Abstract
Aims and Objectives:
The aim of the present study was to evaluate the knowledge of dentists regarding human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS).
Materials and Methods:
A structured questionnaire to evaluate the knowledge, fears, and attitudes was self administered to 102 dentists. The data was then evaluated using Chi-square test and a P < 0.05 was considered statistically significant.
Results and Conclusion:
The findings of the present study suggest that dentists in private practice and affiliated with teaching institutions, had better knowledge than their counterparts who were into private practice alone. It was concluded that despite good knowledge many of the dentists expressed some hesitation in treating patients with HIV/AIDS.
Keywords: Cross infection, human immunodeficiency virus, oral health knowledge, oral mucosal lesions
INTRODUCTION
The total number of people living with human immunodeficiency virus (HIV) in India is estimated at 24 lakhs in 2009 and Tamilnadu (1.5 lakhs) is among one of the four high prevalence states in India.[1] Dental therapeutic procedures frequently involve blood and saliva that may contain a variety of blood-borne pathogens and microorganisms, such as HIV. This environment has become a helpful setting for early detection because most lesions of HIV infection present orally during the first stages of the disease. Accordingly, dentists fall into the high-risk category for cross-contamination.[2]
It is generally accepted that both dentists and other healthcare workers should provide quality treatment and care to all individuals indiscriminately. Dentists have a professional and ethical responsibility to provide treatment to patients with HIV and acquired immunodeficiency syndrome (AIDS), particularly since oral lesions, such as hairy leukoplakia, candidiasis, and Kaposi's sarcoma, are commonly found in HIV-infected patients.[3] Willingness to treat patients with HIV/AIDS appears to be related to knowledge of the disease process, recognition of oral manifestations, and understanding of modes of transmission.[2] Thus this study was conducted with the aim of accessing the Dentist's knowledge pertaining to HIV/AIDS.
MATERIALS AND METHODS
A structured questionnaire was prepared with the following aspects: A section for demographic data; a three item section on knowledge about HIV virus with four to five options where only one is correct; a fifteen item section on possible modes of spread of HIV infection in a dental setting and knowledge about oral lesions in HIV infection with three response categories: Agree, disagree, and not sure/do not know; and a four item section dealing with the fears and attitudes of dentists toward HIV patients. (Adapted from Soukaina et al.,[4] Crossley,[5] and Arjuna et al.[6]) Content and context validity was pretested prior to commencement of the study.
A list of practicing dentists in Cuddalore district, Tamilnadu, India was obtained from the state dental council register and the questionnaires were self administered to139 dentists, while replies were obtained from 102 dentists giving a response rate of 73%. Prior consent was obtained from the dentists participating in the study.
The data was then evaluated using Chi-square test and a P < 0.05 was considered statistically significant.
RESULTS
A total of 102 dentists from Cuddalore district responded to the questionnaire. There were 56 male and 46 female dentists in the present study. Among the respondents 43 were exclusively into private practice (p1 group), while the reminder 59 were involved in private practice as well as being affiliated to some dental teaching institution (p2 group).
