Summary
A 48-year-old hypertensive and diabetic patient presented with a 10-year history of progressive right facial pain, tinnitus, hearing loss, sweating, and palpitations. Investigations revealed a 5.6 cm vascular tumor at the carotid bifurcation. Her blood pressure (BP) was 170/110, on lisinopril 20 mg od and amlodipine 10 mg od and 100 U of insulin daily. A catecholamine-secreting carotid body paraganglioma (CSCBP) was suspected; the diagnosis was confirmed biochemically by determining plasma norepinephrine (NE) level, 89 000 pmol/l, and chromogranin A (CgA) level, 279 μg/l. Meta-iodobenzylguanidine and octreotide scanning confirmed a single tumor in the neck. A week after giving the patient a trial of octreotide 100 μg 8 h, the NE level dropped progressively from 50 000 to 25 000 pmol/l and CgA from 279 to 25 μg/l. Treatment was therefore continued with labetalol 200 mg twice daily (bid) and long-acting octreotide-LA initially using 40 mg/month and later increasing to 80 mg/month. On this dose and with a reduced labetalol intake of 100 mg bid, BP was maintained at 130/70 and her symptoms resolved completely. CgA levels returned to normal in the first week and these were maintained throughout the 3 month treatment period. During tumor resection, there were minimal BP fluctuations during the 10 h procedure. We conclude that short-term high-dose octreotide-LA might prove valuable in the preoperative management of catecholamine-secreting tumors. To the best of our knowledge, this is the first report on the successful use of octreotide in a CSCBP.
Learning points
The value of octreotide scanning in the localization of extra-adrenal pheochromocytoma.
Control of catecholamine secretion using high-dose octreotide.
This is a report of a rare cause of secondary diabetes and hypertension.
Background
Paranganglionomas (PGs) are found distributed throughout the autonomic nervous system. They consist of chief cells, of neural crest origin, which are capable of forming and secreting catecholamines. This occurs in tumours arising predominantly from the sympathetic rather than the parasympathetic nervous system. Adrenal paraganglionomas, usually referred to as phaeochromocytomas, account for 90% of all such tumours, with only 10% being found outside the adrenal and no more than 3–4% of these being in the head and neck. Less than 5% of head and neck PGs secrete catecholamines and as in all extraadrenal catecholamine secreting paraganglionomas (CSPs) they produce predominantly norepinephrine and little epinephrine. Their aetiology is unknown in most cases but about 25% have mutations involving RET, VHL, TVF1, SDHB, SDHC or SDHD genes. The majority of these tumours can be localized by scanning with I-131 labelled MIBG, III In-octreotide or 18F-dopa positron emission tomography (1) (2) (3).
In this paper, we report a patient with a single carotid body catecholamine secreting paraganglionoma (CSP) in whom high dose octreotide produced a complete clinical and near complete biochemical remission. Her details are reported below.
Case presentation
A 48-year-old hypertensive and diabetic patient presented to another hospital with a 10-year history of progressive right facial pain, tinnitus, hearing loss, sweating, and palpitations. Investigations revealed a 5.5 cm tumor close to the carotid bifurcation (Fig. 1a). Her diabetes was poorly controlled although taking 100 U of insulin daily (HbA1c, 10.8%), and her blood pressure (BP) was 170/110 in spite of taking amlodipine 10 mg daily and lisinopril 20 mg daily. She was referred to our hospital for embolization where she was given a β-blocker in addition to her other medications; several hours later her BP increased to 240/130 and the procedure was cancelled. A pheochromocytoma was suspected.
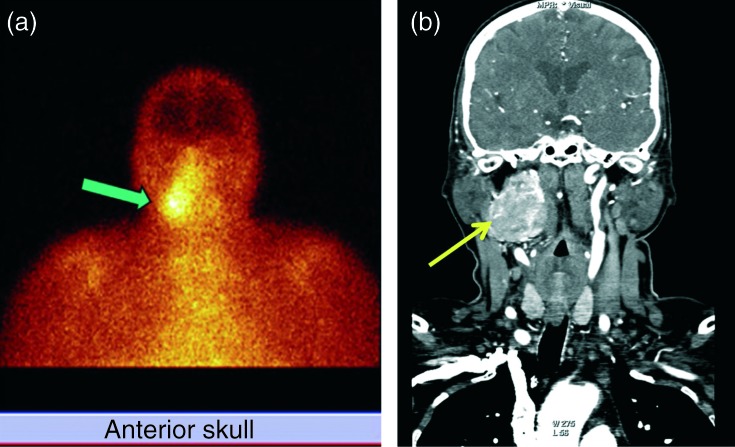
Figure 1.
