Abstract
Background:
In the first half of 20th century; mortality from colorectal surgery often exceeded 20%, mainly due to sepsis. Modern surgical techniques and improved perioperative care have significantly lowered the mortality rate. Mechanical bowel preparation (MBP) is aimed at cleansing the large bowel of fecal content thus reducing morbidity and mortality related to colorectal surgery. We carried out a study aimed to investigate the outcomes of colorectal surgery with and without MBPs, to avoid unpleasant side-effects of MBP and also to design a protocol for preparation of a patient for colorectal surgery.
Materials and Methods:
This was a prospective study over a period of March 2008-May 2010 carried out at Department of General Surgery of our institution. A total of 63 patients were included in this study; among those 32 patients were operated with MBPs and 31 without it; admitted in in-patient department undergoing resection of left colon and rectum for benign and malignant conditions in both emergency and elective conditions.
Results:
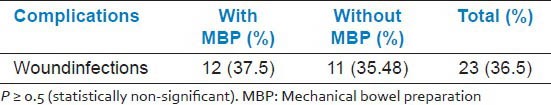
Anastomotic leakage, intra-abdominal collections was detected clinically and radiologically in 2 and 4 patients in each group respectively. P > 0.5 in both situations, indicating statistically no difference between results of two groups. Wound infections were detected in 12 (37.5%) patients with MBP group and 11 (35.48%) patients without MBP.
Conclusion:
The present results suggest that the omission of MBP does not impair healing of colonic anastomosis; neither increases the risk of leakage.
Keywords: Anastomotic leakage, colorectal surgery, pre-operative mechanical bowel preparation
INTRODUCTION
In the first half of 20th century, mortality from colorectal surgery often exceeded 20%,[1] mainly due to sepsis. Modern surgical techniques and improved perioperative care have significantly lowered the mortality rate. Infectious complications, however still are a major cause of morbidity and mortality in colorectal surgery. Mechanical bowel preparation (MBP) is aimed at cleansing the large bowel of fecal content. Bowel preparation by orthograde cleansing prior to colorectal surgery is still commonly recommended in several practical guidelines.[2] The main intention of such practice is to reduce post-operative complication in addition to easing the intraoperative handling of the bowel. Emptying of colon of its content seemed to be a logical step prior to interventions thus pre-operative cleansing was established as a dogma in the early 70s.[3] Traditionally, bowel cleansing was achieved using enemas in combination with oral laxatives. More recently oral cathartic agents to induce diarrhea and cleanse the bowel from solid feces were developed. These new bowel preparation agents such as Polyethylene Glycol and Sodium Phosphate provide superior cleansing and are used by most surgeons in preparation for colorectal surgery.[4] There is however paucity of data showing that MBP by itself, separately from other operative and perioperative measures, actually reduces the rate of infectious complications.
MATERIALS AND METHODS
This was a prospective and randomized control study comprising of 63 patients over the period of March 2008 to May 2010 at Department of General Surgery of a tertiary care institution admitted in inpatient department (emergency as well as elective) who underwent resection and primary anastomosis of left colon and upper rectum. Patients with co-morbid conditions such as Diabetes mellitus and advanced malignancy were excluded, so were the patients with proximal colostomy and those undergoing abdomino-perineal resection. A total sample populations were divided into two equal arms (Patients receiving bowel preparation and patients without bowel preparation) and the outcome of this study were compared between the two groups and also with accepted standards of colorectal surgery. Oral Polyethylene glycol preparation as per manufacturer's instruction along with Phosphate enema All patients were received intravenous ceftriaxone and metronidazole – 1 h prior to Incision and continued for 36 h post-operatively.[5] Patient refusal, any known allergy or contraindication to polyethylene glycol, hepatic, renal or cardiopulmonary abnormality, alcoholism, diabetes, long-term drug therapy, bleeding diathesis, local skin site infections are excluded from this study.
In pre-operative assessment the patients were enquired about any history of drug allergy, previous operations or prolonged drug treatment. General examination, systemic examinations and assessment of the airway were done. Pre-operative fasting of minimum 6 h was ensured before operation in all day-care cases. All patients received premedication of tablet diazepam 10 mg orally the night before surgery as per pre-anesthetic check-up direction to allay anxiety, apprehension and for sound sleep. Patients also received tablet ranitidine 150 mg in the previous night and in the morning of operation with sips of water.
Outcomes of surgery were studied clinically, radiologically and by hematological parameters. Complications with reference to anastomotic dehiscence, intra-abdominal septic complication, wound infections; hospital stay-specifically post-operative hospital stays in days and fluid and electrolyte imbalance were recorded. Post-operative total blood investigation and wound swab culture done after 48 h, on 5th day and thereafter if necessary. Routine ultrasonographic examination was done on 5th day and thereafter if necessary. Contrast enhanced computed tomography scan of abdomen and contrast radiographic examination done in suspected anastomotic dehiscence.
