Abstract
CTSAs are mandated to follow a multidisciplinary model. Requests for applications direct responsive applications to “integrate clinical and translational science across multiple departments, schools,” listing disciplines in addition to medicine such as engineering, nursing, and public health. This inventory of nurse engagement in CTSAs describes the extent of nursing's CTSA engagement from the perspective of participating nurse scientists within individual CTSAs, including institutional/national contributions and best practices that foster a multidisciplinary model. Of the 50 CTSAs affiliated with a nursing school, 44 responded (88% response rate). Of the ten CTSAs not affiliated with a nursing school, four responded (40% response rate). Overall funding success rates of nurse applicants are: TL1 fellowships 81%, KL2 fellowships 54%, and nurse‐led pilots 58%. At most CTSAs nursing is contributing to the accomplishment of the CTSA mandate. The strongest categories of contribution are community engagement, implementation science, and training. Best practices to enhance multidisciplinary collaboration are: (1) inclusion of multiple disciplines on key committees who meet regularly to guide individual core and overall CTSA strategic planning and implementation; (2) required multidisciplinary co‐mentors (ideally from different schools within the CTSA) on training grants and as co‐investigators on pilot projects; and (3) documentation of multidisciplinary activity in annual reports.
Keywords: multidisciplinary, nurse, engagement
Introduction
Clinical and Translational Science Awards (CTSAs) are mandated to follow a multidisciplinary model. At the inception of the CTSA initiative, Elias Zerhouni called for “new ways of combining skills and disciplines” to address complex “factors such as genetics, diet, infectious agents, environment, behavior, and social structures.”1 Francis Collins continues to affirm multidisciplinarity encouraging “a new spirit of cooperation.”2 The multidisciplinary requirement appeared in the initial CTSA request for applications (NIH RFA‐RM‐07‐002) and persisted through the November 16, 2010 RFA (NIH RFA‐RM‐10‐020) that funded the final five CTSAs. Each RFA (Part II, Section 1) directs that responsive applications will “integrate clinical and translational science across multiple departments, schools, clinical research institutes, and hospitals.” Perhaps in an attempt to temper the strong presence of biomedicine in the NIH arena, the RFAs list additional disciplines such as engineering, nursing, public health. Fifty of the existing 60 CTSAs are affiliated with a school of nursing. The aim of this inventory was to describe the extent of nursing's activity within the CTSA initiative from the perspective of participating nurse scientists up to September 19, 2011 and identify best practices that foster the recommended multidisciplinary model. The inventory extends results of a survey of nursing's experience in the initial cohort of 12 CTSAs.3
Methods
The Nursing Engagement in CTSAs inventory was developed by the authors each of whom has had continuous CTSA experience since 2006. It was distributed electronically to members of the Nurse Scientist Special Interest Group (NS‐SIG) on January 28, 2011. NS‐SIG members include nurse scientist faculty of CTSAs affiliated with a nursing school and nurse scientists at CTSAs not affiliated with a school of nursing. On August 17, 2011 invitations were extended to nurse scientists at the schools of nursing affiliated with the five newly funded CTSAs.
A single individual was identified as a respondent for each CTSA. Those not completing the initial inventory were recontacted with an offer of assistance with completion, if needed. The final inventory deadline was September 19, 2011.
The inventory elicited quantitative descriptions of nurse scientist experience at respective CTSAs and within the national CTSA consortium with the following:
Please indicate leadership positions nursing faculty or nurse scientist leaders hold in the CTSA at your institution.
Please indicate supporting activity by nursing faculty or nurse scientist leaders at your institution.
Please indicate leadership positions nurse scientists at your institution hold in national CTSA activities.
CTSA support for faculty development, student training, and nurse‐led pilot grants was elicited using the following items in separate queries for each support mechanism:
Over the life of your CTSA, how many nursing faculty or nurse scientist leaders at your institution have applied for (KL2/TL1/pilot grant) awards?
Of these, how many were funded? That is, total current and previous (KL2/TL1/pilot awards).
Does your CTSA have designated slots for (nurse faculty/students/nurse‐led pilot) support?
