Abstract
Epidermal inclusion cyst (EIC) is a benign lesion, which occurs due to proliferation and implantation of epidermal elements within a circumscribed space in dermis. They usually occur in the head and neck region, trunk and extremities. EIC occurring in the breast is very rare. In this study, we are presenting a rare case of EIC occurring in the breast; which was diagnosed by fine-needle aspiration cytology (FNAC). Later on, histopathology confirmed the diagnosis. We are presenting this case not only because of its rare site of presentation, but also to highlight the role of FNAC in diagnosing this benign lesion.
Keywords: Breast, epidermal inclusion cyst, fine-needle aspiration cytology
INTRODUCTION
Epidermal inclusion cyst (EIC) is a benign cystic lesion, which occurs due to proliferation and implantation of epidermal elements within a circumscribed space in the dermis.[1] Such cysts usually occur on the scalp, skin of head and neck, back and extremities. EIC occurring in the breast is very rare; to date less than 40 cases have been reported in the English literature.[2] When EIC occurs as a subcutaneous nodule in the skin of breast; clinical diagnosis may be easy; but when occurs within the breast parenchyma, correct clinical diagnosis is usually not possible. Cytological diagnosis of EIC in the breast is even rarer and there are only eleven published reports in the cytological literature.[1,2,3,4,5,6] Here, we present a case of EIC of breast primarily diagnosed by fine-needle aspiration cytology (FNAC), which is confirmed by histopathological examination.
CASE REPORT
A 30-year-old female attended to the FNAC clinic of our hospital with a lump in the right breast associated with pain. The lump was present for about 1 year duration. She had a history of pain in the same site 6 months back, but relieved by taking medication after consultation with a local physician. Physical examination revealed a lump in the upper and lower outer quadrant of the right breast measuring 3 cm × 2 cm with glistening overlying skin. The lump was mobile and no axillary lymphadenopathy was detected. Based on the history and physical examination findings, a clinical diagnosis of recurrent mastitis, possibly due to tuberculosis was suspected.
Fine-needle aspiration of the lump was performed using 22-gauge needle. Aspirate was pultaceous and smears were stained with May-Grόnwald-Giemsa stain. Smears examined show many anucleate squames and few benign nucleated squamous cells in a background containing inflammatory infiltrate along with few clusters of ductal epithelial cells with preserved myoepithelial component. Occasional foreign body type giant cells were also scattered in the smears [Figure 1a and b]. Based on these findings, a cytological diagnosis of infected EIC of breast was made and was advised for resection of the lump after a course of antibiotic therapy.
Figure 1.
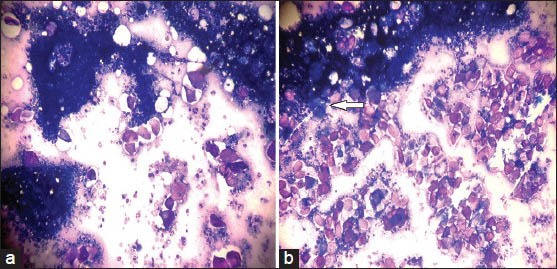
Fine-needle aspiration cytology showing (a) Many anucleate squames and few nucleated benign squamous cells in a background containing neutrophils. Note the presence of benign ductal epithelial cells with myoepithelial component (May-Grünwald-Giemsa, ×200), (b) Anuclete squames, few nucleated benign squamous cells and neutrophils along with foreign-body type giant cell (arrow) (MGG, ×200)
Patient was put on cefpodoxime, a third generation cephalosporin at a dose of 200 mg twice daily for 7 days. After 2 weeks of completion of course of antibiotics, surgical excision of the lump was done and sent for histopathological examination. Histopathology of the lump showed typical features of EIC with squamous lining and the cyst cavity filled with lamellated keratin [Figure 2]. Thus, a diagnosis of EIC was confirmed. Patient recovered uneventfully following surgery and discharged on the 5th post-operative day. Patient was followed-up for a period of 1 year and no recurrence was found during this period.
