Abstract
Background: Despite numerous population-based randomized intervention trials, the impact of such interventions on socioeconomic inequalities has rarely been examined. We used data from a large cluster-randomized trial to assess the impact of a breastfeeding promotion intervention on socioeconomic inequalities in breastfeeding (exclusivity and duration) and in child cognitive ability at early school age.
Methods: The Promotion of Breastfeeding Intervention Trial (PROBIT) randomized 31 Belarusian maternity hospitals and their affiliated polyclinics either to receive a breastfeeding promotion intervention modelled on the WHO/UNICEF Baby-Friendly Hospital Initiative or to continue the standard practices in effect at the time of randomization. We estimated and compared inequalities in discontinuation of exclusive breastfeeding before 3 months and of any breastfeeding before 12 months and in child verbal IQ at age 6.5 years, across maternal education strata between the two intervention arms.
Findings: Socioeconomic inequalities in discontinuing exclusive breastfeeding before 3 months were negligible in the control group. However, graded inequalities by maternal education emerged in the intervention group {relative risk [RR] = 1.12 [95% confidence interval (CI): 1.04, 1.20] for partial university and RR = 1.20 [95% CI: 1.11, 1.31] for secondary education or less vs complete university; risk difference [RD] = 0.06 [95% CI: 0.03, 0.09] and 0.10 [95% CI: 0.06, 0.14], respectively}. For discontinuing any breastfeeding before 12 months, small socioeconomic gradients in the control group were widened in the intervention group (RR = 1.04 and 1.16, respectively, for mothers with secondary education or less). Despite these differential effects on breastfeeding, however, we observed a small, nonsignificant reduction in socioeconomic inequalities in child verbal IQ at age 6.5 years.
Conclusions: A population-based intervention to promote breastfeeding slightly widened socioeconomic inequalities in breastfeeding but not those in child cognitive ability.
Keywords: Health inequalities, randomized intervention trials, breastfeeding, cognitive functioning
Key Messages.
A population-wide, rather than ‘high risk'-targeted, intervention strategy has been criticized for its inadvertent consequence of widening socioeconomic inequalities in health.
Exploiting data from a cluster-randomized intervention of breastfeeding promotion intervention, we found that socioeconomic inequalities in breastfeeding by maternal education, which were negligible without the intervention, emerged in the intervention group in both relative and absolute scale.
However, we found no evidence of widening inequalities in child verbal IQ scores owing to the intervention, despite the beneficial effect of the intervention on cognition.
Overall, the intervention improved both breastfeeding and child cognitive ability, irrespective of maternal education level, by favourably shifting the entire distribution of exclusive and prolonged breastfeeding and of cognitive ability.
Introduction
Reducing socioeconomic inequalities in health is an important public health goal.1 A key first step toward achieving that goal is to evaluate and compare the impact of various interventions across socioeconomic strata. However, intervention studies—both primary studies and systematic reviews—rarely assess impacts on socioeconomic inequalities, and thus little is known about which interventions are effective and cost-effective for reducing those inequalities.2–4
Determining appropriate intervention strategies to reduce health inequalities has been the focus of much recent discussion.5 Rose’s population prevention strategy, which has been widely accepted in public health policies, attempts to shift the risk distribution of the entire population towards a lower risk rather than targeting a population subgroup at ‘high risk’, thereby benefiting the entire population.6 However, some researchers have argued that such population-wide intervention strategy may inadvertently worsen socioeconomic inequalities, because socioeconomically advantaged individuals tend to respond earlier and to a greater degree than those who are disadvantaged.7–9 Few empirical studies have examined this phenomenon and have reported inconsistent results. Smoking prevention,10 folate intake among women of childbearing age11 and water fluoridation12 are among population strategies whose impacts on inequalities have been assessed, and both widening and narrowing of inequalities have been reported. A recent systematic review to identify types of intervention generating inequalities concluded that available evidence is insufficient and that more empirical evidence is required.5
Interventions to improve breastfeeding initiation, exclusivity and duration are based on extensive evidence from both observational and intervention studies of short- and long-term health benefits of breastfeeding for both mothers and infants.13–15 Nevertheless, to our knowledge none of previous studies has systematically examined whether the increases in breastfeeding resulting from such interventions have equally benefited all socioeconomic groups.
