Abstract
Introduction
Prehospital termination of resuscitation (TOR) rules have not been widely validated outside of Western countries. This study evaluated the performance of TOR rules in an Asian metropolitan with a mixed-tier emergency medical service (EMS).
Methods
We analysed the Utstein registry of adult, non-traumatic out-of-hospital cardiac arrests (OHCAs) in Taipei to test the performance of TOR rules for advanced life support (ALS) or basic life support (BLS) providers. ALS and BLS-TOR rules were tested in OHCAs among three subgroups: (1) resuscitated by ALS, (2) by BLS and (3) by mixed ALS and BLS. Outcome definition was in-hospital death. Sensitivity, specificity, positive predictive value (PPV), negative predictive value and decreased transport rate (DTR) among various provider combinations were calculated.
Results
Of the 3489 OHCAs included, 240 were resuscitated by ALS, 1727 by BLS and 1522 by ALS and BLS. Overall survival to hospital discharge was 197 patients (5.6%). Specificity and PPV of ALS-TOR and BLS-TOR for identifying death ranged from 70.7% to 81.8% and 95.1% to 98.1%, respectively. Applying the TOR rules would have a DTR of 34.2–63.9%. BLS rules had better predictive accuracy and DTR than ALS rules among all subgroups.
Conclusions
Application of the ALS and BLS TOR rules would have decreased OHCA transported to the hospital, and BLS rules are reasonable as the universal criteria in a mixed-tier EMS. However, 1.9–4.9% of those who survived would be misclassified as non-survivors, raising concern of compromising patient safety for the implementation of the rules.
Introduction
Out-of-hospital cardiac arrest (OHCA) is the leading cause of premature death in many countries.1 The goal of prehospital resuscitation for OHCAs is to achieve recovery of spontaneous circulation (ROSC) and to transport patients from field to hospital with minimal delay. Since survival from cardiac arrest is rare without presenting shockable rhythm or prehospital ROSC,1,2 emergency medical technicians (EMTs) face the dilemma of whether to transport the patients after unsuccessful field resuscitative attempts. Furthermore, speedy ambulance transports of all OHCA patients, regardless of chance of survival, may put the providers and the public at risk of associated traffic accidents.3 Thus, the latest guidelines for cardiopulmonary resuscitation (CPR) and emergency cardiovascular care recommended applying prediction rules of termination of resuscitation (TOR) for providers of basic life support (BLS) and advanced life support (ALS) prior to transport.4
Current TOR rules were derived and validated in North American and European sites, and the results consistently yielded high specificity and positive predictive values (PPVs).5–10 Recommended criteria for the TOR rule for BLS providers were (1) arrest not witnessed by first responder or emergency medical services (EMS) personnel, (2) no ROSC after three full rounds of CPR and automated external defibrillator (AED) analysis and (3) no AED shock prior to transport. For ALS providers, the criterion of no ROSC after three full rounds of CPR and AED analysis was replaced by no ROSC after receiving full ALS care prior to transport and an additional criterion of (4) no bystander CPR.4 In an area with mixed-tier EMS configuration, that is, a population served by BLS only, ALS only or mixed BLS-ALS services, current guidelines suggest using the BLS-TOR rule as the universal criteria to avoid confusion without impairing diagnostic accuracy.4,5,8,9
Most of the validation studies of the TOR rules have been done in Western countries; evaluations of data from different geographic, ethnic and cultural backgrounds are necessary prior to widespread implementation. Characteristics of OHCAs and configurations of EMS were quite different between the Western versus Asian countries. Key differences in OHCAs and EMS, including relatively lower rates of presenting shockable rhythm (ie, ventricular fibrillation/ventricular tachycardia (VF/VT)), lower rates of bystander CPR ranging from 1.5% to 36.7%, less ALS implementation and public access defibrillators,11,12 create potential threats to the prediction accuracy of the TOR rules. In a recent validation study from Japan, despite high PPVs for favourable neurological outcome of patients, the specificity was not as high as that tested in the Western communities.8,13
By using the Utstein-based OHCA registry of an Asian metropolitan area, we conducted a study to evaluate the performance of the ALS-TOR and BLS-TOR rules in this community and to determine whether the BLS-TOR rule can be implemented as the universal criteria in a mixed-tier EMS.
