Abstract
BACKGROUND
Elevated body mass index (BMI) and waist circumference (WC) are associated with increased mortality risk, but it is unclear which anthropometric measurement most highly relates to mortality. We examined single and combined associations between BMI, WC, waist–hip ratio (WHR) and all-cause, cardiovascular disease (CVD) and cancer mortality.
METHODS
We used Cox proportional hazard regression models to estimate relative risks of all-cause, CVD and cancer mortality in 8061 adults (aged 18–74 years) in the Canadian Heart Health Follow-Up Study (1986–2004). Models controlled for age, sex, exam year, smoking, alcohol use and education.
RESULTS
There were 887 deaths over a mean 13 (SD 3.1) years follow-up. Increased risk of death from all-causes, CVD and cancer were associated with elevated BMI, WC and WHR (P < 0.05). Risk of death was consistently higher from elevated WC versus BMI or WHR. Ascending tertiles of each anthropometric measure predicted increased CVD mortality risk. In contrast, all-cause mortality risk was only predicted by ascending WC and WHR tertiles and cancer mortality risk by ascending WC tertiles. Higher risk of all-cause death was associated with WC in overweight and obese adults and with WHR in obese adults. Compared with non-obese adults with a low WC, adults with high WC had higher all-cause mortality risk regardless of BMI status.
CONCULSION
BMI and WC predicted higher all-cause and cause-specific mortality, and WC predicted the highest risk for death overall and among overweight and obese adults. Elevated WC has clinical significance in predicting mortality risk beyond BMI.
Keywords: waist circumference, body mass index, mortality, cardiovascular, cancer
INTRODUCTION
Elevated body mass index (BMI) and waist circumference (WC) are associated with increased mortality risk,1 yet it is uncertain which clinical measure is the most important predictor for mortality. Differences in the associations between anthropometric measures of obesity and cardiovascular disease (CVD) may not be clinically significant,2 as high BMI, WC and waist–hip ratio (WHR) are each associated with increased risk for heart failure3 and CVD mortality.4 Although there is also an established link between obesity and cancer,1 evidence is especially limited on which anthropometric measure best predicts the associated mortality risk.5 As the degree and distribution of obesity are major criteria for drug and surgical interventions,6 it is important to examine what measure of adiposity confers higher mortality risk. Our aim was to determine the individual and combined associations between BMI, WC and WHR with all-cause, CVD and cancer mortality.
MATERIALS AND METHODS
Survey design and participants
The Canadian Heart Health Survey Follow-Up Study is a longitudinal follow-up of the Canadian Heart Health Survey (CHHS), a national survey of men and women using a stratified, two-stage probability sample of health insurance registries.7 , 8 The original surveys were administered in all 10 provinces between 1986 and 1992, with a second survey in Nova Scotia in 1995. The present analyses were limited to provinces that measured WC and also provided permission for linkage to the Canadian Mortality Database (CMDB), which included Alberta, Manitoba, Saskatchewan and Nova Scotia (1995 only). A total of 8061 participants remained after excluding for missing anthropometric measurements (n=356), death occurring within 6 months of the survey (n=22), age of 75 years or older (n=300), missing alcohol status (n=3) or missing education status (n=31).
Anthropometric data
Anthropometric measurements were obtained in clinic the morning after a 12-h fast. Height and weight were assessed with a calibrated balance beam scale and BMI was calculated (kgm−2). Circumferences were measured using an inelastic tape measure and rounded to the nearest cm. WC (cm) was measured at the level of the minimal waist or at the twelfth or lower floating rib, at the end of normal expiration. Hip circumference (HC; cm) was measured at the maximal gluteal protuberance and WHR was calculated as the ratio of WC divided by HC.
Other variables
An interviewer-administered questionnaire provided information on smoking (never, former, current); alcohol use (never, former, current); and educational attainment (elementary school or less, some secondary school, completed secondary school or completed university degree). Age, sex and year of examination were additional covariates.
