Abstract
Context:
Preterm delivery is associated with high perinatal mortality and morbidity. Although detection of fetal fibronectin in cervical can predict preterm labor, but it is not available in lower source setting area. So, cervical length measurement by ultrasound can be used as an alternative to fetal fibronectin for predicting preterm labor.
Aims:
To find out the effectiveness of assessment of cervical length by endovaginal ultrasonography in predicting preterm delivery.
Settings and Design:
The study was conducted in the infertility clinic of Mahatma Gandhi Medical College and Research Institute, Pondicherry from January 2010 to July 2011.
Materials and Methods:
A total of 130 women with singleton gestation were studied with transvaginal ultrasonography (TVS) to assess the cervical changes (cervical length, dilation of internal os, presence of funneling) between 22 weeks and 24 weeks of gestation. The gestational age at delivery in women with cervical length with ≥25 mm were compared with those of <25 mm.
Statistical Analysis Used:
Statistical analysis was done using Chi-square test. The P value is <0.001 which is statistically significant.
Results:
The mean cervical length in the study population was 33.16 mm. 16 women had cervical length <25 mm at mid trimesters can out of which 13 (40.62%) went for spontaneous preterm delivery. The relative risk of preterm delivery increased as the length of the cervix decreased. The P value is <0.001 which is statistically significant. A significant difference was found between multigravida at risk of preterm being 62.5% compared to primigravida which was 37.5%.
Conclusions:
The risk of spontaneous preterm delivery is increased in women who are found to have a short cervix by TVS during pregnancy and it is a sensitive, simple and cost effective method of assessing risk of preterm delivery.
Keywords: Cervical length, preterm labor, transvaginal ultrasonography
INTRODUCTION
Preterm labor refers to the onset of uterine contractions of sufficient strength and frequency to effect progressive dilatation and effacement of the cervix between 20 and 37 weeks of gestation.[1] Preterm deliveries with its associated mortality and morbidity still represents one of the major unsolved problems in Obstetrics. Preterm birth complicates 5-10%ofpregnancies, but accounts for 85% of perinatal morbidity and mortality.[2] The estimated worldwide incidence of preterm birth in 2005 reported by World Health Organization World: 9.6%; Asia: 9.1%.[3] The incidence of preterm birth in India is estimated to be 11-14%.[4] Socio-economic factors like young maternal age, low maternal weight, poor nutritional status, illiteracy, un controlled fertility, poor sanitation and hygiene causing endemic diseases and general ill-health, hard manual work, lack of prenatal care, broken homes, un married status, substance abuse an demotional stress continue to adversely affect the incidence of preterm births.[5] Treatment of preterm babies is very expensive and unaffordable in developing countries like India. Many attempts have been made to develop methods that may help us to predict the onset of preterm labour so that measures could be taken to prevent its occurrence. One of the earliest indicators of cervical in competence or onset of labour is shortening of the cervix. Currently there is no strong evidence to support routine cervical assessment using ultrasound between 24 and 28 weeks for the purpose of predicting preterm delivery.[6] This is an attempt to find out the relation of cervical length measurement between 22 and 24 weeks by transvaginal ultrasonography (TVS) with the risk of prematurity.
MATERIALS AND METHODS
This was a prospective study conducted in unselected group of women at Mahatma Gandhi Medical College and Research Institute, Puducherry from January 2010 to July 2011. After taking a detail history, women with gestational age, 22-24 weeks were examined. Patients with multiple gestation and previous cervical surgery including cervical encirclage in the present pregnancy were excluded. Eligible patients were informed about the study and those who agreed to enter into the study, written consent was obtained from them. Cervical parameters (cervical length, dilation of internal os, presence of funneling) was assessed by TVS Wipro GE Logiq 200q Pro (6.5 MHRTZ). The study population was divided based on the cervical length in to two groups of <25 mm and ≥25 mm. Patients were followed up till delivery. The total number of deliveries <37 weeks and >37 weeks were recorded. The cervical length assessment was studied in primigravida and multigravida and the outcome was compared. Statistical analysis was done Chi-square test.
RESULTS
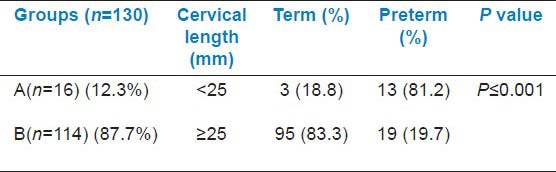
A total of 130 women entered into the study and were divided into two groups based on the cervical length measurement by endovaginal sonography, i.e., Group A-<25 mm and Group B-≥25 mm. The numbers were 16 (12.3%) and 114 (87.7%) in Group A and Group B respectively. In Group A 13 (81.2%) women had preterm delivery whereas in Group B only 19 (19.7%) had preterm delivery [Table 1].
Table 1.