Methods
Study populations and Taipei EMS setting
An Utstein-based registry from Taipei EMS was used to focus on the accuracy of the TOR rules in adult OHCA resuscitated by three types of provider combination: (1) BLS only, (2) ALS only and (3) mixed BLS-ALS. Utstein-based registered data of Taipei EMS, initially developed for quality assurance process of OHCAs, consisted of dispatch records by the Taipei City Fire Department, modes and timeliness of prehospital care, patient demographics (age, sex), arrest characteristics (witness status, bystander CPR, initial monitored rhythm), records of whether AEDs were used, patient records from the EMS-receiving hospitals and patient outcomes (ROSC, survival to emergency department or intensive care unit admission and survival to hospital discharge).
Taipei City is a metropolitan area of 272 km2 with a registered population of 2.65 million; up to 3.0 million if inflow daytime workers are also included. The majority of the population are Taiwanese and Chinese. The metropolitan area is covered by the fire department-based BLS-D system with early defibrillation capability. From 2008 to 2010, the prehospital ALS service covered 3 of 12 administrative districts in Taipei.
The ALS teams comprise a staff of 65 EMT paramedics who have completed 1280 h of training required by the Department of Health, Taiwan. These teams were authorised to perform tracheal intubation and intravenous injections of medications for cardiac arrest. All incoming calls for EMS were processed by a central dispatch centre. For cases originating from the catchment areas where ALS services were available, ALS was activated in addition to BLS-D when predetermined ALS dispatch criteria were met.
Study design and data collection
The study protocol was approved by the Institutional Review Board of the National Taiwan University Hospital. Through testing the performance of the ALS-TOR and BLS-TOR rules in the three subgroups (ie, OHCAs resuscitated by ALS level, by BLS levels or mixed levels of ALS and BLS response together), the study intended to determine whether the BLS-TOR rule has the best accuracy among all subgroups and whether it can be applied as the universal criteria in our community configured with two different tiers of prehospital life support team.
Registered data of all adult (≥18 years) OHCA that activated EMS from 1 January 2008 through 31 December 2009 were included in the study. Patients with traumatic injuries and for whom resuscitation were not attempted by EMS personnel due to obvious death or an existing do-not-attempt-resuscitation (DNAR) orders were excluded from final analysis.
Test criteria, definition of outcome, accuracy and prediction performance
Tested criteria for the ALS-TOR rule were (1) arrest was not witnessed, (2) no bystander CPR was provided, (3) no ROSC after full ALS care in the field and (4) no AED shocks were delivered; tested criteria for the BLS-TOR rule were (1) arrest was not witnessed, (2) no ROSC and (3) no AED shocks were delivered.4 Cases were categorised as test-positive if they met all relevant criteria.
The predicted outcome was death, including death in the emergency department or after admission to the hospital. According to the study design, we separated all enrolled OHCA cases into three subgroups. The diagnostic accuracy, including sensitivity, specificity, PPV and negative predictive value, for the TOR rules among various provider combinations was evaluated. Systemic effects of the TOR rules on EMS were evaluated by PPV for death (ie, within-group number of death divided by the within-group number of test-positive) and by the decreased transport rate (DTR) to the hospital (ie, within-group number of test-positive divided by the within-group number of all resuscitated OHCAs). These two indexes were chosen to evaluate the systemic effect of the TOR rules because the PPV is an indication of patient safety, while DTR indicates the effect of the TOR rules on system efficiency.
Statistical analysis
Data were entered in Excel (Microsoft, Redmond, Washington, USA), subsequently processed and analysed by SAS software V.9.2 (SAS Institute, Cary, North Carolina, USA). Descriptive statistics of the population were given as counts, percentages, mean±SD or median and IQR. We used t test and Mann– Whitney rank sum test to compare the differences as appropriate. The sensitivity, specificity, PPV, negative predictive values and 95% CIs were calculated. A two-tailed p value <0.05 was considered significant.
Results
From 1 January 2008 to 31 December 2009, there were 5525 OHCA cases managed by the Taipei EMS. The flow of patients enrolled and divided is shown in figure 1. In total, 2006 patients without transport to the hospital due to obvious death or request of DNAR (n=1534), traumatic death (n=386), paediatric cases (n=32) and missing outcome (n=84) were excluded; thus 3489 cases were included in the final analyses. The cases were divided into three provider combination subgroups: resuscitated by ALS-level EMTs (n=240), by BLS-level EMTs (n=1727) and by mixed-level EMTs (n=1522) to test the accuracy of the ALS-TOR and BLS-TOR rules, respectively.
Figure 1.
