Abstract
Smoking continues to take an enormous toll on society, and although most smokers would like to quit, most are unsuccessful using existing therapies. These findings call on researchers to develop and test therapies that provide higher rates of long-term smoking abstinence. We report results of a randomized controlled trial comparing a novel smoking cessation treatment using mindfulness training to a matched control based on the American Lung Association's Freedom From Smoking program. Data were collected on 175 low socioeconomic status smokers in 2011-2012 in a medium sized Midwestern city. A significant difference was not found in the primary outcome; intent-to-treat biochemically confirmed 6-month smoking abstinence rates were Mindfulness = 25.0%, Control= 17.9% (p = 0.35). Differences favoring the mindfulness condition were found on measures of urges and changes in mindfulness, perceived stress, and experiential avoidance. While no significant differences were found in quit rates, the mindfulness intervention resulted in positive outcomes.
Keywords: smoking, tobacco, mindfulness, meditation, Freedom from Smoking
1. Introduction
Mindfulness is a cognitive skill of paying attention to internal phenomena (e.g., thoughts, emotions) or external phenomena (e.g., walking, talking) in a way that is intentional rather than automatic, non-reactive rather than reactive, and accepting rather than critical (Kabat-Zinn, 1990; Kabat-Zinn, 1994; Segal et al., 2002). Studies have shown that mindfulness training is associated with decreased smoking urges (Westbrook et al., 2011), decreased stress (Grossman, Niemann, Schmidt, & Walach, 2004), increased distress tolerance (Grossman et al., 2004; Shapiro, Oman, Thoresen, Plante, & Flinders, 2008), decreased anxiety (Creswell, Way, Eisenberger, & Lieberman, 2007; Hofmann, Sawyer, Witt, & Oh, 2010; Koszycki, Benger, Shlik, & Bradwejn, 2007), decreased depression (Teasdale, Segal, & Williams, 1995), and improved emotion regulation (Deckersbach et al., 2012; Farb, Anderson, & Segal, 2012; Hill & Updegraff, 2012; Hofmann et al., 2010; Kemeny et al., 2012; Mars & Abbey, 2010).
Mindfulness training as therapy for smokers has shown some promise. A pilot study of MBSR (with modifications for smokers) yielded smoking abstinence at six weeks post-cessation of 56% (Davis, Fleming, Bonus, & Baker, 2007). A follow up study showed that mindfulness training, compared to telephonic quit line, yielded significantly higher biochemically confirmed abstinence rates at 4-weeks and 24-weeks post-quit in treatment initiators (Davis et al., in press). A study showed “urge surfing” (a mindfulness technique) led to fewer cigarettes smoked per day (Bowen & Marlatt, 2009), and another study found that ACT (including mindfulness training) led to increased rates of smoking abstinence 1-year post-quit (Gifford et al., 2011).
While the initial reports have been promising, more stringently controlled study designs are needed to better isolate the effect of mindfulness in smokers (Baardseth et al., 2013; Chiesa & Serretti, 2009; Maccoon et al., 2012; Wampold et al., 1997; Wampold, 2001). A recent study by Brewer et al. (2011a) compared mindfulness training for smoking cessation to the American Lung Association's Freedom from Smoking (FFS; American Lung Association, 2013). FFS is one of the most widely used intensive (2 months) smoking cessation intervention available in the US (Thieleke, McMahon, Meyer, & Yun, 2005). It provides cognitive behavioral modification, skills training and group support, and has demonstrated 1-year post-quit biochemically confirmed abstinence rates of 16% (Thieleke et al., 2005). The Brewer (2011a) trial showed that mindfulness training compared to FFS produced non-significantly higher abstinence post-treatment and significantly higher abstinence rates 13-weeks post-quit. The study provided the FFS intervention in a way that was faithful to its clinical implementation, but made few alterations in FFS to time/intensity match the mindfulness intervention.
In this paper we describe an intervention providing mindfulness training for smokers (MTS) compared to FFS. Ours study differs from Brewer et al. (2011a) in that substantial “enhancements” were made to FFS (referred to here as FFS-E) in order to more closely match the two interventions, and better isolate and test the effect of mindfulness training. Additionally, recruitment in the present study was carried out with a low socioeconomic status (SES) population. We were unable to find published studies on mindfulness training for low SES smokers or the effect of SES on outcomes in mindfulness training. Low SES smokers were targeted because smoking occurs disproportionately among low-SES individuals (David, Esson, Peruice, & Fitzpatrick, 2010; Hiscock, Bauld, Amos, Fidler, & Munafo, 2012; Kunst, Giskes, & Mackenbach, 2004), and it seemed important to understand whether training in mindfulness – a conceptually abstract cognitive skill - would be well received within a low SES population. It was our supposition that mindfulness training could be provided using concrete language and accessible examples such that it would be well-received and effective in this population. Furthermore, it was felt that if mindfulness training could be provided in a way that was effective in this challenging population, we would have a promising model for use in the wider population of smokers. The purpose of this study was to compare MTS to FFS-E on measures of class attendance, attrition, practice compliance, smoking abstinence, urge intensity, mindfulness acquisition, and psychological outcomes.
2. Materials and Methods
2.1. Study Recruitment
Participants living in low SES areas of a mid-sized Midwestern city were targeted for recruitment via advertisements placed on television, newspaper, and flyers. Phone screening inclusion/exclusion criteria required that participants be at least 18 years of age, smoke five or more cigarettes per day, use no other tobacco products, claim high motivation to quit, and not consume more than four alcoholic drinks on more than four days per week.
2.2. Procedures
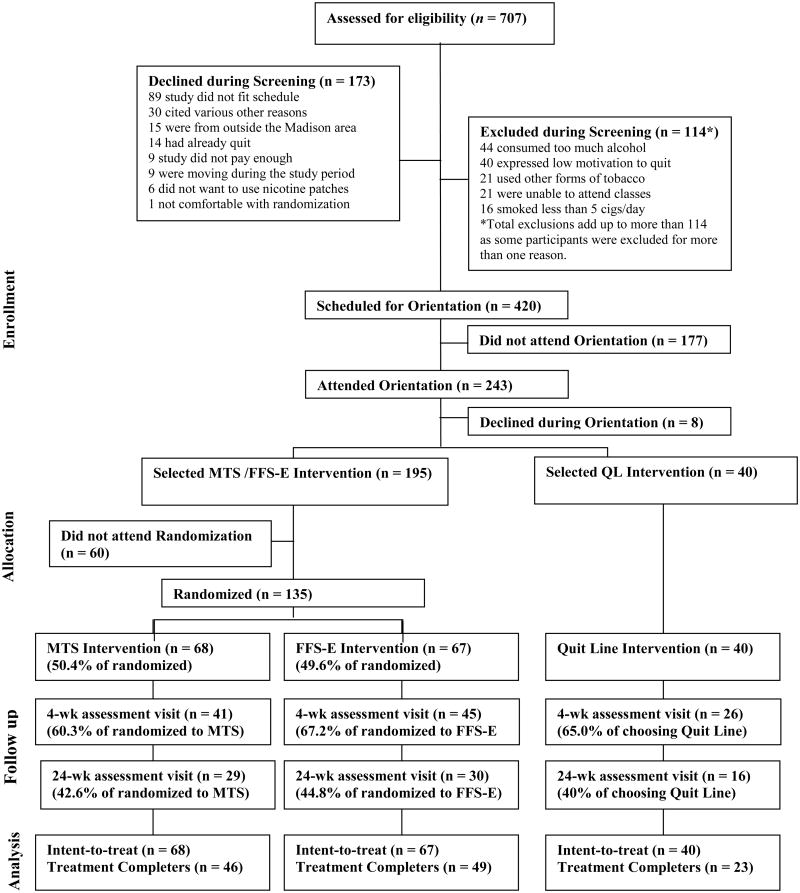
Callers who passed phone screening were invited to an orientation visit at a study center where they were evaluated for suicidality via the Patient Health Questionnaire (PHQ-9; Kroenke, Spitzer, & Williams, 2001). At the orientation meeting, potential participants received an overview of two high intensity interventions (MTS /FFS-E) and a lower intensity Quit Line (QL) intervention that used the Wisconsin Tobacco Quit Line (WTQL) as its behavioral therapy. At the orientation, the WTQL was described as “the most widely used and studied smoking cessation intervention in the state,” FFS-E as an “enhanced version of a well-studied, widely used intervention”, and MTS as a “novel and unproven intervention.” Potential participants were told that all interventions provided equal payment and cessation medications, and were asked to choose whether they wished to be placed in a low intensity (QL) or high intensity (MTS /FFS-E) intervention. This design was employed so MTS/FFS-E participants were not motivated principally by free patches or payment but in part by a desire to attend a high-intensity intervention. Consented individuals completed the baseline assessment visit (Figure 1).