Overall obstetric outcome
Obstetric outcome in primigravida shows that smaller the cervical length more the preterm birth. With the cervical length ≥25 mm, 83.82% of the primigravida delivered after 37 weeks whereas when the cervical length <25 mm, 83.33% of the primigravida delivered before 37 weeks [Table 2].
Table 2.
Obstetric outcome in relation to cervical length in primigravida
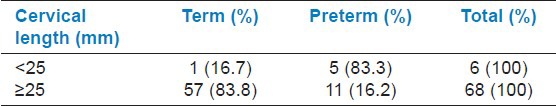
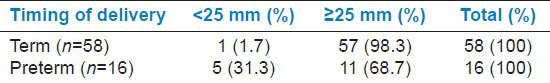
Among the primigravida of all the 58 term deliveries, 98.28% had cervical length of ≥25 mm and 1.72% had cervical length <25 mm. Of all the 16 preterm deliveries, 68.75% had cervical length ≥25 mm and 31.25% had cervical length <25 mm. This shows that preterm deliveries may not associate with smaller cervical length [Table 3].
Table 3.
Cervical length in relation to obstetric outcome in primigravida
The Obstetric outcome in multigravida also shows that smaller the cervical length more the preterm birth. With the cervical length ≥25 mm, 82.6% of the multigravida delivered after 37 weeks whereas when the cervical length <25 mm, 80% of the multigravida delivered before 37 weeks [Table 4].
Table 4.
Obstetric outcome in relation to cervical length in multigravida
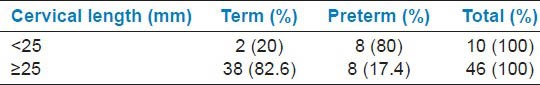
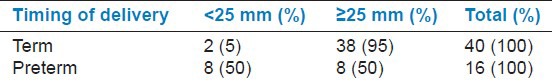
Among the Multigravida of the 40 term deliveries, 95% had cervical length ≥25 mm and 5% of them had cervical length <25 mm. Of the preterm deliveries, 50% had cervical length ≥25 mm and 50% of them had cervical length <25 mm. This also shows that preterm deliveries may not always associate with smaller cervical length [Table 5].
Table 5.
Cervical length in relation to obstetric outcome in multigravida
Although cervical length with measurement <25 mm predisposes to preterm labour, comparison of preterm deliveries between primigravida and multigravida shows, it is more so in multigravida than in primigravida [Table 6].
Table 6.
Comparison of preterm deliveries in primigravida and multigravida

DISCUSSION
Preterm delivery complicates 5-10% of pregnancies and accounts for 85% of perinatal morbidity and mortality. It represents major unsolved problems in obstetrics.[7] The length of the cervix is correlated with the duration of pregnancy: The shorter the cervical length the greater risk of preterm delivery. Progressive cervical changes begin at the internal cervical os and proceed to the external os. These changes are usually established before the dilatation of the external os and can begin as early as 16 to 24 weeks of gestation inpatients who eventually delivery preterm. Many studies have shown that cervical length measured by transvaginal ultrasound is are producible, safe and more accurate method than digital examination or transabdominal or transperineal ultrasound.[7] There appears to be a relationship between risk of preterm delivery and a decreased length of cervix in the general population. Many studies have shown that cervical length assessment by endovaginal sonography at mid trimester ultrasound predicts preterm birth.[8]
The overall incidence of preterm delivery in the present study was 12.31%, whereas according to Hassan et al. and Dilek et al. it is 10%, 7.4% respectively.[7,9] The mean cervical length in our study was 36.16 mm whereas in study by Kore et al. it was 36.4 ± 7.98 mm. Kore found the values of cervical length in primigravidas and multigravidas were almost similar.[10] A similar study conducted by Iams showed a mean cervical length of 35.2 ± 8.3 mm at 24 weeks.[11] Heath et al. measured the cervical length by TVS at 23 weeks in 2567 singleton pregnancies in women attending routine antenatal care.[12]
The risk for delivery at ≤32 weeks decreased from 78% at a cervical length of 5 mm to 4% at 15 mm and 0.5% at 50 mm. There, thus, appears to be a relationship between the risk of preterm delivery and the functional length of the cervix in the general population. Guzman et al. conducted a study on high risk singleton women and found that ultrasonographic assessment of funnelling did not offer any advantage over the cervical length.[13] Heal so observed the cervical changes in women whose functional cervical length decreased after transfundal pressure but digital cervical examination revealed long closed cervix. To et al. measured cervical length among 6819 women with singleton pregnancies at 22-24 weeks and looked for the presence of funnelling to evaluate its possible additional risk.[14]
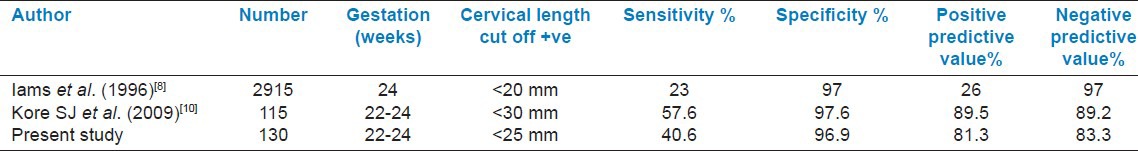
Here, we are mentioning a comparison of sensitivity and specificity of cervical length for predicting preterm labour in different studies [Table 7]. In the present study, the cut-off value of cervical length is <25 mm. It has a sensitivity of 40.6%andspecificityof 96.5%. Therefore, the accuracy of TVS to assess cervical length is specific in predicting preterm labour.
