Abstract
Reducing maternal and child mortality is a priority in the Millennium Development Goals (MDGs), and will likely remain so after 2015. Evidence exists on the investments, interventions and enabling policies required. Less is understood about why some countries achieve faster progress than other comparable countries. The Success Factors for Women’s and Children’s Health studies sought to address this knowledge gap using statistical and econometric analyses of data from 144 low- and middle-income countries (LMICs) over 20 years; Boolean, qualitative comparative analysis; a literature review; and country-specific reviews in 10 fast-track countries for MDGs 4 and 5a. There is no standard formula – fast-track countries deploy tailored strategies and adapt quickly to change. However, fast-track countries share some effective approaches in addressing three main areas to reduce maternal and child mortality. First, these countries engage multiple sectors to address crucial health determinants. Around half the reduction in child mortality in LMICs since 1990 is the result of health sector investments, the other half is attributed to investments made in sectors outside health. Second, these countries use strategies to mobilize partners across society, using timely, robust evidence for decision-making and accountability and a triple planning approach to consider immediate needs, long-term vision and adaptation to change. Third, the countries establish guiding principles that orient progress, align stakeholder action and achieve results over time. This evidence synthesis contributes to global learning on accelerating improvements in women’s and children’s health towards 2015 and beyond.
Résumé
La réduction de la mortalité maternelle et infantile est une priorité des objectifs du Millénaire pour le développement (OMD) et le restera probablement après l'échéance de 2015. Il existe des données sur les investissements, les interventions et les politiques habilitantes nécessaires. On comprend mal pourquoi certains pays ont réalisé des progrès plus rapidement que d'autres pays comparables. Les Facteurs de réussite des études sur la santé des femmes et des enfants ont cherché à combler ce manque de connaissances en utilisant les analyses statistiques et économétriques des données provenant de 144 pays à faible revenu et à revenu intermédiaire et recueillies depuis 20 ans: une analyse comparative qualitative booléenne; une étude bibliographique et des études spécifiques à chaque pays pour les 10 pays à progression rapide pour les points 4 et 5a des OMD. Il n'existe pas de formule standard – les pays à progression rapide ont déployé des stratégies personnalisées et se sont adaptés rapidement aux changements. Cependant, ces pays ont en commun des approches efficaces visant 3 grands axes afin de réduire la mortalité maternelle et infantile. Premièrement, ils impliquent de nombreux secteurs pour traiter les facteurs déterminants et cruciaux pour la santé. Près de la moitié de la réduction de la mortalité infantile dans les pays à faible revenu et à revenu intermédiaire depuis 1990 résulte des investissements dans le secteur de la santé, l'autre moitié étant attribuée aux investissements réalisés dans les secteurs extérieurs à la santé. Deuxièmement, ces pays utilisent des stratégies pour mobiliser les partenaires dans la société, en utilisant des données solides et opportunes pour la prise de décisions et la responsabilisation, ainsi qu'une approche de planification triple pour prendre en considération les besoins immédiats, la vision à long terme et l'adaptation aux changements. Troisièmement, ces pays établissent des principes directeurs qui orientent les progrès, harmonisent les actions des parties prenantes et génèrent des résultats dans le temps. Cette synthèse de données contribue à l’ensemble des connaissances requises pour accélérer les améliorations sur la santé des femmes et des enfants en vue de l'échéance de 2015 et au-delà.
Resumen
La reducción de la mortalidad materna e infantil es una prioridad en los Objetivos de Desarrollo del Milenio (ODM), y probablemente lo seguirá siendo después de 2015. Existen evidencias sobre las inversiones, las intervenciones y las políticas necesarias, pero se sabe menos acerca de por qué algunos países logran un progreso más rápido que otros países comparables. Los estudios relativos a los Factores de Éxito en la Salud de las Mujeres y los Niños han tratado de abordar esta brecha de conocimiento por medio de análisis estadísticos y econométricos de datos de 144 países de ingresos bajos y medianos (PIBM) a lo largo de más de 20 años, análisis comparativos cualitativos booleanos, revisión de la literatura y revisiones específicas de cada país en 10 países bien encarrilados para los ODM 4 y 5a. No existe una fórmula estándar, estos países despliegan estrategias a medida y se adaptan rápidamente a los cambios. Sin embargo, comparten ciertos enfoques eficaces a la hora de abordar tres áreas principales para reducir la mortalidad materna e infantil. En primer lugar, involucran a numerosos sectores para hacer frente a los factores sanitarios decisivos. Alrededor de la mitad de la reducción de la mortalidad infantil en los PIBM desde 1990 es el resultado de inversiones en el sector de la salud, y la otra mitad se atribuye a las inversiones realizadas en sectores fuera del ámbito sanitario. En segundo lugar, estos países utilizan estrategias para movilizar a socios a través de la sociedad, utilizando evidencias oportunas y sólidas para la toma de decisiones y la rendición de cuentas, así como un enfoque de planificación triple para considerar las necesidades inmediatas, la visión a largo plazo y la adaptación al cambio. En tercer lugar, los países establecen principios rectores que orientan el progreso, armonizan las acciones de las partes interesadas y logran resultados en el tiempo. Este compendio de evidencias contribuye al aprendizaje global sobre cómo acelerar las mejoras en la salud de mujeres y niños hacia el 2015 y más adelante.
ملخص
يمثل الحد من وفيات الأمومة والطفولة إحدى أولويات الأهداف الإنمائية للألفية (MDG) ويحتمل أن يظل كذلك بعد عام 2015. وتوجد بينات حول الاستثمارات والتدخلات وسياسات التمكين المطلوبة. ولا يزال ما نفهمه عن أسباب إحراز بعض البلدان للتقدم على نحو أسرع من غيرها من البلدان القابلة للمقارنة قليلاً. وقد استهدفت عوامل النجاح لدراسات صحة المرأة والطفل التعاطي مع هذه الثغرة المعرفية باستخدام التحليلات الإحصائية والاقتصادية القياسية للبيانات المستمدة من 144 بلداً من البلدان المنخفضة والمتوسطة الدخل (LMIC) على مدار 20 سنة؛ وتحليل المقارنة النوعي المنطقي؛ واستعراض الكتابات؛ والاستعراضات الخاصة بكل بلد في البلدان العشر في مبادرة المسار السريع من أجل تحقيق بلوغ الهدف 4 و5أ من الأهداف الإنمائية للألفية. ولا توجد صيغة موحدة - فبلدان مبادرة المسار السريع تنشر استراتيجيات مخصصة وتتكيف بسرعة مع التغيير. ومع ذلك، تشارك بلدان المسار السريع بعض النهج الفعالة في التعاطي مع المجالات الرئيسية الثلاثة بغية الحد من وفيات الأمومة والطفولة. أولاً، تقوم هذه البلدان بإشراك العديد من القطاعات في التعاطي مع المحددات الحاسمة في مجال الصحة. وقد نتج حوالي نصف الانخفاض في وفيات الطفولة في البلدان المنخفضة والمتوسطة الدخل منذ عام 1990 عن الاستثمارات في قطاع الصحة، ويعزى النصف الآخر إلى الاستثمارات في قطاعات خارج الصحة. ثانياً، تستخدم هذه البلدان استراتيجيات لحشد الشركاء في مختلف قطاعات المجتمع، باستخدام البينات القوية في الوقت المناسب لاتخاذ القرارات والمساءلة ونهج تخطيط ثلاثي لدراسة الاحتياجات العاجلة والرؤية طويلة الأمد والتكيف مع التغير. ثالثاً، تضع البلدان المبادئ الإرشادية التي توجه التقدم وتتواءم مع إجراءات أصحاب المصلحة وتحقق النتائج بمرور الوقت. ويسهم تركيب البينات في التعلم العالمي المعني بتسريع التحسينات في مجال صحة المرأة والطفل صوب عام 2015 وما بعده.
