Abstract
Mechanical cardiac unloading with use of a left ventricular assist device (LVAD) is associated with substantial improvements in left ventricular function and enables subsequent LVAD explantation in some patients. We describe the case of a 35-year-old man with dilated nonischemic cardiomyopathy who was supported with an LVAD for 9 months. After the device was removed, he led a normal life for 13 years and 4 months. However, at 49 years of age, he presented with new signs and symptoms of heart failure, necessitating implantation of a 2nd LVAD. Afterwards, he has remained asymptomatic. This case is unique in that the patient lived a normal life for longer than a decade before renewed left ventricular decompensation necessitated repeat LVAD therapy. Histologic examination revealed few changes between the first device's removal in 1999 and the 2nd device's implantation in 2012.
Keywords: Cardiomyopathy, dilated/physiopathology/therapy; device removal; heart failure/physiopathology/therapy; heart-assist devices; myocytes, cardiac/pathology; recovery of function/physiology; recurrence; time factors; treatment outcome; ventricular dysfunction, left/physiology; ventricular remodeling
In patients with advanced heart failure, mechanical support with a left ventricular assist device (LVAD) typically leads to improved circulatory function. Mechanical cardiac unloading is also associated with substantial improvements in left ventricular (LV) function and enables LVAD explantation in some patients.1 After device removal, these patients are treated medically,2,3 and some never need heart transplantation. Conversely, in other patients, emergent implantation of another LVAD is necessary shortly after removal of the first device.4
We describe the case of a patient with familial dilated cardiomyopathy who underwent implantation of an LVAD as a bridge to transplantation. The LVAD had to be removed within a year, and the patient then led a normal life for longer than 13 years before new signs and symptoms of heart failure emerged. We found no previous report of any patient's leading a normal life for so long after device removal before needing a 2nd LVAD.
Case Report
February 1997: Initial Presentation. In February 1997, a 35-year-old man presented at the Texas Heart Institute with advanced heart failure due to idiopathic dilated cardiomyopathy. The patient's family medical history was noteworthy because his father, a sister, and a cousin had died of heart failure. Despite ongoing maximal medical care, the patient's clinical condition had continued to deteriorate, with a decrease in blood pressure and a low cardiac output. A chest radiograph showed considerable cardiomegaly and vascular congestion (Fig. 1).5 Echocardiograms revealed a severely dilated LV and a low systolic LV ejection fraction (LVEF) (Table I). On catheterization, the cardiac index was 1.68 L/min/m2, and the LV end-diastolic pressure was 25 mmHg. The results of coronary angiography were normal. The patient was placed on the waiting list for cardiac transplantation.
Fig. 1.

February 1997. Chest radiograph from the patient's initial presentation shows considerable cardiomegaly and vascular congestion.
Reproduced with permission, from Razeghi P, Myers TJ, Frazier OH, Taegtmeyer H. Reverse remodeling of the failing human heart with mechanical unloading. Emerging concepts and unanswered questions. Cardiology 2002;98(4):167–74.5 Copyright ©2003, Karger Publishers; Basel, Switzerland.
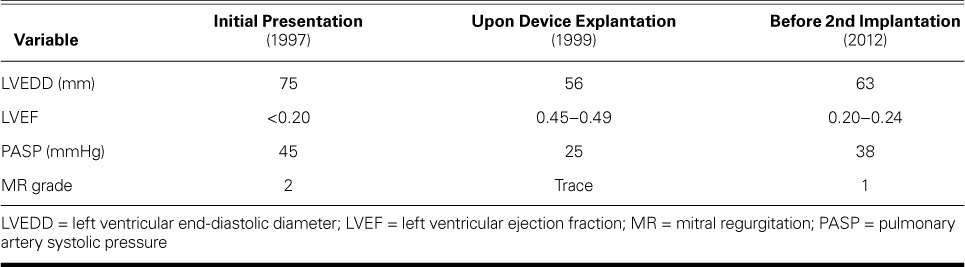
TABLE I.