Fig. 1.
Consort Diagram.
2.3. QL Intervention
If participants chose QL, they were asked to place a phone call to the WTQL (run by Alere-Wellbeing) while still at the study center. This initial call lasted approximately 45 minutes and consisted of speaking to intake personnel and a quit coach who provided motivational interviewing and assistance in developing a quit plan. QL participants were provided with two weeks of nicotine patches, self-help materials, an interactive website, and were offered unlimited free follow-up calls to the WTQL.
2.4. Randomization
Participants who chose the higher intensity intervention (MTS or FFS-E) were scheduled to attend their first class where they were randomized to MTS or FFS-E and immediately began treatment. The use of randomization followed immediately by therapy was employed to reduce dropout. At the first class, MTS participants were given the MTS Manual, meditation CD and access to the MTS website. FFS-E participants were given a FFS-E Manual, relaxation CD and access to the FFS Online Premium Program.
2.5 Mindfulness Training
The MTS course for smokers lasted seven weeks, and was comprised of seven 2½-hour classes and a 6½-hour Quit Day Retreat (total = 24 hours) (Table 1). During each class, instructors would play approximately 20 minutes of the MTS Instructional Video, which provided instruction in mindful meditation, walking, smoking, eating, and mindful management of smoking triggers, urges, addictive thoughts and emotions. After playing the DVD, instructors would lead exercises and provide more nuanced and individualized instruction. The final hour of class was a “Meditation Group,” consisting of guided meditation and group-support practice called “mindful talking and listening.” On the Quit Day Retreat, smokers attempted smoking cessation and initiated a 2-week course of nicotine patches. After the intervention, participants were invited to continue to attend the Meditation Group at any time. Throughout the MTS intervention participants were asked to practice 15-30 minutes of meditation per day at home with a guided meditation CD.
Table 1.
Schedule and Activities for MTS and FFS-E Participants.
| Week | Activity | Hours | Description |
|---|---|---|---|
| 1 | Class 1 | 2.5 | MTS : (mindfulness and mindfulness meditation) + Meditation Group |
| FFS-E: (aspects of addiction, prior obstacles, smoking triggers) +Relaxation Group | |||
| 2 | Class 2 | 2.5 | MTS : (mindfulness for triggers and automatic behavior) + Meditation Group |
| FFS-E: (automatic behavior, stress management, positive messages) + Relaxation Group | |||
| 3 | Class 3 | 2.5 | MTS : (mindfulness for emotions and stressful situations) + Meditation Group |
| FFS-E: (finding support, social situations) + Relaxation Group | |||
| 4 | Class 4 | 2.5 | MTS : (mindfulness for urges and withdrawal symptoms) + Meditation Group |
| FFS-E: (stages of grief, weight control) + Relaxation Group | |||
| 5 | Class 5 | 2.5 | MTS : (mindfulness for addictive thoughts and eating) + Meditation Group |
| FFS-E: (coping strategies, managing urges, quit day planning) + Relaxation Group | |||
| 5 ½ | Quit | 6.5 | MTS : Quit Day Retreat (weekend) (start 2 weeks of patches) |
| Day | FFS-E: Quit Day Retreat (weekend) (start 2 weeks of patches) | ||
| 6 | Class 6 | 2.5 | MTS : (Managing lapse and relapse) + Meditation Group |
| FFS-E: (preventing relapse) + Relaxation Group | |||
| 7 | Class 7 | 2.5 | MTS : (Long term practice) + Meditation Group |
| FFS-E: (physical activity, image of non-smoker, secondhand smoke) + Relaxation Group |
Note. Mindfulness training for smokers (MTS) and Freedom From Smoking-Enhanced (FFS-E) were matched on total number of hours, timing of individual classes and class activities, group interaction time, targeting of similar relapse challenges, materials, meditation/relaxation practice time and instructor qualifications. The total time for each course was 24 hours over 7 weeks.
2.6. Matching of MTS and FFS-E
MTS and FFS-E were matched in time and intensity, pharmacotherapy (2 week of nicotine patches) and in almost every other way feasible (Table 1). The goal of this matching was to maintain the core practices and materials of FFS (American Lung Association, 2013), but to provide “enhancements” to FFS that would allow it to match MTS so as to isolate the core differences between therapies: MTS would provide training in mindfulness and meditation, whereas FFS would provide training in a variety of cognitive skills and relaxation. Matching of FFS-E to MTS included the following “enhancements”: 1) To match MTS, total time in FFS-E was increased to 24 hours (FFS typically provides eight 90-120 minute sessions (12-16 hours) (American Lung Association, 2014) (Prochaska et al., 1993; Stead & Lancaster, 2005); 2) like MTS, FFS-E classes provided an additional 30 minutes per class for group sharing and support, (Rosenbaum & O'Shea, 1992); 3) to match meditation practice in MTS, FFS-E emphasized relaxation, by including a 15-30 minute relaxation practices in each class, 15-30 minute assigned daily guided relaxation with a CD, logged practice time, and weekly discussion on effects of this practice (FFS provides the same relaxation CD, but the practice is not emphasized in this way) (Manzoni, Pagnini, Castelnuovo, & Molinari, 2008); 4) like MTS, FFS-E was provide with an optional long-term weekly support group (Zhu, Stretch, Balabanis, Rosbrook, Sadler, & Pierce, 1996); 5) materials were matched with 90 page manuals and CDs of similar appearance provided to each group; 6) Instructor qualifications and training between the two groups were matched. All instructors for the two interventions had a Masters degree in Psychology (except for one MTS instructor who had a PhD in Sociology), and no instructor had specialized training or certification in addiction therapy (FFS instructors are typically laypeople). MTS instructors were provided with a two-day MTS teacher-training course, whereas, FFS-E instructors were provided with a similarly structured two-day FFS-E teacher-training course (Stein & Lambert, 1995).
2.7. Smoking Measures
Smoking status and self-report data were collected for all groups at three assessment visits: baseline, 4-and 24-weeks after the quit day. Participants were paid $30 for attending each of the two post-quit assessment visits regardless of smoking status. Primary outcome measures were 7-day point-prevalence abstinence at 4- and 24-weeks post-quit day, confirmed by a carbon monoxide (CO) breath test and Timeline Follow-Back smoking calendar (TLFB; Brown et al., 1998). A CO reading below 7 ppm (instead of 10 ppm) was used to define abstinence to minimize the possibility of false positive outcomes (Middleton & Morice, 2000). Additional measures of abstinence included number of days smoked in the first two weeks post-quit, which correlates well with six-month abstinence rates (Baker et al., 2011).
