Abstract
Neuromodulation shows increasing promise in the treatment of psychiatric disorders, particularly obsessive–compulsive disorder (OCD). Development of tools and techniques including deep brain stimulation, transcranial magnetic stimulation, and electroconvulsive therapy may yield additional options for patients who fail to respond to standard treatments. This article reviews the motivation for and use of these treatments in OCD. We begin with a brief description of the illness followed by discussion of the circuit models thought to underlie the disorder. These circuits provide targets for intervention. Basal ganglia and talamocortical pathophysiology, including cortico-striato-thalamo-cortical loops is a focus of this discussion. Neuroimaging findings and historical treatments that led to the use of neuromodulation for OCD are presented. We then present evidence from neuromodulation studies using deep brain stimulation, electroconvulsive therapy, and transcranial magnetic stimulation, with targets including nucleus accumbens, subthalamic nucleus inferior thalamic peduncle, dorsolateral prefrontal cortex, supplementary motor area, and orbitofrontal cortex. Finally, we explore potential future neuromodulation approaches that may further refine and improve treatment.
Electronic supplementary material
The online version of this article (doi:10.1007/s13311-014-0287-9) contains supplementary material, which is available to authorized users.
Keywords: Obsessive–compulsive disorder (OCD), Deep brain stimulation (DBS), Electroconvulsive therapy (ECT), Transcranial magnetic stimulation (TMS), Neuromodulation
Introduction: Obsessive–Compulsive Disorder
Obsessive–compulsive disorder (OCD) is a potentially disabling disorder and a leading cause of morbidity worldwide that occurs in approximately 1–3% of the population [1, 2]. This disorder is characterized by obsessions and compulsions [3]. Obsessions, which include persistent, distressing thoughts, images, or impulses that affected people generally recognize as products of their own minds, cause substantial anxiety and distress. Patients with OCD attempt to neutralize the anxiety and discomfort from the obsessions with compulsions, repetitive behaviors intended to reduce or prevent distress and undesirable situations or events. Recent changes in diagnostic criteria have involved reclassification of OCD from being an “anxiety” disorder to a new group of “obsessive–compulsive and related disorders” with a focus on repetitive behaviors [4]. This change is potentially important when considering the underlying neurocircuitry and potential treatments in OCD.
Unfortunately, inadequate animal models for OCD limit the development of therapeutics. In humans, inadequate pharmacological treatments have motivated circuit-based treatments in refractory patients. These approaches originally focused on ablative surgery, in which a variety of techniques have been used to destroy brain tissue, producing an irreversible lesion. More recently, interest has grown in therapeutic neuromodulation, where electricity is administered to elicit changes in neuronal function. Building on the history of lesion-based neurosurgical treatments in OCD, surgical neuromodulation or electricity delivered by implanted devices, has been used as a favorable alternative to ablative surgery. Less invasive techniques that do not require surgery, including currents applied to the scalp and magnetic fields, have also been investigated as potential treatments for OCD.
Neurocircuitry of OCD
Circuit Models
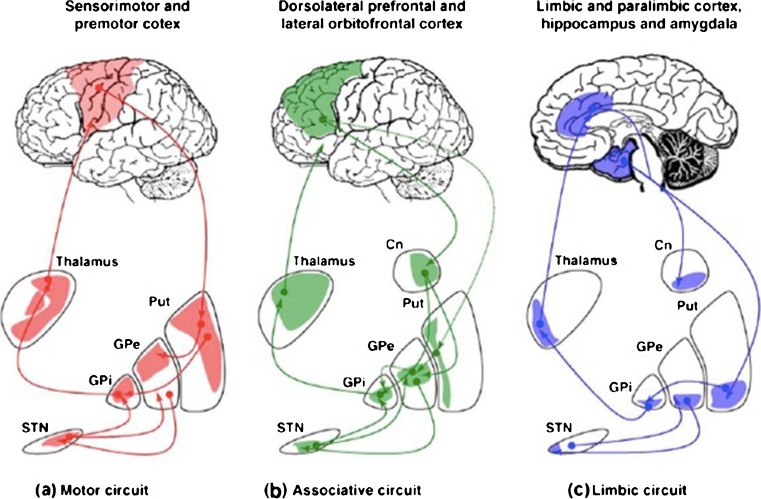
Following decades of research, the neurocircuitry of OCD remains a topic of active investigation. Cortico-striato-thalamo-cortical (CSTC) loops have been implicated in the pathophysiology of a variety of psychiatric symptoms (Fig. 1). The development of Parkinsonism in abusers of 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine provided early evidence for the importance of these loops [5, 6]. Based on evidence from labeling, lesion, and single-cell recording studies, in the mid-1980s Alexander et al. [7] proposed at least 5 parallel but functionally segregated basal ganglia-thalamocortical circuits. While additional data has led to revision of the model of Alexander et al. [7], including less segregated loops and additional brain regions, it remains conceptually important [8]. In this model, the cortical areas involved determine the names of the circuits, and each circuit functions independently to facilitate unique physiological functions. These circuits remain distinct through the basal ganglia and have individual cortical projections via both “direct” and “indirect” pathways [9]. The “direct” pathway includes two excitatory and two inhibitory connections, forming a positive feedback loop in which cortical activity disinhibits the thalamus to activate the cortex. Because the “indirect” pathway has one excitatory and three inhibitory connections, cortical activity results in inhibition of both thalamus and cortex; therefore, the pathway functions as a negative feedback loop. The “motor” circuit hinges primarily on the putamen, which receives projections from the motor and somatosensory cortices. The putamen projects reciprocally to the cortex and also to the globus pallidus and substantia nigra, which, in turn, project to the thalamus. Other loops include “oculomotor”, “dorsolateral prefrontal”, “lateral orbitofrontal”, and “anterior cingulate” cortices.
Fig. 1.
Neurocircuitry: cortico-striato-thalamocortical loops. Pathways in motor, associative, and limbic circuitry. (a) Motor circuit. Neurons from the sensorimotor cortex project to the posterolateral putamen (Put), which, in turn, projects to the posterolateral region of the target nuclei: (i) the direct circuit to the globus pallidus pars interna (GPi) and (ii) the indirect circuit connecting the posterior putamen (Put) to the globus pallidus pars externa (GPe), the subthalamic nucleus (STN) and the GPi. The GPi is the primary output nucleus of the basal ganglia to the cortex via the ventrolateral thalamus. (b) Associative circuit. This circuit originates in the dorsolateral prefrontal and lateral orbitofrontal cortices; projections include the striatal caudate nucleus (Cn) and anteromedial portion of the Put, and subsequently projections to the dorsomedial region of the GPi, and anteromedial portions of the GPe and STN. These, in turn, project onto the GPi and back to the cortex via the ventral anterior nuclei of the thalamus. (c) Limbic circuit. Here, the hippocampus, amygdala, paralimbic and limbic cortices project to the ventral striatum (ventral portion of the caudate and putamen, including nucleus accumbens). The ventral striatum projects to the limbic portion of the GPe, medioventral STN, ventral GPi, and to the cortex via the mediodorsal nucleus of the thalamus. Reproduced with permission from Krack et al. [10]
The model of Alexander et al. [7] contributed to the development of surgical neuromodulatory interventions for Parkinson’s disease, and has supported the use of surgical interventions in OCD. In OCD, CSTC functions have been strongly implicated to mediate symptoms and treatment response. Evidence suggesting that pharmacological treatments reduce caudate hypermetabolism when they improve symptoms indicates the importance of the dysregulation of this circuit in OCD [11]. Several additional lines of evidence support CSTC involvement in this disorder. Common features and neural substrates are shared between OCD and movement disorders; neuronal areas involved in motor function have been implicated in OCD pathogenesis since early observations of the illness. Tourette’s disorder, associated with both motor tics and OCD-like symptoms, supports the idea that a single neural substrate can produce both motor and psychiatric illness. Tourette’s and OCD exhibit significant comorbidity and genetic associations, highlighting the etiological importance of the basal ganglia in OCD symptoms [12–14]. Basal ganglia circuit dysfunction is thought to play a role in the generation of both motor and OCD symptoms in Tourette’s syndrome [15, 16].
The efficacy of serotonergic pharmacotherapies [e.g., selective serotonin reuptake inhibitors (SSRIs)] also supports a role for CSTC loops in the pathogenesis of OCD [17]. High levels of 5-hydroxytryptamine receptor 2A and 5-hydroxytryptamine receptor 2C expression in the striatum offer a mechanism by which serotonergic agents could influence CSTC circuit function [18]. Other neurotransmitters in CSTC circuits are also likely to influence OCD susceptibility, chronicity, severity, and treatment response. Dopaminergic dysfunction has been particularly implicated [19]. Higher basal ganglia dopamine transporter binding ratios have been reported in OCD [20], and decreased caudate D2 binding [21], suggesting alterations of synaptic dopamine in the basal ganglia.
Other CSTC neurotransmitter systems that may have pathophysiological importance include glutatmate, substance P, acetylcholine, and endogenous opioids [22]. Of these, glutamate dysfunction has been most strongly suggested. Magnetic resonance spectroscopy has identified abnormalities of caudate glutamate in patients with OCD, and SSRI treatment corrects these abnormalities [23]. These measurements include both intracellular and synaptic glutamate, and are consistent with increased caudate activity previously reported in OCD. Gene linkage analyses of patients with OCD and their families also support a pathophysiological role for glutamate [24–27]. Also, preliminary evidence suggests that glutamatergic agents such as riluzole and ketamine may be useful in OCD [28–31].
