Abstract
Deep brain stimulation (DBS) is an implanted electrical device that modulates specific targets in the brain resulting in symptomatic improvement in a particular neurologic disease, most commonly a movement disorder. It is preferred over previously used lesioning procedures due to its reversibility, adjustability, and ability to be used bilaterally with a good safety profile. Risks of DBS include intracranial bleeding, infection, malposition, and hardware issues, such migration, disconnection, or malfunction, but the risk of each of these complications is low—generally ≤ 5% at experienced, large-volume centers. It has been used widely in essential tremor, Parkinson’s disease, and dystonia when medical treatment becomes ineffective, intolerable owing to side effects, or causes motor complications. Brain targets implanted include the thalamus (most commonly for essential tremor), subthalamic nucleus (most commonly for Parkinson’s disease), and globus pallidus (Parkinson’s disease and dystonia), although new targets are currently being explored. Future developments include brain electrodes that can steer current directionally and systems capable of “closed loop” stimulation, with systems that can record and interpret regional brain activity and modify stimulation parameters in a clinically meaningful way. New, image-guided implantation techniques may have advantages over traditional DBS surgery.
Electronic supplementary material
The online version of this article (doi:10.1007/s13311-014-0274-1) contains supplementary material, which is available to authorized users.
Keywords: Deep brain stimulation, Movement disorders, Essential tremor, Parkinson’s disease, Dystonia
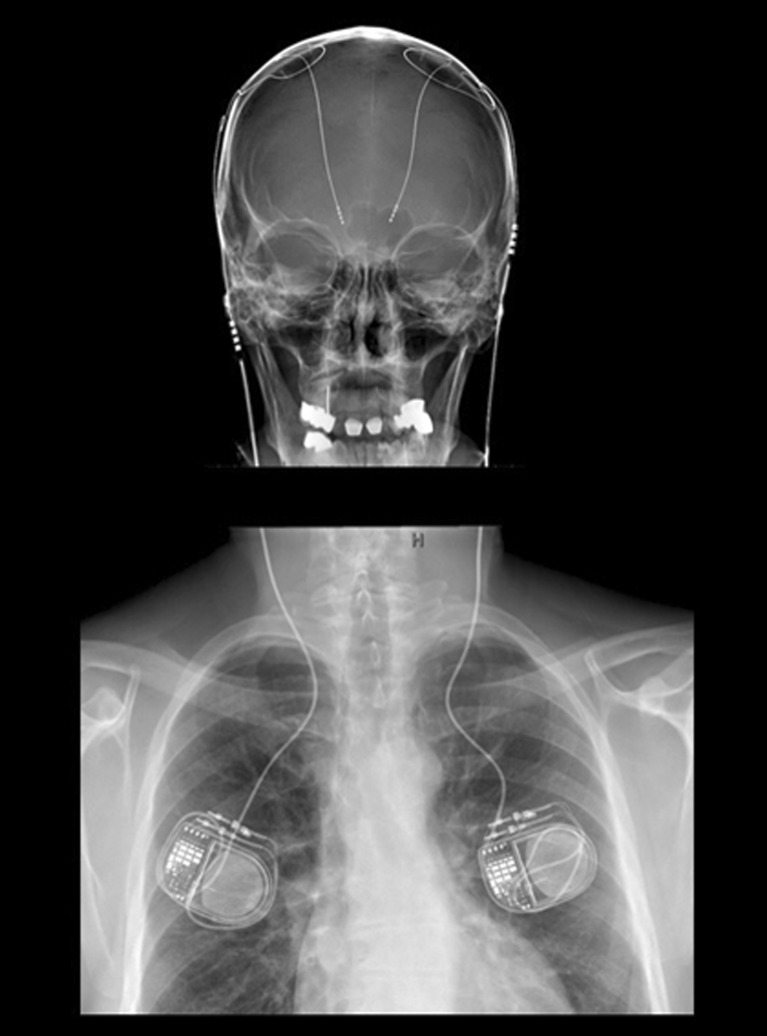
Deep brain stimulation (DBS) is a surgically implanted electronic device used to modulate the neuronal activity in a particular brain region or circuit. One or two electrodes (often referred to as leads) are placed in a specific target in the brain using various stereotactic neurosurgical techniques. The leads are connected to a small internal pulse generator (IPG), which usually resides under the skin in the chest and contains the electronics that generate the stimulating pulses, as well as the battery that powers the system (Fig. 1). Although the exact mechanism of action of DBS is not known and challenging to study in humans, it has both excitatory and inhibitory local effects, as well as widespread network influence, which together can result in symptomatic improvement in a particular disease, most commonly a movement disorder [1–5]. DBS has become the gold standard treatment for many of the most common movement disorders when pharmacologic therapies fail to adequately control symptoms, are not tolerated owing to side effects, or result in motor complications [6, 7].
Fig. 1.
Composite X-rays showing an implanted deep brain stimulation system. The brain leads have 4 circumferential stimulating surfaces (contacts) located at their distal end. In this example, the leads are connected to bilateral single channel pulse generators in the chest; alternatively, both leads could be connected to a larger, 2-channel pulse generator located on either side
DBS first appeared in the literature in 1991 as a potential surgical treatment for human movement disorders, specifically tremor related to Parkinson disease (PD) and essential tremor (ET) [8, 9]. Up to this point, the mainstay of surgical treatment for movement disorders were lesioning procedures, which involved creating a permanent destructive lesion in a specific brain target believed to be involved in the pathophysiology of motor symptoms. For tremor alone, the target was typically the ventral intermediate nucleus (Vim) of the thalamus; for treating tremor, as well as other symptoms of PD, the target was the internal segment of the globus pallidus (GPi) [10–12]. Although clinically effective, these procedures were destructive, irreversible, and in many cases resulted in a higher incidence of complications (including difficulties with speech and cognition) when performed bilaterally [13, 14]. DBS rapidly overtook lesioning as the surgical treatment of choice for a number of reasons. It was nondestructive and, unlike lesioning, it was adjustable; several stimulation parameters, including the location, size, intensity, and even to a certain degree the shape of the stimulating current field, could be adjusted by the practitioner. This allowed clinicians to program the DBS device in such a way as to maximize motoric and minimize side effects, most of which were caused by inadvertent stimulation of structures adjacent to the intended target. Perhaps most importantly, DBS had a lower reported complication rate when used bilaterally [14, 15].
Despite its popularity with both clinicians and patients, DBS also has some drawbacks. The initial cost of the implanted hardware is high, approaching or exceeding $20,000 in the USA. Some studies have presented arguments that DBS is cost-effective in the long term owing to increased quality of life with maintained economic productivity and decreased ongoing medical costs [16, 17]. DBS is subject to hardware-related complications that do not exist with lesioning, such as migration, disconnection, or mechanical malfunction, although the risk of such events is < 2% [18]. The infection rate is definitely higher than lesioning due to the implantation of foreign bodies. The infection rate requiring surgical intervention in well-controlled, large series done at single centers is between 1.7% and 4.5% [18–20]. The rate of symptomatic intracranial hemorrhage in large, single-center series is < 1.5% [18, 21, 22]. Finally, the adjustability of DBS requires more frequent and ongoing follow-up with the neurologist to find and maintain the optimal stimulation parameters. This represents a larger time commitment on the part of the patient, as well as the treatment team, and requires highly trained and experienced practitioners.
DBS has been applied to a variety of movement disorders, but by far the most common [and US Food and Drug Administration (FDA)-approved] indications for DBS are essential tremor, PD, and dystonia. What follows is a brief overview of DBS in these disorders. Each section includes a short list of publications for that disorder that are interesting or unique in some way. Some of these are considered landmark papers, while others are notable because they represent early work in a new target, have a unique study design, or are considered controversial in some circles. Highlighting these particular publications are meant to stimulate further reading and critical thinking, not to be dismissive of other papers; on the contrary, there is very high-quality research being conducted by many centers in the field of DBS. DBS has also been used experimentally for less common movement disorders (including those secondary to multiple sclerosis and trauma, spinocerebellar ataxia, and Holmes tremor). Owing to their rare nature and the relatively small volume of outcomes data, they will not be discussed here.