摘要
降低孕产妇和儿童死亡率是千年发展目标(MDG)的当务之急,在2015年之后可能仍是如此。证据存在于所需的投资、干预和支持政策。一些国家比其他类似国家取得更快进展的原因还有待于进一步探讨。妇女和儿童健康的成功因素研究试图弥合这一知识差距,其中利用了对20多年来144个中低收入国家(LMIC)的数据进行的统计学和计量经济学分析;布尔、定性比较分析;文献综述;在10个取得快速进展国家对MDG 4和5a实现情况的国别回顾。不存在放之四海皆准的公式——高绩效国家因地制宜部署策略,应对变化进行调整时行动迅速。但是在解决三个主要领域问题来降低孕产妇和儿童死亡率方面,走在快车道上的国家拥有某些相同的有效方法。首先,这些国家组织多个部门参与以应对至关重要的健康决定因素。自1990年以来,LMIC国家中大约一半儿童死亡率减少归因于卫生部门投入,另一半则归因于健康以外行业的投入。其次,这些国家使用策略动员全社会合作伙伴:使用及时、健壮的证据进行决策和问责,并采用三重规划方法来考虑紧急需求、长期愿景和应变调整。第三,这些国家建立了确定发展方向、协调利益相关者行动的指导原则,久而久之收到成效。本次证据综合积累了促进2015年及以后妇女和儿童健康改善方面的全球知识。
Резюме
Снижение материнской и детской смертности является одним из приоритетов Целей тысячелетия в области развития (ЦТР) и останется таковым и после 2015 года. Практика показывает, что для реализации этих целей требуется дальнейшее вложение инвестиций, проведение мероприятий и стимулирующей политики. До конца непонятно, почему некоторые страны достигают прогресса в решении проблем быстрее, чем другие сопоставимые страны. Были проведены исследования «Факторы успеха для здоровья женщин и детей» для восполнения этого пробела в знаниях, используя следующие методы: статистический и эконометрический анализ данных для 144 стран с низким и средним уровнем доходов (СНСД) за 20-летний период, логический, качественный и сравнительный анализы, обзор литературы, обзоры 10 опережающих стран по показателям ЦТР 4 и 5а. Для решения этих проблем нет стандартной формулы — страны с опережающими показателями применяют целевые стратегии и быстро адаптируются к изменениям. Тем не менее, опережающие страны делятся некоторыми эффективными подходами в трех основных областях с целью снижения материнской и детской смертности. Во-первых, эти страны привлекают несколько секторов для решения проблем, связанных с важнейшими детерминантами здоровья. Успехи, достигнутые в снижении детской смертности в СНСД с 1990 года, примерно наполовину являются результатом инвестиций в сектор здравоохранения, а другая половина связана с инвестициями в другие сектора помимо здравоохранения. Во-вторых, эти страны используют стратегии для мобилизации партнеров во всех слоях общества, применяя своевременные, надежные доказательства для принятия решений и подотчетности, а также тройной плановый подход, включающий в себя насущные потребности, долгосрочное видение и адаптацию к изменениям. В-третьих, эти страны разрабатывают руководящие принципы, позволяющие направлять развитие, согласовывать действия заинтересованных сторон и достигать результатов с течением времени. Достигнутые в этих странах успехи способствуют всеобъемлющему изучению способов ускоренного достижения улучшений в сфере охраны здоровья женщин и детей к 2015 году и в последующие годы.
Introduction
Worldwide, accelerated progress is required to achieve Millennium Development Goals (MDGs) 4 (reduce child mortality) and 5 (improve maternal health) as highlighted in the United Nations Secretary-General’s Global Strategy for Women’s and Children’s Health.1 There have been substantial achievements from 1990 (the baseline for the MDGs) to date. Child and maternal deaths decreased globally by around 50%, and contraceptive prevalence increased from 55% to 63%.2–4 There is consensus on evidence-based, cost-effective investments and interventions5,6 and on enabling health and multisectoral policies.7
Despite these advances, every year 6.6 million children die before five years of age (44% as newborns) and 289 000 maternal deaths occur, most from preventable causes.2–4Progress varies widely across countries, even where levels of income are similar.8 There is a need for evidence on why some low- and middle-income countries (LMICs) do better than others in preventing maternal and child deaths and on the strategies they use to accelerate progress.8,9
This knowledge gap prompted discussions at the Partnership for Maternal, Newborn & Child Health Partners’ Forum in 2010, leading to a three-year multidisciplinary, multicountry series of studies on Success Factors for Women’s and Children’s Health (hereafter referred to as the Success Factors studies).10 The Success Factors studies were supported by the Partnership for Maternal, Newborn & Child Health, the World Health Organization (WHO), the World Bank and the Alliance for Health Policy and Systems Research, working closely with ministries of health, academic institutions and other partners.10 The studies sought to understand what works to support countries’ progress towards the MDGs and to inform the post-2015 goals and strategies under preparation.
Methods
Analytical framework
The analytical framework for the Success Factors studies (Box 1) builds on the UN Millennium Project’s “clusters of public investments and policies”11 and WHO’s “health systems building blocks”.12 We used literature reviews and expert consultations to identify over 250 related variables to develop the database for these studies.13
Box 1. Analytical framework for the Success Factors for Women’s and Children’s Health study series.
Independent variables
Health sector: investments in health systems with universal access to services
Service delivery (e.g. skilled birth attendance, contraceptive prevalence rate)
Health workforce (e.g. doctors per 1 000 population)
Information (e.g. health information systems)
Medical products, vaccines and technologies (e.g. measles vaccine coverage)
Financing (e.g. total health expenditure per capita)
Health systems governance (e.g. adoption of enabling policies for women’s and children’s health)
Sectors outside health: investments and policies that are health-enhancing
Promoting vibrant rural and urban communities, including through infrastructure development (e.g. electricity: kilowatt hours/capita)
Ensuring universal enrolment and completion of primary education and expanded access to post-primary and higher education (e.g. girls’ primary school enrolment)
Improving environmental management (e.g. access to clean water)
Building national capacities in science, technology and innovation (e.g. number of scientific publications, Global Innovation Index)
Cross-sectoral factors affecting health
Population dynamics (e.g. total fertility rate, % urban population)
Women’s political and socioeconomic participation (e.g. % female parliamentarians)
Overcoming inequalities and realizing rights (e.g. Gini; ratification of human rights treaties)
Economic development (e.g. GDP per capita)
Good governance across sectors (e.g. World Governance Index, Global Leadership and Organizational Behaviour Effectiveness (GLOBE) scores)
Dependent variables
Main outcome variables – MDGs 4 and 5a
Maternal mortality ratio
Under-five mortality rate
Additional outcome variables
Other health status indicators, including neonatal mortality rate, global burden of communicable and noncommunicable diseases, violence and injuries and nutritional status
Countries included
The statistical and econometric analyses included all 144 countries that the World Bank designated as LMICs in 1990. For the in-depth country reviews, we selected 10 of the 75 “Countdown to 2015” high-mortality burden countries:8 Bangladesh, Cambodia, China, Egypt, Ethiopia, Lao People's Democratic Republic, Nepal, Peru, Rwanda and Viet Nam. We refer to these countries as “fast-track” because they were on track in 2012 to achieve both MDGs 4 and 5 ahead of comparable countries. (Other Countdown countries such as Liberia and the Niger are achieving fast-track progress to reduce child mortality. If we consider all 144 LMICs, rather than only the 75 Countdown countries, additional fast-track countries for reducing both maternal and child mortality include the Maldives and Turkey).
Research methods
The Success Factors studies teams developed five primary technical papers based on: (i) quantitative mapping of trends;14 (ii) econometric modelling;15 (iii) Boolean, Qualitative Comparative Analysis;16 (iv) literature review with narrative evidence synthesis;17 and (v) country-specific literature and data reviews in 10 fast-track countries.18
As a following step, ministries of health will convene multistakeholder policy review meetings in the 10 selected fast-track countries to document milestones on each country’s pathway to improving women’s and children’s health. Each country will subsequently publish a policy report.19
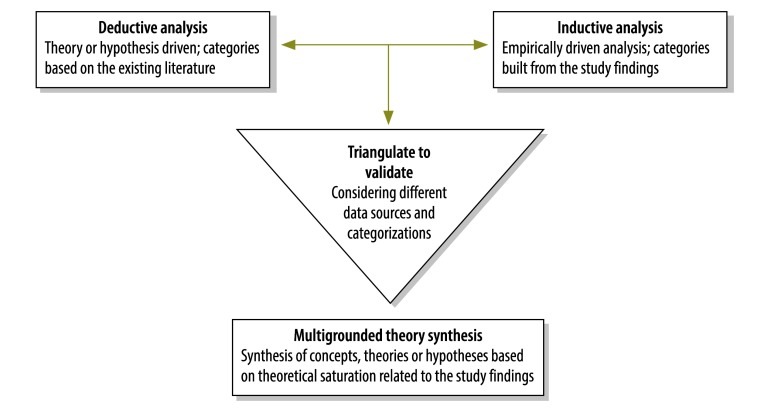
This article is an evidence synthesis across the five primary technical papers.14–18 To synthesize the evidence, we used a multi-grounded theory approach20(Fig. 1). We first categorized the data deductively using the studies’ analytical framework (Box 1). We then refined the thematic categories, inductively and iteratively, using a triangulate to validate approach across the qualitative and quantitative methods. Using a narrative synthesis approach21 we anchored each thematic category to data from the Success Factors studies; for example, with statistical trends, econometric models or country examples. Through regular discussions with the different study teams, we reached a shared understanding and agreement on the emerging narrative synthesis. The narrative synthesis continued until there was thematic saturation;22 that is, when existing thematic categories could accommodate new findings but no new themes were required to categorize the data.