(a) CT of the head and neck showing a large vascular tumor sized 5.6×5 cm extending from the base of skull to C3 and terminating just above the carotid bifurcation. (b) 111In-Octreotide scan showing a catecholamine-secreting carotid body paraganglioma.
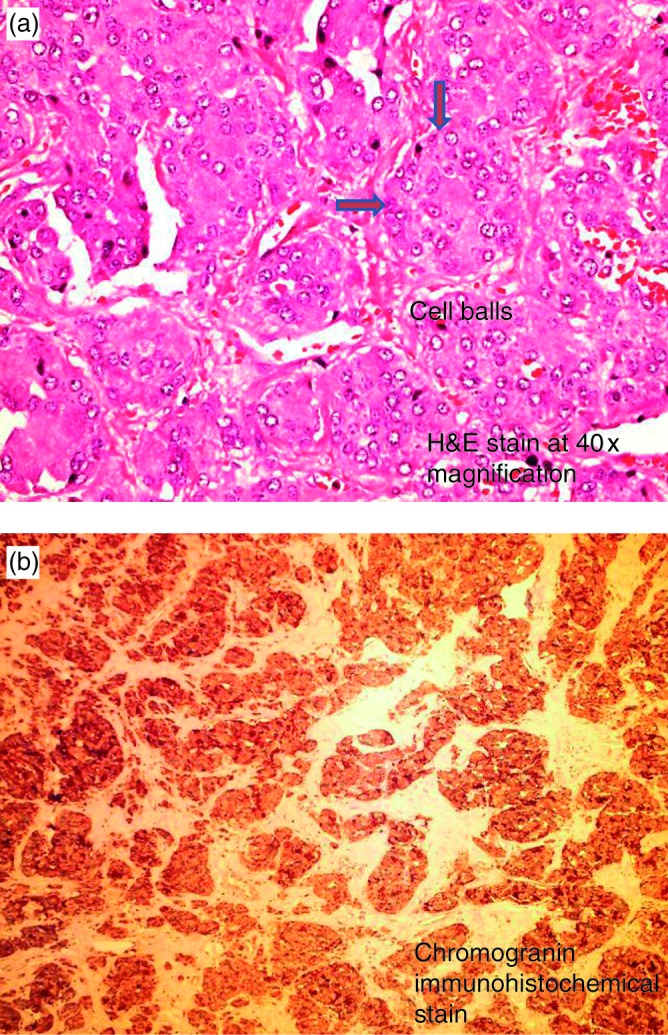
Investigation
Her plasma norepinephrine (NE) level grossly elevated to 89 000 pmol/l (normal value: 240–2400) and dopamine 6506 pmol/l (normal value: <475) with a low normal epinephrine level 39 pmol/l (normal value: <273). The chromogranin A (CgA) level was also raised 279 μg/l (normal range: 27–94). 111In-octreotide (Fig. 1a) and 131 meta-iodobenzylguanidine scanning revealed a solitary tumor in the right neck. CT scanning of the neck revealed a large right-sided vascular tumor extending from the base of the skull and terminating just above the carotid bifurcation (Fig. 1b) and the adrenals were normal. Histopathological examination showed a neoplasm composed of cell balls, which in turn were made up of rounded cells with abundant eosinophilic cytoplasm. The tumor cells were positive for neuroendocrine markers CgA and synaptophysin. The surrounding sustenticular cells were positive for S-100. The morphology and immunohistochemical profile were diagnostic of a paraganglioma. The submandibular salivary gland and lymph nodes were also submitted for histology and were negative for metastatic tumor.
Treatment
After careful explanation, the patient and her family consented to a therapeutic trial of octreotide.
