Abstract
Objective
To report the first successful study to date of in vivo electromechanical reshaping of ear cartilage in a rabbit model.
Methods
Ears of New Zealand white rabbits were re-shaped using percutaneous needle electrode electromechanical reshaping (5 V for 4 minutes) and were then bolstered for 4 weeks. Ten ears were treated, with 2 undergoing sham procedures and serving as controls. The treatment was performed using a platinum array of electrodes consisting of 4 parallel rows of needles inserted across the region of flexures in the ear. After 4 weeks, the animals were killed, and the ears were photographed and sectioned for conventional light microscopy and confocal microscopy (live-dead fluorescent assays).
Results
Significant shape change was noted in all the treated ears (mean, 102.4°; range, 87°-122°). Control ears showed minimal shape retention (mean, 14.5°; range, 4°-25°). Epidermis and adnexal structures were preserved in reshaped ears, and neochondrogenesis was noted in all the specimens. Confocal microscopy demonstrated a localized zone of nonviable chondrocytes (<2.0 mm in diameter) surrounding needle sites in all the treated ears.
Conclusions
Electromechanical reshaping can alter the shape of the rabbit auricle, providing good creation and retention of shape, with limited skin and cartilage injury. Needle electrode electromechanical reshaping is a viable technique for minimally invasive tissue reshaping, with potential applications in otoplasty, septoplasty, and rhinoplasty. Further studies to refine dosimetry parameters will be required before clinical trials.
Congenital external ear malformations, including the protruding ear, occur in 5% of the population.1 Such deformities can lead to long-term psychological trauma from childhood onward.1 Because much of the ear growth is complete by age 3 years2 and because the geometry and dimensions of the adult auricular cartilage are reached by age 6 to 7 years,3 surgical correction of the external ear is recommended before the child is of school age, a time at which teasing and ridicule among children begins.
The underdeveloped antihelix and a large conchal bowl are 2 underlying malformations that require surgery. Classic otoplasty seeks to address these 2 conditions. Otoplasty is a technically demanding procedure, with a steep learning curve in which poor aesthetic outcomes or failure is common. The lack of consensus on a single effective otoplasty technique has led to the development of more than 40 different operations.4 Of these, the corrective method found to be most appropriate has been approached subjectively, with minimal quantifiable data.5 To overcome the limitations of conventional surgery, minimally invasive reshaping techniques (including laser,6 radiofrequency,7 and enzymatic digestion8) have been developed. Electromechanical reshaping (EMR) of cartilage is a minimally invasive technique that was introduced previously9 but is still experimental. It is a novel technique that has significant potential for use in facial reconstructive surgery. Electromechanical reshaping achieves permanent shape change by initiating electrochemical redox reactions in the vicinityofstressconcentrations,alteringmechanical properties of tissue matrix.9
Previous ex vivo experiments have shown that direct current electrical fields around the area of active stress concentration can affect permanent change in cartilage.9 Nonthermogenic redox reactions at the tissue-electrode interface change the composition of cartilage, resulting in relaxation of internal stresses and sustained shape change, without the need for surgical incisions.9-11 Accordingly, surgical embodiments of EMR would use percutaneous or transmucosal needles inserted into the regions of stress distribution in mechanically deformed or reshaped cartilage specimens, and the feasibility of this approach in ex vivo tissues has been previously discussed.12,13
Given that a set of voltage and time parameters has been identified that produce effective shape change in intact ex vivo auricular specimens,12 further optimization of electrical dosimetry variables and electrode configurations in vivo is needed to move this technology toward clinical use.10,12 This study aimed to evaluate the in vivo effects of EMR of ear cartilage in a rabbit model to determine the dependence of shape change, mechanical stability, and tissue injury on dosimetry (voltage and application time) and electrode configuration.
METHODS
The protocol was approved and performed under the guidance of the Institutional Animal Care and Use Committee at the University of California, Irvine. All the regulations were followed throughout the duration of the study.