Fig. 1.
Multi-grounded theory approach used to synthesize the studies’ findings
Adapted from Goldkuhl & Cronholm (2010).20
To ensure research quality and robustness of the findings we used a triangulation of methods, with an experienced, multidisciplinary team and a series of internal and external reviews of the study design, ethics and findings.10
Results
A strong pattern of findings emerges across the Success Factors studies.14–18 Those LMICs which are making fast progress deploy strategies tailored to their unique situations and adapt quickly to change. While there is no standard formula, fast-track countries are moving ahead in three main areas to reduce maternal and child mortality: progress across multiple sectors to address crucial health determinants (hereafter multisector progress); strategies that can catalyse accelerated progress and maximize health outcomes (hereafter catalytic strategies); and principles – based on principles of human rights and development effectiveness and political and economic models – that can help shape policies, align action and steer progress (hereafter guiding principles).
Multisector progress
The Success Factors studies find that the key to progress in fast-track countries is improvement across a range of health determinants within and beyond the health sector (Fig. 2, Fig. 3, Fig 4, Fig. 5, Fig. 6, Fig 7 and Fig. 8, Table 1; Fig 5 and Fig. 6 are available from: http://www.who.int/bulletin/volumes/92/7/14-138131). For example, countries that are making accelerated progress towards MDGs 4 and 5a are also making progress on most of the other MDGs, e.g. to decrease poverty and hunger and improve education, gender equality and environmental sustainability (Fig. 7).
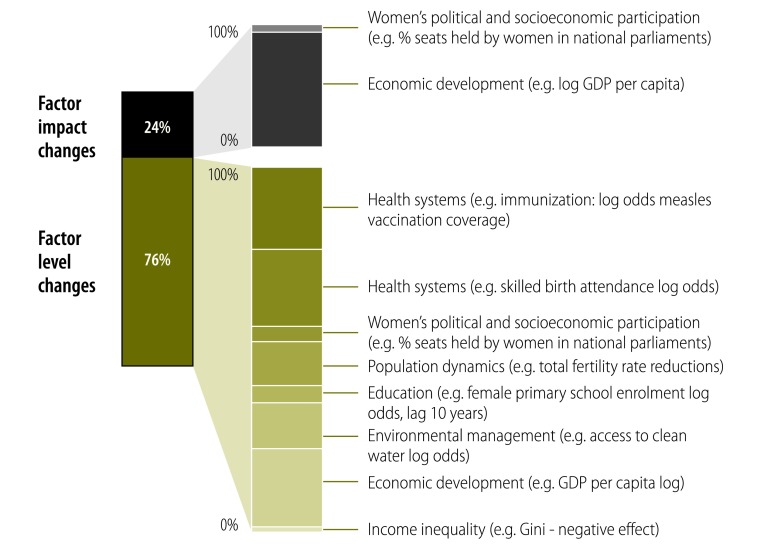
Fig. 2.
Factors involved in declining child mortality in 144 low- and middle-income countries,1990–2010
GDP: gross domestic product.
Note: Factor impact changes refer to the impact of these factors increasing between 1990 and 2010, for example, a given per capita GDP in 2010 was associated with a lower under five years of age mortality rate than the same level of per capita GDP in 1990.15 Factor level changes refer to improvements in the levels or coverage of factors between 1990 and 2010.
Adapted from Bishai et al. (2014).15
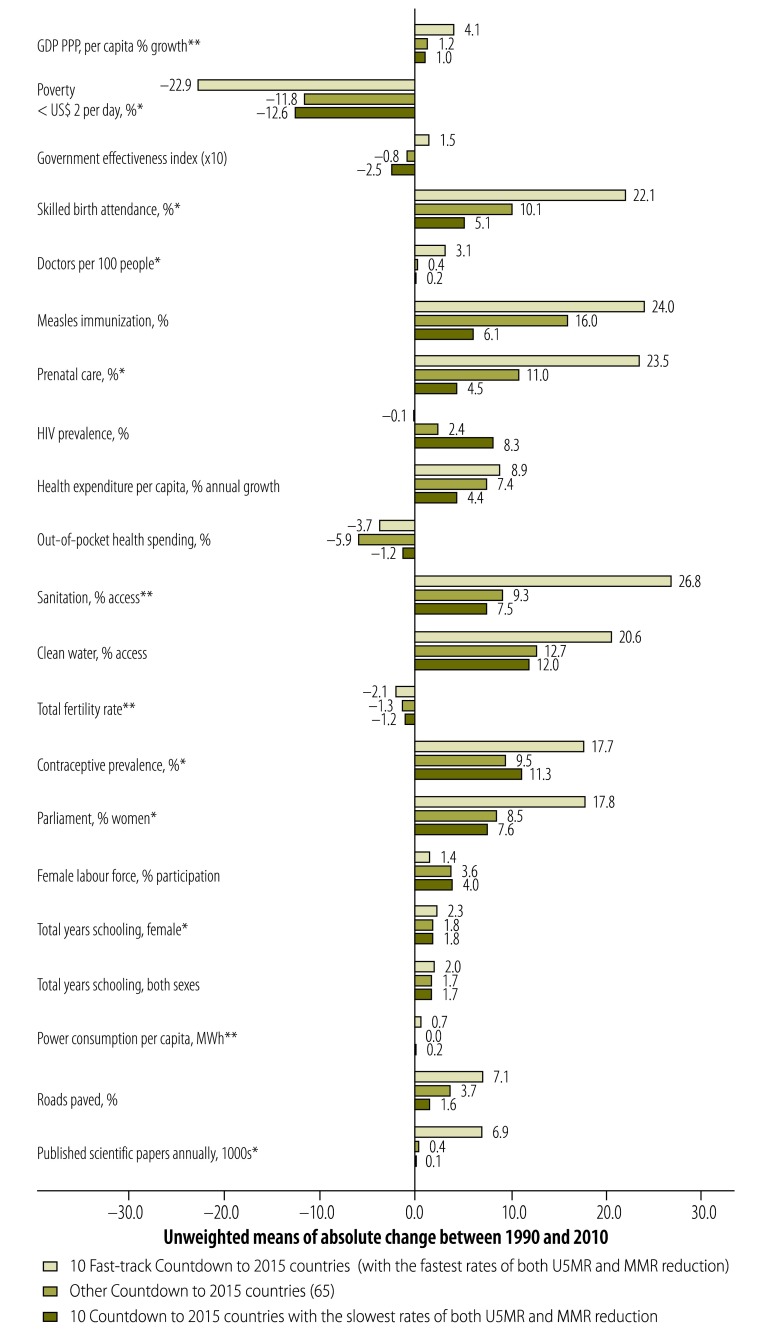
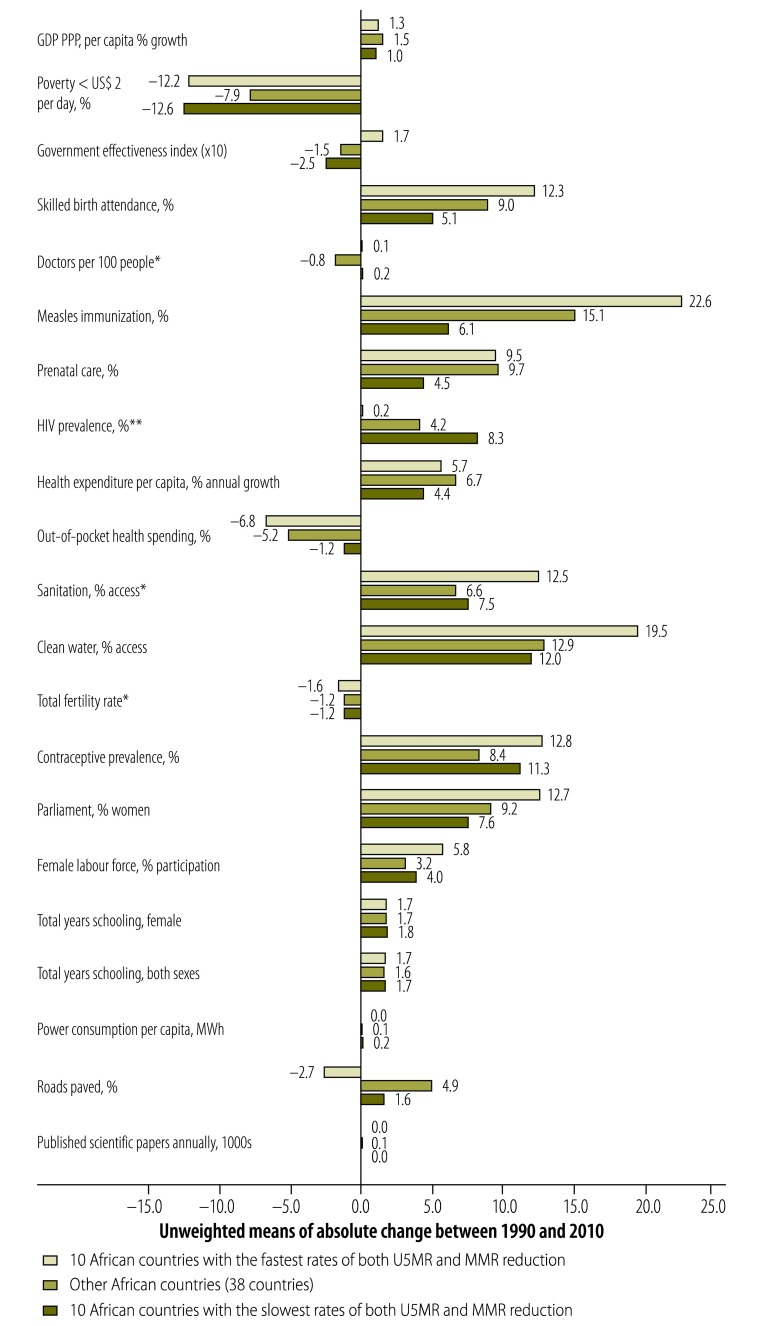
Fig. 3.
