Abstract
Human factors and ergonomics methods are needed to redesign healthcare processes and support patient-centered care, in particular for vulnerable patients such as hospitalized children. We implemented and evaluated a stimulated recall methodology for collective confrontation in the context of family-centered rounds. Five parents and five healthcare team members reviewed video records of their bedside rounds, and were then interviewed using the stimulated recall methodology to identify work system barriers and facilitators in family-centered rounds. The evaluation of the methodology was based on a survey of the participants, and a qualitative analysis of interview data in light of the work system model of Smith and Carayon (1989; 2000). Positive survey feedback from the participants was received. The stimulated recall methodology identified barriers and facilitators in all work system elements. Participatory ergonomics methods such as the stimulated recall methodology allow a range of participants, including parents and children, to participate in healthcare process improvement.
Keywords: work system, bedside round in a pediatric hospital, stimulated recall, participatory ergonomics
1. Introduction
Patient-centered care, defined as “care that is respectful of and responsive to individual patient preferences, needs, and values, and ensures that patient values guide all clinical decisions” (page 49), is one of the six dimensions of healthcare quality identified by the US Institute of Medicine (2001). Engaging patients in care is critical for quality of care as well as patient safety. Hospitalized children who often rely on their parents and other family members to participate in care are at high risk for a range of safety problems (Landrigan, 2005), including medication errors and preventable adverse drug events (Kaushal et al., 2001). Thus, engaging both pediatric patients and their families during care processes is critical for improving the quality and safety of care (Committee on Drugs & Committee on Hospital Care, 2003). In the inpatient setting, family-centered rounds (FCR) is a complex care process where “the patient and family share in the control of the management plan as well as in the evaluation of the process itself” (Sisterhen, Blaszak, Woods, & Smith, 2007). FCR are one type of daily, bedside, multidisciplinary rounds where care providers meet to communicate and make daily and discharge care decisions by engaging family members in the rounding process (Committee on Hospital Care & Institute for Patient- Family-Centered Care, 2012; Gurses & Xiao, 2006). However, various system barriers such as disruption of workflow, decreased efficiency, and rounding team size can hinder family engagement in FCR (Carayon et al., 2011). Human factors and ergonomics (HFE) has been suggested as a key discipline for assessing and improving safety in the pediatric inpatient setting (Scanlon, Karsh, & Densmore, 2006), as well as improving care processes and enhancing family-centered care (B. L. Wilson, 2010). HFE methods can be used to identify the system factors that hinder or facilitate patient-centered care, in particular in pediatric hospitals. In this research, we use the work system model of Smith and Carayon (1989; 2000) to characterize the barriers and facilitators to family engagement in the specific process of FCR.
Various HFE methods have been developed to assess work system barriers and facilitators, such as surveys, interviews and observations (J. R. Wilson & Corlett, 2005). Participatory ergonomics methods aimed at engaging ‘workers’ in the analysis of their activities allow the HFE professional a deeper level of analysis: the workers can reflect on their activities and provide in-depth information about their thoughts and opinions. Falzon, Mollo and colleagues (Faye & Falzon, 2009; Mollo & Falzon, 2004) have developed a range of ‘confrontation’ methods where individual workers review and assess videotapes of their own activities (individual auto-confrontation) or their colleagues’ activities (allo-confrontation), or a group of workers reviews and assesses their own activities or the activities of others (collective confrontation). When work is collaborative and involves multiple people on a team, the members of the team can review the videotapes of their team activities and identify work system barriers and facilitators to team cooperation, coordination and communication. This type of collective confrontation uses the stimulated recall methodology familiar to qualitative researchers (Derosier, Leclercq, Rabardel, & Langa, 2008; Dershimer & Conover, 1989).
