Abstract
Background
In Korea recently, nontuberculous mycobacteria (NTM) have been more frequently isolated in respiratory specimens, while Mycobacterium tuberculosis (MTB) isolations have decreased. The major NTM lung disease species in Korea are M. intracellulare, M. avium, and M. abscessus, whereas M. kansasii is a rare species. This retrospective study was performed to determine if there are region-specific characteristics of lung disease-causing NTM species in Ulsan, a highly industrialized city in Korea.
Methods
Between January 2010 and July 2013, the results of all acid-fast bacilli (AFB) cultures of respiratory specimens performed at Ulsan University Hospital (Ulsan, Korea) were collected. NTM were identified and regional differences of NTM species were compared.
Results
AFB cultures were performed on 33,567 respiratory specimens, obtained from 10,208 patients, during the study period. Further, 10% of the specimens (3,287/33,567) were AFB culture-positive [MTB, 2,288/3,287 (70%); NTM 999/3,287 (30%)]. The proportion of NTM isolations gradually increased between 2010 and 2013, at 25% and 38%, respectively. The most common NTM species was M. intracellulare (356/999, 36%), followed by M. kansasii (295/999, 30%), M. avium (161/999, 16%), M. abscessus (117/999, 12%) and M. fortuitum (39/999, 4%). This trend was maintained throughout the study period.
Conclusions
In Ulsan, NTM isolation from respiratory specimens is increasing, consistent with previous studies performed in Korea. The distribution of respiratory NTM species, however, differed from previous studies that were performed in other regions of Korea: M. kansasii was the second most common NTM species in Ulsan. In Ulsan, there is a regional difference in the NTM species isolated.
Keywords: Nontuberculous mycobacteria (NTM), M. kansasii, Ulsan
Background
In Korea, nontuberculous mycobacteria (NTM) are frequently identified in acid-fast bacilli (AFB) respiratory cultures. Indeed, NTM isolation rates have been reported to be equal to or exceed those of Mycobacterium tuberculosis (MTB) (1-5). With the increasing prevalence of NTM isolations in respiratory specimens, the occurrence of NTM lung disease, which is the most common disease caused by NTM, is increasing in Korea (5).
The NTM species that cause lung disease vary between countries and regions (6-8). In the United States and Japan, M. avium complex (M. intracellular and M. avium) and M. kansasii are the major causes of NTM lung disease. In the United Kingdom, M. kansasii is the most prevalent species in England and Wales. By contrast, M. malmoense is most common in Scotland, and M. xenopi in southeast England. In Korea, M. intracellulare, M. avium, and M. abscessus have been reported to be the major causative species of NTM lung disease (2-4,9). In contrast, M. kansasii is thought to be a rare cause of NTM lung disease in Korea.
This retrospective study was performed to determine if there are region-specific characteristics of lung disease-causing NTM species in Ulsan, a highly industrialized city in Korea.
Methods
Study population
At Ulsan University Hospital, a 1,000-bed referral hospital in Ulsan South Korea, the results of AFB cultures of respiratory specimens, collected between January 2010 and July 2013, were retrospectively analyzed. Respiratory specimens included sputa and bronchoscopic specimens, which included bronchial washing fluids and bronchoalveolar lavage fluids. This study was approved by the Institutional Review Board and Ethics Committee of Ulsan University Hospital.
Acid fast bacilli culture and identification
Respiratory specimens were cultured in both solid and liquid media: 3% Ogawa solid egg-based medium (Asan Pharmaceutical, Seoul, Korea) and Mycobacteria Growth Indicator Tube liquid medium (Becton Dickinson, Sparks, MD, USA). If an AFB culture was positive in either liquid or solid medium, high performance liquid chromatography was performed to identify the mycobacterial species (10).
Diagnostic criteria for NTM lung disease
The diagnosis of NTM lung disease was performed according to the 2007 American Thoracic Society (ATS)/Infectious Diseases Society Of America (IDSA) guidelines (11).
Comparison of the major NTM species in regions of Korea
To date, there have been four detailed surveys of respiratory NTM species in Korea (2,4,9); surveys were performed at the university hospital in Seoul [Seoul Samsung Medical Center (Seoul-SMC) and Seoul National University Hospital (Seoul-SNU)] (5,9), 1 was performed at the university hospital in Jeju (4), and 1 was performed at the referral hospital in Masan (2). To determine the regional differences in NTM species in Korea, the data from the previously published papers were compared to the data obtained in this study. The raw data from the study at Seoul National University (Seoul-SNU) (5) were obtained directly from the corresponding author, as there was insufficient data in the published paper. The number of patients with respiratory NTM and the number patients with NTM lung disease were compared separately. There were data limitations: data from the Jeju study was only available for patients with respiratory NTM and date from the Seoul-SNU study was only available for patients with NTM lung disease.