The inventory elicited qualitative data with the following:
Please list the TITLES or focus of successful (KL2/TL1/pilot awards).
Please list the three most important contributions nurse scientists are making to your CTSA.
Please indicate specific structures or processes in your CTSA that enhance work across schools/disciplines.
Have there been tangible outcomes due to interdisciplinary CTSA cooperation at your institution?
Quantitative data were analyzed using Qualtrics software.4 Content analysis was used to summarize qualitative data. Some analyses, e.g., development fellowships, where nonfaculty nurses would not be eligible, used only data from CTSAs affiliated with nursing schools. For the description of nurse leadership/support positions, contributions made, and best practices that were enhancing multidisciplinary collaboration, the full dataset was used.
Response rate
All 60 CTSAs received at least two invitations to complete the inventory. Of the 50 CTSAs affiliated with a nursing school, 44 responded (88% response rate). Of the 10 CTSAs not affiliated with a nursing school, four responded (40% response rate).
Level of respondent engagement in CTSA
A total of 48 individuals representing CTSAs affiliated with a school of nursing (44) and CTSAs not affiliated with a school of nursing (4) responded. Of these 48 respondents, 43 (90%) were engaged with their institutional CTSA at the level of Core Co‐Director or higher, with many serving on CTSA steering and executive committees. The remaining five of the 48 respondents (10%) served at the CTSA committee member level.
Results
CTSA training and career development fellowships
Research training and faculty development have been a focus of the CTSA program from the outset. The CTSA RFA (RFA‐RM‐06–002) stated:
Applicants are encouraged to include novel methods and approaches for providing an integrated and flexible research education, predoctoral training, and career development environment that is broad enough in scope to train those interested in careers in multidisciplinary team‐based clinical and translational science, and for the development and improvement of new research methodologies that advance the discipline.
Predoctoral research training that focuses on translational science is provided through TL1 support, and research development for faculty through the KL2 component. Although specific structure and content of the TL1 and KL2 programs vary across universities, these programs typically combine formal coursework, mentored research experiences, and opportunities to interact with interdisciplinary colleagues. The goal is to develop and support scientists in the conduct of team science who will become leaders in clinical and translational research.
Nursing students and faculty have been active participants in the TL1 and KL2 programs. Of the 42 respondents reporting the number of nursing students applying for a TL1 award, 14 (33%) indicated that one or more of their students had applied since the beginning of their university's program. Across these 14 schools, there had been a total of 47 TL1 applicants, with most schools reporting four or fewer applicants. At 13 of these 14 schools (93%) one or more applicants had been awarded a TL1. The number of TL1 awardees varied from 1 to 10 across these 13 schools, with most reporting one to two awardees. The total number of TL1 awardees was 38 for an overall success rate of 81% (38/47).
There was greater nursing participation in the KL2 programs. Of the 43 respondents providing data on the number of faculty applying for a KL2 over the course of their university's CTSA, 27 (63%) reported one or more submissions. Across these 27 schools, the total number of submissions was 75. Submissions ranged from 1 to 10, with most schools (60%) reporting four or fewer total submissions. Faculty at 18 of these 27 schools (68%) had received a total of 41 KL2 awards, for an overall success rate of 54% (41/75). Across schools, the number of awards received ranged from one to six, with nine schools reporting receipt of multiple KL2 awards.
Having a guaranteed slot for nursing was relatively unusual. Five schools (11%) reported a guaranteed slot in the TL1 program and only one school reported a guaranteed slot in the KL2 program. At nine schools, applicants had successfully competed for both funding mechanisms. There was some evidence that success in obtaining a TL1 or KL2 was linked to year of CTSA funding. All of the schools with successful TL1 applicants were at universities whose CTSA had been funded in 2006 or 2007, and only one school reported TL1 applicants after 2007. Though somewhat less striking, the same pattern was evident for KL2 submissions and funding. Fifty‐two of the 75 KL2 submissions (60%) came from schools of nursing at universities awarded a CTSA in 2006 or 2007. Twelve of the 18 schools (67%) with successful KL2 applicants were at universities awarded a CTSA during these first 2 years of funding. In comparison, there were only 19 submissions from faculty at universities funded during 2008 or 2009.