Multisector factors in the 75 Countdown to 2015 countries, 1990–2010
* P < 0.05; ** P < 0.01; GDP: gross domestic product; HIV: human immunodeficiency virus; MMR: measles, mumps and rubella; MWh: Mega Watt hour; PPP: purchasing power parity; U5MR: under-five years mortality rate; US$: United States dollars.
Note: P-values estimated using N-way ANOVA comparing fast-track countries with the 65 other countries, (excluding the 10 countries with slower rates of progress), for stronger statistical power. Some values are scaled by factor of 10 to be comparable on a single chart. In 1990, across the countries, levels for most factors were not significantly different, except that fast-track countries had significantly lower prenatal care, power consumption per capita and Gini coefficient.
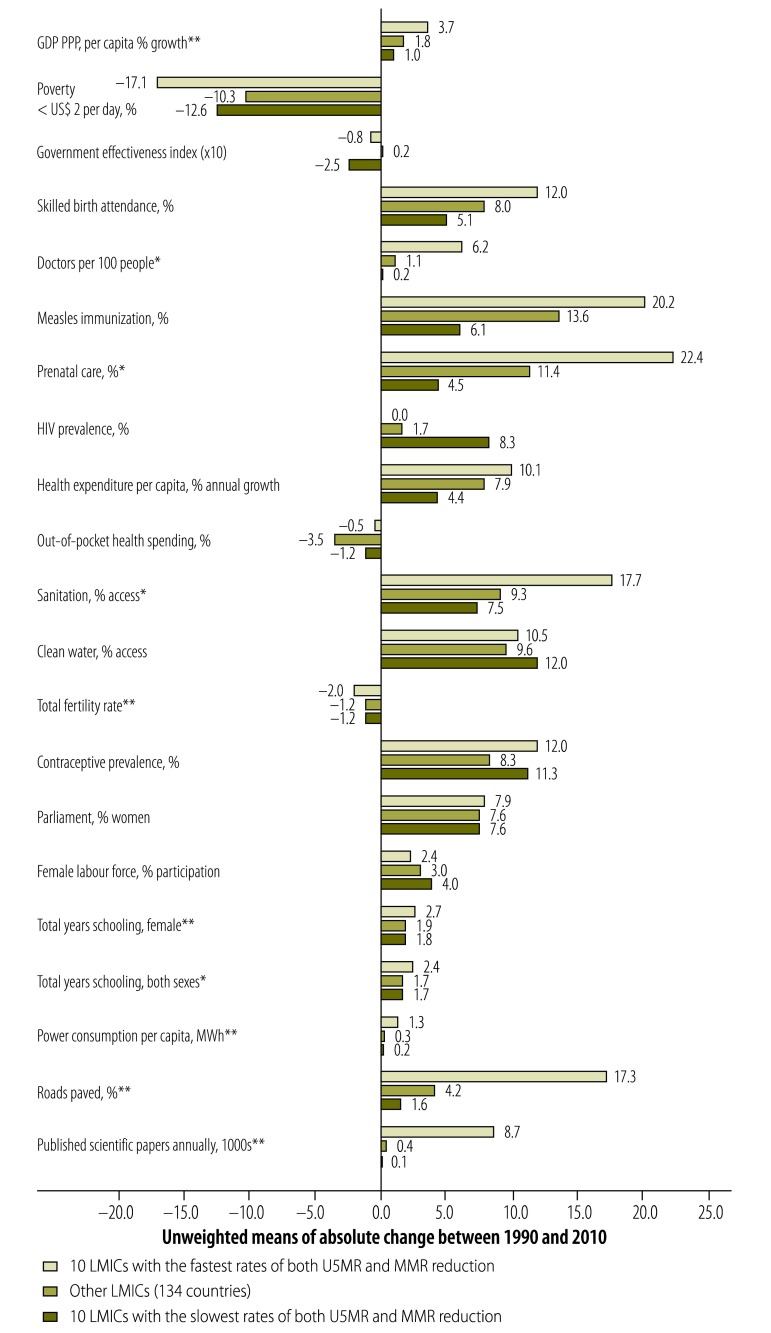
Fig. 4.
Multisector factors in 144 low- and middle-income countries, 1990–2010
* P < 0.05; ** P < 0.01; GDP: gross domestic product; HIV: human immunodeficiency virus; LMIC: low- and middle-income countries; MMR: measles, mumps and rubella; MWh: Mega Watt hour; PPP: purchasing power parity; U5MR: under-five years mortality rate; US$: United States dollars.
Note: P-values estimated using N-way ANOVA. Some values are scaled by factor of 10 to be comparable on a single chart.
Fig. 5.
Multisector factors in African countries with the fastest and slowest rates of maternal and child mortality reduction, 1990–2010
* P < 0.05; ** P < 0.01; GDP: gross domestic product; HIV: human immunodeficiency virus; MMR: measles, mumps and rubella; MWh: Mega Watt hour; PPP: purchasing power parity; U5MR: under-five years mortality rate; US$: United States dollars.
Note: P-values estimated using N-way ANOVA. Some values are scaled by factor of 10 to be comparable on a single chart.
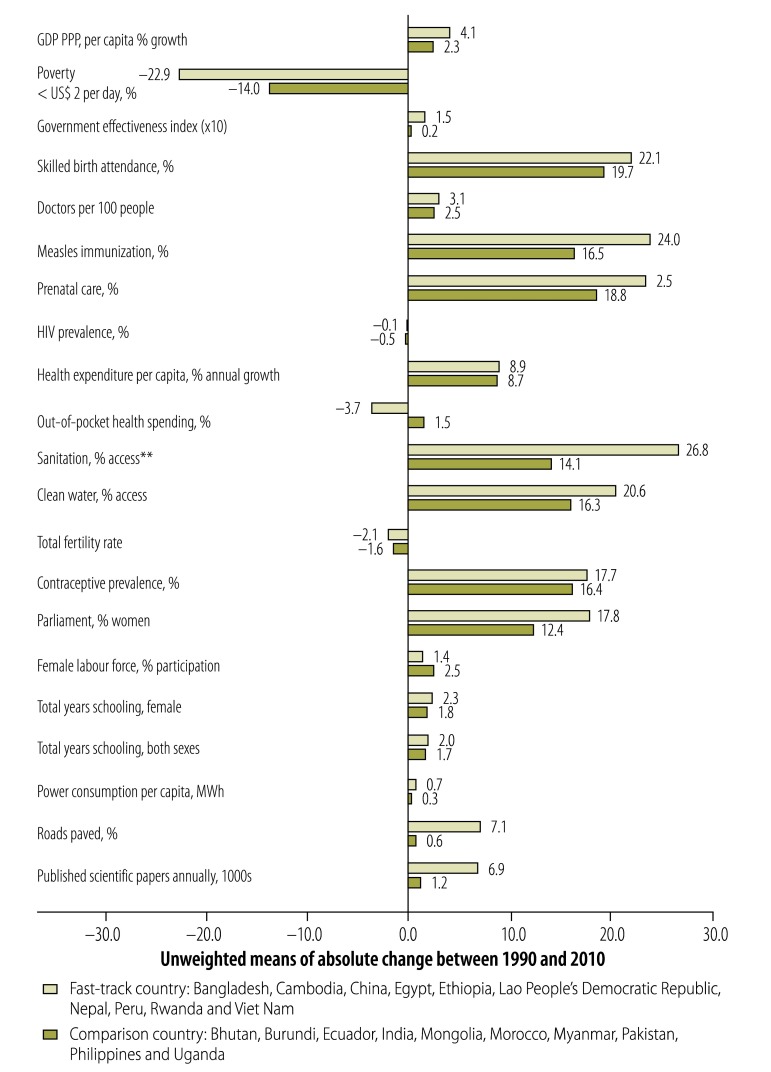
Fig. 6.