Figure 2.
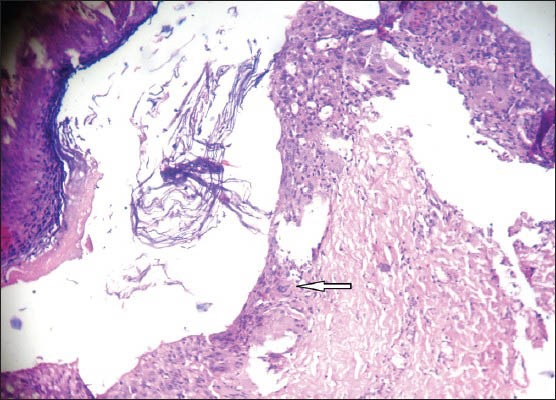
Section showing a cyst cavity lined by keratinized squamous epithelium and contents of cyst comprising of lamellated keratin. Note the presence of foreign-body type giant cell (arrow) (H and E, ×100)
DISCUSSION
EIC is a common benign cystic lesion that involves mainly head and neck region, trunk and the extremities. EIC occurring within the breast is very rare. Various theories have been postulated regarding their etiology within the breast.[3,7,8] They can develop due to various mechanisms that may result in damage to epidermis, which gets implanted within the breast tissue; such as congenital development of cyst secondary to obstructed hair follicles or pores, post-trauma, reduction mammoplasty, following squamous metaplasia of columnar cells within a dilated duct in cases of fibrocystic disease or within fibroadenoma or phyllodes tumors. In our case, as there is no history of previous trauma, surgery or lump; the etiology of EIC appears to be an obstruction of the hair follicle.
As breast contains flexible fat and mammary gland tissue under its skin, EIC in breast grows deep inside the subcutaneous tissue making both clinically and radiologically difficult to distinguish from a breast tumor. In elderly, it may mimic duct carcinoma while in younger patients; it is commonly mistaken as fibroadenoma. However secondary inflammation in EIC of the breast can also give a wrong clinical diagnosis of mastitis as occurs in our case. As the patient had previous and present history of pain associated with glistening overlying skin, we have mistaken it as recurrent mastitis, possibly due to tuberculosis.
EIC typically appears to be well-circumscribed with homogenous increased density on mammography.[1] Ultrasonographic examination of EIC of breast usually shows solid, circumscribed and complex mass.[2] Thus, radiological examination is not sufficient to diagnose EIC of breast as other lesions such as fibroadenoma, phyllodes tumor or even low-grade malignant lesions like mucinous carcinoma may give similar findings. Here, the role of FNAC comes as it is simple, easy to perform, quickly and gives the result with a reliable accuracy.
EIC usually yields pultaceous aspirate. Cytological smears show numerous anucleate squames as well as nucleated benign squamous cells. However if secondary infection occurs, aspirates usually become turbid and shows inflammatory cells such as neutrophils and histiocytes. Due to the intrapenchymal nature of EIC occurring in breast, fine-needle aspirates may include adjacent normal breast epithelial cells and adipocytes. In our case, we have aspirated normal breast ductal epithelial cells and neutrophils along with anucleate squames and nucleated benign squamous cells, making a diagnosis of infected EIC of breast possible.
Cytological differential diagnosis of EIC includes dermoid cyst, branchial cyst, pilomatrixoma, thyroglossal cyst, etc.[9] Smears of dermoid cyst are cytological similar to EIC however; it may also contain skin appendageal elements like hair shafts. Branchial cyst usually occurs in young adults and cytologically similar to EIC. The most important point to differentiate with EIC is the site of presentation, which is the lateral side of the neck. Aspirate from thyroglossal cyst can be cytologically indistinguishable from EIC. The diagnosis is usually based on the anatomical site of lesion. The content of thyroglossal cyst may sometimes be mucinous and mucin secreting and/or ciliated columnar epithelial cells may be present in the smears. Pilomatrixoma may sometimes mimic EIC on aspirates when only anucleate squames and nucleated benign squamous cells are aspirated. Foreign body type giant cells may also be seen in the aspirates of pilomatrixoma. Failure to aspirate basaloid cells and shadow cells usually gives the wrong cytological diagnosis in pilomatrixoma. Surgical excision and histopathological examination in these cases are necessary to establish the correct diagnosis.