It is clear that no single anatomic or physiological defect will likely be identified to be responsible for the pathogenesis of complex psychiatric symptoms (e.g., decreased dopamine in PD). More likely, OCD symptoms may involve multiple neural circuits. A systems-based approach is critical in assessing the clinical data to identify targets for neuromodulation. The multicircuit model hypothesizes that the primary pathogenic mechanism is dysregulation of the basal ganglia/limbic striatal circuits that modulate neuronal activity in and between the orbitofrontal and anterior cingulate cortex (ACC), as well as the medial, dorsomedial (DM), and anterior thalamic nuclei [32]. This neuronal model of OCD includes 3 components. The first involves a reciprocal positive feedback loop between the orbital (OFC) and prefrontal cortex (PFC) and the DM thalamic nucleus, via the anterior limb of the internal capsule. The corticothalamic projection is excitatory and mediated primarily by glutamate and aspartate. The reciprocal thalamocortical pathway’s neurotransmitter is also thought to be excitatory, and likely glutamatergic [32, 33].
The second component of this model involves the OFC/PFC, the ventral caudate, the DM pallidum, and the intralaminar, anterior, and DM thalamic nuclei [7]. Projections from the ventral striatum to the DM pallidum use multiple transmitters. However, the output of this pathway from the DM pallidum to the thalamus is primarily inhibitory and gamma-aminobutyric acid (GABA)-mediated [34, 35]. The GABAergic inhibition is thought to modulate the excitatory positive feedback loop described above. The importance of dopamine and glutamate in this pathway has also been demonstrated [36], and inhibitory serotonergic projections from midbrain dorsal raphe nuclei to the striatum are also involved in this model [37, 38].
The third component involves the limbic system and the Papez circuit. In 1937, Papez [39] proposed that cerebral cortical activity is essential for emotional experience and that emotional expression relies on the integrative action of the hypothalamus. Papez created a model to connect these structures based on his neuroanatomic observations. This connects the hippocampal formation to the mammillary body, which projects via the mammilothalamic tract to the anterior thalamic nuclei; this then connects to the cingulate gyrus. In the OCD model discussed previously, the DM nuclei and orbitofrontal cortex connect extensively to the Papez circuit. Also, ACC projections to the nucleus accumbens (NAc) may mediate some of the emotional and anxiety components of OCD.
Functional Neuroimaging in OCD
Over the last several decades, neuroimaging techniques, such as functional magnetic resonance imaging (fMRI) and positron emission tomography (PET), have been used to investigate neurocircuit functioning in OCD; these studies provide further support for pathophysiological circuit models. A role for CSTC loops in OCD has been suggested in both neutral (i.e., the baseline obsessional thoughts and compulsive behaviors of patients with OCD) and provoked (i.e., following presentation of a stimulus that exacerbates the patient’s symptoms) states. PET and fMRI studies have shown that effective treatments, including medications such as SSRIs and behavioral therapy, correct the abnormally increased metabolism seen in these areas [40, 41]. Endogenous activation patterns also respond following surgical neuromodulatory treatments, suggesting that efficacy is associated with metabolic normalization [42].
Neuromodulatory Approaches
Deep Brain Stimulation
Understanding of circuit and node dysfunction in OCD suggests targets and approaches for intervention. Neurosurgical stimulation initially targeted sites where lesioning or ablative surgery suggested efficacy, though, clearly, neuromodulation has significant advantages over ablative treatments. Stimulation can be adjusted and reversed, while blinding in clinical trials is facilitated by the ability to switch stimulation on or off without the patient’s awareness. Still, DBS treatment has risks, including the induction of hypomania, so frequent follow-up is required. Importantly, DBS involves neurosurgical intervention with craniotomy, and associated risks include infection, hemorrhage, and edema, which can lead to transient or permanent neurological sequelae, or even death.
Early attempts to treat OCD symptoms using deep-brain stimulation (DBS) often suffered from the lack of stringent selection criteria, rigorous assessments, and optimal imaging. Such studies may have limited value for assessing efficacy, but can help guide future investigations. In 1979, low-frequency (5 Hz) bilateral mediothalamic DBS was used for control of phobias [43]. This ameliorated phobias and obsessional symptoms at 1-year follow-up. Also in the 1970s, cerebellar vermis stimulation was the first procedure to use a network approach rather than addressing a particular “target”; it was designed to upregulate septal activity while downregulating amygdala activity. At least a moderate response was reported in 5/5 obsessional patients after 2.5 years [43]. Stimulation of white matter around the cingulum was associated with emotional responses following early trials in 135 patients with a variety of psychiatric diagnoses [44].
Psychiatric and cognitive effects of DBS in movement disorder surgery also indicated that modulation of the neural systems underlying psychiatric illness can be accomplished with electrical stimulation. DBS to the subthalamic nucleus (STN), widely used in Parkinson’s disease, can affect limbic, dorsolateral prefrontal, and orbitofrontal loops that all pass through the STN. In addition to affecting motor function, STN stimulation would be expected to alter neuropsychological function [7]. Accordingly, mood and anxiety improvements have been widely noted in patients receiving STN DBS for Parkinson’s disease [45, 46]. The ventromedial and medial portions of the STN, considered associative and limbic areas, may have been involved, though surrounding or communicating structures such as the lateral hypothalamus or ventral tegmental area may also contribute. Stimulation of either of these structures may activate dopaminergic and serotonergic structures related to the medial forebrain bundle, where direct stimulation has been reported to induce feelings of pleasure [47]. STN DBS also reduced obsessive and compulsive symptoms in patients with Parkinson’s disease with a Yale–Brown Obsessive Compulsive Scale (Y-BOCS) decrease from 32 to 1 in one case, and 58% or 64% decreases in 2 others [48, 49].
However, STN DBS has also been associated with exacerbations of psychiatric symptoms, including stimulation-dependent depressive symptoms [50, 51]. Mania, hypomania, anxiety symptoms, and psychosis have also been reported with STN DBS in Parkinson’s patients [52–55]. DBS of the globus pallidus interna has elicited anxiolytic effects [56], and has also been associated with the relief of depressive symptoms in a patient with dyskinesia [57]. Similarly, in patients treated for comorbid Tourette’s disorder, globus pallidus interna DBS resulted in improvement of OCD symptoms.
Although DBS is widely used in movement disorders, fewer studies have been performed primarily in treatment of psychiatric disorders [58, 59]. In OCD, based on a review of 90 published cases, response rates appear to exceed 50% [60]. A meta-analysis including DBS at all sites and targets (n = 64) found heterogeneity but demonstrated an overall significant benefit with an average improvement in score reduction of 2.77 SDs (95% confidence interval 0.648–4.896) [61]. Currently, OCD is the only psychiatric disorder with US Food and Drug Administration status for DBS; this treatment has been granted a Humanitarian Device Exemption.
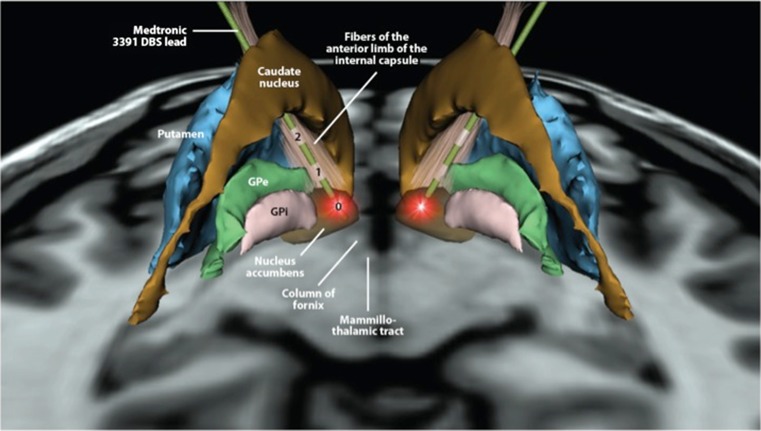
The first reports of DBS treatment primarily for psychiatric conditions, OCD and Tourette’s syndrome, were published in 1999 [62, 63]. Stimulation of the anterior limb of the internal capsule in “targets […] aimed for in capsulotomy” led to symptomatic improvement in 3/4 patients with OCD (Fig. 2). In another case series, 2/3 patients responded with improvements in OCD symptoms following open-label treatment [64]. Another report included efficacy in a single patient with a 79% reduction in scores on the Y-BOCS following 3 months of stimulation [65, 66]. A case of ventral caudate stimulation also led to sustained improvements in OCD symptoms, anxiety, and depression [67, 68]. In 6 severely symptomatic patients with OCD (baseline Y-BOCS > 30) who received double-blinded, bilateral internal capsular stimulation [69], 3/6 patients met the response criteria—a 35% reduction in Y-BOCS. Responders showed reductions in frontal metabolism, assessed by PET, after 3 months of stimulation, and experienced worsening of mood and OCD symptoms when stimulation was turned off. These data were republished in 2008, with additional data from 2 subsequently implanted patients and further follow-up [70]. No infections, deaths, hemorrhages, or significant changes in vegetative signs were reported. Mania was not observed, though disinhibition occurred, which responded to stimulation intensity decreases. Two additional cases also suggested a benefit for depressive symptoms, as well as Y-BOCS improvement [71]. Importantly, in 3 patients, no additional benefit was gained by providing cingulotomy combined with ventral capsule (VC)/ventral striatum (VS) stimulation [72].
