as any detectable BAC (BAC+) versus none. Decedents were further classified into those with a BAC of ≥ 0.08 g/dl (the legal limit for driving in all U.S. states) and those with a BAC of < 0.08 g/dl. Percent of decedents who underwent autopsy in each participating NVDRS states appears in Appendix 1.
Alcohol problem (AP) information was derived from C/ME and law enforcement records and denotes whether the decedent was reported by family, friends, or health care providers to have had an AP prior to death. Gender and age (categorized into 5-year age groups) were obtained from death certificates. Prevalence rates of BAC+ and BAC ≥ 0.08 g/dl were estimated for all groups.
Living Sample
The 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) [16] data were used as the comparison group. The NESARC was conducted by the U.S. Census Bureau under the direction of the National Institute on Alcohol Abuse and Alcoholism and is a nationally representative longitudinal survey of 43,093 noninstitutionalized adults in the United States, involving in-person interviews. It was used to assess alcohol use, heavy episodic drinking, and APs. The NESARC response rate for the first wave (2001–2002) was 81%. Monthly drinkers were asked, “How long has it been since you last drank?” and classified into one of two groups: “reported drinking the day of or up to 48 hours prior to the interview” or “did not drink the day of or up to 48 hours prior to the interview.” Abstainers and non-monthly drinkers were also considered as participants who did not drink prior to the interview. Heavy episodic drinking denoted participants who drank the day of the interview or up to 48 hours prior to the interview and who typically consumed 5 or more drinks (4 or more for women) on the day they drank (versus those using less and not prior to the interview). Alcohol problems were measured with the Alcohol Use Disorder and Associated Disabilities Interview Schedule–Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) Version (AUDADIS-IV), which assesses use of alcohol, and DSM-IV diagnoses of alcohol abuse and dependence [17]. Respondents who met the criteria for alcohol abuse and/or dependence were classified as having an AP. Prevalence rates of alcohol use prior to the interview and heavy episodic drinking were estimated. Table 1 shows the demographic characteristics of NVDRS suicide decedents and NESARC participants used in the analysis.
Table 1.
Characteristics of NVDRS suicide decedents and NESARC participants
| NVDRS (n = 52,276) | NESARC (n = 43,093) | |
|---|---|---|
| Gender | ||
| Men | 76.9 | 47.9 |
| Women | 23.2 | 52.1 |
| Age | ||
| 18-21 | 4.1 | 5.9 |
| 21-24 | 6.8 | 7.1 |
| 25-29 | 8.4 | 8.8 |
| 30-34 | 8.4 | 9.7 |
| 35-39 | 9.5 | 10.4 |
| 40-44 | 11.3 | 10.8 |
| 45-49 | 12.4 | 10.0 |
| 50-54 | 11.6 | 8.8 |
| 55-59 | 8.7 | 6.9 |
| 60-64 | 5.8 | 5.4 |
| 65-69 | 3.8 | 4.6 |
| 70-74 | 2.9 | 4.3 |
| ≥ 75 | 6.4 | 7.4 |
| Race/ethnicity | ||
| White | 85.1 | 70.9 |
| African American | 6.8 | 11.1 |
| AI/AN | 1.5 | 2.1 |
| Asian/PI | 1.8 | 4.4 |
| Hispanic | 4.8 | 11.6 |
| Metropolitan status (MSA) | ||
| Non-MSA | 17.6 | 19.7 |
| MSA | 82.4 | 80.3 |
AI/AN: American Indian/ Alaska Native; PI: Pacific Islander NVDRS: National Violent Death Reporting System; NESARC: National Epidemiologic Survey on Alcohol and Related Conditions
The analyses used all NESARC respondents rather than selecting those from NVDRS participating states to ensure sufficient statistical power. A separate analysis comparing the prevalence of alcohol use among NESARC participants by gender and age between participating NVDRS states and nonparticipating states revealed similar consumption patterns (Appendix 2). Logistic regression models were computed to test whether the rates of drinking in the deceased and the living sample were different after adjusting for race/ethnicity (white, black, American Indian/Alaska Native, Asian/xPacific Islander, and Hispanic) and AP. Models were stratified by age and gender. Estimates and standard errors from NESARC were weighted to reflect the complex sampling design and adjusted for nonresponse and poststratification using SUDAAN 11.0 [18].
Results
Among those tested for blood alcohol, 36% of male and 28% of female suicide decedents were BAC+ (i.e., BAC > 0.0 g/dl). Table 2 shows the prevalence of alcohol use prior to suicide among NVDRS decedents and prior to the interview among NESARC respondents by gender and age. Male and female suicide decedents younger than age 60 years were more likely to drink than their living counterparts. As expected, among nonelderly decedents, men were significantly more likely to be BAC+ than were women. In addition, Table 2 shows that although deceased men were more likely than women to have consumed alcohol prior to death, the rate ratios of men to women were significantly lower in the mortality sample relative to the living sample.
