Abstract
Background: Epidemiological studies have observed protective effects of mid-upper arm circumference (MUAC) against all-cause mortality mostly in Western populations. However, evidence on cause-specific mortality is limited.
Methods: The sample included 19 575 adults from a population-based cohort study in rural Bangladesh, who were followed up for an average of 7.9 years for mortality. Cox proportional hazards regression was used to evaluate the effect of MUAC, as well as the joint effect of body mass index (BMI) and MUAC, on the risk of death from any cause, cancer and cardiovascular disease (CVD).
Results: During 154 664 person-years of follow-up, 744 deaths including 312 deaths due to CVD and 125 deaths due to cancer were observed. There was a linear inverse relationship of MUAC with total and CVD mortality. Each 1-cm increase in MUAC was associated a reduced risk of death from any cause [hazard ratio (HR) = 0.85; 95% confidence interval (C), 0.81–0.89) and CVD (HR = 0.87; 95% CI, 0.80–0.94), after controlling for potential confounders. No apparent relationship between MUAC and the risk of death from cancer was observed. Among individuals with a low BMI (<18.5 kg/m2), a MUAC less than 24 cm was associated with increased risk for all-cause (HR = 1.81; 95% CI, 1.52–2.17) and CVD mortality (HR = 1.45; 95% CI, 1.11–1.91).
Conclusions: MUAC may play a critical role on all-cause and CVD mortality in lean Asians.
Keywords: Mid-upper arm circumference (MUAC), mortality, cardiovascular diseases, cohort study, epidemiology
Key Messages.
Evidence has suggested protective effects of mid-upper arm circumference (MUAC) on all-cause mortality, mostly in Western populations.
We evaluated the association of MUAC and the risk of death from any cause, CVD and cancer in a prospective cohort study in Bangladesh.
MUAC was inversely related to the risk of death from any cause and CVD, particularly in younger individuals and in men.
Low levels of MUAC were related to increased risk of death from any cause and CVD in individuals with a low BMI.
Introduction
Numerous epidemiological studies have evaluated associations of body mass index (BMI; weight in kilograms divided by the square of height in metres) with all-cause and cause-specific mortality.1 Several studies have reported a U-shaped association between BMI and mortality,2,3 especially in Asians or populations with a low BMI.4,5 Whereas a high BMI may be a good marker for a high body fat mass, a low BMI could indicate both low fat-free mass and low fat mass,6 making the interpretation for the relationship between BMI and mortality at the low end of BMI difficult. The usefulness of BMI in predicting disease risk or mortality has been questioned, since it does not give information on body composition by assuming that a value greater than the desirable weight is synonymous with obesity. For instance, a large-scale investigation indicates that fat and overweight are highly correlated only among individuals whose weight exceeds the 95th percentile.7 The consideration of other anthropometric measurements, e.g. extremity circumferences, has become an important complementary approach in the evaluation of disease risk related to obesity or leanness.
Mid-upper arm circumference (MUAC) is a quick, reliable and affordable anthropometric measurement widely used in childhood malnutrition identification and death risk prediction.8 An inverse association between MUAC and all-cause mortality has been reported in several studies;9–11 however, whether low MUAC is an independent risk factor of cause-specific mortality remains unclear. Also, studies of MUAC and mortality in populations with low BMI are sparse.12 Given the fact that the nutritional status of low-income populations is markedly lower than in Western populations,13 MUAC may play a more critical role in disease risk.14 In the present study, using data from the Health Effects of Arsenic Longitudinal Study (HEALS), a prospective cohort study of more than 20 000 participants in rural Bangladesh, we evaluated the association between MUAC and the risk of death from any cause, cancer and cardiovascular disease (CVD). We also assessed the joint status of BMI and MUAC in relation to all-cause and cause-specific mortality.
Methods
Study population
The parent study, Health Effects of Arsenic Longitudinal Study (HEALS), is an ongoing prospective cohort study in Araihazar, Bangladesh. Detailed description of the study has been presented elsewhere.15 Briefly, between October 2000 and May 2002, 11 746 men and women (original cohort), aged 18 years and above, were recruited from a well-defined 25-km2 geographical area. During 2006–08, HEALS was expanded to include an additional 8287 participants (expansion cohort) following the same methodologies. The overall participation rate was 97%. Demographic and lifestyle data were collected using a standardized questionnaire. The original aims of the cohort were to investigate health effects of arsenic exposure from drinking water. Since HEALS is a population-based cohort study, the study resources provide for the investigation of other risk factors of CVD. Informed consent was obtained from the study participants and the study procedures were approved by the Ethical Committee of the Bangladesh Medical Research Council and the Institutional Review Boards of Columbia University and the University of Chicago.
The cohort is being actively followed every 2 years with in-person visits, which include a physical examination and structured interview conducted by trained physicians following the same procedures as those used in the baseline interview. Interim health surveys were conducted every 6 months between the biennial follow-up visits. A field clinic was established exclusively for the cohort participants to receive medical diagnoses and treatments and facilitate the follow-up.15 Information on each HEALS participant, including an identification card with his/her name, is maintained at this clinic. Since this rural population lacks basic healthcare services from the existing healthcare facilities, all participants and their family members come to the clinic for all healthcare needs. The present study includes data on 19 575 participants with a valid measurement of MUAC at baseline after excluding 418 participants with missing data on any of the variables. Demographic and lifestyle distributions among those with measurements and the overall cohort were similar (data not shown).
Measurement of arm circumference and other covariates
Demographic and lifestyle data included in this analysis were collected at baseline using a standardized questionnaire. Trained clinicians measured blood pressure with an automatic sphygmomanometer.16 The MUAC was measured at the midpoint of the right arm. The midpoint was located after bending the right arm to a 90° angle at the elbow. The upper arm was approximately parallel to the trunk. Using an insertion tape, the examiner identified and marked the midpoint of the upper arm, halfway between the tip of the acromial process and the tip of the olecranon process. The skin was marked at this point before the arm was repositioned for the circumference measurement. The right arm was then extended alongside the body. The person's hand was placed through the loop of an inelastic, flexible tape measure. The tape was placed at the marked midpoint and pulled just snug around the arm, but not so tight that the tissues were compressed. The measurement was recorded to the nearest 1 cm.