1.1 Stimulated recall
Stimulated recall (or confrontation) methodology has been used in many domains, including manufacturing (Derosier et al., 2008; Mollo & Falzon, 2004), farming (Mollo & Falzon, 2004), health care (Antonsson, Graneheim, Lundström, & Åström, 2008; Hansebo & Kihlgren, 2001; Mollo & Falzon, 2008; Skovdahl, Kihlgren, & Kihlgren, 2004), education (Dershimer & Conover, 1989; Lyle, 2003), and consulting (Lyddon, Yowell, & Hermans, 2006). For instance, Faye and Falzon (2009) used individual auto-confrontation to assess automotive manufacturing worker self-monitoring of performance and characterize strategies developed by workers. Another study involving a group of oncology practitioners making therapeutic decisions used allo-confrontation to understand the effects of collective confrontation on individual decision-making activities and collective knowledge construction and development (Mollo & Falzon, 2008). Mollo and Falzon (2004) used both auto-confrontation and allo-confrontation methods to assess saffron producers’ technical knowledge based on their actual work practices. The strengths of stimulated recall methodology include ecological validity (Derosier et al., 2008; Lyle, 2003; Mollo & Falzon, 2004), assessment of non-observable cognitive processes (Dershimer & Conover, 1989; Elderkin-Thompson & Waitzkin, 1999; Faye & Falzon, 2009; Lyddon et al., 2006; Lyle, 2003; Skovdahl et al., 2004), enhancement of worker knowledge regarding their own work activities (Antonsson et al., 2008; Dershimer & Conover, 1989; Hansebo & Kihlgren, 2001; Mollo & Falzon, 2008), and assessment of the collaborative process through collective confrontation (Lyddon et al., 2006; Mollo & Falzon, 2008). The weaknesses of stimulated recall include time needed to implement the methodology (Dershimer & Conover, 1989; Mollo & Falzon, 2004), challenges in facilitating knowledge sharing among participants (Dershimer & Conover, 1989; Mollo & Falzon, 2004; Skovdahl et al., 2004), possible discomfort experienced by participants (Hansebo & Kihlgren, 2001; Lyle, 2003), and possible biases introduced by interviewers (Lyle, 2003).
1.2 Study aims and objectives
In this study, we implemented and evaluated the use of a stimulated recall methodology for collective confrontation in the context of FCR. The objective of the stimulated recall methodology was to identify work system barriers and facilitators in FCR from the viewpoint of the rounding participants. Stimulated recall that combines directed content analysis with video-recording review allows participants to identify cognitive processes that are not physically observable (Faye & Falzon, 2009; Mollo & Falzon, 2004). In our study, stimulated recall allowed families and healthcare team members to become analysts of their own activity. When families and healthcare team members analyze their own activity, they can reflect on their own practices during FCR and identify not only what they do, but also the work system factors that either facilitate or hinder family engagement during FCR.
The work system model developed by Smith and Carayon (Carayon, 2009; Carayon & Smith, 2000; Smith & Carayon-Sainfort, 1989) and its extension to healthcare and patient safety (SEIPS or Systems Engineering Initiative for Patient Safety model) (Carayon et al., 2006; Carayon et al., 2014) were used as the conceptual framework for identifying system barriers and facilitators. The aim of this paper was to demonstrate how the stimulated recall methodology can be used to assess work system barriers and facilitators to family engagement in the FCR process.
2. Methods
In the context of a large project aimed at improving family engagement in FCR in a pediatric hospital, we video-recorded FCR and interviewed rounding participants using a stimulated recall methodology. The University of Wisconsin-Madison Health Sciences Institutional Review Board approved this study.
2.1 Setting and sample
The study was conducted at a children’s hospital in the Midwest of the US where FCR are expected to be conducted daily with the family and the patient’s healthcare team members. One researcher operated the camera to record the full session of FCR if possible. To ensure the operator did not influence the rounding process, the operator did not speak or engage with rounding participants. Video-recordings were selected for use in the interview process if (1) we recorded the full session at sufficient audio and video quality to support the stimulated recall analysis, (2) the family was willing to complete the stimulated recall interview, and (3) all persons appearing in the video had given consent to have the video used for this purpose. This produced a total of 37 interviews with healthcare team members, families and patients admitted to one of four inpatient services: two hospitalist services, one pulmonary service, and one hematology/oncology service. Because of a delay in the research process, only 11 of the 37 participants were asked to fill out an evaluation survey on the stimulated recall process. One participant who did not indicate his/her role on the healthcare team member was excluded from data analysis, which limited the final sample to 5 parents and 5 healthcare team members (2 attending physicians, 2 resident physicians, and 1 nurse). This sample represents the range of stakeholders involved in FCR.
2.2 Data collection
Families and members of the healthcare team were asked to review a video-recording of their own rounding session. The stimulated recall methodology consisted of two steps: (1) review of the video by the family or the healthcare team member, and (2) discussion of work system barriers and facilitators of family engagement evident in the video. Participants were able to rewind or pause the video as needed. The discussion between the interviewer and the interviewee of barriers and facilitators was organized around the work system model: probes covered each of the five work system elements, i.e. people, tasks, organization, environment, and tools and technology (Carayon, 2009; Carayon & Smith, 2000; Smith & Carayon-Sainfort, 1989). All stimulated recall interviews were audio-recorded. The duration of the ten interviews ranged from 20 to 56 minutes (mean=43 minutes, SD=10 minutes).