EMR PROCEDURE
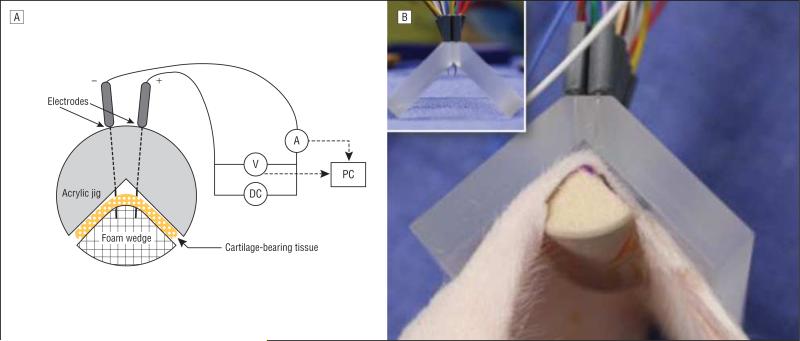
Ten New Zealand white rabbits (Western Oregon Rabbit Company), weighing 3.8 to 4.0 kg, were anesthetized using subcutaneously administered ketamine hydrochloride (20-40 mg/ kg) and xylazine (3-5 mg/kg). The ear was positioned within the EMR jig along a line halfway between the base and tip of the ear (Figure 1). The jig encompassed 4 rows of 19 apertures to extend across the width of the rabbit ear. Apertures were set at 3.0 mm apart from one another. Platinum needles were then inserted through each aperture and through the rabbit ear and were then connected to leads from a direct current power supply (PPS-2322; Amrel) to deliver current. The EMR current was applied at 5 V for 4 minutes for 8 of 10 ears treated. In controls (2 of 10 ears), the same procedure was performed without applying current. Following EMR treatment, both ears were splinted over a gauze roll (1.5 cm in diameter) and sandwiched between two 3×7-cm silicone elastomeric bolsters that were sutured into place using two 3-0 polypropylene sutures. An Elizabethan collar was placed, and the animals were transferred to the vivaria for recovery.
Figure 1.
In vivo electromechanical reshaping of ear cartilage in a rabbit model. A, Schematic representation. B, Acrylic jig used to mechanically deform ears during the procedure. DC indicates direct current; PC, personal computer; and V, voltage.
PROCEDURES AFTER EMR
After surgery, the rabbits were monitored for overall well-being and for signs of pain or agitation; photographic documentation of the ears was obtained at regular intervals. After 4 weeks, the animals were killed with a lethal dose of intraperitoneal pentobarbital, and the splints were removed. The auricles were then harvested in preparation for the subsequent procedures listed in this subsection.
Photography
With the tip pointing superiorly and inferiorly while being supported from the base, each ear was photographed and videotaped. Analysis of the degree of shape change in each ear was measured using a commercially available software package (Photoshop version 9.0; Adobe Systems, Inc).
Mechanical Response Measurement
To test the integrated mechanical response of the reshaped ears to flexural deformation quantitatively, auricular tissue was analyzed using a precision mechanical testing platform (ELF 3200; Bose Corporation). The integrated response of an intact re-shaped ear to mechanical deformation (flexure) was evaluated. The ear was removed from the crania at the level of the external auditory meatus. The bottom of the ear was then embedded in a base consisting of plaster of paris, which was allowed to cure. This base was then mounted onto the upper platen of the mechanical testing platform. Ears were bent 90°, and the bottom platen of the platform was gradually raised until its edge was in contact with the deflected portion of the ear 10.0 mm away from the bend axis of the ear. A static reaction force was recorded at this moment. The upper platen moved up and down at a constant velocity of 2.5 mm/s to a maximum amplitude of 2.5 mm, flexing the ear at its bend (resulting from reshaping). A stationary load cell rated to 250 N attached to the bottom platen measured the integrated reaction force produced by the ear in response to flexing.
Displacement and integrated reaction force were recorded during flexing. The interval where this force changes linearly with displacement was identified, and the integrated elastic modulus was calculated. The mechanical response of control ears (no EMR) was evaluated in a manner similar to that of the treatment ears. In both treatment and control ears, the initial reaction force registering at the moment of contact with the bottom platen and corresponding to the reaction to 90° bending was recorded and was subtracted from the force obtained in subsequent flexing experiments.