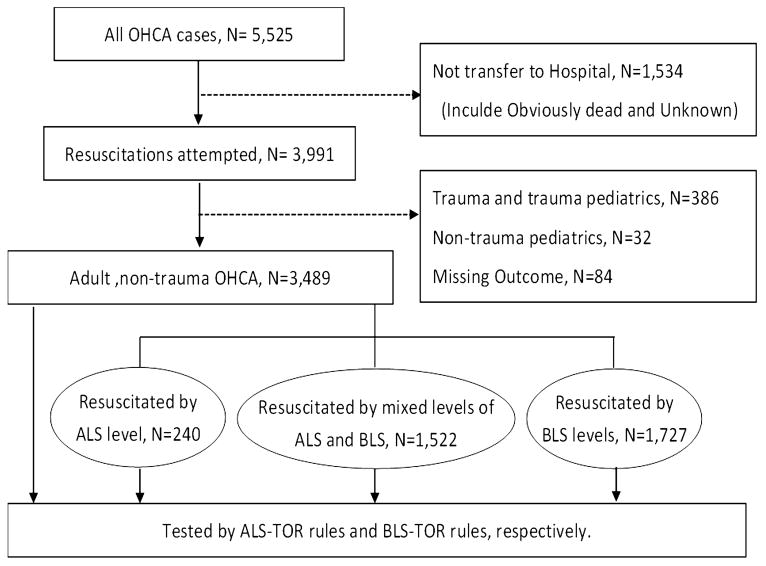
Patient flow and study design.
Demographic data and of enrolled OHCAs in final analyses are tabulated in table 1. Patients' ages, EMS timeliness and distribution of predictors of the TOR rules were different among the three subgroups. Overall survival to hospital discharge was 197 patients (5.6%). Although there was a trend of higher survival rate in those receiving ALS services in terms of sustained ROSC longer than 2 h, survival to discharge and favourable neurological outcome were defined as cerebral performance categories (CPC) scale 1 and 2 . This was compatible with our previous study regards ALS-resuscitated outcomes of OHCAs in Taipei.14
Table 1. Demographic data of OHCA patients responded by different EMS levels.
| Characteristics | All | ALS response | Mixed-level response | BLS response | p Value |
|---|---|---|---|---|---|
| Patients | 3489 | 240 | 1522 | 1727 | |
| Age, year (mean±SD) | 73.0±16.1 | 71.1±17.1 | 74.0±15.6 | 72.4±16.3 | <0.01 |
| Male sex, no. (%) | 2187 (62.7%) | 144 (60.0%) | 935 (61.4%) | 1108 (64.2%) | 0.19 |
| EMS intervals, min (mean±SD) | |||||
| EMS response time | 6.4±3.3 | 6.5±3.3 | 7.3±3.9 | 5.7±2.4 | <0.01 |
| EMS scene time | 13.1±5.6 | 15.9±5.5 | 13.8±5.8 | 12.0±5.1 | <0.01 |
| EMS transport time | 4.5±2.8 | 3.6±1.9 | 4.3±2.5 | 4.8±3.1 | <0.01 |
| EMS prehospital time | 23.9±6.4 | 25.9±6.3 | 25.4±6.0 | 22.4±6.5 | <0.01 |
| EMS response of ≧8 min, no. (%) | 850 (24.4%) | 59 (24.6%) | 544 (35.7%) | 247 (14.3%) | <0.01 |
| Prediction-rule variables, no. (%) | |||||
| No ROSC before left scene | 3192 (91.5%) | 171 (71.3%) | 1363 (89.6%) | 1658 (96.0%) | <0.01 |
| No shock before left scene (no shock) | 3187 (91.3%) | 210 (87.5%) | 1416 (93.0%) | 1561 (90.4%) | <0.01 |
| Not witnessed (no witness) | 2498 (71.6%) | 157 (65.4%) | 1125 (73.9%) | 1216 (70.4%) | <0.01 |
| No bystander CPR | 2887 (82.7%) | 175 (72.9%) | 1186 (77.9%) | 1526 (88.4%) | <0.01 |
| Patients' outcomes (%) | |||||
| Sustained ROSC (>2 h) | 849 (24.3%) | 82 (34.2%) | 363 (23.9%) | 404 (23.5%) | <0.01 |
| Survival to discharge | 197 (5.6%) | 22 (9.2%) | 76 (5.0%) | 99 (5.7%) | 0.03 |
| CPC 1 and 2 | 124 (3.6%) | 16 (6.7%) | 54 (3.5%) | 54 (3.1%) | 0.02 |
BLS, basic life support; CPC, cerebral performance categories; CPR, cardiopulmonary resuscitation; EMS, emergency medical service; OHCA, out-of-hospital cardiac arrest; ROSC, recovery of spontaneous circulation.
