Abstract
Despite many important efforts to increase equity in the US health care system, not all Americans have equal access to health care—or similar health outcomes. With the goal of lowering costs and increasing accessibility to health care, the nation’s new health care reform legislation includes certain provisions that expand health insurance coverage to uninsured and underinsured populations, promote medical homes, and support coordination of care. These provisions may help narrow existing health care disparities. Many of the most vulnerable patients, however, may continue to have difficulty accessing and navigating the complex US health care delivery system. This article explores the unique role that patient navigation can play in improving health outcomes for racial and ethnic minorities, as well as other underserved populations, in the context of a changing healthcare environment. Patient navigators can not only facilitate improved health care access and quality for underserved populations through advocacy and care coordination, but they can also address deep-rooted issues related to distrust in providers and the health system that often lead to avoidance of health problems and non-compliance with treatment recommendations. By addressing many of the disparities associated with language and cultural differences and barriers, patient navigators can foster trust and empowerment within the communities they serve. Specific patient navigator activities are discussed, and metrics to evaluate program efforts are presented.
Keywords: health care disparities, patient navigation, outcome measures, health care reform
INTRODUCTION
Health disparities are differences, or inequalities, in health outcomes and their determinants within and across countries and communities, as defined by social, demographic, environmental, and geographic attributes. Many different segments of our society are affected by disparities, including racial and ethnic minorities, residents of rural areas, women, children, elderly, and persons with disabilities.
Several agencies of the Department of Health and Human Services collect and disseminate information regarding health and health care in America. The Centers for Disease Control and Prevention’s National Center for Health Statistics and the Agency for Healthcare Research and Quality’s National Healthcare Quality and National Healthcare Disparities reports, as well as the Medical Expenditure Panel Survey and Healthcare Cost and Utilization Project provide detailed information on health outcomes and health care delivery in the United States. In addition, organizations such as the Institute of Medicine (IOM) provide unbiased reviews and recommendations on health disparities. The American Cancer Society has prioritized the elimination of cancer health disparities by 2015, and Healthy People 2010 also includes goals related to cancer and many other diseases. However, despite all that is known about the nation’s health, how health is perceived, how it is intricately related to socioeconomic status, and how it is deeply affected by cultural influences and personal choices, the gap between knowledge and effective action to address this national crisis remains widely open and a challenge for the 21st century.
In March 2010, the United States achieved the long-desired but daunting challenge of establishing legislation, the Patient Protection and Affordable Care Act (PPACA Public Law 111 – 148), that aims to overhaul our health care system. Although imperfect and controversial in many ways, it represents the first step toward achieving a more equitable health care system for all Americans. In addition to prioritizing affordability, accessibility, and accountability, the new law also promises to tackle disparities in health and health care.
This article considers the role of patient navigation as a tool in the health care delivery armamentarium that can help to narrow health disparities in the new era of US health care reform.
Health Care Disparities: Historical Perspective
From the country’s inception, the framework for health disparities in the US has revolved primarily around race and ethnicity. W.E.B. Du Bois was among the first to recognize the link between health and socioeconomic status when he published The Philadelphia Negro, which highlighted factors such as low economic and social status, employment, education, leadership, and the black church as contributing to the individual health status. In the area of cancer, the landmark report by Henschke et al1 documented an alarming increase in cancer mortality in the US black population, noting a 20% increase from 1950 to 1967. Throughout the 1980s and 1990s, a series of studies strongly demonstrated the nexus between cancer and social, economic, and cultural factors. Researchers began documenting cancer statistics for racial and ethnic minorities in the 1990s, and by 1995 it was clear that some cancers were more virulent among certain racial/ethnic populations.
In the 21st century, we have continued important efforts to identify, understand, and document health disparities in America. We know that racial, cultural, and socioeconomic disparities in access, utilization, and delivery of services are major contributors to disparities in health outcomes. In this generation, the proposed framework for research includes 3 pillars: transdisciplinary research, community engagement, and translation of evidence-based practice.2 It is in this generation that patient navigation has the opportunity to play its role. Indeed, more than a dozen programs across the country have been instituted to scientifically test the hypothesis that patient navigation can reduce barriers to care and improve outcomes.
Using a Biopsychosocial Approach to Address Health Disparities
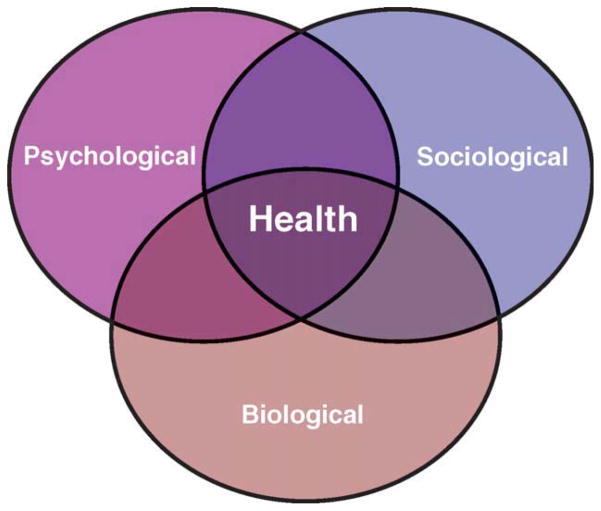
Developed by American psychiatrist George Engel in 1977, the biopsychosocial model (Fig. 1) provides a novel comprehensive approach to understand the health of an individual and outlines the need to consider additional contributing elements to maintaining health.3 According to Engel, “a medical model must also take into account the patient, the social context in which he lives, and the complementary system devised by society to deal with the disruptive effects of illness, that is, the physician role and the health care system.” Engel suggested that the institution and establishment of medicine as a discipline evolved as a result of the societal need to address disease and illness.3 Therefore, the biopsychosocial perspective proposes that health and health services are intrinsically steeped in societal factors and needs.3 For example, disruptions in psychological and biological well-being interpreted by the patient or their family are often what drive patients to seek out a diagnosis and/or treatment.3,4 Furthermore, sociological and psychological factors can affect a patient’s ability to access and/or adhere to treatment.3,4 The assumption that societal, psychological, and biological factors individually and, more important, collectively can influence disease morbidity and mortality makes the biopsychosocial model an appropriate lens through which health disparities should be addressed.