Microscopic Assessments
The ears were sectioned to include 2 specimens for histologic analysis and 2 specimens for live-dead fluorescent assays using confocal microscopy. The live-dead assay (Molecular Probes Inc) uses 2 dyes, calcein acetomethoxy and ethidium homodimer 1. Calcein acetomethoxy emits 517-nm (green) light when excited by light at 494 nm. It is a membrane-permeable esterase substrate that diffuses into the cytoplasm and is hydrolyzed, after which it becomes unable to cross an intact plasma membrane, becoming trapped inside live (viable) cells. Ethidium homodimer 1 has a high affinity for nucleic acids; however, it is unable to cross an intact cell membrane. Therefore, it concentrates predominantly inside dead (nonviable) cells with porous cell membranes. Ethidium homodimer 1 emits 617-nm (red) light when excited by light at 528 nm.
Specimens were cut in serial cross-section with a razor blade and were prepared under minimal lighting conditions because the aforementioned dyes are photoreactive. Both dyes were mixed according to manufacturer instructions, were added to each specimen in a microvial, and were kept in a light-free environment for 30 minutes. The specimens were then washed with phosphate-buffered saline, transported in a light-free box, and immediately imaged using a laser confocal microscope (Meta 510; Carl Zeiss LSM). All the segments incorporated a region in which the needle perforated and where energy was applied.
For histologic analysis, the specimens were formalin fixed and paraffin embedded. A microtome was used to serially section the paraffin blocks, which were then stained with hematoxylin-eosin. Once on the slides, sections were digitized and montaged to reconstruct the specimen. Three individuals (S.O., C.M., and S.F.H.) blinded to the study were trained to analyze each histologic specimen. Cartilage thickness was measured at the apex of the bend using available software (ImageJ; National Institutes of Health). Evidence of scar tissue and any signs of chondrocyte regeneration were noted.
To assess the viability of chondrocyte cells, specimens were stained with calcein acetomethoxy and ethidium homodimer 1 and were viewed using confocal microscopy. Within 48 hours of euthanasia, the harvested ears were stained under low light to prevent premature fluorescence of the dyes used. A 480-nm argon laser confocal microscope was used to image stained specimens at ×10 magnification. One individual (C.M.) blinded to the study was trained to analyze each confocal result. Data were presented blinded, and this individual measured cartilage thickness, width of tissue injury at each electrode, and the width of live cells between electrodes.
RESULTS
All the rabbits tolerated EMR and survived for the duration of the study. Initial exudative scabs at perforation sites resolved by postoperative day 11 (Figure 2); fully intact epithelium was noted in all the ears at the time of euthanasia. No infection, scarring, or bleeding complications were noted. All the treated ears showed significant shape change (mean, 102.4°; range, 87°-122°), exceeding that of control ears (mean, 14.5°; range, 4°-25°) (Table).
Figure 2.
Electromechanical reshaping results. A, Typical appearance of a bolstered-treated ear on postoperative day 5, with dried exudative scabs. By day 11 (×1.5 magnified inset), the scabs are gone, and the underlying skin appears healthy and intact. B and C, Appearance of ears after removal of the bolster on day 28 (after euthanasia) in a control ear (B) and in a treated ear (C).
Table.
Bend Angles After In Vivo Electromechanical Reshaping of Ear Cartilage in a Rabbit Model
| Ear No. | Bend Anglea |
|---|---|
| Control | |
| 1 | 25 |
| 2 | 4 |
| Treated | |
| 1 | 108 |
| 2 | 87 |
| 3 | 97 |
| 4 | 119 |
| 5 | 99 |
| 6 | 97 |
| 7 | 90 |
| 8 | 122 |
Calculated as degrees of bend from a vertical plane.