Statistical analysis
Statistical analyses were performed using the software R (a language and environment for statistical computing, R Foundation for Statistical Computing, Vienna, Austria; Version 3.0.2). Independent t-test and Kruskal-Wallis test were used to compare means. And, Fisher’s exact test and Cochran-Armitage trend test were used to compare frequencies. A P value of less than 0.05 was considered to be significant.
Results
Numbers of patients and respiratory specimens
A total 33,567 respiratory specimens from 10,208 patients were collected for AFB culture during the study period.
Mycobacterial isolations from respiratory specimens
Over the 4-year collection period, 3,287 (10%) AFB culture-positive mycobacteria were isolated from 33,567 specimens. Of the samples in which mycobacteria were isolated, 70% were positive for MTB (2,288/3,287), while the remaining 30% were positive for NTM (999/3,287).
Change in proportions of NTM and MTB isolations from respiratory specimens
The proportion of NTM isolations increased, from 25% to 38% in 2010 and 2013, respectively. Over the same time period, the proportion of MTB isolations significantly decreased (Figure 1; P<0.001, Cochran-Armitage trend test).
Figure 1.

The proportion of nontuberculous mycobacteria (NTM) and Mycobacterium tuberculosis (MTB) isolations in Ulsan, Korea between January 2010 and July 2013.
Identification of NTM species isolated from respiratory specimens
In Ulsan, the most common NTM species was M. intracellulare (356/999, 36%), followed by M. kansasii (295/999, 30%), M. avium (161/999, 16%), M. abscessus (117/999, 12%), M. fortuitum (39/999, 4%), M. szulgai (23/999, 2%), M. chelonae (3/999, 0.3%), M. simiae (1/999, 0.1%), and unidentified NTM (4/999, 0.4%). During the study period, M. kansasii was consistently the second most common NTM species (Figure 2; P=0.43, Cochran-Armitage trend test).
Figure 2.
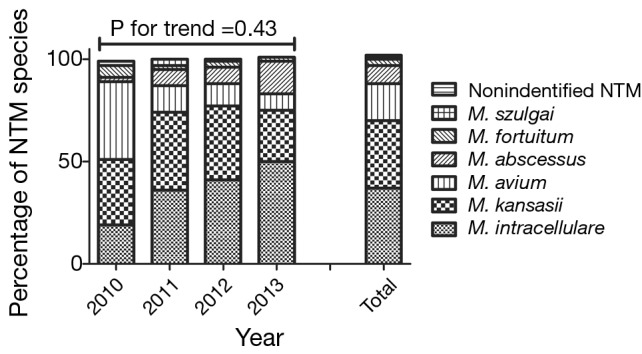
The proportion of nontuberculous mycobacteria (NTM) species in Ulsan, Korea between January 2010 and July 2013.
Pulmonary tuberculosis, respiratory NTM, and NTM lung disease frequency in patients
A total of 12% of patients (1,171/10,208 patients) were identified to be AFB culture-positive with mycobacteria isolated from the specimens. Of the mycobacteria infected patients, 65% (765/1,171) were diagnosed with pulmonary tuberculosis and 35% (410/1,171) were diagnosed with respiratory NTM. A total of 245 of the 410 patients diagnosed with respiratory NTM [21% (245/1,171) of all AFB culture-positive patients] were diagnosed with NTM lung disease.
In the patients diagnosed with respiratory NTM (N=410), the causative mycobacterial species were M. intracellulare (169/410, 41%), M. kansasii (102/410, 25%), M. avium (61/410, 15%), M. abscessus (33/410, 8%), M. fortuitum (24/410, 6%), M. szulgai (15/410, 4%), M. chelonae (3/410, 0.7%), M. simiae (1/410, 0.2%), and unidentified NTM (2/410, 0.5%). In the patients diagnosed with NTM lung disease (N=245), the causative mycobacterial species were M. intracellulare (93/245, 38%), M. kansasii (80/245, 33%), M. avium (39/245, 16%), M. abscessus (22/245, 9%), M. fortuitum (7/245, 3%), M. szulgai (3/245, 1%), and unidentified NTM (1/245, 0.4%).
