Abstract
Xanthogranulomatous pyelonephritis (XGP) is an uncommon form of chronic pyelonephritis and a well recognized entity. It is rarely seen in children and neonates. The preoperative diagnosis is difficult and the etiology is still obscure. The condition is mostly diagnosed on nephrectomy specimen. The focal form mimicking neoplastic condition is rare. A case of XGP is reported here in an 8 month old child in which case nephrectomy was done with the clinical diagnosis of malignant renal tumor. Various modalities of preoperative diagnosis of this entity with conservative approach are also discussed.
Keywords: Infant, pseudotumor, renal, XGP, XPN, xanthogranulomatous pyelonephritis
INTRODUCTION
Xanthogranulomatous pyelonephritis is a severe, atypical form of chronic renal parenchymal disease accounting for 6/1000 surgically proved cases of chronic pyelonephritis.[1] Though the entity has been described about a century ago in 1916 by Schlagenhaufer (quoted by Brown et al.[2]), preoperative diagnosis is difficult and etiology is still obscure. It is an almost exclusively unilateral condition and has variable presentations like renal mass, renal abscess, perirenal tissue involvement and even cutaneous fistula. More than 500 cases have been described in adults and 80 in children. Urinary tract obstruction, congenital urological anomalies, nephrolithiasis, and recurrent urinary infection are mostly accompanying disorders.[3] We report here an unusual case of XGP diagnosed preoperatively as a malignant renal tumor.
CASE REPORT
An 8 months old boy was brought to the hospital for the complaints of moderate grade fever on and off for 1 month. He was treated outside the hospital without any relief. There was no complaint of diarrhea, vomiting or crying during micturtion. Routine hematological examination of blood revealed only microcytic hypochromic anemia (Hb 7.3 gm/dl), white cell count was normal. Routine urine examination was normal. Biochemical parameters like blood urea, serum creatinine, blood glucose were within normal limits. Tests for malarial parasite and typhoid were negative. Abdominal ultrasonography revealed a mass in the mid portion of left kidney. Subsequent contrast enhance computerized tomography (CECT) reported heterogenous ill-defined mass in the mid part of left kidney, measuring 3.3 × 3.1 × 3.2 cm3, extending in full thickness of kidney from renal pelvis to cortex with exophytic extension in perirenal space [Figure 1]. There was mild enlargement of left para aortic lymph nodes at the level of left renal hilum. Based on these findings, a clinical diagnosis of Wilm's tumor was made and left nephrectomy was done.
Figure 1.
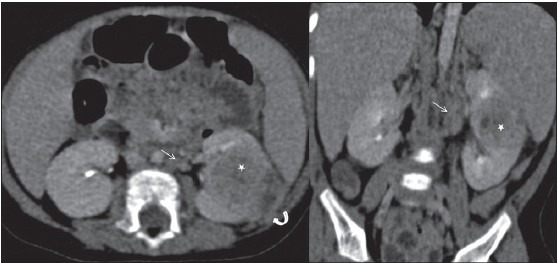
CECT showing a heterogenous ill-defined mass in the mid part of left kidney, extending in full thickness of kidney from renal pelvis to cortex with exophytic extension in perirenal space
The nephrectomy specimen was 4.0 × 3.4 × 2.5 cm3(wt. 60gms.), cut surface showed a yellowish well circumscribed mass in the mid portion measuring 3.0 × 3.0 × 2.5 cm3 [Figure 2]. Adjoining renal tissue was unremarkable. The microscopic examination of the sections showed sheets of foamy cells with normochromic nuclei, admixed with mixed inflammatory cells [Figure 3]. The cells were seen in perirenal fat too. These foamy cells were positive for PAS and macrophage marker CD68. Thus, the diagnosis of XGP stage III was confirmed. The patient is symptom free on 1 year follow-up.
Figure 2.

Photograph of cut surface of kidney showing a yellowish well circumscribed mass in the mid portion
Figure 3.