Progress across 10 fast-track countries and 10 comparison countries, 1990–2010
* P < 0.01; GDP: gross domestic product; HIV: human immunodeficiency virus; MWh: Mega Watt hour; PPP: purchasing power parity; US$: United States dollars.
Note: P-values estimated using N-way ANOVA. Some values are scaled by factor of 10 to be comparable on a single chart. For each Success Factor fast-track country, one matched control country was identified to form a comparison group. These controls were selected based on similarities in 1990 by geographical region, under-five years mortality rate, U5MR, maternal mortality rate, GDP gross domestic product per capita, and population. These control countries have the added benefit of being in different geographical regions and not being affected by high rates of HIV infections, as were the “slow-track” countries in Fig. 3, Fig. 4 and Fig. 5 that were all African countries.
Fig. 7.
A status assessment of 10 fast-track countries’ progress towards the Millennium Development Goals, early 2014
HIV: human immunodeficiency virus; MDG: Millennium Development Goals; N/A: not applicable; UNDP: United Nations Development Programme.
a MDG 5b: As there are no clear “on track” criteria for Target 5b (Unmet need for family planning, total, percentage), across all the countries we used the criteria established based on Bangladesh country report that marked progress as “on track” if the 2015 projected figure was 8% or less, or the percentage change between base and current year was 35% or higher.
b MDG 8: As there are no clear “on track” criteria for MDG 8, countries are marked as “on track” if 2015 projected figure for the indicator – debt service as percentage of exports and net income – is equal to zero.
c Lao People's Democratic Republic is currently considered “off track” for MDG 4 based on 2012 data; however, it was “on track” for MDG 4 based on 2010 reporting and when the fast-track countries were selected for analysis.
Note: The table provides a snapshot of progress towards each MDG based on one or two key target indicators for each MDG. Developed from UNDP MDG country progress reports and MDG database (available from: http://mdgs.un.org/unsd/mdg/Default.aspx)
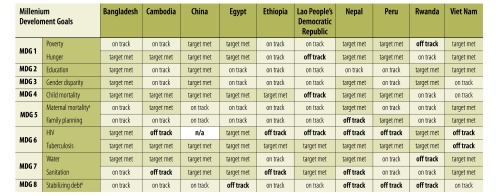
Fig. 8.
Total health expenditure per capita worldwide and in 10 fast-track countries, 2012
Lao PDR, Lao People’s Democratic Republic; US$: United State dollars.
Adapted from World Health Organization (2014) http://gamapserver.who.int/mapLibrary/Files/Maps/PerCapitaUSD_2012.png.
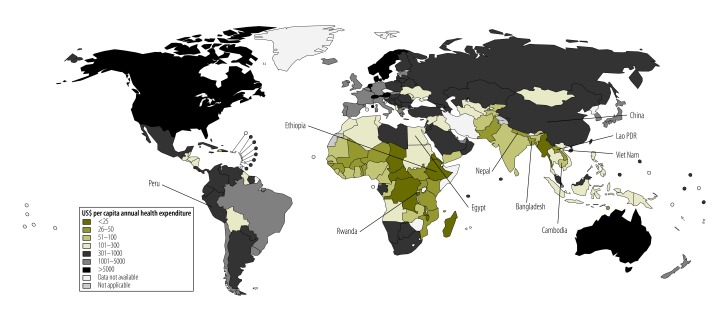
Table 1. Necessary and sufficient conditions for fast-track progress in reducing mortality rates in children under-five years of age in 144 low- and medium-income countries, 1990–2010.
| Factors | Necessity Scoresa | Sufficiency Scoresb |
|---|---|---|
| Ratio of young literate females to males (ages 12–24 years)c | 0.929 | 0.289 |
| Immunization against measles (% children aged 12–13 months vaccinated) | 0.862 | 0.269 |
| Total fertility rate (reduction) | 0.862 | 0.313 |
| Female to male ratio in primary educationc | 0.857 | 0.262 |
| Immunization with DPT (% of children aged 12–13 months vaccinated)c | 0.857 | 0.235 |
| Immunization against measles, lagged (% 12–13 month old children)c | 0.857 | 0.245 |
| Immunization for polio (% of one-year old children receiving three doses)c | 0.857 | 0.212 |
| Access to improved water source (% of population) | 0.828 | 0.273 |
| Birth attendance by skilled health staff (%) | 0.786 | 0.262 |
| Births attended by skilled health staff, lagged (%)c | 0.786 | 0.262 |
| Ethnic fractionalization (negative effect) | 0.786 | 0.282 |
| Expected years of schooling (females)c | 0.786 | 0.314 |
| Expected years of schooling (males)c | 0.786 | 0.289 |
| Pregnant women receiving antenatal care (%)c | 0.786 | 0.212 |
| Total fertility rate (reduction)c | 0.786 | 0.262 |
| Urban population (%) | 0.786 | 0.239 |
| Urban population, lagged (%)c | 0.786 | 0.244 |
| Health expenditure per capita (PPP constant 2005) | 0.714 | 0.333 |
| Immunization with BCG (% of one-year old children)c | 0.714 | 0.189 |
| Improved sanitation facilities (% population with access) | 0.714 | 0.244 |
| Physicians (per 1000 people) | 0.714 | 0.417 |
| Female legislators, senior officials, managers (%) | 0.586 | 0.459 |
| GDP per capita | 0.586 | 0.347 |
| Gini index (negative effect) | 0.483 | 0.259 |
BCG: Bacillus Calmette–Guérin; DPT: diphtheria, pertussis and tetanus; GDP: gross domestic product; PPP: purchasing power parity.
a A necessity score of 1.0 is the highest and 0 the lowest. Several factors have a high necessity score – above 0.75 – indicating that a combination of multisector factors is required for fast track progress. A high necessity score indicates that improving this variable is necessary for fast-track progress. It does not indicate the coverage level – or cut-off point – required for fast-track progress as this varied by country.
b A sufficiency score of 1.0 is the highest and any factor with this score would effectively guarantee fast-track progress. No single factor was sufficient to ensure fast track progress, again indicating that a combination of factors is required.
c With lagged effect of 10 years.
Adapted from: Caramani D, et al. (2014).16
Economic growth underpins multisector progress, but it alone is not sufficient. The Success Factors econometric analysis by Bishai et al. indicates that gross domestic product (GDP) per capita accounted on average for only 12% of the reduction in child mortality in LMICs between 1990 and 2010.15 Further, the relationship between economic growth and health outcomes varies across countries. Many LMICs (e.g. India, Nigeria) experienced fast economic growth, but did not make commensurate progress on maternal and child health. Others (e.g. Bangladesh, China and Rwanda) made good progress while following diverse economic strategies.
Health-sector investments accounted for around half the mortality reduction in children under five years between 1990 and 2010 (Fig. 2). High-impact interventions and systems strengthening were important; e.g. for immunization and other child health interventions, skilled birth attendance and maternal and newborn care, and family planning.15 The remaining gains resulted from health-enhancing investments in other sectors; e.g. from improved levels of education, women’s political and socioeconomic participation and environmental management (e.g. for access to clean water), and reduced levels of fertility and poverty. Income inequalities within countries had a negative impact on child mortality (Fig. 2). The proportions of factors varied by country, and with the statistical models used, but the core set of multisector factors contributing to accelerated progress was the same.15
The Boolean analysis highlighted a similar core set of multisector factors that display high levels of necessity, meaning that countries cannot make fast-track progress without addressing a range of factors within and beyond the health sector (Table 1).16 The Boolean analysis findings also indicate that no single factor approaches a sufficiency score of 1.0, which on its own would effectively guarantee fast-track progress, again emphasizing the importance of progress across sectors.
The Boolean analysis further explored whether there were specific configurations of factors associated with countries making fast-track progress. No single configuration of factors proved necessary or sufficient.16 Instead, results point to a diversity of configurations in different countries associated with fast-track progress. There were also no simple cut-off points, or levels of coverage, associated with fast-track progress, as these varied depending on country contexts, starting levels in 1990 and combined progress across a core set of multisector factors.16
The Boolean analyses indicated that there were similar results for fast track progress on maternal mortality reduction. However, both the Boolean and econometric analyses were limited by the fact that the global maternal mortality estimates, e.g. from the Maternal Mortality Estimation Inter-agency Group,4 are based on a regression model that includes many of the key factors of interest (e.g. GDP per capita, total fertility rate, and skilled birth attendance).