Fig. 2.
Three-dimensional illustration of deep brain stimulation (DBS) in ventral capsule/ventral striatum. This model demonstrates leads and brain structures on the axial plane 5 mm below the intercommisural plane as viewed posterior to anterior. The trajectory of the leads follows the anterior limb of the internal capsule. Each lead has 4 contacts, but only 3 are shown (contacts #0, #1, and #2); contact #3 is hidden by the caudate nucleus. The most ventral contact (#0) is active, as represented by red radiating stimulation fields. GPe = globus pallidus externus; GPi = globus pallidus internus. Image courtesy of Kirk Finnis, Ph.D. [Medtronic Inc., USA]
Several international multicenter studies including 18 patients found that DBS to the VC/VS ameliorated OCD symptoms [73–75]. Later implantation dates were associated with greater efficacy, with response rates nearing 80% and a 60% decrease in Y-BOCS score. Depression and anxiety also improved significantly, though these studies included periods of open-label treatment in addition to controlled assessments [76]. Hypomania [77] and contralateral smiles have also been elicited through stimulation at this site, suggesting engagement with the reward circuitry [78]. These acute changes in mood have been found to predict response [79, 80]. Serious adverse events included 2 small hemorrhages without permanent sequelae, seizure managed with phenytoin, wound infection managed with antibiotics, and lead/extension breakage requiring replacement. Psychiatric adverse events occurred with both active and sham stimulation [81]. Functional changes detected using PET included stimulation-induced perfusion increases in ACC, OFC, striatum, pallidum, and thalamus. Similarly, electroencephalography (EEG) suggested dorsolateral PFC (DLPFC) responses to stimulation, and fMRI indicated blood flow changes in caudate, thalamus, and cingulate cortex that were associated with beneficial effects of stimulation in another case [82]. Importantly, stimulation discontinuation following pulse generator failure led to worsening of symptoms and adverse events, though in most cases symptoms still remained improved from baseline [83]. Fewer side effects were reported in open treatment protocols, which also demonstrated efficacy in 8 patients with improvements in symptom severity on the Y-BOCS (approximately 30% and 60%) and the Hamilton Depression Rating Scale [84, 85]. Furthermore, cognitive function has not been reported to decline and may improve following stimulation at this site [86].
The NAc has been targeted by other groups. Though initially considered to be nearby but structurally distinct, further analysis determined that in many patients receiving stimulation targeted to NAc the electrodes providing benefit were actually localized in the ventral anterior limb of the internal capsule (VC) [87]. Reports of open treatments with small numbers of patients (6 in total) suggested benefit in a high proportion of patients following NAc stimulation [88, 89]. In a double-blind, sham-controlled trial of unilateral DBS to the right NAc (n = 10), illness severity, assessed by the Y-BOCS, following active stimulation differed significantly from baseline, but not from sham; only 10% of patients experienced a > 35% reduction in Y-BOCS score, while 40% experienced decreases between 25% and 35% over a 1-year period [90]. However, after 3 years, 4/8 patients experienced a > 35% reduction in Y-BOCS score, while 2 additional patients experienced a reduction of 25–35% [91]. This group also reported fewer serious adverse events, with only transient symptoms of dysesthesia, agitation, anxiety, poor sleep, and suicidal thoughts in 1 patient [90]. Bilateral DBS of the NAc (i.e., 7 mm lateral to the midline, 3 mm anterior to the anterior commissure, and 4 mm inferior to the intercommissural line) produced better results in a study with open-label and sham-controlled phases [92], including response (Y-BOCS score decrease of ≥ 35%) in 9/16 patients and a 25% difference between active and sham treatments. Reported adverse events were relatively mild, and most frequently included hypomania (8 patients), numbness at incision site, or feeling of leads (7 each), and 1 transient wound infection. Impulsivity has also been noted as a side effect in several patients receiving NAc stimulation [93]. A follow-up report demonstrated associations between Y-BOCS score increases following DBS discontinuation and urinary-free cortisol excretion, a measure of hypothalamic–pituitary–adrenal axis activity [94]. Although measures of anxiety and depression also worsened following discontinuation, these did not correlate with changes in cortisol excretion. Recently, long-term open data from 16 patients were reported, and significant changes were noted in quality of life measures [95].
A multicenter 10-month, double-blind, crossover study of STN DBS was performed with 16 patients completing the assessment period [96]. One additional patient in this study developed infection requiring explantation prior to randomization and assessment. Relative to sham, active stimulation resulted in superior outcomes: decreases in symptom severity (>30% mean decrease on the Y-BOCS), and increases in overall function (Clinical Global Impression and Global Assessment of Functioning scores). Because of placement variations, some patients who benefitted in this study were actually stimulated in the internal capsule (n = 4), zona incerta (n = 4), substantia nigra (n = 3), and H2 field of Forel (n = 2). Fifteen serious adverse events were reported, including hemorrhage leading to permanent finger palsy in one patient and 2 infections, along with transient motor and psychiatric symptoms that resolved. Some psychiatric symptoms reported as adverse events also occurred during sham stimulation. A case series of 4 patients (2 from the prior study) reported 3 responders and 1 partial responder with > 60% mean improvement in Y-BOCS score, though side effects were still common [97]. Benefits associated with STN stimulation also correlated with the normalization of cortical hypermetabolism [42]. Also, abnormalities in single-unit neuronal activity were suggested and shown to reflect symptom severity while predicting response to STN DBS [98, 99].
Following DBS to the inferior thalamic peduncle, 5/5 patients were reported to show meaningful response with mean a Y-BOCS score reduction of approximately 50% [100]. An open follow-up including patients with psychiatric comorbidities (substance use disorders) found improvements in OCD symptoms in 6/6 patients at 12 months with mean a Y-BOCS score improvement of > 50% [101].
Electroconvulsive Therapy
Electroconvulsive therapy (ECT) has a significantly lower risk profile than DBS, though it requires general anesthesia and has side effects, including memory loss. For many decades, there has been inconsistency in reports and interpretation of data regarding the efficacy of ECT in OCD treatment. One early report included retrospective assessments of 31 patients with obsessional disorder who received ECT; 16 of these were improved at follow-up, though 10 stated that they thought ECT was not responsible for their improvement, including 1 who reported being worse following ECT, but subsequently improved [102]. Because only 3 of these patients “positively stated the [ECT] had helped them”, the authors concluded that ECT was not appropriate for treating “obsessional states” without comorbid depression. Others reported that more than two thirds of patients with severe OCD but without major affective disorder referred to their clinic had been treated with ECT; without presenting data on these cases, the authors state that limited published reports of benefit in patients with OCD receiving ECT suggests that the treatment is inappropriate for this condition [103]. In contrast, another early report in patients with symptoms resembling OCD, obsessional neurosis, who had been refractory to standard treatments, included a response rate of approximately 40% in 80 patients following treatment with ECT combined with medication treatment seeking to increase sleep (narcosis) and antidepressants [104]; these authors argued that this technique should be tried prior to leukotomy. However, Jenike et al. [105] reported that 27/33 patients who received cingulotomy were previously treated with ECT; of these, 7 received additional treatments with ECT following surgery. Good symptomatic response to ECT has more recently been reported in cases with atypical clinical characteristics (e.g., acute and late onset) [106, 107] or with catatonia [108]. Case reports of patients with OCD and Tourette’s or other psychiatric comorbidities also suggest efficacy of ECT in reducing symptoms and maintaining improvement [109–116]. Additional cases of favorable response to ECT in patients with medication-refractory OCD have been reported, though others state that an undefined large number of patients were referred to their clinic who had previously failed to respond to ECT, arguing that the benefits derived from ECT may be more related to comorbid psychiatric illnesses [117]. Yet, an open trial found symptomatic benefit in 7/9 patients with no depressive symptoms prior to OCD who received unilateral or bilateral ECT [118]. Symptom resolution in 1 responder was ultimately maintained using ECT, without medications [119]. A retrospective analysis of 13 depressed and 19 nondepressed patients with OCD who received ECT also demonstrated significant improvements in obsessive–compulsive symptoms in both groups, independent of improvements in depressive symptoms [120].
Transcranial Magnetic Stimulation
Transcranial magnetic stimulation (TMS) has a lower risk profile than either of the techniques discussed above, with side effects largely confined to sensations in the skin and headaches, though seizures are a possible risk, and earplugs are often provided to limit the risks of hearing damage. Repetitive TMS (rTMS) to the DLPFC has generally failed to demonstrate superiority over sham. Despite initial reports from open studies [121], multiple sham-controlled studies of rTMS to the DLPFC at 1 or 10 Hz, 110% motor threshold (MT), found no benefit of active treatment over placebo [122–124]. This lack of benefit was replicated in a group of 30 patients receiving active or sham rTMS of the right DLPFC [125]. However, a sham-controlled trial of rTMS of the DLPFC, at 80% MT with frequency defined based on the patient’s intrinsic alpha EEG, found significant improvements in obsessions but not compulsions, with decreases in Y-BOCS scores, as well as symptoms of depression and anxiety [126].