A frequent methodological challenge in evaluating the impact of an intervention on inequalities is the lack of ‘baseline’ inequality data in the unexposed to the intervention measured at the same time and in a population that is similar to the exposed group with respect to confounding. A well-designed randomized trial overcomes that limitation since randomization can ensure that the intervention and the control groups have a similar confounding structure, resulting in optimal ‘baseline’ data from the control group. However, few randomized intervention trials have assessed the impact on socioeconomic inequalities. In this study, we empirically examined the impacts of a cluster-randomized intervention to promote breastfeeding in the Republic of Belarus. We took advantage of the randomized design to accomplish two primary study aims. First, we compared the extent of socioeconomic inequalities in exclusive and prolonged breastfeeding between the intervention and the control groups. Second, because child cognitive ability at age 6.5 years was increased in the intervention group in our intention-to-treat analysis,16 we also compared socioeconomic inequalities in that long-term outcome between the two intervention arms.
Methods
Study participants
Study participants are mother-infant pairs who participated in the Promotion of Breastfeeding Intervention Trial (PROBIT), a cluster-randomized trial to promote exclusivity and duration of breastfeeding in the Republic of Belarus. A full description of PROBIT’s design and methods has been published elsewhere.17 In brief, 31 maternity hospitals and their affiliated polyclinics (where children are followed for routine health care) were randomized either to receive a breastfeeding promotion intervention modelled on the 10 steps to successful breastfeeding of the WHO/UNICEF Baby-Friendly Hospital Initiative (BFHI) or to continue the maternity hospital and polyclinic practices in effect at the time of randomization. A total of 17 046 mothers who initiated breastfeeding and their healthy singleton infants born at ≥37 completed weeks of gestation with birth weight ≥2500 g were recruited during their postpartum stay between June 1996 and December 1997. The mother-infant pairs were followed up at 1, 2, 3, 6, 9 and 12 months, during which infant feeding was reported by the mother; 96.7% (n = 16 491) of them completed the first-year follow-up. A total of 13 889 children (81.5% of the original cohort) were re-examined at 6.5 years, when cognitive ability was measured.
Socioeconomic position
Self-reported maternal education at enrolment was used as the socioeconomic indicator in this study. It was originally measured using a four-category scale: incomplete secondary (3.8%), complete secondary (32.1%), advanced secondary or partial university (50.5%) or complete university (13.6%) education. Owing to small numbers in the lowest education category, we combined incomplete secondary with complete secondary education into a single category for our analysis.
Outcomes
Breastfeeding
Mothers reported their current infant feeding details at each follow-up visit (1, 2, 3, 6, 9 and 12 months) during the first year. Based on those reports, we created two outcomes: discontinuation of exclusive breastfeeding (i.e. introducing any foods other than breast milk) before 3 months and discontinuation of breastfeeding to any degree (weaning) before 12 months.
Cognitive ability at age 6.5 years
At the 6.5-year follow-up, the polyclinic paediatricians measured child cognitive ability using the Wechsler Abbreviated Scales of Intelligence (WASI).18 The WASI consists of vocabulary and similarities subtests for verbal IQ, and block designs and matrices for performance IQ. In a convenience sample of 45 children during a 1-week training workshop provided by child psychologists and psychiatrists, inter-paediatrician agreement was high, with Pearson correlation coefficients of 0.80 (95% confidence interval: 0.67, 0.89) for vocabulary, 0.72 (0.54, 0.83) for similarities, 0.80 (0.67, 0.89) for block designs and 0.79 (0.66, 0.88) for matrices.16 Since we previously reported that the intervention resulted in significantly higher verbal IQ scores in intention-to-treat analysis,16 we focused on results for verbal IQ scores in the present study.
Statistical analysis
We used modified Poisson regression analysis with generalized estimating equations (GEEs) to estimate socioeconomic inequalities in discontinuing exclusive breastfeeding before 3 months and any breastfeeding before 12 months. Modified Poisson models were used to estimate unbiased risks for these common binary outcomes;19 the GEEs were used to account for cluster randomization.20 We estimated both relative and absolute inequalities for breastfeeding outcomes. Absolute inequality measures reflect not only inequalities across socioeconomic subgroups but also public health importance of the outcome in consideration, and they could provide different, even contradictory, patterns of inequalities from relative measures in a given outcome.21,22 However, measuring absolute inequality is often neglected in health inequalities research.23 Relative risks (RRs) and absolute risk differences (RDs) of discontinuing breastfeeding among mothers with lower education compared with mothers with complete university education (reference category) were separately estimated in the intervention and in the control group and then compared between the two groups. We tested for statistical interactions between the group assignment and maternal education. We also estimated relative indices of inequality (RII) and slope indices of inequality (SII) as summary measures of relative and absolute inequalities of breastfeeding outcomes, respectively, across the entire distribution of maternal education.24 For child IQ, linear regression analyses using GEEs were performed to estimate mean IQ differences in lower maternal education from the reference category in each intervention group and compared between the groups.
