Abstract
Dental abnormalities associated with ectodermal dysplasia (ED) cause severe functional, esthetic and psychological problems. This case report describes treatment of a patient with hypohidrotic (Christ-Siemens -Touraine syndrome) ED. Patient was rehabilitated with the use of endosseous implants in mandible following an orthodontic treatment to bring the impacted maxillary canine in the arch. This procedure aided in the preservation of the surrounding bone and retention of the prosthesis. A tooth supported fixed partial denture (FPD) was fabricated for the maxillary arch and three separate (two all-tooth and one all-implant supported) FPDs were fabricated for the mandibular arch. Fixed prostheses boosted the self-esteem of this patient.
Keywords: Ectodermal dysplasia, endosseous implants, fixed partial denture
INTRODUCTION
Ectodermal dysplasia (ED) is a group of inherited disorders affecting more than one ectodermal derivative, primarily skin, hair, nails, eccrine glands and teeth. The condition is usually transmitted as an X-linked recessive trait[1,2] and includes up to 154 distinctive syndromes and 11 subgroups, labeled from 1 to 4 depending on the affected system (hair, teeth, nails or sweat glands). The hypohidrotic (anhidrotic) ED and hydrotic ED are the most common types of ED.[3] A new classification for ED is also proposed, based on the alterations in the proteic molecular functions.[4] Hypohidrotic ED is characterized by several defects such as hypohidrosis, anomalous dentition, onychodysplasia and hypotrichosis, wherein sweat glands are decreased significantly or completely absent. In contrast, the sweat glands of hidrotic ED tend to be normal, but teeth, hair and nails are affected.[5] According to the compendium of birth defects, 1 to 7 in 10,000 births results in a dysplasia of an ectodermally derived structure.[6] Dental abnormalities are associated with 80% of cases,[7] and may include anodontia, hypodontia, misshapen teeth, taurodontia, supernumerary teeth, neonatal teeth, natal teeth, retained primary teeth, enamel hypoplasia and lack of an alveolar ridge.[8] Hypodontia resulting from ED appears to follow a definite pattern. Guckes et al. found that the permanent teeth most likely to be present in 52 ED patients were the maxillary central incisors (42%), followed by maxillary first molars (41%) and mandibular first molars (39%). Mandibular anterior teeth were least likely to be present.[9]
Typical face of an ED patient is characterized by frontal bossing, sunken cheeks, pigmented skin around the eyes and large, low set ears. Strikingly the growth of the jaw is not impaired, but the alveolar processes are under developed due to decreased or absent teeth. This leads to a decreased vertical dimension expressed as protuberant lips and collapsed lower third of the face. Salivary glands, including the intraoral accessory glands are sometimes hypoplastic resulting in xerostomia and dry, cracked lips with pseudo rhagades formation.[10] Furthermore, tooth agenesis has been shown to have a significant impact upon the oral health-related quality- of- life. Compromised appearance of ED patients also affects their social interaction and psychological well-being.
Prosthodontic rehabilitation of ED patient includes overdentures, complete or partial removable dentures or FPDs (tooth-or implant-supported).[11,12] Several published reports describe this treatment approaches in ED patients.[13,14,15,16] However, it is always a challenge to fabricate dentures with optimum stability and retention due to the shape of teeth and thin alveolar ridges. Moreover, loading of the edentulous ridges at an early age may also lead to progressive resorption of the alveolar bone and lead to subsequent prosthetic problems.[5]
Endosseous dental implants have proved to be an effective treatment option for ED patients,[17,18,19,20] with clinical immobility for implants at the stage 2 surgery in ED patients being comparable with those for non-ED patients.[21] Implant- supported prostheses have a functional, esthetic and psychological advantage as it avoids the drawbacks associated with conventional tissue supported dentures.
Oral rehabilitation of ED patient involves interdisciplinary approach. The following clinical report illustrates the treatment of an ED patient with a fixed prosthesis following an orthodontic treatment, crown build-ups and implant placements with one year follow-up.
CASE REPORT
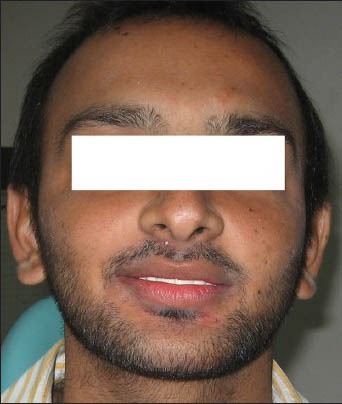
A healthy 21-year old male patient was diagnosed with hypohidrotic ED. Extra-oral examination revealed prominent forehead, large and low set ears, sparse hair, dry skin and abnormal nails [Figures 1 and 2]. Patient had been wearing upper and lower acrylic complete dentures laid over five maxillary and six mandibular teeth since a young age. The teeth supporting the overdenture were root canal treated and prepared to receive the overdenture [Figure 3]. This prosthesis restored his vertical dimension. Due to the social drawbacks associated with dentures, patient insisted on getting a fixed prosthesis. Family history revealed that his elder sibling was also diagnosed with ED and he was rehabilitated with tooth-supported maxillary and mandibular FPDs.
Figure 1.