Follow-up and outcome measures
Death registrations from each province for the years 1986–2004 were extracted from the CMDB and linked with the CHHS data by Statistics Canada.9 Specific causes of death were based on the International Classification of Diseases (ICD) code for CVD mortality (ICD-9: 390– 448; ICD-10: I00– I78) and for cancer mortality (ICD-9: 140– 239; ICD-10: C00–D48). There was a very small potential for missed deaths in the computerized probabilistic matching procedures used.10 The linkage between CMDB and CHHS was approved by the Institutional Review Boards at each participating institution.
Statistical analysis
Baseline differences between survivors and decedents were determined by t-tests for continuous variables and χ2 tests for categorical variables. Relationships among the three anthropometric measures were assessed by partial correlations adjusted for age and sex.
We used Cox proportional hazard regression models to assess the association between anthropometric measures and mortality. We estimated hazard ratios (HRs) with 95% confidence intervals (CIs). BMI, WC and WHR were individually examined for association with all-cause; CVD (ischemic heart disease, stroke and congestive heart failure or other); and cancer (prostate, breast, colon, lung, and other) mortality. Relative risks were expressed per sex-specific standard deviation of each anthropometric index, and in a second analysis, were categorized into tertiles overall and within BMI category (normal weight, overweight or obese) to examine dose-response relationships. Participants were also classified into four groups based on WC and obesity status (high WC if WCX102 cm for men and WC X88 cm for women; obese if BMIX30; National Institute of Health, National Heart, Lung, and Blood Institute (NHLBI)).11 Cox proportional hazard regression models were used to compare all-cause mortality risk of low WC obese (n=281), high WC non-obese (n=722) and high WC obese (n=1308) groups with the low WC non-obese (n=5750) group. Models included age, sex, exam year, smoking, alcohol consumption and education as covariates. SAS software (V.9.2., Cary, NC, USA) was used to conduct analyses.
RESULTS
Mean follow-up occurred at 13 years (range 0.5–15.5 years) over a total of 105 041 person years. There were 547 deaths in men (204 from CVD, 195 from cancer) and 340 deaths in women (112 from CVD, 124 from cancer). Decedents were older and had higher BMI, WC and WHR (Table 1). When controlling for age and sex, BMI was significantly correlated with WC (r=0.84) and WHR (r=0.46), and WC and WHR were significantly correlated (r=0.73).
Table 1.
Characteristics of 8061 adults in the Canadian Heart Health Survey
|
Men |
Women |
|||||
|---|---|---|---|---|---|---|
|
Survivors n = 3456 |
Decedents n = 547 |
P-value |
Survivors n = 3718 |
Decedents n = 340 |
P-value | |
| Person-years | 46829 | 4591 | 50589 | 3032 | ||
| Follow-up time, years (s.d.) | 13.6 (2.5) | 8.4 (4) | <0.0001 | 13.6 (2.5) | 8.9 (4.1) | <0.0001 |
| Age, years (s.d.) | 41.7 (16.1) | 64.6 (10.3) | <0.0001 | 42.3 (16.2) | 65.2 (10) | <0.0001 |
| Body mass index, kg m −2 (s.d.) | 26.7 (4.6) | 27.3 (4.4) | 0.002 | 25.7 (5.4) | 27.6 (6) | <0.0001 |
| Waist circumference, cm (s.d.) | 92.7 (12.1) | 98.7 (11.6) | <0.0001 | 79.8 (13.1) | 88.7 (15) | <0.0001 |
| Waist – hip ratio | 0.91 (0.07) | 0.96 (0.06) | <0.0001 | 0.79 (0.07) | 0.84 (0.08) | <0.0001 |
| Smoking status, % | <0.0001 | 0.824 | ||||
| Never | 29.5 | 12.4 | 43 | 42.9 | ||
| Former | 39.5 | 57 | 30.4 | 29.1 | ||
| Current | 31.1 | 30.5 | 26.6 | 27.9 | ||
| Alcohol Consumption, % | <0.0001 | |||||
| Never | 1.8 | 1.8 | 4.3 | 14.4 | <0.0001 | |
| Former | 11.3 | 20.7 | 13 | 24.4 | ||
| Current | 86.9 | 77.5 | 82.7 | 61.2 | ||
| Education, % | <0.0001 | <0.0001 | ||||
| Elementary school or less | 3.6 | 9 | 2.3 | 10 | ||
| Some secondary school | 26.5 | 52.1 | 26 | 47.7 | ||
| Secondary school completed | 49.4 | 30 | 54 | 31.5 | ||
| University degree completed | 20.6 | 9 | 17.7 | 11 | ||
Single associations of each anthropometric measure with mortality risk revealed that BMI, WC and WHR positively predicted all-cause, CVD and cancer mortality. All three adiposity measures were positively associated with ischemic heart disease mortality risk, and BMI and WC associated with mortality risk from colon cancer and other cancers. Across all-cause and cause-specific mortalities, WC consistently had higher relative risk estimates compared with BMI or WHR (Table 2).