Figure 1.
A biopsychosocial model of health and illness is depicted as a Venn diagram.
Although Engel’s proposal for a “new medical model” was not specifically intended to address health disparities as we have come to understand them, it provides a comprehensive framework. This framework embraces the recognition that health is affected by a complex of social, psychological, biological, environmental, and societal factors.3 In 1999, Congress commissioned the IOM to assess disparities in the kinds of quality of health care received by the US population. In a 2000 report on health care quality, the IOM maintained that problems in patient-physician relationships and gaps in communication contribute significantly to avoidable medical errors, even up to death.5 The biopsychosocial model is crucial to understanding and addressing health disparities because health disparities are often associated with factors that extend beyond biological differences and contribute to disproportionate disease morbidity and mortality rates.6 Potential sources of disparities in care include: 1) health systems factors, 2) patient-level factors, and 3) disparities arising from the clinical encounter. Access to proper and timely medical care, poor quality of care, lack of insurance coverage, and limited knowledge of the health care system are serious contributors to the health status of the population. Among those patient-level factors, poverty, low literacy, lack of access, lack of trust in the system, and emotional stressors play a significant role in the health outcome of the individual (Fig. 1).
The IOM continued to build upon this framework when it released the landmark report, Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care.7 In the report, the IOM committee focused primarily on: 1) issues related to the operational, legal, and regulatory environment of health care systems, and 2) discrimination (bias, prejudices, and stereotyping), as well as clinical uncertainty at the patient-provider level as key contributors to health disparities. The committee’s report presented an integrated model for examining health disparities that demonstrates how internal and external characteristics, or determinants of health, impact the patient’s interaction with providers and other resources within the health system, and how these factors ultimately influence health outcomes. The theory that health outcomes are significantly influenced by complex, integrated, and overlapping structures and systems—including social factors (socioeconomic status, educational and job opportunities, social support mechanisms), health system factors (insurance coverage, access to a usual source of care provider, ease of access to health care services determined by availability of health professionals, hospitals, and other providers), and environmental factors (housing, segregation, neighborhood violence, food)—are well documented in literature examining the determinants of health.8–10 The biopsychosocial model can enhance this integrated, individual-level perspective approach from beginning to end, by the coalescing of a multidisciplinary effort drawing from science, the affected population, and the community to improve health.11
The Persistence of Health Disparities
Although there has been some focus on addressing inequalities in these areas, racial and ethnic disparities in health care access, as well as in evidence-based processes of care and health outcomes, persist. For example, the percentage of blacks and Hispanics living below the poverty level exceeds 25% for both groups compared with 9.4% for whites, according to the most recent data from the US Census Bureau (Table 1). High school drop-out rates are also higher for blacks (9.9%), American Indian/Alaskan Natives (14.6%), and Hispanics (18.3%) compared with whites (4.8%). Blacks also experience higher unemployment rates (16% vs 12.5% for whites) and report lower rates of being married with a spouse in the home (30.1% for blacks and 42.7% for Hispanics compared with 54.6% for whites). Non-elderly American Indian/Alaskan Natives report the highest rates of being covered by public insurance only (63.4% compared with 30.1% for whites). Non-elderly Hispanics also report high rates of public insurance (57.7%), as well as the highest rates of being discontinuously insured (44.6% compared with 25.7% for whites) and rates of being uninsured all year (28.6% compared with 14.4% for whites). Access to a usual source of care provider is similar among the groups, with the exception of Hispanics, who also report the highest rates of experiencing difficulty getting needed care and lower rates of always getting appointments for care as soon as desired compared with whites. These findings are consistent with the literature about the impact of insurance type and continuity on access to care.12–17
Table 1.
Racial/Ethnic Disparities in Selected Determinants of Health
| Measure | Race/Ethnicity %
|
||||
|---|---|---|---|---|---|
| White (SE) | Black (SE) | Asian (SE) | AI/AN (SE) | Hispanic (SE) | |
| % below poverty levela | 9.4 | 25.8 | 12.5 | NA | 25.3 |
| % high school dropouts, 2008b | 4.8 | 9.9 | 4.4 | 14.6 | 18.3 |
| % unemployed (2010)c | 8.7 | 16.0 | 7.5 | NA | 12.5 |
| % married (spouse present)d | 54.6 | 30.1 | 58.7 | NA | 42.7 |
| Health insurance (age <65 y)e | |||||
| % public insurance only | 30.1 (0.5) | 47.2 (1.0) | 26.5 (1.4) | 63.4 (5.1) | 57.7 (0.9) |
| % any private insurance | 69.7 (0.5) | 51.8 (1.0 | 73.2 (1.4) | 36.4 (5.1) | 26.6 (2.2) |
| % uninsured all year | 14.4 (0.4) | 14.6 (0.7) | 12.9 (2.2 | 20.5 (3.3) | 28.6 (0.9) |
| % discontinuously insured | 25.7 (0.6) | 28.5 (1.0) | 22.1 (2.8) | 37.7 (4.1) | 44.6 (1.0) |
| % Usual source of care providere | 86.4 (0.3) | 85.9 (0.6) | 87.6 (0.9 | 81.0 (3.8) | 77.4 (0.8) |
| Limited English proficiencye | |||||
| % with usual source of care | 36.3 (2.1) | NAh | 31.2 (5.3) | NAh | 53.3 (2.0) |
| % with language assistance | 42.3 (2.0) | NAh | 57.0 5.7) | NAh | 41.2 (2.0) |
| % without language assistance | 5.5 (1.1) | NAh | 11.8 (3.4) | NAh | 10.0 (2.7) |
| Timeliness of caree | |||||
| % Difficulty getting care when neededf | 55.8 (1.8) | 55.6 (3.7) | NAh | NAh | 66.0 (3.7) |
| % “Always” received appointment for routine care as soon as wantedf | 49.0 (0.6) | 50.1 (1.6) | 35.1 (3.1) | NAh | 35.1 (3.1) |
| % “Always” received appointment for illness/injury/condition as soon as wantedf | 60.2 (0.8) | 58.0 (2.0) | 45.6 (4.9) | NAh | 20.6 (1.6) |
| % Patient-centerednesse,g | 57.3 (0.5) | 63.0 (1.0) | 49.6 (2.5) | 59.2 (6.9) | 54.2 (1.3) |
| % Utilizatione | |||||
| % with at least 1 office-based or outpatient visite | 75.3 (0.5) | 65.7 (1.0) | 62.7 (2.6) | 70.7 (4.2) | 59.1 (0.9) |
Abbreviations: AI, American Indian; AN, Alaska native; NA, not available; SE, standard error.