Yet the supplementary motor area (SMA) appears to be a more promising target. Open rTMS to the SMA was also found to provide benefit in several reports with medication-resistant OCD [127, 128]. This finding was replicated in 2 sham-controlled trials (n = 22 and n = 18, respectively) of rTMS to the SMA. One demonstrated a 41% response rate following active treatment and a mean reduction of 35% in Y-BOCS score versus a 10% response rate following sham treatment; the other reported a response rate of 67% following active treatment compared with 22% following sham [129, 130]. Although effects on neuronal function and response rates have been associated with symptomatic improvement, significant differences between active and sham treatment in all outcome measures have not been uniformly demonstrated [131]. Ongoing studies of TMS at this site may address these concerns (e.g., clinicaltrials.gov NCT00106249).
The OFC has also been suggested as a target for TMS. The only identified published report of TMS at this target, a 23-patient single-blind sham-controlled trial of rTMS to the left OFC (1 Hz, 80% MT), failed to find a difference between groups at 3 weeks but found significant differences between groups in reduction of Y-BOCS score over 3 months following 3 weeks of active treatment [132].
Other Methods
A variety of other neuromodulatory treatments, including magnetic seizure therapy (see NCT01596608), have also been proposed, but data for OCD are not available. Prefrontal stimulation using a TMS coil designed to reach deeper structures (deep TMS) has also been piloted and an ongoing trial is examining effects of prefrontal stimulation intended to also affect the ACC (NCT01343732). Based on reports of anxiolytic effects in treatment trials for depression, a preliminary study of VNS for anxiety disorders was initiated; this open trial included 7 patients with OCD, 3 of whom were classified as responders based on a ≥ 25% decrease in Y-BOCS score [133]. The authors suggested that double-blind trials may be warranted, but, to our knowledge, these have not been reported.
Conclusions
Important advances have been made in neuromodulation for OCD. These include localized treatments, such as DBS, that are reversible and can allow patients to serve as their own controls. Advances in ECT reduce risk and may provide a less invasive alternative to surgical modulation. Another neuromodulatory option that is less invasive and can be feasibly and ethically used in sham-controlled studies is TMS. Neuromodulation, compared with medications, limits the risks of systemic side effects and may provide advantages in “target engagement”. Yet, challenges remain to reconcile current views of psychiatric pathophysiology with the potential of anatomically localized treatments. These localized treatments may work by altering circuit function, and may act at a distance. For example, DBS can elicit antidromic activation and can involve both GABAergic and glutamatergic transmission [134].
Importantly, because emotion and behavior are likely not localized to discrete centers, but rely on communication between multiple neuronal circuits, neuromodulatory approaches must be continually refined to affect more specific regions that may be spatially distributed throughout the brain. Though it is likely that local stimulation propagates up- or downstream through brain circuits, the incomplete efficacy of DBS treatment may relate to the spatially restricted effects of focal treatments on larger circuits. However, the benefits of ECT may be limited by effects on other brain functions, such as memory. Similarly, TMS may be limited by its impact on surrounding structures. Multiple stereotactic targets, closed-loop systems that provide stimulation only when needed [135], more portable noninvasive stimulation methods, or combinations of neuromodulatory strategies may be required to provide optimal benefit in circuit adjustment and symptom resolution; patient-controlled temporal regulation of stimulation has already been attempted in OCD patients receiving DBS. Larger, well-controlled studies are needed to improve understanding of the potential for neuromodulatory treatments in OCD.
Growth in understanding of OCD has facilitated development of our current treatments from more crude approaches. Unfortunately, many patients with OCD remain ill and impaired despite receiving currently state-of-the-art treatment [136]. In this resistant group, TMS may provide an option with limited risk. Also, ECT may be considered prior to more invasive treatments. For highly-resistant patients, DBS may provide a critical somatic alternative. Tools for understanding psychiatric pathophysiology are also developing rapidly. Techniques such as PET, fMRI, magnetic resonance spectroscopy, magnetoencephalography, and quantitative EEG noninvasively illuminate human brain function in vivo. Knowledge gained from these techniques and ongoing research will facilitate novel treatment development and targeting. This offers the promise of improving the lives of patients who suffer from OCD.
Electronic supplementary material
(PDF 1224 kb)
(PDF 1.19 mb)
(PDF 1.19 mb)
(PDF 1224 kb)
Acknowledgments
Required Author Forms
Disclosure forms provided by the authors are available with the online version of this article.
References
- 1.Murray CJL, Lopez AD, Harvard School of Public Health., World Health Organization, World Bank. The global burden of disease: A comprehensive assessment of mortality and disability from diseases, injuries, and risk factors in 1990 and projected to 2020. Harvard School of Public Health on behalf of the World Health Organization and the World Bank, Cambridge, MA, 1996.
- 2.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593–602. doi: 10.1001/archpsyc.62.6.593. [DOI] [PubMed] [Google Scholar]
- 3.American Psychiatric Association, American Psychiatric Association. Task Force on DSM-IV. Diagnostic and statistical manual of mental disorders: DSM-IV. 4th ed. American Psychiatric Association, Washington, DC, 1994.
- 4.Van Ameringen M, Patterson B, Simpson W. DSM-5 obsessive-compulsive and related disorders: clinical implications of new criteria. Depress Anxiety. 2014;31:487–493. doi: 10.1002/da.22259. [DOI] [PubMed] [Google Scholar]
- 5.Langston JW, Ballard P, Tetrud JW, Irwin I. Chronic Parkinsonism in humans due to a product of meperidine-analog synthesis. Science. 1983;219:979–980. doi: 10.1126/science.6823561. [DOI] [PubMed] [Google Scholar]
- 6.Wright JM, Wall RA, Perry TL, Paty DW. Chronic parkinsonism secondary to intranasal administration of a product of meperidine-analogue synthesis. N Engl J Med. 1984;310:325. doi: 10.1056/NEJM198402023100520. [DOI] [PubMed] [Google Scholar]
- 7.Alexander GE, DeLong MR, Strick PL. Parallel organization of functionally segregated circuits linking basal ganglia and cortex. Annu Rev Neurosci. 1986;9:357–381. doi: 10.1146/annurev.ne.09.030186.002041. [DOI] [PubMed] [Google Scholar]
- 8.Milad MR, Rauch SL. Obsessive-compulsive disorder: beyond segregated cortico-striatal pathways. Trends Cogn Sci. 2012;16:43–51. doi: 10.1016/j.tics.2011.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saxena S, Rauch SL. Functional neuroimaging and the neuroanatomy of obsessive-compulsive disorder. Psychiatr Clin North Am. 2000;23:563–586. doi: 10.1016/s0193-953x(05)70181-7. [DOI] [PubMed] [Google Scholar]
- 10.Krack P, Hariz MI, Baunez C, Guridi J, Obeso JA. Deep brain stimulation: from neurology to psychiatry? Trends Neurosci 2010;33:474–484. [DOI] [PubMed]
- 11.Hansen ES, Hasselbalch S, Law I, Bolwig TG. The caudate nucleus in obsessive-compulsive disorder. Reduced metabolism following treatment with paroxetine: a PET study. Int J Neuropsychopharmacol. 2002;5:1–10. doi: 10.1017/S1461145701002681. [DOI] [PubMed] [Google Scholar]
- 12.Cummings JL, Frankel M. Gilles de la Tourette syndrome and the neurological basis of obsessions and compulsions. Biol Psychiatry. 1985;20:117–126. doi: 10.1016/0006-3223(85)90011-3. [DOI] [PubMed] [Google Scholar]