Results
Inequalities in breastfeeding
Table 1 shows that the intervention was successful in increasing both the exclusivity and duration of breastfeeding in the first year, irrespective of maternal education level. Although prevalences of exclusive or any breastfeeding at each month were higher among mothers with higher level of education within each intervention group, socioeconomic gradients were more pronounced in the intervention group than in the control group, indicating greater benefits of the intervention among mothers with higher education.
Table 1.
Prevalence of exclusive breastfeeding and any breastfeeding in the first year according to maternal education in each intervention group
| Exclusive breastfeeding | 1 month |
3 months |
6 months |
|||
|---|---|---|---|---|---|---|
| Control | Intervention | Control | Intervention | Control | Intervention | |
| Secondary or less | 25.6 | 79.6 | 5.8 | 43.0 | 0.7 | 6.6 |
| Partial university | 26.3 | 80.7 | 6.8 | 46.0 | 0.7 | 6.9 |
| Complete university | 26.6 | 81.5 | 6.9 | 50.8 | 0.5 | 8.3 |
| Any breastfeeding | 6 months |
9 months |
12 months |
|||
|---|---|---|---|---|---|---|
| Control | Intervention | Control | Intervention | Control | Intervention | |
| Secondary or less | 32.9 | 43.1 | 21.5 | 32.0 | 13.9 | 25.8 |
| Partial university | 36.5 | 47.5 | 23.6 | 32.2 | 16.1 | 24.6 |
| Complete university | 40.4 | 58.8 | 27.0 | 44.0 | 17.3 | 35.6 |
Figure 1 displays the cluster-adjusted relative and absolute socioeconomic inequalities for discontinuing exclusive breastfeeding before 3 months according to maternal education in each intervention group. Even though mothers in the control group who had not completed university were more likely to discontinue exclusive breastfeeding before 3 months compared with those who had, the increased risk was negligible, showing only a 2–3% increase in relative risk. In the intervention group, however, mothers with partial university education showed a 12% (95% CI: 1.04, 1.20) higher relative risk of discontinuing exclusive breastfeeding before 3 months relative to mothers with completed university education (Figure 1a). The relative risk increase was greater among mothers with secondary education or less compared with mothers who had completed university (RR = 1.20, 95% CI: 1.11, 1.31). As can be seen from the fact that confidence intervals of these relative risk estimates did not overlap with each other across two intervention groups, formal statistical testing yielded a significant interaction between the intervention group assignment and maternal education (P = 0.0004).
Figure 1.
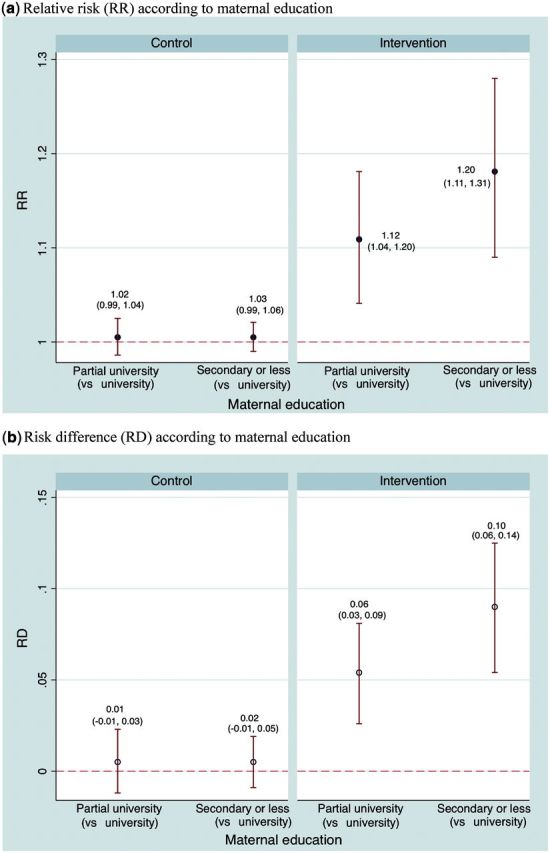
Cluster-adjusted relative and absolute socioeconomic inequalities in discontinuation of exclusive breastfeeding before 3 months in each randomized group
A similar pattern was observed when we estimated risk differences (Figure 1b). No socioeconomic inequalities were observed in the control group, whereas a small gradient was seen in the intervention group (RD = 0.06, 95% CI: 0.03, 0.09 for mothers with partial university education; RD = 0.10, 95% CI: 0.06, 0.14 for mothers with no more than secondary education).