A survey was used to evaluate stimulated recall interviews from the viewpoint of the participants. The survey included three questions used with both healthcare team members and parents: “How comfortable or uncomfortable was this interview process for you?” “How easy or difficult was this interview process for you?” and “How clear or unclear was the purpose of the interview?” The response categories were on a 4-point scale (1 = very comfortable/easy/clear, 2 = comfortable/easy/clear, 3 = uncomfortable/difficult/unclear and 4 = very uncomfortable/difficult/unclear). Healthcare team members were asked one additional question: “To what extent did this experience change how you would do things in your practice in the future?” The responses were on a 4-point scale (1 = change a lot, 2 = moderate change, 3 = a little change and 4 = no change). At the end of the survey, we encouraged participants to provide comments or suggestions about the interview experience by asking them, “What, if anything, was interesting about the interview process?” and “Is there anything else you would like us to know about your interview experience?”
2.3 Data analysis
The evaluation of the stimulated recall methodology relied on an analysis of the survey data to assess participants’ perceptions of the methodology, and a content analysis of the data produced by the methodology to assess the completeness of the information on work system barriers and obstacles.
Survey data were analyzed using descriptive statistics. The audio-recordings of interviews conducted with the 10 participants were reviewed, and instances of strategies aimed at enhancing family engagement on FCR were identified. Conversations around these instances were transcribed from audio recordings. The transcribed interview data were then transferred in the qualitative data analysis software QSR NVivo© version 9.0. The researchers performed a qualitative content analysis of the transcripts (Graneheim & Lundman, 2004), using a combination of both deductive content analysis and an inductive approach (Elo & Kyngäs, 2008). The deductive analysis was guided by the work system model and its five elements: people, tasks, environment, organization, and technology and tools (Carayon, 2009; Carayon & Smith, 2000; Smith & Carayon-Sainfort, 1989). The sub-categories were derived from the data in an inductive way as described by Elo and Kyngäs (2008). A node structure was developed through an iterative, consensus-based process. The interviews were reviewed several times to obtain a sense of the whole and to achieve consistency in coding by three researchers. Two interviews were coded individually and then discussed by three researchers. We developed a preliminary node structure based on the work system model (Carayon et al., 2011). Two researchers coded the 10 interviews and the node structure was revised. The final coding was done and barriers and facilitators were categorized by two researchers, and confirmed by another researcher.
3. Results
The evaluation of the stimulated recall methodology relied on two approaches: (1) survey of participants about the methodology, and (2) review of interview data produced by the methodology in light of the work system model.
3.1 Analysis of survey data
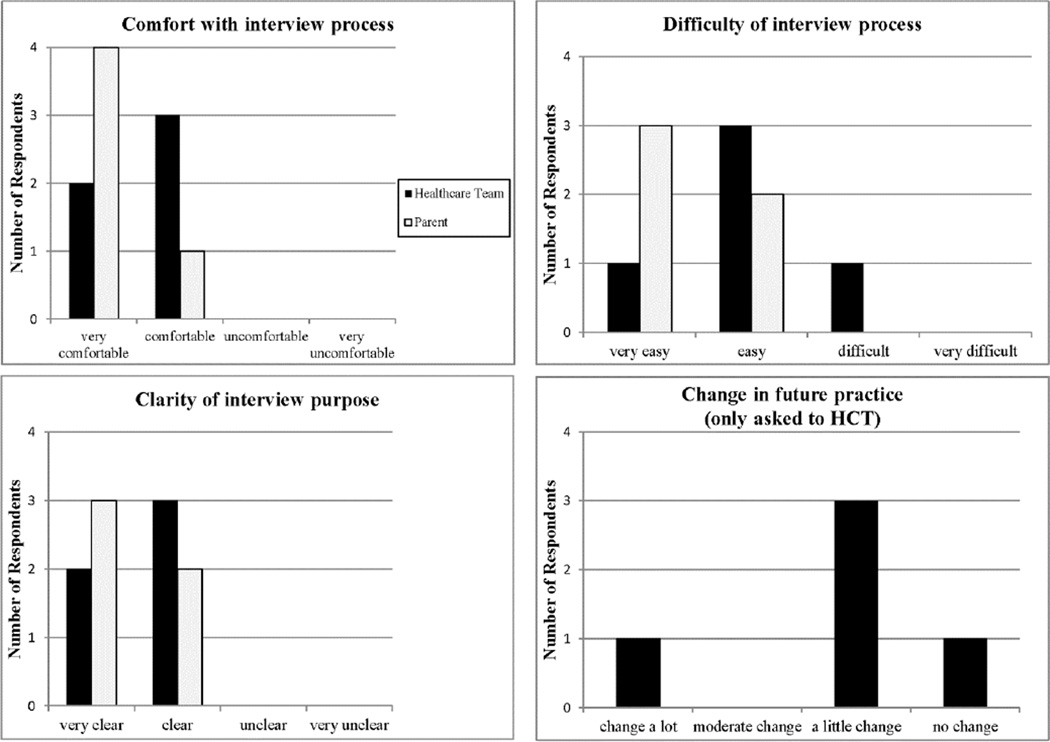
Half of the survey respondents were healthcare team members and the other half were parents. Figure 1 show a summary of the survey data.