Echocardiographic Data of the Patient
November 1998: First Device Implantation. The patient experienced further clinical deterioration while awaiting a donor heart. In November 1998, he underwent implantation of a HeartMate® XVE Left Ventricular Assist System (Thoratec Corporation; Pleasanton, Calif). An LV core biopsy specimen revealed moderate myocyte hypertrophy and interstitial fibrosis (Fig. 2A).5 When examined by means of transmission electron microscopy, the myocardial specimen exhibited cellular features of dilated cardiomyopathy, including a paucity of sarcomeres and mitochondria, large amounts of unspecified cytoplasm, and presumed nuclear heterochromatin (Fig. 2B).5 The patient's condition improved after LVAD implantation, and he was discharged from the hospital on a supplemental medical regimen consisting of a β-blocker, an angiotensin-converting enzyme inhibitor, furosemide, and potassium supplements.
Fig. 2.
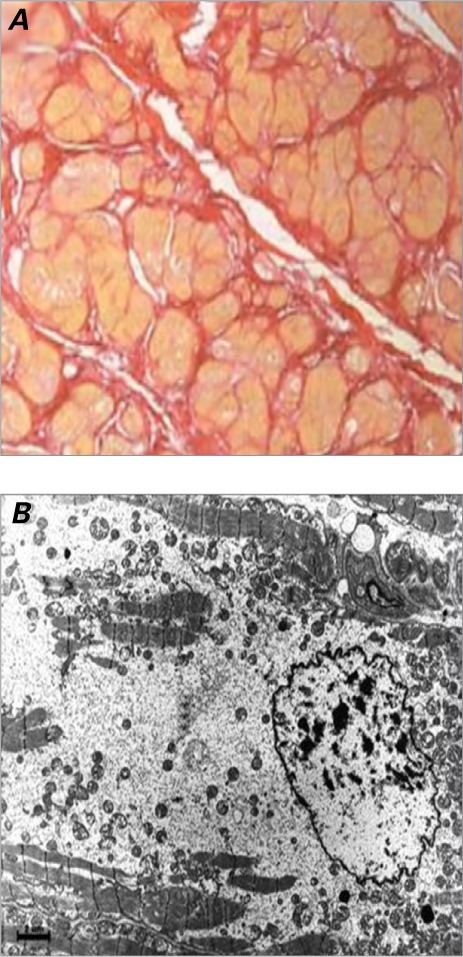
November 1998. Analysis of left ventricular myocardial biopsy specimens upon initial left ventricular assist device implantation. A) Photomicrograph shows moderate myocyte hypertrophy and interstitial fibrosis (picrosirius red stain, orig. ×10).
Reproduced with permission, from Razeghi P, Myers TJ, Frazier OH, Taegtmeyer H. Reverse remodeling of the failing human heart with mechanical unloading. Emerging concepts and unanswered questions. Cardiology 2002;98(4):167–74.5 Copyright ©2003, Karger Publishers; Basel, Switzerland.
B) Transmission electron microscopic image shows few sarcomeres or mitochondria, large amounts of unspecified cytoplasm, and dark spots that are presumably nuclear heterochromatin.
July 1999: Device Explantation. Nine months later (in July 1999), the patient was readmitted with malaise and a fever. An LVAD driveline infection was detected, and cultures grew methicillin-resistant Staphylococcus aureus. Right-sided heart catheterization with minimal device support was performed, to determine the patient's candidacy for LVAD explantation. The results included a pulmonary artery pressure of 24/9 mmHg (mean, 11 mmHg), a pulmonary capillary wedge pressure of 8 mmHg, and a cardiac output of 6.4 L/min. Dobutamine stress echocardiograms revealed an LVEF of 0.45 to 0.49 and a normal LV size (Table I). Because of the driveline infection and the adequate contractile reserve of the LV myocardium, the LVAD was explanted. A chest radiograph showed only mild cardiomegaly (Fig. 3A).5 Histologic examination of LV myocardial specimens yielded a reduction in endomyocardial interstitial fibrosis and myocyte hypertrophy (Fig. 3B).5 Transmission electron microscopic images of the myocardium showed repopulation of the unspecified cytoplasm with sarcomeres and mitochondria, and the nuclear structure was more uniform (Fig. 3C).5 These findings were all consistent with improved LV systolic function.
Fig. 3.
