Abstract
Background:
Letrazole is an aromatase inhibitor, which is useful in ovulation induction. However, evidence on its efficacy over clomiphene citrate, which is the first of drug used for therapy of anovulation, is insufficient in Indian patients.
Aims:
To compare the efficacy of letrozole and clomiphene citrate in attaining optimal follicular growth.
Materials and Methods:
The study was conducted in the infertility clinic of Mahatma Gandhi Medical College and Research Institute, Pondicherry, India from June 2008 to December 2009. Fifty women with ovulatory dysfunction as a cause of infertility were enrolled and randomized into two groups of 25 each. Group 1 received clomiphene citrate in incremental dose from 50 mg up to150 mg and Group 2 patient received letrozole in incremental dose from 2.5 mg to 7.5 mg, depending upon the ovulation response. In both the groups, number of follicles, diameter of large follicle, endometrial thickness, and serum estradiol and pregnancy rate were compared. The data from both groups are represented as mean and standard deviation and statistically compared using Student's t test.
Results:
The number of follicles (1.89 ± 0.9 vs 1.18 ± 0.393) and serum estradiol levels (437.5 ± 293.7 pg/mL vs 291.82 ± 59.86 pg/mL) were higher in Group 1, while follicular diameter (20.67 ± 0.970 mm vs. 20.76 ± 0.903 mm) and endometrial thickness (8.5 mm vs.7.4 mm) were similar in both the Groups.
Conclusions:
Although letrozole is used for ovulation induction in anovulatory infertility, no significant beneficial effects of letrozole compared to use of clomiphene citratewere observedin ourstudy. Hence, we concur with the use of clomiphene citrate as the first line of drug for ovulation induction in Indian population and warrant larger size studiesto further validate our results.
Keywords: Clomiphene citrate, letrozole, ovulation induction
INTRODUCTION
Despite growing population infertility is of great concern among many couples as it affects 10%-15% of reproductively active couples. Several causes of infertility such have male factors (20%-25%), anovulation (15%-20%), tubal defects (15%-40%), endometriosis (5%-10%), and unknown etiology (20%-30%) are documented.[1] Clomiphene citrate is widely accepted as first line of ovulation-inducing agent. The advantages are low cost, easy administration, and high ovulation rate of 60%-80%. However, the disadvantage is low pregnancy rate of about 50%.[2,3] Letrozole, is a potent, highly specific nonsteroidal aromatase inhibitor with ovulation induction potential and high pregnancy rate of 80%, whichis due to its less antiestrogenic effect on endometrium.[4] Previous studies have compared the efficacy of clomiphene citrate and letrozole among Western population; however, the data of comparing the efficacy of these two drugs among Indian population are lacking; hence, the present study was designed.
MATERIALS AND METHODS
The study was conducted in the infertility clinic of Mahatma Gandhi Medical College and Research Institute, Pondicherry, India, during June 2008 to December 2009. A detailed history was obtained from the infertile couple at first visit. Previous records if available were verified for the information such assemen analysis, tubal patency, hormonal assay, and use of any prior use of ovulation inducing agent/s. After ruling out male factor, tubal factor, local factor of infertility, the woman was followed through one natural cycle by transvaginal ultrasound (Wipro GE, Logiq 200, 6.5MHz transducer) for follicular development. Those who did not show the sign of follicular development by ultrasonography were randomized into two groups by using table of random number. Group 1 consisted of 25 women receiving 50 mg of clomiphene citrate from day 2 to day 6 and follicular monitoring was done from day 10 onward till day 18 on alternate days. Women, who did not show optimal follicular growth (20 mm), received 100 mg and 150 mg of clomiphene citrate in subsequent cycle for follicular development and were monitored for optimal follicular growth by transvaginal ultrasound. In Group 2, letrozole 2.5 mg was used from day 2 to day 6 and followed similarly to Group 1. Women, who did not show optimal follicular growth (20 mm), received 5 mg and 7.5 mg of letrozole in subsequent cycle. Person doing ultrasound was blinded for the drug patient received. Both the groups were followed-up for the number of follicles, diameter of large follicle, endometrial thickness, and serum estradiol levels. Women not responding to one drug were given the other drug but not included in the study.