Typical ED Facial Features
Figure 2.

Dry skin and abnormal nails
Figure 3.

Pre-operative intraoral findings
A series of radiographic evaluation was carried out to know the status of teeth and bone. Panoramic radiograph revealed an underdeveloped alveolar bone, two impacted teeth in the right maxillary canine region, one impacted tooth in the left maxillary canine region and a tooth with resorbed root in the right mandibular canine region which showed 3° mobility clinically. Roots of remaining teeth were surrounded by healthy bone [Figure 4]. Hand wrist radiograph was taken to confirm skeletal maturation [Figure 5].
Figure 4.
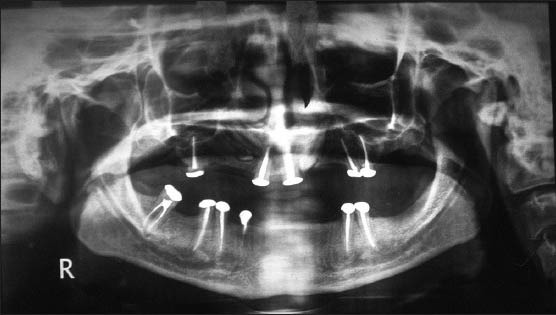
Pre-operative radiograph
Figure 5.

Hand wrist radiograph
A sequential treatment plan was formulated. The two impacted teeth in the right canine region of maxilla were horizontal and highly placed, and disturbing it would result in loss of the large amount of bone and hence was left untouched. The impacted tooth in the left maxillary canine region was in a favorable position, so surgical exposure and orthodontic eruption of that tooth was planned. Starting with discontinuation of dentures, posts were inserted in the overdenture abutments and their cores build up with composite resin to resemble a prepared abutment tooth of a FPD. Orthodontic brackets were fixed on the maxillary teeth and the impacted tooth was surgically exposed. It took six months to bring impacted tooth in arch position by fixed orthodontic treatment [Figure 6]. Clinical and radiographic evaluation indicated mandibular anterior region as an appropriate site for implant placement. During the initial phase of orthodontic treatment, three implants (Tatum Surgical Tapered, USA) were placed in the anterior mandible between the mental foramina. One implant of 4.0 mm × 14 mm was placed in left mandibular canine region, 2nd implant of 3.5 mm × 11 mm was placed in right mandibular lateral region and a 3rd implant of 3.5 mm × 11 mm was placed in the socket of right mandibular canine immediately after extraction. Cover screws were placed over the implants. After through irrigation, the surgical site was closed with sutures. Patient followed a standard regimen of antibiotic (Tablet- Cephadroxyl 500 mg) and analgesics (Tablet-Ibuprofen 400 mg). A period of four months was allowed for the implant osseointegration prior to the stage two surgeries. Straight abutments were attached to the implants and remaining natural teeth were prepared to receive a FPD [Figure 7]. Meanwhile, the orthodontic extrusion brought the left maxillary impacted tooth to an appropriate arch position, which was also prepared to serve as a FPD abutment. All acrylic temporary FPDs were fabricated followed by porcelain fused-to-metal maxillary FPD and three mandibular segmental permanent FPDs [Figures 8 and 9].
Figure 6.

Orthodontic treatment
Figure 7.

Implants with abutments
Figure 8.
Patient after final prosthesis
Figure 9.