Figure 2 shows cluster-adjusted relative and absolute inequalities in discontinuing any breastfeeding before 12 months in the two randomized groups. In the control group, a small gradient was observed between maternal education and complete breastfeeding cessation (weaning). In the intervention group, mothers who had not completed university were also more likely to wean their infants before 12 months than mothers who had, but no dose-response gradient was observed. However, the relative inequalities were larger in the intervention group (P-value <0.001 for the interaction).
Figure 2.
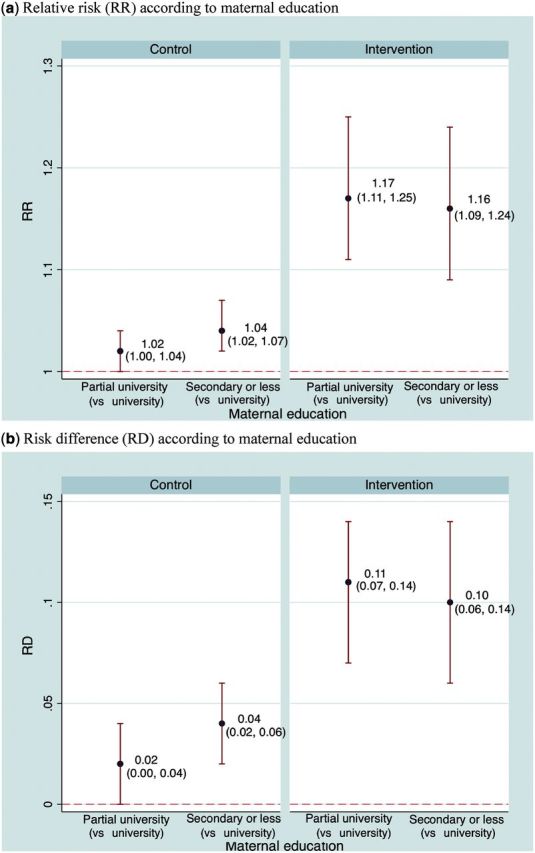
Cluster-adjusted relative and absolute socioeconomic inequalities in complete cessation of breastfeeding (weaning) before 12 months in each randomized group
Absolute inequalities showed a similar pattern (Figure 2b). In the control group, absolute risk differences of weaning before 12 months (vs mothers with complete university education) were 0.02 (95% CI: 0.00, 0.04) for mothers with partial university and 0.04 (95% CI: 0.02, 0.06) for those with secondary education or less. The corresponding risk differences were larger in the intervention group: 0.11 (95% CI: 0.08, 0.15) for mothers with partial university and 0.10 (95% CI: 0.06, 0.14) for mothers with secondary education or less.
Clustering-adjusted relative inequality index (RII) of discontinuing exclusive breastfeeding before 3 months was 0.80 (95% CI: 0.74, 0.87) in the intervention group, indicating a 20% relative risk reduction across the entire distribution of maternal education. The corresponding RII was 0.97 (95% CI: 0.93, 1.01) in the control group, consistent with our stratum-specific analysis results of no relative inequalities by maternal education in this group. The slope inequality index (SII) of discontinuing exclusive breastfeeding before 3 months was −0.12 (95% CI: −0.16, −0.08) in the intervention, indicating a 12% absolute risk reduction from the lowest to the highest education categories, compared with a 3% reduction in the corresponding absolute risk reduction (SII: −0.03, 95% CI: −0.06, 0.01) in the control group. Clustering-adjusted RIIs of weaning before 12 months were 0.89 (95% CI: 0.83, 0.96) and 0.94 (95% CI: 0.92, 0.97) in the intervention and the control groups, respectively. The corresponding figures of SIIs were −0.08 (95% CI: −0.13, −0.03) in the intervention group and −0.05 (95% CI: −0.07, −0.02) in the control group.