Figure 1.
Participants’ perceptions of the stimulated recall interview process [5 parents and 5 healthcare team (HCT) members]
All respondents felt comfortable or very comfortable with the stimulated recall interview process. Positive factors mentioned by the respondents included ease of talking with the interviewer, an informal conversation atmosphere, and comfortable environment. One factor contributing to discomfort was for participants to see themselves in the video. Nine of the ten respondents felt the interview process was easy or very easy. Facilitators included a convenient interview schedule, the informal interview process that lowered the pressure on participants, good followup questions, having ability to pause the video-recording, and talking about their likes and dislikes regarding rounds. The only difficulty was mentioned by a parent who talked about the challenge of “reviewing” their child’s health situation. All ten respondents thought the purpose of the interview was clear or very clear. The only suggestion made by a healthcare team respondent was that he/she “[…] needed prompting questions.”
Four of the five healthcare providers said that they would change their rounding practices in the future by changing: (1) their own behaviors (e.g., “do more bedside teaching”, “the way I stand during the rounds”, “maintaining a look of engagement”), (2) their interaction with families (e.g., “all parents are given a clear opportunity/ invitation to speak”, “reminded me to pay attention to family cues”, “update on current plans for your patient”), and (3) their interaction with other clinicians (e.g., “make sure bedside nurse is at rounds”, “I would like senior resident to talk more.”)
Responses to the survey open-ended question provided comments and suggestions on the stimulated recall methodology that covered a range of issues, including observations of the rounding process (e.g., “think about the logistics of rounds and interesting to see process”), one’s own behaviors (e.g., “helped me reflect on my rounding style and priorities and made me aware of ways I can improve them”), and interactions between clinicians and families (e.g., “how we interact with and try to reassure families”). All comments from parents were positive; they talked about the quality of the rounding session they participated in and the resulting care provided by healthcare professionals (e.g., “good to participate in a process to improve rounds for all patients/families going forward” and “[…] felt always included in the care of my child which matters most”). One parent felt the stimulated recall methodology was a pleasant experience that he/she would participate in again. Another parent described the interview as a good learning experience: “I could view the tape and really see what was said to see if I was understanding the residents. This is a good tool for learning.”
3.2 Analysis of interview data
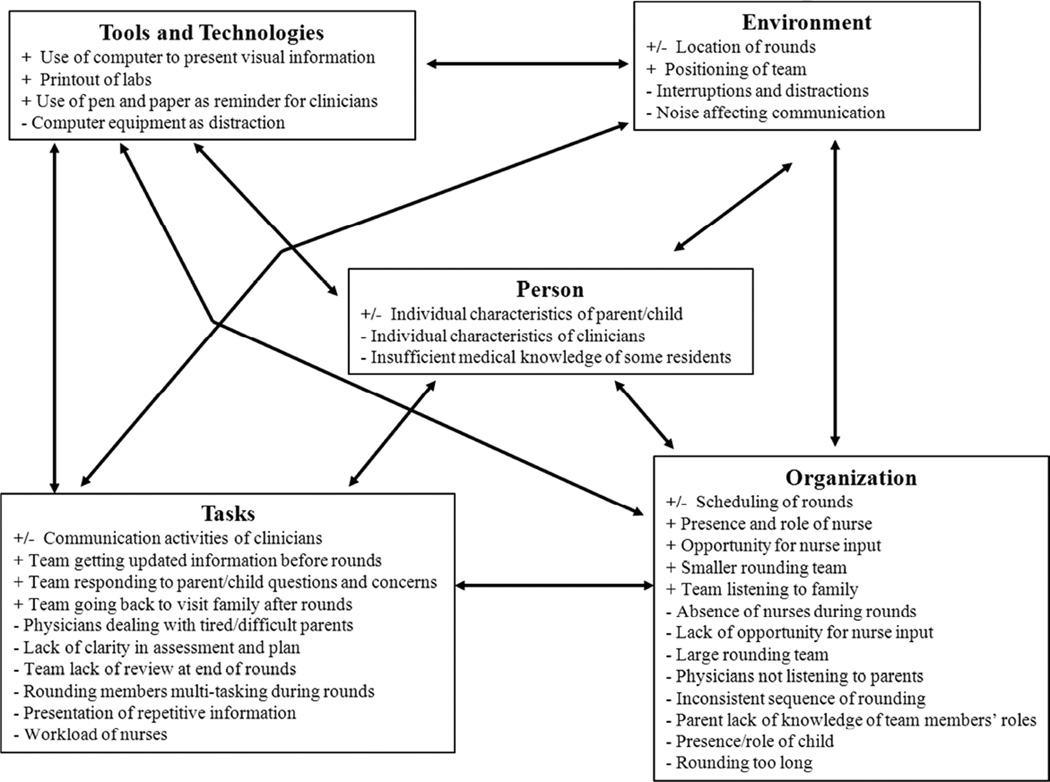
The content analysis of the stimulated recall interview data identified a range of work system barriers and facilitators to family engagement in rounds (see Figure 2 and Appendix for detailed information); specific examples are described below.