- 13.Coffey BJ, Miguel EC, Biederman J, et al. Tourette's disorder with and without obsessive-compulsive disorder in adults: are they different? J Nerv Ment Dis. 1998;186:201–206. doi: 10.1097/00005053-199804000-00001. [DOI] [PubMed] [Google Scholar]
- 14.Worbe Y, Mallet L, Golmard JL, et al. Repetitive behaviours in patients with Gilles de la Tourette syndrome: Tics, compulsions, or both? PLoS One. 2010;5:e12959. doi: 10.1371/journal.pone.0012959. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Singer HS. Neurobiology of Tourette syndrome. Neurol Clin. 1997;15:357–379. doi: 10.1016/s0733-8619(05)70318-2. [DOI] [PubMed] [Google Scholar]
- 16.Felling RJ, Singer HS. Neurobiology of tourette syndrome: current status and need for further investigation. J Neurosci. 2011;31:12387–12395. doi: 10.1523/JNEUROSCI.0150-11.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Soomro GM, Altman D, Rajagopal S, Oakley-Browne M. Selective serotonin re-uptake inhibitors (SSRIs) versus placebo for obsessive compulsive disorder (OCD). Cochrane Database Syst Rev 2008:CD001765. [DOI] [PMC free article] [PubMed]
- 18.Sugden K, Tichopad A, Khan N, Craig IW, D'Souza UM. Genes within the serotonergic system are differentially expressed in human brain. BMC Neurosci. 2009;10:50. doi: 10.1186/1471-2202-10-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Goodman WK, McDougle CJ, Price LH, Riddle MA, Pauls DL, Leckman JF. Beyond the serotonin hypothesis: a role for dopamine in some forms of obsessive compulsive disorder? J Clin Psychiatry 1990;51(Suppl.):36–43. [PubMed]
- 20.van der Wee NJ, Stevens H, Hardeman JA, et al. Enhanced dopamine transporter density in psychotropic-naive patients with obsessive-compulsive disorder shown by [123I]{beta}-CIT SPECT. Am J Psychiatry. 2004;161:2201–2206. doi: 10.1176/appi.ajp.161.12.2201. [DOI] [PubMed] [Google Scholar]
- 21.Denys D, van der Wee N, Janssen J, De Geus F, Westenberg HG. Low level of dopaminergic D2 receptor binding in obsessive-compulsive disorder. Biol Psychiatry. 2004;55:1041–1045. doi: 10.1016/j.biopsych.2004.01.023. [DOI] [PubMed] [Google Scholar]
- 22.Haber SN, McFarland NR. The concept of the ventral striatum in nonhuman primates. Ann N Y Acad Sci. 1999;877:33–48. doi: 10.1111/j.1749-6632.1999.tb09259.x. [DOI] [PubMed] [Google Scholar]
- 23.Rosenberg DR, MacMaster FP, Keshavan MS, Fitzgerald KD, Stewart CM, Moore GJ. Decrease in caudate glutamatergic concentrations in pediatric obsessive-compulsive disorder patients taking paroxetine. J Am Acad Child Adolesc Psychiatry. 2000;39:1096–1103. doi: 10.1097/00004583-200009000-00008. [DOI] [PubMed] [Google Scholar]
- 24.Arnold PD, Rosenberg DR, Mundo E, Tharmalingam S, Kennedy JL, Richter MA. Association of a glutamate (NMDA) subunit receptor gene (GRIN2B) with obsessive-compulsive disorder: a preliminary study. Psychopharmacology (Berl) 2004;174:530–538. doi: 10.1007/s00213-004-1847-1. [DOI] [PubMed] [Google Scholar]
- 25.Arnold PD, Sicard T, Burroughs E, Richter MA, Kennedy JL. Glutamate transporter gene SLC1A1 associated with obsessive-compulsive disorder. Arch Gen Psychiatry. 2006;63:769–776. doi: 10.1001/archpsyc.63.7.769. [DOI] [PubMed] [Google Scholar]
- 26.Dickel DE, Veenstra-VanderWeele J, Cox NJ, Wu X, Fischer DJ, Van Etten-Lee M, et al. Association testing of the positional and functional candidate gene SLC1A1/EAAC1 in early-onset obsessive-compulsive disorder. Arch Gen Psychiatry. 2006;63:778–785. doi: 10.1001/archpsyc.63.7.778. [DOI] [PubMed] [Google Scholar]
- 27.Wendland JR, Moya PR, Timpano KR, Anavitarte AP, Kruse MR, Wheaton MG, et al. A haplotype containing quantitative trait loci for SLC1A1 gene expression and its association with obsessive-compulsive disorder. Arch Gen Psychiatry. 2009;66:408–416. doi: 10.1001/archgenpsychiatry.2009.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Coric V, Taskiran S, Pittenger C, et al. Riluzole augmentation in treatment-resistant obsessive-compulsive disorder: an open-label trial. Biol Psychiatry. 2005;58:424–428. doi: 10.1016/j.biopsych.2005.04.043. [DOI] [PubMed] [Google Scholar]
- 29.Lafleur DL, Pittenger C, Kelmendi B, et al. N-acetylcysteine augmentation in serotonin reuptake inhibitor refractory obsessive-compulsive disorder. Psychopharmacology (Berl) 2006;184:254–256. doi: 10.1007/s00213-005-0246-6. [DOI] [PubMed] [Google Scholar]
- 30.Grant JE, Odlaug BL, Kim SW. N-acetylcysteine, a glutamate modulator, in the treatment of trichotillomania: a double-blind, placebo-controlled study. Arch Gen Psychiatry. 2009;66:756–763. doi: 10.1001/archgenpsychiatry.2009.60. [DOI] [PubMed] [Google Scholar]
- 31.Rodriguez CI, Kegeles LS, Levinson A, et al. Randomized controlled crossover trial of ketamine in obsessive-compulsive disorder: proof-of-concept. Neuropsychopharmacology. 2013;38:2475–2483. doi: 10.1038/npp.2013.150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rauch SL. Neuroimaging and neurocircuitry models pertaining to the neurosurgical treatment of psychiatric disorders. Neurosurg Clin N Am. 2003;14:213–223. doi: 10.1016/s1042-3680(02)00114-6. [DOI] [PubMed] [Google Scholar]
- 33.Breiter HC, Rauch SL, Kwong KK, et al. Functional magnetic resonance imaging of symptom provocation in obsessive-compulsive disorder. Arch Gen Psychiatry. 1996;53:595–606. doi: 10.1001/archpsyc.1996.01830070041008. [DOI] [PubMed] [Google Scholar]
- 34.Penney JB, Jr, Young AB. GABA as the pallidothalamic neurotransmitter: implications for basal ganglia function. Brain Res. 1981;207:195–199. doi: 10.1016/0006-8993(81)90693-4. [DOI] [PubMed] [Google Scholar]
- 35.Koob GF, Swerdlow NR. The functional output of the mesolimbic dopamine system. Ann N Y Acad Sci. 1988;537:216–227. doi: 10.1111/j.1749-6632.1988.tb42108.x. [DOI] [PubMed] [Google Scholar]
- 36.Barroso-Chinea P, Rico AJ, Perez-Manso M, et al. Glutamatergic pallidothalamic projections and their implications in the pathophysiology of Parkinson's disease. Neurobiol Dis. 2008;31:422–432. doi: 10.1016/j.nbd.2008.05.019. [DOI] [PubMed] [Google Scholar]
- 37.Wallman MJ, Gagnon D, Parent M. Serotonin innervation of human basal ganglia. Eur J Neurosci. 2011;33:1519–1532. doi: 10.1111/j.1460-9568.2011.07621.x. [DOI] [PubMed] [Google Scholar]
- 38.Nikolaus S, Antke C, Beu M, Muller HW. Cortical GABA, striatal dopamine and midbrain serotonin as the key players in compulsive and anxiety disorders—results from in vivo imaging studies. Rev Neurosci. 2010;21:119–139. doi: 10.1515/revneuro.2010.21.2.119. [DOI] [PubMed] [Google Scholar]
- 39.Papez JW. A proposed mechanism of emotion. 1937. J Neuropsychiatry Clin Neurosci. 1995;7:103–112. doi: 10.1176/jnp.7.1.103. [DOI] [PubMed] [Google Scholar]
- 40.Saxena S, Brody AL, Maidment KM, et al. Localized orbitofrontal and subcortical metabolic changes and predictors of response to paroxetine treatment in obsessive-compulsive disorder. Neuropsychopharmacology. 1999;21:683–693. doi: 10.1016/S0893-133X(99)00082-2. [DOI] [PubMed] [Google Scholar]
- 41.Nakao T, Nakagawa A, Yoshiura T, et al. Brain activation of patients with obsessive-compulsive disorder during neuropsychological and symptom provocation tasks before and after symptom improvement: a functional magnetic resonance imaging study. Biol Psychiatry. 2005;57:901–910. doi: 10.1016/j.biopsych.2004.12.039. [DOI] [PubMed] [Google Scholar]
- 42.Le Jeune F, Verin M, N'Diaye K, et al. Decrease of prefrontal metabolism after subthalamic stimulation in obsessive-compulsive disorder: a positron emission tomography study. Biol Psychiatry. 2010;68:1016–1022. doi: 10.1016/j.biopsych.2010.06.033. [DOI] [PubMed] [Google Scholar]
- 43.Hitchcock ER, Ballantine HT, Meyerson BA. Modern concepts in psychiatric surgery. In: Proceedings of the 5th World Congress of Psychiatric Surgery, Boston, MA, USA, August 21–25, 1978. Elsevier/North-Holland Biomedical Press, New York, Amsterdam.