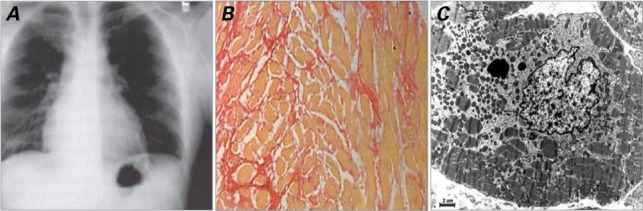
July 1999. Explantation of device. A) Chest radiograph shows only mild cardiomegaly. B) Photomicrograph of left ventricular myocardial specimen shows reduced interstitial fibrosis and myocyte hypertrophy in comparison with preimplantation findings (picrosirius red stain, orig. ×10).
Reproduced with permission, from Razeghi P, Myers TJ, Frazier OH, Taegtmeyer H. Reverse remodeling of the failing human heart with mechanical unloading. Emerging concepts and unanswered questions. Cardiology 2002;98(4):167–74.5 Copyright ©2003, Karger Publishers; Basel, Switzerland.
C) Transmission electron microscopic image of the specimen reveals, in comparison with preimplantation findings, repopulation of the unspecified cytoplasm with sarcomeres and mitochondria, and a more uniform nuclear structure.
The patient was discharged from the hospital and was monitored by his physician at 3-month intervals. He remained in New York Heart Association functional class I on a regimen of furosemide, metoprolol, lisinopril, and digoxin. He returned to his normal activities and resumed gainful employment for the next 13 years.
November 2012: 2nd Device Implantation. In November 2012—13 years and 4 months after device explantation—the 49-year-old patient developed an upper respiratory tract infection and dyspnea on exertion. The infection responded to antibiotic therapy; however, the patient's shortness of breath worsened until it involved orthopnea and frequent episodes of paroxysmal nocturnal dyspnea. A chest radiograph showed cardiomegaly with pulmonary congestion (Fig. 4A). Echocardiograms revealed an LVEF of 0.20 to 0.24 and an LV end-diastolic diameter of 63 mm (Table I). The results of left- and right-sided catheterization included normal coronary arteries, a pulmonary wedge capillary pressure of 35 mmHg, and a cardiac index of 1.3 L/min/m2. An intra-aortic balloon was inserted for hemodynamic support, followed by the implantation of a HeartWare® Ventricular Assist System (HeartWare Inc.; Framingham, Mass). An LV myocardial biopsy specimen exhibited mild-to-moderate hypertrophy (Fig. 4B), with moderate perivascular and interstitial fibrosis similar to what had been seen before the patient's LVAD explantation in 1999. Three weeks later, the patient was discharged from the hospital on a regimen of carvedilol (12.5 mg 2x/d), valsartan (160 mg/d), spironolactone (25 mg/d), bumetanide (1 mg 2x/d), dipyridamole (75 mg 3x/d), and warfarin (5 mg/d). As of June 2014, he continued to undergo evaluation at monthly intervals and remained asymptomatic.
Fig. 4.
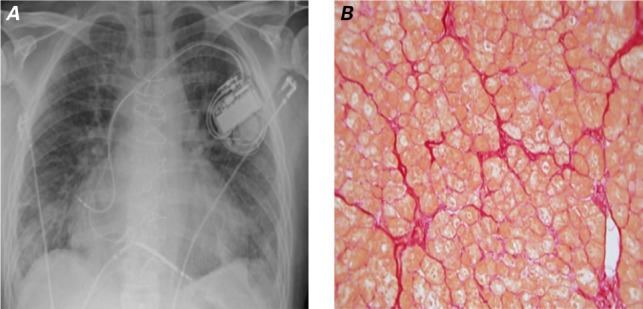
November 2012. At the time of the 2nd left ventricular assist device implantation, A) chest radiograph shows cardiomegaly with pulmonary congestion, and B) photomicrograph shows mild-to-moderate hypertrophy with moderate perivascular and interstitial fibrosis (picrosirius red stain, orig. ×10). The hypertrophy is comparatively reduced, and the histologic appearance is similar to the findings before the first implantation (see Fig. 2A). The interstitial fibrosis appears to have increased only minimally since the first device was explanted (see Fig. 3B).
Discussion
To our knowledge, this is the first report of a patient who underwent LVAD explantation and then needed a 2nd LVAD after a symptom-free interval longer than a decade. The historical experience with LVAD explantation has been short, and only now are long-term results becoming available.6 Our patient's clinical presentation supports the concept of “heart failure in remission” and supports the idea that certain patients can be weaned from cardiac assist devices. However, there is still no reliable predictor of long-term outcome after device removal.7 In addition, our patient's story raises several points to consider.
