Abstract
Objective
This work provides descriptive statistics on hospice users. It also explores the magnitude of relative resource use during hospice episodes and whether such patterns vary by episode length for patients who only use routine home care as compared to those who use multiple levels of hospice care. Examining resource use for hospice users who require different hospice levels of care within an episode versus solely routine home care provides insight to the varied resource use associated with the different patient populations (i.e., those who may require steady routine home care across the entire episode versus those who require varied levels of care across the episode).
Data Source
The analyses were based on a longitudinal analytic file that was constructed from 100% of Medicare claims for hospice users with completed episodes spanning September 1, 2008 through the end of calendar year 2011. In examining resource use for routine home care users and all levels of hospice care, the analyses were restricted to single episode decedents who began their hospice episode on or after April 1, 2010 and whose date of death was on or before December 31, 2011. Daily wage-weighted visit units (WWVUs) were calculated for each patient during their hospice stay. In order to compute a WWVU, one-fourth of the Bureau of Labor Statistics hourly wage rate for each visit discipline (i.e., skilled nursing, medical social services, home health aide, and an average for therapies) was multiplied by the corresponding number of visit units reported on hospice claims.
Principal Findings
Using enhanced data on the intensity of service use, the results confirm previous research that suggested a curved pattern to service use during a hospice episode. For several measures of resource intensity, service use is more intensive during the initial days in the episode and for the last few days prior to death relative to the middle days of the episode. The pattern becomes more pronounced as episodes increase in length, but is otherwise a similar curve when compared by diagnosis. Thus, the results provide useful information for potential policy discussions about Medicare hospice reform.
Keywords: Medicare, Medicare hospice, hospice benefit, hospice resource use, hospice utilization
Introduction
The Medicare hospice benefit was established in 1983 to provide palliative care and support services to terminally ill patients—those with life expectancies of six months or less—and their families. Over time, utilization of the hospice benefit has grown considerably. In 2000, 23% of Medicare decedents used the hospice benefit compared with 44% in 2010 (MedPAC, 2012). Medicare spending increased from approximately $2.2 billion in calendar year 1998 to $12.1 billion in calendar year 2009 (Centers for Medicare & Medicaid Services, 2011).
The majority of beneficiaries electing the hospice benefit in its early years were those with terminal cancer diagnoses. Indeed, the payment system was based upon a demonstration where the majority of patients had a cancer diagnosis. Over time, the mix of beneficiaries electing hospice has shifted significantly; the proportion of users with non-cancer diagnoses has grown steadily (Centers for Medicare & Medicaid Services, 2011; Iglehart, 2009; Stevenson, 2012). These non-cancer diagnoses have been associated with increasingly longer periods of hospice care. Hospice enrollment decisions are likely influenced by a number of factors, including physician treatment preferences, patient and family preferences, and available information. The decision to elect hospice poses unique sensitivities for the patient and family.
Given the shift in mix of hospice users and growth in spending over time, there has been interest in further examination of resource use. The resource use profile for many patients has been referred to as a U shaped curve—most intensive at the beginning and end of a hospice episode with lower, steady resource use during the middle of the episode (MedPAC, 2009, 2012, 2013; Nicosia, Reardon, Lorenz, Lynn, & Buntin. 2009; Stearns, Sheingold, & Zuckerman, 2014). This relationship leads to concerns that some hospices may have incentives to select long stay patients because they may be viewed as more profitable (Nicosia et al., 2009). The prediction of the trajectory of care for a hospice patient may be considerably more variable than found in curative treatments.
The Affordable Care Act (ACA) includes provisions to modify the hospice payment system. Given the important scope of services Medicare’s hospice benefit provides for patients facing end of life care, and the unique circumstances faced by these patients and their families, it is critical that policymakers have high quality information to assess the current system and the potential impacts of any modifications. Since the previous analyses of hospice utilization were conducted, use of the benefit has increased further, and Medicare hospice claims have been modified to include greater information for examining resource use patterns during a hospice episode. This additional information includes the number and type of daily visits by specific disciplines and the time spent during each visit defined in 15 minute increments. The additional claims-based information allows for more detailed examination of the resource use associated with routine home care and other levels of hospice care for a variety of episode lengths.