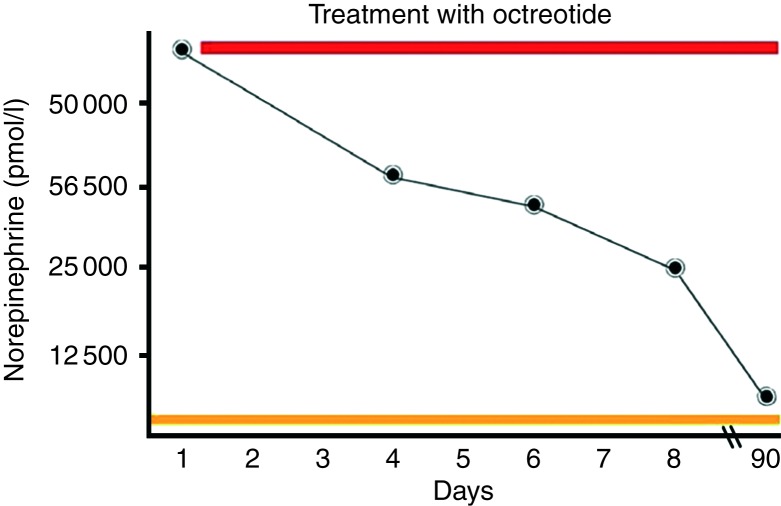
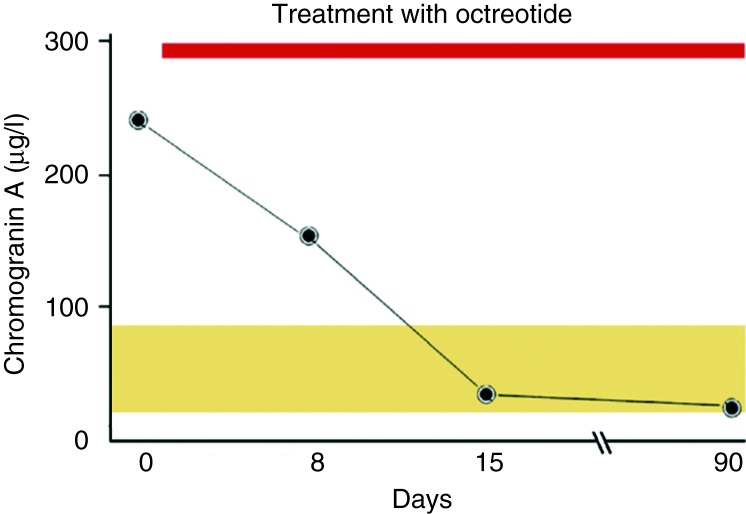
Initially, octreotide was given at a dose of 100 μg 8 h and, after 1 week off all medications, the plasma NE level had dropped from 50 000 to 25 000 pmol/l (Fig. 2) and the CgA level returned to normal (Fig. 3). Having established its potential value, the family consented to the use of octreotide-LA 40 mg every month. This was started together with labetalol 200 mg twice daily to maintain a BP of <150 systolic; she was unable to tolerate more than 400 mg labetalol daily. After 3 months, there was considerable clinical improvement with reduced facial pain, tinnitus, sweating, and palpitation, but the patient still required the use of 200 mg labetalol bid.
Figure 2.
Chromogranin immunohistochemical stain strongly positive in tumor cells.
Figure 3.
Serum NE levels before and during treatment with octreotide.
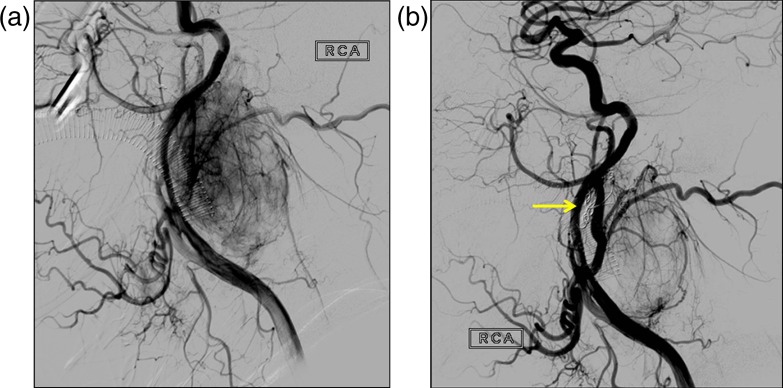
The dose of octreotide was therefore increased to 80 mg a month, a dose similar to that which has proved successful in resistant cases of acromegaly (4). She improved dramatically with loss of all her presenting symptoms. Her hearing aid was discarded. The labetalol was reduced to 100 mg bid after 1 month and was stopped three days before tumor embolization with maintenance of a normal BP of 135/80 and a slightly elevated NE level of 5000 pmol/l (Fig. 2). Blood flow before and after embolization is shown in Fig. 4a and b. The surgery was uneventful with only three mild BP spikes occurring during the 10-h procedure when the tumor 5.6×5 cm was resected completely (Fig. 5).
