Abstract
Background
Ankylosing spondylitis (AS), an inflammatory arthritis that affects the axial skeleton, predisposes patients with severe disease to falls and spinal fractures. Advanced imaging has improved the process of fracture detection. In spite of increased knowledge about early diagnosis and management of AS, little attention is being paid to the environmental hazards that pose a risk for patient outcome.
Objectives
To identify risk factors for falls and fractures and evaluate imaging modalities in the detection of fractures in AS patients.
Methods
A case report and review of the literature using PubMed for English articles from 2000 to 2013 regarding AS patients’ risk factors for falls and fractures and imaging modalities used to diagnose fracture in this population.
Results
Potential impairments in balance and coordination in the AS population include vestibular dysfunction, thoracolumbar kyphosis, and deficits in proprioception. A common and significant environmental risk factor for falls includes the use of a tub-shower arrangement. Furthermore, osteoporosis is a well-known complication of AS that can predispose to fracture. Lastly, there are no comprehensive studies that have evaluated the ability of advanced imaging modalities to identify an acute spine fracture in this patient population.
Conclusions
AS patients with advanced disease are at increased risk of falls and fractures due to many factors including but not limited to a rigid spine and difficulty with peripheral vision. A tub-shower arrangement commonly found in homes and hotel rooms is a major hazard. A consistent approach to diagnosis of fractures involving advanced imaging recommendations should be considered.
Introduction
Ankylosing spondylitis (AS) is a chronic inflammatory disease predominantly involving the axial skeleton that, in more advanced cases, can lead to clinically important problems with balance and coordination, and ultimately falls (1). For example, increased thoracolumbar kyphosis and hip flexion result in changes to the body's center of gravity displacing it anteriorly (1,2). As the kyphosis worsens, horizontal gaze becomes impaired (2). Chronic spine changes in AS, including syndesmophyte formation, ankylosis, and osteoporosis, predisposes these individuals to spine fractures even after minor trauma, particularly falls (3).
The reported prevalence of vertebral fracture in AS patients ranges from 0.4 to 32.4% (4,5,6). In a study coordinated by the Ankylosing Spondylitis International Federation in Germany and Denmark evaluating the prevalence and characteristics of clinically confirmed vertebral fractures, over 15,000 questionnaires were sent to their members (7). It was found that 59 of these members (0.4%) reported having suffered 66 clinically confirmed vertebral fractures (7). Thirty-seven (56%) of these fractures were associated with no to low/medium trauma, with 47% of patients reporting neurologic complications (7). Interestingly, most neurologic complications occurred either without trauma (n=11, 35%) or after minimal trauma (n=7, 23%) with 65% of these patients never regaining full neurologic recovery (7). Standard imaging is not always helpful in diagnosing spine fractures in AS patients. Spine radiographs with their two-dimensional approach are often difficult to read given the distorted anatomy resulting from a kyphotic spine (8,9). Some emphasize the advantage of MRI over CT given that it is more sensitive at detecting soft tissue abnormalities and neurologic manifestations such as spinal cord damage (10). There have been only a few studies regarding the appropriate indications for different imaging modalities to uncover fracture in this patient population. Herein we report the case of an AS patient with a spine fracture resulting from a tub-shower transfer, and we review the literature on risk factors for falls and fractures as well as the appropriateness of currently employed as well as advanced imaging modalities to diagnose fracture in this population
Methods
We searched PubMed for articles published between 2000 and 2013 using the following search terms: “ankylosing spondylitis” and “spine fracture imaging,” “osteoporosis,” “bathtub,” “gait,” and “balance.” The references in retrieved articles were checked. Online sources from the Centers for Disease Control and National Safety council were reviewed for articles and statistics regarding falls and bathroom injuries.