Assessment of causes of deaths
Details of the methods for the assessment of causes of deaths are described elsewhere.17 Briefly, we adapted a validated verbal autopsy procedure, developed by the International Centre for Diarrheal Disease Research, Bangladesh (ICDDR, B), in collaboration with the World Health Organization (WHO), to ascertain the causes of deaths. During the follow-up, upon receipt of a death reported by family or neighbours, a study physician and a trained social worker administered the verbal autopsy form to the next of kin. Medical records and death certificates were collected. These data were reviewed monthly by an outcome assessment committee, consisting of physicians, a consulting cardiologist and a neurologist blinded to the exposure status. Causes of deaths were coded according to the WHO classification18 and the International Classification of Diseases, 10th revision (ICD-10).19 The ICDDR, B has used this method to ascertain causes of deaths since 197120 and documented an overall 95% specificity, with an 85% sensitivity for cancer deaths and 85% sensitivity for deaths due to CVD.21 The mortality data in HEALS have been used to assess the associations of dietary patterns,22 cigarette smoking,23 arsenic exposure17,24 and betel quid chewing25 with risk of all-cause and cause-specific mortality.
For the present study, our outcome of interest was deaths of any cause, deaths due to CVD (ICD-10 I00-I99), and death due to all cancer (ICD-10 C00-C97) in cohort participants from baseline to 1 March 2012.
Statistical analyses
Descriptive analyses were conducted to assess the relationships of demographic and lifestyle variables with MUAC. We computed person-years from baseline to the date of death or date of last follow-up. HRs and their 95% CIs for overall mortality, CVD mortality and cancer mortality in relation to quartiles of baseline MUAC were estimated using Cox proportional hazards regression models. We first adjusted for age and sex, and in separate models additionally adjusted for BMI, educational attainment, smoking status, baseline systolic blood pressure (SBP) level, and betel use, which are major risk factors for mortality in our study population.26 Because BMI was highly positively correlated with MUAC, which may lead to collinearity when adjusting BMI in the models, sensitivity analyses were conducted using BMI-adjusted MUAC that was calculated with a two-step residual model. In the first step, MUAC was regressed on BMI in a linear model, with the residuals computed for each subject. In the second step, BMI-adjusted MUAC was estimated for each subject as the sum of the residual for the subject and the expected MUAC for the mean BMI in the population. The residual method, which has been used in studies with highly correlated exposures,27 was adapted from energy adjustment techniques used within nutritional epidemiology.28
We also conducted stratified analyses to assess the association between MUAC and risk of death from any cause and CVD by sex, age and smoking status. A cross-product term between MUAC and each potential effect modifier (sex, smoking status and age dichotomized at median) was included alternatively, and the P-values for the cross-product terms were considered as the significance of the interactions. Interaction between MUAC and smoking was tested in men and women separately, as most of the ever smokers were men. Analyses were also conducted excluding individuals with history of CVD at baseline or excluding deaths that occurred in the first 2 years of follow-up.
Similar models were also constructed to estimate HRs and their 95% CI for overall mortality, CVD mortality, and cancer mortality in relation to quartiles of baseline BMI, with adjustment for age and sex, and then MUAC, educational attainment, smoking status, baseline systolic blood pressure (SBP) level, and betel use additionally. Sensitivity analyses were conducted adjusting for BMI-adjusted MUAC in place of MUAC. To evaluate the joint effect of BMI and MUAC on the risk of death, we estimated HRs according to joint status of BMI in tertiles (<18.5 kg/m2, 18.5–24.9 kg/m2, ≥25.0 kg/m2) and MUAC in two levels defined by the median (24.0 cm), using participants with normal BMI range (18.5–24.9 kg/m2) and higher MUAC (>24.0 cm) as the reference group. All analyses were conducted in SAS 9.3. Two-tailed (α = 0.05) tests of significance were used.
Results
Overall, the 19 575 participants were followed up for an average of about 7.9 years and generated a total of 154 664 person-years, with 744 deaths, consisting of 312 deaths due to CVD and 125 deaths due to cancer. Generally, this is a lean population, and MUAC follows a normal distribution with a median and a mean of MUAC both estimated at 24.0 cm [interquartile range = 3.5 cm, standard deviation (SD) = 2.7 cm]. Men, participants with a higher BMI, those who owned land or those with a higher educational attainment tended to have a higher MUAC (Table 1). The proportion of ever smokers apparently decreased with increasing MUAC levels in both men and women. Age and systolic blood pressure were positively related to MUAC, whereas betel nut use was negatively related to MUAC.
Table 1.
Baseline demographic and lifestyle factors by levels of mid-upper arm circumference (MUAC)
| Variables |
MUAC (cm) |
P for trenda | |||
|---|---|---|---|---|---|
| <23 | 23–23.9 | 24–24.7 | ≥24.8 | ||
| Age, yrs (SD) | 36.7 (11.0) | 36.4 (10.4) | 36.7 (10.2) | 37.3 (9.8) | <0.01 |
| Men, % | 34.8 | 43.1 | 44.3 | 44.4 | <0.0001 |
| BMI, kg/m2 (SD) | 17.4 (1.7) | 18.9 (1.6) | 19.8 (1.7) | 22.8 (3.0) | <0.0001 |
| Education, yrs (SD) | 2.5 (3.3) | 3.0 (3.6) | 3.4 (3.7) | 4.8 (4.2) | <0.0001 |
| Smoking, % | 34.1 | 35.6 | 33.5 | 28.7 | <0.0001 |
| Smoking among men, % | 81.1 | 75.1 | 71.3 | 61.4 | <0.0001 |
| Smoking among women, % | 9.1 | 5.7 | 3.4 | 2.6 | <0.0001 |
| Ever betel use, % | 34.2 | 31.5 | 32.0 | 31.5 | <0.0001 |
| Own land, % | 42.0 | 47.2 | 49.6 | 57.8 | <0.0001 |
| Systolic blood pressure, mmHg (SD) | 112.9 (17.0) | 115.2 (16.1) | 116.6 (16.4) | 121.4 (17.1) | <0.0001 |
aP-values for trend calculated with arm circumference as a continuous variable.