Studies supported by a TL1 or a KL2 included diverse research topics (e.g., palliative care, obesity prevention, postoperative infection) and populations (e.g., older adults, adolescents, neonates). As a group, the topics reflected the National Institute of Nursing Research emphasis on health promotion, symptom management, quality of life, and palliative and end of life care.5 Investigators also were addressing the innovative use of technology to enhance health care.
CTSA support of nurse‐led research projects
The CTSAs have consistently supported internal pilot research. Of the 48 CTSAs responding, 46 reported that nurse scientists had submitted pilot proposals. A total of 227 proposals had been submitted. On average 4.9 proposals were submitted per CTSA, with considerable variation between CTSAs ranging from 1 to 12. Sixteen reported submitting fewer than four applications. Another 16 submitted four to six.
Success rates for nurse‐led pilot research applications overall was good. Fifty‐eight percent (132/227) of the projects were funded. Success rates varied considerably across institutions, ranging from a 17% success rate (two out of 12 funded) to 100% (12 out of 12 funded). One hundred percent success rates were most commonly seen in CTSAs with just one or two total submissions. Only one CTSA had set aside pilot monies targeted for nursing.
Nurse‐led research projects covered a variety of subjects ranging from metabalomics to clinical interventions to community‐based participatory research. Core support services used primarily focused on methodological development. The research development core was utilized most frequently closely followed by consultation and data management cores (24, 23, and 21 CTSAs, respectively). Less frequently used were the biobank (8), community (4), statistics (4), recruitment (2), education (1), laboratory support (1), and writing/review/IRB (1) cores.
Contributions of nurse‐scientists to the accomplishment of CTSA goals
Many CTSAs have chosen a multiple leadership plan, recognized as Multiple Principal Investigator by NIH. At the local level (see Figure 1) nurses are making key contributions as Multiple Principal Investigator (1), Co‐Principle Investigator (4), Co‐Investigator (Director of a key function or core) (35) or members of their local Executive or Steering Committees (58). Examples provided under “other local CTSA leadership activities” on Figure 1 included leadership in ethics, informatics, mentorship.
Figure 1.
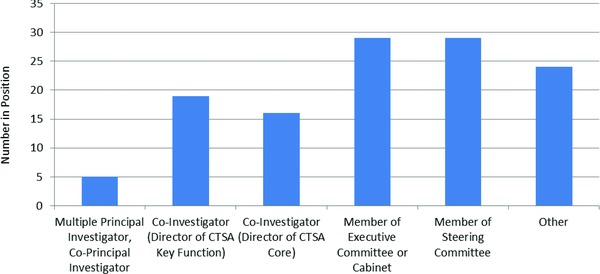
Local CTSA leadership positions held by nurse faculty or nurse scientist leaders.
Nurse scientists are providing considerable supporting activity at the local level. As seen in Figure 2, they are reviewing training grants and pilot applications (n = 66), members of a core (n = 33), mentors or co‐mentors of a trainee (n = 50), and serving as members of a committee or taskforce (n = 41). Of the 50 nurse scientists who were mentoring or co‐mentoring trainees 31 were mentoring a nonnurse trainee. Examples listed under “other supporting activity” included Principle Investigator of a nurse‐led pilot, course director, and member of Council of Mentors.
Figure 2.
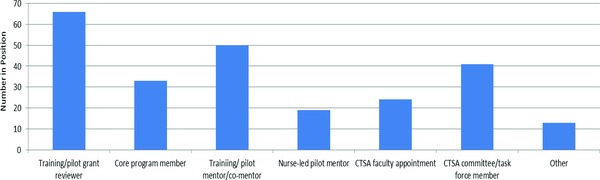
Local CTSA supporting activity provided by nurse faculty or nurse scientist leaders.