RESULTS
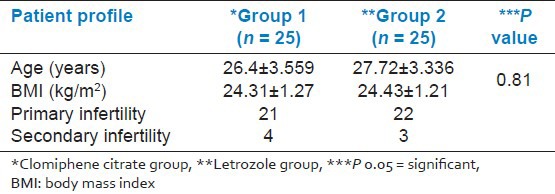
The mean ages (26.4 ± 3.55 and 27.72 ± 3.33 years) and body mass index (24.31 ± 1.27 and 24.43 ± 1.21kg/m2) of women were similar in Group 1 and Group 2, respectively. The numbers of patients with primary infertility were 21 and 22 in Group 1 and Group 2 respectively, while secondary infertility was observed in 4 and 3 patients from Group 1 and Group 2, respectively [Table 1].
Table 1.
Profile of the subjects
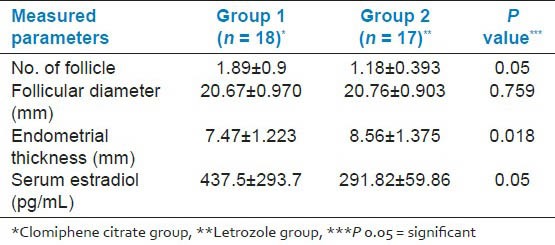
Seven women had one follicle, seven women had two follicles, three women had three follicles, and one woman had four follicles in Group 1, while in Group 2 14 women had one follicle and only 3 women had two follicles. The mean numbers of follicles were 1.89 ± 0.9 and 1.18 ± 0.393 in Group 1 and Group 2, respectively. One woman of Group 1 had 4 follicles [Table 2]. The mean follicular diameter (20.67 ± 0.970 mm vs.20.76 ± 0.903 mm) was similar in Group 1 and Group 2, respectively [Table 2]. The mean endometrial thickness in Group 1 (7.47 ± 1.223 mm) and Group 2 (8.56 ± 1.375 mm) was not statistically different [Table 2]. The mean serum estradiol in Group 1 (437.5 ± 293.7 pg/mL) was significantly higher than Group 2 (291.82 ± 59.86 pg/mL) [Table 2].
Table 2.
Response to ovulation inducing agents
DISCUSSION
Most common treatable cause of infertility is anovulation. For last 40 years, the first line of treatment for women having anovulatory infertility was clomiphene citrate.[5] Unfortunately, despite high rates of ovulation, pregnancy rates per cycle remain relatively low.[4] Both thin endometrium and non-trilaminar pattern of the endometrium at midcycle are associated with low pregnancy rates and early pregnancy loss.[6] For women who experienced these adverse effects with clomiphene citrate, the next optionis induction of ovulation with gonadotropin which increases both cost and risk to the woman. Alternatively, letrozole a potent aromatase inhibitor with excellent oral bioavailability and relatively short half-life is used for ovulation induction.[5]
In our study, both the groups were comparable with respect to age and body mass index. Although previous studies[6,7,8] reported similar ovulation rate by clomiphene citrate and/or letrozole, we observed higher ovulation rate in the clomiphene citrate group compared with letrozole-treated group. However, our results are compared to previous study reporting monofollicular development with letrozole.[9] Nevertheless, we observed similarity in mean follicular diameter between the two groups which is concurrent to previous report.[8]
Effect of clomiphene and letrozole on endometrium in ourstudy was comparable with study by Mitwally et al.,[4,10] who noted that women who had endometrial thickness of 5mm with clomiphene citrate responded well with 2.5 mg of letrozole and showed an increase in endometrial thickness up to 8 mm. Contrary to this, Fisher et al., and Kar[6,7] observed no difference of endometrial thickness in their study.
Estimation of serum estradiol is important especially to know the quality of ovum, and for administration of human gonadotrophin (hCG) in cases of stimulated cycle. However, high serum estradiol predisposes to hyperstimulation syndrome. Although human gonadotrophin was not used in our study, we estimate serum estradiol to know the antiestrogenic property of clomiphene citrate and letrozole. Concurrent to previous reports[6,10] we observed a significantly higher serum estradiol levels in clomiphene citrate-treated group.