2.8. Self-Report Measures
1) Demographics and smoking history. 2) The Fagerstrom Test for Nicotine Dependence (FTND; Heatherton et al., 1991). 3) The Acceptance and Action Questionnaire (AAQ; Boelen & Reijntjes, 2008; Hayes et al., 2004a). 4) The Perceived Stress Scale-10 (PSS; Leung, Lam, & Chan, 2010). 5) The Five-Facet Mindfulness Questionnaire (FFMQ; Baer, Smith, Hopkins, Krietemeyer, & Toney, 2006) is a 39-question survey provided at all three assessment visits to assess mindfulness on five subscales (“observing,” “describing,” “acting with awareness,” “non-judging of inner experience,” and “non-reactivity to inner experience”) and has internal constancy for subscales between α = .75 and .91; (Baer et al., 2008; Lykins & Baer, 2009). 6) Compliance with daily meditation (MTS) or relaxation (FFS-E) was assessed via the Meditation/Relaxation Calendar in which participants were instructed to record daily practice from Class 1 until the 4-week assessment visit. 7) Urge assessment was performed via three phone calls to participants during the week before the intervention and three more calls during the week following the quit day. During each call participants were asked “Over the past 24 hours, how strong have your urges to smoke been on a scale of 0-10?”
2.9. Data Analysis
Seven-day point-prevalence abstinence served as the main outcome measure (Schlomer, Bauman, & Card, 2010). Data analyzed on repeated self-report measures used report completers only. Independent group t -tests and chi-squared tests were used to compare groups on baseline characteristics. Logistic regression was used to compute odds ratios (OR) estimates and confidence intervals for smoking abstinence. Pearson correlations were used to compute associations between secondary outcome measures and continuous smoking outcomes. Univariate ANCOVAs were conducted to identify between-group differences on change in repeated self-report measures. ANCOVAs controlled for abstinence status due to possibility that abstinence might bias ratings on self-report measures. ANCOVAs were tested and met the homogeneity of regression slopes assumption. All analyses were conducted using SPSS XXI.
2.10. Power Analysis
Power analysis was based on results reported by Brewer et al. (2011a) who found biochemically confirmed 17-week abstinence rates for mindfulness training (MT) = 31% vs. 6% for Freedom from Smoking. We planned to use an enhanced version of FFS, and predicted that at most this enhancement might yield 2X the abstinence rate as Brewer's control (12%). Analysis of groups with equal proportion with power = 80%, alpha=.05 (two tailed test) showed that we would need N=146 to detect 31% vs. 12% effect size between groups. Due to financial constraints, final enrollment was N=135, representing 93% of the 146 enrollment goal, or power = 76%.
3. Results
3.1. Recruitment
Recruitment efforts over 12 months led to 707 callers reached for phone screening. After declines, exclusions, and no-shows, 40 participants chose low intensity (QL) and 135 participants were randomized to MTS (n = 67) or FFS-E (n = 68; Figure 1).
3.2. Demographics
Randomized participants (MTS and FFS-E) showed a mean age of 44.50 years (SD = 12.73), 46.7% female, 88.1% Caucasian, and 64.9% with education beyond high school (Table 2). There were no significant differences between MTS and FFS-E on any baseline variable. QL compared to MTS/FFS-E showed no statistically significant baseline differences on age, gender, and years smoked, but did show significant differences on measures of race, education and number of prior quit attempts (Table 2).
Table 2.
Participant Baseline Characteristics.
| Total (MTS /FFS-E/QL) | Total Randomized (MTS /FFS-E) | MTS | FFS-E | QL | |
|---|---|---|---|---|---|
| Baseline Characteristics | 175 | 135 | 68 | 67 | 40 |
|
| |||||
| Age | 44.69 (12.51) | 44.50 (12.73) | 43.24 (12.05) | 45.78 (13.35) | 45.33 (11.89) |
| Gender | |||||
| Male | 52% | 53.3% | 57.4% | 49.3% | 47.5% |
| Female | 48% | 46.7% | 42.6% | 50.7% | 52.5% |
| Race | |||||
| American Indian | 1.1% | 1.5% | 4.4% | 1.5% | 2.5% |
| Asian | 2.3% | 2.2% | 0.0% | 2.2% | 2.5% |
| African American | 13.8% | 3.0% | 2.9% | 3.0% | 50.0% |
| Latino or Hispanic** | 1.7% | 2.2% | 4.4% | 2.2% | 0.0% |
| Caucasian | 78.3% | 88.1% | 85.3% | 88.1% | 45.0% |
| Other | 1.7% | 1.5% | 1.5% | 1.5% | 0.0% |
| Unknown* | 1.1% | 1.5% | 1.5% | 1.5% | 0.0% |
| Education | |||||
| High School or less | 40.1% | 35.1% | 29.9% | 40.3% | 57.9% |
| Beyond High School | 59.9% | 64.9% | 70.1% | 59.7% | 42.1% |
| Number of cigarettes/day | 16.93 (8.27) | 17.67 (8.59) | 17.49 (9.37) | 17.85 (7.78) | 14.38 (6.55) |
| Number of years smoked | 23.95 (12.67) | 24.78 (12.95) | 24.07 (12.57) | 25.49 (13.39) | 21.18 (11.35) |
| Number of quit attempts | 8.84 (18.01) | 10.10 (20.16) | 9.85 (19.88) | 10.36 (20.61) | 4.60 (5.33) |
| FTND | 4.65 (2.18) | 4.78 (2.20) | 4.63 (2.34) | 4.92 (2.05) | 4.23 (2.08) |
Unknown data was typically due to errors filling out data packets.
Recruitment materials and intervention materials were in English only.
Note. MTS and FFS-E did not significantly differ on any characteristics as baseline.
3.3. Pharmacotherapy
Participants in each intervention received two weeks of nicotine patches (14mg for ≤10, and 21 mg >10 cigarettes per day). A total of 71.7% of study participants reported that they completed the two weeks of nicotine patches (MTS = 74.4%, FFS-E = 81.5%, QL = 52.0%), with no reportable medication reactions and no significant differences in abstinence comparing patch users to non-users. Participants were asked whether they used NRT as prescribed (starting on (or near) the quit day and continuing for 2 weeks). In an analysis of all participants together, those who reported using nicotine patches were significantly more likely to be abstinent at both time points, but with larger differences in the more proximal post treatment period. At 4-weeks post quit (NRT = 53.5%, No-NRT = 29.6%, t(109) = -2.19, p = .03) and 24 weeks post quit (NRT = 29.8% vs. No NRT = 14.8 (t(109) = -1.54, p = .09). When treatment groups (MTS, FFS-E, QL) were analyzed individually, use of nicotine patch failed to predict abstinence.
3.4. Attrition and attendance
Intervention attrition was defined for MTS /FFS-E participants as not attending the Quit Day Retreat and defined for QL participants as not reporting a quit attempt on their assigned quit day. Intervention attrition was not significantly associated with any baseline variable and did not differ significantly between groups (MTS = 32.4%, FFS-E = 26.9%, QL = 42.5%). Attrition rates at assessment visits were not significantly different between groups (4-week assessment visit: MTS = 39.7%, FFS-E 32.8%, QL = 35.5%) and (24-week assessment visit: MTS = 57.4%, FFS-E = 55.2%, QL= 60%). Class attendance at eight potential meetings was similar for MTS and FFS-E participants (MTS = 5.35 classes; FFS-E = 5.15 classes, p = .65). Abstinent participants attended significantly more classes than relapsed participants (abstinent: M = 6.94, SD = 1.67 and relapsed: M = 4.35, SD = 2.55, t(133) = 28.68, p < .001).