The CTSA consortium has numerous national committees that work together to share resources and projects to speed the translation of research discovery into improved patient care. Nurses are involved and are leading activities at the national level. As depicted in Figure 3, seven nurse scientists are members of the CTSA National Steering Committee. This committee meets monthly to discuss issues such as consortium projects, papers, and collaborative studies. Ten nurse scientists are members of mock review committees for other CTSAs preparing for competing renewal or are consultants to other CTSAs, e.g., member of an External Advisory Committee. Nineteen nurse scientists are leading or are members of national committees. “Other national activity” examples included serving on scientific review panel for CTSA competing continuation and on planning committee for national CTSA symposia.
Figure 3.
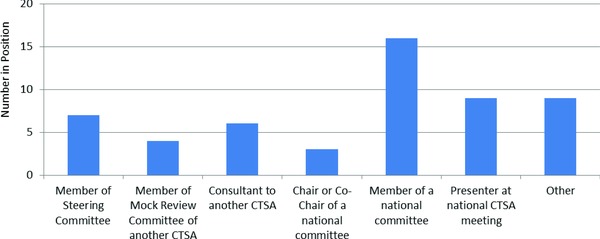
National CTSA leadership positions held by nurses.
Nursing contributions to CTSAs
The most frequently reported nursing contribution was expertise developing productive community collaborations, specifically Community‐Based Participatory Research skills and community‐based models of care. Of the 48 total respondents, 22 identified community partnership development expertise. The second most frequently reported contribution was Implementation/Translational Science expertise (16/48). This expertise was linked to strengthening CTSA commitment to T3 and T4 research, developing point of care research, and helping bench scientists better conceptualize application of their science. Expertise listed with less frequency (one to five mentions) included behavioral science, biobanking, ethics, and informatics.
Additionally, nurses identified service skills that contributed to the broad aims of the CTSA charge. Most frequently listed were contributions to training the next generation of clinical researchers. Of the 44 respondents within CTSAs that include a school of nursing, 19 listed mentoring as an important nursing contribution. Training and pilot proposal review was identified by 19 of 48 respondents. Less frequently listed (one to two mentions) were serving as evaluator for CTSA key functions and expanding appreciation of the contributions of nonmedical clinical scientists to the CTSA mission.
Best practices that promote multidisciplinary collaboration
The most frequently cited practice was the establishment and regular meeting of committees that included representatives from a wide array of health science disciplines (25/48), including regular multidisciplinary meetings reported at the highest levels of CTSA leadership. Multidisciplinary collaboration also occurred at regular core leadership meetings and on pilot and training review panels. Some CTSAs dedicate time to multidisciplinary collaboration at annual CTSA‐wide or key function retreats.
The second best practice identified as advancing multidisciplinary collaboration was pilot application criteria that required or favored multidisciplinary co‐investigators. Twenty‐two of the 48 respondents identified this mechanism, although the definition of discipline difference varied, with some accepting co‐investigators from different departments within the same school, e.g., internal medicine and oncology, while others required co‐investigators from different schools, e.g., engineering and nursing, arguably most consistent with the desired multidisciplinary model. Similar to the practice of requiring multidisciplinary co‐investigators were CTSAs that required co‐mentors from different disciplines on training applications for KL2 or TL1 support (8/48).
Less frequently listed (one to three mentions) were open access to CTSA resources across disciplines via central application and review, multidisciplinary shared databases, documentation of the extent of multidisciplinary collaboration, and multidisciplinary representation on search committees. Four respondents indicated that no structures were in place to enhance work across disciplines. Those CTSAs appeared to be more medically focused with limited inclusion of nursing.
Tangible outcomes attributed to multidisciplinary CTSA activity
The most frequently cited outcome attributed to multidisciplinary CTSA activity was increase (or establishment) of joint faculty appointments (14/48). Increased joint appointments were attributed to the development of applications for external funding and joint publications.
Eight of the 48 respondents reported that shared space (or plans under development) was a tangible outcome. Individual citations identified outcomes well aligned with the CTSA multidisciplinary model, including cross‐listed, co‐taught courses on team research, the development of a university‐wide mentoring analysis and plan, CTSA‐sponsored invited speakers and visiting faculty who represent a variety of disciplines, and progress toward a single interinstitutional IRB.
Discussion
Nursing PhD students and faculty are participating in CTSA research training and development programs competing successfully for both mechanisms. Guaranteed slots for nurse applicants are rare. There is considerable evidence that competing is worth the effort. In those schools where nurses have submitted TL1 or KL2 applications, the success rate is high (81% for TL1 and 54% for KL2).