Inequalities in verbal IQ
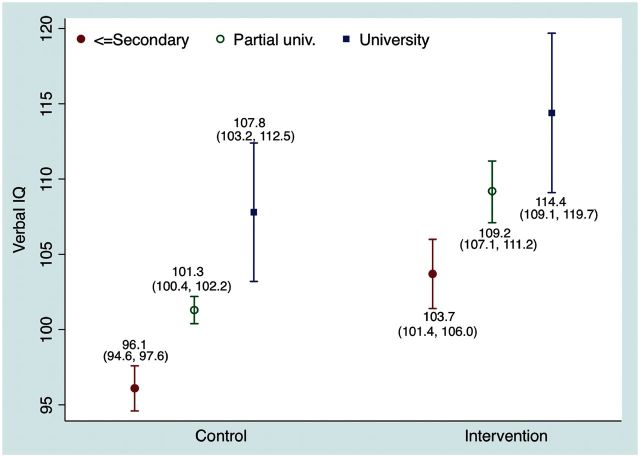
Figure 3 shows the cluster-adjusted mean child verbal IQ scores at age 6.5 years across maternal education in each randomized group. In both the control and the intervention groups, strong positive associations were observed between maternal education and IQ scores. Verbal IQ deficits among children of mothers with lower education compared with those who completed university were somewhat smaller in the intervention group than in the control group: 5.2 (95% CI: 3.1, 7.3) vs 6.5 (95% CI: 5.6, 7.4) points deficit among mothers with partial university education and 10.7 (95% CI: 8.4, 12.9) vs 11.7 (95% CI: 10.2, 13.2) points among those with secondary education or less. However, confidence intervals of these differences were overlapping with each other (P = 0.51 for the interaction), indicating no differential intervention effects on child IQ across maternal education categories. Similar patterns of IQ differences were observed for performance and full-scale IQ scores (data not shown).
Figure 3.
Cluster-adjusted mean verbal IQ at age 6.5 years by maternal education in each randomized group
Discussion
We have examined effects of a cluster-randomized breastfeeding promotion intervention on socioeconomic inequalities in breastfeeding behaviours during the first year and in child verbal ability at age 6.5 years. Socioeconomic inequalities in breastfeeding by maternal education were absent or small in the control group, in whom the standard practices were provided. However, larger socioeconomic inequalities—the higher socioeconomic position, the larger—emerged in the intervention group, both for early discontinuation of exclusive breastfeeding and for weaning before 12 months. We observed consistently widened inequalities in both relative and absolute measures. In contrast, we observed small, nonsignificant intervention-induced reductions in socioeconomic inequalities in child verbal IQ at age 6.5 years. However, the wide confidence intervals of our estimates for socioeconomic inequalities in IQ preclude definite conclusions.
Our intervention to promote the exclusivity and duration of breastfeeding following the Baby Friendly Hospital Initiative of the WHO was provided to all mothers in hospitals and affiliated polyclinics randomly selected for the intervention, irrespective of their education. The increased socioeconomic inequalities in breastfeeding observed in the intervention group supports the argument that population intervention strategies could inadvertently exacerbate, rather than mitigate, socioeconomic inequalities, particularly when the intervention aims to change individual behaviours rather than targeting ‘upstream’ structural changes.25 Our results are also compatible with an observational study from Brazil reporting that breastfeeding rates increased first among the socioeconomically better-off, followed by increases among the poor, over a 20-year period of active breastfeeding promotion campaigns in Brazil.26
Because mean child IQ scores at age 6.5 years, verbal IQ scores in particular, were higher among children in the intervention than the control group,16 we might expect that socioeconomic inequalities in child IQ would be widened in the intervention group, owing to the increase in observed inequalities in breastfeeding. Reasons for the lack of widened IQ inequalities are unclear. It could be due to the only modestly increased inequalities in breastfeeding. Alternatively, it may indicate that in Belarus, at least, maternal education is a stronger determinant of child IQ than breastfeeding. Mothers with higher education may already follow child-rearing practices that stimulate cognitive development of their infants through more frequent verbal interactions and reading. Genetic factors may also play a role in determining child cognitive ability.