3.5. Meditation/Relaxation time
No significant difference was found between MTS and FFS-E in meditation/relaxation practice time (MT: M = 19.60, SD = 13.78; FFS-E: M = 16.40, SD = 18.99, t(76) = .46, p = .40). Meditation/relaxation time was not significantly associated with smoking abstinence in either group, although MTS participants showed the expected relationship of higher numeric meditation time in abstinent participants, whereas FFS-E did not (MTS abstinent: M = 21.50 min, SD = 14.69; MTS relapsed: M = 16.09 min, SD = 11.64), t(35) = .91, p = .26; FFS-E abstinent M = 12.97 min, SD = 15.97; FFS-E relapsed M = 20.78 min, SD = 21.95), t(39) = .91, p = .20).
3.6. Primary Outcomes
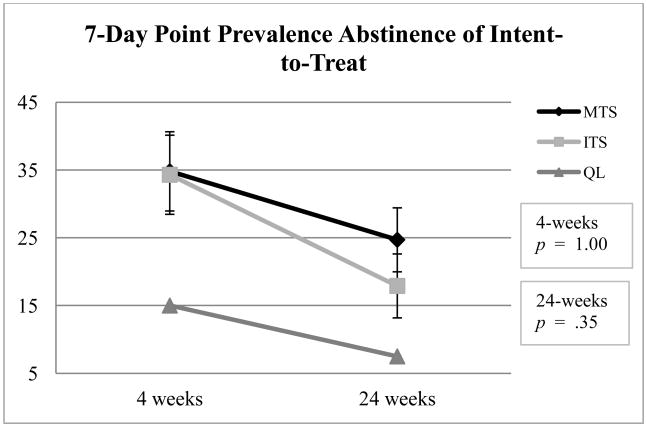
Intent-to-treat analysis of 7-day point prevalence abstinence between two groups was almost identical at 4 weeks (MTS = 35.3%; FFS-E = 34.3%; p = 1.00, OR = 1.04, CI = 0.51-2.19). At 24 weeks however, MTS compared to FFS-E showed higher numerical abstinence rates (MTS = 25.0%; FFS-E = 17.9%; p = 0.35, OR = 1.53, CI = 0.67-3.51), but failed to reach statistical significance (Figure 2).
Fig. 2. Intent-to-Treat Analysis of Biochemically Confirmed 7-Day Point Prevalence.
Intent-to-treat analysis of low socioeconomic state smokers receiving mindfulness training for smokers (MTS) or Freedom From Smoking-Enhanced (FFS-E) on 7-day point prevalence smoking abstinence confirmed by carbon monoxide breath test showed almost identical abstinence rates for the two groups at 4-weeks (MTS = 35.3%; FFS-E = 34.3%) but higher abstinence rates in MTS at 24-weeks post-quit (MTS = 25.0%; FFS-E = 17.9%). Abstinence rates for the Tobacco Quit Line (phone counseling) group was 15% and 7.5% at 4 and 24 weeks respectively and shown for reference only.
3.7. Secondary Outcomes
3.7.1. Urge assessment
Urge rating was calculated by assessing the mean urge ratings for three baseline phone calls and three post-quit calls. There were no significant differences in baseline urge ratings between groups. Repeated-measures ANOVAs comparing MTS to FFS-E participants showed a significant drop in urge ratings from baseline to post-quit (MTS: baseline M = 6.24, SD = 2.08, post-quit M = 5.14, SD = 2.40; FFS-E baseline M = 6.45, SD = 1.58, post-quit M = 6.14, SD = 2.46, F(1,71) = 4.46, p = .04).
Furthermore, post-quit urge ratings were significantly correlated with 7-day point prevalence abstinence at 4-weeks (r(87) = -.23, p = .03) and 24-weeks post-quit (r(87) = -.33, p = .001), such that those who reported lower urges were more likely to be abstinent.
3.7.2. Repeated self-report measures
Analysis of baseline self-report measures using univarate ANOVAs showed no significant differences between MTS and FFS-E on measures of mindfulness (FFMQ), experiential avoidance (AAQ), or perceived stress (PSS; Table 3). At 24-weeks post-quit, MTS compared to FFS-E showed numerically greater changes in the expected direction in every reported measure with significant differences in experiential avoidance (AAQ, p = .02), perceived stress (p = .03), mindfulness (p = .03), and FFMQ subscales: acting with awareness (p = .03), non-judging (p = .04), and non-reacting (p = .04). An intent-to-treat analysis that carried forward baseline scores for participants who did not attend follow-up visits (MTS n = 68, FFS-E = 67, QL = 40) showed no significant differences between MTS and FFS-E at 24-weeks post-quit.
Table 3.
Univariate Analysis of Change in Self-Report Measures.
| Measures | MTS Group (n = 29) | FFS-E Group (n = 30) | QL Group (n = 16) | ANOVA Model Effects at 24-weeks post-quit |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
|
| ||||||||||
|
Baseline mean(SD) |
4-week mean(SD) |
24-week mean(SD) |
Baseline mean(SD) |
4-week mean(SD) |
24-week mean(SD) |
Baseline mean(SD) |
4-week mean(SD) |
24-week mean(SD) |
F statistic, sig | |
| Five Facet Mindfulness Questionnaire | 3.39 (.53) | 3.62 (.49) | 3.72 (.56) | 3.23 (.37) | 3.42 (.41) | 3.43 (.48) | 3.24 (.37) | 3.24 (.40) | 3.27 (.37) | F(1,57) = 4.81, p = .03t |
| (FFMQa) (All 4) | ||||||||||
| FFMQa subscale: Observing | 3.43 (.73) | 3.80 (.43) | 3.69 (.73) | 3.55 (.72) | 3.75 (.54) | 3.72 (.58) | 3.27 (.77) | 3.41 (.69) | 3.22 (.76) | F(1,57) = 0.23, p = .88 |
| FFMQa subscale: Describing | 3.50 (.76) | 3.76 (.63) | 3.77 (.70) | 3.57 (.78) | 3.63 (.76) | 3.69 (.67) | 3.62 (.66) | 3.55 (.47) | 3.44 (.47) | F(1,57) = 0.21, p = .65 |
| FFMQa subscale: Acting with Awareness | 3.38 (.83) | 3.58 (.75) | 3.66 (.79) | 3.06 (.66) | 3.20 (.59) | 3.25 (.65) | 3.26 (.86) | 3.26 (.80) | 3.49 (.79) | F(1,57) = 4.80, p = .03* |
| FFMQa subscale: Non-judging | 3.55 (.78) | 3.55 (.79) | 3.88 (.75) | 3.37 (.51) | 3.51 (.59) | 3.49 (.66) | 3.15 (.75) | 3.13 (.76) | 3.14 (.67) | F(1,57) = 4.50, p = .04* |
| FFMQa subscale: Non-reacting | 3.09 (.57) | 3.59 (.58) | 3.56 (.51) | 2.87 (.48) | 3.33 (.51) | 3.25 (.60) | 2.91 (.53) | 2.98 (.49) | 2.99 (.52) | F(1,57) = 3.78, p = .04* |
| AAQb | 3.51 (.81) | 3.38 (.78) | 3.06 (.74) | 3.53 (.70) | 3.50 (.74) | 3.57 (.83) | 4.01 (.72) | 4.06 (.37) | 4.07 (.63) | F(1,57) = 6.09, p = .02* |
| PSSc | 16.21 (6.15) | 14.86 (7.22) | 13.00 (6.48) | 17.47 (5.91) | 17.20 (7.49) | 16.93 (7.07) | 19.38 (6.31) | 20.25 (7.40) | 19.69 (6.84) | F(1,57) = 4.96, p = .03* |
FFMQ = Five-Facet Mindfulness Questionnaire (Baer et al., 2006)
AAQ = Acceptance and Action Questionnaire and measures experiential avoidance (Boelen & Reijntjes, 2008; Hayes et al., 2004a)
PSS = Perceived Stress Scale (Leung, Lam, & Chan, 2010)
Note. Data are derived only from participants who completed all three study assessment visits.