Table 2.
Presence and use of alcohol in deceased and living samples by gender and age
| NVDRS (BAC>0 g/dl) |
NESARC (Drank within 48 hours of the interview) |
Male to Female Ratio (95% CI) |
Adjusted odds of drinking prior to suicide OR (95% CI) |
|||||
|---|---|---|---|---|---|---|---|---|
| Men, % (n) | Women, % (n) | Men, % (n) | Women, % (n) | NVDRS | NESARC | Men | Women | |
| All | 36.6 (14508) | 29.3 (3499) | 21.6 (4018) | 11.7 (2598) | 1.2 (1.3 - 1.2) | 1.8 (1.9 - 1.8) | 1.83 (1.73 - 1.93) | 2.40 (2.24 - 2.57) |
| 18-21 | 30.0 (528) | 24.8 (88) | 13.5 (137) | 5.3 (53) | 1.2 (1.4 - 1.1) | 2.5 (2.8 - 2.3) | 4.87 (3.58 - 6.63) | 6.97 (4.71 - 10.31) |
| 21-24 | 43.3 (1262) | 34.1 (203) | 23.1 (286) | 11.7 (179) | 1.3 (1.4 - 1.2) | 2.0 (2.1 - 1.9) | 3.41 (2.76 - 4.20) | 3.94 (3.20 - 4.86) |
| 25-29 | 42.1 (1446) | 30.5 (269) | 22.0 (310) | 11.4 (226) | 1.4 (1.5 - 1.3) | 1.9 (2.0 - 1.8) | 2.64 (2.19 - 3.19) | 3.21 (2.67 - 3.86) |
| 30-34 | 42.9 (1455) | 33.4 (311) | 19.6 (388) | 12.2 (280) | 1.3 (1.4 - 1.2) | 1.6 (1.6 - 1.6) | 2.94 (2.48 - 3.48) | 3.00 (2.49 - 3.61) |
| 35-39 | 42.4 (1572) | 30.4 (365) | 21.6 (436) | 13.3 (313) | 1.4 (1.5 - 1.3) | 1.6 (1.7 - 1.6) | 2.38 (2.11 - 2.69) | 2.08 (1.77 - 2.44) |
| 40-44 | 43.1 (1877) | 35.5 (529) | 21.6 (455) | 13.4 (308) | 1.2 (1.3 - 1.2) | 1.6 (1.7 - 1.6) | 2.37 (2.05 - 2.72) | 2.67 (2.26 - 3.16) |
| 45-49 | 41.7 (1948) | 32.6 (566) | 24.2 (462) | 14.8 (288) | 1.3 (1.3 - 1.2) | 1.6 (1.7 - 1.5) | 1.74 (1.52 - 2.00) | 1.86 (1.54 - 2.26) |
| 50-54 | 39.6 (1727) | 30.1 (484) | 24.4 (404) | 13.3 (255) | 1.3 (1.4 - 1.3) | 1.8 (1.9 - 1.8) | 1.46 (1.21 - 1.76) | 1.79 (1.44 - 2.23) |
| 55-59 | 34.0 (1125) | 27.1 (314) | 23.4 (295) | 12.1 (170) ^ | 1.3 (1.3 - 1.2) | 1.9 (2.0 - 1.8) | 1.04 (0.85 - 1.26) | 2.01 (1.60 - 2.53) |
| 60-64 | 31.9 (710) | 22.2 (171) | 22.9 (238) | 11.0 (128) | 1.4 (1.5 - 1.3) | 2.1 (2.2 - 2.0) | 1.14 (0.93 - 1.40) | 1.52 (1.18 - 1.96) |
| 65-69 | 21.9 (330) | 22.8 (98) | 24.6 (215) | 11.6 (120) | 1.0 (1.0 - 0.9) | 2.1 (2.2 - 2.0) | 0.59 (0.47 - 0.75) | 1.20 (0.94 - 1.53) |
| 70-74 | 17.5 (220) | 13.6 (36) | 21.3 (169) | 10.4 (106) | 1.3 (1.5 - 1.1) | 2.1 (2.1 - 2.0) | 0.57 (0.44 - 0.74) | 0.83 (0.60 - 1.15) |
| ≥ 75 | 11.1 (308) | 12.6 (65) | 17.8 (223) | 7.4 (172) | 0.9 (1.0 - 0.8) | 2.4 (2.5 - 2.3) | 0.46 (0.38 - 0.56) | 1.47 (1.20 - 1.80) |
In the 2003–11 National Violent Death Reporting System (NVDRS), alcohol presence refers to suicide decedents with a positive BAC (>0.0g/dl). In the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), monthly drinkers (living subjects) were asked, “How long has it been since you last drank?” and classified into one of two groups: “reported drinking the day of or up to 48 hours prior to the interview” or “did not drink the day of or up to 48 hours prior to the interview.” CI = confidence interval. Odds ratios (ORs) and 95% CIs from logistic regression models adjusted for alcohol problems and race/ethnicity.