Despite the widened socioeconomic inequalities by the intervention in rates of prolonged exclusive and any breastfeeding, breastfeeding rates were even higher among mothers with the lowest education (secondary school or less) in the intervention group than they were among mothers who completed university in the control group. Mean verbal IQ scores of children in the lowest maternal education category in the intervention were also substantially higher than those of their counterparts in the control group. These findings support the notion that a population-wide intervention strategy, without focusing on low socioeconomic groups, would benefit the entire population by successfully shifting the distribution of breastfeeding rates across all socioeconomic strata despite the small, unintended increases in socioeconomic inequalities.6 This benefit might be particularly evident in our study, because levels of exclusive and prolonged breastfeeding, even among mothers with the highest education, did not achieve recommended levels of breastfeeding, suggesting ample room for improvement. That socioeconomic inequalities in child cognitive functioning did not widen further supports such a population intervention strategy.
The randomized intervention design is one of strengths in our study, providing less biased estimates of impact of the intervention on socioeconomic inequalities. Moreover, our intervention sites were hospitals and affiliated polyclinics matched on a number of characteristics including geographical region and urban vs rural status, and the study sample is representative of general population of Belarus. Another strength is that our results provide a more complete assessment of socioeconomic inequalities in breastfeeding rates, by estimating both relative and absolute inequalities, than common practice in inequality assessments.23 Finally, our study analysed effects of the intervention not only on an immediate, direct outcome (breastfeeding) but also on a long-term consequence of breastfeeding (child cognitive ability) that is associated with important health and behavioural outcomes in later life.27
However, our study also has weaknesses. First, our results may not be generalizable to other study settings in Western or developed countries where breastfeeding is strongly patterned by socioeconomic position or in countries with lower breastfeeding rates than Belarus, where more than 95% of mothers initiated breastfeeding at the time of PROBIT.28 Belarus, a former Soviet country, is one of the countries with the least socioeconomic inequalities as reflected, for example, in their low Gini index of 27 in 2008 compared with 42 in Russia, 45 in the USA and 24 in Sweden. Belarus has also a very high literacy rate and quality of universal education as evidenced by only 4% of our sample having less than secondary education. Nonetheless, higher education in Belarus (and in our sample) is far more variable, which is why we observe inequalities in both breastfeeding behaviour and child cognitive ability. Second, the relatively high level of clustering of child IQ scores between sites represented by the intraclass correlation coefficient of 0.316 may reduce our statistical power to detect the small socioeconomic differences in child cognitive ability induced by the intervention.
In conclusion, our study intervention, which was designed to promote prolonged and exclusive breastfeeding, slightly widened socioeconomic inequalities in discontinuation of exclusive breastfeeding by 3 months and of any breastfeeding by 12 months. However, inequalities were not widened in cognitive functioning at early school age, despite the beneficial effect of the intervention on cognition. More importantly, the breastfeeding promotion intervention improved both breastfeeding and child cognitive ability, irrespective of maternal education, by favourably shifting the entire distribution of exclusive and prolonged breastfeeding and of cognitive ability. Our study illustrates that a randomized intervention trial with good socioeconomic information can help assess interventions designed to improve population health not only by examining the intervention effects on primary outcomes but also by evaluating the intervention's impact on socioeconomic inequalities.
Funding
This study was supported by the Canadian Institutes of Health Research (MOP-53155).
Conflict of interest: None declared.