The QL group is excluded in the analysis and descriptives are provided for reference only.
Univariate ANOVAs are shown comparing mindfulness training for smokers (MTS) to Freedom From Smoking-Enhanced (FFS-E) at 24-weeks post-quit assessment visit.
p < .10
p < .05
p < .01
p < .001
At 24-weeks post-quit, MTS compared to FFS-E showed numerically greater changes in the expected direction in every reported measure with significant differences in experiential avoidance, perceived stress, mindfulness, and mindfulness subscales: acting with awareness, non-judging, and non-reacting.
4. Discussion
4.1. Key findings
In this study comparing mindfulness training for smokers (MTS) to an enhanced version of the American Lung Association Freedom From Smoking program (FFS-E), we found that abstinence rates between the two groups were almost identical 4 weeks post quit, but that MTS showed numerically (but not significantly) higher abstinence rates at 24 weeks post quit. In addition, MTS compared to FFS-E demonstrated a significantly larger decrease in reported post-treatment urge intensity, and MTS compared to FFS-E showed significantly larger increases in self-reported mindfulness and decreases in self-reported stress and experiential avoidance.
This study provided a closely matched active control (FFS-E) in order to experimentally isolate the impact of mindfulness training as a therapeutic ingredient. The absence of significant differences between the two groups on baseline variables, intervention attrition, class attendance, and practice of mindfulness/relaxation suggests that participants engaged in the interventions similarly, allowing for a meaningful comparison between groups. The fact that MTS and FFS-E were matched in length, schedule, materials, home practice requirements, instructor qualifications, and targeted relapse challenges suggests that differences in outcomes might be attributed to mindfulness training.
The numerical advantage in abstinence rates at 24-weeks (MTS = 25.0% vs. FFS-E = 17.9%, OR = 1.52) in this small sample size study raises the possibility that mindfulness training might provide a degree of long-term relapse resistance. This advantage is more meaningful when taken in the context of other studies with similar findings. Brewer et al. (2011a) reported a small benefit to mindfulness training compared to FFS at 4-weeks, but a large benefit at 17-weeks (Brewer et al., 2011a). A study on ACT showed nearly identical abstinence post treatment, but abstinence of ACT = 35% vs. control = 15% at 1-year post-quit (Gifford et al., 2004). The possibility that mindfulness training may confer extended relapse resistance is important because treatment with pharmacotherapy often shows high relapse rates once medications are discontinued (Goldstein, Niaura, Follick, & Abrams, 1989), and ultimately the goal for tobacco treatment is long-term abstinence (Goldstein et al., 1989; Hajek, Stead, West, Jarvis, & Lancaster, 2009; Hays et al., 2001). One plausible reason that MTS might provide a long-term effect is that MTS teaches only one skill for relapse prevention—mindfulness. It is reasonable to think a single skill practiced repeatedly might be entrained more deeply, better integrated into daily life, and more accessible during late relapse challenges.
MTS compared to FFS-E showed a significant decrease in pre- to post-quit urge ratings, a meaningful finding because urges are the most commonly cited cause of relapse in smokers (Cummings, Jaen, & Giovino, 1985; Hughes, Keely, & Naud, 2004; Marlatt & Gordon, 1985; Norregaard, Tonnesen, & Petersen, 1993; Shiffman et al., 1996). The significant comparative decrease suggests mindfulness training may have led to decreases in post-quit urges. Urge reduction after mindfulness practice has been seen in other studies (Cropley, Ussher, & Charitou, 2007; Westbrook et al., 2011), and is perhaps related to suppression of activity in the default mode network (Brewer et al., 2011b). The correlation of urge to relapse found in this study suggests the possibility that mindfulness training might affect smoking behavior via changes in urge intensity. In addition to the observation that mindfulness may effect the intensity of craving itself, it has also been proposed that mindfulness training perhaps more importantly may effect a smoker's response to craving (Elwafi, Witkiewitz, Mallik, Thornhill, & Brewer, 2012). The importance of craving is now being explored in greater depth in the literature (Tiffany & Wray, 2011) as it has become clear that craving as assessed in experimental settings is not predictably associated with smoking behavior. Additional design elements would be necessary to better understand how mindfulness training in MTS might affect craving, or modulate a response to craving, and whether craving or a modulated response craving might affect smoking behavior.
MTS compared to FFS-E participants scored higher on post-treatment mindfulness tests, supporting the notion that MTS participants were acquiring mindfulness skills as they might in a more established mindfulness intervention (MBSR, MBCT; Baardseth et al., 2013; Maccoon et al., 2012). It is noteworthy that MTS compared to FFS-E participants showed larger decreases in post-treatment stress scores. Stress reduction is commonly found in mindfulness interventions (Carlson, Speca, Faris, & Patel, 2007; Carlson, Speca, Patel, & Goodey, 2004), and it is promising that a novel intervention demonstrates this finding. The fact that MTS participants showed larger decreases in experiential avoidance compared to FFS-E is relevant because MTS teaches participants explicitly to “accept” rather than “avoid or fix” uncomfortable thoughts, feelings, or physical sensations (Baer et al., 2008; Kabat-Zinn, 1990). Data suggests that avoidance of urges or negative affect may be a poor relapse prevention strategy and that use of acceptance-based strategies may be more effective (Hayes et al., 2004b; Stewart, Zvolensky, & Eifert, 2002). A decrease in experiential avoidance in this study suggests mindfulness training may affect smoking behavior in part through changes in experiential avoidance.
The study was targeted to a low SES population because most smokers are more likely to be low SES and it was important to demonstrate effectiveness in this population. Multiple investigations have highlighted the disparities in tobacco dependence and smoking cessation among different socioeconomic groups. Those in lower socioeconomic status groups have been more likely to be smokers (Hiscock, Bauld, Amos, Fidler, & Munafo, 2012) and less likely to succeed in efforts to quit smoking (Broms, Silventoinen, Lahelma, Koskenvuo, 2004; Gilman, Abrams, & Buka, 2003; Hiscock et al., 2012). When treatment is available to those of lower socioeconomic status, they are less likely to begin treatment (Adler & Newman, 2002), and are more likely to stop treatment program before completion (Hiscock et al., 2012).
This study used a non-conventional study design that allowed smokers to choose a less intensive group if they did not wish to participate in MTS or FFS-E. This design was chosen to limit the number of participants who might join MTS or FFS-E primarily to obtain free medications or study payment. The study design provided ecological validity in that participants in a high intensity smoking intervention in a clinical setting have chosen to be in that intervention. An interesting finding in this study was that only 40 of 175 participants (22.9%) chose to enroll in the less intensive QL intervention although the WTQL was promoted as being the most “well-studied and widely used” of the three interventions (Lichtenstein, Glasgow, Lando, Ossip-Klein, & Boles, 1996; Stead, Perea, & Lancaster, 2006).
4.2. Limitations
One potential limitation in this study is that participants were not blinded to their respective treatment conditions. MTS and FFS-E were, however, described as being equivalent in almost every way. Attrition represents another limitation, reducing power and generalizability. It is possible that study completers were more receptive to mindfulness (provided in MTS) or CBT (provided in FFS-E) than study dropouts, artificially inflating self-report measures. Another limitation is the possibility with any lengthy intervention there will be change in motivation over time. Participants in MTS and FFS-E waited 5 weeks between the start of these interventions and their quit day and self-reported “high motivation” might have dropped leading to decrease in abstinence rates. Interventions of greater intensity tend to lead to higher abstinence rates (Prochaska et al., 1993; Stead & Lancaster, 2005), making it undesirable to decrease intervention intensity. One way to decrease this potential effect would be to run MTS over a shorter time period, or at least provide measurements of motivation on the quit day to see if they have changed.