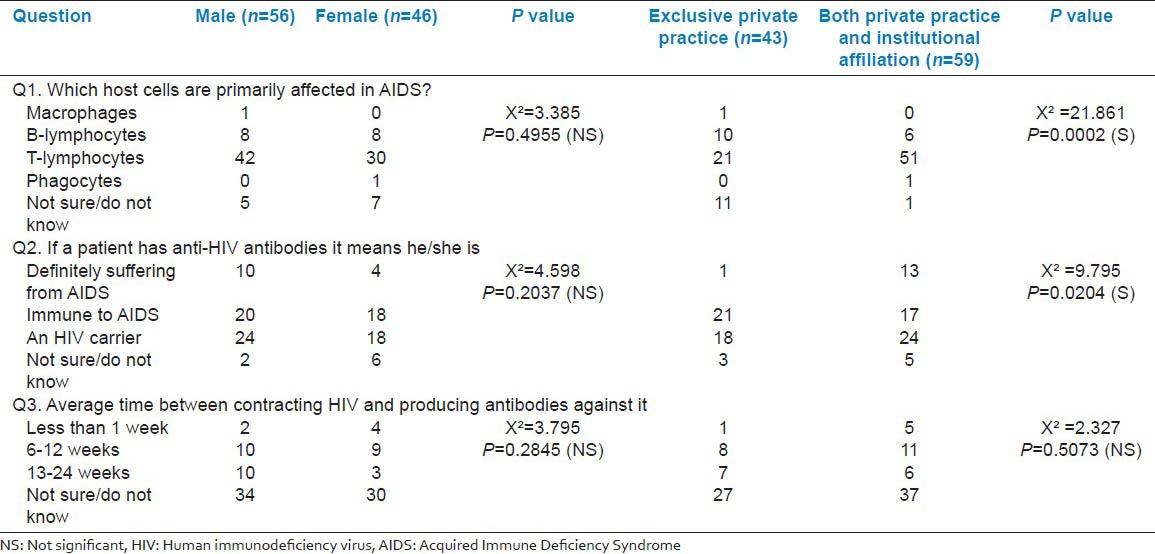
A total of 70.5% of the respondents correctly identified T-lymphocytes as the host cells primarily affected in AIDS. Only 41.2% agreed that if a person had anti-HIV antibodies, they were HIV carriers. The time period of 6-12 weeks being the average time between contracting HIV and producing antibodies against it was identified by only 18.6% of the study sample [Table 1].
Table 1.
Dentists response to questions about knowledge of HIV virus
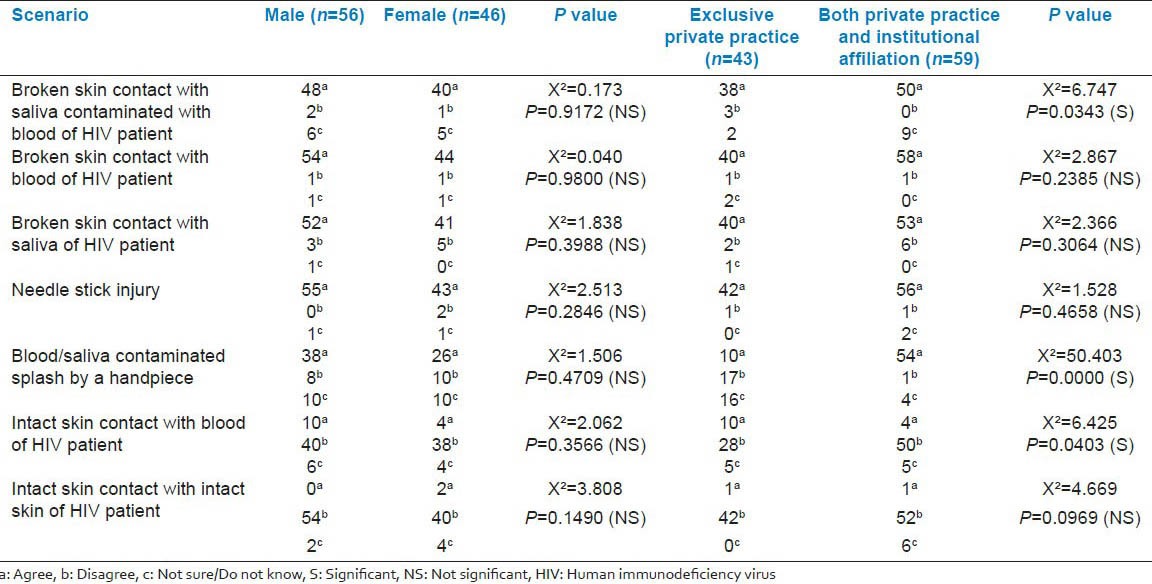
Broken skin contact with saliva contaminated with blood of HIV patient, broken skin contact with blood of HIV patient, broken skin contact with saliva of HIV patient, needle stick injuries, and blood/saliva contaminated splash by a handpiece were correctly identified as possible sources of infection in a dental setting by 86.3%, 96.1%, 91.2%, 96.1%, and 62.7% of the respondents, respectively. A total of 76.5% and 92.2% of the dentists correctly identified that intact skin contact with blood of HIV patient and intact skin contact with intact skin of HIV patient, respectively, were not sources of spread of infection [Table 2].