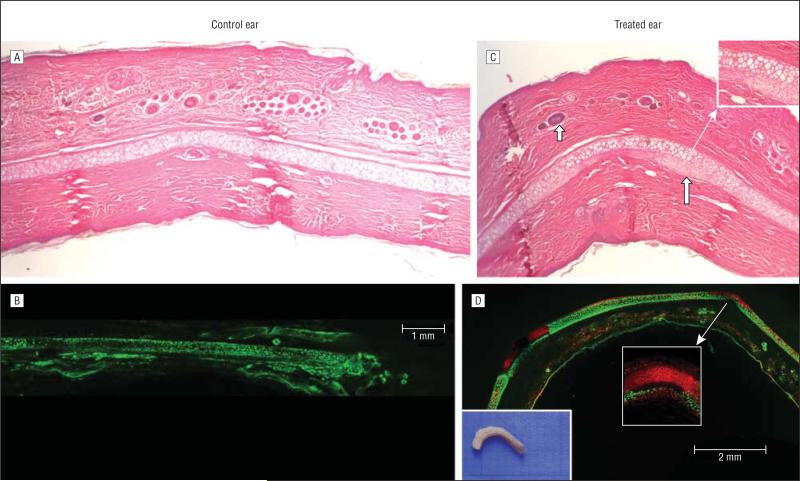
HISTOLOGIC EXAMINATION
Histologic examination of the electroformed sites showed an intact epidermis and adnexal structures (Figure 3). Platinum needle electrode (30-gauge) perforations in the ear created a discontinuous cartilaginous layer spanning 0.3 to 0.8 mm. A chondroblastic proliferation was observed near the area of the cartilaginous defect. This correspondstoasubperichondrialformationofcartilagearound the periphery of the site where EMR was applied.
Figure 3.
Histologic findings. A, Control ear shows normal-appearing cartilage and epithelial lining. B, Live-dead fluorescent assay confocal microscopy shows viable chondrocytes (green) throughout the control specimen. C, Treated ear shows curved geometry with intact epithelial lining and adnexal structures (short blue arrow). Neochondrogenesis is noted along the undersurface of the cartilage in the periphery of perforated sites (long blue arrow and ×2 magnified inset). D, Live-dead fluorescent assay confocal microscopy shows limited zones of nonviable chondrocytes (red) around needle electrode sites, with live cells along the undersurface of the cartilage, presumably representing ingrowth of new chondrocytes (×10 magnified inset). The gross section is shown on the left.
CONFOCAL MICROSCOPY
Confocal microscopy demonstrated a localized zone of nonviable chondrocytes less than 2.0 mm in diameter surrounding the point of insertion of needle electrodes in all the treated ears (Figure 3). Within this zone was evidence of fibrocartilage scar tissue. The anodic and cathodic rows were similar in appearance for live-dead fluorescent assays.
MECHANICAL RESPONSE MEASUREMENT
Ears treated with EMR and control ears demonstrated statistically similar integrated elastic modulus. The mean (SD) values were 0.43 (0.05) MPa for EMR-treated ears and 0.48 (0.06) MPa for the control ears (P < .01).
COMMENT
In this pilot study, we demonstrated that EMR can be used to alter the shape of the ear in an in vivo rabbit model. The low cost, technically simple, and nonthermogenic features of EMR make this modality an appealing alternative to other minimally invasive systems, such as laser and RF-mediated reshaping. To advance toward clinical trials, the safety and efficacy of EMR on living tissue must be assessed.14 This study demonstrated that EMR technology can be applied along the entire width of the auricle to create shape change, without complications of major skin injury, necrosis, or infection. Skin injury merits discussion because the electrodes were in contact with the skin and cartilage during the procedure. A major concern was that EMR performed without the use of an insulation layer covering portions of the needle electrode not in contact with cartilage might lead to cutaneous injury and adverse outcomes. On inspection and with histologic analysis, we found no sustained injury, despite the observation of crusting and serous exudates immediately after EMR was performed. Based on this information, we conclude that epithelial injury with the present protocol will not be a major hurdle for using this technology.
The dosimetry parameters were derived from prior ex vivo investigations12 as a starting point for producing effective shape change in live rabbit ears. Future experiments will further examine the dependence of shape change on dosimetry in vivo, with the broad goal of developing methods to optimize the electrical dosimetry, as well as needle electrode design and placement. Geometry of electrode placement, voltage difference, and application time would affect the viability of the chondrocytes and the shape change.
On subjective assessment of ear mechanical behavior, manual inspection of each treated auricle demonstrated that shape change after splint removal was maintained and that qualitatively the reshaped segments had elastic behavior similar to that of native nontreated adjacent tissue. We observed that the thicker, anterior portion of each ear sustained more consistent and robust shape change than the adjacent thinner regions, and we attribute this to the increased tissue mass here that is available for the electro-chemical changes that accompany the EMR effect.
