Abstract
Background
The psychological outcomes that accompany smoking cessation are not yet conclusive but positive outcomes could help to persuade quitting.
Method
We use data from the longitudinal National Epidemiological Study of Alcohol and Related Conditions. Logistic regression was used to examine associations between cigarette smoking reduction and Wave 2 status of addiction/mental health disorder among daily smokers at Wave 1, stratified by status of the diagnosis of interest at Wave 1. We adjusted for differences in baseline covariates between smokers with different levels of smoking reduction between Wave 1 and Wave 2 using propensity score regression adjustment.
Results
After adjusting for propensity scores and other mental health/addiction comorbidities at Wave 2, among daily smokers who had current or lifetime history diagnosis of the outcome of interest at Wave 1, quitting by Wave 2 predicted a decreased risk of mood/anxiety disorder (aOR 0.6, 95% CI 0.4, 0.9) and alcohol disorder (aOR 0.7, 95% CI 0.5, 0.99) at Wave 2. Among daily smokers with no lifetime history diagnosis of the outcome of interest at Wave 1, quitting smoking by Wave 2 predicted a decreased risk of drug use disorder at Wave 2 aOR 0.3, 95% CI 0.1, 0.9).
Conclusions
There is no support in our data for the concern that smoking cessation would result in smokers’ increased risk of some mental disorders. To the contrary, our data suggest that smoking cessation is associated with risk reduction for mood/anxiety or alcohol use disorder, even among smokers who have had a pre-existing disorder.
Keywords: smoking, mental health, cessation, psychiatry, substance use disorders, longitudinal data
Introduction
Despite substantial declines in smoking rates since the 1960’s, cigarette smoking remains the leading cause of preventable death in the U.S. (Adhikari et al. 2008; Viswanath et al. 2010). From 1965 to 2011, the annual prevalence of smoking decreased more than 50% (CDC, 2012); however, the rates of smoking among those with psychiatric and substance use disorders remains elevated at two to four times that of a general population of smokers (Brown et al. 1996; Lewinsohn et al. 1999; Upadhyaya et al. 2002; Ramsey et al. 2005; Myers & Kelly 2006; Tobias et al. 2008; Launiainen et al. 2011). For instance, 45% of adults with an affective disorder diagnosis and 38% with an anxiety disorder diagnosis are cigarette smokers versus 21% of adults without a psychiatric diagnosis (Lawrence et al. 2009).
It is challenging to separate the role of smoking cessation in mental health functioning (Hughes, 2008). Some research indicates that smoking cessation could result in an increase in depressive (Borrelli et al. 1996; Stage et al. 1996; Killen et al. 2003; Hughes, 2007) or anxiety symptoms (West & Hajek, 1997; Becoña et al. 2002) which in turn influences smoker’s ability or motivation to quit (Shiffman, 1982; Covey et al. 1990; Hall et al. 1993; Bock et al. 1996; Glassman et al. 2001; Burgess et al. 2002). Studies vary in their reports on the risk for developing major depressive disorder following smoking cessation, with ranges from 0% to ~30% with the higher rates reported among smokers with a history of major depressive disorder (Borrelli et al. 1996; Covey et al. 1997; Killen et al. 2003; Glassman et al. 2001; Hughes, 2007). On the contrary and irrespective of cessation treatment, additional studies have found that smoking cessation is seldom associated with worsening mental health functioning (Leistikow & Shipley, 1999; Tsoh et al. 2000; Hall et al. 2006; Klungsoyr et al. 2006; McFall et al. 2006; Munafò et al. 2008; Prochaska et al. 2008; Shahab & West, 2009; Hajek et al. 2010; Torres et al. 2010; Shahab, 2012; Donald et al. 2013; Mathew et al. 2013). For instance, a recent study by Morissette et al. (2012) additionally found that smokers with and without anxiety disorders and/or other psychological disorders responded equally to high-risk smoking triggers during the quit process with respect to smoking urges and anxiety response; these are relevant findings given that most smokers encounter anxiety and other mental health problems. In another promising study, Shahab et al. (2012) found that a large majority of former smokers (69% of n=879) considered themselves happier after they quit smoking.