Case Report
A 51-year-old male with long-standing AS presented to the emergency department (ED) after falling backwards while exiting a tub-shower in a hotel room and hitting his head. He provided this history to the ED and also complained of neck and mid-back pain. He was neurologically intact. He had normal upper and lower extremity strength, no pathologic reflexes, and no bowel or bladder incontinence with normal rectal tone. A plain radiograph of the cervical spine was limited to approximately the C5 spine level, and follow-up CT imaging of the entire cervical spine did not show evidence of a fracture (Figure 1). He was discharged home with pain medications. Almost 24 hours later from his initial visit, the patient returned to the ED, this time complaining of severe mid-back pain. On exam, he was noted to have mild right triceps weakness and decreased sensation of the right hand. An MRI of the thoracic spine, which also captured part of the lower cervical spine, was completed approximately 20 hours after the initial CT scan. The findings demonstrated an acute fracture extending through the anterior superior aspect of the C7 vertebral body extending into the C6-7 disc (Figure 2a). This finding was not seen, even on retrospective analysis, on the initial CT scan. A repeat CT scan following the MR study also revealed a fracture with 5mm of anterior subluxation at C6-7 level (Figure 2b). The patient was subsequently placed in a cervical collar and urgently transferred to another facility for neurosurgical evaluation.
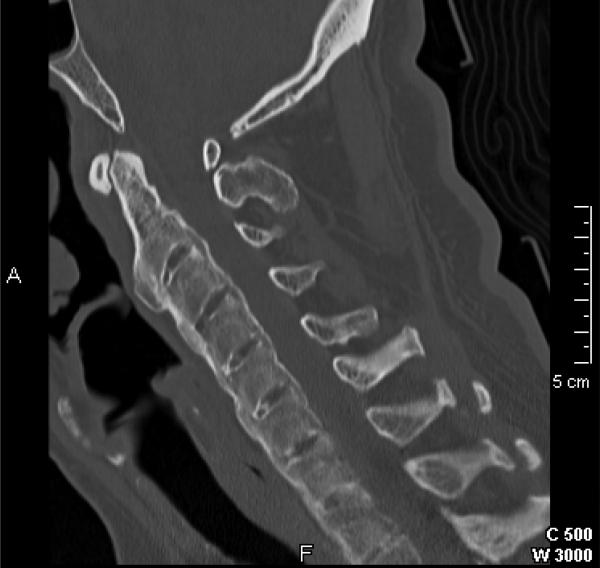
Figure 1.
CT scan of the cervical spine with sagittal reconstruction completed on 5/15/12 at 12:47am, no fracture identified.
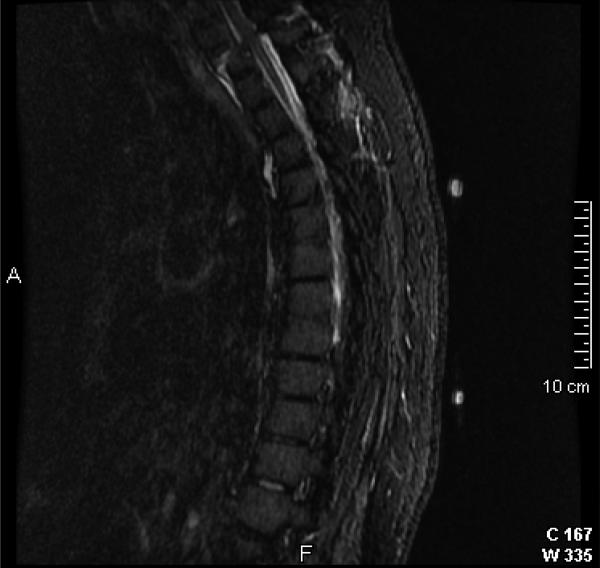
Figure 2a.
MR thoracic spine completed on 5/15/12 at 9:15pm, displaced fracture involving the C7 vertebral body extending into the C6-7 disc space.
Figure 2b.
Repeat CT scan of the cervical spine with sagittal reconstruction completed on 5/16/12 at 1:28am, same level pictured as CT scan completed approximately 25 hours prior now demonstrates a displaced fracture at the C7 vertebral body.