Figure 2.
Work system barriers and facilitators to family engagement in family-centered rounds (FCR). The “+” symbol indicates a facilitator and the “−” symbol indicates a barrier.
Note that barriers and facilitators are assigned to one work system element; however, many system elements interact with each other. See examples in the text.
Individual characteristics of the parent, such as their lack of confidence in asking questions (“when I first started, it was really hard for me to speak up”) and fatigue (“[parent] maybe hasn’t got that much sleep overnight; things were crazy”), can limit their engagement. Parents with medical knowledge are more likely to understand the rounding presentation and be more involved. Lack of communication skills of clinicians can also be a barrier to family engagement during rounds.
With regard to tasks, communication activities of clinicians can limit family engagement if there is no eye contact with parents or excessive use of medical jargon (“I feel like we’re almost into the habit of saying what all the numbers are… I think the lab value is confusing for the majority of the patients”). When team members respond to parents’ questions or concerns, this enhances family engagement during rounds.
A range of organizational barriers and facilitators were also identified. For instance, appropriately scheduling rounds (“the nurse at that time did give me the forewarning that rounds would be coming… and I was prepared for that”) and role clarity of clinicians (“they [parents] really want to know what your role is on the team, that might help people figure out what the different roles are on the team”) can facilitate the rounding process. In contrast, delayed rounds (“that is a huge source of frustration for patients and families”) and absence of nurses during rounds (“sometimes them [nurses] are not there, and to me this is definitely a drawback”) are considered as major barriers to family engagement.
Environmental barriers include interruptions and distractions (“when they [rounding team] come in, to maybe talk to the kid, could you please turn that [TV] down or off”). Environmental facilitators include positioning of team, such as clinicians standing close to each other and sitting down with the parent and the child.
Figure 2 shows barriers and facilitators associated with specific work system elements; however, there are numerous interactions between themes across the five work system elements. For instance, high workload of nurses who have to care for multiple patients (task) may result in their absence during rounds (organization) and limit their opportunity to provide input (organization). For example, a parent was saying: “The nurse is in another kid’s room… maybe they need to see if they can get another nurse to step in… because for me it’s really important that my nurse is there.” When the rounding team is large (organization), when rounds occur outside of the room (environment), or when rounding members perform multiple tasks (task), interruptions, distractions and noise are more likely to occur (environment) and affect communication as indicated by one parent: “the commotion in the hallway is loud”, and one resident physician: “Everybody is multi-tasking … you remove some of these distractions, it [the round] would be focusing on the patient”. Similarly, parent confidence to ask questions (person) and use of computer to present visual information (tool) can facilitate parent engagement during rounds, as indicated by a nurse: “when talking about engaging family in, I think that the best way to do it was to bring the actual computer screen in to show them [families] the picture…the visual is extremely helpful for that family.”
Some work system factors can be both barriers and facilitators. For example, use of the computer could be a distraction (barrier) or a good way to present visual information to engage the family (facilitator). The following quotes illustrate this: “I don’t think the person presenting or doing the conversation with the family should have technology in front of them. It seems distractive.” “I think that the best way to do it is bringing the actual computer screen in to show them [family] the picture.”
4. Discussion
Our study demonstrated how the stimulated recall methodology can be used to assess work system barriers and facilitators to family engagement in FCR. The evaluation relied on two methods: a survey of participants and an analysis of the data produced by the stimulated recall methodology. The positive survey feedback from participants highlights their feelings of comfort and trust, assuring their ability to freely discuss their experiences with FCR. When they reflected upon their own activities during rounds, parents raised concerns and proposed suggestions for improving the rounding process. Healthcare providers paid more attention to their interactions with families when reviewing the video-recordings. The value of the stimulated recall methodology was also seen in the participants’ responses to open-ended questions in the survey.
The small sample of participants who filled out the surveys limited our ability to evaluate the stimulated recall methodology. Data from a larger sample would have provided more convincing evidence about the value of the methodology from the participants’ viewpoint. In addition, the process of reviewing the video-recording of rounds could have also influenced the participants and their evaluation of the rounding process.