Essential Tremor
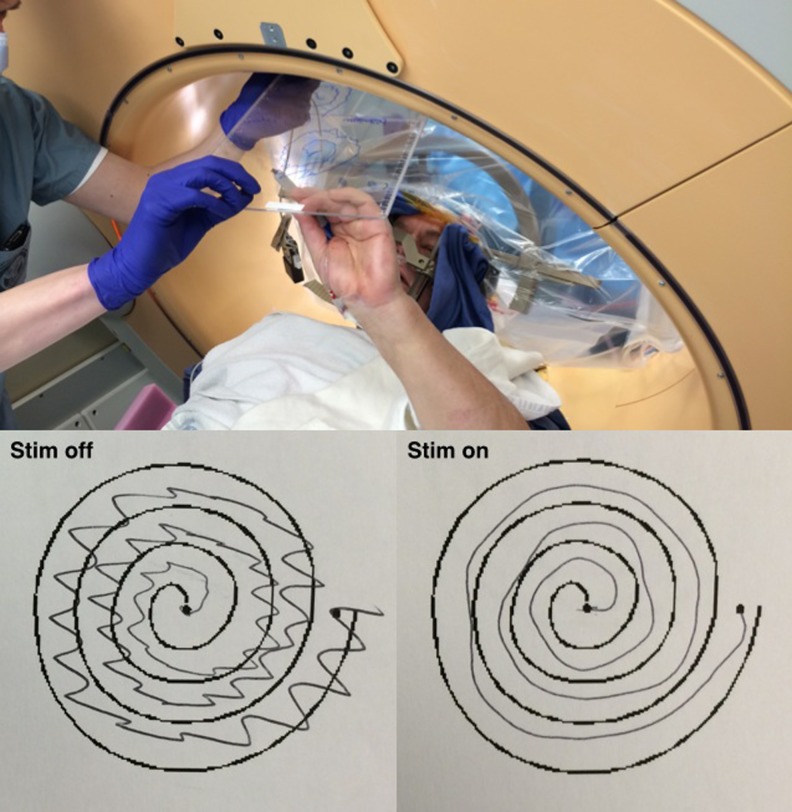
Essential tremor is the most common movement disorder, with a prevalence of 4.0–5.6% in persons over the age of 40 years; this rises to as high as 9.0% in people over the age of 60 years [23–25]. Historically referred to as “benign essential tremor”, the disorder can, in fact, be quite disabling, with social anxiety, distress, and isolation owing to the tremor being perhaps as disabling as the tremor itself [26]. The exact pathophysiology is unknown. The tremor typically involves the upper extremities, but can also be present in the head, voice, and the lower extremities. Although the absence of resting tremor is often a differentiating feature between ET and PD, patients with ET can have a resting component to their tremor, as well as other features, such as tandem gait disturbance [27, 28]. There is frequently a family history of ET, and the tremor is often responsive to alcohol consumption. The mainstays of medical treatment are propranolol and primidone, although these agents only provide acceptable tremor control without bothersome side effects in roughly 50–70% of patients [29]. Other agents that may provide some benefit include topiramate, atenolol, alprazolam, clonazepam, sotalol, and zonisamide [28]. The severity of tremor is measured objectively using scales such as the Fahn–Tolosa–Marin Tremor Rating Scale or the Essential Tremor Rating Scale. Drawing spirals or writing their name is a rapid way of assessing tremor during awake surgery or DBS programming in the office (Fig. 2).
Fig. 2.
(Top) Stereotactic deep brain stimulation (DBS) implantation in an awake patient with essential tremor. The DBS lead has been placed into the right thalamus, and the patient is being asked to trace a spiral on a clipboard. (Bottom) The ability of the patient to perform this task is compared with stimulation off and stimulation on, and the result is used, in part, to determine intraoperatively if the lead is appropriately placed in the thalamus
Historically, the most commonly used target for DBS in ET is the Vim, and this is currently the only US FDA-approved target for DBS in the USA. Numerous studies report significant improvement with both unilateral and bilateral Vim stimulation, with long-term follow-up showing anywhere from 40% to 80% reduction in tremor severity and corresponding improvement in quality of life [30–36]. Stimulation-induced adverse effects, including dysarthria, paresthesias, and ataxia can present in upwards of 30% of patients receiving bilateral stimulation [31, 35, 37, 38]. Although these are reversible by changing the stimulation parameters, this may complicate the clinician’s ability to program the device in a way that maximizes tremor control. Approximately 10% of patients do not have adequate tremor control with Vim stimulation (particularly those with a proximal component to their upper extremity tremor), and upwards of 15–20% of patients improve initially, but then lose efficacy within the first year of surgery [39, 40]. It is unclear if the loss of benefit in the latter group is due to progression of disease or development of tolerance to stimulation.
Other targets have emerged as an alternative to the Vim for patients with ET. To date, the most widely studied area is inferior to the thalamus, and posterior and superior to the subthalamic nucleus (STN). Several targets have stimulated by different centers in this region, including zona incerta and the prelemniscal radiations, although as is the case with most DBS targets it is difficult to tell exactly where the mechanism of action is taking place. A broader anatomic term that incorporates both of these targets is the posterior subthalamic area (PSA). This region is of interest because it appears to provide tremor reduction that is comparable to Vim but may have a lower adverse effect profile, better efficacy with proximal and intention tremor, and may avoid the question of “tolerance” seen with Vim stimulation [41–45]. However, many of these early studies are small, others have a heterogeneous patient population that include disorders other than ET, and not all seem to have a rigorous analysis of stimulation-related adverse events. More recent studies have started to compare PSA to Vim directly, with better overall results seen with PSA stimulation [46, 47]. A number of centers have abandoned Vim DBS (particularly outside the USA), and our own center is starting to use the PSA in cases of failed Vim DBS. More work is needed in this area with prospective, randomized and blinded studies.
Table 1 shows a list of interesting reading to learn more about DBS for essential tremor.
Table 1.
Interesting reading—deep brain stimulation (DBS) for essential tremor
| Authors [ref.] | Why it is interesting | Potential shortcomings |
|---|---|---|
| Rehncrona et al. [36] | Open-label stimulation, then double-blind assessment. Long follow-up, 6–7 years. No disease progression seen (n = 19). Very little change in stimulation parameters over time | Difficult to blind patients with thalamic stimulation. Different washout periods used at 2-year evaluation and 6–7-year evaluation. No lead location data |
| Favilla et al. [40] | Twenty-eight DBS patients compared with 21 age-matched controls over time. Six DBS patients showed disease progression off stimulation similar to controls. One possible stimulation tolerance | Retrospective. Possible microthalamotomy in DBS patients may confound results. No detailed lead location data. Patient with possible tolerance had suboptimal lead location |
| Fytagoridis et al. [45] | Prospective (n = 15). Mean ETRS improvement decreased slightly over time. Stable stimulation settings. Detailed lead locations | Open label. All but 2 patients implanted unilaterally. Limited discussion of complications of stimulation |
| Baizabal-Carvallo et al. [30] | Very long follow-up, 8–13 years. Number of IPG replacements, complications of surgery and stimulation included | Not prospective. Difficult to maintain high numbers during very long-term follow-up (n = 13). Very short washout period for stimulation-off evaluations (15 min). |
ETRS = Essential Tremor Rating Scale; IPG = internal pulse generator.
PD
Although ET is more common than PD, PD is by far the most common disorder treated with DBS. PD is a progressive neurodegenerative disorder characterized by a loss of dopaminergic neurons in the substantia nigra, as well as other brain regions, that results in varying degrees of tremor, rigidity, bradykinesia, akinesia, and postural instability in affected individuals. Nonmotor symptoms are also common, including cognitive impairment, depression, constipation, and autonomic symptoms. Although the exact prevalence of PD is not known, it is estimated to be present in 1–2% of the population in the USA over the age of 65 years with an annual economic burden in 2010 of approximately $14.4 billion [48–50]. Given the expected growth in the aging population over the next several decades, the number of people with PD is expected to double by 2040 [50]. Although PD becomes more common as age increases, the age of onset ranges from 40 to 75 years, with early-onset PD occurring in younger patients between the age of 21 and 40 years [51].
The mainstay of treatment is medical in the early stages of the disease, with the primary goal of either elevating the level of dopamine in the brain (such as with carbidopa/levodopa, the most commonly used medication) and/or prolonging the action of the dopamine that is present [52, 53]. It is important to make a distinction between idiopathic PD and atypical parkinsonism that is seen in other neurologic disorders, such as progressive supranuclear palsy and corticobasal degeneration. In idiopathic PD, dopaminergic therapy and DBS are generally effective, while in the atypical syndromes they are not [54–56]. The severity of PD at a given time point is quantified using measures such as the Unified PD Rating Scale (UPDRS), which includes both patient reported and clinician evaluated elements, and the Hoehn and Yahr scale [57–59].
Most patients with PD typically start to develop complications of medical therapy after 5–15 years of treatment with these agents. These include motor fluctuations, dyskinesia and intolerance of increasing amounts of medications required owing to progression of disease and worsening PD symptoms. It is at this stage of PD when most experts advocate DBS for properly selected patients [60–62]. Patient selection is perhaps the most important predictor of a good clinical outcome for DBS in PD, aside from proper electrode placement and appropriate stimulation parameters. One of the best predictors of response to DBS is an adequate clinical improvement with oral levodopa; most advocate at least a 25–30% improvement in the Unified PD Rating Scale Part III (clinician scored motor examination) between the off and the on medication state [61]. Generally, symptoms that improve with oral levodopa will also respond to DBS; the one possible exception is tremor in patients with tremor dominant PD. Other factors that should be considered include confidence in the diagnosis, minimal presence of nonmotor symptoms (particularly cognitive decline and depression), minimal medical comorbidities, age, realistic expectations on the part of all parties involved, reasonable social support and the ability to handle the responsibilities of a complex therapy. Many centers perform on medication, off medication examinations, as well as full neuropsychological evaluations to assess many of these factors before deciding to proceed with surgery.