The patient was diagnosed with AS at 43 years of age. Past medical history included hypertension, hyperlipidemia, and “hip pain” that started when he was 17 years-old. By his mid-30s, the patient had increased morning stiffness and neck pain. An episode of acute anterior uveitis occurred at age 42. Medications at presentation to the ED included adalimumab, simvastatin, nebivolol, valsartan, and 325 mg of daily aspirin. The patient had no known drug allergies. His social history was significant for being a life-long non-smoker, occasional alcohol consumption, and no illicit drug use. His family history was negative for ankylosing spondylitis or other rheumatologic diseases.
Laboratory data at presentation was remarkable for a leukocytosis with neutrophil predominance. The white blood cell count was 16.9 uL (normal, 4.5-10 × (10) 3/uL) with 14.01 uL absolute neutrophils (normal 2.25-7.00 × (10) 3/uL). At the time of his AS diagnosis at age 43, anterior, posterior and lateral lumbar spine radiographs revealed complete fusion of the sacroiliac joints (grade 4 sacroiliitis) as well as advanced syndesmophytic changes in the lumbar spine and ossification of the spinal ligaments (Figure 3). Though he had significant radiographic damage, the patient experienced improvement in pain, flexibility and function during 8 years on anti-TNF therapy.
Figure 3.
AP and lateral lumbar spine radiograph completed at the time of diagnosis of AS, showing fused SI joints, lumbar spine vertebral bodies, and facet joints
The patient failed conservative management using both Gardner-Wells tongs and halo placement to help stabilize the cervical spine, which were instituted during the first two days of his hospitalization. He was subsequently taken to the operating room for posterior cervical instrumentation and fusion from C4 to T2. Although he did well postoperatively, there remained a non-union at the fracture site. Given the patient's longstanding history of AS, the stability of the fracture site was thought to be suboptimal. The next morning, the patient underwent surgical correction with C6-7 anterior cervical fusion, open reduction and internal fixation of C6-7 fracture, and anterior cervical plating. The patient was discharged several days later with a normalized white blood cell count, ambulatory, and with minimal pain. He was asked to hold his daily aspirin post-procedure but otherwise continued his other medications. He has done well since, returned to work, and resumed his daily aspirin.
Results
Balance and Coordination
Amor-Dorado et al. described an increased frequency of vestibular impairments, including abnormalities in head-shaking nystagmus, caloric tests, and clinical tests of sensory integration and balance in patients with AS compared to healthy-matched controls (11). The authors did not adjust for NSAID use, which may have confounded the results. While the majority of AS patients used NSAIDs, the majority of controls did not. Use of NSAIDs may increase the frequency of NSAID-induced audiovestibular dysfunction (11). However, the only NSAID with known ototoxic properties is aspirin and there is only one published study reporting persistent vestibulopathy linked to a 3-day course of high-dose aspirin use (12).
A review by Pompeu et al., describes how thoracolumbar kyphosis and hip flexion increase with progression of AS (1). As kyphosis worsens, horizontal gaze becomes impaired (1). Compensation may occur through knee flexion and ankle plantar flexion as seen in static posture analysis (1). Del Din et al. used three-dimensional kinematics to assess gait in 12 AS patients on anti-TNF therapy compared with 12 healthy controls (13). Significant abnormalities were seen in the sagittal plane including reduced hip and knee joint extension (p < 0.044), decreased ankle plantar-flexion (p<0.048) and the absence of the heel rocker (heel strike at initial contact with subsequent ankle plantarflexion) (13). Both static and dynamic balance were significantly compromised in the AS group (13).
Spinal enthesopathy may contribute to impaired proprioception through deficits in sensing spine position (1). We were unable to find any studies that evaluated the impact of impaired proprioception in AS patients.
Slips and Falls
Slips and falls in general are a major clinical problem and hold an increased risk for devastating consequences in AS subjects. They account for about 8.9 million emergency room visits each year (14). In 2010, the United States Centers for Disease Control (CDC) reported that the rate of nonfatal fall injury episodes for which a healthcare provider was contacted was 43 per 1000 population (15). The highest rate was for individuals over the age of 75 years (15,16). In 2008, the highest rate of bathroom injuries occurred in and around the tub or shower, approximating 65.8 per 100,000 population (16).