This study shows that the stimulated recall methodology was able to identify a range of work system barriers and facilitators to family engagement during rounds that addressed all five elements of the work system model. The procedure of reviewing the video-recordings of the rounding process helped to focus participants’ attention on specific rather than general issues (Dershimer & Conover, 1989), which generated a rich dataset to help us identify various factors that either facilitate or hinder family engagement during rounds. Data were categorized according to the work system model (Carayon, 2009; Smith & Carayon-Sainfort, 1989) and addressed all of the system elements.
This information can be used to redesign the rounding process; this is the next step of the larger project in which this study is embedded (Kelly et al., 2013). For example, some parents lack the confidence to ask questions; one possible strategy to deal with this barrier to family engagement is to let the nurse represent the family and assist in advocating for the patient and family. Regarding the problem that nurses are absent during rounds, several strategies might help, such as scheduling rounds and letting nurses know about schedule, or delegation of nurses’ tasks to others so that they can participate in rounds.
The stimulated recall methodology is one way of including “workers” (i.e. parents and healthcare team members) in the analysis of a process. This fits with participatory ergonomics that advocates for worker involvement in human factors and ergonomics analysis (Haims & Carayon, 1998; J. R. Wilson & Haines, 1997). In this study, the participatory ergonomics approach with stimulated recall interviewing allowed for the assessment of multiple viewpoints, i.e. healthcare professionals and parents. This collective confrontation is important in complex healthcare processes that involve various stakeholders.
Future research could investigate how to take advantage of the self-reflection opportunity of the stimulated recall methodology to train healthcare team members to improve their rounding practice. According to the survey data, four of the five healthcare team members indicated that they would change their rounding practices in the future. Therefore, the stimulated recall methodology using video-recording may be an effective method to encourage healthcare professionals in changing their behaviors. Future research could also examine the role of stimulated recall methodology in teaching clinicians communication skills and ways to engage families and patients in care, similar to the use of video-recording for behavior modeling training (May & Kahnweiler, 2000).
5. Conclusion
HFE methods, such as the stimulated recall methodology, can provide opportunities for a range of participants, including parents and children, to become involved in improving healthcare processes. This study demonstrates the value of the stimulated recall methodology to identify a range of work system factors that either positively or negatively influence family engagement during FCR. Stimulated recall or ‘confrontation’ methods have been typically used with single workers; we have extended the methodology to teamwork where multiple individuals (e.g., physician, nurse, parent) communicate and collaborate to provide and/or support patient care. Understanding the viewpoints of the various stakeholders in the rounding process is critical to ensure that their needs are adequately addressed (Xie et al., 2012).
Highlights.
Parents and healthcare team members who reviewed video records of their bedside rounds participated in the analysis of work system barriers and facilitators in familycentered rounds.
The stimulated recall methodology was positively received by parents and healthcare team members.
The stimulated recall methodology allowed the identification of a wide range of work system barriers and facilitators in family-centered rounds.
Stimulated recall methodology can be used to improve healthcare work systems and processes.
Acknowledgments
Funding for this study was provided by the National Patient Safety Foundation and the Agency for Healthcare Research and Quality (R18-HS018680). This study was also partially supported by the Clinical and Translational Science Award (CTSA) program, previously through the National Center for Research Resources (NCRR) grant 1UL1RR025011, and now by the National Center for Advancing Translational Sciences (NCATS), grant 9U54TR000021. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Appendix. Detailed analysis of work system barriers and facilitators to family engagement in family-centered rounds (FCR)
| Work system elements |
Barriers | Facilitators |
|---|---|---|
| P | Individual characteristics of parent/child
|