Patients with NTM lung disease were older than those with pulmonary tuberculosis (mean age 62 and 55 years, respectively; P<0.001). There was a predominance of men in both the pulmonary tuberculosis and NTM lung disease patient populations. However, there were sex differences in the causative mycobacterial species isolated from the NTM lung disease patients. Patients with lung disease caused by M. kansasii were predominantly male, while patients with lung disease caused by the other NTM species were predominantly female (P<0.001; Table 1).
Table 1. Patients with pulmonary tuberculosis (Mycobacterium tuberculosis) and NTM lung disease in Ulsan, Korea between January 2010 and July 2013.
| Patients (number) | Male (%) | P value | Age, years (mean) | P value | |
|---|---|---|---|---|---|
| M. tuberculosis | 765 | 56 | 0.825 | 55.2±19.6 | <0.001 |
| NTM lung disease | 245 | 55 | 61.6±14.3 | ||
| NTM lung disease by species | <0.001 | 0.001 | |||
| M. intracellulare | 93 | 41 | 66.6±13.1 | ||
| M. avium | 39 | 41 | 58.1±13.6 | ||
| M. kansasii | 80 | 85 | 59.4±13.9 | ||
| M. abscessus | 22 | 32 | 59.1±16.8 | ||
| M. fortuitum | 7 | 29 | 58.9±16.2 | ||
| M. szulgai | 3 | 100 | 62.7±15.4 | ||
| Unidentified NTM | 1 | 0 | 38 |
NTM, nontuberculous mycobacteria.
Regional differences in NTM species in patients with respiratory NTM and NTM lung disease
When the results of previous Korean NTM distribution studies were compared with the results obtained in this study, we found that in patients with respiratory NTM, the major causative species differed (Figure 3A). In the Masan study (2), the causative mycobacterial species were M. intracellulare (28/57, 49%), M. abscessus (12/57, 21%), M. fortuitum (7/57, 12%), M. chelonae (4/57, 7%), and M. avium (3/57, 5%). In the Jeju study (4), the causative mycobacterial species were M. intracellulare (27/62, 44%), M. avium (14/62, 23%), M. abscessus (8/62, 13%), M. kansasii (5/62, 8%), and M. fortuitum (4/62, 7%). In the Seoul-SMC study (9), the causative mycobacterial species were M. fortuitum (217/794, 27%), M. abscessus (141/794, 18%), M. avium (111/794, 14%), M. intracellulare (108/794, 14%), M. gordonae (84/794, 11%), M. terrae (48/794, 6%), M. szulgai (32/794, 4%), M. chelonae (25/794, 3%), and M. kansasii (14/794, 2%). In contrast, in Ulsan the proportion of respiratory NTM patients infected with M. kansasii was significantly higher (P<0.001; Figure 3B).
Figure 3.
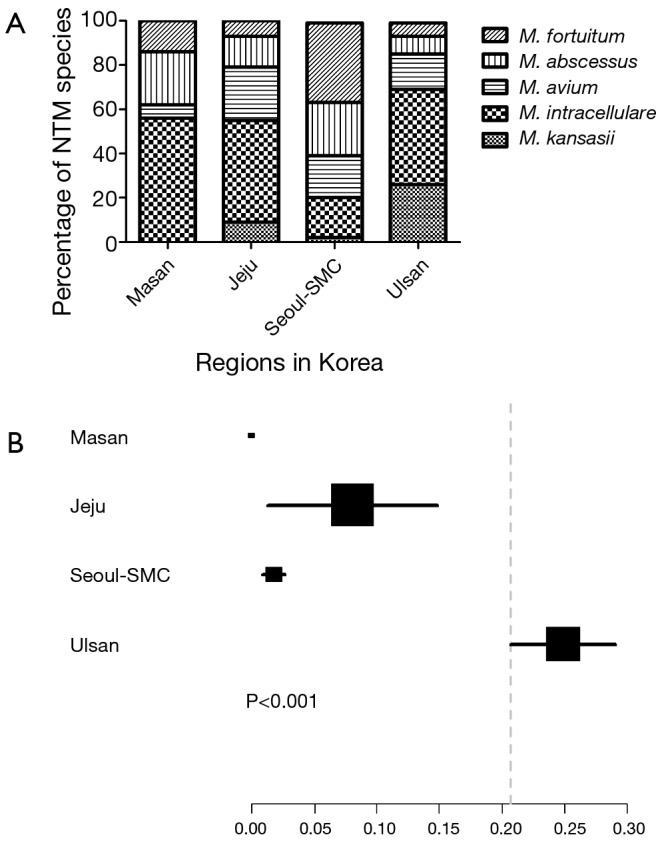
Nontuberculous mycobacteria (NTM) species in patients with respiratory NTM: (A) the distribution of NTM species in regions of Korea; (B) the ratios of Mycobacterium kansasii isolation by region of Korea. Seoul-SMC, Seoul Samsung Medical Center.