The test characteristics of the TOR rules are tabulated in table 2A–F. Detailed case numbers among various subgroups of provider combination and the calculated sensitivity, specificity, PPVs and negative predictive values of the ALS-TOR and BLS-TOR rules are shown. Among various provider combinations, specificity ranged from 70.7% (BLS-resuscitated OHCAs tested by the BLS-TOR rule) to 81.8% (ALS-resuscitated OHCAs tested by the ALS-TOR rule), while the PPVs ranged from 95.1% (ALS-resuscitated OHCAs tested by the ALS-TOR rule) to 98.1% (all OHCAs tested by the BLS-TOR rule). The misclassification rates of survivors with favourable neurological outcome (CPC scale 1 and 2) in those who were predicted to die in every subgroup ranged from 1.34% (mixed-tier-resuscitated OHCAs tested by the BLS-TOR rule) to 3.66% (ALS-resuscitated OHCAs tested by the ALS-TOR rule) among different situations.
Table 2. Test characteristics of the ALS-TOR and BLS-TOR rules among various provider combinations.
| Death | Survival | Sn % (95% CI) | Sp % (95% CI) | PPV % (95% CI) | NPV % (95% CI) | |
|---|---|---|---|---|---|---|
| (A) ALS-TOR rule for OHCAs resuscitated by ALS response | ||||||
| ALS response | ||||||
| ALS-TOR rule | ||||||
| Met 4/4 criteria | 78 | 4 | 35.8 (29.5 to 42.6) | 81.8 (59.0 to 94.0) | 95.1 (87.3 to 98.4) | 11.4 (7.1 to 17.7) |
| Did not meet criteria | 140 | 18 | ||||
| (B) ALS-TOR rule for OHCAs resuscitated by mixed-tier response | ||||||
| Mixed-tier response | ||||||
| ALS-TOR rule | ||||||
| Met 4/4 criteria | 821 | 16 | 56.8 (54.2 to 59.3) | 78.9 (67.8 to 87.1) | 98.1 (96.8 to 98.9) | 8.8 (6.8 to 11.2) |
| Did not meet criteria | 625 | 60 | ||||
| (C) BLS-TOR rule for OHCAs resuscitated by BLS response | ||||||
| BLS response | ||||||
| BLS-TOR rule | ||||||
| Met 3/3 criteria | 1051 | 29 | 64.6 (62.2 to 66.9) | 70.7 (60.6 to 79.2) | 97.3 (96.1 to 98.2) | 10.8 (8.6 to 13.5) |
| Did not meet criteria | 577 | 70 | ||||
| (D) BLS-TOR rule for OHCAs resuscitated by mixed-tier response | ||||||
| Mixed-tier response | ||||||
| BLS-TOR rule | ||||||
| Met 3/3 criteria | 954 | 18 | 66.0 (63.5 to 68.4) | 76.3 (64.9 to 85.0) | 98.1 (97.0 to 98.9) | 10.5 (8.2 to 13.5) |
| Did not meet criteria | 492 | 58 | ||||
| (E) ALS-TOR rule tested for all enrolled OHCAs | ||||||
| All enrolled OHCAs | ||||||
| ALS-TOR rule | ||||||
| Met 4/4 criteria | 1896 | 48 | 57.6 (55.8 to 59.3) | 75.6 (68.9 to 81.3) | 97.5 (96.7 to 98.2) | 9.6 (8.2 to 11.3) |
| Did not meet criteria | 1396 | 149 | ||||
| (F) BLS-TOR rule tested for all enrolled OHCAs | ||||||
| All enrolled OHCAs | ||||||
| BLS-TOR rule | ||||||
| Met 3/3 criteria | 2105 | 51 | 63.9 (62.3 to 65.6) | 74.1 (67.3 to 80.0) | 97.6 (96.9 to 98.2) | 10.1 (9.4 to 12.8) |
| Did not meet criteria | 1187 | 146 | ||||
Death: pronounced dead in the emergency department and died after admission to the hospital.
Survival: survival to hospital discharge.
ALS, advanced life support; BLS, basic life support; NPV, negative predictive value; OHCA, out-of-hospital cardiac arrest; PPV, positive predictive value; Sn, sensitivity; Sp, specificity; TOR, termination of resuscitation.