Individual characteristics of parent/child
|
| P | Individual characteristics of clinicians
|
|
| P | Insufficient medical knowledge of some residents | |
| T | Communication activities of clinicians
|
Communication activities of clinicians
|
| T | Physicians dealing with tired/difficult parents | |
| T | Lack of clarity in assessment and plan | |
| T | Team lack of review at end of rounds | |
| T | Rounding members multi-tasking during rounds | |
| T | Presentation of repetitive information | |
| T | Workload of nurses | |
| T | Team getting updated information before rounds | |
| T | Team responding to parent/child questions and concerns | |
| T | Team going back to visit family after rounds | |
| O | Scheduling rounds
|
Scheduling of rounds
|
| O | Absence of nurses during rounds | Presence and role of nurse |
| O | Lack of opportunity for nurse input | Opportunity for nurse input |
| O | Large rounding team | Smaller rounding team |
| O | Physicians not listening to parents | Team listening to family |
| O | Inconsistent sequence of rounding | |
| O | Parent lack of knowledge of team members’ roles | |
| O | Presence/role of child
|
|
| O | Rounding too long | |
| O | Team coming into round with a preliminary plan | |
| O | Introduction of team members to family | |
| O | Role of attending as a leader or teacher | |
| O | Role clarity of clinicians | |
| O | Opportunity for parent input | |
| O | Parent involvement during rounds | |
| O | Rapport between parents and clinicians | |
| E | Location of rounds
|
Location of rounds
|
| E | Interruptions and distractions | |
| E | Noise affecting communication | |
| E | Positioning of team
|
|
| T-T | Computer equipment as distraction | |
| Use of computer to present visual information | ||
| T-T | Printout of labs | |
| T-T | Use of pen and paper as reminder for clinicians |
Note: P=person; T=tasks; O=organization; E=environment; T-T=tools and technologies (elements of the work system model (Carayon, 2009; Carayon & Smith, 2000; Smith & Carayon-Sainfort, 1989))
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Antonsson H, Graneheim UH, Lundström M, Åström S. Caregivers' reflections on their interactions with adult people with learning disabilities. Journal of Psychiatric and Mental Health Nursing. 2008;15(6):484–491. doi: 10.1111/j.1365-2850.2008.01259.x. [DOI] [PubMed] [Google Scholar]
- Carayon P. The Balance Theory and the work system model… Twenty years later. International Journal of Human-Computer Interaction. 2009;25(5):313–327. [Google Scholar]
- Carayon P, DuBenske LL, McCabe BC, Shaw B, Gaines ME, Kelly MM, Cox ED. Work system barriers and facilitators to family engagement in rounds in a pediatric hospital. In: Albolino S, Bagnara S, Bellandi T, Llaneza J, Rosal G, Tartaglia R, editors. Healthcare Systems Ergonomics and Patient Safety. Vol. 2011. Boca Raton, FL: CRC Press; 2011. pp. 81–85. [Google Scholar]
- Carayon P, Hundt AS, Karsh B-T, Gurses AP, Alvarado CJ, Smith MJ, Brennan PF. Work system design for patient safety: The SEIPS model. Quality & Safety in Health Care. 2006;15(Supplement I):i50–i58. doi: 10.1136/qshc.2005.015842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayon P, Smith MJ. Work organization and ergonomics. Applied Ergonomics. 2000;31:649–662. doi: 10.1016/s0003-6870(00)00040-5. [DOI] [PubMed] [Google Scholar]
- Carayon P, Wetterneck TB, Rivera-Rodriguez AJ, Hundt AS, Hoonakker P, Holden R, Gurses AP. Human factors systems approach to healthcare quality and patient safety. Applied Ergonomics. 2014;45(1):14–25. doi: 10.1016/j.apergo.2013.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Committee on Drugs, & Committee on Hospital Care. Prevention of medication errors in the pediatric inpatient setting. Pediatrics. 2003;112(2):431–436. doi: 10.1542/peds.112.2.431. [DOI] [PubMed] [Google Scholar]
- Committee on Hospital Care, & Institute for Patient- Family-Centered Care. Patient- and family-centered care and the pediatrician's role. Pediatrics. 2012;129(2):394–404. doi: 10.1542/peds.2011-3084. [DOI] [PubMed] [Google Scholar]
- Derosier C, Leclercq S, Rabardel P, Langa P. Studying work practices: A key factor in understanding accidents on the level triggered by a balance disturbance. Ergonomics. 2008;51(12):1926–1943. doi: 10.1080/00140130802567061. [DOI] [PubMed] [Google Scholar]
- Dershimer RA, Conover S. The stimulated recall technique: a qualitative evaluation of an in-service workshop. Hospice Journal. 1989;5(2):85–93. doi: 10.1080/0742-969x.1989.11882651. [DOI] [PubMed] [Google Scholar]
- Elderkin-Thompson V, Waitzkin H. Using videotapes in qualitative research. In: Crabtree BF, Miller WL, editors. Doing Qualitative Research. 2nd ed. Thousand Oaks, CA: Sage Publications; 1999. pp. 239–252. [Google Scholar]