Rates of cigarette smoking are even higher among those with substance use disorders with estimates up to 80% (Lawrence et al. 2009; Kalman et al. 2005). Importantly, most people in addiction treatment want to quit smoking (Flach & Diener, 2004) and will accept concurrent smoking cessation treatment (Seidner et al. 1996). While a number of studies suggest that cessation of cigarette smoking and other substances enhance clinical outcomes (Sobell & Sobell, 1996: Stuyt, 1997; Kohn et al. 2003; Prochaska et al. 2004a; Prochaska et al. 2004b), smokers with co-morbid substance use disorders do report smoking to cope with urges to drink alcohol or use other drugs when trying to abstain (Asher et al. 2003; Cooney et al. 2003; Rohsenow et al. 2005; Baca & Yahne, 2009).
New research indicates that smokers will lose a decade of their life but smoking cessation reduces that loss by about 90% if it occurs before the age of 40 years (Pirie et al. 2013). The psychological outcomes that accompany smoking cessation are not yet conclusive; they could potentially play a role in persuading quitting behaviors if benefits exist. As a result, population-based studies can help to reconcile the inconsistent empirical evidence on this topic by clarifying the mental health outcomes that are associated with smoking reduction and cessation. Our study uses two waves of data from the National Institute on Alcohol Abuse and Alcoholism's (NIAAA) National Epidemiological Study of Alcohol and Related Conditions (NESARC), allowing us to examine the relationship between cigarette smoking reduction and cessation from Wave 1 to Wave 2 and changes in the risk of three disorders that highly co-occur with smoking: mood/anxiety disorders, alcohol use disorders, and drug use disorders.
Methods and Materials
Data source and respondents
The analyses presented in this study utilized data from the National Epidemiologic Study on Alcohol and Related Conditions (NESARC; Grant et al. 2004). The NESARC collected data on the prevalence of alcohol and drug use, abuse, and dependence as well as associated psychiatric and other medical conditions. Under contract and supervised by the National Institute on Alcohol Abuse and Alcoholism, the US Census Bureau conducted face-to-face interviews with a multi-stage probability sample of adults ages 18 and older that is nationally representative. The NESARC is a longitudinal survey consisting of Wave 1 (N=43,093, 81% response rate), conducted from 2001–2002, and a 3-year follow-up interview with 34,653 respondents (Wave 2). The Wave 2 response rate was 86.7%. Of the 8,440 Wave 1 respondents who were not included in Wave 2, 3,134 were not eligible for a Wave 2 interview because they were institutionalized, mentally/physically impaired, on active duty in the armed forces, deceased, or deported. The remaining individuals (n=5,306) were eligible but were not re-interviewed because they refused or could not be reached or located. Wave 2 sampling weights reflect design characteristics of the NESARC and account for nonresponse as well as sample attrition. The weighted Wave 2 data represent the same baseline population as represented in Wave 1 (Ruan et al. 2008; Chen et al. 2010). A detailed description of the survey methods, other quality control procedures, and test–retest reliability tests have been documented (Grant et al. 2003). Waves 1 and 2 of the NESARC were used for analyses.
Only Wave 1 daily smokers who reported smoking daily within the past year at Wave 1 and were re-interviewed at Wave 2 were included in the analysis (N=6,554). We excluded 1,607 respondents who increased their smoking between Wave 1 and Wave 2 (i.e., average number cigarettes smoked per day increased by ≥10%). Ninety four respondents with missing data for amount of cigarettes smoked at either Wave 1 or Wave 2 were also excluded, resulting in 4,853 respondents for analysis.
A greater percentage of those with missing data, compared to those without missing data, were male (66.2% vs 52.2%, Χ2 4.9, p=.031), and were 30 years or older (87.6% vs 75.8%, Χ2 7.1, p=.010). We also multiply imputed the number of cigarettes smoked daily at Wave 1 and Wave 2 for those with missing data. Due to a low percentage of respondents that had missing data and because results from multiply imputed data were similar to complete case analysis indicating no evidence of bias, we present here the complete case analysis results.