Source: US Census. People and Families in Poverty by Selected Characteristics, 2008 and 2009.
The status dropout rate is the percentage of 16- to 24-year-olds who are not enrolled in high school and who lack a high school credential. A high school credential includes a high school diploma or equivalent credential such as a General Educational Development (GED) certificate. Source: US Department of Education, National Center for Education Statistics. The Condition of Education 2010 (NCES 2010-028), Indicator 20.
Source: Bureau of Labor Statistics. Current Population Survey, Household Data Annual Averages, 2010. In 2010, unemployment was 15.2% for American Indians and 21.3% for Alaska natives, according to the Economic Policy Institute.
Source: US Census Bureau. Marital Status of People 15 Years and Over, by Age, Sex, Personal Earnings, Race, and Hispanic Origin, 2010.
Source: Agency for Healthcare Research and Quality. National Healthcare Disparities Report, 2009.
Within 12 months of survey.
Adults who had a doctor’s office or clinic visit in the last 12 months whose health providers always listened carefully, explained things clearly, respected what they had to say, and spent enough time with them.
Data do not meet the criteria for statistical reliability, data quality, or confidentiality.
Many of the socioeconomic disparities—including race and ethnicity—associated with reduced or unsatisfactory access to care are also prominent when examining cancer processes of care and outcomes. As noted in Table 2, although black women have mammography and Pap test rates similar to those of white women, they experience higher rates of advanced-stage breast cancer and mortality. Hispanic women report Pap test rates similar to those of white women, but they experience higher rates of advanced-stage cervical cancer and mortality. Racial and ethnic minorities also report lower rates of colorectal cancer screenings (fecal occult blood test or colonoscopy/sigmoidoscopy/proctoscopy), but only blacks experience higher rates of advanced-stage disease and mortality compared with whites. Mortality for all cancer types, prostate and lung cancers, are also highest among blacks and account for the majority of the racial/ethnic disparities. Blacks, compared with whites, report similar rates of receiving smoking cessation and exercise counseling but lower rates of diet and nutrition counseling. Hispanics report lower rates of counseling for all 3 lifestyle modifications compared with whites. Access to hospice care and hospice-delivered pain medications were similar for whites and racial/ethnic minorities, although racial/ethnic minorities reported lower rates of having their end-of-life wishes met.
Table 2.
Percent of Racial/Ethnic Disparities in Selected Cancer Health Outcomes and Processes of Care
| Measure | Race/Ethnicity %
|
Hispanic (SE) | |||
|---|---|---|---|---|---|
| White (SE) | Black (SE) | Asian (SE) | AI/AN (SE) | ||
| Breast cancer | |||||
| Mammographya | 67.3 (0.6) | 64.3 (1.6) | 54.0 (3.5) | 67.1 (7.4) | 58.9 (1.7) |
| Advanced-stage breast cancerb | 93.7 (0.8) | 111.1 (2.6) | 64.3 (1.9) | 40.3 (4.8) | 73.0 (1.8) |
| Radiation therapy ≤1 y after breast-conserving surgeryc | 76.5 (0.3) | 68.5 (0.9) | 72.5 (1.6) | NAd | 61.6 (1.3) |
| Breast cancer mortalitye | 22.9 (0.1) | 31.6 (0.4) | 12.1 (0.4)f | 12.8 1.0) | 15.0 (0.3) |
| Cervical cancer | |||||
| Pap smearg | 78.2 (0.4) | 80.0 (1.0) | 63.9 (2.7) | 71.2 (5.5) | 74.4 (1.1) |
| Advanced-stage cervical cancerh | 11.0 (0.2) | 13.1 (0.7) | 9.9 (0.6)f | NAd | 16.5 (0.6) |
| Cervical cancer mortalitye,i | 2.2 | 4.3 | 2.0 | 2.3 | 4.0 |
| Colorectal cancer | |||||
| Fecal occult blood testj | 17.4 (0.5) | 15.7 (1.2) | 12.9 (2.3) | NAd | 12.1 (1.3) |
| Colonoscopy/sigmoidoscopy/ proctoscopyk | 51.2 (0.6) | 42.6 (1.6) | 34.2 (3.1) | 32.3 (9.0) | 32.3 (1.8) |
| Advanced-stage colorectal cancerl | 77.1 (0.7) | 97.1 (2.4) | 64.2 (1.9)f | 50.2 (5.5) | 65.8 (1.8) |
| Colorectal cancer mortalitye | 16.7 (0.1) | 24.3 (0.3) | 10.9 (0.3) | 11.2 (0.8) | 12.6 (0.2) |
| Other cancers | |||||
| Prostate cancer mortalitye | 21.7 (0.1) | 50.5 (0.8) | 9.6 (0.5) | 14.4 (1.5) | 18.1 (0.5) |
| Lung cancer mortalitye | 52.1 (0.1) | 56.8 (0.5) | 25.2 (0.5) | 31.2 (1.3) | 20.7 (0.3) |
| All cancer mortalitye | 179.9 (0.3) | 217.4 (0.9) | 106.5 (1.0) | 119.4 (2.5) | 118.0 (0.8) |
| Lifestyle modification | |||||
| Smoking-cessation counseling | 63.8 (1.5) | 66.9 (2.5) | NAd | NAd | 53.4 (3.8) |
| Exercise counseling | 59.0 (1.0) | 56.6 (1.6) | NAd | NAd | 48.5 (1.9) |
| Diet/nutrition counseling | 51.5 (1.0) | 44.5 (1.7) | NAd | NAd | 42.2 (1.6) |
| Palliative care | |||||
| Appropriate hospice referral | 88.0 (0.1) | 89.4 (0.6) | 90.5 (1.1) | 85.2 (1.5) | 87.8 (0.7) |
| Hospice patients: appropriate pain medication | 94.6 (0.1) | 91.6 (0.6) | 89.4 (1.3) | 92.8 (1.2) | 93.0 (0.6) |
| Hospice patients: end-of-life care wishes met | 94.7 (0.1) | 88.0 (0.8) | 83.5 (1.6) | 87.3 (1.7) | 89.1 (0.8) |
Abbreviations: AI, American Indian; AN, Alaska native; NA, not available; SE, standard error. Source: Agency for Healthcare Research and Quality. National Healthcare Disparities Report, 2009.