Findings from this study suggest that mindfulness training compared to a matched control produced similar smoking abstinence rates post treatment, but at 24-weeks post-quit attempt, numeric abstinence rates diverged favoring the mindfulness condition. Findings also suggest that mindfulness training was associated with decreased urges, increased mindfulness, and decreased stress and experiential avoidance, all symptoms associated with smoking relapse. Results suggest that a larger study is warranted to examine how these factors might mediate the relationship between mindfulness training and smoking behavior.
Acknowledgments
This study was supported by funding from NIDA Grant K23 DA022471. Study oversight was provided by Michael Fiore and Tim Baker. Manuscript preparation was provided by Wendy Theobald and Hillary Merry. Study implementation was provided by Maggie Anderson, Kristin Stankevitz, David Mills, Andrew Sandgren, Allison Couilliard, Alex Strassman, Chelsea Davenport, Isabel Cupino, James Neitzel, Joeseph Chase, and Steven Gilbert. Study intervention developers included Jim Powell, Beth Wortzel, Jan Shappard Jesse Kaye, Katherine Hefner, and Steve Perlman.
Glossary
- Mindfulness
a cognitive skill of paying close attention to one's moment-to-moment experience and encountering sensations, emotions and thoughts with non-reactivity and acceptance.
- Mindfulness Training
a novel eight-meeting group intervention that uses training in mindfulness targeted to management of smoking triggers, urges, and withdrawal symptoms.
- Freedom from Smoking
a well-known (American Lung Association) eight-meeting group intervention that uses training in relaxation and cognitive techniques targeted to management of smoking triggers, urges, and withdrawal symptoms
Footnotes
Clinicaltrials.gov registration number: NCT01299909
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Adler NE, Newman K. Socioeconomic disparities in health: pathways and policies. Health Affairs. 2002;21(2):60–76. doi: 10.1377/hlthaff.21.2.60. [DOI] [PubMed] [Google Scholar]
- American Lung Association. Freedom From Smoking Online. [accessed on 2013 Jul 22];2013 Retrieved from: http://www.ffsonline.org/
- American Lung Association. Freedom From Smoking Group Classes. [accessed on 2014 Jan 13];2014 Retrieved from: http://www.lung.org/associations/charters/midland-states/learning-opportunities/patient-family/ffs-clinics/
- Baardseth TP, Goldberg SB, Pace BT, Wislocki AP, Frost ND, Siddiqui JR, et al. Wampold BE. Cognitive-behavioral therapy versus other therapies: redux. Clinical Psychology Review. 2013;33(3):395–405. doi: 10.1016/j.cpr.2013.01.004. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Baer RA, Smith GT, Lykins E, Button D, Krietemeyer J, Sauer S, Walsh E, Duggan D, Williams JM. Construct validity of the five facet mindfulness questionnaire in meditating and nonmeditating samples. Assessment. 2008;15(3):329–342. doi: 10.1177/1073191107313003. [DOI] [PubMed] [Google Scholar]
- Baker TB, Brandon TH, Chassin L. Motivational influences on cigarette smoking. Annual Review of Psychology. 2004;55:463–491. doi: 10.1146/annurev.psych.55.090902.142054. [DOI] [PubMed] [Google Scholar]
- Baker TB, Mermelstein R, Collins LM, Piper ME, Jorenby DE, Smith SS, Christiansen BA, Schlam TR, Cook JW, Fiore MC. New methods for tobacco dependence treatment research. Annals of Behavioral Medicine. 2011;41(2):192–207. doi: 10.1007/s12160-010-9252-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boelen PA, Reijntjes A. Measuring experiential avoidance: reliability and validity of the Dutch 9-item Acceptance and Action Questionnaire (AAQ) Journal of Psychopathology and Behavioral Assessment. 2008;30:241–251. doi: 10.1007/s10862-008-9082-4. [DOI] [Google Scholar]
- Bowen S, Marlatt A. Surfing the urge: brief mindfulness-based intervention for college student smokers. Psychology of Addictive Behavior. 2009;23:666–671. doi: 10.1037/a0017127. [DOI] [PubMed] [Google Scholar]
- Brewer JA, Mallik S, Babuscio TA, Nich C, Johnson HE, Deleone CM, et al. Rounsaville BJ. Mindfulness training for smoking cessation: results from a randomized controlled trial. Drug and Alcohol Dependence. 2011;119(1-2):72–80. doi: 10.1016/j.drugalcdep.2011.05.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewer JA, Worhunsky PD, Gray JR, Tang YY, Weber J, Kober H. Meditation experience is associated with differences in default mode network activity and connectivity. Proceedings of the National Academy of Sciences. 2011;108:20254–20259. doi: 10.1073/pnas.1112029108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Broms U, Silventoinen K, Lahelma E, Koskenvuo M, Kaprio J. Smoking cessation by socioeconomic status and marital status: the contribution of smoking behavior and family background. Nicotine & Tobacco Research. 2004;6(3):447–455. doi: 10.1080/14622200410001696637. [DOI] [PubMed] [Google Scholar]
- Brown RA, Burgess ES, Sales SD, Whiteley JA, Evans DM, Miller IW. Reliability and validity of a smoking timeline follow-back interview. Psychology of Addictive Behaviors. 1998;12:101–112. doi: 10.1037/0893-164X.12.2.101. [DOI] [Google Scholar]
- Carlson LE, Speca M, Patel KD, Goodey E. Mindfulness-based stress reduction in relation to quality of life, mood, symptoms of stress and levels of cortisol, dehydroepiandrosterone sulfate (DHEAS) and melatonin in breast and prostate cancer outpatients. Psychoneuroendocrinology. 2004;29(4):448–474. doi: 10.1016/S0306-4530(03)00054-4. [DOI] [PubMed] [Google Scholar]
- Carlson LE, Speca M, Faris P, Patel KD. One year pre-post intervention follow-up of psychological, immune, endocrine and blood pressure outcomes of mindfulness-based stress reduction (MBSR) in breast and prostate cancer outpatients. Brain Behavior and Immunity. 2007;21(8):1038–1049. doi: 10.1016/j.bbi.2007.04.002. [DOI] [PubMed] [Google Scholar]
- Chambers R, Gullone E, Allen NB. Mindful emotion regulation: An integrative review. Clinical Psychology Review. 2009;29(6):560–572. doi: 10.1016/j.cpr.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Chiesa A, Serretti A. Mindfulness-based stress reduction for stress management in healthy people: a review and meta-analysis. Journal of Alternative and Complementary Medicine. 2009;15(5):593–600. doi: 10.1089/acm.2008.0495. [DOI] [PubMed] [Google Scholar]
- Cinciripini PM, Wetter DW, Fouladi RT, Blalock JA, Carter BL, Cinciripini LG, Baile WF. The effects of depressed mood on smoking cessation: mediation by postcessation self-efficacy. Journal of Consulting and Clinical Psychology. 2003;71(2):292–301. doi: 10.1037/0022-006X.71.2.292. [DOI] [PubMed] [Google Scholar]
- Cosci F, Corlando A, Fornai E, Pistelli F, Paoletti P, Carrozzi L. Nicotine dependence, psychological distress and personality traits as possible predictors of smoking cessation. Results of a double-blind study with nicotine patch. Addictive Behaviors. 2009;34(1):28–35. doi: 10.1016/j.addbeh.2008.08.003. [DOI] [PubMed] [Google Scholar]
- Creswell JD, Way BM, Eisenberger NI, Lieberman MD. Neural correlates of dispositional mindfulness during affect labeling. Psychosomatic Medicine. 2007;69(6):560–565. doi: 10.1097/PSY.0b013e3180f6171f. [DOI] [PubMed] [Google Scholar]