Compared with individuals with a MUAC ranging from 22 cm to 23.4 cm (reference group), an increased risk of death from any cause was observed for participants with lowest level of MUAC (<22 cm) (HR = 1.38; 95% CI = 1.13–1.68, Table 2). The associations remained apparent after additional adjustment for BMI, educational attainment, betel nut use, cigarette smoking status, and systolic blood pressure. For each 1-cm increase in MUAC, the risk of death from any cause was reduced by 15% (HR = 0.85; 95% CI, 0.81–0.89) (Model 2). Similar patterns of associations were observed for risk of death due to CVD, with a marginally significant increased risk observed for MUAC <22 cm (HR = 1.38; 95% CI, 1.00–1.91) in the fully adjusted model. For each 1-cm increase in MUAC, the risk of death from CVD was reduced by 13% (HR = 0.87; 95% CI, 0.80–0.94). There was in general no consistent relationship between MUAC and the risk of death from cancer. Sensitivity analyses conducted based on BMI-adjusted MUAC generated very similar results (Appendix 2, available as Supplementary data at IJE online).
Table 2.
Associations between mid-upper arm circumference (MUAC) and all-cause and cause-specific mortality
| Cause of death |
HR (95% CI), by BMI-adjusted arm circumference (cm) quartiles |
HR (95% CI) per 1 cm increase of ACc | P for trendc | |||
|---|---|---|---|---|---|---|
| <22 | 22–23.4 (Ref.) | 23.5–25.4 | ≥25.5 | |||
| No. of subjects | 4075 | 5197 | 5246 | 5057 | ||
| Person-years of follow-up | 33377 | 41690 | 41279 | 38319 | 154664 | |
| All-cause death | ||||||
| Number of cases | 242 | 212 | 138 | 152 | 744 | |
| Model 1a | 1.41 (1.17, 1.70) | Ref. | 0.64 (0.52, 0.80) | 0.73 (0.59, 0.90) | 0.89 (0.86, 0.91) | <0.0001 |
| Model 2b | 1.38 (1.13, 1.68) | Ref. | 0.66 (0.53, 0.82) | 0.79 (0.60, 1.05) | 0.85 (0.81, 0.89) | <0.0001 |
| CVD death | ||||||
| Number of cases | 84 | 80 | 64 | 84 | 312 | |
| Model 1a | 1.27 (0.94, 1.73) | Ref. | 0.79 (0.57, 1.10) | 1.07 (0.79, 1.46) | 0.97 (0.93, 1.01) | 0.1311 |
| Model 2b | 1.38 (1.00, 1.91) | Ref. | 0.72 (0.51, 1.02) | 0.82 (0.54, 1.25) | 0.87 (0.80, 0.94) | 0.0003 |
| All cancer death | ||||||
| Number of cases | 30 | 37 | 31 | 27 | 125 | |
| Model 1a | 1.00 (0.61, 1.62) | Ref. | 0.83 (0.51, 1.33) | 0.75 (0.45, 1.22) | 0.94 (0.88, 1.01) | 0.0833 |
| Model 2b | 0.86 (0.52, 1.44) | Ref. | 0.94 (0.57, 1.55) | 1.08 (0.56, 2.11) | 1.00 (0.88, 1.13) | 0.9532 |
aHRs were adjusted for age and sex.
bHRs were adjusted for age, sex, BMI, education level, betel use, smoking status and baseline systolic blood pressure.
cHRs and P-values calculated with MUAC as a continuous variable.
We also examined the association between MUAC and all-cause and CVD mortality in different subgroups (Table 3). The inverse association between MUAC and the risk of death from any cause remained similar by age, sex and smoking status. The HR for the risk of death from any cause associated with each 1-cm increase in MUAC ranged from 0.83 to 0.87 (P-values for trend < 0.01). Excluding subjects with previous history of CVD, or excluding deaths in the first 2 years of follow-up, did not change the strength of association appreciably. For CVD mortality, similar patterns of associations were observed. The risk reduction for death from CVD associated with each 1-cm increase in MUAC ranged from 12% to 25% in the subgroups, with a greater reduction in risk observed in younger participants (P for interaction = 0.02) and in men (P for interaction = 0.02). Additional stratified analyses by smoking status in men and women separately did not suggest a significant interaction between MUAC and smoking in the risk of death from CVD among men or women (data not shown). For instance, in men the HR for the risk of death from CVD associated with each 1-cm increase in MUAC was 0.86 (95% CI, 0.79–0.90) in smokers and 0.87 (0.70–1.08) in never smokers (P for interaction = 0.80). The significance of effect estimates in certain subgroups was reduced, probably due to a reduced sample size in stratified analyses, although the magnitude of the association was similar. For the risk of death from cancer, there was no apparent association with MUAC in any subgroups (data not shown).
Table 3.