Table 2.
Dentist's knowledge on possible modes of spread of HIV infection in a dental setting
Oral candidiasis (98%), Kaposis sarcoma (93.1%), hairy leukoplakia (96.1%), and oral lesions of herpetic infections (88.2%) were correctly identified by vast majority of the study population as lesions associated with HIV infection. However, less number of respondents identified melanotic hyper-pigmentation (39.2%) and neurologic disturbances like facial palsy (59.8%) as lesions associated with HIV infection [Table 3].
Table 3.
Dentist's knowledge on oral lesions associated with HIV
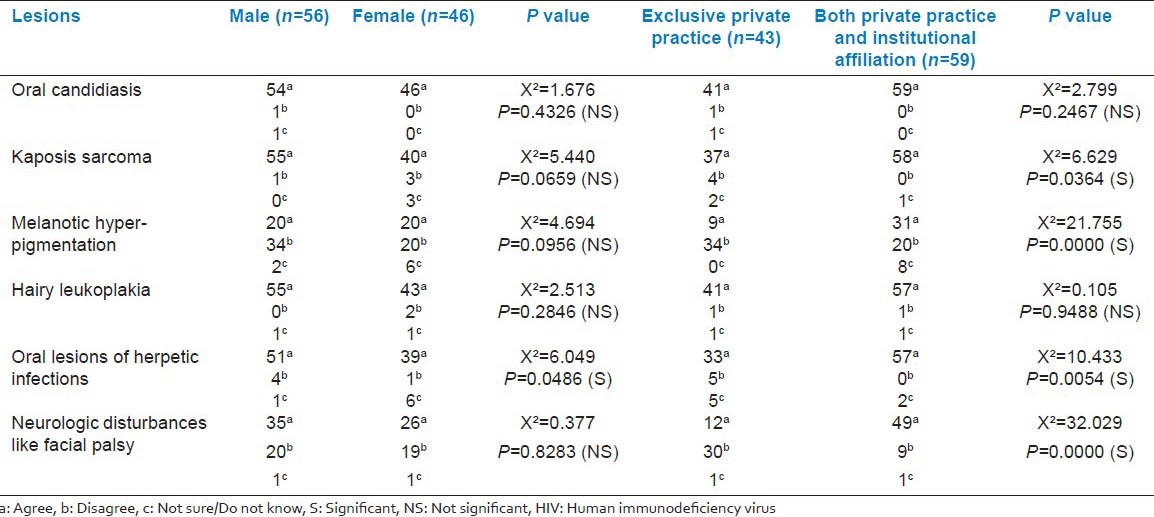
The knowledge of dentists in p2 group was better than those in p1 group and this difference was statistically significant in most of the questions when analyzed by Chi-square test [Tables 1–3]. There was, however, no difference in knowledge between male and female dentists with the exception of identification of oral herpetic lesions as being associated with HIV infection in which males fared better than females and this was also statistically significant (P = 0.0486) [Table 3].
With regard to attitude, 67.4% of the dentists in p1 group would refer HIV patients who sought treatment in their clinic, to be treated elsewhere and in contrast 78% of the dentists belonging to p2 group would treat such patients with some hesitation (P = 0.0000) [Table 4].
Table 4.