The two targets used primarily for PD are the STN and the GPi. Both have been studied extensively, including a prospective, randomized blinded study in 299 patients, conducted by the Veterans Affairs Cooperative Studies Program [63]. Both targets provide fairly equivalent improvements in the cardinal motor symptoms of PD, as well as dyskinesia [63–66]. However, these studies have demonstrated some differences in these two targets that are starting to influence how centers chose one target versus the other. For example, the Veterans Affairs Cooperative Study showed that STN stimulation had a higher rate of potential worsening of cognition and mood, but allowed more aggressive medication reduction after surgery [63]. Historically, the Vim was used initially as a target for PD-related tremor, and although stimulation of the Vim does not improve any parkinsonian symptoms aside from tremor, its favorable safety profile with regard to cognition still make it a reasonable choice in very elderly or cognitively borderline patients with tremor-dominant PD.
The zona incerta/prelemniscal radiations/PSA region has been explored for PD, and some have reported equivalent or even better motoric improvement with DBS in this region compared with STN stimulation [67–69]. This target has not yet gained significant traction in PD, largely because the STN and GPi are well established, known to be effective, and are US FDA-approved. The pedunculopontine nucleus has also been proposed as a target for PD, particularly with those patients that have axial symptoms, such as freezing of gait and postural disability [70, 71]. Small clinical trials have demonstrated improvement in axial and postural symptoms in PD patients with pedunculopontine nucleus stimulation [72–75]. Larger, more rigorous studies are needed to better understand the utility of this target for PD, and further work is needed to clarify the optimal target in this structure and when it should be considered as a standalone target versus in combination with another target, such as STN.
There has been a recent change in thinking regarding the timing of DBS surgery in PD. Current practice dictates that DBS not be considered until patients progress to the point where they start to develop either motor fluctuations and/or dyskinesias. However, by this point, many patients have already experienced significant decline in quality of life, social impairment, and interruption of professional activity if they are still working. Some clinicians advocating surgery earlier in the disease course, when patients are more dopamine responsive and nonmotor symptoms have not yet become significant [76]. A recent, highly anticipated clinical trial (EARLYSTIM) in 251 patients provided data showing that quality of life scores were higher when DBS was done in earlier stage PD patients [77]. The patient population in this study was carefully selected, and some feel that the age, high dopamine responsiveness, and the lack of comorbidities in this cohort of patients (particularly with respect to cognition and mood) do not accurately represent “typical” PD patients. Further work is ongoing in this area.
Table 2 shows a list of interesting reading to learn more about DBS for PD.
Table 2.
Interesting reading—deep brain stimulation (DBS) for Parkinson disease (PD)
| Publication | Why it is interesting | Potential shortcomings |
|---|---|---|
| Follett et al. [63] | Very large (n = 299). Prospective, double blind to target, 2-year follow-up. Primary outcome UPDRS, extensive QoL and neuropsychological data collected. Motor improvement lower than expected in both targets. Interesting differences seen between targets in secondary outcomes | Multicenter (6 VA + 6 university affiliates), potential for inconsistent implantation and programming. Blinded programmers may result in suboptimal programming. Lower than expected motor improvement in both targets questions generalizability of data |
| Odekerken et al. [66] | Large (n = 128). Prospective, double blind. Novel primary outcomes of disability and composite score for cognition, mood and behavior. Lower average preoperative Hoehn and Yahr than VA study (2.5 vs 3.3). | Very little detail on surgical technique or lead location. Larger than expected variance in primary outcome (disability) measure makes data susceptible to a type II statistical error |
| Schuepbach et al. [77] | Large (n = 251). Earlier-stage PD patients, prospectively randomized to DBS + medical treatmen or medical treatment alone. QoL primary outcome. First large study to examine DBS in earlier stage PD. | Inclusion criteria of > 50% improvement with dopaminergic meds resulted in highly selected patients; may not represent “typical” DBS candidates. Upper age limit of 60 years. Only STN stimulated |
UPDRS = Unified Parkinson Disease Rating Scale; QoL = quality of life; VA = Veterans Affairs; STN = subthalamic nucleus.
Dystonia
Dystonia is a movement disorder characterized by abnormal, sustained muscle contractions, often in agonist and antagonist muscle groups, which result in abnormal postures or repetitive movements. Dystonias occur in a variety of settings and, as such, are classified according to age of onset, anatomic distribution, and cause [78]. Age of onset can be early (<26 years) or late; early-onset dystonia is a common movement disorder in the pediatric population. Anatomic distribution can be generalized (affecting the majority or all of the body), segmental (two adjacent body regions), multifocal (multiple regions that are not all adjacent), or focal (one body part, such as the hand in writer’s cramp). Causes can be primary or secondary. Primary dystonias are characterized by a lack of any identifiable cause or underling neurologic abnormality. These are frequently, but not always, associated with known genetic mutations, such as DYT1 (associated with early-onset torsional dystonia) or DYT6 (autosomal dominant dystonia, frequently cranio-cervical) [79, 80]. Secondary dystonias are associated with a known risk factor or cause. Examples include tardive dystonia, which is associated with prior neuroleptic or antiemetic use, and dystonias associated with cerebral palsy, Wilson’s disease, multiple sclerosis, and stroke [81–84]. The severity of dystonia is quantified by several rating scales, such as the Burk–Fahn–Marsden Dystonia Rating Scale (BFMDRS) for generalized dystonia and the Toronto–Western Spasmodic Torticollis Rating Scale for cervical and craniocervical dystonia.
As we have seen with the other movement disorders, the initial treatment is medical, with anticholinergics, gamma-aminobutyric acidergics, benzodiazepines, muscle relaxants (particularly baclofen, either oral or intrathecal), and physical or occupational therapy [85]. While effective in some cases, they frequently cause side effects that are not tolerated. Botulinum toxin has been used for focal and regional treatment of more widespread dystonias, including blepharospasm, spasmodic dysphonia, writer’s cramp, and cervical dystonia [85]. DBS is considered when medical treatments are either ineffective or not tolerated, and the degree of disability and/or disease burden on either the patient or caregiver is sufficiently high to warrant surgical intervention. Unlike the other movement disorders, dystonia is unique in that there are other “nonmotor” factors to consider prior to surgery. These include the caregiver and home environments (particularly for pediatric patients), how prominent pain is as a feature of the dystonia (and how that has been managed), and whether there is a fixed skeletal deformity present that would limit functional outcome.
Historically, the target of choice for DBS in dystonia has been the GPi; although effective, there are some drawbacks to this target. These include stimulation-induced bradykinesia in previously asymptomatic body parts with bilateral implantation, and a delay of weeks, months, or even years between onset of stimulation and realization of maximal clinical benefit [86–88]. This may reflect a different mechanism of action of DBS in dystonia, at least when using this target. More recently, the STN has been proposed as a target for primary and cervical dystonia [89–91]. The STN may avoid stimulation-induced bradykinesia, but other issues, such as transient dyskinesia and possible weight gain in some patients, have been observed. Finally, there are a few published reports of DBS in the ventrooralis and Vim nucleus of the thalamus for writer’s cramp and the ventrooralis anterior nucleus for a postanoxic dystonia [92, 93]. Larger, prospective studies are needed to compare and contrast these targets in a scientifically meaningful way [94].
It is interesting that the various subtypes of dystonia respond to DBS differently. Primary generalized dystonia has been the most studied, and bilateral GPi stimulation generally results in a 60–85% improvement in the BFMDRS in open-label studies and roughly 40–50% improvement in prospective, double-blind randomized trials with 6–12 months of follow-up [80, 95–99]. Improvement in the secondary dystonias is more variable and appears to be dependent on the cause. Of these, tardive dystonia appears to have the most favorable outcome to DBS, with several small, open-label studies showing a 50–70% improvement [100, 101]. DBS for other secondary dystonias, such as cerebral palsy, have shown less favorable results with improvements in BFMDRS in the range of ≤ 20% [102, 103]. Primary cervical and craniocervical dystonias fare better, with a 40% to > 70% improvement in Toronto–Western Spasmodic Torticollis Rating Scale severity [104–107].
Table 3 shows a list of interesting reading to learn more about DBS for dystonia.
Table 3.
Interesting reading—deep brain stimulation (DBS) for dystonia
| Publication | Why it is interesting | Potential shortcomings |
|---|---|---|
| Kupsch et al. [98] | Large (n = 40). Prospective, randomized, and sham-controlled (sham stimulation period) with blinded assessors | Blinded phase only 3 months long. Follow-up for open label stimulation period only 6 months. Detailed lead location data not provided |
| Walsh et al. [107] | Prospective. Two blinded video raters. Very long follow-up, 5 to almost 11 years. Most improvement was realized in first year | n = 10. Prospective blinded rating difficult to maintain over such a long time span. Detailed lead location data not provided |
| Damier et al. [100] | Largest (n = 10) series of DBS for tardive dystonia. Prospective. Double-blind on/off evaluation after 6 months open-label stimulation. Used unique rating scale (ESRS). Pooled lead location data provided | Unclear if blinded on/off evaluation fully accounted for potential washout. Hard to compare ESRS outcomes with other studies. Ten patients enrolled at 6 centers; unclear if consistency a factor |
| Schjerling et al. [94] | First prospective (n = 13) comparison of 2 targets for dystonia. Simultaneous implantation of STN and GPi. Randomized and blinded to one target then other for 6 months each. Well-documented lead locations | Five of 13 did not follow original crossover protocol. Rating scales changed during study. Lead location suboptimal in 3 patients. Maximum amplitude of 4v may be too low. Implications of microlesion effects/stimulation in one target before other not known |
ESRS = Extrapyramidal Symptom Rating Scale; STN = subthalamic nucleus; GPi = globus pallidus.