In this paper, we examine hospice enrollment and utilization. In addition, we explore the magnitude of relative resource use during episodes and whether such patterns vary by episode length for patients who only use routine home care and those who use multiple levels of hospice care. In examining multiple levels of hospice care, we examine resource use for those hospice users who may receive any routine home care (RHC) as compared to those who solely receive RHC. Examining resource use for hospice users who require different hospice levels of care within an episode versus solely RHC provides insight to the varying resource use associated with the different patient populations (i.e., those who may require steady RHC across the entire episode versus those whose require varied levels of care across the episode).
For purposes of examining relative resource use, we restricted the sample to hospice users with one episode of hospice ending in death or single episode decedents. This approach allows us to explore the unique resource intensity for those patients whose episodes end in death. This paper does not focus on the resource use associated with hospice users who experience improvement or other confounding factors that may result in a live discharge from the Medicare hospice benefit.
Background
When a Medicare beneficiary elects the hospice benefit they waive coverage of curative treatment for the terminal illness. During a hospice election, Medicare will pay for (1) covered hospice services provided by a participating hospice and (2) other Medicare covered services unrelated to the terminal illness. There are four levels of hospice care, each with a prospective per diem rate. The most common level of care provided is RHC, which is provided on a typical day. Second, continuous home care (CHC) is provided during a crisis. Third, inpatient respite care (IRC) provides a respite or break for the family or caregiver for a hospice patient at home. Fourth, general inpatient care (GIC) may be provided for a condition that cannot be treated in another setting. Payment per day for hospice services is constant, regardless of service use or the rendering of a visit on any day during hospice election, for three levels of hospice care: RHC, IRC, and GIC. CHC is paid on a per diem basis, but varies based on the hours of service provided. Medicare hospices are paid a per diem rate, wage adjusted for the location of the patient, for each of these levels.
The 2013 hospice per diem payment rates before wage adjustment are (Centers for Medicare & Medicaid Services, 2012)1
RHC $153.45;
CHC $895.56 full per diem rate for 24 hours, billed hourly at $37.32/hour;
IRC $158.72; and
GIC $682.59.
Data and Methods
The Office of the Assistant Secretary for Planning and Evaluation (ASPE) and Acumen LLC created an episode database of Medicare hospice users to analyze hospice enrollment and utilization. The analyses were based on a longitudinal analytic file that was constructed from 100% of Medicare claims for hospice users with completed episodes spanning September 1, 2008 through the end of calendar year 2011. The claims were arrayed into episodes with the start of the episode being the date of hospice election and the end being the date of death or live discharge. Hospice users who are discharged alive and subsequently elect hospice are referred to as multi-episode users. The database included 3,008,137 beneficiaries and 3,232,580 episodes.
For examining resource use, we restricted the analyses to single episode decedents who began their hospice episode on or after April 1, 2010 and whose date of death was on or before December 31, 2011. Limiting the analyses to decedents allows us to explore the unique resource intensity for patients who represent the vast majority of hospice users. This time period was chosen because CMS required daily visit reporting by discipline in 15 minute time increments for RHC, CHC, and IRC in calendar year 2010. The first quarter of calendar year 2010 visit data reported to CMS was excluded from this analysis due to concerns with the quality of the data. Several aspects of resource use were examined including the number of visits by each discipline (e.g., skilled nursing, home health aide, social services, and therapy services) and the number of visit units (i.e., 15 minute increments of time spent during a visit). Visit data per day is available for RHC, CHC, and IRC, but not for GIC data, which are only reported on a weekly basis per the hospice billing instructions. One limitation of the analysis is the inability to include GIC visit information allocated to a specific day within an episode of care due to the weekly reporting requirements. Another limitation is the potential underrepresentation of long stay users due to the analytic timeframe. Specifically, long episodes that are completed after the end of the study period are not included, so long stays are underrepresented.
In order to simplify the analyses, we developed a single measure of resource use that combines all of these dimensions. Specifically, we calculated daily wage-weighted visit units (WWVUs) for each patient during their hospice stay. The 2009 Bureau of Labor Statistics (BLS) hourly wage data were used in the calculation of WWVUs. In order to compute a WWVU, one-fourth of the 2009 BLS hourly wage rate for each visit discipline (i.e., skilled nursing, medical social services, home health aide, and an average for therapies) was multiplied by the corresponding number of visit units reported on hospice claims. It is important to note that while WWVU represents a single value resource measure, it is not intended to measure the full costs, or even the full labor costs, of providing hospice care.