Percent of women ≥40 years who received a mammogram within past 2 years.
Breast cancer diagnosed at advanced stage (regional, distant stage, or local stage with tumor >2 cm) per 100,000 women aged ≥40 years.
Women <70 years treated for breast cancer with breast-conserving surgery who received radiation therapy to the breast within 1 year of diagnosis.
Data do not meet the criteria for statistical reliability, data quality, or confidentiality.
Per 100,000 female population per year.
Includes Asians and Native Hawaiian/Pacific Islanders.
Women ≥18 years who received a Pap smear within past 3 years.
Cervical cancer diagnosed at advanced stage (all invasive tumors) per 100,000 women ≥20 years.
Source: Centers for Disease Control and Prevention.
Adults ≥50 years who received a fecal occult blood test (FOBT) within past 2 years.
Adults ≥50 years who ever received a colonoscopy, sigmoidoscopy, or proctoscopy.
Colorectal cancer diagnosed at advanced stage (tumors diagnosed at regional or distant stage) per 100,000 population adults ≥50 years.
Patient Navigation as a Tool to Reduce Disparities in Health and Health Care
Unfortunately, communities with the highest proportions of racial/ethnic minorities are considered among the most vulnerable to reduced health care access and quality. These communities also tend to be burdened with other socioeconomic barriers to care, including high rates of uninsured and medically indigent populations. Appropriate mammography utilization has been shown to be of particular importance to racial/ethnic minorities—most specifically black women, who are often less likely than white women to receive adequate screening and follow-up diagnostic mammography than white women and have higher prevalence of advanced breast tumors but whose advanced cancer rates may be attenuated or eliminated when stratified by screening history.18,19 Women who are immigrants and those with lower incomes, with less education, without insurance, and lacking a usual health care provider are less likely to get screening mammograms but continue to have high rates of mortality.20,21 In addition, older, poor, less educated, and immigrant women are less likely to be screened for cervical cancer.20 Among Hispanic women, key barriers to cervical cancer screening include language/communication barriers, continuity of care, cultural barriers/lack of knowledge, and low socioeconomic status.22 These barriers, particularly language/communication barriers, have also been linked to reduced access to preventive screening tests for women of other races/ethnicities (in addition to Hispanic women).23,24 Racial and ethnic disparities in actual and perceived barriers to health care access and quality are also evident in the continuum of care for other cancers, including colorectal and lung cancers.25–27 These and other studies offer evidence that, in addition to racial and ethnic minorities, low-income individuals and families, women, children, young adults, the elderly, residents of rural areas, and individuals with disabilities or special health care needs (such as childhood cancer survivors transitioning to adulthood) may potentially benefit from individualized assistance to overcome health care system barriers and facilitate timely access to quality medical and psychosocial care from pre-diagnosis through all phases of the cancer experience.28 Patient navigation, therefore, using a biopsychosocial approach to providing a comprehensive range of health care services and support, represents a potentially powerful tool in the arsenal to target health disparities.
What Disparities Are Amenable to Patient Navigation?
Provisions of the Affordable Care Act address 4 key issues important to reducing health disparities in the United States, all of which are amenable to improved implementation through patient navigation: prevention and early detection; health care access and coordination; insurance coverage and continuity; and diversity and cultural competency.29
Prevention and early detection
Appropriate utilization of cancer screening tests has increased for all races/ethnicities over the past 2 decades but still falls short of Healthy People 2010 goals.20 Major national policy initiatives—for example, the National Breast and Cervical Cancer Early Detection Program (NBCCEDP) to provide breast and cervical cancer screening services to underserved women, as well as the Cancer Prevention and Treatment Act of 2000 authorizing states to provide medical assistance through Medicaid to eligible women who were screened through the NBCCEDP and diagnosed with breast or cervical cancer—have likely played a role in narrowing these differences.30 Disparities persist, however, particularly for immigrants and those with lower incomes, with less education, without insurance, and without a usual health care provider.20
Patient navigators can help bridge the gaps between racial/ethnic groups related to compliance with evidence-based guidelines for cancer prevention and early detection. Patient navigators can facilitate access to the system for underserved populations by connecting them to resources most appropriate for each patient’s individual needs—including access to Federally Qualified Health Centers (FQHCs), which tend to be major providers of preventive care and screening services to racial/ethnic minorities and other underserved populations. Patient navigation has been shown to be a critical component in helping racial/ethnic minorities gain access to FQHCs, as well as to other safety net facilities, which provide not only direct screening, diagnostic, and treatment services but also public education and outreach to facilitate disease prevention.31–35 In addition, because many cancer screening guidelines vary based on family history and personal risk factors, navigators can offer individualized advice regarding screening services that may improve compliance by increasing patients’ cancer knowledge and risk perception.36–38 Additional studies to investigate the effectiveness of patient navigation as a mechanism to reduce cancer health disparities are under way.39
Health care access and coordination
Access to care refers to entry into or use of the health care system, or the factors influencing entry or use. This may be measured by structural factors that facilitate health care, such as having health insurance or a usual source of care (USOC) provider; patient perceptions of their ability to gain access to health care services (ie, difficulties or delays in obtaining care or receiving appointments for care as soon as desired); and actual utilization of health care services, such as visits to physicians or use of hospital inpatient or ambulatory care services.40 Significant racial/ ethnic disparities in health care access have been well documented.41 People with a usual source of care, however, are more likely to receive appropriate preventive health services.42,43
The PPACA contains several provisions to improve health care access for racial/ethnic minorities and other underserved populations, including providing planning grants to states to facilitate promotion of medical homes for Medicaid enrollees with chronic conditions; funding for community-based interdisciplinary teams to provide support services to primary care practices; and funding for consortiums of health care providers to coordinate and integrate health care services for low-income uninsured and underinsured populations (Pub. L. 111–118). These additional resources will contribute to the existing care continuum, which includes a provider or team of providers responsible for comprehensive case management, care coordination and health promotion, transitional care, patient and family support, and referral to community services.