Future Directions
As successful as DBS for movement disorders has been, there are a number of areas of potential growth for the device, stimulation paradigms, and implantation techniques. The commercially available IPGs have gone through several generations with slow, but incremental, increases in sophistication. However, the DBS leads that are in use today are of the same design as the leads that were used in the late 1990s. They consist of 4 stimulating surfaces (often referred to as contacts) that are only capable of concentric stimulation. The contacts can be neutral, or positively or negatively charged, which allows for some shaping or “steering” of the stimulation current vertically (i.e., along the long axis of the lead). Current steering is desirable to maximize current delivery to the intended target and limit spread of current to adjacent structures, which can cause stimulation-induced adverse effects. Unfortunately, for the targets commonly used in movement disorders, the adjacent structures of concern are almost always lateral to the lead, and none of the commercially available leads are capable of steering current laterally. Leads capable of lateral current steering are currently under development by a number of companies. This is an obvious and long overdue improvement that will significantly improve patient outcomes and reduce reoperation rates.
Another area of development is the establishment of closed loop stimulation. Current DBS systems are not capable of recording neuronal activity of any kind, and deliver stimulation continuously based on the parameters that were set in the last programming session. As a result, DBS is not “responsive”; it does not change according to the patient’s disease or behavioral state. Closed loop stimulation paradigms consist of some form of sensing function that provides feedback to the IPG, which then alters the stimulation in a meaningful way [5, 108, 109]. A neuromodulation device for epilepsy recently incorporated such technology, and the major manufacturer of DBS systems worldwide has a closed loop system under investigation [110, 111]. One challenge with closed loop paradigms is to determine what neuronal signal to look for in a chronically behaving human; there are very good, acute studies of both subcortical and cortical physiology with and without active stimulation, but chronic studies in humans are lacking [112, 113].
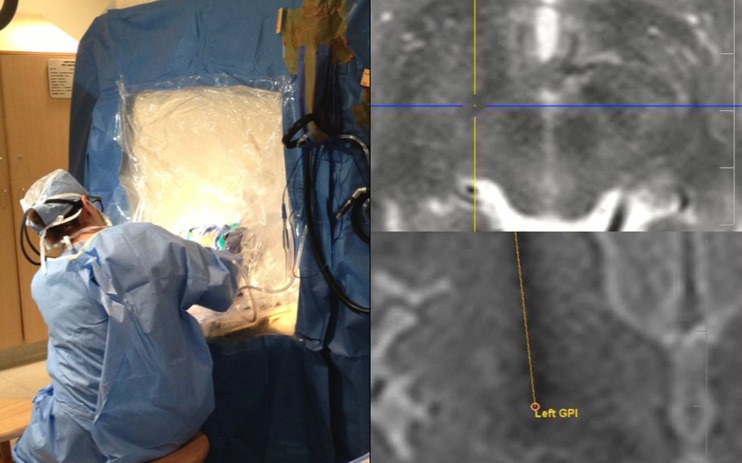
The traditional method of DBS implantation involves frame-based stereotactic surgery with some form of physiologic mapping and testing to ensure that the optimal location within the target has been implanted (Fig. 2). This mapping and testing can take the form of microelectrode recording of single neurons, local field potential recording of populations of neurons, or macrostimulation of the intended target with observation of the patient for improvement in symptoms and/or stimulation-induced side effects that can help inform the surgeon of the proximity of adjacent structures [114]. This process is generally undertaken for a variety of reasons, primarily because we wish to implant the motor subterritories of these various targets and because there are multiple sources of potential error secondary to image fusion, intraoperative brain shift, human factors, and equipment failure. However, these techniques require that the patient be awake for much of the procedure, which is difficult for some to tolerate. It also is time consuming, technically demanding, and requires multiple brain penetrations. For targets such as the GPi and STN that are visible on particular magnetic resonance imaging (MRI) sequences, new techniques for placing DBS leads using real-time MRI guidance have been developed [115–117]. Surgery is performed entirely within a 1.5-T or 3-T MRI scanner, and relies on direct visualization of the STN or GPi as the sole method of targeting (Fig. 3). MRI is the only imaging modality used, no image fusion is needed, and targeting is performed after cranial opening so brain shift can be taken into account. These techniques are also faster, have higher accuracy than a stereotactic frame, can detect intraoperative complications, and reduce the procedure to a single brain penetration in most cases [117, 118]. They also allow the patient to be under general anesthesia while producing clinical outcomes that are comparable to traditional, awake surgery [119]. Computed tomography has also been used for asleep, image-guided surgery with comparable accuracy [120]. This technique is fast and easier to implement, as it does not involve the technical complexities of performing surgery within an MRI scanner. However, it is still reliant on the fusion of intraoperative computed tomography images (with low tissue discrimination and varying degrees of brain shift) to preoperative MRI for targeting and evaluation of placement error. Time will tell how these techniques compare with each other and with traditional, awake surgery.
Fig. 3.
Interventional magnetic resonance imaging (MRI) deep brain stimulation lead placement. (Left) A custom drape is used to create a sterile field in a standard 1.5-T scanner located in radiology. The entire procedure is performed in the MRI scanner with a plastic skull mounted aiming device and MRI compatible instrumentation. (Above right) The subthalamic nucleus is targeted using direct visualization of the nucleus on T2-weighted MRI images. (Below right) Real-time imaging is used to monitor insertion; in this case, the globus pallidus (GPi) is being implanted
Finally, although DBS has largely supplanted traditional lesioning surgery, such as thalamotomy and pallidotomy, it is apparent that there are some situations in which the complexity of DBS therapy may not be the best choice. Examples are patients who are at a very high risk of infection or have had DBS explanted owing to multiple infections; who are geographically and/or socially isolated such that programming would be logistically difficult; and in whom unilateral treatment would be reasonable. After many years of moving almost completely away from lesioning, our center is using it again in selected cases, and this approach is not only shared by others, but may also be expanding owing to new technology in surgical lesioning techniques [121, 122].