Table 2 also shows the adjusted odds of drinking prior to the event in the deceased sample relative to the living sample. The results showed deceased men aged < 45 years were 2 to 4 times more likely to have ingested alcohol prior to the event, compared with the living sample. Similarly, female decedents under the age of 65 years also were more likely to have used alcohol prior to the event.
Table 3 shows that acute, heavy use of alcohol is a potent risk factor for suicide in U.S. men and women across the age spectrum, with risk estimates ranging from fourfold to greater than 20- fold. Women’s odds ratios exceeded those of men for all age groups. However, the female versus male differences in odds ratios were only statistically significant for the oldest age group (p < 0.01).
Table 3.
Heavy episodic drinking in deceased and living sample by gender and age
| NVDRS (BAC ≥ 0.08 g/dl) |
NESARC (≥ 4 drinks for women or ≥ 5 for men) |
Adjusted odds of heavy drinking prior to suicide (95% CI) |
||||
|---|---|---|---|---|---|---|
| Men,% (n) | Women,% (n) | Men,% (n) | Women,% (n) | Men | Women | |
| All | 24.4 (9442) | 18.0 (2107) | 5.4 (953) | 1.9 (420) | 6.18 (5.57 - 6.86) | 10.04 (8.67 - 11.64) |
| < 30 | 27.2 (2164) | 20.6 (371) | 9.7 (331) | 3.3 (145) | 4.29 (2.75 - 6.71) | 8.62 (4.81 - 15.42) |
| 30-39 | 29.2 (2018) | 20.1 (419) | 5.6 (221) | 2.8 (127) | 6.63 (5.53 - 7.97) | 7.50 (5.77 - 9.74) |
| 40-49 | 29.2 (2566) | 21.3 (674) | 5.2 (204) | 1.9 (89) | 7.58 (6.17 - 9.31) | 9.92 (7.34 - 13.39) |
| 50-59 | 24.0 (1797) | 17.4 (473) | 3.9 (112) | 1.3 (41) | 5.77 (4.41 - 7.55) | 9.18 (6.15 - 13.70) |
| ≥ 60 | 11.8 (906) | 8.8 (171) | 1.8 (85) | 0.3 (18) | 5.71 (4.28 - 7.61) | 22.65 (12.66 - 40.51) |
Heavy episodic drinking in the National Violent Death Reporting System (NVDRS) refers to suicide decedents with a BAC of ≥0.08g/dl. Heavy episodic drinking among National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) respondents refers to 5 or more drinks (4 or more for women) on a typical drinking day among those who drank prior to the interview. CI = confidence interval. Odds ratios (ORs) and 95% CIs from logistic regression models adjusted for alcohol problems and race/ethnicity.
Finally, YPLL prior to age 65 were computed from those suicides that had been tested for alcohol. For all suicides, male and female YPLL were 1,937,081 and 547,680, respectively. For acute alcohol-related suicides, the male and female YPLL were 738,720 and 148,764, respectively. Thus, according to these data, alcohol-related suicides accounted for 36% of YPLL, which is consistent with CDC alcohol-related disease impact estimates [7].
Discussion
Alcohol was detected in nearly 36% of male and 28% of female suicide decedents. There were noteworthy age differences in the relative likelihoods of drinking for suicide decedents versus survey respondents. Looking first at any alcohol ingestion, nonelderly male and female suicide decedents were two to four times more likely to use alcohol prior to suicide than the living sample was likely to drink in the 48 hours prior to the interview. Above age 65, the ratio was less than one, suggesting that for older people, alcohol ingestion per se does not acutely elevate the risk of suicide. However, the most striking findings concerned heavy alcohol ingestion, with the ratio (heavy drinking probability among suicide decedents versus that in living respondents) rising rapidly and remaining high even in older age. These findings suggest that suicide decedents were more likely to drink and more likely to drink heavily relative to the living population.
Another important finding, largely consistent with Zerbini et al. [19] and Holmgren and Jones [20], is that BAC levels among male and female suicide decedents were surprisingly similar. In other words, although general living population data have consistently showed that men are more likely than women to drink and to drink in excess [21-23], among suicide decedents there appeared to be virtual gender parity in acute alcohol use immediately prior to their death. One possible explanation for this finding is that women are more likely than men to poison themselves and alcohol may be used as one of the poisoning agents in combination with other substances. Indeed, the NVDRS showed that BAC+ female decedents were two to five times more likely to die of poison (including ethanol, illicit drugs, and medications) ingestion than their male counterparts [8].