A substantial proportion of the TL1 and KL2 funding has gone to students/faculty at universities whose CTSA was funded during 2006 or 2007. We did not have data on when in the life of the university's CTSA these awards were funded, but there is evidence that submissions dropped off in subsequent years. Given the high success rates, the drop‐off in submissions is perplexing.
Nurse‐led pilot studies have reasonable success in the CTSAs (58%), but submission rates are fairly low with the majority submitting four or fewer applications over CTSA lifetime. What is the reason for low submission rates? Can they be improved?
Inventory data suggest that increased involvement of nurse scientists in the CTSAs would result in increased nurse‐led research submissions.
Of note, the four respondents not citing specific multidisciplinary structures/processes within their CTSA consistently indicated that there were also no tangible outcomes to report. More recently established CTSAs were less likely to report tangible outcomes, but added such comments as, “Not (tangible outcomes) yet, but we are at the table most of the time now (as a College of Nursing) much more than in the past,” indicating a more positive climate for collaborative work going forward and setting the stage “to encourage a new spirit of cooperation” advocated by Collins.2
Limitations
Final inventory data were collected on September 19, 2011. Given the emerging, rapidly changing activities of CTSAs, particularly those more recently established, some aspects of nurse engagement are likely not captured in this report. Further, the variable longevity of CTSA existence (some established in 2011 and others having completed an initial 5‐year cycle) imposes variation on the potential for tangible outcomes.
We did not have data to calculate the total pool of nurses eligible to apply for the various funding mechanisms. Nor were we able to compare the success of nurse applicants versus the overall applicant pool in each CTSA. Future studies should collect this data.
The data represent input gathered from a single nurse scientist at each CTSA and not a compilation of data from all nurse scientists and trainees associated with each CTSA institution. Because respondents were nurse scientists, given the purpose of the inventory to describe nursing's experience in CTSAs, they reflected a nursing perspective. In future studies such data would be strengthened by CTSA Principal Investigator verification or further vetting using respective annual reports.
Conclusions
At most CTSAs nursing is contributing to the accomplishment of the CTSA's mandate. The strongest categories of contribution are in the areas of community engagement, implementation science, and training. The extent of nursing contribution is seriously limited or nonexistent when a particular CTSA fails to provide infrastructure that enhances multidisciplinary collaboration. Recommended best practices to accomplish multidisciplinary collaboration are:
Inclusion of multiple disciplines on key committees who meet regularly to guide individual core and overall CTSA strategic planning and implementation
Required multidisciplinary co‐mentors (ideally from different schools within the CTSA) on training grants and as co‐investigators on pilot projects
Documentation of multidisciplinary activity in annual reports
Acknowledgments
This project has been funded in whole or in part with Federal funds from the National Center for Research Resources and National Center for Advancing Translational Sciences (NCATS), National Institutes of Health (NIH), through the Clinical and Translational Science Awards Program (CTSA), part of the Roadmap Initiative, Re‐Engineering the Clinical Research Enterprise. The manuscript was approved by the CTSA Consortium Publications Committee.
The project described was supported by the National Center for Research Resources, Grants UL1RR024986, UL1RR025747, and UL1 RR024153 and is now at the National Center for Advancing Translational Sciences, Grants UL1TR000433, UL1TR000083, and UL1TR000005. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1. Zerhouni E. The NIH roadmap. Science. 2003; 302: 63–64, 72. [DOI] [PubMed] [Google Scholar]
- 2. Collins F. ASCB 50th anniversary essay: change, change, change: heeding the call. Mol Biol Cell. 2010; 21(22): 3793–3794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Knafl K, Grey M. Clinical Translational Science Awards: opportunities and challenges for nurse scientists. Nurs Outlook. 2008; 56: 132–137. [DOI] [PubMed] [Google Scholar]
- 4. www.Qualtrics.com 2010.
- 5. Bringing Science to Life NINR Strategic Plan‐ NIH publication #11–7783; Printed October 2011.