Table 2.
Adjusted Cox proportional hazard ratios for all-cause and cause-specific mortality per s.d. of body mass index, waist circumference or waist – hip ratio
|
HR (95% CI) |
||||
|---|---|---|---|---|
| Deaths | BMI | WC | WHR | |
| All-cause | 887 | 1.10 (1.03 – 1.18) | 1.19 (1.11 – 1.27) | 1.15 (1.07 – 1.23) |
| Cardiovascular disease | 316 | 1.23 (1.09 – 1.37) | 1.33 (1.19 – 1.48) | 1.22 (1.09 – 1.37) |
| Ischemic heart disease | 169 | 1.28 (1.10 – 1.48) | 1.35 (1.16 – 1.57) | 1.21 (1.03 – 1.42) |
| Stroke | 63 | 1.10 (0.84 – 1.44) | 1.29 (0.99 – 1.67) | 1.24 (0.96 – 1.61) |
| Congestive heart failure and other | 84 | 1.22 (0.98 – 1.52) | 1.34 (1.08 – 1.66) | 1.24 (0.99 – 1.55) |
| Cancer | 319 | 1.13 (1.01 – 1.27) | 1.23 (1.10 – 1.37) | 1.16 (1.03 – 1.30) |
| Prostate (men) | 27 | 1.13 (0.74 – 1.73) | 1.12 (0.73 – 1.71) | 1.20 (0.78 – 1.84) |
| Breast (women) | 20 | 1.05 (0.67 – 1.64) | 1.27 (0.83 – 1.95) | 1.20 (0.78 – 1.84) |
| Colon | 25 | 1.42 (1.02 – 1.96) | 1.47 (1.06 – 2.04) | 1.36 (0.91 – 2.02) |
| Lung | 92 | 0.96 (0.77 – 1.20) | 1.04 (0.84 – 1.30) | 1.09 (0.89 – 1.35) |
| Other cancers | 155 | 1.24 (1.06 – 1.44) | 1.34 (1.15 – 1.56) | 1.17 (0.99 – 1.38) |
Abbreviations: BMI, body mass index; CI, confidence interval; HR, hazard ratio; WC, waist circumference; WHR, waist –hip ratio.
Note. Models are adjusted for age, sex, exam year, alcohol consumption status, smoking status and educational level. HRs (95% CI) are stated per s.d.