Systemic effects of the ALS-TOR and BLS-TOR rules regarding PPV and DTR among all enrolled OHCAs in prespecified subgroups are presented in table 3. The DTR values (the higher the better for system efficiency) ranged from 34.2% (ALS-resuscitated OHCAs tested by the ALS-TOR rule) to 63.9% (all OHCAs tested by the BLS-TOR rule). When compared with the ALS-TOR rule, the BLS-TOR rule had a better performance both on PPV and DTR under all provider combinations. However, among all subgroups, none of the PPV values could achieve 99% (ie, <1% missed prediction).
Table 3. Systemic effects of the ALS-TOR and BLS-TOR rules on EMS among various provider combinations.
| Subgroups | ALS-TOR rule | BLS-TOR rule |
|---|---|---|
| 1. OHCAs resuscitated by ALS response (n=240) | PPV*=95.1 (87.3–98.4) | PPV=96.2 (89.9–98.8) |
| DTR†=34.2 (28.3–40.6) | DTR=43.3 (37.0–49.9) | |
| 2. OHCAs resuscitated by BLS response (n=1727) | PPV=97.3 (96.0–98.1) | PPV=97.3 (96.1–98.2) |
| DTR=59.4 (57.0–61.7) | DTR=62.5 (60.2–64.8) | |
| 3. OHCAs resuscitated by mixed-tier response (n=1522) | PPV=98.1 (96.8–98.9) | PPV=98.1 (97.0–98.9) |
| DTR=55.0 (52.5–57.5) | DTR=63.9 (61.4–66.3) | |
| 4. All enrolled OHCAs (n=3489) | PPV=97.5 (96.7–98.2) | PPV=97.6 (96.9–98.2) |
| DTR=55.7 (57.1–57.4) | DTR=61.8 (60.2–63.4) |
Please see the ‘Method’ section for the definition of PPV and DTR.
PPV, positive predictive value; having effect on patient safety.
DTR: decreased transport rate; having effect on system efficiency.
ALS, advanced life support; BLS, basic life support; EMS, emergency medical service; OHCA, out-of-hospital cardiac arrest; TOC, termination of resuscitation.
Discussion
There were two major findings in this study. First, application of the ALS-TOR and BLS-TOR rules reduced unnecessary transport rates, ranging from 34.2% to 63.9% on various provider and rule combinations. However, 1.9–4.9% of those who survived would have been misclassified as non-survivors. This differs significantly from previous studies done in Western countries in that the misclassification rate was never higher than 1%. Second, the BLS-TOR rule demonstrated better performance regarding PPV for non-survivors and DTR for unnecessary transport among all subgroups compared with the ALS-TOR rule. Implementation of the BLS-TOR rule as the universal criteria in a mixed-tier EMS area would therefore be more reasonable.
Both system efficiency and patient safety should be considered equally before implementation of the TOR rule. Our study found that field termination would reduce unnecessary transport to the hospital by 34.2–55.0% with the ALS-TOR rule for those resuscitated by ALS-only or mixed-tier response, and 62.5– 63.9% with the BLS-TOR rule for those resuscitated by BLS-only or mixed-tier response. These findings were compatible with previous validation by data of Resuscitation Outcome Consortium (ROC), which showed a reduction in unnecessary transport to the hospital by 54.4% with the BLS-TOR rule and 31% with the ALS-TOR rule5 and indicated that the TOR rules can significantly improve system efficiency. For those who received mixed-tier response, the BLS-TOR rule, compared with the ALS-TOR rule, had higher increment of system efficiency (DTR for unnecessary transport 63.9% vs 55.0%) without impairing patient safety (equal PPV for non-survivor 98.1%). The results supported the BLS-TOR rule as the universal criteria in a mixed-tier EMS area to reduce confusion in an already challenging prehospital environment.5
The misclassification rates of the TOR rules were higher than 1% in all provider combinations in this study. None of them achieved the standard in general principle of medical futility, that is, less than 1% chance of survival of a given treatment.15 The result was inconsistent with studies carried out in North American and European sites, which stated the TOR rules with misclassified rate from 0% to 0.5%,5,6,8,10 with the best results both specificity and PPV reaching 100% in the Cardiac Arrest Registry to Enhance Survival (CARES) database.8 There are two possible reasons for the discrepancies. First, the high tertiary hospital density in Taipei might have an influence on the predictability of OHCAs outcome. Those who would have met the criteria for TOR rules and predicted “dead” may have instead been salvaged. There are 18 base hospitals as EMS destinations in Taipei, with a short transport time (4.5±2.8 min in this study), of which 7 are tertiary hospitals with ALS technique such as extracorporeal membrane oxygenation (ECMO).11 Local observation in Taiwan and data from Japan demonstrated increase in neurologically favourable survival when patients without field ROSC were transported to a tertiary care hospital.16