Dependent variables
All NESARC interviews utilized the National Institute on Alcohol Abuse and Alcoholism Alcohol Use Disorder and Associated Disabilities Interview Schedule – DSM IV Version (AUDADIS-IV; Grant et al. 2003), a structured diagnostic interview with the list of symptom questions that assesses DSM-IV disorders. A number of psychometric studies have documented the reliability and validity of the AUDADIS-IV (Grant et al. 2003). All diagnostic variables discussed below exclude symptoms due to drugs, alcohol, or medical condition.
Status at Wave 2: Current (past 12 month) mood or anxiety disorders
Four DSM-IV mood disorders are assessed in the NESARC: major depression, dysthymia, mania, and hypomania. The following anxiety disorders are also assessed according to DSM-IV criteria: panic (with and without agoraphobia), agoraphobia without history of panic disorder, social phobia, specific phobia, and generalized anxiety disorder. In order to receive a formal DSM-IV diagnosis, respondents must endorse a requisite number of symptoms pertaining to the DSM-IV criteria for a diagnosis of interest and report the presence of social and/or occupational dysfunction associated with the disorder (Chen et al. 2006). A participant was assigned a mood or anxiety disorder if they met criteria in the 12 months preceding Wave 2 assessment for any of the mood or anxiety disorders.
Status at Wave 2: Current (past 12 month) DSM-IV alcohol use disorder
A diagnosis of past 12 month DSM-IV alcohol abuse was given to participants who meet at least one of four criteria for alcohol abuse in the year preceding the interview, without meeting criteria for alcohol dependence. A diagnosis of past 12 month DSM-IV alcohol dependence was given to participants who met at least three of seven alcohol dependence criteria in the year preceding the interview.
Status at Wave 2: Current (past 12 month) DSM-IV drug use disorder
The DSM-IV drug use disorder diagnoses assessed in the NESARC include the following drug groups: sedatives, tranquilizers, opiates (other than heroin or methadone), amphetamines, cannabis, hallucinogens, cocaine (including crack cocaine), inhalants/solvents, heroin, or other drugs. For a drug-specific abuse diagnosis, at least one of the four abuse criteria is required. To meet a drug-specific dependence diagnosis, at least three of the seven dependence criteria are required (diagnoses for cannabis, hallucinogen, or inhalant dependence do not use the withdrawal criterion) (Chen et al. 2006). A participant was considered to have a diagnosis of DSM-IV drug use disorder if they met the abuse or dependence criteria in the past 12 months for any of 10 drug categories.
Independent variable of interest
The primary independent variable was percent change in number of cigarettes per day from Wave 1 to Wave 2. All participants included in the analysis were daily smokers at Wave 1. The number of cigarettes they smoked per day at Wave 1 was reported as the usual quantity when they smoked. The average number of cigarettes per day at Wave 2 was calculated using the items assessing the usual frequency when the respondents smoked in the past year (i.e., every day, 5–6 days/week, 3–4 days/week, 1–2 days/week, 2–3 days/month, once a month or less) and the usual quantity when they smoked. The percent reduction in number of cigarettes per day was calculated as the percent change in daily smoking from Wave 1 to Wave 2. Percent change in daily smoking was then categorized as follows: no or minimal (1–9%) change (reference group), 10–49% reduction, 50–99% reduction, and 100% reduction. Those who increased daily smoking by ≥10% were excluded from analysis.