- 44.Laitinen LV. Emotional responses to subcortical electrical stimulation in psychiatric patients. Clin Neurol Neurosurg. 1979;81:148–157. doi: 10.1016/0303-8467(79)90002-7. [DOI] [PubMed] [Google Scholar]
- 45.Ardouin C, Pillon B, Peiffer E, et al. Bilateral subthalamic or pallidal stimulation for Parkinson's disease affects neither memory nor executive functions: a consecutive series of 62 patients. Ann Neurol. 1999;46:217–223. doi: 10.1002/1531-8249(199908)46:2<217::aid-ana11>3.0.co;2-z. [DOI] [PubMed] [Google Scholar]
- 46.Woods SP, Fields JA, Troster AI. Neuropsychological sequelae of subthalamic nucleus deep brain stimulation in Parkinson's disease: A critical review. Neuropsychol Rev. 2002;12:111–126. doi: 10.1023/a:1016806711705. [DOI] [PubMed] [Google Scholar]
- 47.Heath RG. Pleasure and brain activity in man. Deep and surface electroencephalograms during orgasm. J Nerv Ment Dis. 1972;154:3–18. doi: 10.1097/00005053-197201000-00002. [DOI] [PubMed] [Google Scholar]
- 48.Mallet L, Mesnage V, Houeto JL, et al. Compulsions, Parkinson's disease, and stimulation. Lancet. 2002;360:1302–1304. doi: 10.1016/S0140-6736(02)11339-0. [DOI] [PubMed] [Google Scholar]
- 49.Fontaine D, Mattei V, Borg M, et al. Effect of subthalamic nucleus stimulation on obsessive-compulsive disorder in a patient with Parkinson disease. Case report. J Neurosurg. 2004;100:1084–1086. doi: 10.3171/jns.2004.100.6.1084. [DOI] [PubMed] [Google Scholar]
- 50.Bejjani BP, Damier P, Arnulf I, et al. Transient acute depression induced by high-frequency deep-brain stimulation. N Engl J Med. 1999;340:1476–1480. doi: 10.1056/NEJM199905133401905. [DOI] [PubMed] [Google Scholar]
- 51.Tommasi G, Lanotte M, Albert U, et al. Transient acute depressive state induced by subthalamic region stimulation. J Neurol Sci. 2008;273:135–138. doi: 10.1016/j.jns.2008.06.012. [DOI] [PubMed] [Google Scholar]
- 52.Temel Y. Limbic effects of high-frequency stimulation of the subthalamic nucleus. Vitam Horm. 2010;82:47–63. doi: 10.1016/S0083-6729(10)82003-5. [DOI] [PubMed] [Google Scholar]
- 53.Temel Y, Kessels A, Tan S, Topdag A, Boon P, Visser-Vandewalle V. Behavioural changes after bilateral subthalamic stimulation in advanced Parkinson disease: a systematic review. Parkinsonism Relat Disord. 2006;12:265–272. doi: 10.1016/j.parkreldis.2006.01.004. [DOI] [PubMed] [Google Scholar]
- 54.Witt K, Daniels C, Reiff J, et al. Neuropsychological and psychiatric changes after deep brain stimulation for Parkinson's disease: a randomised, multicentre study. Lancet Neurol. 2008;7:605–614. doi: 10.1016/S1474-4422(08)70114-5. [DOI] [PubMed] [Google Scholar]
- 55.Mallet L, Schupbach M, N'Diaye K, et al. Stimulation of subterritories of the subthalamic nucleus reveals its role in the integration of the emotional and motor aspects of behavior. Proc Natl Acad Sci U S A. 2007;104:10661–10666. doi: 10.1073/pnas.0610849104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Higginson CI, Fields JA, Troster AI. Which symptoms of anxiety diminish after surgical interventions for Parkinson disease? Neuropsychiatry Neuropsychol Behav Neurol. 2001;14:117–121. [PubMed] [Google Scholar]
- 57.Kosel M, Sturm V, Frick C, et al. Mood improvement after deep brain stimulation of the internal globus pallidus for tardive dyskinesia in a patient suffering from major depression. J Psychiatr Res. 2007;41:801–803. doi: 10.1016/j.jpsychires.2006.07.010. [DOI] [PubMed] [Google Scholar]
- 58.Lapidus KA, Kopell BH, Ben-Haim S, Rezai AR, Goodman WK. History of psychosurgery: A psychiatrist's perspective. World Neurosurg. 2013;80(S27):e1–16. doi: 10.1016/j.wneu.2013.02.053. [DOI] [PubMed] [Google Scholar]
- 59.Goodman WK, Alterman RL. Deep brain stimulation for intractable psychiatric disorders. Annu Rev Med. 2012;63:511–524. doi: 10.1146/annurev-med-052209-100401. [DOI] [PubMed] [Google Scholar]
- 60.Blomstedt P, Sjoberg RL, Hansson M, Bodlund O, Hariz MI. Deep brain stimulation in the treatment of obsessive-compulsive disorder. World Neurosurg. 2013;80:e245–253. doi: 10.1016/j.wneu.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 61.Nangunoori R, Tomycz ND, Quigley M, Oh MY, Whiting DM. Deep brain stimulation for psychiatric diseases: a pooled analysis of published studies employing disease-specific standardized outcome scales. Stereotact Funct Neurosurg. 2013;91:345–354. doi: 10.1159/000351156. [DOI] [PubMed] [Google Scholar]
- 62.Nuttin B, Cosyns P, Demeulemeester H, Gybels J, Meyerson B. Electrical stimulation in anterior limbs of internal capsules in patients with obsessive-compulsive disorder. Lancet. 1999;354:1526. doi: 10.1016/S0140-6736(99)02376-4. [DOI] [PubMed] [Google Scholar]
- 63.Vandewalle V, van der Linden C, Groenewegen HJ, Caemaert J. Stereotactic treatment of Gilles de la Tourette syndrome by high frequency stimulation of thalamus. Lancet. 1999;353:724. doi: 10.1016/s0140-6736(98)05964-9. [DOI] [PubMed] [Google Scholar]
- 64.Gabriels L, Cosyns P, Nuttin B, Demeulemeester H, Gybels J. Deep brain stimulation for treatment-refractory obsessive-compulsive disorder: psychopathological and neuropsychological outcome in three cases. Acta Psychiatr Scand. 2003;107:275–282. [PubMed] [Google Scholar]
- 65.Goodman WK, Price LH, Rasmussen SA, et al. The Yale-Brown Obsessive Compulsive Scale. I. Development, use, and reliability. Arch Gen Psychiatry. 1989;46:1006–1011. doi: 10.1001/archpsyc.1989.01810110048007. [DOI] [PubMed] [Google Scholar]
- 66.Anderson D, Ahmed A. Treatment of patients with intractable obsessive-compulsive disorder with anterior capsular stimulation. Case report. J Neurosurg. 2003;98:1104–1108. doi: 10.3171/jns.2003.98.5.1104. [DOI] [PubMed] [Google Scholar]
- 67.Aouizerate B, Cuny E, Martin-Guehl C, et al. Deep brain stimulation of the ventral caudate nucleus in the treatment of obsessive-compulsive disorder and major depression. Case report. J Neurosurg. 2004;101:682–686. doi: 10.3171/jns.2004.101.4.0682. [DOI] [PubMed] [Google Scholar]
- 68.Aouizerate B, Martin-Guehl C, Cuny E, et al. Deep brain stimulation for OCD and major depression. Am J Psychiatry. 2005;162:2192. doi: 10.1176/appi.ajp.162.11.2192. [DOI] [PubMed] [Google Scholar]
- 69.Nuttin BJ, Gabriels LA, Cosyns PR, et al. Long-term electrical capsular stimulation in patients with obsessive-compulsive disorder. Neurosurgery. 2003;52:1263–1272. doi: 10.1227/01.neu.0000064565.49299.9a. [DOI] [PubMed] [Google Scholar]
- 70.Nuttin BJ, Gabriels LA, Cosyns PR, et al. Long-term electrical capsular stimulation in patients with obsessive-compulsive disorder. Neurosurgery. 2008;62(6 Suppl. 3):966–977. doi: 10.1227/01.neu.0000333764.20575.d6. [DOI] [PubMed] [Google Scholar]
- 71.Aouizerate B, Cuny E, Bardinet E, et al. Distinct striatal targets in treating obsessive-compulsive disorder and major depression. J Neurosurg. 2009;111:775–779. doi: 10.3171/2009.2.JNS0881. [DOI] [PubMed] [Google Scholar]
- 72.Chang WS, Roh D, Kim CH, Chang JW. Combined bilateral anterior cingulotomy and ventral capsule/ventral striatum deep brain stimulation for refractory obsessive-compulsive disorder with major depression: do combined procedures have a long-term benefit? Restor Neurol Neurosci. 2013;31:723–732. doi: 10.3233/RNN-120290. [DOI] [PubMed] [Google Scholar]
- 73.Greenberg BD, Gabriels LA, Malone DA, Jr, et al. Deep brain stimulation of the ventral internal capsule/ventral striatum for obsessive-compulsive disorder: Worldwide experience. Mol Psychiatry. 2010;15:64–79. doi: 10.1038/mp.2008.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Abelson JL, Curtis GC, Sagher O, et al. Deep brain stimulation for refractory obsessive-compulsive disorder. Biol Psychiatry. 2005;57:510–516. doi: 10.1016/j.biopsych.2004.11.042. [DOI] [PubMed] [Google Scholar]