-
1)
Improved or normal contractile function is a hallmark of the remission of heart failure. Our patient's cardiac functional improvement enabled LVAD explantation; however, the abnormality underlying the cardiomyopathy remained. Despite pharmacologic therapy and normal cardiac function for a prolonged period, late decompensation of LV function occurred. This occurrence lends credence to the following concept: mechanical unloading of the failing heart might induce remission but not recovery from the idiopathic process responsible for heart failure, which involves a complex process of myocardial remodeling.5 Nevertheless, the prolonged improvement in our patient's cardiac function—achieved through mechanical unloading—produced a substantial clinical benefit. In a series described by Birks and colleagues,6 40 patients underwent LVAD implantation as a bridge to recovery. Their overall duration of support was 331.6 ± 223.4 days. After undergoing device removal, 4 patients (10%) required heart transplantation (at 34, 512, 1,019, and 1,213 d). At 7 years, the overall survival rate was 73.9%, and the rate of freedom from death or transplantation was 69%. None of the patients needed another LVAD. The longest survival period in that series was 7 years after LVAD removal, whereas our patient lived without an LVAD almost twice as long. However, Birks and colleagues6 did not distinguish “recovery” (their term) from “remission” (our term) of heart failure by means of mechanical unloading.
-
2)
Mechanical unloading benefits specific characteristics of myocardial structure and cardiovascular function,8 including hemodynamic performance,9,10 LV chamber size and mass,1,11 myocyte size,12,13 myocyte contractility,14–17 and β-adrenergic sensitivity.14 Mechanical cardiac support also improves many aspects of intracellular calcium cycling2,18,19 and reduces circulating levels of neurohormones20 and inflammatory mediators.21 Furthermore, mechanical support is associated with improved respiratory capacity and increased nitric oxide-dependent control of mitochondrial respiration.22–24
-
3)
Despite the benefits of ventricular unloading at the cellular and clinical levels, relatively few patients have undergone LVAD explantation.3,4,25–29 To date, only a few investigators have evaluated long-term survival after LVAD explantation.6,28 The beneficial effects of LVAD unloading appear to be related to the origin of the cardiomyopathy and the severity and duration of the disease.30 Although a genetic cause for our patient's cardiac dilation and heart failure has not yet been ruled out, we have been unable to establish a specific cause. Mechanical unloading results in much greater improvement in patients who have nonischemic dilated cardiomyopathy than in patients who have end-stage heart failure related to an acute myocardial infarction.31 Moreover, device-related recovery of function is better in patients who have acute heart failure than in those who have chronic heart failure.31,32 A possible reason for this difference is the reactivation of the fetal gene program in patients with chronic heart failure.33
-
4)
Currently, no blood-borne markers can reliably predict sustained myocardial improvement consequent to mechanical support. However, in previous studies, Müller and colleagues3 found elevated anti-β1-adrenoceptor autoantibody levels in the sera of 80% of patients who had idiopathic dilated cardiomyopathy. Levels of these antibodies returned to normal in the patients whose LV function improved after mechanical unloading. In addition, evaluating histologic values at the time of LVAD implantation might help to identify patients whose mechanical circulatory support might be safely discontinued later.34 Fewer structural changes (less hypertrophy and fibrosis) and lower cardiac expression levels of miR-23a and miR-195 transcripts are observed in the hearts of patients whose LVADs can be explanted than in patients who need continued ventricular support.34,35 Our patient's histologic results showed an improved architecture after LVAD support, with a reduction in myocyte size and only mild-to-moderate perivascular fibrosis at the time of LVAD explantation. Similar histologic changes were seen in the new LV core specimen upon implantation of the 2nd device, with a very small increase in the amount of interstitial collagen in some areas. In all the examined sections, there was minimal replacement fibrosis. Our patient's heart failure clearly went into remission; however, the causative disease process remained.
The medical literature contains other reports of recurrent heart failure after device explantation36; however, those recurrences took place just months to 3 years after LVAD removal, and the recurrence rate was higher in older patients and in those with longer durations of heart failure.28 Our patient's case is unique for 2 reasons: his symptom-free interval of 13 years and 4 months after LVAD removal, and the notably few histologic cardiac changes observed between device explantation and reimplantation. Currently, we have an incomplete understanding of the reverse remodeling changes that might enable long-term cardiac functional improvement and the remission of heart failure.37 Further studies are needed to define the molecular mechanisms for the remission of heart failure consequent to LV mechanical unloading.