Statistical Analysis
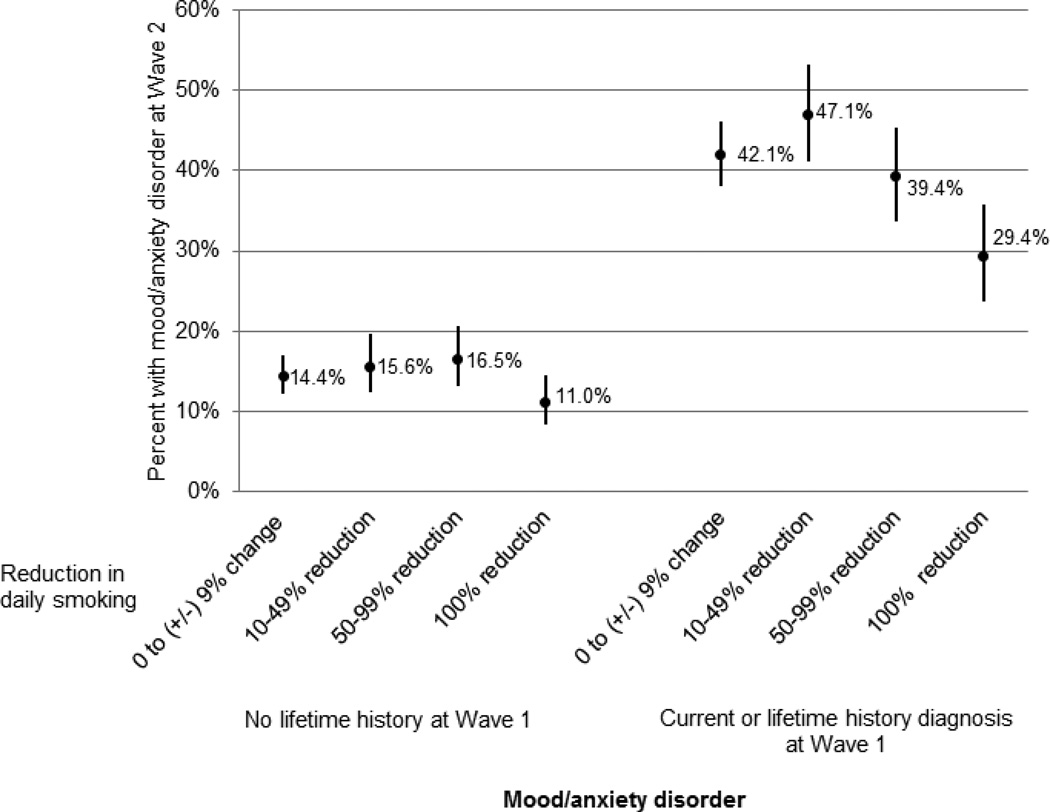
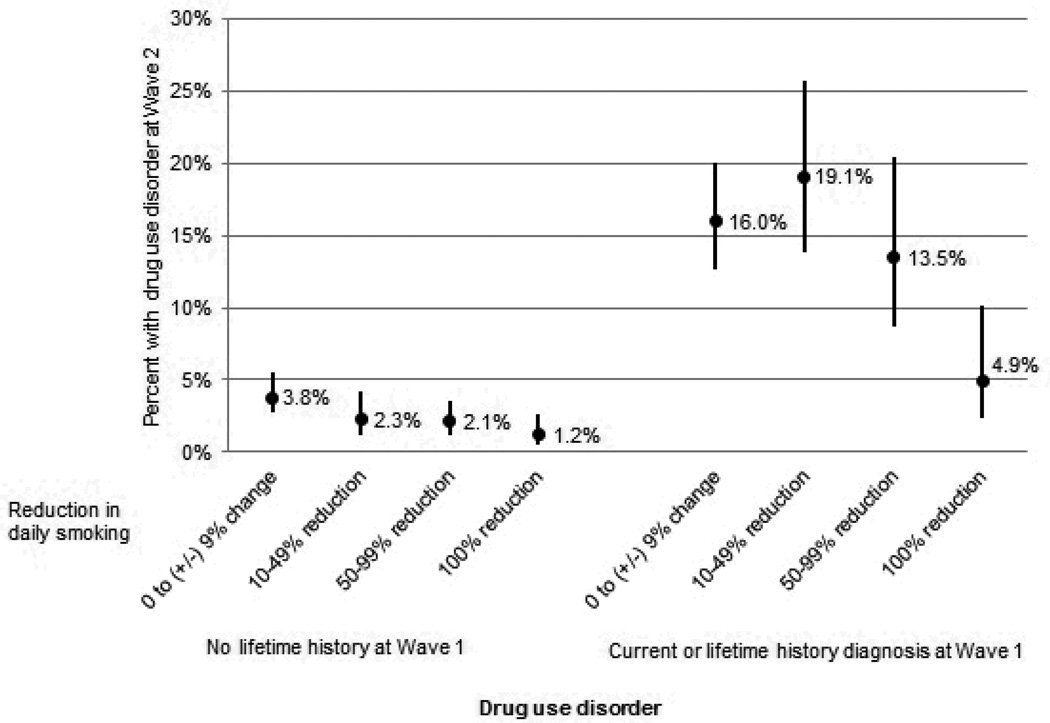
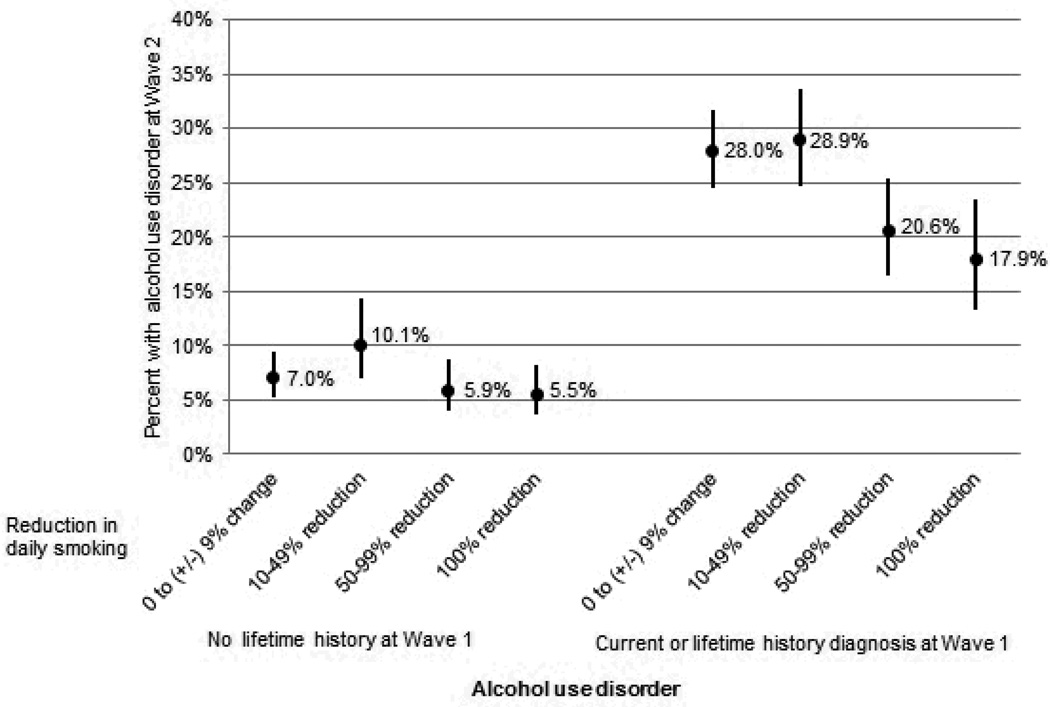
Percent of daily smokers with the three outcomes of interest within the past 12 months at Wave 2 (mood/anxiety disorder, alcohol use disorder, drug use disorder) was examined by the amount of reduction in daily smoking from Wave 1 to Wave 2. These percentages, unadjusted for other variables, are presented in Figures 1–3. Analyses were stratified by history of the diagnosis of interest at Wave 1. We examined smokers with no lifetime history (ever in lifetime up to the time of the interview) of the specific diagnosis at Wave 1 to study the effect of change in cigarettes per day on incident cases of the diagnosis at Wave 2. We separately analyzed smokers with current (within the past year) or lifetime history diagnosis at Wave 1 to study the effect of change in cigarettes per day on recurrent/persistent cases of the diagnosis at Wave 2.
Figure 1.
Prevalence of mood/anxiety disorder within the past 12 months at Wave 2, by smoking reduction from Wave 1 to Wave 2, stratified by status of mood/anxiety disorder at Wave 1. Circles represent prevalence estimates, and lines represent 95% confidence intervals.
Figure 3.
Prevalence of drug use disorder within the past 12 months at Wave 2, by smoking reduction from Wave 1 to Wave 2, stratified by status of drug use disorder at Wave 1. Circles represent prevalence estimates, and lines represent 95% confidence intervals.