Associations between mid-upper arm circumference (MUAC) and all-cause and cause-specific mortality in different subgroups
| Cause of death |
HR (95% CI), by MUAC (cm) quartilesa |
HR (95% CI) per 1 cm increase ACb | P for trendb | p for interactionc | |||
|---|---|---|---|---|---|---|---|
| <22 | 22–23.4 (Ref.) | 23.5–25.4 | ≥25.5 | ||||
| All-cause death | |||||||
| Number of cases | 242 | 212 | 138 | 152 | 744 | ||
| <36 yrs of age | 1.20 (0.75, 1.93) | Ref. | 0.63 (0.36, 1.11) | 1.03 (0.50, 2.09) | 0.87 (0.76, 0.99) | 0.0325 | 0.0624 |
| ≥36 yrs of age | 1.37 (1.10, 1.70) | Ref. | 0.65 (0.51, 0.83) | 0.74 (0.55, 1.01) | 0.85 (0.80, 0.90) | <.0001 | |
| Smoker | 1.45 (1.14, 1.85) | Ref. | 0.61 (0.46, 0.81) | 0.78 (0.55, 1.11) | 0.83 (0.78, 0.89) | <.0001 | 0.5991 |
| Nonsmoker | 1.17 (0.82, 1.66) | Ref. | 0.68 (0.47, 0.99) | 0.71 (0.45, 1.14) | 0.86 (0.79, 0.94) | 0.0011 | |
| Men | 1.51 (1.19, 1.92) | Ref. | 0.63 (0.48, 0.82) | 0.77 (0.55, 1.07) | 0.84 (0.79, 0.90) | <.0001 | 0.2658 |
| Women | 1.06 (0.75, 1.49) | Ref. | 0.69 (0.46, 1.04) | 0.72 (0.42, 1.23) | 0.84 (0.77, 0.93) | 0.0003 | |
| Excluding baseline CVD | 1.36 (1.11, 1.66) | Ref. | 0.63 (0.50, 0.80) | 0.74 (0.56, 0.99) | 0.84 (0.80, 0.88) | <.0001 | |
| Excluding first 2 years’ deaths | 1.30 (1.04, 1.62) | Ref. | 0.64 (0.50, 0.82) | 0.81 (0.60, 1.11) | 0.87 (0.82, 0.92) | <.0001 | |
| CVD death | |||||||
| Number of cases | 84 | 80 | 64 | 84 | 312 | ||
| <36 yrs of age | 1.26 (0.53, 2.99) | Ref. | 0.36 (0.12, 1.04) | 0.38 (0.10, 1.45) | 0.75 (0.62, 0.91) | 0.0039 | 0.0183 |
| ≥36 yrs of age | 1.37 (0.97, 1.95) | Ref. | 0.75 (0.52, 1.08) | 0.86 (0.56, 1.32) | 0.88 (0.82, 0.96) | 0.0025 | |
| Smoker | 1.46 (0.99, 2.17) | Ref. | 0.73 (0.48, 1.10) | 0.81 (0.49, 1.34) | 0.85 (0.78, 0.93) | 0.0006 | 0.4497 |
| Nonsmoker | 1.18 (0.66, 2.09) | Ref. | 0.57 (0.31, 1.05) | 0.67 (0.33, 1.37) | 0.88 (0.76, 1.01) | 0.0646 | |
| Men | 1.43 (0.97, 2.10) | Ref. | 0.71 (0.48, 1.05) | 0.80 (0.50, 1.26) | 0.87 (0.80, 0.94) | 0.0009 | 0.0167 |
| Women | 1.10 (0.60, 2.01) | Ref. | 0.61 (0.30, 1.24) | 0.60 (0.24, 1.51) | 0.84 (0.71, 0.98) | 0.0312 | |
| Excluding baseline CVD | 1.36 (0.97, 1.89) | Ref. | 0.70 (0.49, 0.99) | 0.76 (0.50, 1.16) | 0.86 (0.80, 0.93) | 0.0002 | |
| Excluding first 2 years’ deaths | 1.40 (0.99, 1.98) | Ref. | 0.64 (0.44, 0.94) | 0.82 (0.53, 1.28) | 0.88 (0.81, 0.95) | 0.0018 | |
aHRs were adjusted for age, sex, BMI, smoking status, education level, betel use and baseline SBP level except for categorical stratifying variables.
bHRs and P-values calculated with arm circumference as a continuous variable.
cP-value for interaction was calculated by including a cross-product term of age/sex/smoking and MUAC.
The association between BMI and the risk of deaths from all-cause, CVD, and cancer are shown in Appendix Table 2 (available as Supplementary data at IJE online). An increased risk was observed in individuals with a BMI ≥21.5 kg/m2 for the risk of death from all-cause (HR = 1.35; 95% CI, 1.05–1.73) and CVD (HR = 1.34; 95% CI, 0.94–1.90), compared with individuals with a normal BMI (19.3–21.4 kg/m2). Individuals with a BMI ranging from 17.5 to 19.2 kg/m2 experienced a reduced risk of death from all-cause (HR = 0.80; 95% CI, 0.63–1.01) and CVD (HR = 0.68; 95% CI, 0.48–0.98). There was no apparent association between BMI and cancer mortality (Appendix Table 2, available as Supplementary data at IJE online).
Table 4 shows the HRs for the risk of death from any cause and CVD by joint status of BMI and MUAC (unadjusted for BMI). There were very few deaths (n = 15) with a high BMI (≥25 kg/m2) and low MUAC (<24 cm) and therefore effect estimates for this group were unstable and are not shown. Compared with those with normal BMI range (18.5–24.9 kg/m2) and higher MUAC (>24.0 cm), elevated risk of death from any cause was noted for those with a lower MUAC (<24 cm) who had a normal (18.5–24.9 kg/m2) or low BMI (<18.5 kg/m2), with a HR of 1.31 (95% CI, 1.02–1.68) and 1.81 (95% CI, 1.52–2.17), respectively (Model 2). For the risk of death from CVD, a significantly elevated risk was observed for subjects with a lower MUAC (<24 cm) and low BMI (<18.5 kg/m2) (HR = 1.45; 95% CI, 1.11–1.91, Model 2). There was also a suggestion of increased risk of death from CVD mortality among those with a lower MUAC(<24 cm) who had a normal (18.5–24.9 kg/m2) or those with a high BMI (≥25 kg/m2); however, effect estimates did not approach statistical significance.
Table 4.