References
- 1.Commission on Social Determinants of Health (CSDH). Closing the Gap in a Generation: Health Equity Through Action on the Social Determinants of Health. Geneva: World Health Organization, 2008. [Google Scholar]
- 2.Gepkens A, Gunning-Schepers LJ. Interventions to reduce socioeconomic health differences: A review of the international literature. Eur J Public Health 1996;63:218–26. [Google Scholar]
- 3.Main C, Thomas S, Ogilvie D, et al. Population tobacco control interventions and their effects on social inequalities in smoking: placing an equity lens on existing systematic reviews. BMC Public Health 2008;8:1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Haines A, Sanders D, Lehmann U, et al. Achieving child survival goals: potential contribution of community health workers. Lancet 2007;369:2121–31. [DOI] [PubMed] [Google Scholar]
- 5.Lorenc T, Petticrew M, Welch V, Tugwell P. What types of interventions generate inequalities? Evidence from systematic reviews. J Epidemiol Community Health 2013;67:190–93. [DOI] [PubMed] [Google Scholar]
- 6.Rose G. Sick individuals and sick population. Int J Epidemiol 1985;14:32–38. [DOI] [PubMed] [Google Scholar]
- 7.Victora CG, Vaughan JP, Barros FC, Silva AC, Tomasi E. Explaining trends in inequities: evidence from Brazilian child health studies. Lancet 2000;356:1093–98. [DOI] [PubMed] [Google Scholar]
- 8.Macintyre S, Chalmers I, Horton R, Smith R. Using evidence to inform health policy: case study. BMJ 2001;322:222–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frohlich KL, Potvin L. The inequality paradox: The population approach and vulnerable populations. Am J Public Health 2008;98:216–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thomas S, Fayter D, Misso K, et al. Population tobacco control interventions and their effects on social inequalities in smoking: systematic review. Tob Control 2008;17:230–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sumar N, McLaren L. Impact on social inequalities of population strategies of prevention for folate intake in women of childbearing age. Am J Public Health 2011;10:1218–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.NHS Centre for Reviews and Dissemination (NHS CRD). A Systematic Review of Public Water Fluoridation . York, UK: NHS Centre for Reviews and Dissemination, University of York, 2000. [Google Scholar]
- 13.Kramer MS, Kakuma R. Optimal duration of exclusive breastfeeding. Cochrane Database Syst Rev 2012;8:CD003517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Renfrew MJ, McCormick FM, Wade A, Quinn B, Dowswell T. Support for healthy breastfeeding mothers with healthy term babies. Cochrane Database Syst Rev 2012;5:CD001141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Imdad A, Yakoob MY, Bhutta ZA. Effect of breastfeeding promotion interventions on breastfeeding rates, with special focus on developing countries. BMC Public Health 2011;11(Suppl 3):S24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kramer MS, Aboud F, Mironova E, et al. Breastfeeding and child cognitive development: new evidence from a large randomized trial. Arch Gen Psychiatry 2008;65:578–84. [DOI] [PubMed] [Google Scholar]
- 17.Kramer MS, Chalmers B, Hodnett ED, et al. Promotion of Breastfeeding Intervention Trial (PROBIT): a randomized trial in the Republic of Belarus. JAMA 2001;285:413–20. [DOI] [PubMed] [Google Scholar]
- 18.Wechsler D. Wechsler Abbreviated Scales of Intelligence. San Antonio, TX: Psychological Corporation, 1999. [Google Scholar]
- 19.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159:702–06. [DOI] [PubMed] [Google Scholar]
- 20.Yelland LN, Salter AB, Ryan P. Performance of the modified poisson regression approach for estimating relative risks from clustered prospective data. Am J Epidemiol 2011;174:984–92. [DOI] [PubMed] [Google Scholar]
- 21.Lynch J, Davey Smith G, Harper S, Bainbridge K. Explaining the social gradient in coronary heart disease: comparing relative and absolute risk approaches. J Epidemiol Community Health 2006;60:436–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dowd JB, Aiello AE. Did national folic acid fortification reduce socioeconomic and racial disparities in folate status in the US. Int J Epidemiol 2008;37:1059–66. [DOI] [PubMed] [Google Scholar]
- 23.King NB, Harper S, Young ME. Use of relative and absolute effect measures in reporting health inequalities: structured review. BMJ 2012;345:e5774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mackenbach JP, Kunst AE. Measuring the magnitude of socio-economic inequalities in health: an overview of available measures illustrated with two examples from Europe. Soc Sci Med 1997;44:757–71. [DOI] [PubMed] [Google Scholar]
- 25.McLaren L, McIntyre L, Kirkpatrick S. Rose's population strategy of prevention need not increase social inequalities in health. Int J Epidemiol 2010;39:372–77. [DOI] [PubMed] [Google Scholar]
- 26.Victora CG, Matijasevich A, Santos IS, Barros AJD, Horta BL, Barros FC. Breastfeeding and feeding patterns in three birth cohorts in Southern Brazil: trends and differentials. Cad Saude Publica 2008;24:s409–s16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Deary IJ, Batty D, Gottfredson LS. Human hierarchies, health, and IQ. Science 2005;309:703; author reply 703. [DOI] [PubMed] [Google Scholar]
- 28.Patel R, Oken E, Bogdanovich N, Matush L, Sevkovskaya Z, Chalmers B, et al. Cohort Profile: The Promotion of Breastfeeding Intervention Trial (PROBIT). Int J Epidemiol 2013, 8 May. Epub ahead of print. PMID: 23471837. [DOI] [PMC free article] [PubMed] [Google Scholar]