RESULTS AND ANALYSIS
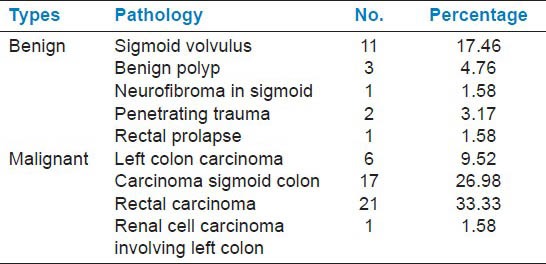
In this prospective study 37 (58.73%) patients were between 40 and 60 years. age group, 17 (26.98%) patients were more than 60 years. and 9 (14.28%) patients were between 20 and 40 years [Table 1]. Here 28.57% cases were benign and 71.42% cases were of malignant conditions [Table 2 and 3]. 61.9% of patients undergoing surgery were male and 38.09% were female [Table 2].
Table 1.
Age distributions of patients undergoing operative interventions
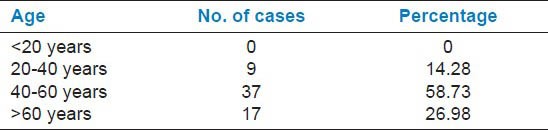
Table 2.
Sex distributions of patients undergoing operative interventions
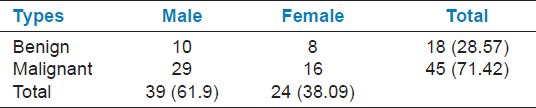
Table 3.
Pathological conditions which required operative interventions
Majority of patients (45 out of 63) had undergone elective operative interventions. Patients undergoing emergency surgery had mostly benign conditions (12 out of 18) and there was no scope for mechanical bowel preparation in those patients [Table 4]. Out of 63 patients 32 received MBP and 31 underwent without MBP [Table 5] which means both the groups were quite comparable. Anastomotic leak was observed in 2 patients in each group [Table 6] and 4 patients of each group suffered from intraabdominal collection [Table 7]. These clearly indicate complications are quite similar among two groups. Wound infections were almost same among two groups [Table 8].
Table 4.
Type of surgery patients required (emergency/elective)
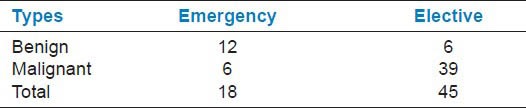
Table 5.
Operations with and without mechanical bowel preparation
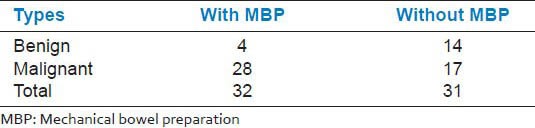
Table 6.
Anastomotic leak rate after colorectal surgery with and without mechanical bowel preparation
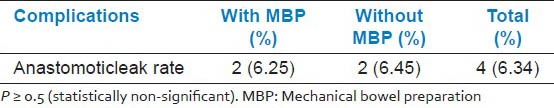
Table 7.
Incidence of intra-abdominal collection after colorectal surgery with and without MBP
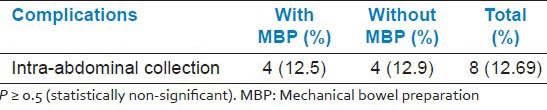
Table 8.
Wound infections after colorectal surgery with and without MBP
DISCUSSION
In our study, total 63 cases included of which 18 (28.57%) cases are with benign conditions and 45 (71.42%) cases with malignant conditions. 37 (58.73%) patients are between 40 and 60 years age group, 17 (26.98%) patients are more than 60 years and 9 (14.28%) patients are between 20 and 40 years age group. 61.9% of patients undergoing surgery are male and 38.09% are female.
Majority of patients (45 out of 63) have undergone elective operative interventions. Patients undergoing emergency surgery had mostly benign conditions (12 out of 18) and there was no scope for MBP in these patients. The study is designed to test the hypothesis that patients given no MBP before colorectal surgery do not have a higher risk of anastomotic leakage than those given MBP. There were conflicting results in the non-randomized studies with some showing an increased rate of infection and others reporting no difference in infection rates between the groups. The reported leakage rate varied greatly from 0% to 30%, but averages 5%[6,7,8,9,10,11,12,13,14] and rate of surgical wound infection has been 11% in patients undergoing colorectal operations with antibiotic prophylaxis.[15,16,17]
In 2003, Zmora et al.[16] compared orthograde MBP, with polyethylene glycol solution, versus no MBP. All patients received intravenous antibiotic prophylaxis before and during surgery. No information on anastomosis technique is given. This study enrolled a total of 380 patients with 78% (296 patients) suffering a neoplastic condition. There was a statistically insignificant decrease in anastomotic leak, wound infection and abdominal abscess rates in the no MBP group (P > 0.05).