Associations between all-cause and cause-specific mortality and BMI-arm circumference combinationsa
| Cause of death |
HR (95% CI), by BMI (kg/m2) and arm circumference (cm) |
||||
|---|---|---|---|---|---|
|
BMI <18.5 |
18.5≤ BMI ≤24.9 |
BMI ≥25.0 | |||
| AC <24.0 | AC ≥24.0 | AC <24.0 | AC ≥24.0 | AC ≥24.0 | |
| Person-years of follow-up pyrs | 54316 | 6432 | 28586 | 53914 | 11283 |
| All-cause death (total number of cases = 743) | |||||
| Number of cases | 377 | 28 | 93 | 206 | 39 |
| Model 1b | 1.64 (1.38–1.94) | 0.88 (0.59–1.31) | 1.23 (0.96–1.57) | Ref. | 1.05 (0.75–1.48) |
| Model 2c | 1.81 (1.52–2.17) | 0.95 (0.64–1.41) | 1.31 (1.02–1.68) | Ref. | 0.99 (0.70–1.41) |
| CVD death (total number of cases = 311) | |||||
| Number of cases | 133 | 14 | 37 | 102 | 25 |
| Model 1b | 1.13 (0.88–1.47) | 0.86 (0.49–1.50) | 1.08 (0.74–1.57) | Ref. | 1.46 (0.94–2.27) |
| Model 2c | 1.45 (1.11–1.91) | 1.02 (0.58–1.79) | 1.26 (0.86–1.85) | Ref. | 1.28 (0.82–1.99) |
| All cancer death (total number of cases = 125) | |||||
| Number of cases | 57 | 7 | 15 | 41 | 5 |
| Model 1b | 1.24 (0.83–1.86) | 1.11 (0.50–2.48) | 0.99 (0.55–1.80) | Ref. | 0.68 (0.27–1.72) |
| Model 2c | 1.22 (0.80–1.87) | 1.09 (0.49–2.46) | 0.98 (0.54–1.78) | Ref. | 0.67 (0.26–1.71) |
a15 participants with BMI ≥25.0 and AC <24.0 cm were excluded.
bModel 1 adjusted for age and sex,
cModel 2 adjusted for age, sex, education level, betel use, smoking status and baseline SBP level.
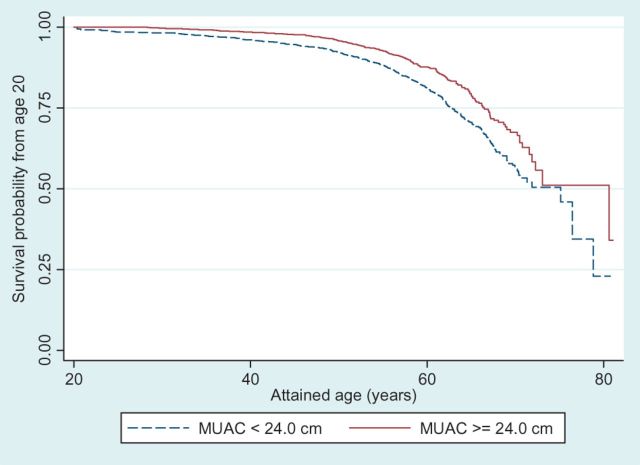
Figure 1 shows the survival curves of participants with MUAC below and above the median (24.0 cm), respectively. Among subjects with MUAC above 24.0 cm, 80% of them survived to age 64.8 years, whereas in the lower MUAC group, 80% of the participants survived to age 60.9, resulting in a nearly 4-year difference in life expectancy.
Figure 1.
Survival from age 20 years for all participants with mid-upper arm circumference (MUAC) below 24.0 cm (median) and above 24.0 cm, respectively
Discussion
In this large cohort study conducted in a rural South Asian population, we observe a significant inverse association between MUAC and the risk for all-cause and CVD deaths but not for cancer deaths. For each 1-cm difference of MUAC, a risk reduction of 15% and 13% were observed for the risk of death from any cause and CVD, respectively, independently of BMI and other conventional risk factors. The associations did not differ by age, sex or smoking status. Among individuals with a normal BMI (18.5–24.9 kg/m2) or a low BMI (<18.5 kg/m2), a MUAC lower than <24 cm was a risk factor for all-cause and CVD deaths.
Several previous studies in Western and Asian populations have investigated the association between MUAC and all-cause mortality. Bates and colleagues reported that for each standard deviation (3.3 cm) increase in MUAC, the risk for overall mortality over 15 years of follow-up was reduced by 15% in a British population aged 65 years and over.29 Another study conducted in the Netherlands revealed that the HRs for mortality associated with each lower SD of MUAC were 1.79 (95%CI, 1.48–2.16) and 2.26 (95%CI, 1.71–3.00) in men and women, respectively.30 In the British Regional Heart Study, mid-arm muscle circumference (MUAC 0.3142 × triceps skinfold thickness) was inversely related to mortality in older men.31 Three studies conducted among elderly Taiwanese,12 elderly Chinese32 and young Bangladeshi women,14 respectively, also revealed a reduced risk of death from any cause associated with a higher MUAC. Hosegood and colleagues conducted a 19-year longitudinal study among rural Bangladeshi women, a study population similar to ours, with mean age 27.5 years and mean BMI 18.5 kg/m2 at enrolment. Protective effect of higher MUAC on all-cause mortality was observed in bivariate analysis in this study, but no confounding factors were considered in this study. The contribution of MUAC as a component in mortality prediction models have also been evaluated in several studies in the USA,33 Canada10 and European countries.34–36 The present study confirmed that low MUAC is an independent risk factor for the risk of death from any cause, even in a low-BMI population.
Studies on the association between MUAC and cause-specific mortality are limited and have generated inconsistent findings. An earlier analysis based on 20-year follow-up of 1712 men aged 40–59 years in the two Italian cohorts of the Seven Countries Study found an inverse association of MUAC with the risk of deaths from all-cause, stroke, coronary heart disease (CHD) and overall CVD,37 adjusting for smoking, blood pressure and age, but not BMI. However, although a significant association was observed for all-cause mortality only,37,38 the inverse association between MUAC and CVD mortality was marginally significant (t = −1.91, the level of 1.96 corresponds to P = 0.05).37 In a subset of 599 men also from the Seven Countries Study, MUAC was not considered a predictor of CHD mortality, based on backward elimination procedures.39 In a prospective study of 1975 US railroad male workers with a mean age of 49 years and 20 years of follow-up, mid-arm circumference was significantly inversely associated with baseline prevalence of hypertension; however, the association between MUAC and age-adjusted CHD mortality was not apparent.40 A 15-year prospective study among French men reported that the sum of mid-arm plus mid-thigh circumferences was not a significant predictor of cardiac deaths after adjusting for age, height and smoking.41 In the Charleston Heart Study, mid-arm circumference was significantly inversely related to coronary heart disease mortality in Black men but not in White men, after adjusting for BMI and other factors.42 It is worth noting that almost all the above-mentioned studies were conducted in middle-aged men in Western populations. Most studies did not generate relative risk estimates to describe the association between MUAC and CVD risk, as such measures were not standard in earlier epidemiological studies.