Second, there may have been selection bias within our cohort for analysis. Although regulations in Taiwan did not allow EMTs to pronounce death of OHCA patients at the field, there are some anecdotes that families chose not to transport the patient if the patient was very old or was in long-term bedridden status even without a documented DNAR order. If the OHCA patients were not transported to the hospital, they were not included in the final analyses. In this study, 27.8% (1534/5525) OHCAs did not receive attempts of resuscitation or received just a very brief resuscitation before the families decided to give up, leading to a lot of reduction of test-positive non-survivors in our predictive matrix. However, even if we assumed that all the 1534 cases were not transported to the hospital due to selection bias, the misclassification rates of all OHCAs were still higher than 1% (recalculated PPV: 98.6 (95% CI 98.1 to 98.9) with both ALS-TOR and BLS-TOR rules). In one study, delayed or token resuscitative efforts were self-reported by paramedics to occur in 27% of OHCAs.17 To avoid this, we made changes in education of EMTs, stipulation of protocols and requested registry system for causes of non-transport.
In comparison to previous validation studies, our study provided additional knowledge and insight on implementation of TOR rules in several aspects. First, we confirmed that the BLS-TOR rule provided better accuracy not only in BLS response or mixed-tier response but also in ALS response EMS. Previous validation studies tested the TOR rules in OHCA cases resuscitated (1) by BLS response or (2) by mixed-tier response,5 8 10 13 and identified the BLS-TOR rule as the universal criteria. Because of geographic distribution of ambulance stations in Taipei, we also had OHCA cases resuscitated by ALS response only. Through the subgroup analyses based on different provider combinations in our study, we found that the BLS-TOR rule invariably provides better predictive performance even for those resuscitated by ALS response only, thereby offering supplementary evidence for the suggestions in the latest resuscitation guidelines4: use of the three BLS-TOR criteria as a universal TOR rule for EMS systems staffed by any level of provider.
Second, we identified regional differences in the application of TOR rules, especially for those areas with lower rates of presenting shockable rhythm in a prehospital setting. Among previous large-scale validation studies, the shockable rhythm (ie, VF/VT) rates were different (Ontario 30%,10 ROC 30%,5 CARES 23.6%,8 Japan 11.1%13 and Taiwan 8.7% in this study). The misclassified rates by the TOR criteria were greater than 1% in Japan and in our current report (Japan 1%13 and Taiwan 2.4%; others 0–0.5%), paralleling the lower VF/VT rates. The reasons leading to such observation are not certain. The proportion of survival to discharge was similar in various validation studies (Ontario 3%,10 ROC 5.4%,5 CARES 7.1%,8 Japan 5.1% (surrogated by 1-month survival rate)13 and Taiwan 5.6% in this study). Given the similar overall survival and assumption of better survival for shockable rhythms versus non-shockable rhythms, we could infer that patients with non-shockable rhythms who would have been predicted dead by the current TOR rules derived from Western community survived in our community, which leads to lower accuracy of the TOR rules in this subgroup.
Finally, we suggest examining the TOR rules at a regular time interval. Of course, it is necessary to set up TOR rules for a prehospital setting to balance road hazards, system efficiency and in-hospital cost for futile resuscitation.2,3,15,18 However, the TOR rules were derived mainly from 1986 to 2002,19–22 without considering new postresuscitation care in the past decade, including therapeutic hypothermia and ECMO.23 Relevant validation studies of the TOR rules also seldom put the transport time, hospital characteristics and ethnic variation into consideration. Moreover, new evidence indicates that some population (ie, females of childbearing age), even being found with poorer prognostic arrest characteristics such as presenting non-shockable rhythms, were still associated with increased odds of survival.24 Considering new evidence in examining the accuracy of the TOR rules regularly may guarantee patient safety.