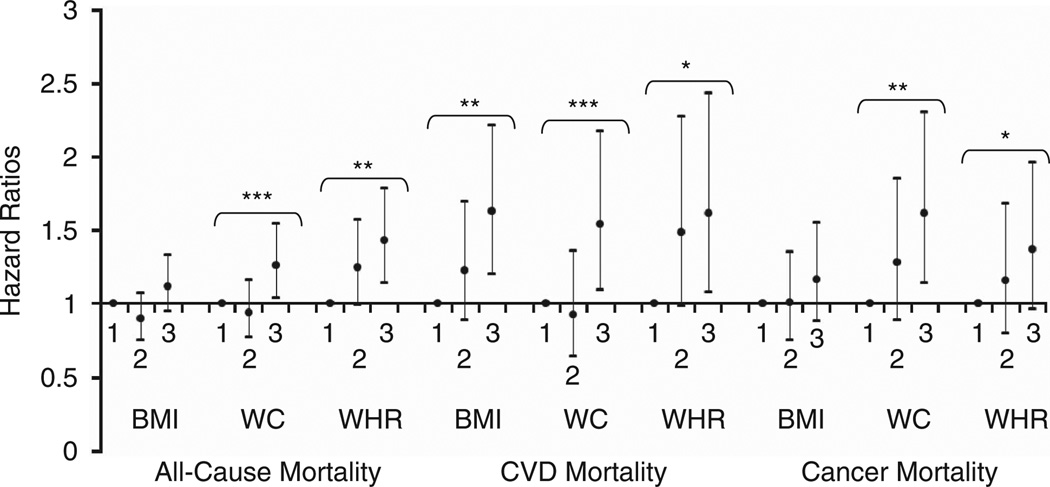
There was a significant pattern across tertiles of WC and WHR for all-cause, CVD and cancer mortality, and across tertiles of BMI for CVD mortality only (all P for trend < 0.05) (Figure 1). Compared with the lowest tertile, adults in the highest tertile of WC had higher all-cause (HR 1.26, 95% CI 1.04–1.54); CVD (HR 1.54, 95% CI 1.09–2.17); and cancer (HR 1.62, 95% CI 1.14–2.30) mortality. Those in the highest tertile of WHR had higher all-cause (HR 1.43, 95% CI 1.14–1.78) and CVD (HR 1.62, 95% CI 1.08–2.43) mortality versus the lowest WHR tertile. Adults in the highest tertile of BMI had higher CVD (HR 1.63, 95% CI 1.20–2.21) mortality compared with the lowest BMI tertile.
Figure 1.
Hazard ratios for all-cause, CVD and cancer mortality per tertile of BMI, WC or WHR. Models are adjusted for age, sex, exam year, alcohol consumption status, smoking status and educational level. Error bars indicate 95% CI. ***Indicates P for trend < 0.001. **Indicates P for trend < 0.01. *Indicates P for trend < 0.05.
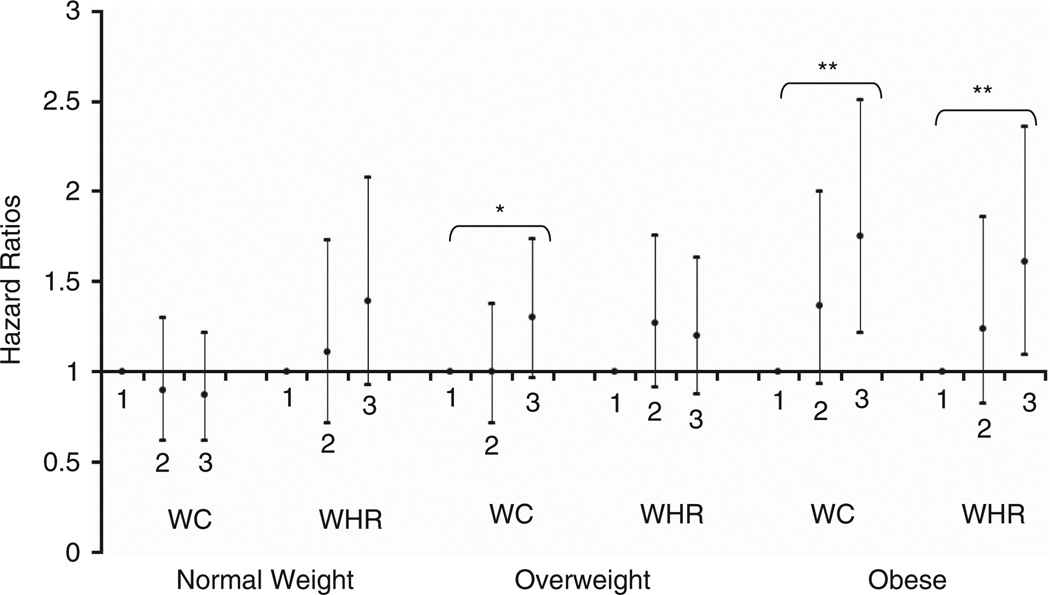
All-cause mortality risks were also compared within each BMI category (normal weight, overweight or obese) across tertiles of WC and WHR (Figure 2). In normal weight adults, there was no relationship between increasing WC or WHR and all-cause mortality risk. In overweight adults, there was a significant pattern of ascending WC related to higher all-cause mortality risk (P for trend=0.03). In obese adults, there were significant patterns between both ascending WC (P for trend=0.002) and ascending WHR (P for trend=0.008) with higher mortality risk. Compared with the lowest tertile, obese adults in the highest tertile of WC had a higher mortality risk (HR 1.75, 95% CI 1.22–2.51), as did obese adults in the highest tertile of WHR (HR 1.61, 95% CI 1.10–2.36).