In the present study, there was a significant inverse relationship between MUAC and risk of death from CVD. The association was dose-response and remained similar with different adjustment methods for BMI, excluding individuals with history of CVD at baseline, or excluding deaths that occurred in the first 2 years of follow-up. Our study indicates that MUAC may be an important predictor of all-cause and CVD mortality in a lean, South Asian population, particularly in younger individuals and in men. MUAC may be a simple and direct measure of physical activity or physical fitness43 which has protective effect on CVD risk,44 especially in a lean population. It is unclear, however, whether the association between MUAC and CVD risk is independent of the influence of physical activity or physical fitness, as we did not have objective measurements for these factors in the cohort. Future studies with more refined measures of arm muscles and fat as well as measurements of physical activity are needed to delineate the inter-relationships of physical activity, physical fitness, MUAC and CVD risk.
We also found that among individuals with a low BMI (<18.5 kg/m2), a low MUAC was a risk factor for all-cause and CVD deaths. Among individuals with a normal BMI (18.5–24.9 kg/m2), a low MUAC also was a risk factor for all-cause deaths. Several cohort studies in Asians, including analyses from our cohort45 and a recent pooled analysis of 1.1 million participants from 20 prospective cohorts in Asia,46 have reported a U-shaped association between BMI and the risk of all-cause47 and CVD46 mortality,47 albeit the association was less apparent in South Asians.46 A low MUAC among individuals with low or regular BMI may indicate a low total muscle or fat-free mass, which has been related to total mortality.33,48 The lack of subcutaneous muscle might also influence glucose and lipid metabolism. The relationship between intramuscular lipid accumulation and insulin resistance has been described,49 and glucose clearance is higher in arm than leg muscles.50 Reduced plasma fatty acid uptake and oxidation in the arm51,52 have been observed in type 2 diabetics as compared with healthy individuals. Recent evidence from prospective studies have suggested that a low thigh circumference is associated with an increased risk of developing heart disease or premature death independent of general obesity, with the plausibility that small thighs might be related to too little muscle mass in the region.53 Emerging data also indicate a role of upper body subcutaneous fat, estimated by neck circumference in CVD risk factors.54 However, we did not have data on thigh circumference, waist-to-hip ratio, skinfold thicknesses or neck circumference to assess whether the high risk associated with a low MUAC and low BMI can be attributable to other anthropometric measures. Nevertheless, our data suggest that having information on MUAC may help identify lean individuals who are susceptible to premature death and help stratify risk associated with low BMI.
Strengths of the present study include the prospective nature of the study design, population-based recruitment, and detailed information on lifestyle factors as well as cause-specific mortality data, which are rarely available in cohorts of South Asians. Several potential limitations should be taken into consideration when interpreting the results of our study. First, we could not control for the influence of waist circumference or waist-to-hip ratio on the association between MUAC and mortality. Second, we used mortality, not incidence data. The use of death certificates may involve some misclassification in CVD deaths. However, such errors are not likely to be differential by MUAC levels. Non-fatal CVD events remained unidentified and were therefore misclassified as non-cases. Although we believe that any misclassification of CVD deaths is unlikely to have been affected by MUAC levels, we cannot predict the exact direction or extent of the potential bias with certainty. Future large studies that include incidence data are needed. Third, the number of deaths from cancer was limited, and we could not exclude a small association between MUAC and cancer mortality. For the same reason, we could not assess the risk of subtypes of cancer or CVD. Future large studies that include incidence data on subtypes of cancer and CVD are needed.
Conclusions
In conclusion, we observe a significant inverse association between MUAC and risk for all-cause and CVD deaths but not for cancer deaths in a Bangladeshi population. Among individuals with a normal BMI (18.5–24.9 kg/m2) or a low BMI (<18.5 kg/m2), a MUAC lower than <24 cm was a risk factor for all-cause and CVD deaths. The present study, however, is limited in lacking other anthropometric measures such as the circumferences of thigh, neck or waist and hip. Given that leanness is more prevalent in Asian than in Western populations, data from the present study and previous studies suggest the need of information on other anthropometric measures in assessing BMI-associated disease risk, especially in Asian populations.
Supplementary Data
Supplementary data are available at IJE online.
Funding
This work was supported by the National Institutes of Health [grants R01ES017541, P42ES010349, P30ES000260, R21ES023421, and R01CA107431]. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Supplementary Material
Acknowledgments
Y.C. and H.A. designed the study. W.G. analysed the data. Y.C. and W.G. wrote the paper. F.P., M.A. and H.A. helped interpret the results. M.E., A.A., T.I., M.R.Z., R.H., D.L. and G.S. contributed to the acquisition of data and revised the manuscript critically for important intellectual content. All authors read and approved the final version of the manuscript. Y.C. is the guarantor for the paper. References have been checked for accuracy and completeness.
Conflict of interest: None declared.