- Elo S, Kyngäs H. The qualitative content analysis process. Journal of Advanced Nursing. 2008;62(1):107–115. doi: 10.1111/j.1365-2648.2007.04569.x. [DOI] [PubMed] [Google Scholar]
- Faye H, Falzon P. Strategies of performance self-monitoring in automotive production. Applied Ergonomics. 2009;40(5):915–921. doi: 10.1016/j.apergo.2009.01.005. [DOI] [PubMed] [Google Scholar]
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Education Today. 2004;24(2):105–112. doi: 10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Gurses AP, Xiao Y. A systematic review of the literature on multidisciplinary rounds to design information technology. 2006:267–276. doi: 10.1197/jamia.M1992. (1067–5027 (Print)) [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haims MC, Carayon P. Theory and practice for the implementation of 'in-house', continuous improvement participatory ergonomic programs. Applied Ergonomics. 1998;29(6):461–472. doi: 10.1016/s0003-6870(98)00012-x. [DOI] [PubMed] [Google Scholar]
- Hansebo G, Kihlgren M. Carers' reflections about their video-recorded interactions with patients suffering from severe dementia. Journal of Clinical Nursing. 2001;10(6):737–747. doi: 10.1046/j.1365-2702.2001.00558.x. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21 st Century. Washington, DC: National Academy Press; 2001. [Google Scholar]
- Kaushal R, Bates DW, Landrigan C, McKenna KJ, Clapp MD, Federico F, Goldmann DA. Medication errors and adverse drug events in pediatric inpatients. Journal of the American Medical Association. 2001;285(16):2114–2120. doi: 10.1001/jama.285.16.2114. [DOI] [PubMed] [Google Scholar]
- Kelly MM, Xie A, Carayon P, DuBenske LL, Ehlenbach ML, Cox ED. Strategies for improving family engagement during family-centered rounds. Journal of Hospital Medicine. 2013 doi: 10.1002/jhm.2022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landrigan CP. The safety of inpatient pediatrics: Preventing medical errors and injuries among hospitalized children. Pediatric Clinics of North America. 2005;52(4):979–993. doi: 10.1016/j.pcl.2005.05.001. [DOI] [PubMed] [Google Scholar]
- Lyddon WJ, Yowell DR, Hermans HJM. The self-confrontation method: Theory, research, and practical utility. Counselling Psychology Quarterly. 2006;19(1):27–43. [Google Scholar]
- Lyle J. Stimulated Recall: A report on its use in naturalistic research. British Educational Research Journal. 2003;29(6):861–878. [Google Scholar]
- May GL, Kahnweiler WM. The effect of a mastery practice design on learning and transfer in behavior modeling training. Personnel Psychology. 2000;53(2):353–373. [Google Scholar]
- Mollo V, Falzon P. Auto- and allo-confrontation as tools for reflective activities. Applied Ergonomics. 2004;35(6):531–540. doi: 10.1016/j.apergo.2004.06.003. [DOI] [PubMed] [Google Scholar]
- Mollo V, Falzon P. The development of collective reliability: A study of therapeutic decision-making. Theor. Issues Ergonomics. 2008;9(3):223–254. [Google Scholar]
- Scanlon MC, Karsh B-T, Densmore EM. Human factors engineering and patient safety. Pediatric Clinics of North America. 2006;53(6):1105–1119. doi: 10.1016/j.pcl.2006.09.012. [DOI] [PubMed] [Google Scholar]
- Sisterhen LL, Blaszak RT, Woods MB, Smith CE. Defining Family-Centered Rounds. Teaching and Learning in Medicine. 2007;19(3):319–322. doi: 10.1080/10401330701366812. [DOI] [PubMed] [Google Scholar]
- Skovdahl K, Kihlgren AL, Kihlgren M. Dementia and aggressiveness: stimulated recall interviews with caregivers after video-recorded interactions. Journal of Clinical Nursing. 2004;13(4):515–525. doi: 10.1046/j.1365-2702.2003.00881.x. [DOI] [PubMed] [Google Scholar]
- Smith MJ, Carayon-Sainfort P. A balance theory of job design for stress reduction. International journal of industrial ergonomics. 1989;4(1):67–79. [Google Scholar]
- Wilson BL. Keeping an eye on patient safety using human factors engineering (HFE): A family affair for the hospitalized child. Journal for Specialists in Pediatric Nursing. 2010;15(1):84–87. doi: 10.1111/j.1744-6155.2009.00221.x. [DOI] [PubMed] [Google Scholar]
- Wilson JR, Corlett N, editors. Evaluation of Human Work. Third ed. Boca Raton, FL: CRC Press; 2005. [Google Scholar]
- Wilson JR, Haines HM. Participatory ergonomics. In: Salvendy G, editor. Handbook of Human Factors and Ergonomics. New York: John Wiley & Sons; 1997. pp. 490–513. [Google Scholar]
- Xie A, Carayon P, Kelly MM, Li Y, Cartmill R, DuBenske LL, Cox ED. Managing different perspectives in the redesign of family-centered rounds in a pediatric hospital. In: The Human Factors and Ergonomics Society, editor. Proceedings of the Human Factors and Ergonomics Society 56 th Annual Meeting. Santa Monica, CA: The Human Factors and Ergonomics Society; 2012. pp. 1733–1737. [Google Scholar]