Clinical photograph showing the completed restoration
DISCUSSION
Oral rehabilitation of ED patients have historically involved partial or complete removable prostheses supported by tissue or teeth (overdentures). When the number and distribution of the teeth seems to be optimum, a FPD is frequently the treatment of choice. The development and acceptance of screw type osseointegreted dental implants has provided an additional treatment modality for ED patients. Several published reports have provided evidence of success as well as failure of dental implants in ED patients. However, implants are highly preferred in rehabilitation of ED patients because of their bone preserving ability and enhanced retention of the prosthesis. Hence, implants should definitely be considered in the treatment planning of ED patients.
Implants survival rates vary from 88.5% to 97.6% in ED patients.[22] In ED patients, implant failure is higher in the maxilla (5-29%) than in the mandible (0-9%), which is attributed to deficiencies in bone volume at the implant site and sites with previous surgeries (e.g. removal of impacted canines, maxillary osteotomy, iliac crest grafted sites and immediate implant placement)[5,23,24] rather than ED. It is always advisable to bring the impacted teeth in the arch, if possible, to maintain healthy bone in that region and add to the number of abutments.
Removable prosthesis is the treatment of choice over FPDs or implants during the growing age to accommodate the growth of jaws. However, evidence supporting the claim that implants placed in ED patients younger than 18 years have high-risk of failure is very scarce.[23] Moreover, the anterior region of the mandible is regarded as transversely stable by the age of six years.[25,26] Hence, a careful selection of the site of placement in the posterior mandible of a growing individual results in the success of the implants as it can overcome the problem resulting due to remodeling of the lingual bony plate.[27] Transverse growth of the maxilla persists late into the 2nd decade and hence, the placement of implants should be delayed until growth completion.[28,29] Hence, when osseointegrated implants are being considered in the treatment planning of ED patients, dental and skeletal maturity not the chronologic age of the patient and proper site selection must be taken into consideration to prevent future infraocclusion of the prosthesis.[27,30]
As the age of ED patient advances, their social development and interaction becomes increasingly important. It has been reported that children rejected by their peer groups are more likely to become aggressive and delinquent. In addition, they are more likely to remain unaccepted by their peers and even to experience mental health problems in adulthood. Thus, psychological benefits associated with fixed (tooth-supported and implant-borne) prostheses have significant positive effects on growth, social development, self-image and food choice. Quality of life also improves in oligodontia patients receiving implants and prosthodontic treatment.[31]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Kupietzky A, Houpt M. Hypohidrotic ectodermal dysplasia: Characteristics and treatment. Quintessence Int. 1995;26:285–91. [PubMed] [Google Scholar]
- 2.Park JW, Hwang JY, Lee SY, Lee JS, Go MK, Whang KU. A case of hypohidrotic ectodermal dysplasia. J Dermatol. 1999;26:44–7. doi: 10.1111/j.1346-8138.1999.tb03508.x. [DOI] [PubMed] [Google Scholar]
- 3.Pinheiro M, Freire–Maia N. Ectodermal dysplasias: A clinical classification and a casual review. Am J Med Genet. 1994;53:153–62. doi: 10.1002/ajmg.1320530207. [DOI] [PubMed] [Google Scholar]
- 4.Lamartine J. Towards a new classification of ectodermal dysplasias. Clin Exp Dermatol. 2003;28:351–5. doi: 10.1046/j.1365-2230.2003.01319.x. [DOI] [PubMed] [Google Scholar]
- 5.Kearns G, Sharma A, Perrott D, Schmidt B, Kaban L, Vargervik K. Placement of endosseous implants in children and adolescents with hereditary ectodermal dysplasia. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88:5–10. doi: 10.1016/s1079-2104(99)70185-x. [DOI] [PubMed] [Google Scholar]
- 6.Dhanrajani PJ, Jiffry AO. Management of ectodermal dysplasia: A literature review. Dent Update. 1998;25:73–5. [PubMed] [Google Scholar]
- 7.Holbrook KA. Structural abnormalities of the epidermally derived appendages in the skin from patients with ectodermal dysplasia: Insight into developmental errors. Birth Defects Orig Artic Ser. 1988;24:15–44. [PubMed] [Google Scholar]
- 8.Witkop CJ, Jr, Brearly LJ, Gentry WC., Jr Hypoplastic enamel, onycholysis, and hypohidrosis inherited as an autosomal dominant trait. A review of ectodermal dysplasia syndromes. Oral Surg Med Oral Pathol. 1975;39:71–86. doi: 10.1016/0030-4220(75)90398-9. [DOI] [PubMed] [Google Scholar]