Electronic supplementary material
(PDF 1224 kb)
References
- 1.Agnesi F, Johnson MD, Vitek JL. Deep brain stimulation: how does it work? Handb Clin Neurol. 2013;116:39–54. doi: 10.1016/B978-0-444-53497-2.00004-8. [DOI] [PubMed] [Google Scholar]
- 2.Li Q, Qian ZM, Arbuthnott GW, Ke Y, Yung WH. Cortical effects of deep brain stimulation: implications for pathogenesis and treatment of Parkinson disease. JAMA Neurol. 2014;71:100–103. doi: 10.1001/jamaneurol.2013.4221. [DOI] [PubMed] [Google Scholar]
- 3.Arle JE, Mei LZ, Shils JL. Modeling parkinsonian circuitry and the DBS electrode. I. Biophysical background and software. Stereotact Funct Neurosurg. 2008;86:1–15. doi: 10.1159/000108584. [DOI] [PubMed] [Google Scholar]
- 4.Shils JL, Mei LZ, Arle JE. Modeling parkinsonian circuitry and the DBS electrode. II. Evaluation of a computer simulation model of the basal ganglia with and without subthalamic nucleus stimulation. Stereotact Funct Neurosurg. 2008;86:16–29. doi: 10.1159/000108585. [DOI] [PubMed] [Google Scholar]
- 5.Chang JY, Shi LH, Luo F, Zhang WM, Woodward DJ. Studies of the neural mechanisms of deep brain stimulation in rodent models of Parkinson's disease. Neurosci Biobehav Rev. 2008;32:352–366. doi: 10.1016/j.neubiorev.2007.09.002. [DOI] [PubMed] [Google Scholar]
- 6.Fox SH, Katzenschlager R, Lim SY, Ravina B, Seppi K, Coelho M, et al. The Movement Disorder Society Evidence-Based Medicine Review Update: Treatments for the motor symptoms of Parkinson's disease. Move Disord. 2011;26(Suppl. 3):S2–41. doi: 10.1002/mds.23829. [DOI] [PubMed] [Google Scholar]
- 7.Weaver FM, Follett K, Stern M, Hur K, Harris C, Marks WJ, Jr, et al. Bilateral deep brain stimulation vs best medical therapy for patients with advanced Parkinson disease: a randomized controlled trial. JAMA. 2009;301:63–73. doi: 10.1001/jama.2008.929. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Benabid AL, Pollak P, Gervason C, Hoffmann D, Gao DM, Hommel M, et al. Long-term suppression of tremor by chronic stimulation of the ventral intermediate thalamic nucleus. Lancet. 1991;337:403–406. doi: 10.1016/0140-6736(91)91175-t. [DOI] [PubMed] [Google Scholar]
- 9.Blond S, Siegfried J. Thalamic stimulation for the treatment of tremor and other movement disorders. Acta Neurochir Suppl (Wien) 1991;52:109–111. doi: 10.1007/978-3-7091-9160-6_30. [DOI] [PubMed] [Google Scholar]
- 10.Nagaseki Y, Shibazaki T, Hirai T, Kawashima Y, Hirato M, Wada H, et al. Long-term follow-up results of selective VIM-thalamotomy. J Neurosurg. 1986;65:296–302. doi: 10.3171/jns.1986.65.3.0296. [DOI] [PubMed] [Google Scholar]
- 11.Laitinen LV, Bergenheim AT, Hariz MI. Ventroposterolateral pallidotomy can abolish all parkinsonian symptoms. Stereotact Funct Neurosurg. 1992;58:14–21. doi: 10.1159/000098965. [DOI] [PubMed] [Google Scholar]
- 12.Laitinen LV, Bergenheim AT, Hariz MI. Leksell's posteroventral pallidotomy in the treatment of Parkinson's disease. J Neurosurg. 1992;76:53–61. doi: 10.3171/jns.1992.76.1.0053. [DOI] [PubMed] [Google Scholar]
- 13.Intemann PM, Masterman D, Subramanian I, DeSalles A, Behnke E, Frysinger R, et al. Staged bilateral pallidotomy for treatment of Parkinson disease. J Neurosurg. 2001;94:437–444. doi: 10.3171/jns.2001.94.3.0437. [DOI] [PubMed] [Google Scholar]
- 14.Schuurman PR, Bosch DA, Merkus MP, Speelman JD. Long-term follow-up of thalamic stimulation versus thalamotomy for tremor suppression. Move Disord. 2008;23:1146–1153. doi: 10.1002/mds.22059. [DOI] [PubMed] [Google Scholar]
- 15.Tasker RR. Deep brain stimulation is preferable to thalamotomy for tremor suppression. Surg Neurol. 1998;49:145–153. doi: 10.1016/s0090-3019(97)00459-x. [DOI] [PubMed] [Google Scholar]
- 16.Dams J, Siebert U, Bornschein B, Volkmann J, Deuschl G, Oertel WH, et al. Cost-effectiveness of deep brain stimulation in patients with Parkinson's disease. Move Disord. 2013;28:763–771. doi: 10.1002/mds.25407. [DOI] [PubMed] [Google Scholar]
- 17.Eggington S, Valldeoriola F, Chaudhuri KR, Ashkan K, Annoni E, Deuschl G. The cost-effectiveness of deep brain stimulation in combination with best medical therapy, versus best medical therapy alone, in advanced Parkinson's disease. J Neurol. 2014;261:106–116. doi: 10.1007/s00415-013-7148-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Fenoy AJ, Simpson RK., Jr Risks of common complications in deep brain stimulation surgery: management and avoidance. J Neurosurg. 2014;120:132–139. doi: 10.3171/2013.10.JNS131225. [DOI] [PubMed] [Google Scholar]
- 19.Sillay KA, Larson PS, Starr PA. Deep brain stimulator hardware-related infections: incidence and management in a large series. Neurosurgery. 2008;62:360–366. doi: 10.1227/01.neu.0000316002.03765.33. [DOI] [PubMed] [Google Scholar]
- 20.Piacentino M, Pilleri M, Bartolomei L. Hardware-related infections after deep brain stimulation surgery: review of incidence, severity and management in 212 single-center procedures in the first year after implantation. Acta Neurochir. 2011;153:2337–2341. doi: 10.1007/s00701-011-1130-2. [DOI] [PubMed] [Google Scholar]
- 21.Binder DK, Rau G, Starr PA. Hemorrhagic complications of microelectrode-guided deep brain stimulation. Stereotact Funct Neurosurg. 2003;80:28–31. doi: 10.1159/000075156. [DOI] [PubMed] [Google Scholar]
- 22.Falowski S, Ooi YC, Smith A, Verhargen Metman L, Bakay RA. An evaluation of hardware and surgical complications with deep brain stimulation based on diagnosis and lead location. Stereotact Funct Neurosurg. 2012;90:173–180. doi: 10.1159/000338254. [DOI] [PubMed] [Google Scholar]
- 23.Dogu O, Sevim S, Camdeviren H, Sasmaz T, Bugdayci R, Aral M, et al. Prevalence of essential tremor: door-to-door neurologic exams in Mersin Province, Turkey. Neurology. 2003;61:1804–1806. doi: 10.1212/01.wnl.0000099075.19951.8c. [DOI] [PubMed] [Google Scholar]
- 24.Rautakorpi I, Takala J, Marttila RJ, Sievers K, Rinne UK. Essential tremor in a Finnish population. Acta Neurol Scand. 1982;66:58–67. doi: 10.1111/j.1600-0404.1982.tb03129.x. [DOI] [PubMed] [Google Scholar]
- 25.Louis ED, Ottman R, Hauser WA. How common is the most common adult movement disorder? estimates of the prevalence of essential tremor throughout the world. Move Disord. 1998;13:5–10. doi: 10.1002/mds.870130105. [DOI] [PubMed] [Google Scholar]
- 26.Lundervold DA, Ament PA, Holt P. Social anxiety, tremor severity, and tremor disability: a search for clinically relevant measures. Psychiatry J. 2013;2013:257459. doi: 10.1155/2013/257459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Deuschl G, Elble R. Essential tremor—neurodegenerative or nondegenerative disease towards a working definition of ET. Move Disord. 2009;24:2033–2041. doi: 10.1002/mds.22755. [DOI] [PubMed] [Google Scholar]
- 28.Zesiewicz TA, Shaw JD, Allison KG, Staffetti JS, Okun MS, Sullivan KL. Update on treatment of essential tremor. Curr Treat Options Neurol. 2013;15:410–423. doi: 10.1007/s11940-013-0239-4. [DOI] [PubMed] [Google Scholar]
- 29.Deuschl G, Raethjen J, Hellriegel H, Elble R. Treatment of patients with essential tremor. Lancet Neurol. 2011;10:148–161. doi: 10.1016/S1474-4422(10)70322-7. [DOI] [PubMed] [Google Scholar]
- 30.Baizabal-Carvallo JF, Kagnoff MN, Jimenez-Shahed J, Fekete R, Jankovic J. The safety and efficacy of thalamic deep brain stimulation in essential tremor: 10 years and beyond. J Neurol Neurosurg Psychiatry. 2014;85:567–572. doi: 10.1136/jnnp-2013-304943. [DOI] [PubMed] [Google Scholar]
- 31.Zhang K, Bhatia S, Oh MY, Cohen D, Angle C, Whiting D. Long-term results of thalamic deep brain stimulation for essential tremor. J Neurosurg. 2010;112:1271–1276. doi: 10.3171/2009.10.JNS09371. [DOI] [PubMed] [Google Scholar]