Figure 2.
Hazard ratios for all-cause mortality per tertile of WC or WHR within normal weight, overweight and obese BMI category. Models are adjusted for age, sex, exam year, alcohol consumption status, smoking status and educational level. Tertiles are calculated within each sex and BMI category. Error bars indicate 95% CI. **Indicates P for trend < 0.01. *Indicates P for trend < 0.05.
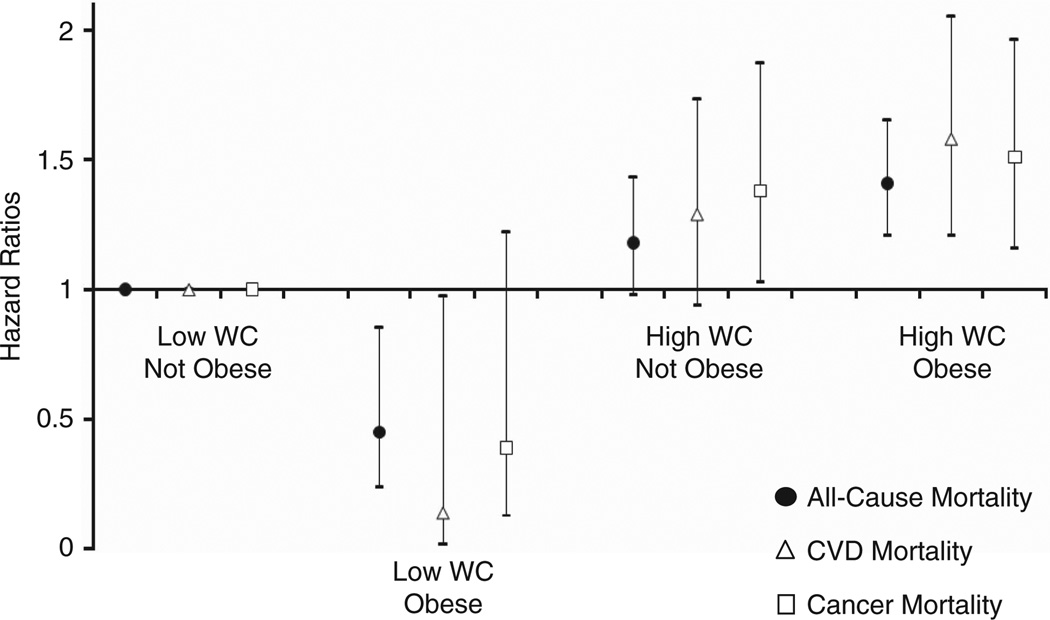
In the comparison across combined WC and BMI categories, cancer mortality risk was higher in adults with high WC (for non-obese, HR 1.38, 95% CI 1.03–1.87; for obese, HR 1.51, 95% CI 1.16–1.96) compared with the low WC non-obese group (Figure 3). All-cause (HR 1.41, 95% CI 1.21–1.65) and CVD (HR 1.58, 95% CI 1.21–2.05) mortality risk were also higher in obese adults with high WC. In contrast, adults with low WC who were obese had a lower all-cause (HR 0.45, 95% CI 0.24–0.85) and CVD (HR 0.14, 95% CI 0.02–0.97) mortality risk than the low WC non-obese group.
Figure 3.
Relative risk of all-cause, cardiovascular and cancer mortality in WC by BMI groups. Models are adjusted for age, sex, exam year, alcohol consumption status, smoking status and educational level. WC considered high if ≥88 cm for women and ≥102 cm for men. Obese classified as BMI ≥30.