But health care systems are laden with complexity. Navigators, who operate best in their local environment, are brokers with the ability to confront health system and environmental barriers that tend to disproportionately burden racial and ethnic minorities. These barriers include financial and insurance issues, paperwork and documentation, cultural beliefs and language barriers, as well as issues related to transportation, childcare, and neighborhood resources. Patient navigators, therefore, may play a critical role in coordinating access to a comprehensive continuum of services by tailoring their assistance to help vulnerable patients identify a medical home, by facilitating communication and cooperation between providers, and by providing the patient education and support necessary to increase access to care and their ability to comply with prescribed therapies.44–46
Insurance coverage and continuity
Racial and ethnic minorities, as well as people with low incomes, are disproportionately uninsured or underinsured. One of the most significant elements in the PPACA is the expansion of Medicaid to cover most individuals up to 133% of the federal poverty level, as well as the development of health insurance exchanges. This is important to addressing health disparities because health insurance facilitates entry into the health care system.14 Uninsured individuals report more problems getting care, are diagnosed at later disease stages, and get less therapeutic care.12,47,48
Navigators can play an important role in not only helping patients gain consistent access to insurance through publicly-funded programs such as Medicaid but also in helping them to remain consistently insured.49,50 In addition, patient navigators may advocate on behalf of patients who have historically experienced insurance discrimination, which is banned under PPACA, so sicker individuals will no longer be excluded from coverage or charged higher premiums. Finally, navigators may play a role in advising patients—particularly those facing severe health literacy issues—regarding their selection of health insurance plans and in completing necessary applications.
Diversity and cultural competency
Factors beyond biological differences, including cultural beliefs, language, acculturation, nativity status, and health beliefs, often contribute to disparities in health outcomes and health-seeking behavior.51–53 For example, studies have consistently found that black and Hispanic participants report higher rates of distrust and feeling disrespected by the health care system and health care providers.54–56 Distrust in health care services and providers contributes significantly to delays in treatment services, the receipt of less than quality services, and increased rates of nonadherence to treatment.54,56 Similarly, participants who feel disrespected by the health care system and providers are less likely to be compliant with treatment and are more likely to put off getting medical services.56 Patient navigation services are ideal to address many of the disparities associated with diversity and culture because they foster trust and empowerment within the communities they serve.57,58
In their study of patients who received navigation services, Carroll et al identify providing emotional support, “being there,” and providing helpful information as the most important services received.59 These findings highlight the importance of trust in the patient/navigator relationship. In the study, patients recognized the navigator as existing in two worlds, one as an insider to the health care system and the other as a caring companion.59 As an insider, the navigator is able to provide patients useful information to assist in accessing and navigating the health care system.10 In their other role, the patient navigator is a supportive ally to the patient.57,59 Patient navigators have the unique opportunity to establish trust with patients and are the link that will help to extend that trust from the patient/navigator relationship to the larger health care system.57,59 In conjunction with increasing utilization of medical and screening services, patient navigation services have been shown to decrease the anxiety associated with medical treatment and increase patient satisfaction with services received among underserved populations.45,57 Underserved populations who receive patient navigation services report fewer disruptions in care and are more likely to complete required treatment.57 Many of the studies attribute these positive findings to the use of representative community members as patient navigators.57,58 The use of representative community members as navigators cultivates trust between the patient and the navigator and the health care system they will be engaging. Community member navigators can be a resource in addressing issues related to language, and they can also be instrumental in communicating and promoting acceptance of cultural differences to service providers.57 The benefits of applying patient navigator services to address health disparities related to diversity and cultural competence are essentially limitless: “The navigator acts as a bridge between two worlds—the fragmented, poorly coordinated health care system and the complex biopsychosocial needs of cancer patients, especially those who are underserved.”59 The opportunity for patient navigators to utilize the biopsychosocial approach to serve diverse patient populations will be expanded and strengthened by the Patient Protection and Affordable Care Act, which will expand initiatives to increase racial and ethnic diversity in the health care professions, strengthen cultural competency training for all health care providers, and require health plans to use language services and community outreach in underserved communities (Table 3).
Table 3.