Fears and attitudes of dentists towards HIV patient
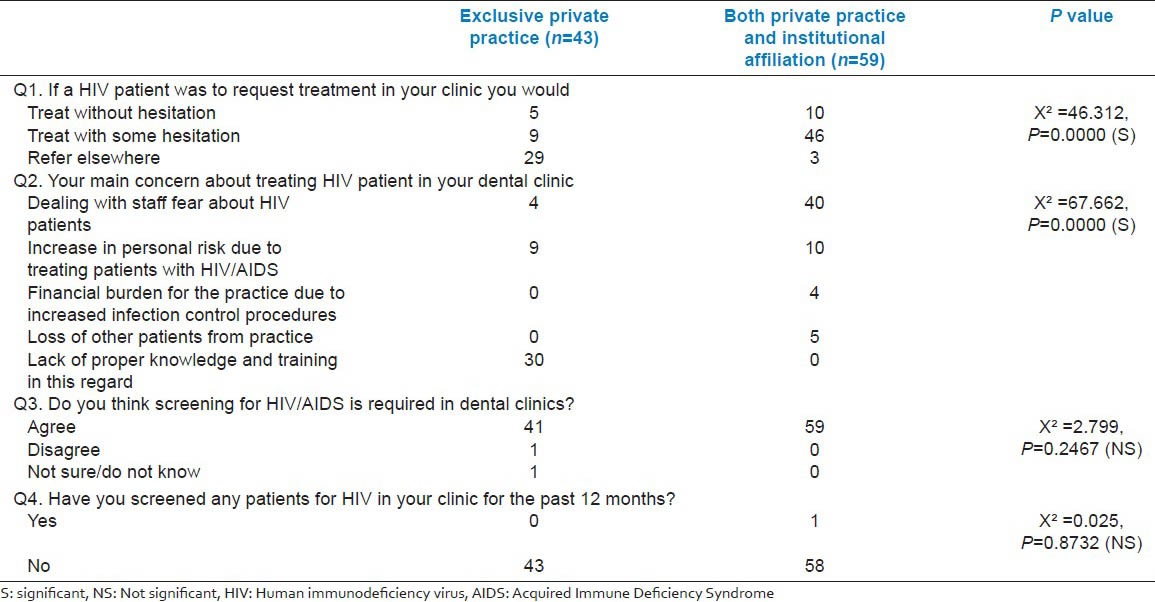
A total of 69.8% of the dentists in the p1 group reported that lack of proper knowledge and training in handling a HIV patient were their main concerns in treating such patients as compared with 67.8% of dentists in group p2 reporting that, dealing with staff fear about HIV patients was their main concern in treating these patients (P = 0.0000) [Table 4].
About 98% of the study sample felt that it was necessary to screen patients for HIV in dental clinics but only one dentist in the study sample of 102 dentists reported of having done any screening test for HIV on their patients for the past 12 months [Table 4].
DISCUSSION
The care of people with HIV/AIDS is challenging due to its multidisciplinary nature, its medical complexity, physical manifestations, the need for infection control procedures, and the associated stigma and discrimination.[7]
A rather interesting finding of the study was that close to 37% of the respondents believed that if a patient had anti-HIV antibodies it meant he/she was immune to dental caries and close to 62% did not know the average time between contracting HIV and producing antibodies against it.
With regard to possible modes of spread of infection in a dental setting the dentists in the present study had fairly good knowledge [Table 2].
The oral lesions more commonly associated with HIV/AIDS[8] like oral candidiasis, Kaposis sarcoma, hairy leukoplakia, and oral lesions of herpetic infections were readily identified by the dentists in the present study; however, knowledge regarding the lesions less commonly associated with the disease like neurologic disturbances and melanotic hyper-pigmentation was lacking [Table 3].
In most of the questionnaire categories, the dentists belonging to p2 category fared better than the p1 category. Domestically and internationally, HIV is a disease that is embedded in social and economic inequity, as it affects those of lower socioeconomic status (SES) at a disproportionately high rate.[9] Furthermore it has been reported that dental services are more likely to be accessed by people of lower SES if the services are provided locally and are free at point of delivery.[10] This would imply that more number of patients with HIV infection would turn up at dental colleges as the treatment here would be free of cost. This increased and repeated exposure of dentists involved in academic institutions (p2) to HIV patients could be the most probable reason so as to why they had better knowledge of the disease when compared with their counterparts who were involved in exclusive private practice (p1). Additionally, the dentists of p2 group, involved in dental schools tend to attend regular classes, seminars, and are involved in clinical case discussions as part of the teaching curriculum, which could have led to their better understanding of the disease process.