- 32.Pilitsis JG, Metman LV, Toleikis JR, Hughes LE, Sani SB, Bakay RA. Factors involved in long-term efficacy of deep brain stimulation of the thalamus for essential tremor. J Neurosurg. 2008;109:640–646. doi: 10.3171/JNS/2008/109/10/0640. [DOI] [PubMed] [Google Scholar]
- 33.Blomstedt P, Hariz GM, Hariz MI, Koskinen LO. Thalamic deep brain stimulation in the treatment of essential tremor: a long-term follow-up. Br J Neurosurg. 2007;21:504–509. doi: 10.1080/02688690701552278. [DOI] [PubMed] [Google Scholar]
- 34.Limousin P, Speelman JD, Gielen F, Janssens M. Multicentre European study of thalamic stimulation in parkinsonian and essential tremor. J Neurol Neurosurg Psychiatry. 1999;66:289–296. doi: 10.1136/jnnp.66.3.289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Sydow O, Thobois S, Alesch F, Speelman JD. Multicentre European study of thalamic stimulation in essential tremor: a six year follow up. J Neurol Neurosurg Psychiatry. 2003;74:1387–1391. doi: 10.1136/jnnp.74.10.1387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Rehncrona S, Johnels B, Widner H, Tornqvist AL, Hariz M, Sydow O. Long-term efficacy of thalamic deep brain stimulation for tremor: double-blind assessments. Move Disord. 2003;18:163–170. doi: 10.1002/mds.10309. [DOI] [PubMed] [Google Scholar]
- 37.Putzke JD, Uitti RJ, Obwegeser AA, Wszolek ZK, Wharen RE. Bilateral thalamic deep brain stimulation: midline tremor control. J Neurol Neurosurg Psychiatry. 2005;76:684–690. doi: 10.1136/jnnp.2004.041434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Pahwa R, Lyons KL, Wilkinson SB, Carpenter MA, Troster AI, Searl JP, et al. Bilateral thalamic stimulation for the treatment of essential tremor. Neurology. 1999;53:1447–1450. doi: 10.1212/wnl.53.7.1447. [DOI] [PubMed] [Google Scholar]
- 39.Benabid AL, Pollak P, Gao D, Hoffmann D, Limousin P, Gay E, et al. Chronic electrical stimulation of the ventralis intermedius nucleus of the thalamus as a treatment of movement disorders. J Neurosurg. 1996;84:203–214. doi: 10.3171/jns.1996.84.2.0203. [DOI] [PubMed] [Google Scholar]
- 40.Favilla CG, Ullman D, Wagle Shukla A, Foote KD, Jacobson CEt, Okun MS. Worsening essential tremor following deep brain stimulation: disease progression versus tolerance. Brain 2012;135:1455-1462. [DOI] [PubMed]
- 41.Murata J, Kitagawa M, Uesugi H, Saito H, Iwasaki Y, Kikuchi S, et al. Electrical stimulation of the posterior subthalamic area for the treatment of intractable proximal tremor. J Neurosurg. 2003;99:708–715. doi: 10.3171/jns.2003.99.4.0708. [DOI] [PubMed] [Google Scholar]
- 42.Plaha P, Patel NK, Gill SS. Stimulation of the subthalamic region for essential tremor. J Neurosurg. 2004;101:48–54. doi: 10.3171/jns.2004.101.1.0048. [DOI] [PubMed] [Google Scholar]
- 43.Hamel W, Herzog J, Kopper F, Pinsker M, Weinert D, Muller D, et al. Deep brain stimulation in the subthalamic area is more effective than nucleus ventralis intermedius stimulation for bilateral intention tremor. Acta Neurochir. 2007;149:749–758. doi: 10.1007/s00701-007-1230-1. [DOI] [PubMed] [Google Scholar]
- 44.Blomstedt P, Sandvik U, Tisch S. Deep brain stimulation in the posterior subthalamic area in the treatment of essential tremor. Move Disord. 2010;25:1350–1356. doi: 10.1002/mds.22758. [DOI] [PubMed] [Google Scholar]
- 45.Fytagoridis A, Sandvik U, Astrom M, Bergenheim T, Blomstedt P. Long term follow-up of deep brain stimulation of the caudal zona incerta for essential tremor. J Neurol Neurosurg Psychiatry. 2012;83:258–262. doi: 10.1136/jnnp-2011-300765. [DOI] [PubMed] [Google Scholar]
- 46.Blomstedt P, Lindvall P, Linder J, Olivecrona M, Forsgren L, Hariz MI. Reoperation after failed deep brain stimulation for essential tremor. World Neurosurg. 2012;78:554. doi: 10.1016/j.wneu.2011.12.013. [DOI] [PubMed] [Google Scholar]
- 47.Blomstedt P, Sandvik U, Hariz MI, Fytagoridis A, Forsgren L, Hariz GM, et al. Influence of age, gender and severity of tremor on outcome after thalamic and subthalamic DBS for essential tremor. Parkinsonism Relat Disord. 2011;17:617–620. doi: 10.1016/j.parkreldis.2011.05.014. [DOI] [PubMed] [Google Scholar]
- 48.Hirtz D, Thurman DJ, Gwinn-Hardy K, Mohamed M, Chaudhuri AR, Zalutsky R. How common are the "common" neurologic disorders? Neurology. 2007;68:326–337. doi: 10.1212/01.wnl.0000252807.38124.a3. [DOI] [PubMed] [Google Scholar]
- 49.Dorsey ER, Constantinescu R, Thompson JP, Biglan KM, Holloway RG, Kieburtz K, et al. Projected number of people with Parkinson disease in the most populous nations, 2005 through 2030. Neurology. 2007;68:384–386. doi: 10.1212/01.wnl.0000247740.47667.03. [DOI] [PubMed] [Google Scholar]
- 50.Kowal SL, Dall TM, Chakrabarti R, Storm MV, Jain A. The current and projected economic burden of Parkinson's disease in the United States. Move Disord. 2013;28:311–318. doi: 10.1002/mds.25292. [DOI] [PubMed] [Google Scholar]
- 51.Schrag A, Schott JM. Epidemiological, clinical, and genetic characteristics of early-onset parkinsonism. Lancet Neurol. 2006;5:355–363. doi: 10.1016/S1474-4422(06)70411-2. [DOI] [PubMed] [Google Scholar]
- 52.Mestre T, Ferreira JJ. Pharmacotherapy in Parkinson's disease: case studies. Ther Adv Neurol Disord. 2010;3:117–126. doi: 10.1177/1756285609352366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Jankovic J, Poewe W. Therapies in Parkinson's disease. Curr Opin Neurol. 2012;25:433–447. doi: 10.1097/WCO.0b013e3283542fc2. [DOI] [PubMed] [Google Scholar]
- 54.Stamelou M, Hoeglinger GU. Atypical parkinsonism: an update. Curr Opin Neurol. 2013;26:401–405. doi: 10.1097/WCO.0b013e3283632da6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Wenning GK, Krismer F, Poewe W. New insights into atypical parkinsonism. Curr Opin Neurol. 2011;24:331–338. doi: 10.1097/WCO.0b013e3283480569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Okun MS, Fernandez HH, Pedraza O, Misra M, Lyons KE, Pahwa R, et al. Development and initial validation of a screening tool for Parkinson disease surgical candidates. Neurology. 2004;63:161–163. doi: 10.1212/01.wnl.0000133122.14824.25. [DOI] [PubMed] [Google Scholar]
- 57.Siderowf A, McDermott M, Kieburtz K, Blindauer K, Plumb S, Shoulson I, et al. Test-retest reliability of the unified Parkinson's disease rating scale in patients with early Parkinson's disease: results from a multicenter clinical trial. Move Disord. 2002;17:758–763. doi: 10.1002/mds.10011. [DOI] [PubMed] [Google Scholar]
- 58.Goetz CG, Tilley BC, Shaftman SR, Stebbins GT, Fahn S, Martinez-Martin P, et al. Movement Disorder Society-sponsored revision of the Unified Parkinson's Disease Rating Scale (MDS-UPDRS): scale presentation and clinimetric testing results. Move Disord. 2008;23:2129–2170. doi: 10.1002/mds.22340. [DOI] [PubMed] [Google Scholar]
- 59.Goetz CG, Poewe W, Rascol O, Sampaio C, Stebbins GT, Counsell C, et al. Movement Disorder Society Task Force report on the Hoehn and Yahr staging scale: status and recommendations. Move Disord. 2004;19:1020–1028. doi: 10.1002/mds.20213. [DOI] [PubMed] [Google Scholar]
- 60.Rodriguez RL, Fernandez HH, Haq I, Okun MS. Pearls in patient selection for deep brain stimulation. Neurologist. 2007;13:253–260. doi: 10.1097/NRL.0b013e318095a4d5. [DOI] [PubMed] [Google Scholar]
- 61.Lang AE, Houeto JL, Krack P, Kubu C, Lyons KE, Moro E, et al. Deep brain stimulation: preoperative issues. Move Disord. 2006;21(Suppl. 14):S171–196. doi: 10.1002/mds.20955. [DOI] [PubMed] [Google Scholar]
- 62.Uc EY, Follett KA. Deep brain stimulation in movement disorders. Semin Neurol. 2007;27:170–182. doi: 10.1055/s-2007-971175. [DOI] [PubMed] [Google Scholar]
- 63.Follett KA, Weaver FM, Stern M, Hur K, Harris CL, Luo P, et al. Pallidal versus subthalamic deep-brain stimulation for Parkinson's disease. N Engl J Med. 2010;362:2077–2091. doi: 10.1056/NEJMoa0907083. [DOI] [PubMed] [Google Scholar]