Navigation Activities to Reduce Health Disparities
| Health Disparities | Navigator Activities to Reduce Disparities | Metrics and Data Sets |
|---|---|---|
| Preventive care/early detection | Educate patients regarding screening guidelines appropriate for their status | For racial/ethnic minorities: |
| Timely cancer screenings | Identify providers and/or programs to perform screenings as needed | Increased likelihood of screening according to guidelines (eg, likelihood of mammography within 2 y for women age ≥40 y, or % of women age ≥40 y screened within past 2 y, by race/ethnicity |
| Early-stage disease detection | Educate patients regarding early signs/symptoms of cancer | Cancer diagnosed at early stage |
| Population cancer rates, by race ethnicity | Reduction in differences between cancer rates, by race/ethnicity | |
| Mortality | Cancer deaths per 100,000 population per year | |
| Data sets: MEPS, NHIS, CHIS, HEDIS, SEER, NIS, MI | ||
| Healthcare access and coordination | Assist patients with identifying a primary care “medical home” | For racial/ethnic minorities: |
| Medical home or USOC | Assist with facilitating appointments as needed | Increased likelihood of having USOC or medical home |
| Annual physical exam | Assist with facilitating ancillary care, medications, equipment as needed | Increased likelihood of at least 1 visit during year |
| Perceived patient-provider relationship (trust, communication, etc.) | Provide/coordinate patient education | Decreased comorbidities (such as diabetes and cardiovascular disease) |
| Perceived and actual ability to obtain timely, needed care at all levels | Assist with transportation to appointments as needed | Increased likelihood of perceiving provider listened, respected, showed respect, and spent enough time with patient |
| Access to evidence-based care | Decreased likelihood of perceiving problems obtained needed care | |
| Compliance with provider recommendations | Increased cancer knowledge and appropriate risk perception | |
| Increased likelihood of exercise and nutrition counseling | ||
| Increased likelihood and/or increased mean values of physical activity/hours, eating fruits and vegetables/servings % of population receiving evidence-based continuum of care for their condition | ||
| Increased likelihood of receiving appropriate end-of-life care Data sets: MEPS, NHIS, CHIS NAMCS, NHANES, HINTS, MCBS, HEDIS, SEER, NHHCS |
||
| Insurance coverage | Determine eligibility for Medicaid, Medicare, and other public programs | For racial/ethnic minorities: |
| Insurance coverage | Provide forms and assist with completion | Increased likelihood of being insured |
| Insurance continuity | Monitor eligibility renewal dates as needed, and follow up/assist with renewal to ensure insurance continuity | Increased likelihood of being continuously insured all year |
| Assist with identifying/advocating for patient for coverage of needed services | Reduced likelihood of reporting problems receiving care | |
| Assist patient with selecting/applying for health insurance | Increased % of population receiving evidence-based continuum of care for their condition | |
| Data sets: MEPS, NHIS, CHIS, NAMCS, HEDIS, SEER, NIS | ||
| Diversity and cultural competency | Can organize or provide translation services | For racial/ethnic minorities: |
| Language barriers | Serve as support for medical visits | Increased likelihood of perceiving provider listened, showed respect, and spent enough time with patient |
| Conflicting cultural views | Assist patient/physician with communicating expectations, needs, and perspectives | Increased likelihood of receiving language assistance (when needed) |
| Patient vs physician perspective of disease | Coordinate medical visits | Increased health-literacy scores |
| Patient perspective of health care services | Identify and access community resources | Data sets: MEPS, NHIS, CHIS, CAHPS, HINTS |
| Differences in perspectives of self/family care | ||
| Trust | ||
| History of experience with healthcare services |
Abbreviations: CAHPS, Consumer Assessment of Healthcare Providers and Systems; CHIS, California Health Interview Survey; HEDIS, Healthcare Effectiveness Data and Information Set; HINTS, Health Information National Trends Survey; MCBS, Medicare Current Beneficiary Survey; MEPS, Medical Expenditure Panel Survey; MI, Mortality Index; NAMCS, National Ambulatory Medical Care Survey; NCI-SEER, National Cancer Institute-Surveillance Epidemiology and End Results; NHANES, National Health and Nutrition Examination Survey; NHHCS, National Home and Hospice Care Survey; NHIS, National Health Interview Survey; NIS, National Inpatient Sample; USOC, usual source of care.
Conclusions
Despite many important efforts to increase equity in the US health care system, not all Americans have equal access to health care—or similar health care outcomes. Low-income Americans, racial and ethnic minorities, and other underserved populations often have higher rates of disease, fewer treatment options, and reduced access to care. Patient navigation is a clinical tool that, when applied in the context of a biopsychosocial approach to health, particularly among ethnic populations, can play a significant role in improving individual and population health. Navigators are uniquely positioned to play an integral role in the changing environment of health care delivery by facilitating access to care, as well as addressing language and cultural barriers. Patient navigators can break through literacy barriers (including health literacy and functional health literacy), build trust, reduce fear, and support the improvement of patient-provider communication. In doing so, navigators can plan an integral role in the changing environment of health care delivery, with the potential to help in delivering better quality and more efficient care and ensuring that access to care is for all.
Acknowledgments
FUNDING SOURCES
This conference and supplement were cosponsored by Pfizer Oncology, Livestrong (Lance Armstrong Foundation), Susan G. Komen for the Cure, the Oncology Nursing Society (ONS), the American College of Surgeons Commission on Cancer, the American Cancer Society, and AstraZeneca.
Footnotes
National Patient Navigator Leadership Summit (NPNLS): Measuring the Impact and Potential of Patient Navigation, Supplement to Cancer.
The articles in this supplement are based on presentations at the “National Patient Navigator Leadership Summit”; March 23–24, 2010; Atlanta, GA.
The opinions or views expressed in this supplement are those of the authors, and do not necessarily reflect the opinions or recommendations of the publisher, the editors, the University of Illinois at Chicago, the American Cancer Society, or the Ralph Lauren Center for Cancer Care and Prevention.