- 75.Goodman WK, Foote KD, Greenberg BD, et al. Deep brain stimulation for intractable obsessive compulsive disorder: pilot study using a blinded, staggered-onset design. Biol Psychiatry. 2010;67:535–542. doi: 10.1016/j.biopsych.2009.11.028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Okun MS, Mann G, Foote KD, et al. Deep brain stimulation in the internal capsule and nucleus accumbens region: responses observed during active and sham programming. J Neurol Neurosurg Psychiatry. 2007;78:310–314. doi: 10.1136/jnnp.2006.095315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Chang CH, Chen SY, Hsiao YL, Tsai ST, Tsai HC. Hypomania with hypersexuality following bilateral anterior limb stimulation in obsessive-compulsive disorder. J Neurosurg. 2010;112:1299–1300. doi: 10.3171/2009.10.JNS09918. [DOI] [PubMed] [Google Scholar]
- 78.Okun MS, Bowers D, Springer U, et al. What's in a “smile?” Intra-operative observations of contralateral smiles induced by deep brain stimulation. Neurocase. 2004;10:271–279. doi: 10.1080/13554790490507632. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Haq IU, Foote KD, Goodman WG, et al. Smile and laughter induction and intraoperative predictors of response to deep brain stimulation for obsessive-compulsive disorder. Neuroimage. 2011;54(Suppl. 1):S247–S255. doi: 10.1016/j.neuroimage.2010.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Tsai HC, Chang CH, Pan JI, et al. Acute stimulation effect of the ventral capsule/ventral striatum in patients with refractory obsessive-compulsive disorder - a double-blinded trial. Neuropsychiatr Dis Treat. 2014;10:63–69. doi: 10.2147/NDT.S54964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Haq IU, Foote KD, Goodman WK, et al. A case of mania following deep brain stimulation for obsessive compulsive disorder. Stereotact Funct Neurosurg. 2010;88:322–328. doi: 10.1159/000319960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Baker KB, Kopell BH, Malone D, et al. Deep brain stimulation for obsessive-compulsive disorder: using functional magnetic resonance imaging and electrophysiological techniques: technical case report. Neurosurgery. 2007;61(5 Suppl. 2):E367–E368. doi: 10.1227/01.neu.0000303995.66902.36. [DOI] [PubMed] [Google Scholar]
- 83.Vora AK, Ward H, Foote KD, Goodman WK, Okun MS. Rebound symptoms following battery depletion in the NIH OCD DBS cohort: clinical and reimbursement issues. Brain Stimul. 2012;5:599–604. doi: 10.1016/j.brs.2011.10.004. [DOI] [PubMed] [Google Scholar]
- 84.Tsai HC, Chang CH, Pan JI, et al. Pilot study of deep brain stimulation in refractory obsessive-compulsive disorder ethnic Chinese patients. Psychiatry Clin Neurosci. 2012;66:303–312. doi: 10.1111/j.1440-1819.2012.02352.x. [DOI] [PubMed] [Google Scholar]
- 85.Roh D, Chang WS, Chang JW, Kim CH. Long-term follow-up of deep brain stimulation for refractory obsessive-compulsive disorder. Psychiatry Res. 2012;200:1067–1070. doi: 10.1016/j.psychres.2012.06.018. [DOI] [PubMed] [Google Scholar]
- 86.Kubu CS, Malone DA, Chelune G, et al. Neuropsychological outcome after deep brain stimulation in the ventral capsule/ventral striatum for highly refractory obsessive-compulsive disorder or major depression. Stereotact Funct Neurosurg. 2013;91:374–378. doi: 10.1159/000348321. [DOI] [PubMed] [Google Scholar]
- 87.van den Munckhof P, Bosch DA, Mantione MH, Figee M, Denys DA, Schuurman PR. Active stimulation site of nucleus accumbens deep brain stimulation in obsessive-compulsive disorder is localized in the ventral internal capsule. Acta Neurochir Suppl. 2013;117:53–59. doi: 10.1007/978-3-7091-1482-7_9. [DOI] [PubMed] [Google Scholar]
- 88.Sturm V, Lenartz D, Koulousakis A, et al. The nucleus accumbens: a target for deep brain stimulation in obsessive-compulsive- and anxiety-disorders. J Chem Neuroanat. 2003;26:293–299. doi: 10.1016/j.jchemneu.2003.09.003. [DOI] [PubMed] [Google Scholar]
- 89.Franzini A, Messina G, Gambini O, et al. Deep-brain stimulation of the nucleus accumbens in obsessive compulsive disorder: clinical, surgical and electrophysiological considerations in two consecutive patients. Neurol Sci. 2010;31:353–359. doi: 10.1007/s10072-009-0214-8. [DOI] [PubMed] [Google Scholar]
- 90.Huff W, Lenartz D, Schormann M, et al. Unilateral deep brain stimulation of the nucleus accumbens in patients with treatment-resistant obsessive-compulsive disorder: Outcomes after one year. Clin Neurol Neurosurg. 2010;112:137–143. doi: 10.1016/j.clineuro.2009.11.006. [DOI] [PubMed] [Google Scholar]
- 91.Greenberg BD, Malone DA, Friehs GM, et al. Three-year outcomes in deep brain stimulation for highly resistant obsessive-compulsive disorder. Neuropsychopharmacology. 2006;31:2384–2393. doi: 10.1038/sj.npp.1301165. [DOI] [PubMed] [Google Scholar]
- 92.Denys D, Mantione M, Figee M, et al. Deep brain stimulation of the nucleus accumbens for treatment-refractory obsessive-compulsive disorder. Arch Gen Psychiatry. 2010;67:1061–1068. doi: 10.1001/archgenpsychiatry.2010.122. [DOI] [PubMed] [Google Scholar]
- 93.Luigjes J, Mantione M, van den Brink W, Schuurman PR, van den Munckhof P, Denys D. Deep brain stimulation increases impulsivity in two patients with obsessive-compulsive disorder. Int Clin Psychopharmacol. 2011;26:338–340. doi: 10.1097/YIC.0b013e32834af505. [DOI] [PubMed] [Google Scholar]
- 94.de Koning PP, Figee M, Endert E, Storosum JG, Fliers E, Denys D. Deep brain stimulation for obsessive-compulsive disorder is associated with cortisol changes. Psychoneuroendocrinology. 2013;38:1455–1459. doi: 10.1016/j.psyneuen.2012.12.006. [DOI] [PubMed] [Google Scholar]
- 95.Ooms P, Mantione M, Figee M, Schuurman PR, van den Munckhof P, Denys D. Deep brain stimulation for obsessive-compulsive disorders: Long-term analysis of quality of life. J Neurol Neurosurg Psychiatry. 2014;85:153–158. doi: 10.1136/jnnp-2012-302550. [DOI] [PubMed] [Google Scholar]
- 96.Mallet L, Polosan M, Jaafari N, et al. Subthalamic nucleus stimulation in severe obsessive-compulsive disorder. N Engl J Med. 2008;359:2121–2134. doi: 10.1056/NEJMoa0708514. [DOI] [PubMed] [Google Scholar]
- 97.Chabardes S, Polosan M, Krack P, et al. Deep brain stimulation for obsessive-compulsive disorder: subthalamic nucleus target. World Neurosurg. 2013;80(S31):e1–e8. doi: 10.1016/j.wneu.2012.03.010. [DOI] [PubMed] [Google Scholar]
- 98.Piallat B, Polosan M, Fraix V, et al. Subthalamic neuronal firing in obsessive-compulsive disorder and Parkinson disease. Ann Neurol. 2011;69:793–802. doi: 10.1002/ana.22222. [DOI] [PubMed] [Google Scholar]
- 99.Welter ML, Burbaud P, Fernandez-Vidal S, et al. Basal ganglia dysfunction in OCD: subthalamic neuronal activity correlates with symptoms severity and predicts high-frequency stimulation efficacy. Transl Psychiatry. 2011;1:e5. doi: 10.1038/tp.2011.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Jimenez-Ponce F, Velasco-Campos F, Castro-Farfan G, et al. Preliminary study in patients with obsessive-compulsive disorder treated with electrical stimulation in the inferior thalamic peduncle. Neurosurgery. 2009;65(6 Suppl.):203–209. doi: 10.1227/01.NEU.0000345938.39199.90. [DOI] [PubMed] [Google Scholar]
- 101.Jimenez F, Nicolini H, Lozano AM, Piedimonte F, Salin R, Velasco F. Electrical stimulation of the inferior thalamic peduncle in the treatment of major depression and obsessive compulsive disorders. World Neurosurg. 2013;80(S30):e17–25. doi: 10.1016/j.wneu.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 102.Grimshaw L. The outcome of obsessional disorder. A follow-up study of 100 cases. Br J Psychiatry. 1965;111:1051–1056. doi: 10.1192/bjp.111.480.1051. [DOI] [PubMed] [Google Scholar]
- 103.Janike MA, Baer L, Minichiello WE. Somatic treatments for obsessive-compulsive disorders. Compr Psychiatry. 1987;28:250–263. doi: 10.1016/0010-440x(87)90032-0. [DOI] [PubMed] [Google Scholar]
- 104.Walter CJ, Mitchell-Heggs N, Sargant W. Modified narcosis, ECT and antidepressant drugs: a review of technique and immediate outcome. Br J Psychiatry. 1972;120:651–662. doi: 10.1192/bjp.120.559.651. [DOI] [PubMed] [Google Scholar]
- 105.Jenike MA, Baer L, Ballantine T, et al. Cingulotomy for refractory obsessive-compulsive disorder. A long-term follow-up of 33 patients. Arch Gen Psychiatry. 1991;48:548–555. doi: 10.1001/archpsyc.1991.01810300060009. [DOI] [PubMed] [Google Scholar]