Although the numbers of follicles developed per cycle by using clomiphene citrate was higher; nevertheless, it increases the chances of ovarian hyperstimulation syndrome and multiple pregnancy. However, in our study no multiple pregnancy was noted. Interestingly, Kar[7] also showed monofolliculogenesis similar to our study; however, the pregnancy rate was higher in letrozole group in contrast to clomiphene group.[7] This result may be due to increase resistance to the clomiphene in polycystic ovarian syndrome (PCOS). In contrast, our study response to the clomiphene was good as none of our cases were PCOS.
On the basis of our study we conclude that clomiphene citrate should be considered as first line of drug and failing which letrozole may be tried as alternative. We acknowledge small sample size as limitation of our study and warrant future studies with larger sample size to the compare the efficacy of clomiphene citrate and letrozole.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Bhattacharya S. Infertility. In: Edmonds DK, editor. Dewhurst's Text Book of Obstetrics and Gynaecology. 7th ed. Milton: Australia Blackwell Publishing Asia Pvt Ltd; 2007. pp. 440–60. [Google Scholar]
- 2.Gorlitsky GA, Kase NG, Speroff L. Ovulation and pregnancy rates with clomiphene citrate. Obstet Gynecol. 1978;51:265–9. doi: 10.1097/00006250-197803000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Dickey RP, Taylor SN, Curole DN, Rey PH, Pyrzak R. Incidence of spontaneous abortion in clomiphene pregnancies. Hum Reprod. 1996;11:2623–8. doi: 10.1093/oxfordjournals.humrep.a019182. [DOI] [PubMed] [Google Scholar]
- 4.Mitwally MF, Casper RF. Use of an aromatase inhibitor for induction of ovulation in patients with an inadequate response to clomiphene citrate. Fertil Steril. 2001;75:305–9. doi: 10.1016/s0015-0282(00)01705-2. [DOI] [PubMed] [Google Scholar]
- 5.Casper RF, Mitwally MF. Review: Aromatase inhibitors for ovulation induction. J Clin Endocrinol Metab. 2006;91:760–71. doi: 10.1210/jc.2005-1923. [DOI] [PubMed] [Google Scholar]
- 6.Fisher SA, Reid RL, Van Vugt DA, Casper RF. A randomized double blind comparison of the effects of clomiphene citrate and the aromatase inhibitor letrozole on ovulatory function in normal women. Fertil Steril. 2002;78:280–5. doi: 10.1016/s0015-0282(02)03241-7. [DOI] [PubMed] [Google Scholar]
- 7.Kar S. Clomiphene citrate or letrozole as first-line ovulation induction drug in infertile PCOS women: A prospective randomized trial. J Hum Reprod Sci. 2012;5:262–5. doi: 10.4103/0974-1208.106338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zeinalzadeh M, Basirat Z, Esmailpour M. Efficacy of letrozole in ovulation induction compared to that of clomiphene citrate in patient with polycystic ovarian syndrome. J Reprod Med. 2010;55:36–40. [PubMed] [Google Scholar]
- 9.Begum MR, Quadir E, Begum A, Begum RA, Begum M. Role of aromatase inhibitor in ovulation induction in patient with poor response to clomiphene citrate. J Obstet Gynaecol Res. 2006;32:502–6. doi: 10.1111/j.1447-0756.2006.00434.x. [DOI] [PubMed] [Google Scholar]
- 10.Sh Tehrani Nejad E, Abediasl Z, Rashidi BH, Azimi Nekoo E, Shariat M, Amirchaghmaghi E. Comparison of the efficacy of aromatase inhibitor letrozole and clomiphene citrate, gonadotrophins in controlled ovarian hyperstimulatin: A prospective randomized clinical trial. J Assist Reprod Genet. 2008;25:187–90. doi: 10.1007/s10815-008-9209-2. [DOI] [PMC free article] [PubMed] [Google Scholar]