The finding suggests opportunities for interventions aimed at reducing female suicides. For example, health care providers need to be vigilant about misuse of alcohol among their at-risk depressed and suicidal female as well as male patients [24]. On the other hand, the male preference for using firearms limits possible suicide prevention strategies. As Kaplan et al. [25] observed, the use of highly lethal means provides a limited window for rescue and psychiatric treatment. Even for patients who have been identified as suicidal, in only half the instances would physicians inquire whether or not the patient had access to a firearm [26]. Nonetheless, health care providers should suggest to family members of depressed and alcohol-misusing patients that they reduce the patients’ access to firearms.
An additional key finding is that nearly a quarter of all decedents under the age of 21 years were BAC+ at the time of death, highlighting the risk of suicide associated with drinking (and heavy drinking). This result is especially troublesome because these decedents are considered underage and not allowed to drink under current U.S. state laws. In particular, the high mean BAC among younger suicide decedents warrants immediate clinical and policy attention, including (a) social media in promoting a message of alcohol abuse and risk for suicide, (b) school personnel might be enlisted in carrying the message, (c) increased access to treatment programs, and (d) enhanced enforcement of restrictions on youth access to alcohol [27, 28]. Moreover, these younger decedents could have obtained alcohol in their homes, which indicates a need to educate parents about the dangers of maintaining alcohol in the home, especially if not in locked cabinets. Other interventions that might arise from the findings include promoting the identification of BAC and other drug testing in the event of suicide and encouraging widespread autopsy of possible suicide decedents.
There are many challenges in the population comparisons described here. Of course, suicide decedents may differ from survey respondents in innumerable ways. For example, decedent alcohol data were derived from blood tests, whereas respondent information came from self-reports. Numerous so-called coverage studies [29] have found that self-reported alcohol consumption accounts for (at most) about half the alcohol sold (based on tax data). Also, survey respondents were volunteers, who may well have changed their usual drinking behaviors in the day(s) prior to interview. Given the comparison challenges, it is reasonable to inflate the drinking probabilities estimated from the survey data.
The findings need to be considered in light of some additional data limitations. First, BAC testing rates vary across the states participating in the NVDRS [8]. Fortunately, only a few states (Alaska, Georgia, and Oregon) had testing rates below 50%. A supplementary sensitivity analysis showed that the exclusion of these states did not alter the findings (Appendix 3). Second, toxicology testing is often determined by availability of state funding. Unfortunately, current federal resources provided to the NVDRS states do not cover toxicological testing. However, in a follow-up analysis, all demographic subgroups except those aged 60 years and older had toxicological testing rates at or above 65% (for decedents 60 years and older, the testing rate was 62%; Appendix 4). Third, the information regarding the precipitating circumstances, including APs, is derived from family, friends, health care professionals, and death scene investigations [13]. Fourth, the NVDRS, as noted, is limited to 17 states and may not be nationally representative [13]. Fifth, the time periods between NESARC and NVDRS differ. A separate analysis of National Survey on Drug Use and Health (2002-2011) data [30] showed that average drinking trends for men and women did not change over time (Appendix 5). Sixth, NESARC and NVDRS were not matched by dates of death or interview; however, we compared the prevalence of BAC+ and alcohol use by day of the week and month of the year and found parallel trends (Appendix 6). Lastly, results may be subject to residual confounding or potential effect modification due to unmeasured health conditions or other substance abuse; however, adjustment for alcohol problem in the models had a relatively small impact on the estimates.
Despite these limitations, data from the NVDRS have numerous strengths. First, the NVDRS data set provides BAC information for most suicide decedents. Second, although the NVDRS states are not necessarily representative of the United States, the decedents in these 17 states are similar to the demographic profile for the country as a whole in terms of gender, age, ethnic/racial composition, urban/rural characteristics, and national suicide mortality rates [8]. Finally, collection of postmortem data is particularly challenging when states have decentralized medicolegal death investigation systems rather than a centralized medical examiner system. It is worth noting that 69% of the states participating in the NVDRS have a centralized medical examiner system compared with only 15% of non-NVDRS states [31].
Taken as a whole, these findings suggest that acute alcohol misuse is a common concomitant of suicidal behavior for men and women across the age span. Also, most alcohol-related suicide decedents had BAC levels exceeding 0.08 g/dl. The findings reported herein point to the need for further analyses of the role of alcohol involvement in suicidal behavior in all age groups. Because of the high rate of alcohol dependence in the NVDRS sample (40% in some age groups), health care providers need to recognize and discuss with their at-risk patients the role that acute alcohol use plays in suicidal behavior. Equally important, the findings underscore the crucial need to design policies that minimize harmful use of alcohol and intoxication as an essential component of suicide prevention initiatives [24, 27].
Acknowledgments
This study was supported by grant R01 AA020063 from the National Institute on Alcohol Abuse and Alcoholism. All analyses, interpretations, and conclusions based on the analysis of these data are solely the responsibility of the authors and do not represent the views of either the U.S. Centers for Disease Control and Prevention or the states participating in the National Violent Death Reporting System.