As described above, there is policy interest in how hospice resources, particularly visits provided on RHC days, are used over the course of a hospice episode. There is also interest in learning more about very short and very long episodes, and if any other factors effect variation in resource use. Therefore, we examine resource use for beneficiaries who received multiple levels of care in an episode and separately for those hospice users who solely receive RHC in an episode. We examined and compared these patterns for episodes of varying lengths and by selected diagnosis.
Beneficiary Characteristics
Exhibit 1 displays beneficiary characteristics and utilization for the hospice benefit. Among the highlights from the table are that RHC is the most common level of hospice care; approximately 84% of hospice users receive RHC and about 67% only receive RHC during hospice episodes. Beneficiaries with non-cancer diagnoses comprise 70% of hospice episodes. These beneficiaries tended to receive their care in a variety of settings: at home (47%), nursing facilities (NF)/skilled nursing facilities (SNF)2 (32%), or assisted living facilities (10%). In contrast, 73% of beneficiaries with cancer diagnoses received their care at home. Hospice users with non-cancer diagnoses experienced a greater proportion of long episodes and higher average total days of hospice care than beneficiaries with cancer. Despite this difference in average episode length, median days of care were similar for the two groups because a high proportion of both experienced very short episodes (1–7 days).
Exhibit 1. Hospice User Characteristics Analytical Measure.
| All Diagnoses | Cancers Diagnoses | Non-cancer Diagnoses | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of Beneficiaries | 3,008,137 | 893,957 | 2,114,180 | ||||||||||||
| Number of Episodes | 3,232,580 | 943,439 | 2,289,141 | ||||||||||||
| Demographics | |||||||||||||||
| Age (first day of election period) | |||||||||||||||
| <65 | 5% | 8% | 4% | ||||||||||||
| 65–<75 | 17% | 30% | 11% | ||||||||||||
| 75–<85 | 32% | 38% | 30% | ||||||||||||
| 85+ | 46% | 25% | 55% | ||||||||||||
| Gender | |||||||||||||||
| Male | 42% | 50% | 38% | ||||||||||||
| Female | 58% | 50% | 62% | ||||||||||||
| All cancers | 30% | 100% | 0% | ||||||||||||
| All non-cancers | 70% | 0% | 100% | ||||||||||||
| Hospice Level of Care (LOC) | |||||||||||||||
| Receive any care (not mutually exclusive) | |||||||||||||||
| Any RHC | 84% | 86% | 83% | ||||||||||||
| Any CHC | 6% | 7% | 6% | ||||||||||||
| Any GIC | 26% | 27% | 26% | ||||||||||||
| Any IRC | 3% | 3% | 3% | ||||||||||||
| LOC combinations (mutually exclusive) | |||||||||||||||
| RHC only | 67% | 66% | 67% | ||||||||||||
| GIC only | 16% | 13% | 17% | ||||||||||||
| RHC/CHC | 5% | 5% | 5% | ||||||||||||
| RHC/GIC | 9% | 12% | 8% | ||||||||||||
| Other | 4% | 4% | 4% | ||||||||||||
| Hospice Site of Service | |||||||||||||||
| Sites of service (not mutually exclusive) | |||||||||||||||
| Patient home | 55% | 73% | 47% | ||||||||||||
| Assisted living facility | 8% | 4% | 10% | ||||||||||||
| Nursing facility/SNF | 27% | 14% | 32% | ||||||||||||
| Inpatient hospital | 11% | 11% | 12% | ||||||||||||
| Inpatient hospice facility | 16% | 18% | 15% | ||||||||||||
| Other sites | 2% | 2% | 2% | ||||||||||||
| Number of days per beneficiary (summary statistics) | |||||||||||||||
| Average number of total days | 83 | 53 | 96 | ||||||||||||
| Median number of total days | 19 | 18 | 19 | ||||||||||||
| Number of days per beneficiary (categories) | |||||||||||||||
| 1–3 days | 16% | 13% | 17% | ||||||||||||
| 4–7 days | 16% | 15% | 16% | ||||||||||||
| 8–10 days | 7% | 8% | 7% | ||||||||||||
| 11–14 days | 7% | 8% | 6% | ||||||||||||
| 15–30 days | 14% | 18% | 12% | ||||||||||||
| 31–60 days | 11% | 15% | 10% | ||||||||||||
| 61–90 days | 7% | 7% | 6% | ||||||||||||
| 91–180 days | 10% | 9% | 10% | ||||||||||||
| 181+ days | 13% | 7% | 16% | ||||||||||||
| Hospice Discharge Status | |||||||||||||||
| Died in hospice | 83% | 89% | 81% | ||||||||||||
| Still in hospice | 8% | 5% | 9% | ||||||||||||
| Discharged from hospice | |||||||||||||||
| Died after discharge | 5% | 5% | 6% | ||||||||||||
| Average number of days until death | 136 | 54 | 165 | ||||||||||||
| Alive after discharge | 3% | 1% | 4% | ||||||||||||
SOURCE: 100% of Medicare claims for hospice users with completed episodes spanning September 1, 2008 through the end of calendar year 2011.