Although it is intuitive that a tub-shower arrangement would pose a significant challenge to someone with the impairments present in AS subjects, there are no studies addressing tub-shower transfers in the AS population. In a study of 60 healthy subjects without lower limb disease or balance disorders divided into three age groups ranging from 20 to 70 years, the friction of subjects entering and exiting a typical bathtub under dry and wet conditions was measured using force plates (17). Normally, when the feet contact a potentially slippery surface, adaptations including using a flatter foot angle, as well as decreased shear force and friction are used (17). Subjects in the oldest age group displayed more caution than their younger counterparts by using less friction during exiting movements (17).
In an investigation that might be more relevant to our AS patients, examination of environmental utilization during bathtub transfers was evaluated in a study of 89 elderly adults aged 60 and older who reported independence in bathing (18). Of these 89 adults, 53% were evaluated during a bath transfer and the remaining 47% were evaluated transferring into a shower stall (18). In subjects evaluated during bathtub transfers, 19.4% were found to unsafely use their environment, such as by using towel bars or shower curtains to maintain balance (18). It is not difficult to imagine that an AS patient would be significantly challenged by this environment.
Osteoporosis and Fractures
Osteoporosis is a well-known complication of AS (19,20,21). There are no existing guidelines for the screening of osteoporosis in AS (20) and imaging in this population is difficult to interpret. Syndesmophyte formation and ligament ossification seen in advanced disease may obscure the results of lumbar spine dual-energy X-ray absorptiometry (DXA), making it a less reliable (22). Because bone loss is often more significant in the lumbar spine, the presence of osteopenia may not be detected in hip imaging (22).
Vertebral fractures are associated with low bone mineral density scores of the femoral neck in AS patients (19). Klingberg et al. evaluated 204 AS patients (57% male) with a mean age of 50 ± 13 years and disease duration of 15 ± 11 years (19). According to the World Health Organization (WHO) definition for osteopenia and osteoporosis for patients aged 50 years and older, 21% of the patients in this study had osteopenia and 44% had osteoporosis (19). In subjects younger than 50 years of age, 5% were found to have bone mineral densities below that expected for their age (19). The prevalence of vertebral fracture as diagnosed through lateral spine radiographs was 11.8%; only three of the 24 subjects diagnosed with a fracture had previous knowledge of this diagnosis (19). Using logistic regression analysis, independent risk factors for vertebral fractures included high Bath Ankylosing Spondylitis Patient Global Score-2 (BASG-2), low bone mineral density in the femoral neck, and low lumbar volumetric bone mineral density (19).
Ghozlani et al. found the prevalence of osteoporosis to be 25% in a study of 67 men and 13 women with a mean age of 38.9 ± 11.8 and disease duration of 10.8 ± 6.6 years using DXA scans of the lumbar spine and femurs (23). To diagnose vertebral fracture, software known as “vertebral fracture assessment” was used to review lateral lumbar DXA images (23). Vertebral fractures were present in 35.3% of those with osteoporosis in the lumbar spine and 33.3% of those with osteoporosis in the hip (23).
Jun et al. observed an association between low bone mineral density scores of the femoral neck and increased risk of vertebral fracture in their AS study population (24). In this cross-sectional study, 68 men with AS aged 30.7 ± 6.5 years with 86 ± 65 month disease duration and 91 age and sex-matched controls were enrolled to assess for an association between vertebral fractures and other clinical variables (24). Radiographs revealed that 11 of the 68 AS patients had lumbar vertebral fractures (24). Using multiple logistic regression analyses, it was found that low intertrochanteric bone mineral density values correlated with an increased risk of these vertebral fractures (p<0.041) (24). Interestingly, in a study regarding early spondyloarthropathy and osteoporosis, low bone mineral density was strongly associated with male sex and severity of disease activity as indicated by high functional disease activity scores (BASMI and BASFI) and correlated with elevated inflammatory markers such as CRP (25).