Two factors identified as key enablers across the quantitative and qualitative findings in the Success Factors studies are good governance and women’s political and socioeconomic participation.
Good governance
Good governance, and particularly control of corruption, as measured by the World Bank’s Worldwide Governance Indicators,23 is associated with country progress (Fig. 3). Ensuring value for money is also a key feature of enabling governance, as most fast-track countries improved health outcomes despite relatively low levels of investment (Fig. 8) resulting in part from low GDP per capita and significant political and economic problems.
The Success Factors literature review found decentralized governance to be an enabling factor for accelerated progress.16,17 However, the reach, influence and even definition of decentralized governance varies considerably between countries. Rwanda has a highly centralized policy-making approach supported by district-level planning and implementation.24 In other countries, such as Nepal, geography and politics necessitated a much more regionalized approach. Caution is therefore needed when interpreting decentralized governance as a success factor.
Women’s participation in politics and workforce
The Success Factors studies confirm established evidence on the links between better education and improved maternal and child health (Fig. 3 and Fig. 4).14–18 The Success Factors studies further highlight the importance of women’s political and socioeconomic participation. Fast-track countries have significantly more women parliamentarians (Fig. 3 and Fig. 4). In Rwanda, 64% of parliamentarians are women.19,23 In Lao People's Democratic Republic, the proportion of women members in the national legislature tripled between 1990 and 2003, with the government explicitly recognizing the importance of gender parity and rights for women, including through the Law on the Development and Protection of Women (2004).18,25
Fast-track countries also had a higher average female labour-force participation rate than other “Countdown” countries in 1990 (64% to 54%) and this rate still remained higher in 2010 (Fig. 3). Many fast-track countries (e.g. Bangladesh, Cambodia, China and Viet Nam) developed industries that employ large numbers of women.18 The increased wages these workers earn are potentially available for expenditure on their own health, as well as that of their children and families, and further work is needed to understand these links.
Catalytic strategies
While fast-track countries deployed unique context-specific strategies, the Success Factors studies identified some shared catalytic strategies that these countries used to optimize the use of resources, accelerate progress and maximize health outcomes.
Leadership and partnerships
In the fast-track countries, actors across society played leadership roles in improving women’s and children’s health, sometimes compensating for limited government resources.
In Bangladesh, the government partners with nongovernmental organizations, communities and the private sector in the provision of health services. In 2010, over half of the births in health facilities occurred in the private sector.26 Nongovernmental organizations such as BRAC and the Grameen Foundation cross-subsidize health services with revenues from their commercial activities. Telemedicine and mobile phones also help increase access to health services, particularly for underserved populations.27
Partnerships between communities and service providers in the “Casa Materna” scheme in Peru enable pregnant women in remote rural areas to await delivery in dedicated maternity centres. Transportation to hospitals is available if they need specialist care. These centres also offer culturally sensitive birthing options to promote utilization. Between 2005 and 2010, this scheme contributed to the halving of maternal mortality in the Ayacucho district.28
In Cambodia, multistakeholder partnerships promoted maternal and child health through behaviour-change communication campaigns. In 2004, the BBC World Service Trust launched a mass-media campaign using television series and radio broadcasts to promote maternal and child health themes such as exclusive breastfeeding.29 Knowledge and practice improved and national exclusive breastfeeding rates increased from 11% in 2000 to 60% in 2005 and to 74% in 2010.29
In Ethiopia, the National Nutrition Programme uses multisector partnerships to tackle undernutrition and includes social protection, food security, community nutrition programmes, micronutrient supplementation, treatment of severe acute malnutrition and a package of free health services. The country is now on track to achieve MDG 1c to reduce hunger. Child stunting rates dropped from 57% in 2000 to 44% in 2010.18,30
Decision-making and accountability
Despite limited resources, fast-track countries have developed capacities to collect, analyse and use robust evidence to inform policy, investment, implementation and accountability.
The Success Factors literature review highlights the value of evidence-based tools and health information systems.17 Save the Children’s “Saving Newborn Lives” programme demonstrated the value of decision-support tools, such as the Lives Saved Tool, now included in the United Nations One Health Tool, to support national planning.31
In Ethiopia, scorecards are used at all levels of the health system – community, regional, and national – to monitor progress on women’s and children’s health. The government views scorecards as a powerful tool to track progress and identify inequities in health services delivery.32
In China, the National Maternal and Child Health Routine Reporting System covers the whole population.33 A national system of contracts and agreements for health providers and administrators, monitors quality and service delivery at all levels.18,19
In Egypt, quality-of-care indicators (e.g. on patient satisfaction) were added to performance-based financing programmes, resulting in increased use and better quality of family planning services.34
Testing innovative, evidence-based approaches to address context-specific needs has also been critical to progress. Nepal, for example, has emphasized testing and scaling up community-based approaches.35
Approach to sustain progress
Fast-track countries achieve rapid progress by adopting a triple planning approach that focuses on: (i) quick wins with targeted or emergency strategies to address immediate, urgent needs; (ii) longer-term gains from building strong, sustainable systems to achieve a long-term vision; and (iii) adaptation to address change and sustain progress.
After the genocide, in 1994, Rwanda deployed community health workers and volunteers for urgent health needs. At the same time the country promoted investments in a long-term vision to build its professional health workforce and health facilities with medical colleges, referral hospitals and international academic and professional collaborations.36,37
Progress is not always unidirectional and countries need to adapt their strategies to sustain it. The Success Factors literature review identifies cases where progress has plateaued or reversed.17 For example, in Namibia, an upper-middle-income country, the maternal mortality ratio increased from to 271 to 449 per 100 000 live births between 1991 and 2007. Zere et al.38 discuss how this increase was due to unequal access to quality emergency obstetric care between the rural poor and the urban wealthy. In Brazil and Peru, concerted efforts to address similar sub-national inequalities have brought about progress.18,39
The Success Factors literature review discusses how countries also adapt strategies based on changing needs and available resources, Malaysia, Sri Lanka and Thailand initially focused on improving primary and community-based health care in rural areas. As their health systems became stronger, the emphasis shifted to quality improvements and then to macro-level health reforms for universal health coverage that all contributed to improved maternal and child health outcomes.17,40,41 The progress that accrues over time from strengthening systems and adaptive strategies should not be undervalued by measuring a country’s progress only by the initial rates of decline in mortality.14,17
Different ways of measuring a country's rates of mortality reduction result in different pictures of progress, for example, sub-Saharan African countries reduced deaths of children under five years of age on average by 60/1000 live births between 1990 and 2012 —making it second only to South Asia (74/1000) in terms of absolute decline in mortality. However, when reported as the annual rate of change, it appears that the least progress has been achieved in this region (for example, the Latin American/Caribbean region reduced under-five mortality by 5%, south Asia by 3.7%, and sub-Saharan Africa by just 2%). By looking at absolute decline in mortality, we get a better idea of overall reduction in numbers of deaths over time.14
Guiding principles
Fast-track countries use guiding principles to chart their own pathways to progress. These principles are not a panacea, but they nevertheless shape government strategies, align stakeholder action and orient progress towards agreed results. The principles are continually being defined, tested and reformed.
Some fast-track countries explicitly adopted human rights-based principles to guide their health and development strategies. For example, Nepal’s interim constitution is founded on human rights. The Secretary of the Ministry of Health and Population affirmed that: “Many government strategies and policies related to safer motherhood, neonatal health, nutrition and gender are anchored in the principles of human rights.”18,42
Other fast-track countries used guiding principles aligned with frameworks for effective development, for example the Paris Principles and Accra Agenda for Action.43 In these countries, the government’s interaction with health and development partners is defined by principles of national ownership of policies and programmes, and alignment of partners with country priorities.
Principles based on different political systems and models of economic and social development also steer progress. China has experienced a clear evolution of different political philosophies and systems.18,19 Currently it aims to address the challenge of achieving harmonization and balance across five axes of national development: rural–urban, western–eastern regions of the country, national–international, economic–social, and human development–natural development.18,19
Discussion
The Success Factors studies used a multidisciplinary approach to explore why some countries do better than others at preventing maternal and child mortality. The studies indicate that while fast-track countries did not have a simple formula for success, progress across a core set of multisector factors is essential. Fast-track countries maximize health outcomes using catalytic strategies, including through leadership and partnerships across society, and evidence-informed, innovative, context-specific approaches. They also define and test guiding principles to shape policies, align action and achieve results.
The 10 fast-track countries improved health outcomes despite relatively low health expenditures and GDP per capita, and in the face of considerable political and socioeconomic challenges.18,19 These findings are consistent with the “Good Health at Low Cost” studies that show that health can be achieved with relatively few resources if these are used strategically.44 Aligned with the Global Investment Framework for Women’s and Children’s Health,5 the Success Factors analysis shows that investments in packages of high-impact interventions and health systems contribute to better progress: for example, in immunization and other child health interventions, skilled birth attendance and maternal and newborn health care, and family planning.