It is generally accepted that attitudes are affected by the level of knowledge. Most of the studies on HIV/AIDS have investigated attitudes in combination with the level of knowledge, and have concluded that more and continuous education is required to change negative attitudes. However, in the present study it was strange to note that the dentists in the p2 category despite having high levels of knowledge about HIV/AIDS; about 77% [Table 4] of them would treat these patients with some hesitation. This is in accordance with the study by Mitchell,[11] who reported that knowledge alone does not seem to change the attitude of most healthcare professionals, as some of them still experienced difficulty in establishing good relationship with AIDS patients. But still the attitude of this p2 group was overall better than the p1 group; as 67% of the p1 group dentists would refer these patients elsewhere without treating them and this difference we attribute to the better knowledge of the p2 dentists.
About 98% of the dentists felt that HIV screening was necessary in dental clinics but only one dentist in the current study had done such testing in the past 12 months. This variation could be attributed to several factors like ethical concerns, cost of the testing procedure, and nonexistence of laws and legislations that mandate such a test in dental setting.
We recommend that continuing dental education (CDE) programs on HIV/AIDS specifically targeted toward dentists exclusively involved in private practice, be developed to improve their knowledge. In addition, HIV testing prior to dental treatment and knowledge about patients’ infection state can reassure dentists and allow them to confidently do their jobs and thereby eliminate their hesitation in treating these patients. One of the latest types of testing, OraQuick (Orasure Technologies Inc), which detects antibodies to HIV-1 and HIV-2 in oral fluid and is noninvasive may be useful in this regard.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Annual Report 2011-12. National AIDS Control Organisation India, Department of AIDS Control, and Ministry of Health and Family Welfare (2012) [Last accessed on 02-05-2013]. Available from: http://aidsdatahub.org/dmdocuments/NACO_Annual_Report_2011_12.pdf .
- 2.Sadeghi M, Hakimi H. Iranian dental students’ knowledge of and attitudes towards HIV/AIDS patients. J Dent Educ. 2009;73:740–5. [PubMed] [Google Scholar]
- 3.Nasir EF, Astrom AN, David J, Ali RW. HIV and AIDS related knowledge, sources of information, and reported need for further education among dental students in Sudan: A cross sectional study. BMC Public Health. 2008;8:286. doi: 10.1186/1471-2458-8-286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Ryalat ST, Sawair FA, Shayyab MH, Amin WM. The knowledge and attitude about HIV/AIDS among Jordanian dental students: (Clinical versus pre clinical students) at the University of Jordan. BMC Res Notes. 2011;4:191. doi: 10.1186/1756-0500-4-191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Crossley ML. An investigation of dentists’ knowledge, attitudes and practices towards HIV+and patients with other blood-borne viruses in South Cheshire, UK. Br Dent J. 2004;196:749–54. doi: 10.1038/sj.bdj.4811382. [DOI] [PubMed] [Google Scholar]
- 6.Ellepola AN, Sundaram DB, Jayathilake S, Joseph BK, Sharma PN. Knowledge and attitudes about HIV/AIDS of dental students from Kuwait and Sri Lanka. J Dent Educ. 2011;75:574–81. [PubMed] [Google Scholar]
- 7.Naidoo P. Barriers to HIV care and treatment by doctors: A review of the literature. S Afr Fam Pract J. 2006;48:55–66. [Google Scholar]
- 8.An update of the classification and diagnostic criteria of oral lesions in HIV infection. EEC Clearinghouse on Oral Problems Related to HIV Infection and WHO Collaborating Centre on Oral Manifestations of the Human Immunodeficiency Virus. J Oral Pathol Med. 1991;20:97–100. [PubMed] [Google Scholar]
- 9.HIV/AIDS and socioeconomic status. American Psychological Association (APA) factsheet. [Last accessed on 02-05-2013]. Available from: http://www.apa.org/pi/ses/resources/publications/factsheet-hiv-aids.pdf .
- 10.Tickle M, Moulding G, Milsom K, Blinkhorn A. A study of primary dental care provision in young children with special reference to deprived communities. Br Dent J. 2000;188:559–62. doi: 10.1038/sj.bdj.4800539. [DOI] [PubMed] [Google Scholar]
- 11.Mitchell B. Attitudes of nurses towards AIDS patients. [Last accessed on 02-05-2013];Aust Electron J Nurs Educ. 1999 4 Available from: http://www.scu.edu.au/schools/nhcp/aejne/archive/vol4-2/studentmitchvol4_2.htm . [Google Scholar]