References
- 1.Whitlock G, Lewington S, Sherliker P, et al. Body-mass index and cause-specific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet 2009;373:1083–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ajani UA, Lotufo PA, Gaziano JM, et al. Body mass index and mortality among US male physicians. Ann Epidemiol 2004;14:731–39. [DOI] [PubMed] [Google Scholar]
- 3.Allison D, Gallagher D, Heo M, Pi-Sunyer F, Heymsfield S. Body mass index and all-cause mortality among people age 70 and over: the Longitudinal Study of Aging. In J Obes Relat Metab Disord 1997;21:424. [DOI] [PubMed] [Google Scholar]
- 4.Song Y-M, Sung J. Body mass index and mortality: a twelve-year prospective study in Korea. Epidemiology 2001;12:173–79. [DOI] [PubMed] [Google Scholar]
- 5.Gu D, He J, Duan X, et al. Body weight and mortality among men and women in China. JAMA 2006;295:776–83. [DOI] [PubMed] [Google Scholar]
- 6.Heitmann BL, Erikson H, Ellsinger BM, Mikkelsen KL, Larsson B. Mortality associated with body fat, fat-free mass and body mass index among 60-year-old Swedish men – a 22-year follow-up. The study of men born in 1913. Int J Obes Relat Metab Disord 2000;24:33–37. [DOI] [PubMed] [Google Scholar]
- 7.Abraham S, Carroll MD, Najjar MF, Fulwood R. Obese and overweight adults in the United States. Vital Health Stat 1983;11:1–93. [PubMed] [Google Scholar]
- 8.Mwangome MK, Fegan G, Fulford T. Mid-upper arm circumference at age of routine infant vaccination to identify infants at elevated risk of death: a retrospective cohort study in the Gambia. Bull World Health Organ 2012;90:887–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Allison DB, Zhu SK, Plankey M, Faith MS, Heo M. Differential associations of body mass index and adiposity with all-cause mortality among men in the first and second National Health and Nutrition Examination Surveys (NHANES I and NHANES II) follow-up studies. Int J Obes Relat Metab Disord 2002;26:410–16. [DOI] [PubMed] [Google Scholar]
- 10.Mason C, Craig CL, Katzmarzyk PT. Influence of central and extremity circumferences on all-cause mortality in men and women. Obesity (Silver Spring) 2008;16: 2690–95. [DOI] [PubMed] [Google Scholar]
- 11.Landi F, Russo A, Liperoti R, et al. Midarm muscle circumference, physical performance and mortality: results from the aging and longevity study in the Sirente geographic area (ilSIRENTE study). Clin Nutr 2010;29:44–47. [DOI] [PubMed] [Google Scholar]
- 12.Tsai AC, Chang TL. The effectiveness of BMI, calf circumference and mid-arm circumference in predicting subsequent mortality risk in elderly Taiwanese. Br J Nutr 2011;105:275–81. [DOI] [PubMed] [Google Scholar]
- 13.Mondal D, Minak J, Alam M, et al. Contribution of enteric infection, altered intestinal barrier function, and maternal malnutrition to infant malnutrition in Bangladesh. Clin Infect Dis 2012;54:185–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hosegood V, Campbell OM. Body mass index, height, weight, arm circumference, and mortality in rural Bangladeshi women: a 19-y longitudinal study. Am J Clin Nutr 2003;77:341–47. [DOI] [PubMed] [Google Scholar]
- 15.Ahsan H, Chen Y, Parvez F, et al. Health Effects of Arsenic Longitudinal Study (HEALS): description of a multidisciplinary epidemiologic investigation. J Expo Sci Environ Epidemiol 2006;16:191–205. [DOI] [PubMed] [Google Scholar]
- 16.Wang YH, Wu MM, Hong CT, et al. Effects of arsenic exposure and genetic polymorphisms of p53, glutathione S-transferase M1, T1, and P1 on the risk of carotid atherosclerosis in Taiwan. Atherosclerosis 2007;192:305–12. [DOI] [PubMed] [Google Scholar]
- 17.Chen Y, Graziano JH, Parvez F, et al. Arsenic exposure from drinking water and mortality from cardiovascular disease in Bangladesh: prospective cohort study. BMJ 2011;342:d2431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Aho K, Harmsen P, Hatano S, Marquardsen J, Smirnov VE, Strasser T. Cerebrovascular disease in the community: results of a WHO collaborative study. Bull World Health Organ 1980;58:113–30. [PMC free article] [PubMed] [Google Scholar]
- 19.Mumford JL, Wu K, Xia Y, et al. Chronic arsenic exposure and cardiac repolarization abnormalities with QT interval prolongation in a population-based study. Environ Health Perspect 2007;115:690–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ronsmans C, Vanneste AM, Chakraborty J, Van Ginneken J. A comparison of three verbal autopsy methods to ascertain levels and causes of maternal deaths in Matlab, Bangladesh. Int J Epidemiol 1998;27:660–66. [DOI] [PubMed] [Google Scholar]
- 21.Sohel N, Persson LA, Rahman M, et al. Arsenic in drinking water and adult mortality: a population-based cohort study in rural Bangladesh. Epidemiology 2009;20:824–30. [DOI] [PubMed] [Google Scholar]
- 22.Chen Y, McClintock TR, Segers S, et al. Prospective investigation of major dietary patterns and risk of cardiovascular mortality in Bangladesh. Int J Cardiol 2013;167:1495–501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wu F, Chen Y, Parvez F, et al. A prospective study of tobacco smoking and mortality in Bangladesh. PloS One 2013;8:e58516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Argos M, Kalra T, Rathouz PJ, et al. Arsenic exposure from drinking water, and all-cause and chronic-disease mortalities in Bangladesh (HEALS): a prospective cohort study. Lancet 2010;376:252–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Heck JE, Marcotte EL, Argos M, et al. Betel quid chewing in rural Bangladesh: prevalence, predictors and relationship to blood pressure. Int J Epidemiol 2012;41:462–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ahsan H, Chen Y, Parvez F, et al. Arsenic exposure from drinking water and risk of premalignant skin lesions in Bangladesh: baseline results from the Health Effects of Arsenic Longitudinal Study. Am J Epidemiol 2006;163:1138–48. [DOI] [PubMed] [Google Scholar]
- 27.Cavallari JM, Eisen EA, Fang SC, et al. PM2.5 metal exposures and nocturnal heart rate variability: a panel study of boilermaker construction workers. Environ Health 2008;7:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Willet W. Nutritional Epidemiology. New York: Oxford Uniersity Press, 1998. [Google Scholar]