The Success Factors studies note the importance of robust and timely evidence to support decision-making and promote accountability in fast-track countries. This aligns with a previous World Bank analysis emphasizing that knowledge is at least as important as economic capital in improving well-being.45
The Success Factors studies findings support previous analyses showing that building on the complementary objectives and principles for development effectiveness and human rights is potentially beneficial for women’s and children’s health.43,46,47 There is a recognized need to continually research the definition, implementation and impact of these principles on women’s and children’s health and for inclusive, sustainable development overall.19 These findings are aligned with ongoing research on the impact of different political and institutional models to explain why nations fail.48 Political and policy analyses, and related implementation and impact assessments, are important areas for further research investment, including to understand how nations succeed.
Study approach and limitations
The Success Factors studies used different methods which highlighted some challenges. Key strategies identified in the qualitative country review data were difficult to measure quantitatively. For example, there are limited measures of enabling factors such as value for money and the adaptive capacities of different countries. For other factors such as leadership, indicators and data exist, but only for a limited set of countries and years.49
The Success Factors studies did not include as factors other health-related outcomes such as the prevalence of human immunodeficiency virus (HIV) or nutritional status of the population and thus did not ascertain the effect of these variables. Further, women’s and children’s health extends well beyond mortality reduction to addressing risk factors and promoting well-being throughout the life course. While recognizing this broader context, reducing preventable maternal and child mortality was the focus of the Success Factors studies.
The quantitative analyses compared progress between fast-track LMICs and other LMICs (Fig. 3, Fig. 4, Fig. 5, Fig. 6 and Table 1). The in-depth country-specific reviews were limited by their focus on 10 fast-track countries, without a counterfactual or comparative analysis. Examining cases with unexpectedly poor performance would be helpful for future research and planning.
Policy and research implications
Multisector progress is key to accelerating positive results. Having shared goals and investments across sectors could further strengthen these results, for example ensuring clean water and sustainable energy for health-care facilities, reducing air pollution, and promoting health and nutrition in schools. However, institutional barriers to meaningful multisector collaboration are formidable. Further analysis is needed to identify how fast-track countries overcame these barriers.
In progressing towards MDGs 4 and 5, fast-track countries took into account the global development agenda and goals, but emphasized context-specific needs, priorities and capacities. This suggests that global goals could be usefully augmented and operationalized by taking into account country-specific targets.50
The country multistakeholder policy reviews19 indicate that there is considerable interest in understanding and documenting what works to support national planning, promote policy dialogue across different stakeholders and sectors, and facilitate learning across countries. Policy analysis, within and beyond the health sector, is an important area for further research, technical assistance and policy collaboration.
Policy-makers in the fast-track countries may build on lessons learnt to address ongoing and new challenges. There is the unfinished MDG agenda around mortality reduction, particularly newborn mortality and preventing stillbirths. In addition, high-, middle- and low-income countries all face challenges in promoting the well-being of their populations across the life course, addressing inequalities, managing climate change and population dynamics, and balancing economic, social and sustainable development.
Conclusion
The Success Factors studies confirm, as posited by the UN Millennium Project,20 that investments across multiple sectors are required for countries to accelerate progress towards health and development goals. Importantly, this integrative, cross-sectoral approach is being emphasized in the design of the post-2015 sustainable development goals.51 Other enabling factors include good governance, evidence-informed, context-specific strategies, and guiding principles to orient progress. This evidence synthesis contributes to a growing field of knowledge on how to accelerate progress for women’s and children’s health towards 2015 and beyond.
Acknowledgements
We gratefully acknowledge the contributions of all colleagues on the Success Factors Study Groups and Country Multistakeholder Policy Review Groups. The full list of contributors, technical papers and country policy reports can be accessed at: http://www.who.int/pmnch/knowledge/publications/successfactors
Funding:
Partnership for Maternal, Newborn & Child Health, World Bank, World Health Organization and Alliance for Health Policy and Systems Research.
Competing interests:
None declared.
References
- 1.United Nations Secretary-General. Global strategy for women's and children's health. New York (NY): United Nations; 2010. Available from: http://www.everywomaneverychild.org/images/content/files/global_strategy/full/20100914_gswch_en.pdf [cited 2014 May 12].
- 2.UN Inter-agency Group for Child Mortality Estimation. Levels and trends in child mortality. New York (NY): United Nations Children’s Fund; 2013. Available from: http://www.childinfo.org/files/Child_Mortality_Report_2013.pdf [cited 2014 May 20].
- 3.Say L, Chou D, Gemmill A, Tunçalp Ö, Moller A-B, Daniels J, et al. Global causes of maternal death: a WHO systematic analysis. Lancet Global Health. 2014;2(6):e323–33 10.1016/S2214-109X(14)70227-X [DOI] [PubMed] [Google Scholar]
- 4.Trends in maternal mortality: 1990 to 2013. Estimates by WHO, UNICEF, UNFPA, The World Bank and the United Nations Population Division. Geneva: World Health Organization; 2014. Available from: http://apps.who.int/iris/bitstream/10665/112682/2/9789241507226_eng.pdf?ua=1 [cited 2014 June 12]. [Google Scholar]
- 5.Stenberg K, Axelson H, Sheehan P, Anderson I, Gülmezoglu AM, Temmerman M, et al. ; Study Group for the Global Investment Framework for Women’s and Children’s Health. Advancing social and economic development by investing in women’s and children’s health: a new Global Investment Framework. Lancet. 2014;383(9925):1333–54 10.1016/S0140-6736(13)62231-X [DOI] [PubMed] [Google Scholar]
- 6.World Health Organization, Aga Khan University, Partnership for Maternal, Newborn & Child Health and partners. Essential interventions, commodities and guidelines for reproductive, maternal, newborn and child health. Geneva: World Health Organization; 2011. [Google Scholar]
- 7.World Health Organization, Partnership for Maternal, Newborn & Child health and partners . A policy guide for implementing essential interventions for reproductive, maternal, newborn and child health (RMNCH): a multisectoral policy compendium for RMNCH. Geneva: World Health Organization; 2014 [Google Scholar]
- 8.Countdown to 2015. Countdown to 2015 and beyond: fulfilling the health agenda for women and children. Geneva: World Health Organization & United Nations Children’s Fund; 2014. Forthcoming. [Google Scholar]
- 9.MacFarquhar N. UN poverty goals face accountability questions. The New York Times. 2010 Sep 18.
- 10.Success Factors for Women's and Children's Health [Internet]. Geneva: World Health Organization; 2014. Available from: http://www.who.int/pmnch/knowledge/publications/successfactors/en/ [cited 2014 May 12].
- 11.United Nations Millennium Project. Investing in development: a practical plan to achieve the Millennium Development Goals. New York (NY): United Nations Development Programme; 2005 [Google Scholar]
- 12.Everybody’s business: strengthening health systems to improve health outcomes. WHO’s framework for action. Geneva: World Health Organization; 2007. [Google Scholar]
- 13.Variables included in the Success Factors for Women's and Children's Health study database [Partnership for Maternal, Newborn & Child Health and partners Technical Paper]. Geneva: World Health Organization; 2014. Available from: http://www.who.int/pmnch/knowledge/publications/annex1.pdf?ua=1 [cited 2014 May 12].
- 14.Adam T, Franz-Vasdeki J. A quantitative mapping of trends in reductions of maternal and child mortality in the high mortality-burden Countdown to 2015 countries [Partnership for Maternal, Newborn & Child Health and partners Technical Paper]. Geneva: World Health Organization; 2012 [Google Scholar]
- 15.Bishai D, Cohen RL, Alfonso YN, Adam T, Kuruvilla S, Schweitzer J. Factors contributing to child mortality reductions in 142 low-and middle-income countries between 1990 and 2010. In: Population Association of America, 2014 Annual Meeting; 2014 May 1; Boston, United States of America. Silver Spring (MD): Population Association of America: 2014. [Google Scholar]
- 16.Caramani D, Eugster B. Which factors are necessary and/or sufficient for accelerated reduction of maternal and child mortality in low and middle-income countries? Results from a Boolean, Qualitative Comparative Analysis (QCA). [Partnership for Maternal, Newborn & Child Health and partners Technical Paper]. Geneva: World Health Organization; 2014. [Google Scholar]
- 17.Frost L, Pratt BA. Review of the literature on factors contributing to the reductions of maternal and child mortality in low income and middle income countries: an evidence synthesis for the success factors study [Partnership for Maternal, Newborn & Child Health and partners Technical Paper]. Geneva: World Health Organization; 2014. Available from: http://www.who.int/pmnch/knowledge/publications/qualitative_evidence_synthesis.pdf?ua=1 [cited 2014 May 12].