Histologic analysis of the ear showed patterns promising to remodeling that lead to permanent shape change with EMR. Normal tissue regions that were 2.0 mm away from the electrodes showed no signs of necrosis, fibrotic changes, or other damage. Regions near the vicinity of each electrode (<2.0 mm away) showed chondrocyte proliferation. The cells were most dense by the needle sites and where curvature was greatest. Needle insertion sites there were replaced with a fibrotic process or remained unchanged, indicating that a longer study period is warranted to observe complete closure. The toxic pH gradient created by the EMR procedure seems spatially limited and perhaps may be mitigated in part by blood flow through vascularized tissues. Blood does not flow through cartilage tissue, and this fact is exploited when performing EMR.
Assessing chondrocyte viability using laser confocal microscopy and live-dead fluorescent assays is a well-established technique,15,16 aiding the optimization of EMR dosimetry and geometry of electrode placement. Confocal microscopy identified some regions of tissue injury, which were spatially limited to the immediate vicinity around each needle electrode up to 1.2-mm away. The tissue injury surrounding each electrode insertion was consistent among all the specimens, but these regions were small and represented a fraction of the total tissue volume in the specimen. In addition, the visualization of chondrocyte neogenesis coincided with the histologic results of the same ear. Previous in vitro investigations12 examining cell injury in EMR-altered cartilage specimens showed results similar to our in vivo investigations. This degree of tissue injury is limited in its spatial extent and is on par with results using conventional techniques, such as cartilage morselization. Like radiofrequency and laser cartilage reshaping, EMR achieves shape change at the expense of cell injury.
The objective herein was to assess the safety and efficacy of EMR in vivo. To our knowledge, this is the first study to demonstrate that shape change can be achieved via mild injury to the cartilage, with no persistent damage to the epithelial lining. Future studies will examine longer survival times, which will provide more information on the long-term in vivo response of cartilage tissue (and overlying skin) to EMR.
In conclusion, EMR altered the shape of the rabbit auricle, providing good creation and retention of shape, with limited skin and cartilage injury. Needle electrode EMR is a viable technique for minimally invasive tissue reshaping, with potential applications in otoplasty, septoplasty, and rhinoplasty. Further studies to refine dosimetry parameters and to assess reshaping over time with the auricular splints removed will be required before clinical trials.
Acknowledgments
Funding/Support: This study was supported by grant ERT 44380-29302 from the National Institutes of Health (Dr Wong).
Footnotes
Author Contributions: Study concept and design: Oliaei, Manuel, Protsenko, and Wong. Acquisition of data: Oliaei, Manuel, Karam, Hussain, and Hamamoto. Analysis and interpretation of data: Oliaei, Manuel, Karam, Hamamoto, Protsenko, and Wong. Drafting of the manuscript: Oliaei, Manuel, Karam, and Wong. Critical revision of the manuscript for important intellectual content: Oliaei, Karam, Hussain, Protsenko, and Wong. Statistical analysis: Oliaei. Obtained funding: Wong. Administrative, technical, and material support: Hussain and Wong. Study supervision: Manuel, Protsenko, and Wong.
Conflict of Interest Disclosures: Dr Wong has intellectual property (licensed by Aerin Medical, Inc, and by Praxis BioSciences, LLC) that pertains to the research performed in this study. He also has equity with Praxis BioSciences, LLC. Aerin Medical, Inc, will license the intellectual property from the University of California, Irvine, from which Dr Wong may benefit.