EIC of the breast can cause severe complications, which includes spontaneous rupture leading to inflammation and abscesses.[2] Other rare but important complication of EIC includes malignant transformation into squamous cell carcinoma. The reported malignant transformation of the cyst wall varies from 0.045% to 19%.[10,11] However, as the overall incidence of EIC of the breast is less, reports are variable on its malignant transformation; thus the actual percentage is uncertain. Again, Paget's disease can rarely occur in the EIC arising from nipple/peri-nipple epidermis.
Surgical excision is the treatment of choice in EIC of breast. Although some author believes that asymptomatic cases can be followed-up radiologically and clinically, we recommend surgical excision in these cases to prevent any potential complication that may arise in the future.
Lastly, we have presented this case because of its rare site of presentation. This case also highlights the role of FNAC in arriving at a correct pre-operative diagnosis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Lam SY, Kasthoori JJ, Mun KS, Rahmat K. Epidermal inclusion cyst of the breast: A rare benign entity. Singapore Med J. 2010;51:e191–4. [PubMed] [Google Scholar]
- 2.Singh M, Maheshwari B, Khurana N, Jain S. Epidermal inclusion cyst in breast: Is it so rare? J Cytol. 2012;29:169–72. doi: 10.4103/0970-9371.101165. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chantra PK, Tang JT, Stanley TM, Bassett LW. Circumscribed fibrocystic mastopathy with formation of an epidermal cyst. AJR Am J Roentgenol. 1994;163:831–2. doi: 10.2214/ajr.163.4.8092018. [DOI] [PubMed] [Google Scholar]
- 4.Das DK, Junaid TA, Mathews SB, Ajrawi TG, Ahmed MS, Madda JP, et al. Fine needle aspiration cytology diagnosis of male breast lesions. A study of 185 cases. Acta Cytol. 1995;39:870–6. [PubMed] [Google Scholar]
- 5.Kapila K, Verma K. Fine needle aspiration cytology of epidermal inclusion cysts in the male breast. Acta Cytol. 2003;47:315–7. [PubMed] [Google Scholar]
- 6.Lilleng R, Paksoy N, Vural G, Langmark F, Hagmar B. Assessment of fine needle aspiration cytology and histopathology for diagnosing male breast masses. Acta Cytol. 1995;39:877–81. [PubMed] [Google Scholar]
- 7.Gerlock AJ. Epidermal inclusion cyst of the breast associated with needle aspiration biopsy. Radiology. 1974;112:69–70. doi: 10.1148/112.1.69. [DOI] [PubMed] [Google Scholar]
- 8.Davies JD, Nonni A, D’Costa HF. Mammary epidermoid inclusion cysts after wide-core needle biopsies. Histopathology. 1997;31:549–51. doi: 10.1046/j.1365-2559.1997.3290905.x. [DOI] [PubMed] [Google Scholar]
- 9.Handa U, Chhabra S, Mohan H. Epidermal inclusion cyst: Cytomorphological features and differential diagnosis. Diagn Cytopathol. 2008;36:861–3. doi: 10.1002/dc.20923. [DOI] [PubMed] [Google Scholar]
- 10.Cameron DS, Hilsinger RL., Jr Squamous cell carcinoma in an epidermal inclusion cyst: Case report. Otolaryngol Head Neck Surg. 2003;129:141–3. doi: 10.1016/S0194-59980300466-2. [DOI] [PubMed] [Google Scholar]
- 11.Menville JG. Simple dermoid cysts of the breast. Ann Surg. 1936;103:49–56. doi: 10.1097/00000658-193601000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]