- 64.Sako W, Miyazaki Y, Izumi Y, Kaji R. Which target is best for patients with Parkinson's disease? A meta-analysis of pallidal and subthalamic stimulation. J Neurol Neurosurg Psychiatry 2014 Jan 20 [Epub ahead of print]. [DOI] [PubMed]
- 65.Lukins TR, Tisch S, Jonker B. The latest evidence on target selection in deep brain stimulation for Parkinson's disease. J Clin Neurosci. 2014;21:22–27. doi: 10.1016/j.jocn.2013.05.011. [DOI] [PubMed] [Google Scholar]
- 66.Odekerken VJ, van Laar T, Staal MJ, Mosch A, Hoffmann CF, Nijssen PC, et al. Subthalamic nucleus versus globus pallidus bilateral deep brain stimulation for advanced Parkinson's disease (NSTAPS study): a randomised controlled trial. Lancet Neurol. 2013;12:37–44. doi: 10.1016/S1474-4422(12)70264-8. [DOI] [PubMed] [Google Scholar]
- 67.Plaha P, Ben-Shlomo Y, Patel NK, Gill SS. Stimulation of the caudal zona incerta is superior to stimulation of the subthalamic nucleus in improving contralateral parkinsonism. Brain. 2006;129:1732–1747. doi: 10.1093/brain/awl127. [DOI] [PubMed] [Google Scholar]
- 68.Blomstedt P, Fytagoridis A, Astrom M, Linder J, Forsgren L, Hariz MI. Unilateral caudal zona incerta deep brain stimulation for Parkinsonian tremor. Parkinsonism Relat Disord. 2012;18:1062–1066. doi: 10.1016/j.parkreldis.2012.05.024. [DOI] [PubMed] [Google Scholar]
- 69.Kitagawa M, Murata J, Uesugi H, Kikuchi S, Saito H, Tashiro K, et al. Two-year follow-up of chronic stimulation of the posterior subthalamic white matter for tremor-dominant Parkinson's disease. Neurosurgery. 2005;56:281–289. doi: 10.1227/01.neu.0000148167.49105.a3. [DOI] [PubMed] [Google Scholar]
- 70.Tattersall TL, Stratton PG, Coyne TJ, Cook R, Silberstein P, Silburn PA, et al. Imagined gait modulates neuronal network dynamics in the human pedunculopontine nucleus. Nat Neurosci. 2014;17:449–454. doi: 10.1038/nn.3642. [DOI] [PubMed] [Google Scholar]
- 71.Grabli D, Karachi C, Folgoas E, Monfort M, Tande D, Clark S, et al. Gait disorders in parkinsonian monkeys with pedunculopontine nucleus lesions: a tale of two systems. J Neurosci. 2013;33:11986–11993. doi: 10.1523/JNEUROSCI.1568-13.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Stefani A, Lozano AM, Peppe A, Stanzione P, Galati S, Tropepi D, et al. Bilateral deep brain stimulation of the pedunculopontine and subthalamic nuclei in severe Parkinson's disease. Brain. 2007;130:1596–1607. doi: 10.1093/brain/awl346. [DOI] [PubMed] [Google Scholar]
- 73.Ferraye MU, Debu B, Fraix V, Krack P, Charbardes S, Seigneuret E, et al. Subthalamic nucleus versus pedunculopontine nucleus stimulation in Parkinson disease: synergy or antagonism? J Neural Transm. 2011;118:1469–1475. doi: 10.1007/s00702-011-0673-y. [DOI] [PubMed] [Google Scholar]
- 74.Thevathasan W, Cole MH, Graepel CL, Hyam JA, Jenkinson N, Brittain JS, et al. A spatiotemporal analysis of gait freezing and the impact of pedunculopontine nucleus stimulation. Brain. 2012;135:1446–1454. doi: 10.1093/brain/aws039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Thevathasan W, Coyne TJ, Hyam JA, Kerr G, Jenkinson N, Aziz TZ, et al. Pedunculopontine nucleus stimulation improves gait freezing in Parkinson disease. Neurosurgery. 2011;69:1248–1253. doi: 10.1227/NEU.0b013e31822b6f71. [DOI] [PubMed] [Google Scholar]
- 76.deSouza RM, Moro E, Lang AE, Schapira AH. Timing of deep brain stimulation in Parkinson disease: a need for reappraisal? Ann Neurol. 2013;73:565–575. doi: 10.1002/ana.23890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Schuepbach WM, Rau J, Knudsen K, Volkmann J, Krack P, Timmermann L, et al. Neurostimulation for Parkinson's disease with early motor complications. N Engl J Med. 2013;368:610–622. doi: 10.1056/NEJMoa1205158. [DOI] [PubMed] [Google Scholar]
- 78.Fahn S. Classification of movement disorders. Move Disord. 2011;26:947–957. doi: 10.1002/mds.23759. [DOI] [PubMed] [Google Scholar]
- 79.Ozelius LJ, Hewett J, Kramer P, Bressman SB, Shalish C, de Leon D, et al. Fine localization of the torsion dystonia gene (DYT1) on human chromosome 9q34: YAC map and linkage disequilibrium. Genome Res. 1997;7:483–494. doi: 10.1101/gr.7.5.483. [DOI] [PubMed] [Google Scholar]
- 80.Vercueil L, Pollak P, Fraix V, Caputo E, Moro E, Benazzouz A, et al. Deep brain stimulation in the treatment of severe dystonia. J Neurol. 2001;248:695–700. doi: 10.1007/s004150170116. [DOI] [PubMed] [Google Scholar]
- 81.Spindler MA, Galifianakis NB, Wilkinson JR, Duda JE. Globus pallidus interna deep brain stimulation for tardive dyskinesia: case report and review of the literature. Parkinsonism Relat Disord. 2013;19:141–147. doi: 10.1016/j.parkreldis.2012.09.016. [DOI] [PubMed] [Google Scholar]
- 82.Marks WA, Honeycutt J, Acosta F, Jr, Reed M, Bailey L, Pomykal A, et al. Dystonia due to cerebral palsy responds to deep brain stimulation of the globus pallidus internus. Move Disord. 2011;26:1748–1751. doi: 10.1002/mds.23723. [DOI] [PubMed] [Google Scholar]
- 83.Witt J, Starr PA, Ostrem JL. Use of pallidal deep brain stimulation in postinfarct hemidystonia. Stereotact Funct Neurosurg. 2013;91:243–247. doi: 10.1159/000345262. [DOI] [PubMed] [Google Scholar]
- 84.Svetel M, Kozic D, Stefanova E, Semnic R, Dragasevic N, Kostic VS. Dystonia in Wilson's disease. Move Disord. 2001;16:719–723. doi: 10.1002/mds.1118. [DOI] [PubMed] [Google Scholar]
- 85.Jankovic J. Medical treatment of dystonia. Move Disord. 2013;28:1001–1012. doi: 10.1002/mds.25552. [DOI] [PubMed] [Google Scholar]
- 86.Berman BD, Starr PA, Marks WJ, Jr, Ostrem JL. Induction of bradykinesia with pallidal deep brain stimulation in patients with cranial-cervical dystonia. Stereotact Funct Neurosurg. 2009;87:37–44. doi: 10.1159/000195718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Zauber SE, Watson N, Comella CL, Bakay RA, Metman LV. Stimulation-induced parkinsonism after posteroventral deep brain stimulation of the globus pallidus internus for craniocervical dystonia. J Neurosurg. 2009;110:229–233. doi: 10.3171/2008.6.17621. [DOI] [PubMed] [Google Scholar]
- 88.Volkmann J, Wolters A, Kupsch A, Muller J, Kuhn AA, Schneider GH, et al. Pallidal deep brain stimulation in patients with primary generalised or segmental dystonia: 5-year follow-up of a randomised trial. Lancet Neurol. 2012;11:1029–1038. doi: 10.1016/S1474-4422(12)70257-0. [DOI] [PubMed] [Google Scholar]
- 89.Pahapill PA, O'Connell B. Long-term follow-up study of chronic deep brain stimulation of the subthalamic nucleus for cervical dystonia. Neuromodulation. 2010;13:26–30. doi: 10.1111/j.1525-1403.2009.00231.x. [DOI] [PubMed] [Google Scholar]
- 90.Ostrem JL, Racine CA, Glass GA, Grace JK, Volz MM, Heath SL, et al. Subthalamic nucleus deep brain stimulation in primary cervical dystonia. Neurology. 2011;76:870–878. doi: 10.1212/WNL.0b013e31820f2e4f. [DOI] [PubMed] [Google Scholar]
- 91.Kleiner-Fisman G, Liang GS, Moberg PJ, Ruocco AC, Hurtig HI, Baltuch GH, et al. Subthalamic nucleus deep brain stimulation for severe idiopathic dystonia: impact on severity, neuropsychological status, and quality of life. J Neurosurg. 2007;107:29–36. doi: 10.3171/JNS-07/07/0029. [DOI] [PubMed] [Google Scholar]
- 92.Fukaya C, Katayama Y, Kano T, Nagaoka T, Kobayashi K, Oshima H, et al. Thalamic deep brain stimulation for writer's cramp. J Neurosurg. 2007;107:977–982. doi: 10.3171/JNS-07/11/0977. [DOI] [PubMed] [Google Scholar]
- 93.Ghika J, Villemure JG, Miklossy J, Temperli P, Pralong E, Christen-Zaech S, et al. Postanoxic generalized dystonia improved by bilateral Voa thalamic deep brain stimulation. Neurology. 2002;58:311–313. doi: 10.1212/wnl.58.2.311. [DOI] [PubMed] [Google Scholar]
- 94.Schjerling L, Hjermind LE, Jespersen B, Madsen FF, Brennum J, Jensen SR, et al. A randomized double-blind crossover trial comparing subthalamic and pallidal deep brain stimulation for dystonia. J Neurosurg. 2013;119:1537–1545. doi: 10.3171/2013.8.JNS13844. [DOI] [PubMed] [Google Scholar]