Imaging modalities
The lower cervical spine is the most common site of spine injury in patients with AS and poses the greatest threat to patient safety as well as marked challenges to selection of imaging assessments (26). There are no practice guidelines that outline which image modality to use in AS patients following a fall. Harrop et al. describe a patient with a cervical fracture who was not diagnosed with plain radiographs, single-detector CT with reconstructed images, and MRI; instead, a transverse fracture through the C6-7 spine was seen by high-definition multidetector CT after the standard imaging was negative (26). It is unclear how much time elapsed from the time of fracture to the time of eventual diagnosis for this patient. The authors argue that standard imaging failed to detect the cervical fracture and infer that the high-resolution multi-detector CT was necessary (26). Others report that MRI may be a better imaging modality as it is more sensitive than CT at detecting soft tissue abnormalities and neurologic manifestations such as spinal cord damage, intramedullary edema, and epidural hematomas (10).
Wang et al. conducted the only study that compares radiographs, CT, 3D-CT and MRI in both acute and chronic spine fractures in AS (27). In this retrospective review, MR imaging files of 12 subjects with spine fractures and a previous diagnosis of AS were identified (27). All 12 subjects had conventional radiographs and MRI scans, 7 had CT scans, and 4 had 3D-CT scans (27). MRI and 3D-CT both had 100% sensitivity in detecting facet fractures and spinous process fractures of the thoracic and cervical spines (27). CT and plain radiographs had 80% and 40% sensitivity, respectively, for detecting facet fractures (27). None of the subjects who had CT scans had spinous process fractures in the cervical spine; however, plain films displayed 100% sensitivity for detecting fractures in that region (27). For spinous process fractures in the thoracic spine, CT scan had 50% sensitivity whereas radiographs had 75% sensitivity (27). Lastly, while MRI had 100% sensitivity and specificity for detecting occult fractures, there was no data available to evaluate the ability of 3D-CT to detect these fractures (27). Time from trauma varied from 1 day to over 30 months before imaging was completed, which obscures the utility of this data when deciding which imaging modality to choose in the acute care setting when the patient presents with pain after a fall (27).
Discussion
To our knowledge, this is the first manuscript addressing the lack of comprehensive studies regarding the diagnosis of acute cervical spine fracture in this high-risk population. Our patient had a potentially avoidable complication of an unstable displaced cervical spine fracture after a slip and fall during a shower-tub transfer. The fracture was only diagnosed when it had already displaced and produced a neurologic deficit prompting the patient to return ED. His initial physical exam was unremarkable, and the CT scan taken at presentation to the ED failed to reveal the fracture. After continued pain and the presence of a new neurologic deficit, this fracture was seen on MRI approximately 20 hours after the negative CT scan; it is entirely possible that an MRI taken at the time of the initial visit to the ED would have revealed the fracture and prompted immediate stabilization of the patient’ spine.
Our literature review shows that there are no comprehensive studies comparing different imaging modalities to assess acute spine fracture in the AS population. Consequently, we recommend that a high index of suspicion should be maintained for spine fracture in the setting of minor trauma with a normal physical exam and negative imaging on x-ray or CT scan. However, there are no studies to convincingly demonstrate whether an MRI may be more sensitive than a CT scan for an acute spine fracture. Nevertheless, our case does demonstrate that an acute fracture can be present with a negative CT in an AS subject. An earlier diagnosis in this patient might have prevented the subsequent fracture displacement and its sequelae including a two stage surgical procedure. We suggest, from this experience and the absence of confirmation in the literature, that an MRI should be considered when suspicion is high and initial work up with plain x-ray or CT scan is negative. More studies are needed to identify which imaging modalities are optimal at the outset for detecting potentially life-altering pathology when an AS subject presents with a fracture risk.
Conclusion
From our literature review it is apparent that AS patients are at high risk for fracture of the spine due to impairments in balance and coordination, susceptibility to slips and falls from environmental hazards, and osteoporosis. In the future, studies regarding the optimal imaging modality to diagnose acute cervical fracture in this high-risk patient population need to be completed. Hazardous areas for slips and falls include the bathroom and more specifically a tub-shower arrangement that is found in most hotel rooms and likely in many residences. Efforts to reduce potential morbidity, including falls resulting in spinal fractures when transferring in this hazardous environment should be made on a large scale with an educational focus for patients and their families.