Abbreviations
- AOR
adjusted odds ratio
- AP
alcohol problems
- ATF
Bureau of Alcohol, Tobacco, Firearms and Explosives
- AUDADIS-IV
Alcohol Use Disorder and Associated Disabilities Interview Schedule
- BAC
blood alcohol concentration
- C/ME
coroner/medical examiner
- CDC
Centers for Disease Control and Prevention
- DSM-IV
Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition
- NESARC
National Epidemiologic Survey on Alcohol and Related Conditions
- NVDRS
National Violent Death Reporting System
- YPLL
years of potential life lost
Appendix 1
Prevalence (%) of suicide decedents autopsied by state
| Alaska | 23.2 |
| Colorado | 73.9 |
| Georgia | 66.7 |
| Kentucky | 51.3 |
| Maryland | 68.3 |
| Massachusetts | 47.5 |
| New Jersey | 72.8 |
| New Mexico | 90.1 |
| North Carolina | 31.3 |
| Ohio | 65.4 |
| Oklahoma | 15.5 |
| Oregon | 11.1 |
| Rhode Island | 71.1 |
| South Carolina | 69.9 |
| Utah | 47.9 |
| Virginia | 80.6 |
| Wisconsin | 51.0 |
Appendix 2
Presence of alcohol (% and 95% CI) among NESARC respondents residing in NVDRS states versus non-NVDRS states by age groups
| Men |
Women |
|||
|---|---|---|---|---|
| Non-NVDRS states | NVDRS states | Non-NVDRS states | NVDRS states | |
| 18-21 | 12.0 (9.3 - 15.3) | 16.5 (11.9 - 22.5) | 5.0 (3.5 - 7.1) | 6.0 (3.6 - 10.0) |
| 21-24 | 23.1 (20.1 - 26.4) | 23.2 (17.8 - 29.5) | 10.3 (8.3 - 12.8) | 14.6 (11.5 - 18.5) |
| 25-29 | 22.9 (19.8 - 26.2) | 20.1 (15.6 - 25.5) | 12.0 (9.7 - 14.8) | 9.9 (7.5 - 13.1) |
| 30-34 | 18.6 (15.6 - 21.9) | 21.9 (18.2 - 26.1) | 11.1 (9.3 - 13.2) | 14.6 (11.8 - 18.1) |
| 35-39 | 21.9 (19.6 - 24.3) | 20.9 (17.4 - 24.8) | 12.9 (11.2 - 14.8) | 14.1 (10.9 - 18.2) |
| 40-44 | 22.4 (19.8 - 25.3) | 19.9 (16.6 - 23.7) | 13.7 (11.7 - 16.0) | 12.7 (9.8 - 16.2) |
| 45-49 | 24.7 (21.7 - 27.9) | 23.2 (20.0 - 26.8) | 15.5 (12.9 - 18.5) | 13.4 (10.0 - 17.8) |
| 50-54 | 25.3 (22.1 - 28.7) | 22.6 (18.2 - 27.5) | 13.7 (11.6 - 16.1) | 12.4 (9.3 - 16.2) |
| 55-59 | 23.0 (19.8 - 26.6) | 24.2 (19.7 - 29.3) | 12.2 (10.1 - 14.8) | 11.9 (8.1 - 17.0) |
| 60-64 | 23.2 (19.8 - 27.1) | 22.2 (17.7 - 27.5) | 11.1 (8.7 - 14.0) | 10.8 (7.7 - 14.9) |
| 65-69 | 24.1 (20.4 - 28.2) | 25.7 (20.6 - 31.5) | 12.2 (10.1 - 14.8) | 10.4 (7.1 - 14.9) |
| 70-74 | 20.1 (16.7 - 23.9) | 24.1 (18.0 - 31.4) | 11.0 (8.7 - 13.8) | 9.0 (6.2 - 12.8) |
| ≥ 75 | 18.2 (15.4 - 21.5) | 16.5 (12.6 - 21.4) | 8.0 (6.5 - 9.9) | 5.8 (4.1 - 8.2) |
NVDRS: National Violent Death Reporting System; NESARC: National Epidemiologic Survey on Alcohol and Related Conditions
Appendix 3
Sensitivity analysis excluding NVDRS states with low alcohol testing rates* by age and gender
| Men | Women | |
|---|---|---|
| Adjusted odds of drinking prior to suicide (95% CI) | ||
| 18-21 | 7.05 (4.95 - 10.05) | 8.26 (5.40 - 12.63) |
| 21-24 | 3.81 (2.95 - 4.92) | 4.75 (3.70 - 6.09) |
| 25-29 | 2.25 (1.86 - 2.72) | 4.26 (3.49 - 5.21) |
| 30-34 | 3.23 (2.73 - 3.82) | 3.29 (2.68 - 4.04) |
| 35-39 | 2.32 (2.06 - 2.62) | 2.13 (1.79 - 2.53) |
| 40-44 | 2.47 (2.15 - 2.82) | 3.76 (3.20 - 4.41) |
| 45-49 | 1.79 (1.56 - 2.04) | 2.00 (1.64 - 2.44) |
| 50-54 | 1.28 (1.05 - 1.56) | 2.24 (1.84 - 2.73) |
| 55-59 | 1.34 (1.12 - 1.59) | 1.20 (0.97 - 1.47) |
| 60-64 | 1.93 (1.59 - 2.35) | 1.26 (0.89 - 1.78) |
| 65-69 | 0.52 (0.42 - 0.65) | 2.91 (2.30 - 3.67) |
| 70-74 | 0.94 (0.73 - 1.19) | 4.67 (3.65 - 5.96) |
| ≥ 75 | 0.57 (0.47 - 0.69) | 2.47 (2.02 - 3.02) |
| Adjusted odds of heavy drinking prior to suicide (95% CI) | ||
| < 30 | 5.96 (3.56 - 9.98) | 9.60 (5.20 - 17.75) |