Service Use over the Hospice Episode
In the following sections, we examine variation in intensity of service use (WWVUs) during hospice episodes of selected lengths for single episode decedents: 1–7 days, 15–30 days, and 91–180 days. While the focus of previous work has been RHC, we also display resource patterns during episodes of different lengths, which allow examination of the mix of all hospice care levels as well as intensity. As stated above, the WWVU is a resource measure intended as a common metric for combining several aspects of visit intensity. This measure is not intended to represent the full labor or non-labor costs of hospice care that is in any way comparable to payments for assessing overall profitability.
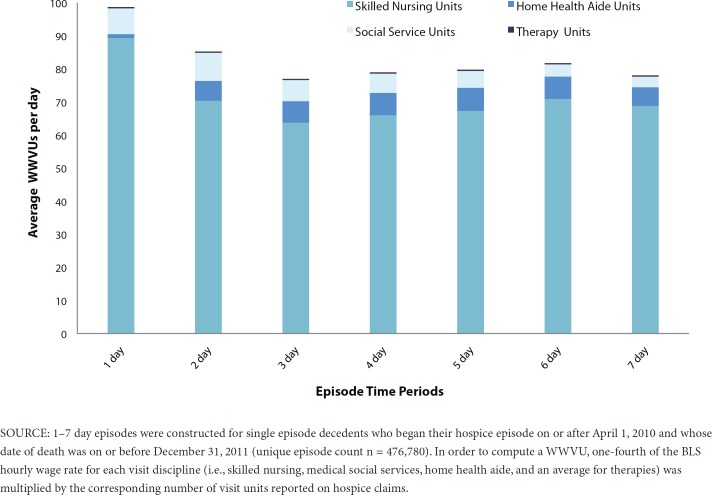
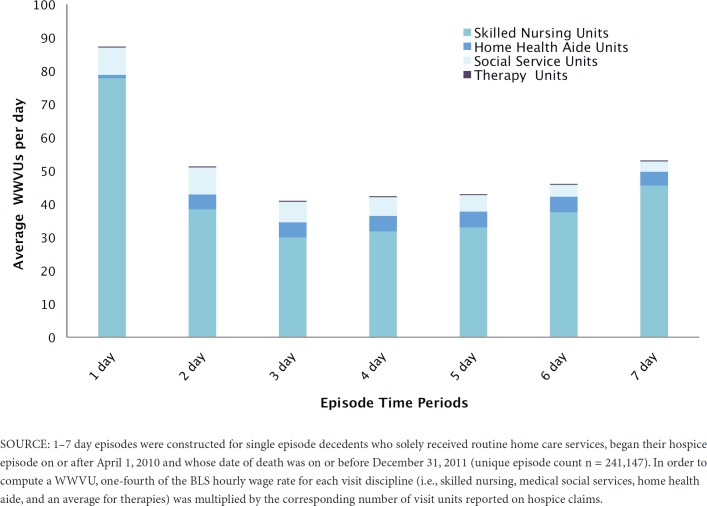
Hospice Episodes 1–7 Days
Exhibit 2a displays WWVUs per day for 1–7 day episodes (unique episode count n = 476,780). The left y-axis or bar height shows the average total WWVUs each day as reported for RHC, CHC, and IRC levels of care. Exhibit 2b (unique episode count n = 241,147) displays short episodes for patients who only used RHC. In general, total WWVUs are comparable each day except for the first day, which is somewhat more resource intensive. Many factors may contribute to the intensity of service provided to patients who enter hospice within a short period of time before death (i.e., within 7 days or less).