- Cropley M, Ussher M, Charitou E. Acute effects of a guided relaxation routine (body scan) on tobacco withdrawal symptoms and cravings in abstinent smokers. Addiction. 2007;102(6):989–993. doi: 10.1111/j.1360-0443.2007.01832.x. [DOI] [PubMed] [Google Scholar]
- Cummings KM, Jaen CR, Giovino G. Circumstances surrounding relapse in a group of recent exsmokers. Preventive Medicine. 1985;14(2):195–202. doi: 10.1016/0091-7435(85)90035-0. [DOI] [PubMed] [Google Scholar]
- David A, Esson K, Peruice AM, Fitzpatrick C. Tobacco use: equity and social determinants. In: Blas E, Sivasankara Kurup A, editors. Equity, social determinants and public health programmes. Geneva, Switzerland: World Health Organization; 2010. pp. 199–218. [Google Scholar]
- Davis JM, Fleming MF, Bonus KA, Baker TB. A pilot study on mindfulness based stress reduction for smokers. BMC Complementary and Alternative Medicine, 7. 2007;2 doi: 10.1186/1472-6882-7-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davis JM, Goldberg SB, Anderson MC, Manley AR, Smith SS, Baker TB. Randomized trial on mindfulness training for smokers targeting a disadvantaged population. Substance Use and Misuse. doi: 10.3109/10826084.2013.770025. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deckersbach T, Holzel BK, Eisner LR, Stange JP, Peckham AD, Dougherty DD, Rauch SL, Lazar S, Nierenberg AA. Mindfulness-based cognitive therapy for nonremitted patients with bipolar disorder. CNS Neuroscience & Therapeutics. 2012;18(2):133–141. doi: 10.1111/j.1755-5949.2011.00236.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elwafi HM, Witkiewitz K, Mallik S, Thornhill TA, Brewer JA. Mindfulness training for smoking cessation: Moderation of the relationship between craving and cigarette use. Drug and Alcohol Dependence. 2012;130(1):222–229. doi: 10.1016/j.drugalcdep.2012.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farb NA, Anderson AK, Segal ZV. The mindful brain and emotion regulation in mood disorders. Canadian Journal of Psychiatry. 2012;57(2):70–77. doi: 10.1177/070674371205700203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gifford EV, Kohlenberg BS, Hayes SC, Pierson HM, Piasecki MP, Antonuccio DO, Palm KM. Does acceptance and relationship focused behavior therapy contribute to bupropion outcomes? A randomized controlled trial of functional analytic psychotherapy and acceptance and commitment therapy for smoking cessation. Behavior Therapy. 2011;42(4):700–715. doi: 10.1016/j.beth.2011.03.002. [DOI] [PubMed] [Google Scholar]
- Gifford EV, Kohlenberg BS, Hayes SC, Antonuccio DO, Piasecki MM, Rasmussen-Hall ML, Palm KM. Acceptance-based treatment for smoking cessation. Behavior Therapy. 2004;35(4):689–705. doi: 10.1016/S0005-7894(04)80015-7. [DOI] [PubMed] [Google Scholar]
- Goldstein MG, Niaura R, Follick MJ, Abrams DB. Effects of behavioral skills training and schedule of nicotine gum administration on smoking cessation. American Journal of Psychiatry. 1989;146(1):56–60. doi: 10.1176/ajp.146.1.56. [DOI] [PubMed] [Google Scholar]
- Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits. A meta-analysis. Journal of Psychosomatic Research. 2004;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Hajek P, Stead LF, West R, Jarvis M, Lancaster T. Relapse prevention interventions for smoking cessation. Cochrane Database of Systematic Reviews. 2009;1:CD003999. doi: 10.1002/14651858.CD003999.pub2. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Strosahl K, Wilson K. Acceptance and commitment therapy: An experiential approach to behavior change. New York, NY: Guilford Press; 1999. [Google Scholar]
- Hayes SC, Strosahl K, Wilson KG, Bissett RT, Pistorello J, Toarmino D, et al. McCurry SM. Measuring experiential avoidance: A preliminary test of a working model. The Psychological Record. 2004;54(4):553–578. [Google Scholar]
- Hayes SC, Wilson KG, Gifford EV, Bissett R, Piasecki M, Batten SV, et al. Gregg J. A preliminary trial of Twelve-Step Facilitation and Acceptance and Commitment Therapy with polysubstance-abusing methadone-maintained opiate addicts. Behavior Therapy. 2004;35(4):667–688. doi: 10.1016/S0005-7894(04)80014-5. [DOI] [Google Scholar]
- Hays JT, Hurt RD, Rigotti NA, Niaura R, Gonzales D, Durcan MJ, et al. White JD. Sustained-release bupropion for pharmacologic relapse prevention after smoking cessation. A randomized, controlled trial. Annals of Internal Medicine. 2001;135(6):423–433. doi: 10.7326/0003-4819-135-6-200109180-00011. doi: 0.7326/0003-4819-135-6-200109180-00011. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerstrom KO. The Fagerstrom Test for Nicotine Dependence: a revision of the Fagerstrom Tolerance Questionnaire. British Journal of Addiction. 1991;86(9):1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Hill CL, Updegraff JA. Mindfulness and its relationship to emotional regulation. Emotion. 2012;12(1):81–90. doi: 10.1037/a0026355. [DOI] [PubMed] [Google Scholar]
- Hiscock R, Bauld L, Amos A, Fidler JA, Munafo M. Socioeconomic status and smoking: a review. Annals of the New York Academy of Sciences. 2012;1248:107–123. doi: 10.1111/j.1749-6632.2011.06202.x. [DOI] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78(2):169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR. Smokers' beliefs about the inability to stop smoking. Addictive Behaviors. 2009;34(12):1005–1009. doi: 10.1016/j.addbeh.2009.06.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR, Keely J, Naud S. Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction. 2004;99(1):29–38. doi: 10.1111/j.1360-0443.2004.00540.x. [DOI] [PubMed] [Google Scholar]
- Johnson KA, Farris SG, Schmidt NB, Zvolensky MJ. Anxiety sensitivity and cognitive-based smoking processes: Testing the mediating role of emotion dysregulation among treatment-seeking daily smokers. Journal of Addictive Diseases. 2012;31(2):143–157. doi: 10.1080/10550887.2012.665695. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J. Wherever you go, there you are: Mindfulness meditation in everyday life. New York NY: Hyperion; 1994. [Google Scholar]
- Kabat-Zinn J. Full catastrophe living. New York NY: Dell Publishing; 1990. [Google Scholar]
- Kemeny ME, Foltz C, Cavanagh JF, Cullen M, Giese-Davis J, Jennings P, et al. Ekman P. Contemplative/emotion training reduces negative emotional behavior and promotes prosocial responses. Emotion. 2012;12(2):338–350. doi: 10.1037/a0026118. [DOI] [PubMed] [Google Scholar]
- Koszycki D, Benger M, Shlik J, Bradwejn J. Randomized trial of a meditation-based stress reduction program and cognitive behavior therapy in generalized social anxiety disorder. Behaviour Research and Therapy. 2007;45(10):2518–2526. doi: 10.1016/j.brat.2007.04.011. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kunst A, Giskes K, Mackenbach J. Socioeconomic inequalities in smoking in the European Union: applying an equity lens to tobacco control policies. Rotterdam Netherlands: Department of Public Health, Erasmus Medical Center Rotterdam; 2004. [Google Scholar]