Acknowledgments
Funding Source
No funding was provided to aid in the completion of this article.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Competing Interests
None of the authors declared competing interests
References
- 1.Pompeu JE, Romano RS, Pompeu SM, Lima SM. Static and dynamic balance in subjects with ankylosing spondylitis: literature review. Rev Bras Reumatol. 2012;52(3):409–16. [PubMed] [Google Scholar]
- 2.Debarge R, Demey G, Roussouly P. Sagittal balance analysis after pedicle subtraction osteotomy in ankylosing spondylitis. Eur Spine J. 20(5):619–625. doi: 10.1007/s00586-011-1929-9. 201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chaudhary SB, Hullinger H, Vives MJ. Management of Acute Spinal Fractures in Ankylosing Spondylitis. ISRN Rheumatol. 2011:150484. doi: 10.5402/2011/150484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Montala N, Juanola X, Collantes E, Munoz-Gomariz E, Gonzalez C, Gratacos J, et al. Prevalence of Vertebral Fractures by Semiautomated Morphometry in Patients with Ankylosing Spondylitis. J Rheumatol. 2011;38(5):893–897. doi: 10.3899/jrheum.100851. [DOI] [PubMed] [Google Scholar]
- 5.Klingberg E, Geijer M, Gothlin J, Mellstrom D, Lorentzon M, Hilme E, et al. Vertebral Fractures in Ankylosing Spondylitis are Associated with Lower Bone Mineral Density in Both Central and Peripheral Skeleton. J Rheumatol. 2012;39(10):1987–1995. doi: 10.3899/jrheum.120316. [DOI] [PubMed] [Google Scholar]
- 6.Sambrook PN, Geusens P. The Epidemiology of Osteoporosis and Fractures in Ankylosing Spondylitis. Ther Adv Musculoskelet Dis. 2012;4(4):287–92. doi: 10.1177/1759720X12441276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Vosse D, Feldtkeller E, Erlendsson J, Guesens P, van der Linden S. Clinical vertebral fractures in patients with ankylosing spondylitis. J Rheumatol. 2004;31(10):1981–1985. [PubMed] [Google Scholar]
- 8.Jacobs WB, Fehlings MG. Ankylosing spondylitis and spinal cord injury: origin, incidence, management, and avoidance. Neurosurgical Focus. 2008;24(1):E12. doi: 10.3171/FOC/2008/24/1/E12. [DOI] [PubMed] [Google Scholar]
- 9.Anwar F, Al-Khayer A, Joseph G, Fraser MH, Jigajinni MV, Allan DB. Delayed presentation and diagnosis of cervical spine injuries in long-standing ankylosing spondylitis. Eur Spine J. 2011;20(3):403–407. doi: 10.1007/s00586-010-1628-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anwar F, Al-Khayer A, Joseph G, Fraser MH, Jigajinni MV, Allan DB. Delayed presentation and diagnosis of cervical spine injuries in long-standing ankylosing spondylitis. Eur Spine J. 2011;20(3):403–407. doi: 10.1007/s00586-010-1628-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Amor-Dorado JC, Barreira-Fernandez MP, Vazquez-Rodriguez TR, Gomez-Acebo I, Miranda-Filloy JA, Diaz de Teran T, et al. Audiovestibular manifestations in patients with ankylosing spondylitis. Medicine (Baltimore) 2011;90(2):99–109. doi: 10.1097/MD.0b013e3182079866. [DOI] [PubMed] [Google Scholar]
- 12.Strupp M, Jahn K, Brandt T. Another adverse effect of aspirin: bilateral vestibulopathy. J Neurol Neurosurg Psychiatry. 2003;74(5):691. doi: 10.1136/jnnp.74.5.691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Del Din S, Carraro E, Sawacha Z, Guitto A, Bonaldo L, Stefano M, et al. Impaired gait in ankylosing spondylitis. Med Biol Eng Comput. 2011;49(7):801–809. doi: 10.1007/s11517-010-0731-x. [DOI] [PubMed] [Google Scholar]
- 14. [April 5, 2013];National Safety Council. Falls. http://www.nsc.org/safety_home/HomeandRecreationalSafety/Falls/Pages/Falls.aspx.