REFERENCES
- 1.Brent B. The pediatrician's role in caring for patients with congenital microtia and atresia. Pediatr Ann. 1999;28(6):374–383. doi: 10.3928/0090-4481-19990601-09. [DOI] [PubMed] [Google Scholar]
- 2.Balogh B, Millesi H. Are growth alterations a consequence of surgery for prominent ears? Plast Reconstr Surg. 1992;89(4):623–630. doi: 10.1097/00006534-199204000-00005. [DOI] [PubMed] [Google Scholar]
- 3.Stenstrom SJ, Heftner J. The Stenstrom otoplasty. Clin Plast Surg. 1978;5(3):465–470. [PubMed] [Google Scholar]
- 4.Zaoli G. Otoplasty. In: Gonzalez-Ulloa M, Meyer R, Smith JW, Zaoli G, editors. Aesthetic Plastic Surgery. Vol. 2. Piccin; Padova, Italy: 1987. pp. 165–297. [Google Scholar]
- 5.Kompatscher P, Schuler CH, Clemens S, Seifert B, Beer GM. The cartilage-sparing versus the cartilage-cutting technique: a retrospective quality control comparison of the Francesconi and Converse otoplasties. Aesthetic Plast Surg. 2003;27(6):446–453. doi: 10.1007/s00266-003-3062-6. [DOI] [PubMed] [Google Scholar]
- 6.Wong BJ, Milner TE, Harrington A, et al. Feedback-controlled laser-mediated cartilage reshaping. Arch Facial Plast Surg. 1999;1(4):282–287. doi: 10.1001/archfaci.1.4.282. [DOI] [PubMed] [Google Scholar]
- 7.Keefe MW, Rasouli A, Telenkov SA, et al. Radiofrequency cartilage reshaping: efficacy, biophysical measurements, and tissue viability. Arch Facial Plast Surg. 2003;5(1):46–52. doi: 10.1001/archfaci.5.1.46. [DOI] [PubMed] [Google Scholar]
- 8.Thomas L. Reversible collapse of rabbit ears after intravenous papain, and prevention of recovery by cortisone. J Exp Med. 1956;104(2):245–252. doi: 10.1084/jem.104.2.245. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ho KH, Diaz Valdes SH, Protsenko DE, Aguilar G, Wong BJ. Electromechanical reshaping of septal cartilage. Laryngoscope. 2003;113(11):1916–1921. doi: 10.1097/00005537-200311000-00011. [DOI] [PubMed] [Google Scholar]
- 10.Wu EC, Protsenko DE, Khan AZ, Dubin S, Karimi K, Wong BJ. Needle electrode–based electromechanical reshaping of rabbit septal cartilage: a systematic evaluation. IEEE Trans Biomed Eng. 2011 doi: 10.1109/TBME.2011.2157155. [published online May 19, 2011] doi:10 .1109/TBME.2011.2157155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Wu EC, Khan A, Protsenko DE, et al. Electromechanical reshaping of rabbit septal cartilage: a six needle electrode geometric configuration. [August 25, 2012];Proc SPIE. 2009 7161:716128–1-716128-11. http://adsabs.harvard.edu/abs/2009SPIE.7161E.49W. [Google Scholar]
- 12.Manuel CT, Foulad A, Protsenko DE, Sepehr A, Wong BJ. Needle electrode-based electromechanical reshaping of cartilage. Ann Biomed Eng. 2010;38(11):3389–3397. doi: 10.1007/s10439-010-0088-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Protsenko DE, Ho K, Wong BJF. Stress relaxation in porcine septal cartilage during electromechanical reshaping: mechanical and electrical responses. Ann Biomed Eng. 2006;34(3):455–464. doi: 10.1007/s10439-005-9051-y. [DOI] [PubMed] [Google Scholar]
- 14.Danter J, Siegert R, Weerda H. Ultrasound measurement of skin and cartilage thickness in healthy and reconstructed ears with a 20-MHz ultrasound device. Laryngorhinootologie. 1996;75(2):91–94. doi: 10.1055/s-2007-997542. [DOI] [PubMed] [Google Scholar]
- 15.Choi IS, Chae YS, Zemek A, Protsenko DE, Wong BJF. Viability of human septal cartilage after 1.45 microm diode laser irradiation. Lasers Surg Med. 2008;40(8):562–569. doi: 10.1002/lsm.20663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Li C, Protsenko DE, Zemek A, Chae YS, Wong B. Analysis of Nd:YAG laser-mediated thermal damage in rabbit nasal septal cartilage. Lasers Surg Med. 2007;39(5):451–457. doi: 10.1002/lsm.20514. [DOI] [PubMed] [Google Scholar]