Exhibit 2a. Average Total WWVUs Per Day (Single-Episode Decedents, 1–7 Day Episodes).
Exhibit 2b. Average Total WWVUs Per Day Routine Home Care Only (Single-Episode Decedents, 1–7 Day Episodes).
The composition of services by discipline (represented by the shaded areas within a bar) does not vary significantly during these short stays. Skilled nursing services account for the largest proportion each day due to higher skilled need associated with shorter stay hospice patients, higher hourly wages associated with skilled nursing care, and more time spent during skilled nursing visits per the 15 minute visit unit increments reported on hospice claims. For patients receiving multiple levels of care, home health aide services account for a slightly larger proportion of WWVUs during days 2–7, ranging from 7–9% as compared to 1% on day 1.
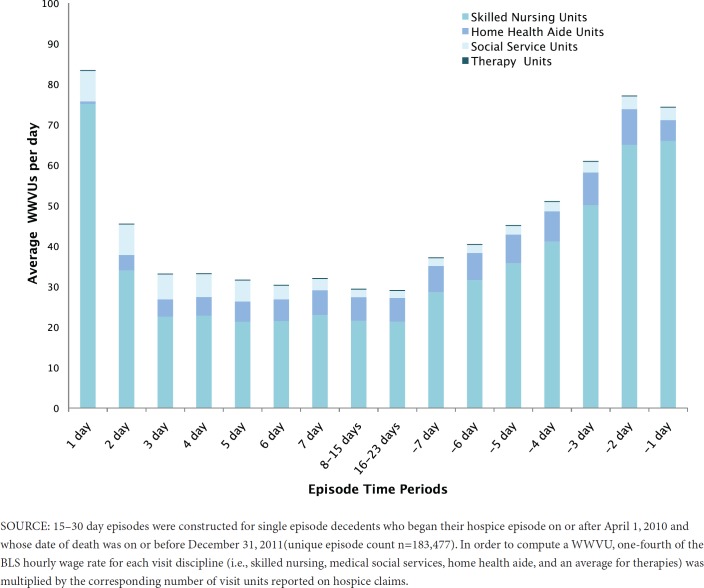
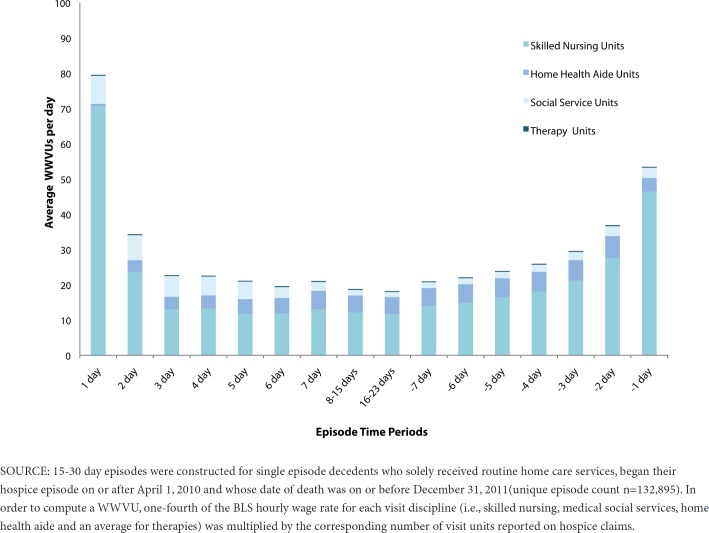
Hospice Episodes 15–30 Days
Exhibit 3a displays average WWVUs per day for 15–30 day episodes (unique episode count n=183,477). On this graph, the days with minus signs indicate the number of days prior to death (e.g., –7 is seven days prior to death). The curved pattern is more pronounced for this episode length than for the shorter episode, both when all visit types are considered and when only RHC visits are considered (Exhibit 3b). That is, fewer resources are used during middle portions of the episode than at entrance to hospice care and just prior to death.