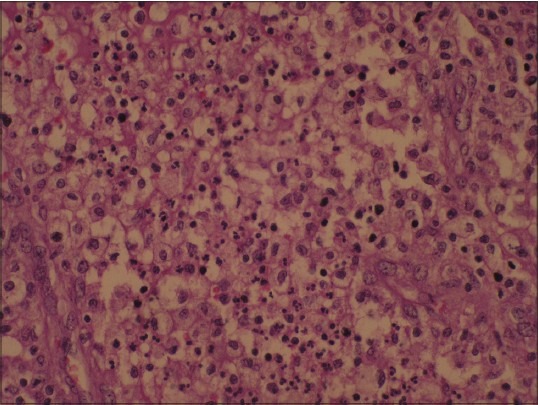
Microphotograph showing sheets of foamy cells with normochromic nuclei, admixed with mixed inflammatory cells (H and E, ×400)
DISCUSSION
XGP is a disease predominantly affecting adults above 40 years of age but can occur in all age groups ranging from 21 days to 90 years. There are some epidemiological and clinical differences between children and adults. In children, the disease most frequently occur below 8 years of age with male predominance and is focal, localized and acalculous, affecting left kidney predominantly. In adults, females are affected more than males and right kidney has been noted to be involved more often than the left. The symptoms are usually nonspecific and include fever, flank pain, weight loss, malaise/anorexia and constipation, along with urinary symptoms like frequency, dysuria, and frequent urination. On clinical examination abdominal tenderness and palpable flank mass are common. Urinary tract infections, pyuria, leucocytosis and raised erythrocyte sedimentation rate (ESR) are frequently associated with XGP.[2]
On the basis of morphological involvement, two forms are described, more common diffuse form and relatively rarer focal form. The focal form closely mimics renal carcinoma. Based on severity of the disease, XGP has been described to have three stages. In stage I the lesion is confined to the kidney, in stage II the lesion extends to Gerota's fascia and in stage III it extends to paranephric space and other retroperitoneal structures.[4]
The present case is unique in a way that it was in an 8 month old male child with only complaints of fever without any other complaints associated with XGP and scanning revealed a single mass in the left kidney. Urine was normal, there was no leucocytosis and hence the clinical diagnosis of renal tumor was made. Fine-needle aspiration cytology in this case may have helped in the preoperative diagnosis.[5]
Preoperative diagnosis of this condition is not easy, particularly in the localized form. Awareness about the condition, along with radiological findings and FNAC may help make this diagnosis before surgery and allowconservative management[2] or partial nephrectomy, particularly in children. In the focal form of XGP, ultrasonography shows a localized hypoechoic mass, often misdiagnosed as a renal tumor.[6,7] CT scan is usually indicated and demonstrates renal parenchyma replacement by multiple low attenuation rounded areas with peripheral enhancement and perirenal involvement. There is little data on magnetic resonance imaging (MRI) findings in the focal form. The lesion has slightly low signal intensity on T2 weighted sequences and is isointense with the renal parenchyma on T1. The FAST T2 sequences seem to be very useful with the absence of hyperintensity in the differentiation of XGP from tumor masses.[6,7] Imaging features not consistent with Wilm's tumor include the absence of sharp definition and encapsulation of the mass or ill-defined margins with inflammatory infiltration of the perinephric fat. Internal calcification is rare in Wilm's tumor.[8]
Fine needle aspiration cytology can be conclusive in cases of XGP in children.[5] However, one of its criticism is that FNAC can cause tumor spill if the lesion turnsout to be Wilm's tumor; tumor cell seeding can be avoided by employing a postero-lateral approach.[9]
Though it is generally accepted that the prognosis for the child is excellent after nephrectomy, increased risk of hypertension, persistent bacteriuria, and rarely renal amyloidosis have been reported as late complications. It seems reasonable to initiate a trial of antibiotic therapy in cases of focal XGP when there is significant residual function in the affected kidney, especially in cases involving children.[2]
Previous reports on this disease conclude that preoperative diagnosis is not easy and the viewpoint seems to have been generally accepted. Quinn et al.,[10] thought that because of the increasing awareness of the condition, XGP is a diagnosis that can and should be made preoperatively, as was reported by the authors in 20 of the last 21 cases in a series of 31 cases.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Mark RS, Grene LF, DeWeerd JH, Farnow GM. Xanthogranulomatous pyelonephritis. Br J Urol. 1972;44:295–308. doi: 10.1111/j.1464-410x.1972.tb10080.x. [DOI] [PubMed] [Google Scholar]
- 2.Brown PS, Dodson M, Weintrub PS. Xanthogranulomatous pyelonephritis: Report of nonsurgical management of a case and review of the literature. Clin Infect Dis. 1996;22:308–14. doi: 10.1093/clinids/22.2.308. [DOI] [PubMed] [Google Scholar]
- 3.Yildiz K, Kose N, Ozdanar S. Xanthogranulomatous pyelonephritis in a child presenting with cutaneous fistula. Aegean Pathol J. 2005;2:77–9. [Google Scholar]
- 4.Khalid M, Ahmad M, Siddiqui MA, Khalid S. Diagnostic difficulties in diffuse Xanthogranulomatous pyelonephritis: A case report and review of literature. Kidney Int. 2010;19:73–5. [Google Scholar]
- 5.Sugie S, Tanaka T, Nishikawa A, Yoshimi N, Kato K, Mori H, et al. Fine-needle aspiration cytology of Xanthogranulomatous pyelonephritis. Urology. 1991;37:376–9. doi: 10.1016/0090-4295(91)80272-9. [DOI] [PubMed] [Google Scholar]
- 6.Cakmakci H, Tasdelen N, Obuz F, Yilmaz E, Kovanlikaya A. Pediatric focal Xanthogranulomatous pyelonephritis: Dynamic contrast-enhanced MRI findings. Clin Imaging. 2002;26:183–6. doi: 10.1016/s0899-7071(01)00387-4. [DOI] [PubMed] [Google Scholar]
- 7.Gasmi M, Jemai R, Fitouri F, Slama AB, Sahli S, Hamzaoui M. Xanthogranulomatous pyelonephritis in childhood: Disgnosis difficulties and success of conservative treatment. Tunis Med. 2010;88:427–9. [PubMed] [Google Scholar]
- 8.Samuel M, Duffy P, Capps S, Mouriquand P, Williams D, Ransley P. Xanthogranulomatous pyelonephritis in childhood. J Paediatr Surg. 2001;36:598–601. doi: 10.1053/jpsu.2001.22292. [DOI] [PubMed] [Google Scholar]
- 9.Alam K, Prasad S, Maheshwari V, Aggarwal S, Chana RS. Diagnostic role of fine needle aspiration cytology in Wilm's tumor. J Cytol. 2007;24:134–6. [Google Scholar]
- 10.Quinn FM, Dick AC, Corbally MT, McDermott MB, Guiney EJ. Xanthogranulomatous pyelonephritis in childhood. Arch Dis Child. 1999;81:483–6. doi: 10.1136/adc.81.6.483. [DOI] [PMC free article] [PubMed] [Google Scholar]