In 1994, Burke et al.[17] compared orthograde MBP, with sodium picosulfate solution, versus no MBP in patients undergoing elective colorectal surgery. All patients received intravenous antibiotic prophylaxis (ceftriaxone and Metronidazole) during and after surgery for 24 h. The anastomosis technique was either manual or mechanical. 17 patients were excluded because bowel continuity was not restored after surgery or a colostomy was performed. This study enrolled a total of 186 patients with 79% (133 patients) suffering a neoplastic condition. No statistical difference in wound infection and anastomotic leak rates were seen between the two groups. Hughes et al.[18,19] reported on a small randomized trial in 1972. The 46 patients who underwent MBP fared no better than those 51 who did not.
In 1987, Irving and Scrimgeour[20,21] wrote a seminal article on 72 consecutive elective and emergency colectomies with primary anastomosis, where all MBP was omitted and the patient was only covered by a single pre-operative dose of cefuroxime and Metronidazole. No anastomotic dehiscence was clinically apparent and wound infection was noted in 8.3% of patients. In 1998, Platell and Hall[22] gave an excellent review of the literature and performed a meta-analysis of three trials in patients undergoing elective colorectal operations. It revealed a markedly greater incidence of wound infection in patients who received MBP (10.8% vs.7.4%).
In our study, 32 patients were operated after MBP with oral Polyethylene glycol preparation as per manufacturer's instruction along with Phosphate enema and 31 patients without MBP. All patients received intravenous ceftriaxone and metronidazole – 1 h prior to Incision and continued for 36 h post-operatively. The anastomosis technique was manual by a single layer interrupted serosubmucosal suture as advised by Matheson and Irving.
Among the post-operative complications, anastomotic leakage was detected clinically and radiologically in 2 patients in each group (6.25% with MBP and 6.45% without MBP) and intra-abdominal collections was detected radio logically in 4 patients in each group (12.5% with MBP and 12.9% without tMBP). P value was more than 0.5 in both situations, indicating statistically no difference between results of two groups. Wound infections were detected in 12 (37.5%) patients with MBP group and 11 (35.48%) patients without MBP. No statistically significant result was seen in post-operative incidence of persistent fever after 2nd post-operative day, post-operative change of blood picture indicating infections and post-operative hospital stay. Pre-operative electrolyte imbalance was more commonly noticed in older age group patients who presented with intestinal obstruction, but statistically no difference was found in between the two groups.
CONCLUSION
Utilization of pre-operative MBP in colorectal surgery has been evaluated in many clinical and experimental studies. Fecal loading and spillage have been reported as contributory factors to anastomotic leakage. Therefore, MBP can prevent fecal content from coming in contact with the small gaps between the sutures on the anastomotic line and thereby prevent fecal soiling of the peritoneal cavity. Based on these assumptions, most colorectal surgeons believe MBP is necessary for safe colorectal surgery. The present results suggest that the omission of MBP does not impair healing of colonic anastomosis; neither increases the risk of leakage.
Due to the small sample size in this study, there remains a chance of statistical error. There is a need for more prospective clinical studies with large sample size to evaluate the role of MBP in outcomes of colorectal surgery.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Glenn F, McSherry CK. Carcinoma of the distal large bowel: 32-year review of 1,026 cases. Ann Surg. 1966;163:838–49. doi: 10.1097/00000658-196606000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Duxbury MS, Brodribb AJ, Oppong FC, Hosie KB. Management of colorectal cancer: Variations in practice in one hospital. Eur J Surg Oncol. 2003;29:400–2. doi: 10.1053/ejso.2002.1426. [DOI] [PubMed] [Google Scholar]