Figure 4.
Serum CgA levels before and during treatment with octreotide.
Figure 5.
(a) Pre-embolization showing a vascular tumor. (b) Post-embolization showing reduced tumor vascularity.
Outcome and follow-up
The patient's diabetes throughout her medical treatment still required 100 U insulin daily. Two months after surgery, however, she no longer required insulin and had a normal BP (130/80), CgA, and NE levels. After 21 months, the patient remains completely normal and is taking only indapamide for mild systolic hypertension.
Discussion
Paragangliomas are rare neuroendocrine tumors (NETs), the majority of which have receptors for somatostatin and should theoretically respond to treatment with the somatostatin analogue octreotide (5) (6). Although there is abundant literature on the beneficial use of octreotide in patients with NETs in the thyroid gland, the chest, the pancreas, and the gut (7) (8) (9), there are no previous reports of its successful use in the control of the clinical and biochemical abnormalities of patients with CSP. In fact, several publications suggested that it is not useful. Plouin et al. (10) found no significant effect of octreotide on BP or plasma catecholamines when given acutely over a 24-h period. In another study (11), octreotide-LA 30 mg was given monthly for 3 months to eight patients with head and neck paragangliomas. Catecholamine levels were not reported, but two of the 18 tumors shrunk by more than 20%. The authors concluded that octreotide-LA is not useful in the preoperative management of paragangliomas. Of considerable interest to us, however, was the authors' observation that the largest reduction in tumor volume occurred in the only patient whose tumor secreted catecholamines.
The patient in this case report had extremely elevated levels of NE (37 times the upper limit). NE levels progressively decreased along with CgA levels during a short 8 day trial of octreotide (Figs 3 and 4). As the patient initially refused to undergo surgery, she was managed with long-acting octreotide every month combined with labetalol. After 3 months, she had improved but still required 200 mg labetalol bid in addition to octreotide in order to maintain a normal BP. We then decided to double her octreotide-LA dose to 80 mg a month.
There was a dramatic clinical response, upon which her labetalol was safely reduced to 100 mg bid. Three days before surgery, labetalol was completely withdrawn with maintenance of a normal BP, normal CgA levels, and a modest elevation of her NE levels. The dose of octreotide-LA used by us was prompted by the observation that patients with acromegaly, resistant to conventional doses, subsequently respond to a much higher dose (4). It is also of interest that the patient continued to require large doses of insulin during treatment, presumably because her insulin secretion was inhibited by octreotide. This postulation is supported by the fact that insulin was no longer required for the control of her diabetes after discontinuation of the octreotide, removal of the tumor, and normalization of NE levels. We and others find CgA levels to be of value in the diagnosis and follow-up of patients with pheochromocytomas (12). It is now 21 months since our patient's surgery. She remains normotensive without treatment with a normal CgA 15 μg/l.
Patient consent
We confirm that we have obtained written informed consent from the patient for publication of the submitted article and accompanying images.
Author contribution statement
O Elshafie, A Almamari, and N Woodhouse were responsible for the diagnosis and management of the patient throughout treatment and preparation of the manuscript. Y Al Badaai and K Alwahaibi performed the surgery. A Qureshi reported the pathology. S Hussein and F Al Azzri were responsible for performing the imaging and reporting the studies as well as embolization of the tumor.
Declaration of interest
The authors declare that there is no conflict of interest that could be perceived as prejudicing the impartiality of the research reported.
Funding
This research did not receive any specific grant from any funding agency in the public, commercial or not-for-profit sector.
References
- 1.Neumann HP. Phaeochromocytoma. In Harrison's Endocrinology, 2nd edn, pp 133–141, 2010.