- Leung DY, Lam TH, Chan SS. Three versions of Perceived Stress Scale: validation in a sample of Chinese cardiac patients who smoke. BMC Public Health. 2010;10(513) doi: 10.1186/1471-2458-10-513. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lichtenstein E, Glasgow RE, Lando HA, Ossip-Klein DJ, Boles SM. Telephone counseling for smoking cessation: rationales and meta-analytic review of evidence. Health Education Research. 1996;11(2):243–257. doi: 10.1093/her/11.2.243. [DOI] [PubMed] [Google Scholar]
- Linehan M. Cognitive behavioral therapy of borderline personality disorder. New York NY: Guliford Press; 1993. [Google Scholar]
- Lykins ELB, Baer RA. Psychological functioning in a sample of long-term practitioners of mindfulness meditation. Journal of Cognitive Psychotherapy. 2009;23(3):226–241. doi: 10.1891/0889-8391.23.3.226. [DOI] [Google Scholar]
- Maccoon DG, Imel ZE, Rosenkranz MA, Sheftel JG, Weng HY, Sullivan JC, et al. Lutz A. The validation of an active control intervention for Mindfulness Based Stress Reduction (MBSR) Behaviour Research and Therapy. 2012;50(1):3–12. doi: 10.1016/j.brat.2011.10.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manzoni GM, Pagnini F, Castelnuovo G, Molinari E. Relaxation training for anxiety: a ten-years systematic review with meta-analysis. BMdC psychiatry. 2008;8(1):41. doi: 10.1186/1471-244X-8-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt GA, Gordon JR. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. New York, NY: Guilford; 1985. [Google Scholar]
- Mars T, Abbey H. Mindfulness meditation practise as a healthcare intervention: A systematic review. International Journal of Osteopathic Medicine. 2010;13(2):56–66. doi: 10.1016/j.ijosm.2009.07.005. [DOI] [Google Scholar]
- Middleton ET, Morice AH. Breath carbon monoxide as an indication of smoking habit. Chest. 2000;117(3):758–763. doi: 10.1378/chest.117.3.758. [DOI] [PubMed] [Google Scholar]
- Moore A, Malinowski P. Meditation, mindfulness and cognitive flexibility. Consciousness and Cognition. 2009;18(1):176–186. doi: 10.1016/j.concog.2008.12.008. [DOI] [PubMed] [Google Scholar]
- Norregaard J, Tonnesen P, Petersen L. Predictors and reasons for relapse in smoking cessation with nicotine and placebo patches. Preventive Medicine. 1993;22(2):261–271. doi: 10.1006/pmed.1993.1021. [DOI] [PubMed] [Google Scholar]
- Price M, Gros DF, McCauley JL, Gros KS, Ruggiero KJ. Nonuse and dropout attrition for a web-based mental health intervention delivered in a post-disaster context. Psychiatry. 2012;75(3):267–284. doi: 10.1521/psyc.2012.75.3.267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC, Velicer WF, Rossi JS. Standardized, individualized, interactive, and personalized self-help programs for smoking cessation. Health Psychology. 1993;12(5):399–405. doi: 10.1037/0278-6133.12.5.399. [DOI] [PubMed] [Google Scholar]
- Rosenbaum P, O'Shea R. Large-scale study of freedom from smoking clinics – factors in quitting. Public Health Reports. 1992;107(2):150–155. [PMC free article] [PubMed] [Google Scholar]
- Schlomer GL, Bauman S, Card NA. Best practices for missing data management in counseling psychology. Journal of Counseling Psychology. 2010;57(1):1–10. doi: 10.1037/a0018082. [DOI] [PubMed] [Google Scholar]
- Segal Z, Williams JW, Teasdale J. Mindfullness-based cognitive therapy for depression: A new approach to preventing relapse. New York, NY: The Guilford Press; 2002. [Google Scholar]
- Shapiro SL, Oman D, Thoresen CE, Plante TG, Flinders T. Cultivating mindfulness: effects on well-being. Journal of Clinical Psychology. 2008;64(7):840–862. doi: 10.1002/jclp.20491. [DOI] [PubMed] [Google Scholar]
- Shiffman S. A cluster-analytic classification of smoking relapse episodes. Addictive Behaviors. 1986;11(3):295–307. doi: 10.1016/0306-4603(86)90057-2. [DOI] [PubMed] [Google Scholar]
- Shiffman S, Paty JA, Gnys M, Kassel JA, Hickcox M. First lapses to smoking: Within-subjects analysis of real-time reports. Journal of Consulting and Clinical Psychology. 1996;64(2):366–379. doi: 10.1037/0022-006X.64.2.366. [DOI] [PubMed] [Google Scholar]
- Stead LF, Lancaster T. Group behaviour therapy programmes for smoking cessation. Cochrane Database of Systematic Reviews. 2005;2 doi: 10.1002/14651858.CD001007.pub2. [DOI] [PubMed] [Google Scholar]
- Stead LF, Perea R, Lancaster T. Telephone counselling for smoking cessation. Cochrane Database of Systematic Reviews. 2006;3:CD002850. doi: 10.1002/14651858.CD002850.pub2. [DOI] [PubMed] [Google Scholar]
- Stein DM, Lambert MJ. Graduate training in psychotherapy: Are therapy outcomes enhanced? Journal of Consulting and Clinical Psychology. 1995;63(2):182–196. doi: 10.1037/0022-006X.63.2.182. [DOI] [PubMed] [Google Scholar]
- Stewart SH, Zvolensky MJ, Eifert GH. The relations of anxiety sensitivity, experiential avoidance, and alexithymic coping to young adults' motivations for drinking. Behavior Modification. 2002;26(2):274–296. doi: 10.1177/0145445502026002007. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, Segal Z, Williams JM. How does cognitive therapy prevent depressive relapse and why should attentional control (mindfulness) training help? Behaviour Research and Therapy. 1995;33(1):25–39. doi: 10.1016/0005-7967(94)E0011-7. [DOI] [PubMed] [Google Scholar]
- Thieleke J, McMahon J, Meyer G, Yun KA. An evaluation of the Freedom From Smoking Online cessation program among Wisconsin residents. Wisconsin Medical Journal. 2005;104(4):41–44. [PubMed] [Google Scholar]
- Tiffany ST, Wray JM. The clinical significance of drug craving. Vol. 1248. Annals of the New York Academy of Sciences; 2012. pp. 1–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uhart M, Wand GS. Stress, alcohol and drug interaction: an update of human research. Addiction Biology. 2009;14(1):43–64. doi: 10.1111/j.1369-1600.2008.00131.x. doi: 0.1111/j.1369-1600.2008.00131.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wampold BE. The great psychotherapy debate. Mahwah, New Jersey: Lawrence Erlbaum; 2001. [Google Scholar]
- Wampold BE, Mondin GW, Moody M, Stich F, Benson K, Ahn HN. A meta-analysis of outcome studies comparing bona fide psychotherapies: Empiricially, ‘all must have prizes’. Psychological Bulletin. 1997;122(3):203–215. doi: 10.1037//0033-2909.122.3.203. [DOI] [Google Scholar]
- Westbrook C, Creswell JD, Tabibnia G, Julson E, Kober H, Tindle HA. Mindful attention reduces neural and self-reported cue-induced craving in smokers. Social Cognitive and Affective Neuroscience. 2011;8(1):73–84. doi: 10.1093/scan/nsr076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA, Walker D. Mindfulness-based relapse prevention for alcohol and substance use disorders. Journal of Cognitive Psychotherapy. 2005;19(3):211–228. doi: 10.1891/jcop.2005.19.3.211. [DOI] [Google Scholar]
- Ziedonis D, Hitsman B, Beckham JC, Zvolensky MJ, Adler LE, Audrain-McGovern J, et al. Riley WT. Tobacco use and cessation in psychiatric disorders: National Institute of Mental Health report. Nicotine and Tobacco Research. 2008;10(12):1691–1715. doi: 10.1080/14622200802443569. [DOI] [PubMed] [Google Scholar]