Exhibit 3a. Average Total WWVUs Per Day (Single-Episode Decedents, 15–30 Day Episodes).
Exhibit 3b. Average Total WWVUs Per Day. Routine Home Care Only (Single-Episode Decedents, 15–30 Day Episodes.
In Exhibit 3a, the composition of the bar heights illustrates a higher proportion of skilled nursing visits as opposed to home health aides at the beginning and end of these episodes. The WWVUs in the middle portion of the 15–30 day episodes reflect a higher proportion of home health aide services. On day 1, skilled nursing services comprise 90% of average WWVUs per day as compared to about 1% for home health aide services. On days 8–15, the skilled nursing services decrease to about 73% of average WWVUs per day and home health aide services increase to approximately 20%. On the last day of the episode, the skilled nursing services reflect 89% of average WWVUs and the home health services component decreases to 7%.
In Exhibit 3b, we observe similar shifts in the proportion of service mix associated with the WWVUs for RHC only episodes (unique episode count n=132,895). On day 1, skilled nursing services reflect 89% of WWVUs as compared to 1% for home health services. On days 8–15, skilled nursing services decrease to 64% of WWVUs and home health aide services increase to about 26% of WWVUs. On the last day of the episode, the skilled nursing services component increases to 87% of WWVUs as home health aide services decrease to 7%.
Hospice Episodes 91–180 Days
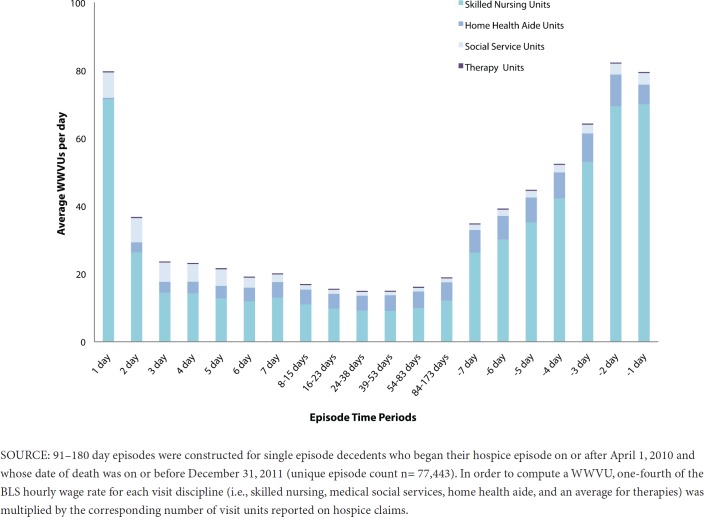
Exhibit 4a illustrates WWVUs per day for 91–180 day episodes (unique episode count n= 77,443). When all hospice services are considered, the U shape is apparent, with service use again beginning a steep increase about 7 days prior to death. The pattern is again similar when only RHC patients are considered in Exhibit 4b (unique episode count n=55,692).
Exhibit 4a. Average Total WWVUs Per Day (Single-Episode Decedents, 91–180 Day Episodes).
Exhibit 4b. Average Total WWVUs Per Day. Routine Home Care Only (Single-Episode Decedents, 91–180 Day Episodes).
The decomposed bar heights on both Figures display an increasing proportion of home health aide services in the middle portion of the episodes, relative to skilled nursing services that are more heavily used at the beginning and end of episodes. In Exhibit 4a, skilled nursing services reflect 90% of WWVUs as compared to 1% for home health services on day 1. On days 84–173 during the middle section of the episode, the skilled nursing proportion of WWVUs decreases to 64% as the home health service proportion increases to 29%. On the last day of the episode, the skilled nursing proportion increases to 88% as the home health services proportion decreases to 7%. For these RHC only episodes in Exhibit 4b, we observe a similar curve with a slightly more pronounced shift toward home health aide services during the middle days.
Exhibit 5 summarizes the above Figures by comparing WWVUs on the first, second and last day to a middle day for the various episode lengths. For WWVUs for three service levels (RHC, CHC, and IRC) and those related to RHC only, the ratio of beginning and ending days to middle days increases as the episodes get longer. For episodes of 91–180 days, RHC WWVUs for the last and first days are 4.23–6.00 times greater than the middle day as compared with 1.29–2.12 times greater for the shorter episode. On closer examination, the WWVUs for the beginning and end of the stay do not vary considerably; the major differences in these ratios appear to be due to the declining resources used in the middle days as episodes get longer.