Acknowledgments
The authors thank Sylvia Carranza, BS, and Ralph Nichols, BS, for technical assistance, Dr. Nicholas Banner and Ms Virginia Fairchild for critical review of the manuscript, and Mrs. Roxy A. Tate for editorial help.
Footnotes
Drs. Segura and Dris contributed equally to the manuscript.
Dr. Taegtmeyer's laboratory is supported by a grant from the U.S. Public Health Service (R01 HL 061483).
References
- 1.Levin HR, Oz MC, Chen JM, Packer M, Rose EA, Burkhoff D. Reversal of chronic ventricular dilation in patients with end-stage cardiomyopathy by prolonged mechanical unloading. Circulation. 1995;91(11):2717–20. doi: 10.1161/01.cir.91.11.2717. [DOI] [PubMed] [Google Scholar]
- 2.Ambardekar AV, Buttrick PM. Reverse remodeling with left ventricular assist devices: a review of clinical, cellular, and molecular effects. Circ Heart Fail. 2011;4(2):224–33. doi: 10.1161/CIRCHEARTFAILURE.110.959684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Muller J, Wallukat G, Weng YG, Dandel M, Spiegelsberger S, Semrau S et al. Weaning from mechanical cardiac support in patients with idiopathic dilated cardiomyopathy. Circulation. 1997;96(2):542–9. doi: 10.1161/01.cir.96.2.542. [DOI] [PubMed] [Google Scholar]
- 4.Mancini DM, Beniaminovitz A, Levin H, Catanese K, Flannery M, DiTullio M et al. Low incidence of myocardial recovery after left ventricular assist device implantation in patients with chronic heart failure. Circulation. 1998;98(22):2383–9. doi: 10.1161/01.cir.98.22.2383. [DOI] [PubMed] [Google Scholar]
- 5.Razeghi P, Myers TJ, Frazier OH, Taegtmeyer H. Reverse remodeling of the failing human heart with mechanical unloading. Emerging concepts and unanswered questions. Cardiology. 2002;98(4):167–74. doi: 10.1159/000067313. [DOI] [PubMed] [Google Scholar]
- 6.Birks EJ, George RS, Firouzi A, Wright G, Bahrami T, Yacoub MH, Khaghani A. Long-term outcomes of patients bridged to recovery versus patients bridged to transplantation. J Thorac Cardiovasc Surg. 2012;144(1):190–6. doi: 10.1016/j.jtcvs.2012.03.021. [DOI] [PubMed] [Google Scholar]
- 7.Hetzer R, Muller JH, Weng Y, Meyer R, Dandel M. Bridging-to-recovery. Ann Thorac Surg. 2001;71(3 Suppl):S109–15. doi: 10.1016/s0003-4975(00)02638-2. [DOI] [PubMed] [Google Scholar]
- 8.Razeghi P, Young ME, Ying J, Depre C, Uray IP, Kolesar J et al. Downregulation of metabolic gene expression in failing human heart before and after mechanical unloading. Cardiology. 2002;97(4):203–9. doi: 10.1159/000063122. [DOI] [PubMed] [Google Scholar]
- 9.Frazier OH, Benedict CR, Radovancevic B, Bick RJ, Capek P, Springer WE et al. Improved left ventricular function after chronic left ventricular unloading. Ann Thorac Surg. 1996;62(3):675–82. doi: 10.1016/s0003-4975(96)00437-7. [DOI] [PubMed] [Google Scholar]
- 10.Drakos SG, Kfoury AG, Stehlik J, Selzman CH, Reid BB, Terrovitis JV et al. Bridge to recovery: understanding the disconnect between clinical and biological outcomes. Circulation. 2012;126(2):230–41. doi: 10.1161/CIRCULATIONAHA.111.040261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Madigan JD, Barbone A, Choudhri AF, Morales DL, Cai B, Oz MC, Burkhoff D. Time course of reverse remodeling of the left ventricle during support with a left ventricular assist device. J Thorac Cardiovasc Surg. 2001;121(5):902–8. doi: 10.1067/mtc.2001.112632. [DOI] [PubMed] [Google Scholar]