CONFLICT OF INTEREST DISCLOSURES
The authors made no disclosures.
References
- 1.Henschke UK, Leffall LD, Mason CH, Reinhold AW, Schneider RL, White JE. Alarming increase of the cancer mortality in the U.S. black population (1950–1967) Cancer. 1973;31:763–768. doi: 10.1002/1097-0142(197304)31:4<763::aid-cncr2820310401>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 2.Thomas S, Crouse-Quinn S. Poverty and the Elimination of Urban Health Disparities: Challenge and Opportunity. Ann NY Acad Sci. 2008;1136:111–125. doi: 10.1196/annals.1425.018. [DOI] [PubMed] [Google Scholar]
- 3.Engel GL. The need for a new medical model: a challenge for biomedicine. J Interprofessional Care. 1989;4:37–53. [Google Scholar]
- 4.Engel G. From biomedical to biopsychosocial. Being scientific in the human domain. Psychosomatics. 1997;38:521–528. doi: 10.1016/S0033-3182(97)71396-3. [DOI] [PubMed] [Google Scholar]
- 5.Hurtado MP, Swift EK, Corrigan JM. Envisioning the National Health Care Quality Report. Washington, DC: Institute of Medicine; 2000. [PubMed] [Google Scholar]
- 6.Yamada S, Greene G, Bauman K, Maskarinec G. A biopsychosocial approach to finding common ground in the clinical encounter. Acad Med. 2000;75:643–648. doi: 10.1097/00001888-200006000-00017. [DOI] [PubMed] [Google Scholar]
- 7.Smedley B, Stith A, Nelson A. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: Institute of Medicine; 2002. [PubMed] [Google Scholar]
- 8.Marmot M. Social determinants of health inequalities. Lancet. 2005;365:1099–1104. doi: 10.1016/S0140-6736(05)71146-6. [DOI] [PubMed] [Google Scholar]
- 9.Andersen R, Newman JF. Societal and Individual Determinants of Medical Care Utilization in the United States. Milbank Q. 2005;83:1–28. [PubMed] [Google Scholar]
- 10.Berkman LF. Social epidemiology: social determinants of health in the United States: are we losing ground? Annu Rev Public Health. 2009;30:27–41. doi: 10.1146/annurev.publhealth.031308.100310. [DOI] [PubMed] [Google Scholar]
- 11.King D, Miranda P, Gor B, et al. Addressing cancer health disparities using a global biopsychosocial approach. Cancer. 2010;116:264–269. doi: 10.1002/cncr.24765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schoen C, DesRoches C. Uninsured and unstably insured: the importance of continuous insurance coverage. Health Serv Res. 2000;35(1 pt 2):187–206. [PMC free article] [PubMed] [Google Scholar]
- 13.Haas J, Adler N. The Causes of Vulnerability: Disentangling the Effects of Race, Socioeconomic Status and Insurance Coverage on Health. Washington, DC: The Institute of Medicine Committee on the Consequences of Uninsurance; 2001. [Google Scholar]
- 14.Hargraves JL, Hadley J. The contribution of insurance coverage and community resources to reducing racial/ethnic disparities in access to care. Health Serv Res. 2003;38:809–829. doi: 10.1111/1475-6773.00148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zuvekas SH, Taliaferro GS. Pathways to access: health insurance, the health care delivery system, and racial/ethnic disparities, 1996–1999. Health Aff. 2003;22:139–153. doi: 10.1377/hlthaff.22.2.139. [DOI] [PubMed] [Google Scholar]
- 16.Lillie-Blanton M, Hoffman C. The role of health insurance coverage in reducing racial/ethnic disparities in health care. Health Aff. 2005;24:398–408. doi: 10.1377/hlthaff.24.2.398. [DOI] [PubMed] [Google Scholar]
- 17.Greene J, Blustein J, Weitzman B. Race, segregation, and physicians’ participation in Medicaid. Milbank Q. 2006;84:239–272. doi: 10.1111/j.1468-0009.2006.00447.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Elkin E, Ishill N, Snow J, et al. Geographic access and the use of screening mammography. Med Care. 2010;48:349–356. doi: 10.1097/MLR.0b013e3181ca3ecb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Smith-Bindman R, Miglioretti DL, Lurie N, et al. Does utilization of screening mammography explain racial and ethnic differences in breast cancer? Ann Intern Med. 2006;144:541–553. doi: 10.7326/0003-4819-144-8-200604180-00004. [DOI] [PubMed] [Google Scholar]
- 20.Cancer Trends Progress Report-Breast Cancer Screening, 2010. Washington, DC: National Cancer Institute; 2010. [Google Scholar]
- 21.Miranda P, Wilkinson A, Etzel C, et al. Policy implications of early onset breast cancer among Mexican-origin women. Cancer. 2011;117:390–397. doi: 10.1002/cncr.25397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Flores K, Bencomo C. Preventing cervical cancer in the Latina population. J Womens Health. 2009;18:1935–1943. doi: 10.1089/jwh.2008.1151. [DOI] [PubMed] [Google Scholar]
- 23.Ponce N, Chawla N, Babey S, et al. Is there a language divide in Pap test use? Med Care. 2006;44:998–1004. doi: 10.1097/01.mlr.0000233676.61237.ef. [DOI] [PubMed] [Google Scholar]
- 24.Ponce N, Ku L, Cunningham W, Brown E. Language barriers to health care access among Medicare beneficiaries. Inquiry. 2006;43:66–76. doi: 10.5034/inquiryjrnl_43.1.66. [DOI] [PubMed] [Google Scholar]
- 25.Ayanian J, Zaslavsky A, Guadagnoli E, et al. Patients’ perceptions of quality of care for colorectal cancer by race, ethnicity, and language. J Clin Oncol. 2005;23:6576–6586. doi: 10.1200/JCO.2005.06.102. [DOI] [PubMed] [Google Scholar]
- 26.Ayanian JZ, Zaslavsky AM, Arora NK, et al. Patients’ experiences with care for lung cancer and colorectal cancer: findings from the Cancer Care Outcomes Research and Surveillance Consortium. J Clin Oncol. 2010;28:4154–4161. doi: 10.1200/JCO.2009.27.3268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Doubeni CA, Laiyemo AO, Reed G, Field TS, Fletcher RH. Socioeconomic and racial patterns of colorectal cancer screening among Medicare enrollees in 2000 to 2005. Cancer Epidemiol Biomarkers Prev. 2009;18:2170–2175. doi: 10.1158/1055-9965.EPI-09-0104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Freeman H, Muth B, Kerner J. Expanding access to cancer screening and clinical follow-up among the medically under-served. Cancer Pract. 1995;3:19–30. [PubMed] [Google Scholar]
- 29.Dohan D, Schrag D. Using navigators to improve care of underserved patients. Cancer. 2005;104:848–855. doi: 10.1002/cncr.21214. [DOI] [PubMed] [Google Scholar]
- 30.Adams EK, Breen N, Joski PJ. Impact of the National Breast and Cervical Cancer Early Detection Program on mammography and pap test utilization among white, Hispanic, and African American women: 1996–2000. Cancer. 2007;109:348–358. doi: 10.1002/cncr.22353. [DOI] [PubMed] [Google Scholar]
- 31.Breast and Cervical Cancer Legislation. Atlanta, GA: Centers for Disease Control and Prevention; 2010. [Google Scholar]