- 9.Guckes AD, Roberts MW, McCarthy GR. Pattern of permanent teeth present in individuals with ectodermal dysplasia and severe hypodontia suggests treatment with dental implants. Pediatr Dent. 1998;20:278–80. [PubMed] [Google Scholar]
- 10.Besserman, Nielsen M. Hypohydrotic ectodermal dysplasia. Oral manifestation and genetic aspects. Tandlaegebladet. 1971;75:1057–76. [PubMed] [Google Scholar]
- 11.Bolender CL, Law DB, Austin LB. Prosthodontic treatment of ectodermal dysplasia: A case report. J Prosthet Dent. 1995;19:167–72. [Google Scholar]
- 12.Snawder KD. Considerations in dental treatment of children with ectodermal dysplasia. J Am Dent Assoc. 1976;93:1177–9. doi: 10.14219/jada.archive.1976.0286. [DOI] [PubMed] [Google Scholar]
- 13.Nortje CJ, Farman AG, Thomas CJ, Watermeyer GJ. X-linked hypohidrotic ectodermal dysplasia: An unusual prosthetic problem. J Prosthet Dent. 1978;40:137–42. doi: 10.1016/0022-3913(78)90005-7. [DOI] [PubMed] [Google Scholar]
- 14.Herer PD. Treatment of anhidrotic ectodermal dysplasia: Report of case. J Dent Child. 1975;42:133–6. [PubMed] [Google Scholar]
- 15.Grinberg S, Jover P, Quiros L, Diaz L, Terron F. Ectodermal dysplasia: Report of two female cases. J Dent Child. 1980;47:193–5. [PubMed] [Google Scholar]
- 16.Sarnat BG, Brodie AG, Kubacki WH. Fourteen year report of facial growth in case of complete anodontia with ectodermal dysplasia. Am J Dis Child. 1953;86:162–9. doi: 10.1001/archpedi.1953.02050080171004. [DOI] [PubMed] [Google Scholar]
- 17.Perrott DH, Sharma A, Vargervik K. Endosseous implants for pediatric patients. Oral and Maxillofac Surg Clin North Am. 1994;6:79–88. [Google Scholar]
- 18.Bergendal T, Eckerdal O, Hallensten AL, Koch G, Kurol J, Kvint S. Osseointegrated implants in the oral habilitation of a boy with ectodermal dysplasia: A case report. Int Dent J. 1991;41:149–56. [PubMed] [Google Scholar]
- 19.Guckes AD, Brahim JS, McCarthy GR, Rudy SF, Cooper LF. Using endosseous implants for patients with ectodermal dysplasia. J Am Dent Assoc. 1991;122:59–62. doi: 10.14219/jada.archive.1991.0307. [DOI] [PubMed] [Google Scholar]
- 20.Smith RA, Vargervik K, Kearns G, Bosch C, Koumjian J. Placement of an endosseous implant in a growing child with ectodermal dysplasia. Oral Surg Oral Med Oral Pathol. 1993;75:669–73. doi: 10.1016/0030-4220(93)90419-5. [DOI] [PubMed] [Google Scholar]
- 21.Guckes AD, Brahim JS, Rudy SF, McCarthy GR. Use of titanium screw implants in individual with ectodermal dysplasia. J Dent Res. 1991;70:487. [Google Scholar]
- 22.Yap AK, Klineberg I. Dental implants in patients with ectodermal dysplasia and tooth agenesis: A critical review of the literature. Int J Prosthodont. 2009;22:268–76. [PubMed] [Google Scholar]
- 23.Guckes AD, Scurria MS, King TS, McCarthy GR, Brahim JS. Prospective clinical trial of dental implants in persons with ectodermal dysplasia. J Prosthet Dent. 2002;88:21–5. [PubMed] [Google Scholar]
- 24.Sweeney IP, Ferguson JW, Heggie AA, Lucas JO. Treatment outcomes for adolescent ectodermal dysplasia patients treated with dental implants. Int J Paediatr Dent. 2005;15:241–8. doi: 10.1111/j.1365-263X.2005.00610.x. [DOI] [PubMed] [Google Scholar]
- 25.Thilander B, Odman J, Gröndahl K, Friberg B. Osseointegrated implants in adolescents. An alternative in replacing missing teeth? Eur J Orthod. 1994;16:84–95. doi: 10.1093/ejo/16.2.84. [DOI] [PubMed] [Google Scholar]
- 26.Oesterle LJ. Implant considerations in the growing child. In: Higuchi KW, editor. Orthodontic applications of osseointegrated implants. Chicago: Quintessence Publishing Co; 2000. pp. 133–59. [Google Scholar]
- 27.Singer SL, Henry PJ, Liddelow G, Rosenberg I. Long-term follow-up of implant treatment for oligodontia in an actively growing individual: A clinical report. J Prosthet Dent. 2012;108:279–85. doi: 10.1016/S0022-3913(12)60176-0. [DOI] [PubMed] [Google Scholar]
- 28.Björk A, Skieller V. Growth in width of the maxilla studied by the implant method. Scand J of Plast Reconstr Surg. 1974;8:26–33. doi: 10.3109/02844317409084367. [DOI] [PubMed] [Google Scholar]
- 29.Gandini LG, Jr, Buschang PH. Maxillary and mandibular width changes studied using metallic implants. Am J Orthod Dentofacial Orthop. 2000;117:75–80. doi: 10.1016/s0889-5406(00)70251-4. [DOI] [PubMed] [Google Scholar]
- 30.Itthagarun A, King NM. Ectodermal dysplasia. A review and case report. Quintessence Int. 1997;28:595–602. [PubMed] [Google Scholar]
- 31.Finnema KJ, Raghoebar GM, Meijer HJ, Vissink A. Oral rehabilitation with dental implants in oligodontia patients. Int J Prosthodont. 2005;18:203–9. [PubMed] [Google Scholar]