- 2.Telischi FF, Bustillo A, Whiteman ML, Serafini AN, Reisberg MJ, Gomez-Marin O, Civantos FJ & Balkany TJ. 2000Octreotide scintigraphy for the detection of paragangliomas. Otolaryngology – Head and Neck Surgery. 358–362 [DOI] [PubMed] [Google Scholar]
- 3.Hoegerle S, Ghanem N, Altehoefer C, Schipper J, Brink I, Moser E & Neumann HP. 2003 18F-DOPA positron emission tomography for the detection of glomus tumours. European Journal of Nuclear Medicine and Molecular Imaging. 30: 689–694 10.1007/s00259-003-1115-3 [DOI] [PubMed] [Google Scholar]
- 4.Giustina A, Bonadonna S, Bugari G, Colao A, Cozzi R, Cannavo S, de Marinis L, Uberti E, Bogazzi F, Mazziotti Get al. 2009High-dose intramuscular octreotide in patients with acromegaly inadequately controlled on conventional somatostatin analogue therapy: a randomized controlled trial. European Journal of Endocrinology. 161: 331–338 10.1530/EJE-09-0372 [DOI] [PubMed] [Google Scholar]
- 5.Erickson D, Kudva YC, Ebersold MJ, Thompson GB, Grant CS, van Heerden JA & Young WF Jr2001Benign paragangliomas: clinical presentation and treatment outcomes in 236 patients. Journal of Clinical Endocrinology and Metabolism. 86: 5210–5216 10.1210/jcem.86.11.8034 [DOI] [PubMed] [Google Scholar]
- 6.Schwaber MK, Glasscock ME, Nissen AJ, Jackson CG & Smith PG. 1984Diagnosis and management of catecholamine secreting glomus tumours. Laryngoscope. 94: 1008–1015 10.1288/00005537-198408000-00002 [DOI] [PubMed] [Google Scholar]
- 7.Hearn PR, Reynolds CL, Johansen K & Woodhouse NJY. 1988Lung carcinoid with Cushing's syndrome: control of serum ACTH and cortisol levels using SMS 201-995 (Sandostatin). Clinical Endocrinology. 28: 181–185 10.1111/j.1365-2265.1988.tb03654.x [DOI] [PubMed] [Google Scholar]
- 8.Johansen K, Reid K & Woodhouse NJY. 1988Acute ACTH-lowering effect of SMS 201-995 (Sandostatin) in a patient with Cushing's syndrome due to ectopic ACTH-producing lung carcinoid. Saudi Medical Journal. 9: 513–514 [Google Scholar]
- 9.Woodhouse NJY, Dagogo-Jack S & Ahmed M. 1993Acute and long-term effects of octreotide in ACTH dependent Cushing's syndrome. American Journal of Medicine. 95: 305–308 10.1016/0002-9343(93)90283-U [DOI] [PubMed] [Google Scholar]
- 10.Plouin PF, Bertherat J, Chateiller O, Billaud E, Azizi M, Grouzmann E & Epelbaum J. 1995Short-term effects of octreotide on blood pressure and plasma catecholamines and neuropeptide Y levels in patients with phaeochromocytoma: a placebo-controlled trial. Clinical Endocrinology. 42: 289–294 10.1111/j.1365-2265.1995.tb01877.x [DOI] [PubMed] [Google Scholar]
- 11.Duet M, Guichard JP, Rizzo N, Boudiaf M, Herman P & Tran Ba Huy P. 2005Are somatostatin analogs therapeutic alternatives in the management of head and neck paragangliomas?. Laryngoscope. 115: 1381–1384 10.1097/01.MLG.0000165806.99675.A9 [DOI] [PubMed] [Google Scholar]
- 12.Grossrubatscher E, Dalino P, Vignati F, Gambacorta M, Pugliese R, Boniardi M, Rossetti O, Marocchi A, Bertuzzi M & Loli P. 2006The role of chromogranin A in the management of patients with phaeochromocytoma. Clinical Endocrinology. 65: 287–293 10.1111/j.1365-2265.2006.02591.x [DOI] [PubMed] [Google Scholar]



 This work is licensed under a
This work is licensed under a