| 30-39 | 6.07 (5.06 - 7.29) | 7.89 (5.93 - 10.50) |
| 40-49 | 7.43 (6.08 - 9.08) | 9.91 (7.33 - 13.38) |
| 50-59 | 4.99 (3.83 - 6.49) | 11.64 (7.79 - 17.40) |
| ≥ 60 | 9.44 (7.01 - 12.70) | >26.72 (15.17 - 47.08) |
Alaska, Georgia, Oregon. CI: confidence interval. NVDRS: National Violent Death Reporting System; NESARC: National Epidemiologic Survey on Alcohol and Related Conditions
Appendix 4
Prevalence (%) of suicide decedents tested for blood alcohol content in NVDRS
| Gender | |
| Men | 68.8 |
| Women | 73.3 |
| Age | |
| <30 | 72.7 |
| 30-39 | 72.5 |
| 40-49 | 72.3 |
| 50-59 | 69.7 |
| ≥ 60 | 62.0 |
| Race/ethnicity | |
| White | 65.1 |
| African American | 72.7 |
| AI/AN | 80.1 |
| Asian/PI | 71.6 |
| Hispanic | 73.5 |
| Educational attainment | |
| < High school degree | 77.3 |
| High school degree | 77.4 |
| > High school degree | 79.5 |
| Method of suicide | |
| Firearm | 65.1 |
| Sharp or blunt instrument | 72.7 |
| Poison | 80.1 |
| Hanging or suffocation | 71.6 |
| Fall | 73.5 |
| Drowning | 72.8 |
| Other | 69.5 |
AI/AN: American Indian/ Alaska Native; PI: Pacific Islander; NVDRS: National Violent Death Reporting System
Appendix 5
Percent of weekly drinkers in NSDUH
| Male | Female | |
|---|---|---|
| 2001 | 27.8 | 16.0 |
| 2002 | 30.4 | 17.4 |
| 2003 | 29.6 | 17.9 |
| 2004 | 30.1 | 17.9 |
| 2005 | 29.6 | 18.7 |
| 2006 | 29.3 | 18.1 |
| 2007 | 29.9 | 19.0 |
| 2008 | 30.4 | 18.8 |
| 2009 | 30.5 | 20.6 |
| 2010 | 30.3 | 20.3 |
| 2011 | 29.8 | 20.3 |
NSDUH: National Survey on Drug Use and Health
Appendix 6
Prevalence (%) of alcohol use by week day and month
| NVDRS | NESARC | BRFSS 2010 | |
|---|---|---|---|
| Sunday | 37.6 | 19.7 | |
| Monday | 32.1 | 15.6 | |
| Tuesday | 32.1 | 15.5 | |
| Wednesday | 32.1 | 16.5 | |
| Thursday | 32.5 | 16.0 | |
| Friday | 33.2 | 15.6 | |
| Saturday | 37.7 | 18.0 | |
| January | 34.3 | 15.5 | 19.0 |
| February | 32.4 | 17.7 | 18.7 |
| March | 31.9 | 14.3 | 17.9 |
| April | 33.0 | 14.8 | 18.9 |
| May | 33.5 | -- | 18.9 |
| June | 34.1 | -- | 18.6 |
| July | 36.4 | -- | 19.3 |
| August | 36.8 | 16.1 | 19.6 |
| September | 34.3 | 16.3 | 19.5 |
| October | 32.5 | 17.1 | 19.2 |
| November | 33.2 | 16.3 | 20.1 |
| December | 33.1 | 16.5 | 18.6 |
Alcohol use refers to suicide decedents in the National Violent Death Reporting System (NVDRS) with a positive BAC (>0.0g/dl). In the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), monthly drinkers (living subjects) were asked, “How long has it been since you last drank?” and classified into one of two groups: “reported drinking the day of or up to 48 hours prior to the interview” or “did not drink the day of or up to 48 hours prior to the interview.” In the 2010 Behavioral Risk Factor Surveillance System (BRFSS), respondents were asked “during the past 30 days, how many days per week or per month did you have at least one drink of any alcoholic beverage” and classified as those who drank at least once a week versus non-weekly drinkers relative to the month of interview.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- [1].World Health Organization . Public health action for the prevention of suicide. World Health Organization; Geneva, Switzerland: 2012. [Google Scholar]
- [2].Centers for Disease Control and Prevention. National Center for Injury Prevention and Control Web-based Injury Statistics Query and Reporting System (WISQARS) 2010 [cited 2013 June 3]; Available from: http://webappa.cdc.gov/sasweb/ncipc/mortrate10_us.html.