Limitation
There are two limitations to this study. First, our data could not fulfil with the request of three-round CPR/AED analysis by BLS or at least 20 min resuscitation by ALS before the determination of TOR or transport suggested by the National Association of EMS Physician in North America.25 The average scene time in this study was 13.1±5.6 min. This reflected EMS protocols in Taiwan that stipulate BLS teams to perform only two cycles of 30:2 CPR and rhythm analysis and ALS teams to perform additional ALS intervention prior to transport. EMTs seldom were at the field for resuscitation longer than 20 min in Asian communities.12,13 Second, we do not have the records of postresuscitation hospital care in the original database, which might have a positive influence on survival. Further prospective validations, including records of these variables, should be considered.
Conclusion
In this validation study, the ALS-TOE and BLS-TOR rules performed well in decreasing unnecessary transport of OHCA patients in an Asian metropolitan city, with the BLS-TOR rule having a better performance compared with the ALS-TOR rule under all provider combinations in an area with a mixed-tier response EMS system. However, because greater than 1% of those living will be misclassified as non-survivors by the current TOR rules, implementation in this community or in other areas with similar characteristics should be done with caution.
Acknowledgments
We appreciate the administrative support provided by the Taipei City Fire Department and Taipei City Health Department for the development and implementation of the web-based Utstein-style OHCA registry.
Contributors W-CC, AMC, M-SL and MH-MM planned and conducted the study. W-CC wrote the majority of the article. PC-IK helped collect data. SS-HL, H-CW, C-WY, M-JH and S-YC provided important suggestions on preparation of the manuscript.
Funding The research was funded by the National Science Council of Taiwan (NSC 99-2314-B-002-135-MY3). AMC was supported by Award Number 1K12HL108974-01 from the National Heart, Lung, and Blood Institute, USA.
Footnotes
Competing interests: None.
Ethics approval: Institutional Review Board of the National Taiwan University Hospital.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Lloyd-Jones D, Adams RJ, Brown TM, et al. Heart disease and stroke statistics– 2010 update: a report from the American Heart Association. Circulation. 2010;121:e46–215. doi: 10.1161/CIRCULATIONAHA.109.192667. [DOI] [PubMed] [Google Scholar]
- 2.Rosamond W, Flegal K, Furie K, et al. Heart disease and stroke statistics—2008 update: a report from the American Heart Association Statistics Committee and Stroke Statistics Subcommittee. Circulation. 2008;117:e25–146. doi: 10.1161/CIRCULATIONAHA.107.187998. [DOI] [PubMed] [Google Scholar]
- 3.Slattery DE, Silver A. The hazards of providing care in emergency vehicles: an opportunity for reform. Prehosp Emerg Care. 2009;13:388–97. doi: 10.1080/10903120802706104. [DOI] [PubMed] [Google Scholar]
- 4.Morrison LJ, Kierzek G, Diekema DS, et al. Part 3: ethics: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S665–75. doi: 10.1161/CIRCULATIONAHA.110.970905. [DOI] [PubMed] [Google Scholar]
- 5.Morrison LJ, Verbeek PR, Zhan C, et al. Validation of a universal prehospital termination of resuscitation clinical prediction rule for advanced and basic life support providers. Resuscitation. 2009;80:324–8. doi: 10.1016/j.resuscitation.2008.11.014. [DOI] [PubMed] [Google Scholar]
- 6.Ong ME, Jaffey J, Stiell I, et al. Comparison of termination-of-resuscitation guidelines for basic life support: defibrillator providers in out-of-hospital cardiac arrest. Ann Emerg Med. 2006;47:337–43. doi: 10.1016/j.annemergmed.2005.05.012. [DOI] [PubMed] [Google Scholar]
- 7.Richman PB, Vadeboncoeur TF, Chikani V, et al. Independent evaluation of an out-of-hospital termination of resuscitation (TOR) clinical decision rule. Acad Emerg Med. 2008;15:517–21. doi: 10.1111/j.1553-2712.2008.00110.x. [DOI] [PubMed] [Google Scholar]
- 8.Sasson C, Hegg AJ, Macy M, et al. Prehospital termination of resuscitation in cases of refractory out-of-hospital cardiac arrest. JAMA. 2008;300:1432–8. doi: 10.1001/jama.300.12.1432. [DOI] [PubMed] [Google Scholar]