- 3.Beck DE, Fazio VW. Current preoperative bowel cleansing methods. Results of a survey. Dis Colon Rectum. 1990;33:12–5. doi: 10.1007/BF02053194. [DOI] [PubMed] [Google Scholar]
- 4.Solla JA, Rothenberger DA. Preoperative bowel preparation. A survey of colon and rectal surgeons. Dis Colon Rectum. 1990;33:154–9. doi: 10.1007/BF02055549. [DOI] [PubMed] [Google Scholar]
- 5.Zinner M, Ashley S. 11th ed. New York: McGraw-Hill; 2007. Maingot's Abdominal Operations; pp. 644–5. [Google Scholar]
- 6.Nwiloh J, Dardik H, Dardik M, Aneke L, Ibrahim IM. Changing patterns in the morbidity and mortality of colorectal surgery. Am J Surg. 1991;162:83–5. doi: 10.1016/0002-9610(91)90209-v. [DOI] [PubMed] [Google Scholar]
- 7.Lothian and Borders large bowel cancer project: Immediate outcome after surgery. The consultant surgeons and pathologists of the Lothian and Borders Health Boards. Br J Surg. 1995;82:888–90. doi: 10.1002/bjs.1800820709. [DOI] [PubMed] [Google Scholar]
- 8.Fingerhut A, Hay JM, Elhadad A, Lacaine F, Flamant Y. Supraperitoneal colorectal anastomosis: Hand-sewn versus circular staples – A controlled clinical trial. French Associations for Surgical Research. Surgery. 1995;118:479–85. doi: 10.1016/s0039-6060(05)80362-9. [DOI] [PubMed] [Google Scholar]
- 9.Mann B, Kleinschmidt S, Stremmel W. Prospective study of hand-sutured anastomosis after colorectal resection. Br J Surg. 1996;83:29–31. doi: 10.1002/bjs.1800830108. [DOI] [PubMed] [Google Scholar]
- 10.Singh KK, Aitken RJ. Outcome in patients with colorectal cancer managed by surgical trainees. Br J Surg. 1999;86:1332–6. doi: 10.1046/j.1365-2168.1999.01234.x. [DOI] [PubMed] [Google Scholar]
- 11.Singh KK, Barry MK, Ralston P, Henderson MA, McCormick JS, Walls AD, et al. Audit of colorectal cancer surgery by non-specialist surgeons. Br J Surg. 1997;84:343–7. [PubMed] [Google Scholar]
- 12.Sørensen LT, Jørgensen T, Kirkeby LT, Skovdal J, Vennits B, Wille-Jørgensen P. Smoking and alcohol abuse are major risk factors for anastomotic leakage in colorectal surgery. Br J Surg. 1999;86:927–31. doi: 10.1046/j.1365-2168.1999.01165.x. [DOI] [PubMed] [Google Scholar]
- 13.Alves A, Panis Y, Pocard M, Regimbeau JM, Valleur P. Management of anastomotic leakage after nondiverted large bowel resection. J Am Coll Surg. 1999;189:554–9. doi: 10.1016/s1072-7515(99)00207-0. [DOI] [PubMed] [Google Scholar]
- 14.Platell C, Hall JC. The role of wound infection as a clinical indicator after colorectal surgery. J Qual Clin Pract. 1997;17:203–7. [PubMed] [Google Scholar]
- 15.Song F, Glenny AM. Antimicrobial prophylaxis in colorectal surgery: A systematic review of randomized controlled trials. Br J Surg. 1998;85:1232–41. doi: 10.1046/j.1365-2168.1998.00883.x. [DOI] [PubMed] [Google Scholar]
- 16.Zmora O, Mahajna A, Bar-Zakai B, Rosin D, Hershko D, Shabtai M, et al. Colon and rectal surgery without mechanical bowel preparation: A randomized prospective trial. Ann Surg. 2003;237:363–7. doi: 10.1097/01.SLA.0000055222.90581.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Burke P, Mealy K, Gillen P, Joyce W, Traynor O, Hyland J. Requirement for bowel preparation in colorectal surgery. Br J Surg. 1994;81:907–10. doi: 10.1002/bjs.1800810639. [DOI] [PubMed] [Google Scholar]
- 18.Hughes ES. Asepsis in large-bowel surgery. Ann R Coll Surg Engl. 1972;51:347–56. [PMC free article] [PubMed] [Google Scholar]
- 19.Hughes ES, McDermott FT, Polglase AL, Johnson WR, Pihl EA. Sepsis and asepsis in large bowel cancer surgery. World J Surg. 1982;6:160–5. doi: 10.1007/BF01654683. [DOI] [PubMed] [Google Scholar]
- 20.Irving AD, Scrimgeour D. Mechanical bowel preparation for colonic resection and anastomosis. Br J Surg. 1987;74:580–1. doi: 10.1002/bjs.1800740711. [DOI] [PubMed] [Google Scholar]
- 21.Ansari MZ, Collopy BT, Hart WG, Carson NJ, Chandraraj EJ. In-hospital mortality and associated complications after bowel surgery in Victorian public hospitals. Aust N Z J Surg. 2000;70:6–10. doi: 10.1046/j.1440-1622.2000.01733.x. [DOI] [PubMed] [Google Scholar]
- 22.Platell C, Hall J. What is the role of mechanical bowel preparation in patients undergoing colorectal surgery? Dis Colon Rectum. 1998;41:875–82. doi: 10.1007/BF02235369. [DOI] [PubMed] [Google Scholar]