Similarly, when the distributions of NTM lung disease causative mycobacterial species were compared, the major causative species differed between the Korean regions examined previously (Figure 4A). In the Masan study (2), the NTM lung disease causative mycobacterial species were M. intracellulare (19/26, 73%), M. abscessus (5/26, 19%), M. fortuitum (1/26, 4%), and M. chelonae (1/26, 4%). In the Seoul-SMC study (9), the NTM lung disease causative mycobacterial species were M. abscessus (64/195, 33%), M. intracellulare (56/195, 29%), M. avium (38/195, 19%), M. fortuitum (21/195, 11%), M. kansasii (7/195, 4%), M. chelonae (6/195, 3%), and M. szulgai (2/195, 1%). In the Seoul-SNU study (5), the major causative mycobacterial species were M. avium (212/585, 36%), M. abscessus (163/585, 28%), M. intracellulare (156/585, 27%), M. kansasii (18/585, 3%), M. gordonae (7/585, 1%), and M. terrae (4/585, 0.7%). In our study of Ulsan patients, the proportion of cases in which M. kansasii was the NTM lung disease causative species was significantly higher (P<0.001; Figure 4B).
Figure 4.

Nontuberculous mycobacteria (NTM) species in patients with NTM lung disease: (A) the distribution of NTM species in regions of Korea; (B) the ratios of Mycobacterium kansasii isolation by region of Korea. Seoul-SMC, Seoul Samsung Medical Center; Seoul-SNU, Seoul National University Hospital.
Discussion
Similar to what has been observed previously in other regions of Korea, we showed that NTM isolation is increasing in Ulsan. However, the distribution of NTM species was different from previous studies: M. kansasii was the second most common NTM species in Ulsan; whereas in other regions of Korea, M. kansasii is rarely reported. Thus, we concluded that there is a regional difference in the NTM species isolated in Ulsan, Korea.
Consistent with previous studies, we found that in Ulsan, the proportion of NTM isolations has been increasing. Specifically, between 2010 and 2013, the proportion of NTM isolations increased from 25% to 38%. Over the same time period, the proportion of MTB isolations significantly decreased. In a previous study in Seoul, it was found that the proportion of NTM isolations increased from 22.2% in 2002 to 45.9% in 2008 (5); in a previous study in Jeju, the proportion of NTM isolations increased from 7% in 2003 to 19% in 2011 (4). The increase in NTM isolation appears to be happening throughout Korea, and the rate of NTM isolations seems to be proportionally correlated with the degree of urbanization, as Seoul is the most populated city in Korea and Jeju is a rural resort town in Korea.
Worldwide, NTM isolations have been increasing, a phenomenon that can be partially explained (3). First, improved laboratory diagnostic methods have enhanced recovery of mycobacteria (12). Second, exposure to NTM via aerosolized water is considered to be a cause of increased NTM infection in modern people (8). Finally, host factors including old age and chronic obstructive pulmonary disease are risk factors for the development of NTM disease (13). Further studies are required to fully elucidate the reason for the worldwide rapid increase in NTM isolations.
Depending on countries and/or regions, the distributions of lung disease-causing NTM species are different (6-8). In Korea, according to previous studies, M. intracellulare, M. avium, and M. abscessus are the major NTM lung disease species (2-4,9), in contrast, M. kansasii is a rare NTM lung disease species (3). In the current study, we showed that in Ulsan the distribution of NTM species differed when compared with other regions of Korea. M. kansasii was identified in 25% of patients with respiratory NTM and in 33% of patients with NTM lung disease. Thus, there is a significant regional difference in the distribution of NTM species within Korea.
The high proportion of M. kansasii isolations in Ulsan is not well understood. Unlike other NTM, M. kansasii is not found in soil or natural water supplies, but it has been recovered from tap water in cities where M. kansasii is endemic (11,14). In addition, M. kansasii is more likely to be isolated in urban or industrialized regions (14,15). However, urbanization and/or industrialization are not critical factors for M. kansasii infection, as there have been reports of rare M. kansasii—distribution in highly urbanized or industrialized cities (2,5,9). It is possible that there are environmental and occupational risk factors that are associated with M. kansasii infection. Thus, further studies to elucidate factors that are associated with M. kansasii infection are required.