DISCUSSION
Both BMI and WC were associated with increased all-cause, CVD and cancer mortality risk in this sample of Canadian adults. Importantly, WC consistently demonstrated the highest relative risk estimates for all-cause and cause-specific mortality, compared with BMI or WHR. In tertile analyses, CVD mortality risk was related to all three anthropometric measures. A previous analysis of the CHHS sample concluded that WC was the single best indicator of CVD risk factors,12 and our analysis shows that BMI, WC and WHR are each significant predictors for subsequent CVD mortality. Cancer mortality was most highly associated with WC and the upper tertile of WC was associated with elevated cancer mortality risk, whereas the upper tertiles of BMI and WHR were not significantly associated. Prior evidence of a strong association between adiposity and colon cancer death1 was confirmed in the present findings, in which one standard deviation unit of BMI and WC were each related to a 42% and 47% higher mortality risk for colon cancer, respectively.
WC remained significantly related to all-cause mortality even when stratified by BMI category. Upper tertiles of WC were associated with increased mortality in overweight and obese adults, indicating the influence of elevated WC above and beyond that indicated by BMI. Additionally, adults with high WC had higher mortality risk regardless of BMI obesity status, when compared with low WC non-obese adults. This aligns with findings of an elevated health risk (that is, metabolic syndrome) found in overweight and obese women with high WC compared with those with low WC,13 as well as increased hypertension, diabetes and dyslipidemia in individuals with high WC in each BMI category.14 In contrast, there was no statistically significant association between tertiles of WC or WHR and all-cause mortality risk for individuals classified as normal weight based on BMI. This finding contradicts a prior study, which found individuals with normal weight BMI had the most prominent association between WC and mortality risk compared with overweight or obese adults.15 Moreover, among adults with low WC, those with high BMI actually had a lower risk of all-cause and CVD mortality risk compared with those with a normal or overweight BMI. A possible explanation for this counterintuitive finding is that BMI, as a measure of general obesity, does not differentiate lean mass from fat mass. Thus, low WC and high BMI may be indicative of high muscle mass, which confers protective benefits against mortality.16 The distinct mortality risks derived from the combination of WC and BMI indicate that both adiposity measures are important considerations in health promotion efforts.
WC consistently predicted a higher mortality risk than WHR for all-cause, CVD and cancer. WC also predicted an increased risk for congestive heart failure, colon cancer and other cancers, whereas WHR did not. Moreover, ascending tertiles of WC were associated with increased all-cause mortality in both overweight and obese adults versus only in obese adults for WHR. Although two studies indicate that WHR was superior to both BMI and WC in predicting all-cause mortality17 and acute myocardial infarction,18 results may vary when multiple non-standard methods are used to measure WC compared with a more standard HC. Additionally, waist and hip circumferences may exert opposing effects on mortality.19 WC may therefore be a better predictor of mortality risk than WHR, and it requires one less anthropometric measurement so is a simpler choice.5
Proposed mechanisms of the putative pathway between obesity and mortality warrant discussion. Obesity contributes to adverse cardiometabolic changes, including insulin resistance, dyslipidemia and systemic inflammation, leading to both cardiovascular complications and certain cancers.20,21 An elevated WC increases susceptibility to dyslipidemia and insulin resistance, likely because of its strong association with visceral fat.22 Cancer risk is also elevated by excess adipose tissue due to increased free fatty acid release, which promotes cellular proliferation and tumor growth (see Calle and Kaaks23).
A major strength of this study was the longitudinal cohort sample that included standardized clinical measures of BMI, WC and WHR, which linked to specific causes of death. This study addressed limitations of prior obesity-mortality studies by controlling for smoking and age, and by eliminating participants whose death occurred less than 6 months after data collection to control for weight loss due to pre-existing illness.1
This study was limited in the number of deaths from certain causes, which reduced power to detect associations for individual types of death, such as prostate and breast cancer. The relatively small number of deaths prevented analyses stratified by age or sex, though both were used as covariates. Regardless, significant effects emerged between both general and abdominal adiposity and cause-specific mortality rates. It is also a limitation that the most recent known mortalities are from 2004. However, the average follow-up of 13 years was sufficient to detect significant associations with mortality risk. We feel these obesity-mortality associations are relevant for the current adult population. Finally, given that baseline data collection for this study occurred between 15 and 25 years ago, the measurement of WC in this study did not follow one of the currently recommended protocols of the World Health Organization24 or the US National Institutes of Health,25 which are now widely used. The degree to which the choice of measurement protocol used in the CHHS may have affected the results is not known.