- 15.Centers for Disease Control and Prevention [April 10, 2013];Home and recreational safety. http://www.cdc.gov/homeandrecreationalsafety/falls/index.html.
- 16.Stevens JA. Nonfatal bathroom injuries among persons aged >15 years – United States 2008. Weekly. 2011;60(22):729–733. [PubMed] [Google Scholar]
- 17.Siegmund GP, Flynn J, Mang DW, Chimich DD, Gardiner JC. Utilitzed friction when entering and exiting a dry and wet bathtub. Gait Posture. 2010;31(4):473–478. doi: 10.1016/j.gaitpost.2010.02.003. [DOI] [PubMed] [Google Scholar]
- 18.Murphy SL, Nyquist LV, Strasburg DM, Alexander NB. Bath transfers in older adult congregate housing residents: assessing the person-environment interaction. J Am Geriatr Soc. 2006;54(8):1265–1270. doi: 10.1111/j.1532-5415.2006.00814.x. [DOI] [PubMed] [Google Scholar]
- 19.Klingberg E, Geijer M, Gothlin J, Mellstrom D, Lorentzon M, Hilme E, et al. Vertebral fractures in ankylosing spondylitis are associated with lower bone mineral density in both central and peripheral skeleton. J Rheumatol. 2012;39(10):1987–1995. doi: 10.3899/jrheum.120316. [DOI] [PubMed] [Google Scholar]
- 20.Magrey M, Khan MA. Osteoporosis in anlyosing spondylitis. Curr Rheumatol Rep. 2010;12(5):332–336. doi: 10.1007/s11926-010-0122-1. [DOI] [PubMed] [Google Scholar]
- 21.Van der Weijden MAC, Claushuis TAM, Nazari T, Lems WF, Dijkmans BAC, van der Horst-Bruinsma IE. High prevalence of low bone mineral density in patients within 10 years of onset of ankylosing spondylitis: a systematic review. Clin Rheumatol. 2012;31(11):1529–1535. doi: 10.1007/s10067-012-2018-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Geusens P, Vosse D, van der Linden S. Osteoporosis and vertebral fractures in ankylosing spondylitis. Curr Opin Rheumatol. 2007;19(4):335–339. doi: 10.1097/BOR.0b013e328133f5b3. [DOI] [PubMed] [Google Scholar]
- 23.Ghozlani I, Ghazi M, Nouijai A, Mounach A, Rezqi A, Achemlal L, et al. Prevalence and risk factors of osteoporosis and vertebral fractures in patients with ankylosing spondylitis. Bone. 2009;44(5):772–776. doi: 10.1016/j.bone.2008.12.028. [DOI] [PubMed] [Google Scholar]
- 24.Jun JB, Joo KB, Her MY, Kim TH, Bae SC, Yoo DH, et al. Femoral bone mineral density is associated with vertebral fractures in patients with ankylosing spondylitis: a cross-sectional study. J Rheumatol. 2006;33(8):1637–1641. [PubMed] [Google Scholar]
- 25.Van der Weijden MA, van Denderen JC, Lems WF, Heymans MW, Dijkmans BA, van der Horst-Bruinsma IE. Low bone mineral density is related to male gender and decreased functional capacity in early spondylarthropathies. Clin Rheumatol. 2011;30(4):497–503. doi: 10.1007/s10067-010-1538-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Harrop JS, Sharan A, Anderson G, Hillibrand AS, Albert TJ, Flanders A, et al. Failure of standard imaging to detect a cervical fracture in a patient with ankylosing spondylitis. Spine (Phila Pa 1976) 2005;30(14):E417–419. doi: 10.1097/01.brs.0000170594.45021.67. [DOI] [PubMed] [Google Scholar]
- 27.Wang YF, Teng MM, Chang CY, Wu HT, Wang ST. Imaging manifestations of spinal fractures in ankylosing spondylitis. AJNR Am J Neuroradiol. 2005;26(8):2067–2076. [PMC free article] [PubMed] [Google Scholar]