- [3].Langhinrichsen-Rohling J, Snarr JD, Slep AM, Heyman RE, Foran HM. Risk for suicidal ideation in the U.S. Air Force: an ecological perspective. J Consult Clin Psychol. 2011;79(5):600–12. doi: 10.1037/a0024631. Epub 2011/07/27. [DOI] [PubMed] [Google Scholar]
- [4].Gonzalez VM, Hewell VM. Suicidal ideation and drinking to cope among college binge drinkers. Addict Behav. 2012;37(8):994–7. doi: 10.1016/j.addbeh.2012.03.027. Epub 2012/04/24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [5].Kim HM, Smith EG, Stano CM, Ganoczy D, Zivin K, Walters H, et al. Validation of key behaviourally based mental health diagnoses in administrative data: suicide attempt, alcohol abuse, illicit drug abuse and tobacco use. BMC Health Serv Res. 2012;12:18. doi: 10.1186/1472-6963-12-18. Epub 2012/01/25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Cherpitel CJ, Borges GLG, Wilcox HC. Acute alcohol use and suicidal behavior: A review of the literature. Alcohol Clin Exp Res. 2004;28(5):18S–28S. doi: 10.1097/01.alc.0000127411.61634.14. [DOI] [PubMed] [Google Scholar]
- [7].Centers for Disease Control and Prevention Alcohol Related Disease Impact (ARDI) application. 2013 [cited 2014 January, 23]; Available from: http://apps.nccd.cdc.gov/DACH_ARDI/Default.aspx.
- [8].Kaplan MS, McFarland BH, Huguet N, Conner K, Caetano R, Giesbrecht N, et al. Acute alcohol intoxication and suicide: a gender-stratified analysis of the National Violent Death Reporting System. Inj Prev. 2013;19(1):38–43. doi: 10.1136/injuryprev-2012-040317. Epub 2012/05/26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Caetano R, Kaplan MS, Huguet N, McFarland BH, Conner K, Giesbrecht N, et al. Acute alcohol intoxication and suicide among United States ethnic/racial groups: findings from the national violent death reporting system. Alcohol Clin Exp Res. 2013;37(5):839–46. doi: 10.1111/acer.12038. Epub 2013/02/07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Conner KR, Huguet N, Caetano R, Giesbrecht N, McFarland BH, Nolte KB, et al. Acute use of alcohol and methods of suicide in a US national sample. Am J Public Health. 2014;104(1):171–8. doi: 10.2105/AJPH.2013.301352. Epub 2013/05/18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Branas CC, Richmond TS, Ten Have TR, Wiebe DJ. Acute alcohol consumption, alcohol outlets, and gun suicide. Subst Use Misuse. 2011;46(13):1592–603. doi: 10.3109/10826084.2011.604371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Wilsnack RW, Wilsnack SC. Gender and alcohol: consumption and consequences. In: Boyle P, Boffetta P, Lowenfels AB, Burns H, Brawley O, Zatonski W, et al., editors. Alcohol: Science, Policy and Public Health. Oxford University Press; Oxford, United Kingdom: 2013. pp. 153–60. [Google Scholar]
- [13].Centers for Disease Control and Prevention. National Center for Injury Prevention and Control National Violent Death Reporting System. 2012 [cited 2013 June, 3]; Available from: http://wisqars.cdc.gov:8080/nvdrs/nvdrsDisplay.jsp.