- 29.Bates CJ, Hamer M, Mishra GD. A study of relationships between bone-related vitamins and minerals, related risk markers, and subsequent mortality in older British people: the National Diet and Nutrition Survey of People Aged 65 Years and Over. Osteoporos Int 2012;23:457–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wijnhoven HA, van Bokhorst-de van der Schueren MA, Heymans MW, et al. Low mid-upper arm circumference, calf circumference, and body mass index and mortality in older persons. J Gerontol A Biol Sci Med Sci 2010;65:1107–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wannamethee SG, Shaper AG, Lennon L, Whincup PH. Decreased muscle mass and increased central adiposity are independently related to mortality in older men. Am J Clin Nutr 2007;86:1339–46. [DOI] [PubMed] [Google Scholar]
- 32.Woo J, Ho SC, Sham A. Longitudinal changes in body mass index and body composition over 3 years and relationship to health outcomes in Hong Kong Chinese age 70 and older. J Am Geriatr Soc 2001;49:737–46. [DOI] [PubMed] [Google Scholar]
- 33.Zhu S, Heo M, Plankey M, Faith MS, Allison DB. Associations of body mass index and anthropometric indicators of fat mass and fat free mass with all-cause mortality among women in the first and second National Health and Nutrition Examination Surveys follow-up studies. Ann Epidemiol 2003;13:286–93. [DOI] [PubMed] [Google Scholar]
- 34.Menotti A, Puddu PE, Lanti M, Maiani G, Fidanza F. Cardiovascular risk factors predict survival in middle-aged men during 50 years. Eur J Intern Med 2013;24:67–74. [DOI] [PubMed] [Google Scholar]
- 35.Puddu PE, Menotti A, Tolonen H, Nedeljkovic S, Kafatos AG. Determinants of 40-year all-cause mortality in the European cohorts of the Seven Countries Study. Eur J Epidemiol 2011;26:595–608. [DOI] [PubMed] [Google Scholar]
- 36.Dontas AS, Menotti A, Aravanis C, Ioannidis P, Seccareccia F. Comparative total mortality in 25 years in Italian and Greek middle aged rural men. J Epidemiol Community Health 1998;52:638–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Menotti A, Giampaoli S. A single risk factor measurement predicts 35-year mortality from cardiovascular disease. Giornale italiano di cardiologia 1998;28:1354–62. [PubMed] [Google Scholar]
- 38.Menotti A, Conti S, Dima F, et al. Prediction of all causes of death as a function of some factors commonly measured in cardiovascular population surveys. Prev Med 1983;12:318–25. [DOI] [PubMed] [Google Scholar]
- 39.Pitsavos C, Panagiotakos DB, Chrysohoou C, Stefanadis C. Epidemiology of cardiovascular risk factors in Greece: aims, design and baseline characteristics of the ATTICA study. BMC Public Health 2003;3:32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Yao CH, Slattery ML, Jacobs DR, Jr, Folsom AR, Nelson ET. Anthropometric predictors of coronary heart disease and total mortality: findings from the US Railroad Study. Am J Epidemiol 1991;134:1278–89. [DOI] [PubMed] [Google Scholar]
- 41.Oppert JM, Charles MA, Thibult N, Guy-Grand B, Eschwege E, Ducimetiere P. Anthropometric estimates of muscle and fat mass in relation to cardiac and cancer mortality in men: the Paris Prospective Study. Am J Clin Nutr 2002;75:1107–13. [DOI] [PubMed] [Google Scholar]
- 42.Stevens J, Keil JE, Rust PF, et al. Body mass index and body girths as predictors of mortality in black and white men. Am J Epidemiol 1992;135:1137–46. [DOI] [PubMed] [Google Scholar]
- 43.Seccareccia F, Menotti A. Physical activity, physical fitness and mortality in a sample of middle aged men followed up 25 years. J Sports Med Phys Fitness 1992;32:206–13. [PubMed] [Google Scholar]
- 44.Hu G, Tuomilehto J, Silventoinen K, Barengo N, Jousilahti P. Joint effects of physical activity, body mass index, waist circumference and waist-to-hip ratio with the risk of cardiovascular disease among middle-aged Finnish men and women. Eur Heart J 2004;25:2212–19. [DOI] [PubMed] [Google Scholar]
- 45.Pierce BL, Kalra T, Argos M, et al. A prospective study of body mass index and mortality in Bangladesh. Int J Epidemiol 2010;39:1037–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Chen Y, Copeland WK, Vedanthan R, et al. Association between body mass index and cardiovascular disease mortality in east Asians and south Asians: pooled analysis of prospective data from the Asia Cohort Consortium. BMJ 2013;347:f5446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zheng W, McLerran DF, Rolland B, et al. Association between body-mass index and risk of death in more than 1 million Asians. N Engl J Med 2011;364:719–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Heitmann BL, Erikson H, Ellsinger BM, Mikkelsen KL, Larsson B. Mortality associated with body fat, fat-free mass and body mass index among 60-year-old Swedish men – a 22-year follow-up. The study of men born in 1913. Int J Obes Relat Metab Disord 2000;24:33–37. [DOI] [PubMed] [Google Scholar]
- 49.Chenskikh EP, Nikolenko NK. [Electric stimulation of muscles in patients with tuberculous spondylitis complicated by spastic paresis and paralysis]. Ortopediia Travmatologiia i Protezirovanie 1975:66–68. [PubMed] [Google Scholar]
- 50.Olsen DB, Sacchetti M, Dela F, Ploug T, Saltin B. Glucose clearance is higher in arm than leg muscle in type 2 diabetes. J Physiol 2005;565:555–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Blaak EE, Wagenmakers AJ, Glatz JF, et al. Plasma FFA utilization and fatty acid-binding protein content are diminished in type 2 diabetic muscle. Am J Physiol Endocrinol Metab 2000;279:E146–54. [DOI] [PubMed] [Google Scholar]
- 52.Blaak EE, Wagenmakers AJ. The fate of [U-(13)C]palmitate extracted by skeletal muscle in subjects with type 2 diabetes and control subjects. Diabetes 2002;51:784–89. [DOI] [PubMed] [Google Scholar]
- 53.Heitmann BL, Frederiksen P. Thigh circumference and risk of heart disease and premature death: prospective cohort study. BMJ 2009;339:b3292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Preis SR, Pencina MJ, D'Agostino RB, Sr, Meigs JB, Vasan RS, Fox CS. Neck circumference and the development of cardiovascular disease risk factors in the Framingham Heart Study. Diabetes Care 2013;36:e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.