In conclusion, WC consistently exhibited the most prominent association with mortality risk for all-cause, CVD and cancer mortality compared with weaker associations for BMI and WHR. Results indicate the need to account for WC in examining the relationship between adiposity and mortality. The clinical importance of maintaining a low WC regardless of BMI bears significant implications for preventing premature mortality attributable to cardiovascular or cancer complications.
ACKNOWLEDGEMENTS
This research was supported by a New Emerging Team grant from the Heart and Stroke Foundation of Canada and the Canadian Institutes of Health Research. PTK is partially supported by the Louisiana Public Facilities Authority Endowed Chair in Nutrition. Special thanks to Alison Edwards for assistance with data management.
Footnotes
CONFLICT OF INTEREST
The authors declare no conflict of interest.
REFERENCES
- 1.World Health Organization. Waist circumference and waist-hip ratio. [Accessed 15 July 2011];Report of a WHO expert consultation, Geneva, 8 – 11 December 2008. 2011
- 2.Gelber RP, Gaziano JM, Orav EJ, Manson JE, Buring JE, Kurth T. Measures of obesity and cardiovascular risk among men and women. J Am Coll Cardiol. 2008;52:605–615. doi: 10.1016/j.jacc.2008.03.066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hu G, Jousilahti P, Antikainen R, Katzmarzyk PT, Tuomilehto J. Joint effects of physical activity, body mass index, waist circumference and waist-hip ratio with the risk of heart failure. Circulation. 2010;121:237–244. doi: 10.1161/CIRCULATIONAHA.109.887893. [DOI] [PubMed] [Google Scholar]
- 4.Reis JP, Macera CA, Araneta MR, Lindsay SP, Marshall SJ, Wingard DL. Comparison of overall obesity and body fat distribution in predicting risk of mortality. Obesity. 2009;17:1232–1239. doi: 10.1038/oby.2008.664. [DOI] [PubMed] [Google Scholar]
- 5.Seidell JC. Waist circumference and waist/hip ratio in relation to allcause mortality, cancer and sleep apnea. Eur J Clin Nutr. 2010;64:35–41. doi: 10.1038/ejcn.2009.71. [DOI] [PubMed] [Google Scholar]
- 6.Lau DCW, Douketis JD, Morrison KM, Hramiak IM, Sharma AM, Ur E. Canadian clinical practice guidelines on the management and prevention of obesity in adults and children. CMAJ. 2007;176(Suppl 8):1–117. doi: 10.1503/cmaj.061409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Katzmarzyk P, Reeder BA, Elliott S, Joffres MR, Pahwa P, Raine K, et al. Body mass index and mortality from cardiovascular disease and cancer among Canadian adults. Can J Public Health. doi: 10.1007/BF03404221. (in press). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.MacLean DR, Petrasovits A, Nargundkar M, Connelly PW, MacLeod E, Edwards A, et al. Canadian Heart Health Surveys: A profile of cardiovascular risk. Survey methods and data analysis. Can Med Assoc J. 1992;146:1969–1974. [PMC free article] [PubMed] [Google Scholar]
- 9.Statistics Canada. Vital statistics - death database: Detailed information for 2005. Ottawa, ON: Statistics Canada; 2007. [Accessed 13 July 2011]. www.statcan.gc.ca/ [Google Scholar]
- 10.Schnatter AR, Acquavella JF, Thompson FS, Donaleski D, Theriault G. An analysis of death ascertainment and follow-up through Statistics Canada’s Mortality Database System. Can J Public Health. 1990;81:60–65. [PubMed] [Google Scholar]
- 11.National Institute of Health, National Heart, Lung, and Blood Institute (NHLBI) Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults: The evidence report. Obes Res. 1998;6(Suppl 2):S51–S210. [PubMed] [Google Scholar]