- [14].World Health Organization . International Classification of Diseases, 10th Revision. World Health Organization; Geneva, Switzerland: 1996. [Google Scholar]
- [15].Karch DL, Logan J, McDaniel D, Parks S, Patel N. Surveillance for violent deaths--National Violent Death Reporting System, 16 states, 2009. Morbidity and Mortality Weekly Report Surveillance Summaries (Washington, DC: 2002) 2012;61(6):1–43. [PubMed] [Google Scholar]
- [16].Grant BF, Moore TC, Kaplan K. Source and Accuracy Statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) National Institute on Alcohol Abuse and Alcoholism; Bethesda, Md: 2003. [Google Scholar]
- [17].Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71(1):7–16. doi: 10.1016/s0376-8716(03)00070-x. Epub 2003/06/25. [DOI] [PubMed] [Google Scholar]
- [18].Research Triangle Institute . SUDAAN statistical software version 11.0. Research Triangle Institute; Triangle Park, NC: 2012. [Google Scholar]
- [19].Zerbini T, Ponce Jde C, Mayumi Sinagawa D, Barbosa Cintra R, Munoz DR, Leyton V. Blood alcohol levels in suicide by hanging cases in the state of Sao Paulo, Brazil. J Forensic Leg Med. 2012;19(5):294–6. doi: 10.1016/j.jflm.2012.02.022. Epub 2012/06/13. [DOI] [PubMed] [Google Scholar]
- [20].Holmgren A, Jones AW. Demographics of suicide victims in Sweden in relation to their blood-alcohol concentration and the circumstances and manner of death. Forensic Sci Int. 2010;198(1-3):17–22. doi: 10.1016/j.forsciint.2009.12.015. [DOI] [PubMed] [Google Scholar]
- [21].Hilton ME. The demographic distribution of drinking patterns in 1984. In: Clark WB, Hilton M, editors. Alcohol in America: Drinking Practices and Problems in a National Survey. State University of New York Press; Albany, NY: 1991. pp. 73–86. [Google Scholar]
- [22].Dawson DA, Grant BF, Chou SP, Pickering RP. Subgroup variation in U.S. drinking patterns: results of the 1992 national longitudinal alcohol epidemiologic study. J Subst Abuse. 1995;7(3):331–44. doi: 10.1016/0899-3289(95)90026-8. Epub 1995/01/01. [DOI] [PubMed] [Google Scholar]
- [23].Caetano R, Baruah J, Ramisetty-Mikler S, Ebama MS. Sociodemographic predictors of pattern and volume of alcohol consumption across Hispanics, Blacks, and Whites: 10-year trend (1992-2002) Alcohol Clin Exp Res. 2010;34(10):1782–92. doi: 10.1111/j.1530-0277.2010.01265.x. Epub 2010/07/22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Kaner EF, Dickinson HO, Beyer F, Pienaar E, Schlesinger C, Campbell F, et al. The effectiveness of brief alcohol interventions in primary care settings: a systematic review. Drug Alcohol Rev. 2009;28(3):301–23. doi: 10.1111/j.1465-3362.2009.00071.x. Epub 2009/06/06. [DOI] [PubMed] [Google Scholar]
- [25].Kaplan MS, McFarland BH, Huguet N. Characteristics of adult male and female firearm suicide decedents: findings from the National Violent Death Reporting System. Inj Prev. 2009;15(5):322–7. doi: 10.1136/ip.2008.021162. Epub 2009/10/07. [DOI] [PubMed] [Google Scholar]
- [26].Kaplan MS, Adamek ME, Rhoades JA. Prevention of elderly suicide. Physicians’ assessment of firearm availability. Am J Prev Med. 1998;15(1):60–4. doi: 10.1016/s0749-3797(98)00019-1. Epub 1998/07/04. [DOI] [PubMed] [Google Scholar]
- [27].Babor TF, Caetano R, Casswell S, Edwards G, Giesbrecht N, Grube J, et al. Alcohol: No ordinary commodity – research and public policy - Revised edition. Oxford University Press; Oxford, U.K.: 2010. [Google Scholar]
- [28].Grucza RA, Hipp PR, Norberg KE, Rundell L, Evanoff A, Cavazos-Rehg P, et al. The legacy of minimum legal drinking age law changes: long-term effects on suicide and homicide deaths among women. Alcohol Clin Exp Res. 2012;36(2):377–84. doi: 10.1111/j.1530-0277.2011.01608.x. Epub 2011/11/17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [29].Kerr WC, Greenfield TK. Distribution of alcohol consumption and expenditures and the impact of improved measurement on coverage of alcohol sales in the 2000 National Alcohol Survey. Alcohol Clin Exp Res. 2007;31(10):1714–22. doi: 10.1111/j.1530-0277.2007.00467.x. Epub 2007/07/27. [DOI] [PubMed] [Google Scholar]
- [30].United States Department of Health and Human Services. Substance Abuse and Mental Health Services Administration. Center for Behavioral Health Statistics and Quality . National Survey on Drug Use and Health, 2011. ICPSR 34481-v1. Inter-university Consortium for Political and Social Research; Ann Arbor, MI: 2011. [Google Scholar]
- [31].National Research Council . Strengthening forensic science in the united states: A path forward. The National Academies Press; Washington, DC: 2009. [Google Scholar]