Exhibit 5. Relative Values of Resource Use Across Episode Time Periods.
| Episode 1–7 Days | Episode 15–30 | Episode 91–180 | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| First Day | Second Day | Last Day | First Day | Second Day | Last Day (–1) | First Day | Second Day | Last Day (–1) | |||||||||||
| WWVU/Middle | 1.29 | 1.10 | 1.01 | 2.80 | 1.53 | 2.47 | 5.33 | 2.47 | 5.33 | ||||||||||
| WWVU RHC Only/Middle | 2.12 | 1.24 | 1.29 | 4.21 | 1.79 | 2.84 | 6.00 | 2.31 | 4.23 | ||||||||||
NOTES: For episodes 1–7 days, this analysis assumes day 7 is the last day of the episode.
For episodes 1–7 days, day 3 is the middle time period value.
For episodes 15–30 days, 8–15 days is the middle time period value.
For episodes 91–180 days, 39–53 days is the middle time period value.
SOURCE: Single episode decedent episodes were defined as 1–7 days (i.e., assuming a 7 day episode for this analysis), 15–30 days, and 91–180 days for users with multiple hospice services and solely routine home care services during each respective episode definition. The WWVU total for the first, second, and last day was divided by the WWVU total for a chosen middle day of each episode definition to explore the relative value of resource use across episodes of various lengths.
All Episodes - Cancer and Alzheimer’s/Non-Alzheimer’s Dementia
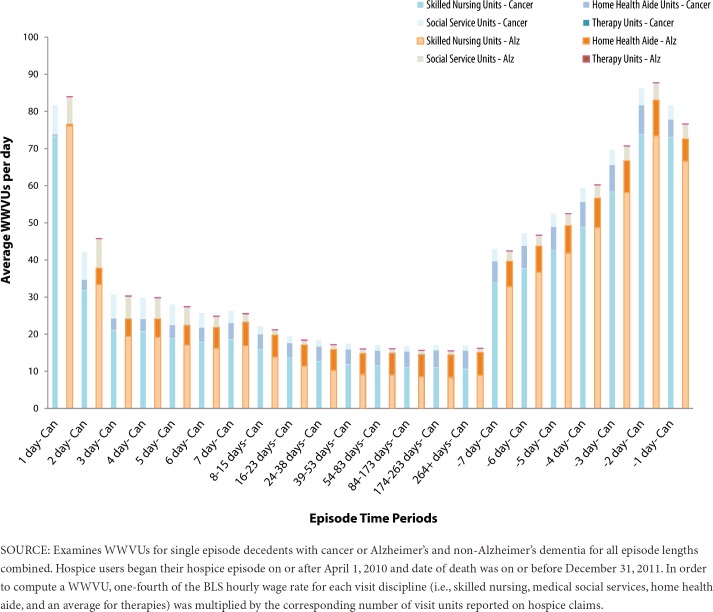
Another important question is whether the observed utilization patterns would differ by patient characteristics. Exhibit 6 compares WWVUs for hospice users with cancer and users with combined Alzheimer’s and non-Alzheimer’s dementia. The height of the first bar corresponds to average total WWVUs per day for users with cancer (e.g., day 1 Can). On day 1, the height of the second bar without a label on the x-axis corresponds to total average WWVUs per day for Alzheimer’s and non-Alzheimer’s dementia diagnoses combined. The days further to the right represent the last seven days of an episode, regardless of its overall length for episodes ending in death. The patterns of WWVUs per day are very similar for the cancer and Alzheimer’s patients. It does appear, however, that particularly for middle days, cancer patients use a higher proportion of skilled nursing services (relative to home health aides) than do Alzheimer’s patients.
Exhibit 6. Average Total WWVUs Per Day (Single-Episode Decedents, Cancer or Alzheimer’s/Non-Alzheimer’s Dementia Diagnosis).