- 12.Zafeiridis A, Jeevanandam V, Houser SR, Margulies KB. Regression of cellular hypertrophy after left ventricular assist device support. Circulation. 1998;98(7):656–62. doi: 10.1161/01.cir.98.7.656. [DOI] [PubMed] [Google Scholar]
- 13.Rivello HG, Meckert PC, Vigliano C, Favaloro R, Laguens RP. Cardiac myocyte nuclear size and ploidy status decrease after mechanical support. Cardiovasc Pathol. 2001;10(2):53–7. doi: 10.1016/s1054-8807(01)00068-0. [DOI] [PubMed] [Google Scholar]
- 14.Dipla K, Mattiello JA, Jeevanandam V, Houser SR, Margulies KB. Myocyte recovery after mechanical circulatory support in humans with end-stage heart failure. Circulation. 1998;97(23):2316–22. doi: 10.1161/01.cir.97.23.2316. [DOI] [PubMed] [Google Scholar]
- 15.Heerdt PM, Holmes JW, Cai B, Barbone A, Madigan JD, Reiken S et al. Chronic unloading by left ventricular assist device reverses contractile dysfunction and alters gene expression in end-stage heart failure. Circulation. 2000;102(22):2713–9. doi: 10.1161/01.cir.102.22.2713. [DOI] [PubMed] [Google Scholar]
- 16.Ogletree-Hughes ML, Stull LB, Sweet WE, Smedira NG, McCarthy PM, Moravec CS. Mechanical unloading restores beta-adrenergic responsiveness and reverses receptor downregulation in the failing human heart. Circulation. 2001;104(8):881–6. doi: 10.1161/hc3301.094911. [DOI] [PubMed] [Google Scholar]
- 17.Drakos SG, Wever-Pinzon O, Selzman CH, Gilbert EM, Alharethi R, Reid BB et al. Magnitude and time course of changes induced by continuous-flow left ventricular assist device unloading in chronic heart failure: insights into cardiac recovery. J Am Coll Cardiol. 2013;61(19):1985–94. doi: 10.1016/j.jacc.2013.01.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hall JL, Fermin DR, Birks EJ, Barton PJ, Slaughter M, Eckman P et al. Clinical, molecular, and genomic changes in response to a left ventricular assist device. J Am Coll Cardiol. 2011;57(6):641–52. doi: 10.1016/j.jacc.2010.11.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hall JL, Birks EJ, Grindle S, Cullen ME, Barton PJ, Rider JE et al. Molecular signature of recovery following combination left ventricular assist device (LVAD) support and pharmacologic therapy. Eur Heart J. 2007;28(5):613–27. doi: 10.1093/eurheartj/ehl365. [DOI] [PubMed] [Google Scholar]
- 20.James KB, McCarthy PM, Thomas JD, Vargo R, Hobbs RE, Sapp S, Bravo E. Effect of the implantable left ventricular assist device on neuroendocrine activation in heart failure. Circulation. 1995;92(9 Suppl):II191–5. doi: 10.1161/01.cir.92.9.191. [DOI] [PubMed] [Google Scholar]
- 21.Torre-Amione G, Stetson SJ, Youker KA, Durand JB, Radovancevic B, Delgado RM et al. Decreased expression of tumor necrosis factor-alpha in failing human myocardium after mechanical circulatory support: a potential mechanism for cardiac recovery. Circulation. 1999;100(11):1189–93. doi: 10.1161/01.cir.100.11.1189. [DOI] [PubMed] [Google Scholar]
- 22.Lee SH, Doliba N, Osbakken M, Oz M, Mancini D. Improvement of myocardial mitochondrial function after hemodynamic support with left ventricular assist devices in patients with heart failure. J Thorac Cardiovasc Surg. 1998;116(2):344–9. doi: 10.1016/s0022-5223(98)70136-9. [DOI] [PubMed] [Google Scholar]
- 23.Mital S, Loke KE, Addonizio LJ, Oz MC, Hintze TH. Left ventricular assist device implantation augments nitric oxide-dependent control of mitochondrial respiration in failing human hearts. J Am Coll Cardiol. 2000;36(6):1897–902. doi: 10.1016/s0735-1097(00)00948-7. [DOI] [PubMed] [Google Scholar]