- 106.Swartz CM, Shen WW. Is episodic obsessive compulsive disorder bipolar? A report of four cases. J Affect Disord. 1999;56:61–66. doi: 10.1016/s0165-0327(99)00021-x. [DOI] [PubMed] [Google Scholar]
- 107.Mellman LA, Gorman JM. Successful treatment of obsessive-compulsive disorder with ECT. Am J Psychiatry. 1984;141:596–597. doi: 10.1176/ajp.141.4.596. [DOI] [PubMed] [Google Scholar]
- 108.D'Urso G, Mantovani A, Barbarulo AM, Labruna L, Muscettola G. Brain-behavior relationship in a case of successful ECT for drug refractory catatonic OCD. J Ect. 2012;28:190–193. doi: 10.1097/YCT.0b013e3182542649. [DOI] [PubMed] [Google Scholar]
- 109.Hanisch F, Friedemann J, Piro J, Gutmann P. Maintenance electroconvulsive therapy for comorbid pharmacotherapy-refractory obsessive-compulsive and schizoaffective disorder. Eur J Med Res. 2009;14:367–368. doi: 10.1186/2047-783X-14-8-367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Casey DA, Davis MH. Obsessive-compulsive disorder responsive to electroconvulsive therapy in an elderly woman. South Med J. 1994;87:862–864. doi: 10.1097/00007611-199408000-00027. [DOI] [PubMed] [Google Scholar]
- 111.Bulbul F, Copoglu US, Alpak G, Unal A, Tastan MF, Savas HA. Maintenance therapy with electroconvulsive therapy in a patient with a codiagnosis of bipolar disorder and obsessive-compulsive disorder. J Ect. 2013;29:e21–e22. doi: 10.1097/YCT.0b013e31827b4e76. [DOI] [PubMed] [Google Scholar]
- 112.Strassnig M, Riedel M, Muller N. Electroconvulsive therapy in a patient with Tourette's syndrome and co-morbid Obsessive Compulsive Disorder. World J Biol Psychiatry. 2004;5:164–166. doi: 10.1080/15622970410029930. [DOI] [PubMed] [Google Scholar]
- 113.Gadit AM, Smigas T. Efficacy of ECT in severe obsessive-compulsive disorder with Parkinson's disease. BMJ Case Rep 2012;2012. [DOI] [PMC free article] [PubMed]
- 114.Lavin MR, Halligan P. ECT for comorbid obsessive-compulsive disorder and schizophrenia. Am J Psychiatry. 1996;153:1652–1653. doi: 10.1176/ajp.153.12.1652b. [DOI] [PubMed] [Google Scholar]
- 115.Chaves MP, Crippa JA, Morais SL, Zuardi AW. Electroconvulsive therapy for coexistent schizophrenia and obsessive-compulsive disorder. J Clin Psychiatry. 2005;66:542–543. doi: 10.4088/jcp.v66n0420c. [DOI] [PubMed] [Google Scholar]
- 116.Thomas SG, Kellner CH. Remission of major depression and obsessive-compulsive disorder after a single unilateral ECT. J Ect. 2003;19:50–51. doi: 10.1097/00124509-200303000-00011. [DOI] [PubMed] [Google Scholar]
- 117.Beale MD, Kellner CH, Pritchett JT, Burns CM. ECT for OCD. J Clin Psychiatry. 1995;56:81–82. [PubMed] [Google Scholar]
- 118.Khanna S, Gangadhar BN, Sinha V, Rajendra PN, Channabasavanna SM. Electroconvulsive therapy in obsessive-compulsive disorder. Convuls Ther. 1988;4:314–320. [PubMed] [Google Scholar]
- 119.Husain MM, Lewis SF, Thornton WL. Maintenance ECT for refractory obsessive-compulsive disorder. Am J Psychiatry. 1993;150:1899–1900. doi: 10.1176/ajp.150.12.1899c. [DOI] [PubMed] [Google Scholar]
- 120.Maletzky B, McFarland B, Burt A. Refractory obsessive compulsive disorder and ECT. Convuls Ther. 1994;10:34–42. [PubMed] [Google Scholar]
- 121.Greenberg BD, George MS, Martin JD, et al. Effect of prefrontal repetitive transcranial magnetic stimulation in obsessive-compulsive disorder: A preliminary study. Am J Psychiatry. 1997;154:867–869. doi: 10.1176/ajp.154.6.867. [DOI] [PubMed] [Google Scholar]
- 122.Sarkhel S, Sinha VK, Praharaj SK. Adjunctive high-frequency right prefrontal repetitive transcranial magnetic stimulation (rTMS) was not effective in obsessive-compulsive disorder but improved secondary depression. J Anxiety Disord. 2010;24:535–539. doi: 10.1016/j.janxdis.2010.03.011. [DOI] [PubMed] [Google Scholar]
- 123.Kang JI, Kim CH, Namkoong K, Lee CI, Kim SJ. A randomized controlled study of sequentially applied repetitive transcranial magnetic stimulation in obsessive-compulsive disorder. J Clin Psychiatry. 2009;70:1645–1651. doi: 10.4088/JCP.08m04500. [DOI] [PubMed] [Google Scholar]
- 124.Alonso P, Pujol J, Cardoner N, et al. Right prefrontal repetitive transcranial magnetic stimulation in obsessive-compulsive disorder: a double-blind, placebo-controlled study. Am J Psychiatry. 2001;158:1143–1145. doi: 10.1176/appi.ajp.158.7.1143. [DOI] [PubMed] [Google Scholar]
- 125.Mansur CG, Myczkowki ML, de Barros Cabral S, et al. Placebo effect after prefrontal magnetic stimulation in the treatment of resistant obsessive-compulsive disorder: a randomized controlled trial. Int J Neuropsychopharmacol. 2011;14:1389–1397. doi: 10.1017/S1461145711000575. [DOI] [PubMed] [Google Scholar]
- 126.Ma X, Huang Y, Liao L, Jin Y. A randomized double-blinded sham-controlled trial of alpha electroencephalogram-guided transcranial magnetic stimulation for obsessive-compulsive disorder. Chin Med J (Engl) 2014;127:601–606. [PubMed] [Google Scholar]
- 127.Kumar N, Chadda RK. Augmentation effect of repetitive transcranial magnetic stimulation over the supplementary motor cortex in treatment refractory patients with obsessive compulsive disorder. Indian J Psychiatry. 2011;53:340–342. doi: 10.4103/0019-5545.91909. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Mantovani A, Lisanby SH, Pieraccini F, Ulivelli M, Castrogiovanni P, Rossi S. Repetitive transcranial magnetic stimulation (rTMS) in the treatment of obsessive-compulsive disorder (OCD) and Tourette's syndrome (TS) Int J Neuropsychopharmacol. 2006;9:95–100. doi: 10.1017/S1461145705005729. [DOI] [PubMed] [Google Scholar]
- 129.Gomes PV, Brasil-Neto JP, Allam N. Rodrigues de Souza E. A randomized, double-blind trial of repetitive transcranial magnetic stimulation in obsessive-compulsive disorder with three-month follow-up. J Neuropsychiatry Clin Neurosci. 2012;24:437–443. doi: 10.1176/appi.neuropsych.11100242. [DOI] [PubMed] [Google Scholar]
- 130.Mantovani A, Simpson HB, Fallon BA, Rossi S, Lisanby SH. Randomized sham-controlled trial of repetitive transcranial magnetic stimulation in treatment-resistant obsessive-compulsive disorder. Int J Neuropsychopharmacol. 2010;13:217–227. doi: 10.1017/S1461145709990435. [DOI] [PubMed] [Google Scholar]
- 131.Mantovani A, Rossi S, Bassi BD, Simpson HB, Fallon BA, Lisanby SH. Modulation of motor cortex excitability in obsessive-compulsive disorder: an exploratory study on the relations of neurophysiology measures with clinical outcome. Psychiatry Res. 2013;210:1026–1032. doi: 10.1016/j.psychres.2013.08.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Ruffini C, Locatelli M, Lucca A, Benedetti F, Insacco C, Smeraldi E. Augmentation effect of repetitive transcranial magnetic stimulation over the orbitofrontal cortex in drug-resistant obsessive-compulsive disorder patients: a controlled investigation. Prim Care Companion J Clin Psychiatry. 2009;11:226–230. doi: 10.4088/PCC.08m00663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.George MS, Ward HE, Jr, Ninan PT, et al. A pilot study of vagus nerve stimulation (VNS) for treatment-resistant anxiety disorders. Brain Stimul. 2008;1:112–121. doi: 10.1016/j.brs.2008.02.001. [DOI] [PubMed] [Google Scholar]
- 134.McCracken CB, Grace AA. High-frequency deep brain stimulation of the nucleus accumbens region suppresses neuronal activity and selectively modulates afferent drive in rat orbitofrontal cortex in vivo. J Neurosci. 2007;27:12601–12610. doi: 10.1523/JNEUROSCI.3750-07.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Morrell MJ. Responsive cortical stimulation for the treatment of medically intractable partial epilepsy. Neurology. 2011;77:1295–1304. doi: 10.1212/WNL.0b013e3182302056. [DOI] [PubMed] [Google Scholar]
- 136.Skoog G, Skoog I. A 40-year follow-up of patients with obsessive-compulsive disorder. Arch Gen Psychiatry. 1999;56:121–127. doi: 10.1001/archpsyc.56.2.121. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)
(PDF 1.19 mb)
(PDF 1.19 mb)
(PDF 1224 kb)