- 32.Green A, Peters-Lewis A, Percac-Lima S, et al. Barriers to screening colonoscopy for low-income Latino and white patients in an urban community health center. J Gen Intern Med. 2008;23:834–840. doi: 10.1007/s11606-008-0572-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Steinberg ML, Fremont A, Khan DC, et al. Lay patient navigator program implementation for equal access to cancer care and clinical trials. Cancer. 2006;107:2669–2677. doi: 10.1002/cncr.22319. [DOI] [PubMed] [Google Scholar]
- 34.Petereit DG, Molloy K, Reiner M, et al. Establishing a patient navigator program to reduce cancer disparities in the American Indian communities of western South Dakota: initial observations and results. Cancer Control. 2008;15:254–259. doi: 10.1177/107327480801500309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Robinson-White S, Conroy B, Slavish KH, Rosenzweig M. Patient navigation in breast cancer: a systematic review. Cancer Nurs. 2010;33:127–140. doi: 10.1097/NCC.0b013e3181c40401. [DOI] [PubMed] [Google Scholar]
- 36.Powe BD, Cooper DL, Harmond L, Ross L, Mercado FE, Faulkenberry R. Comparing knowledge of colorectal and prostate cancer among African American and Hispanic men. Cancer Nurs. 2009;32:412–417. doi: 10.1097/NCC.0b013e3181aaf10e. [DOI] [PubMed] [Google Scholar]
- 37.Kim SE, Perez-Stable EJ, Wong S, et al. Association between cancer risk perception and screening behavior among diverse women. Arch Intern Med. 2008;168:728–734. doi: 10.1001/archinte.168.7.728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Orom H, Kiviniemi MT, Underwood W, Ross L, Shavers VL. Perceived cancer risk: why is it lower among nonwhites than whites? Cancer Epidemiol Biomarkers Prev. 2010;19:746–754. doi: 10.1158/1055-9965.EPI-09-1085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hendren S, Griggs J, Epstein R, et al. Study protocol: a randomized controlled trial of patient navigation-activation to reduce cancer health disparities. BMC Cancer. 2010;10:551. doi: 10.1186/1471-2407-10-551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.National Healthcare Disparities Report. Rockville, MD: Agency for Healthcare Research and Quality; 2007. [Google Scholar]
- 41.Mayberry RM, Mili F, Ofili E. Racial and ethnic differences in access to medical care. Med Care Res Rev. 2000;57(4 suppl):108–145. doi: 10.1177/1077558700057001S06. [DOI] [PubMed] [Google Scholar]
- 42.DeVoe JE, Fryer GE, Phillips R, Green L. Receipt of preventive care among adults: insurance status and usual source of care. Am J Public Health. 2003;93:786–791. doi: 10.2105/ajph.93.5.786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Corbie-Smith G, Flagg EW, Doyle JP, O’Brien MA. Influence of usual source of care on differences by race/ethnicity in receipt of preventive services. J Gen Intern Med. 2002;17:458–464. doi: 10.1046/j.1525-1497.2002.10733.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ell K, Padgett D, Vourlekis B, et al. Abnormal mammogram follow-up. Cancer Pract. 2002;10:130–138. doi: 10.1046/j.1523-5394.2002.103009.x. [DOI] [PubMed] [Google Scholar]
- 45.Ferrante J, Chen P-H, Kim S. The effect of patient navigation on time to diagnosis, anxiety, and satisfaction in urban minority women with abnormal mammograms: a randomized controlled trial. J Urban Health. 2008;85:114–124. doi: 10.1007/s11524-007-9228-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Dohan D, Schrag D. Using navigators to improve care of underserved patients: current practices and approaches. Cancer. 2005;104:848–855. doi: 10.1002/cncr.21214. [DOI] [PubMed] [Google Scholar]
- 47.Hadley J. Insurance coverage, medical care use, and short-term health changes following an unintentional injury or the onset of a chronic condition. JAMA. 2007;297:1073–1084. doi: 10.1001/jama.297.10.1073. [DOI] [PubMed] [Google Scholar]
- 48.Hadley J. Sicker and poorer—the consequences of being uninsured: a review of the research on the relationship between health insurance, medical care use, health, work, and income. Med Care Res Rev. 2003;60(2 suppl):3S–75S. doi: 10.1177/1077558703254101. [DOI] [PubMed] [Google Scholar]
- 49.Saunders M, Alexander G. Turning and churning: loss of health insurance among adults in Medicaid. J Gen Intern Med. 2009;24:133–134. doi: 10.1007/s11606-008-0861-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Wells KJ, Battaglia TA, Dudley DJ, et al. Patient navigation: state of the art or is it science? Cancer. 2008;113:1999–2010. doi: 10.1002/cncr.23815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Bastida E, Brown HS, III, Pagan JA. Persistent disparities in the use of health care along the US-Mexico border: an ecological perspective. Am J Public Health. 2008;98:1987–1995. doi: 10.2105/AJPH.2007.114447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Kagawa-Singer M, Dadia AV, Yu MC, Surbone A. Cancer, culture, and health disparities: time to chart a new course? CA Cancer J Clin. 2010;60:12–39. doi: 10.3322/caac.20051. [DOI] [PubMed] [Google Scholar]
- 53.Gaskin DJ, Arbelaez JJ, Brown JR, Petras H, Wagner FA, Cooper LA. Examining racial and ethnic disparities in site of usual source of care. J Natl Med Assoc. 2007;99:22–30. [PMC free article] [PubMed] [Google Scholar]
- 54.Dovidio JF, Penner LA, Albrecht TL, Norton WE, Gaertner SL, Shelton JN. Disparities and distrust: the implications of psychological processes for understanding racial disparities in health and health care. Soc Sci Med. 2008;67:478–486. doi: 10.1016/j.socscimed.2008.03.019. [DOI] [PubMed] [Google Scholar]
- 55.Armstrong K, Ravenell KL, McMurphy S, Putt M. Racial/ ethnic differences in physician distrust in the United States. Am J Public Health. 2007;97:1283–1289. doi: 10.2105/AJPH.2005.080762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Blanchard J, Lurie N. R-E-S-P-E-C-T: patient reports of disrespect in the health care setting and its impact on care. J Family Pract. 2004;53:721–730. [PubMed] [Google Scholar]
- 57.Han HR, Lee H, Kim MT, Kim KB. Tailored lay health worker intervention improves breast cancer screening outcomes in non-adherent Korean-American women. Health Educ Res. 2009;24:318–329. doi: 10.1093/her/cyn021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Petereit DG, Molloy K, Reiner ML, et al. Establishing a patient navigator program to reduce cancer disparities in the American Indian communities of Western South Dakota: initial observations and results. Cancer Control. 2008;15:254–259. doi: 10.1177/107327480801500309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Carroll JK, Humiston SG, Meldrum SC, et al. Patients’ experiences with navigation for cancer care. Patient Educ Counseling. 2010;80:241–247. doi: 10.1016/j.pec.2009.10.024. [DOI] [PMC free article] [PubMed] [Google Scholar]