- 24.Hill JA, Olson EN. Cardiac plasticity. N Engl J Med. 2008;358(13):1370–80. doi: 10.1056/NEJMra072139. [DOI] [PubMed] [Google Scholar]
- 25.Maybaum S, Kamalakannan G, Murthy S. Cardiac recovery during mechanical assist device support. Semin Thorac Cardiovasc Surg. 2008;20(3):234–46. doi: 10.1053/j.semtcvs.2008.08.003. [DOI] [PubMed] [Google Scholar]
- 26.Frazier OH, Myers TJ. Left ventricular assist system as a bridge to myocardial recovery. Ann Thorac Surg. 1999;68(2):734–41. doi: 10.1016/s0003-4975(99)00801-2. [DOI] [PubMed] [Google Scholar]
- 27.Yacoub MH. A novel strategy to maximize the efficacy of left ventricular assist devices as a bridge to recovery. Eur Heart J. 2001;22(7):534–40. doi: 10.1053/euhj.2001.2613. [DOI] [PubMed] [Google Scholar]
- 28.Dandel M, Weng Y, Siniawski H, Potapov E, Lehmkuhl HB, Hetzer R. Long-term results in patients with idiopathic dilated cardiomyopathy after weaning from left ventricular assist devices. Circulation. 2005;112(9 Suppl):I37–45. doi: 10.1161/CIRCULATIONAHA.104.525352. [DOI] [PubMed] [Google Scholar]
- 29.Birks EJ, Tansley PD, Hardy J, George RS, Bowles CT, Burke M et al. Left ventricular assist device and drug therapy for the reversal of heart failure. N Engl J Med. 2006;355(18):1873–84. doi: 10.1056/NEJMoa053063. [DOI] [PubMed] [Google Scholar]
- 30.Butler CR, Jugdutt BI. The paradox of left ventricular assist device unloading and myocardial recovery in end-stage dilated cardiomyopathy: implications for heart failure in the elderly. Heart Fail Rev. 2012;17(4–5):615–33. doi: 10.1007/s10741-012-9300-8. [DOI] [PubMed] [Google Scholar]
- 31.Maybaum S, Mancini D, Xydas S, Starling RC, Aaronson K, Pagani FD et al. Cardiac improvement during mechanical circulatory support: a prospective multicenter study of the LVAD Working Group. Circulation. 2007;115(19):2497–505. doi: 10.1161/CIRCULATIONAHA.106.633180. [DOI] [PubMed] [Google Scholar]
- 32.Frazier OH, Gradinac S, Segura AM, Przybylowski P, Popovic Z, Vasiljevic J et al. Partial left ventriculectomy: which patients can be expected to benefit? Ann Thorac Surg. 2000;69(6):1836–41. doi: 10.1016/s0003-4975(00)01344-8. [DOI] [PubMed] [Google Scholar]
- 33.Razeghi P, Young ME, Alcorn JL, Moravec CS, Frazier OH, Taegtmeyer H. Metabolic gene expression in fetal and failing human heart. Circulation. 2001;104(24):2923–31. doi: 10.1161/hc4901.100526. [DOI] [PubMed] [Google Scholar]
- 34.Segura AM, Frazier OH, Demirozu Z, Buja LM. Histopathologic correlates of myocardial improvement in patients supported by a left ventricular assist device. Cardiovasc Pathol. 2011;20(3):139–45. doi: 10.1016/j.carpath.2010.01.011. [DOI] [PubMed] [Google Scholar]
- 35.Ramani R, Vela D, Segura A, McNamara D, Lemster B, Samarendra V et al. A micro-ribonucleic acid signature associated with recovery from assist device support in 2 groups of patients with severe heart failure. J Am Coll Cardiol. 2011;58(22):2270–8. doi: 10.1016/j.jacc.2011.08.041. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Helman DN, Maybaum SW, Morales DL, Williams MR, Beniaminovitz A, Edwards NM et al. Recurrent remodeling after ventricular assistance: is long-term myocardial recovery attainable? Ann Thorac Surg. 2000;70(4):1255–8. doi: 10.1016/s0003-4975(00)01826-9. [DOI] [PubMed] [Google Scholar]
- 37.Mann DL, Barger PM, Burkhoff D. Myocardial recovery and the failing heart: myth, magic, or molecular target? J Am Coll Cardiol. 2012;60(24):2465–72. doi: 10.1016/j.jacc.2012.06.062. [DOI] [PMC free article] [PubMed] [Google Scholar]