Table 7.
Sensitivity and specificity of cervical length for predicting preterm labour in different studies
CONCLUSION
From the above study, it was concluded that the acceptance of trans-vaginal ultra sound was good amongst women. Since the cervical length measurement was combined with targeted imaging for fetal anomalies scan, no additional cost was acquired by the women. A shorter cervical length at mid trimester scan was found to be associated with a risk of preterm delivery. Studies to look in to the cut off values of cervical lengths at different gestations may be useful to predict preterm labour. A larger study is required to confirm the findings of the present study.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Edwin C, Sabaratnam A. Recent advances in management of preterm labor. J Obstet Gynecol India. 2005;55:118–24. [Google Scholar]
- 2.Goswami K, Thornton S. Progress in Obstetrics and Gynaecology. Vol. 17. New Delhi: John Studd, Edinburg, Churchill Livingstone; 2006. The prevention and treatment of preterm labor. [Google Scholar]
- 3. Available from: http://premierhelp.com/about.premiers/premierfacts-a-figures/general-premier.statistics/incidenceofpretermbirth .
- 4.Singh U, Singh N, Shikha S. A prospective analysis of aetiology and outcome of preterm labor. J Obstet Gynaecol India. 2007;57:48–52. [Google Scholar]
- 5.Arias F, Daftary SN, Bhide AG. 3rd ed. New Delhi: Elsevier; 2008. Practical guide to high risk pregnancy and delivery. [Google Scholar]
- 6.Owen J, Iams JD, Hauth JC. Vaginal sonography and cervical incompetence. Am J Obstet Gynecol. 2003;188:586–96. doi: 10.1067/mob.2003.137. [DOI] [PubMed] [Google Scholar]
- 7.Dilek TU, Yazici G, Gurbuz A, Tasdelen B, Gulhan S, Dilek B, et al. Progressive cervical length changes versus single cervical length measurement by transvaginal ultrasound for prediction of preterm delivery. Gynecol Obstet Invest. 2007;64:175–9. doi: 10.1159/000106486. [DOI] [PubMed] [Google Scholar]
- 8.Iams JD, Goldenberg RL, Meis PJ, Mercer BM, Moawad A, Das A, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996;334:567–72. doi: 10.1056/NEJM199602293340904. [DOI] [PubMed] [Google Scholar]
- 9.Hassan SS, Romero R, Berry SM, Dang K, Blackwell SC, Treadwell MC, et al. Patients with an ultrasonographic cervical length ≤15 mm have nearly a 50% risk of early spontaneous preterm delivery. Am J Obstet Gynecol. 2000;182:1458–67. doi: 10.1067/mob.2000.106851. [DOI] [PubMed] [Google Scholar]
- 10.Kore SJ, Parikh MP, Lakhotia S, Kulkarni V, Ambiye VR. Prediction of risk of preterm delivery by cervical assessment by trans vaginal ultrasonography. J Obstet Gynecol India. 2009;59:131–5. [Google Scholar]
- 11.Heath VC, Southall TR, Souka AP, Elisseou A, Nicolaides KH. Cervical length at 23 weeks of gestation: Prediction of spontaneous preterm delivery. Ultrasound Obstet Gynecol. 1998;12:312–7. doi: 10.1046/j.1469-0705.1998.12050312.x. [DOI] [PubMed] [Google Scholar]
- 12.Guzman ER, Vintzileos AM, McLean DA, Martins ME, Benito CW, Hanley ML. The natural history of a positive response to transfundal pressure in women at risk for cervical incompetence. Am J Obstet Gynecol. 1997;176:634–8. doi: 10.1016/s0002-9378(97)70560-x. [DOI] [PubMed] [Google Scholar]
- 13.To MS, Skentou C, Liao AW, Cacho A, Nicolaides KH. Cervical length and funneling at 23 weeks of gestation in the prediction of spontaneous early preterm delivery. Ultrasound Obstet Gynecol. 2001;18:200–3. doi: 10.1046/j.1469-0705.2001.00437.x. [DOI] [PubMed] [Google Scholar]
- 14.Okitsu O, Mimura T, Nakayama T, Aono T. Early prediction of preterm delivery by transvaginal ultrasonography. Ultrsound Obstet Gynecol. 1992;2:402–9. doi: 10.1046/j.1469-0705.1992.02060402.x. [DOI] [PubMed] [Google Scholar]