- 12.Dobbelsteyn CJ, Joffres MR, MacLean DR, Flowerdew G. A comparative evaluation of waist circumference, waist-to-hip ratio and body mass index as indicators of cardiovascular risk factors: The Canadian Heart Health Surveys. Int J Obes. 2001;25:652–661. doi: 10.1038/sj.ijo.0801582. [DOI] [PubMed] [Google Scholar]
- 13.Ardern C, Katzmarzyk PT, Janssen I, Ross R. Discrimination of health risk by combined body mass index and waist circumference. Obes Res. 2003;11:135–142. doi: 10.1038/oby.2003.22. [DOI] [PubMed] [Google Scholar]
- 14.Janssen I, Katzmarzyk PT, Ross R. Body mass index, waist circumference, and health risk: evidence in support of current National Institutes of Health guidelines. Arch Intern Med. 2002;162:2074–2079. doi: 10.1001/archinte.162.18.2074. [DOI] [PubMed] [Google Scholar]
- 15.Pischon T, Boeing H, Hoffman K, Bergmann M, Schulze MB, Overvad K, et al. General and abdominal adiposity and risk of death in Europe. N Engl J Med. 2008;359:2105–2120. doi: 10.1056/NEJMoa0801891. [DOI] [PubMed] [Google Scholar]
- 16.Heitmann BL, Erikson H, Ellsinger BM, Mikkelsen KL, Larsson B. Mortality associated with body fat, fat-free mass and body mass index among 60-yearold Swedish men-a 22-year follow-up. The study of men born in 1913. Int J Obes Relat Metab Disord. 2000;24:33–37. doi: 10.1038/sj.ijo.0801082. [DOI] [PubMed] [Google Scholar]
- 17.Welborn TA, Dhaliwal SS. Preferred clinical measures of central obesity for predicting mortality. Eur J Clin Nutr. 2007;61:1373–1379. doi: 10.1038/sj.ejcn.1602656. [DOI] [PubMed] [Google Scholar]
- 18.Yusuf S, Hawken S, Ounpuu S, Bautista L, Franzosi MG, Commerford P, et al. Obesity and the risk of myocardial infarction in 27,000 participants from 52 countries: A case-control study. Lancet. 2005;366:1640–1649. doi: 10.1016/S0140-6736(05)67663-5. [DOI] [PubMed] [Google Scholar]
- 19.Bigaard J, Frederiksen K, Tjonneland A, Thomsen BL, Overvard K, Heitmann BL, et al. Waist and hip circumferences and all-cause mortality: Usefulness of the waist-to-hip ratio? Int J Obes. 2004;28:741–747. doi: 10.1038/sj.ijo.0802635. [DOI] [PubMed] [Google Scholar]
- 20.Prospective Studies Collaboration. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet. 2009;373:1083–1096. doi: 10.1016/S0140-6736(09)60318-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Zhang C, Rexrode KM, van Dam RM, Li TY, Hu FB. Abdominal obesity and the risk of all-cause, cardiovascular, and cancer mortality: sixteen years of follow-up in US women. Circulation. 2008;117:1658–1667. doi: 10.1161/CIRCULATIONAHA.107.739714. [DOI] [PubMed] [Google Scholar]
- 22.Kuk JL, Katzmarzyk PT, Nichaman MZ, Church TS, Blair SN, Ross R. Visceral fat is an independent predictor of all-cause mortality in men. Obesity. 2006;14:336–341. doi: 10.1038/oby.2006.43. [DOI] [PubMed] [Google Scholar]
- 23.Calle EE, Kaaks R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nature Rev Cancer. 2004;33:751–758. doi: 10.1038/nrc1408. [DOI] [PubMed] [Google Scholar]
- 24.WHO. WHO STEP wise Approach to Surveillance (STEPS) World Health Organization (WHO); Geneva: 2008. [Google Scholar]
- 25.NHLBI Obesity Education Initiative. The Practical Guide: Identification, Evaluation and Treatment of Overweight and Obesity in Adults National Institutes of Health (NIH Publication Number 00 – 4084) 2000 [Google Scholar]