- 9.Skrifvars MB, Vayrynen T, Kuisma M, et al. Comparison of Helsinki and European Resuscitation Council “do not attempt to resuscitate” guidelines, and a termination of resuscitation clinical prediction rule for out-of-hospital cardiac arrest patients found in asystole or pulseless electrical activity. Resuscitation. 2010;81:679–84. doi: 10.1016/j.resuscitation.2010.01.033. [DOI] [PubMed] [Google Scholar]
- 10.Morrison LJ, Visentin LM, Kiss A, et al. Validation of a rule for termination of resuscitation in out-of-hospital cardiac arrest. N Engl J Med. 2006;355:478–87. doi: 10.1056/NEJMoa052620. [DOI] [PubMed] [Google Scholar]
- 11.Chiang WC, Ko PC, Wang HC, et al. EMS in Taiwan: past, present, and future. Resuscitation. 2009;80:9–13. doi: 10.1016/j.resuscitation.2008.10.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ong ME, Shin SD, Tanaka H, et al. Pan-Asian Resuscitation Outcomes Study (PAROS): rationale, methodology, and implementation. Acad Emerg Med. 2011;18:890–7. doi: 10.1111/j.1553-2712.2011.01132.x. [DOI] [PubMed] [Google Scholar]
- 13.Kajino K, Kitamura T, Iwami T, et al. Current termination of resuscitation (TOR) guidelines predict neurologically favorable outcome in Japan. Resuscitation. 2013;84:54–9. doi: 10.1016/j.resuscitation.2012.05.027. [DOI] [PubMed] [Google Scholar]
- 14.Ma MH, Chiang WC, Ko PC, et al. A randomized trial of compression first or analyze first strategies in patients with out-of-hospital cardiac arrest: results from an Asian community. Resuscitation. 2012;83:806–12. doi: 10.1016/j.resuscitation.2012.01.009. [DOI] [PubMed] [Google Scholar]
- 15.Schneiderman LJ, Jecker NS, Jonsen AR. Medical futility: its meaning and ethical implications. Ann Intern Med. 1990;112:949–54. doi: 10.7326/0003-4819-112-12-949. [DOI] [PubMed] [Google Scholar]
- 16.Kajino K, Iwami T, Daya M, et al. Impact of transport to critical care medical centers on outcomes after out-of-hospital cardiac arrest. Resuscitation. 2010;81:549–54. doi: 10.1016/j.resuscitation.2010.02.008. [DOI] [PubMed] [Google Scholar]
- 17.Sherbino J, Guru V, Verbeek PR, et al. Prehospital emergency medical services. CJEM. 2000;2:246–51. [PubMed] [Google Scholar]
- 18.Suchard JR, Fenton FR, Powers RD. Medicare expenditures on unsuccessful out-of-hospital resuscitations. J Emerg Med. 1999;17:801–5. doi: 10.1016/s0736-4679(99)00086-4. [DOI] [PubMed] [Google Scholar]
- 19.Aprahamian C, Thompson BM, Gruchow HW, et al. Decision making in prehospital sudden cardiac arrest. Ann Emerg Med. 1986;15:445–9. doi: 10.1016/s0196-0644(86)80185-8. [DOI] [PubMed] [Google Scholar]
- 20.Bonnin MJ, Pepe PE, Kimball KT, et al. Distinct criteria for termination of resuscitation in the out-of-hospital setting. JAMA. 1993;270:1457–62. [PubMed] [Google Scholar]
- 21.Verbeek PR, Vermeulen MJ, Ali FH, et al. Derivation of a termination-of-resuscitation guideline for emergency medical technicians using automated external defibrillators. Acad Emerg Med. 2002;9:671–8. doi: 10.1111/j.1553-2712.2002.tb02144.x. [DOI] [PubMed] [Google Scholar]
- 22.Marsden AK, Ng GA, Dalziel K, et al. When is it futile for ambulance personnel to initiate cardiopulmonary resuscitation? BMJ. 1995;311:49–51. doi: 10.1136/bmj.311.6996.49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Peberdy MA, Callaway CW, Neumar RW, et al. Part 9: post-cardiac arrest care: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2010;122:S768–86. doi: 10.1161/CIRCULATIONAHA.110.971002. [DOI] [PubMed] [Google Scholar]
- 24.Johnson MA, Haukoos JS, Larabee TM, et al. Females of childbearing age have a survival benefit after out-of-hospital cardiac arrest. Resuscitation. 2013;84:639–44. doi: 10.1016/j.resuscitation.2012.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bailey ED, Wydro GC, Cone DC. Termination of resuscitation in the prehospital setting for adult patients suffering nontraumatic cardiac arrest. National Association of EMS Physicians Standards and Clinical Practice Committee. Prehosp Emerg Care. 2000;4:190–5. doi: 10.1080/10903120090941498. [DOI] [PubMed] [Google Scholar]