- 18.Options Consultancy Services/ Evidence for Action (E4A), Cambridge Economic Policy Associates (CEPA), The Partnership for Maternal Newborn & Child Health. Country-specific literature and data review for 10 fast track countries making progress towards MDGs 4 and 5 [Partnership for Maternal, Newborn & Child Health and partners Technical Paper]. Geneva: World Health Organization; 2014. Available from: http://www.who.int/pmnch/knowledge/publications/country_data_review.pdf?ua=1 [cited 2014 May 12].
- 19.Success Factors for Women's and Children's Health: country multistakeholder policy reviews [Internet]. Geneva: World Health Organization; 2014. Available from: http://www.who.int/pmnch/knowledge/publications/successfactors/en/index2.htmlhttp://[cited 2014 May 12].
- 20.Goldkuhl G, Cronholm S. Adding theoretical grounding to grounded theory: toward multi-grounded theory. Int J Qual Methods. 2010;9(2):187–205 [Google Scholar]
- 21.Mays N, Pope C, Popay J. Systematically reviewing qualitative and quantitative evidence to inform management and policy-making in the health field. J Health Serv Res Policy. 2005;10Suppl 1:6–20 10.1258/1355819054308576 [DOI] [PubMed] [Google Scholar]
- 22.Glaser BG, Strauss AL. The discovery of grounded theory. Chicago (IL): Aldine; 1967 [Google Scholar]
- 23.The Worldwide Governance Indicators (WGI) project [Internet]. Washington (DC): World Bank; 2014. Available from: http://info.worldbank.org/governance/wgi/index.aspx [cited 2014 May 12].
- 24.Shaping our development: economic development and poverty reduction strategy 2013–2018. Kigali: Republic of Rwanda; 2013. Available from: http://www.minecofin.gov.rw/fileadmin/General/EDPRS_2/EDPRS_2_FINAL1.pdfhttp://[cited 2014 May 12].
- 25.Lao People’s Democratic Republic fact sheet. New York (NY): UN Women; 2013. Available from: http://www.unwomen-eseasia.org/docs/factsheets/04 Lao PDR factsheet.pdf [cited 2014 May 12].
- 26.Bangladesh Demographic and Health Survey 2011. Dhaka and Calverton (MD): National Institute of Population Research and Training, Mitra and Associates, ICF International; 2013. [Google Scholar]
- 27.El Arifeen S, Christou A, Reichenbach L, Osman FA, Azad K, Islam KS, et al. Community-based approaches and partnerships: innovations in health-service delivery in Bangladesh. Lancet. 2013;382(9909):2012–26 10.1016/S0140-6736(13)62149-2 [DOI] [PubMed] [Google Scholar]
- 28.Suarez R. In Peru, life for the life-givers. PBS Newshour. 2010 Mar 29. Available from: http://www.pbs.org/newshour/rundown/in-peru-life-for-the-life-givers/ [cited 2014 May 12].
- 29.Koam T. Changing Cambodia one message at a time. The Phnom Penh Post. 2010 Aug 25. Available from: http://www.phnompenhpost.com/lift/changing-cambodia-one-message-time [cited 2014 May 23]. [Google Scholar]
- 30.Ethiopia community-based nutrition program helps reduce child malnutrition [Internet]. Washington (DC): World Bank; 2012. Available from: http://www.worldbank.org/en/news/feature/2012/10/16/ethiopia-community-based-nutrition-program-helps-reduce-child-malnutrition [cited 2014 May 12].
- 31.Lawn JE, Kinney MV, Black RE, Pitt C, Cousens S, Kerber K, et al. Newborn survival: a multi-country analysis of a decade of change. Health Policy Plan. 2012;27Suppl 3:iii6–28 10.1093/heapol/czs053 [DOI] [PubMed] [Google Scholar]
- 32.Tackling Ethiopia's maternal deaths [Internet]. Nairobi: IRIN; 2013. Available from: http://www.irinnews.org/report/97383/analysis-tackling-ethiopia-s-maternal-deaths [cited 2014 May 12].
- 33.Yanqiu G, Ronsmans C, Lin A. Time trends and regional differences in maternal mortality in China from 2000 to 2005. Bull World Health Organ. 2009;87(12):913–20 10.2471/BLT.08.060426 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Chowdhury S, Vergeer P, Schmidt H, Barroy H, Bishai D, Halpern S. Economics and ethics of results-based financing for family planning: evidence and policy implications. Washington (DC): World Bank; 2013. [Google Scholar]
- 35.Khanal L, Dawson P, Silwal RC, Sharma J, Kc NP, Upreti SR. Exploration and innovation in addressing maternal, infant and neonatal mortality. J Nepal Health Res Counc. 2012;10(21):88–94 [PubMed] [Google Scholar]
- 36.VanRooyen MJ, Erickson TB, Jones PW, Townes DA, Jurkowski ET, Levy P. Health care in post-war Rwanda: re-establishing a national hospital using a mentor approach. J Health Adm Educ. 1997. Spring;15(2):101–11 [PubMed] [Google Scholar]
- 37.Human resources for health program [Internet]. Kigali: Republic of Rwanda; 2014. Available from: http://hrhconsortium.moh.gov.rw/about-hrh/program-overview [cited 2014 May 12].
- 38.Zere E, Tumusiime P, Walker O, Kirigia J, Mwikisa C, Mbeeli T. Inequities in utilization of maternal health interventions in Namibia: implications for progress towards MDG 5 targets. Int J Equity Health. 2010;9(1):16 10.1186/1475-9276-9-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Victora CG, Aquino EM, do Carmo Leal M, Monteiro CA, Barros FC, Szwarcwald CL. Maternal and child health in Brazil: progress and challenges. Lancet. 2011;377(9780):1863–76 10.1016/S0140-6736(11)60138-4 [DOI] [PubMed] [Google Scholar]
- 40.Pathmanathan I, Liljestrand J. Investing in maternal health: learning from Malaysia and Sri Lanka. Washington (DC): World Bank; 2003. p. 182. [Google Scholar]
- 41.Vapattanawong P, Hogan MC, Hanvoravongchai P, Gakidou E, Vos T, Lopez AD, et al. Reductions in child mortality levels and inequalities in Thailand: analysis of two censuses. Lancet. 2007;369(9564):850–5 10.1016/S0140-6736(07)60413-9 [DOI] [PubMed] [Google Scholar]
- 42.Patel A, Sharma S, Prost A, Sander G, Hunt P, editors. Maternal and child health in Nepal. Geneva: World Health Organization; 2013 [Google Scholar]
- 43.Integrating human rights into development: donor approaches, experiences and challenges. 2nd ed. Washington (DC): World Bank and Organisation for Economic Co-operation and Development; 2013 [Google Scholar]
- 44.Balabanova D, Mills A, Conteh L, Akkazieva B, Banteyerga H, Dash U, et al. Good Health at Low Cost 25 years on: lessons for the future of health systems strengthening. Lancet. 2013;381(9883):2118–33 10.1016/S0140-6736(12)62000-5 [DOI] [PubMed] [Google Scholar]
- 45.World development report 1998–1999. Washington (DC): World Bank; 1999.
- 46.Kuruvilla S, Bustreo F, Hunt P, Singh A, Friedman E, Luchesi T, et al. ; and other members of the Working Group on the MDGs and Human Rights for the UN Secretary-General’s Global Strategy for Women’s and Children’s Health. The Millennium Development Goals and human rights: realizing shared commitments. Hum Rights Q. 2012;34(1):141–77 10.1353/hrq.2012.0010 [DOI] [Google Scholar]
- 47.Bustreo F, Hunt P, Gruskin S, Eide A, McGoey L, Rao S, et al. Women’s and children’s health: evidence of impact of human rights. Geneva: World Health Organization; 2013. [Google Scholar]
- 48.Acemoglu D, Robinson JA. Why nations fail: the origins of power, prosperity and poverty. New York (NY): Crown Publishers; 2012 [Google Scholar]
- 49.House RJ, Hanges PJ, Javidan M, Dorfman PW, Gupta V. Culture, leadership, and organizations: The GLOBE study of 62 societies. Thousand Oakes (CS): SAGE Publications Inc.; 2004. [Google Scholar]
- 50.Cohen R, Alfonso YN, Kuruvilla S, Scweitzer J, Bishai D. Post-2015 health targets: could country-specific targets supplement global ones? Lancet Global Health. Forthcoming. [DOI] [PubMed] [Google Scholar]
- 51.United Nations Sustainable Development Knowledge Platform. Post-2015 process. New York (NY): United Nations; 2014. Available from: http://sustainabledevelopment.un.org/index.php?menu=1561 [cited 2014 May 12].