- 95.Coubes P, Cif L, El Fertit H, Hemm S, Vayssiere N, Serrat S, et al. Electrical stimulation of the globus pallidus internus in patients with primary generalized dystonia: long-term results. J Neurosurg. 2004;101:189–194. doi: 10.3171/jns.2004.101.2.0189. [DOI] [PubMed] [Google Scholar]
- 96.Cif L, El Fertit H, Vayssiere N, Hemm S, Hardouin E, Gannau A, et al. Treatment of dystonic syndromes by chronic electrical stimulation of the internal globus pallidus. J Neurosurg Sci. 2003;47:52–55. [PubMed] [Google Scholar]
- 97.Vidailhet M, Vercueil L, Houeto JL, Krystkowiak P, Benabid AL, Cornu P, et al. Bilateral deep-brain stimulation of the globus pallidus in primary generalized dystonia. N Engl J Med. 2005;352:459–467. doi: 10.1056/NEJMoa042187. [DOI] [PubMed] [Google Scholar]
- 98.Kupsch A, Benecke R, Muller J, Trottenberg T, Schneider GH, Poewe W, et al. Pallidal deep-brain stimulation in primary generalized or segmental dystonia. N Engl J Med. 2006;355:1978–1990. doi: 10.1056/NEJMoa063618. [DOI] [PubMed] [Google Scholar]
- 99.Valldeoriola F, Regidor I, Minguez-Castellanos A, Lezcano E, Garcia-Ruiz P, Rojo A, et al. Efficacy and safety of pallidal stimulation in primary dystonia: results of the Spanish multicentric study. J Neurol Neurosurg Psychiatry. 2010;81:65–69. doi: 10.1136/jnnp.2009.174342. [DOI] [PubMed] [Google Scholar]
- 100.Damier P, Thobois S, Witjas T, Cuny E, Derost P, Raoul S, et al. Bilateral deep brain stimulation of the globus pallidus to treat tardive dyskinesia. Arch Gen Psychiatry. 2007;64:170–176. doi: 10.1001/archpsyc.64.2.170. [DOI] [PubMed] [Google Scholar]
- 101.Chang EF, Schrock LE, Starr PA, Ostrem JL. Long-term benefit sustained after bilateral pallidal deep brain stimulation in patients with refractory tardive dystonia. Stereotact Funct Neurosurg. 2010;88:304–310. doi: 10.1159/000316763. [DOI] [PubMed] [Google Scholar]
- 102.Vidailhet M, Yelnik J, Lagrange C, Fraix V, Grabli D, Thobois S, et al. Bilateral pallidal deep brain stimulation for the treatment of patients with dystonia-choreoathetosis cerebral palsy: a prospective pilot study. Lancet Neurol. 2009;8:709–717. doi: 10.1016/S1474-4422(09)70151-6. [DOI] [PubMed] [Google Scholar]
- 103.Koy A, Hellmich M, Pauls KA, Marks W, Lin JP, Fricke O, et al. Effects of deep brain stimulation in dyskinetic cerebral palsy: a meta-analysis. Move Disord. 2013;28:647–654. doi: 10.1002/mds.25339. [DOI] [PubMed] [Google Scholar]
- 104.Skogseid IM, Ramm-Pettersen J, Volkmann J, Kerty E, Dietrichs E, Roste GK. Good long-term efficacy of pallidal stimulation in cervical dystonia: a prospective, observer-blinded study. Eur J Neurol. 2012;19:610–615. doi: 10.1111/j.1468-1331.2011.03591.x. [DOI] [PubMed] [Google Scholar]
- 105.Hung SW, Hamani C, Lozano AM, Poon YY, Piboolnurak P, Miyasaki JM, et al. Long-term outcome of bilateral pallidal deep brain stimulation for primary cervical dystonia. Neurology. 2007;68:457–459. doi: 10.1212/01.wnl.0000252932.71306.89. [DOI] [PubMed] [Google Scholar]
- 106.Kiss ZH, Doig-Beyaert K, Eliasziw M, Tsui J, Haffenden A, Suchowersky O, et al. The Canadian multicentre study of deep brain stimulation for cervical dystonia. Brain. 2007;130:2879–2886. doi: 10.1093/brain/awm229. [DOI] [PubMed] [Google Scholar]
- 107.Walsh RA, Sidiropoulos C, Lozano AM, Hodaie M, Poon YY, Fallis M, et al. Bilateral pallidal stimulation in cervical dystonia: blinded evidence of benefit beyond 5 years. Brain. 2013;136:761–769. doi: 10.1093/brain/awt009. [DOI] [PubMed] [Google Scholar]
- 108.Beuter A, Lefaucheur JP, Modolo J. Closed-loop cortical neuromodulation in Parkinson's disease: An alternative to deep brain stimulation? Clin Neurophysiol. 2014;125:874–885. doi: 10.1016/j.clinph.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 109.Rosin B, Slovik M, Mitelman R, Rivlin-Etzion M, Haber SN, Israel Z, et al. Closed-loop deep brain stimulation is superior in ameliorating parkinsonism. Neuron. 2011;72:370–384. doi: 10.1016/j.neuron.2011.08.023. [DOI] [PubMed] [Google Scholar]
- 110.Morrell MJ, Group RNSSiES Responsive cortical stimulation for the treatment of medically intractable partial epilepsy. Neurology. 2011;77:1295–1304. doi: 10.1212/WNL.0b013e3182302056. [DOI] [PubMed] [Google Scholar]
- 111.Ryapolova-Webb E, Afshar P, Stanslaski S, Denison T, de Hemptinne C, Bankiewicz K, et al. Chronic cortical and electromyographic recordings from a fully implantable device: preclinical experience in a nonhuman primate. J Neural Eng. 2014;11:016009. doi: 10.1088/1741-2560/11/1/016009. [DOI] [PubMed] [Google Scholar]
- 112.Shimamoto SA, Ryapolova-Webb ES, Ostrem JL, Galifianakis NB, Miller KJ, Starr PA. Subthalamic nucleus neurons are synchronized to primary motor cortex local field potentials in Parkinson's disease. J Neurosci. 2013;33:7220–7233. doi: 10.1523/JNEUROSCI.4676-12.2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Air EL, Ryapolova-Webb E, de Hemptinne C, Ostrem JL, Galifianakis NB, Larson PS, et al. Acute effects of thalamic deep brain stimulation and thalamotomy on sensorimotor cortex local field potentials in essential tremor. Clin Neurophysiol. 2012;123:2232–2238. doi: 10.1016/j.clinph.2012.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Starr PA, Christine CW, Theodosopoulos PV, Lindsey N, Byrd D, Mosley A, et al. Implantation of deep brain stimulators into the subthalamic nucleus: technical approach and magnetic resonance imaging-verified lead locations. J Neurosurg. 2002;97:370–387. doi: 10.3171/jns.2002.97.2.0370. [DOI] [PubMed] [Google Scholar]
- 115.Martin AJ, Larson PS, Ostrem JL, Starr PA. Interventional magnetic resonance guidance of deep brain stimulator implantation for Parkinson disease. Top Magn Reson Imaging. 2009;19:213–221. doi: 10.1097/RMR.0b013e3181963b2c. [DOI] [PubMed] [Google Scholar]
- 116.Starr PA, Martin AJ, Larson PS. Implantation of deep brain stimulator electrodes using interventional MRI. Neurosurg Clin North Am. 2009;20:193–203. doi: 10.1016/j.nec.2009.04.010. [DOI] [PubMed] [Google Scholar]
- 117.Starr PA, Martin AJ, Ostrem JL, Talke P, Levesque N, Larson PS. Subthalamic nucleus deep brain stimulator placement using high-field interventional magnetic resonance imaging and a skull-mounted aiming device: technique and application accuracy. J Neurosurg. 2010;112:479–490. doi: 10.3171/2009.6.JNS081161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Larson PS, Starr PA, Bates G, Tansey L, Richardson RM, Martin AJ. An optimized system for interventional magnetic resonance imaging-guided stereotactic surgery: preliminary evaluation of targeting accuracy. Neurosurgery. 2012;70(1 Suppl. Operative):95–103. doi: 10.1227/NEU.0b013e31822f4a91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Ostrem JL, Galifianakis NB, Markun LC, Grace JK, Martin AJ, Starr PA, et al. Clinical outcomes of PD patients having bilateral STN DBS using high-field interventional MR-imaging for lead placement. Clin Neurol Neurosurg. 2013;115:708–712. doi: 10.1016/j.clineuro.2012.08.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Burchiel KJ, McCartney S, Lee A, Raslan AM. Accuracy of deep brain stimulation electrode placement using intraoperative computed tomography without microelectrode recording. J Neurosurg. 2013;119:301–306. doi: 10.3171/2013.4.JNS122324. [DOI] [PubMed] [Google Scholar]
- 121.Strauss I, Kalia SK, Lozano AM. Where are we with surgical therapies for Parkinson's disease? Parkinsonism Relat Disord. 2014;20(Suppl. 1):S187–191. doi: 10.1016/S1353-8020(13)70044-0. [DOI] [PubMed] [Google Scholar]
- 122.Elias WJ, Huss D, Voss T, Loomba J, Khaled M, Zadicario E, et al. A pilot study of focused ultrasound thalamotomy for essential tremor. N Engl J Med. 2013;369:640–648. doi: 10.1056/NEJMoa1300962. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF 1224 kb)