There are limitations to this study. First, this study was a retrospective, single-center study. There may sources of bias that have not been identified or controlled for in this study. As our hospital is the only referral medical center in Ulsan, the results are likely indicative of the extent of respiratory NTM isolations in Ulsan. Second, our research identified the high proportion of M. kansasii species isolations in Ulsan, although we were unable to explain this observation. Therefore, further research is required.
Conclusions
In conclusion, we showed that in Ulsan respiratory NTM infection and NTM lung disease is increasing, similar to what has been observed worldwide and in other regions of Korea. However, the distribution of NTM species differed from previous studies in Korea: M. kansasii, a rarely reported organism in other areas of Korea, was extremely common and was the second most commonly observed NTM species following M. intracellulare. Therefore, there is a regional difference in the distribution of NTM species in Ulsan, Korea.
Acknowledgements
Funding: This work was funded by Ulsan University Hospital (Biomedical Research Center Promotion Fund, UUH-2014-2).
Disclosure: The authors declare no conflict of interest.
References
- 1.Yoo JW, Jo KW, Kim MN, et al. Increasing trend of isolation of non-tuberculous mycobacteria in a tertiary university hospital in South Korea. Tuberc Respir Dis (Seoul) 2012;72:409-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Choi SP, Lee BK, Min JH, et al. Pathogenic Classification and Clinical Characteristics of Nontuberculous Mycobacterial Pulmonary Disease in a National Tuberculosis Hospital. Tuberc Respir Dis 2005;59:606-12 [Google Scholar]
- 3.Koh WJ, Chang B, Jeong BH, et al. Increasing Recovery of Nontuberculous Mycobacteria from Respiratory Specimens over a 10-Year Period in a Tertiary Referral Hospital in South Korea. Tuberc Respir Dis (Seoul) 2013;75:199-204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Oh MS, Lee J. The Increase of Nontuberculous Mycobacterial Isolation in the Specimens from Respiratory System in Jeju. Ann Clin Microbiol 2013;16:13-8 [Google Scholar]
- 5.Park YS, Lee CH, Lee SM, et al. Rapid increase of non-tuberculous mycobacterial lung diseases at a tertiary referral hospital in South Korea. Int J Tuberc Lung Dis 2010;14:1069-71 [PubMed] [Google Scholar]
- 6.Koh WJ, Kwon OJ, Lee KS. Diagnosis and treatment of nontuberculous mycobacterial pulmonary diseases: a Korean perspective. J Korean Med Sci 2005;20:913-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Hoefsloot W, van Ingen J, Andrejak C, et al. The geographic diversity of nontuberculous mycobacteria isolated from pulmonary samples: an NTM-NET collaborative study. Eur Respir J 2013;42:1604-13 [DOI] [PubMed] [Google Scholar]
- 8.Kendall BA, Winthrop KL. Update on the epidemiology of pulmonary nontuberculous mycobacterial infections. Semin Respir Crit Care Med 2013;34:87-94 [DOI] [PubMed] [Google Scholar]
- 9.Koh WJ, Kwon OJ, Jeon K, et al. Clinical significance of nontuberculous mycobacteria isolated from respiratory specimens in Korea. Chest 2006;129:341-8 [DOI] [PubMed] [Google Scholar]
- 10.Jeong J, Kim SR, Lee SH, et al. The Use of High Performance Liquid Chromatography to Speciate and Characterize the Epidemiology of Mycobacteria. Lab Med 2011;42:612-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Griffith DE, Aksamit T, Brown-Elliott BA, et al. An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. Am J Respir Crit Care Med 2007;175:367-416 [DOI] [PubMed] [Google Scholar]
- 12.Chihota VN, Grant AD, Fielding K, et al. Liquid vs. solid culture for tuberculosis: performance and cost in a resource-constrained setting. Int J Tuberc Lung Dis 2010;14:1024-31 [PubMed] [Google Scholar]
- 13.Andréjak C, Nielsen R, Thomsen VØ, et al. Chronic respiratory disease, inhaled corticosteroids and risk of non-tuberculous mycobacteriosis. Thorax 2013;68:256-62 [DOI] [PubMed] [Google Scholar]
- 14.Steadham JE. High-catalase strains of Mycobacterium kansasii isolated from water in Texas. J Clin Microbiol 1980;11:496-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rapid increase of the incidence of lung disease due to Mycobacterium kansasii in Japan. Chest 1983;83:890-2 [DOI] [PubMed] [Google Scholar]