Conclusion
For a number of reasons, there has been growing interest in evaluating Medicare’s current hospice benefit. Among the concerns is whether current payment methods are an appropriate match for patterns of resource use during a hospice episode; in particular, whether they create any financial incentives that may result in less than optimal use of the benefit. In this paper, we have used more recent data that contain improved resource intensity measures and developed service use profiles over various episode lengths. These analyses confirm the earlier findings concerning the curved pattern of resource use and demonstrate that the curve becomes more pronounced as episode lengths increase for hospice users. This effect occurs because resource use declines more substantially for the middle days relative to beginning and ending days in longer episodes of hospice care than it does for shorter episodes. This decline is deeper for those users who only receive RHC during their hospice episode.
This analysis cannot and should not be used to assess financial margins for hospice providers. It does suggest hospices with a larger proportion of long-stay patients who solely use RHC may have the ability to average the higher resource use needs at uptake and at the end of the episode due to a greater number of days with lower resource use at the steady per-diem rate in a longer middle period of the episode.
Section 3132 of the ACA contains provisions for hospice payment reform. Based on the analyses to date, MedPAC recommended modifying the current flat per diem payment system by weighting payments to be higher at the beginning and ending of a hospice episode (MedPAC 2009, 2012). In using these types of analyses for future deliberations, policy makers would also likely consider a number of other factors, such as incentives and disincentives of various approaches and how they may impact on high quality hospice care. Thus, the results presented here may also support a variety of other payment methods that may be considered.
Disclaimer
The authors have been requested to report any funding sources and other affiliations that may represent a conflict of interest. The authors reported that there are no conflict of interest sources. The programming and analytic support for the data brief was provided to ASPE under contract with Acumen LLC (HHSP23320095602W, HHSP23337002T).
Acknowledgment
The authors would like to acknowledge Kyle Price, Acumen LLC, Jesselyn Friley, Acumen LLC, Daniel Rogers, Acumen LLC, Martha Kelly, Acumen LLC, Alshadye Yemane (formerly ASPE), and the Centers for Medicare & Medicaid Services for their contributions to the manuscript.
Footnotes
Per diem rates are divided into labor and non-labor portions. Labor portion updated by applicable wage index.
NF and SNF sites of service were combined in the analysis due to limitations in decomposing the sites of service on the claims.
References
- Centers for Medicare & Medicaid Services. Medicare Hospice Data Trends 1998–2009. 2011 Retrieved from http://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/Hospice/Medicare_Hospice_Data.html. [PubMed]
- Centers for Medicare & Medicaid Services. Medicare Learning Network Matters Update to the Hospice Payment Rates, Hospice Cap, Wage Index, and the Hospice Pricer for FY 2013. 2012 Retrieved from http://www.cms.gov/Outreach-and-Education/Medicare-Learning-Network-MLN/MLNMattersArticles/downloads/MM7857.pdf.
- Iglehart JK. A New Era of For-Profit Hospice Care—the Medicare Benefit. The New England Journal of Medicine. 2009;360:2701–2703. doi: 10.1056/NEJMp0902437. [DOI] [PubMed] [Google Scholar]
- MedPAC (Medicare Payment Advisory Commission) Report to Congress: Medicare payment policy. Washington, DC: MedPAC; 2009. [Google Scholar]
- MedPAC (Medicare Payment Advisory Commission) Report to Congress: Medicare payment policy. Washington, DC: MedPAC; 2012. [Google Scholar]
- MedPAC (Medicare Payment Advisory Commission) Report to Congress: Medicare payment policy. Washington, DC: MedPAC; 2013. [Google Scholar]
- Nicosia N, Reardon E, Lorenz K, Lynn J, Buntin M. The Medicare Hospice Payment System: A Consideration of Potential Refinements. Health Care Financing Review. 2009;30(4):47–59. [PMC free article] [PubMed] [Google Scholar]
- Stearns SC, Sheingold S, Zuckerman RB. Explaining Variation in Hospice Visit Intensity for Routine Home Care. Medical Care. 2014;52(1):56–62. doi: 10.1097/MLR.0000000000000009. [DOI] [PubMed] [Google Scholar]
- Stevenson DG. Growing Pains for the Medicare Hospice Benefit. The New England Journal of Medicine. 2012;367:1683–1685. doi: 10.1056/NEJMp1208465. [DOI] [PubMed] [Google Scholar]