Logistic regression models were used to quantify the association between percent change in daily cigarette use from Wave 1 to Wave 2 and status of the three separate outcomes of interest at Wave 2 (Table 2). Models were stratified by status of the diagnosis of interest at Wave 1 as described above. We first examined the association in unadjusted bivariate analysis. We then used propensity score methods to adjust for potential confounding. Such methods are used in nonrandomized, observational studies to balance “treatment” groups on observed covariates to reduce bias and aid in causal inference (Rosenbaum & Rubin, 1983). We have multiple levels of our “treatment” variable (i.e., percent reduction in smoking between Wave 1 and Wave 2: no or minimal (1–9%) change (reference group), 10–49% reduction, 50–99% reduction, and 100% reduction). Thus, we used the multiple or “generalized” propensity score as suggested by Imbens (2000), which is the conditional probability of receiving a particular level of the treatment given the pre-treatment variables. Baseline (Wave 1) variables that were likely to be associated with our outcomes of interest were selected for inclusion in the propensity score model (Brookhart et al. 2006). These included age, sex, race/ethnicity, education, income, marital status, employment status, private insurance, self-perceived health, number of cigarettes smoked daily, history of nicotine dependence, desire to quit smoking, conduct/personality disorder, history of alcohol use disorder, frequency of drinking, heavy drinking (i.e., ≥ 5 drinks when drank), ever sought help for drinking, family history of alcoholism, history of drug disorder, frequency of drug use, ever sought help for drug use, family history of drug problems, history of mood/anxiety disorder, NBS8 norm-based mental health scale, how often felt downhearted/depressed, family history of depression, and ever sought help for mood/anxiety disorders. We also included Wave 2 survey weights as a covariate in the propensity score model, as suggested by Zanutto et al. (2005). The above baseline variables are similar to those chosen in a propensity score model using the NESARC to examine effects of drinking to self-medicate anxiety symptoms on alcohol dependence outcomes (Crum et al. 2013). Each of the variables chosen was significantly associated with at least one of our diagnosis outcomes of interest. Because we stratified our final analyses by history of the diagnosis of interest at Wave 1, we included interaction terms for each diagnosis of interest at Wave 1 with all other variables in the propensity score models. Due to the difficulty of matching or stratifying across multiple propensity scores (further complicated by stratifying final models by Wave 1 history of diagnoses), we used the regression adjustment method (i.e., covariance adjustment) and followed the steps outlined in Spreeuwenberg et al. (2010).
Table 2.
Associations of smoking reduction with substance use and mood/anxiety disorders at Wave 2
| Mood/anxiety disorder within past 12 months at Wave 2 a |
Alcohol use disorder within past 12 months at Wave 2 b |
Drug use disorder within past 12 months at Wave 2 c |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Model 1 (Bivariate association) OR (95% CI) |
Model 2 (Adjusts for Propensity scores) aOR (95% CI) |
Model 3 d (Adjusts for propensity scores and W2 comorbidities) aOR (95% CI) |
Model 1 (Bivariate association) OR (95% CI) |
Model 2 (Adjusts for propensity scores) aOR (95% CI) |
Model 3 d (Adjusts for propensity scores and W2 comorbidities) aOR (95% CI) |
Model 1 (Bivariate association) OR (95% CI) |
Model 2 (Adjusts for propensity scores) aOR (95% CI) |
Model 3 d (Adjusts for Propensity scores and W2 comorbidities)aOR (95% CI) |
|
| New onset of disorder at Wave 2 (among those with no lifetime history diagnosis at Wave 1) | |||||||||
| Reduction in daily smoking | |||||||||
| 0 to (+/−) 9% change | Ref | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| 10–49% reduction | 1.1 (0.8, 1.6) | 1.0 (0.7, 1.4) | 1.0 (0.7, 1.4) | 1.5 (0.9, 2.4) | 1.2 (0.7, 2.0) | 1.3 (0.8, 2.1) | 0.6 (0.3, 1.2) | 0.6 (0.3, 1.2) | 0.5 (0.3, 1.2) |
| 50–99% reduction | 1.2 (0.8, 1.6) | 1.2 (0.8, 1.6) | 1.2 (0.8, 1.7) | 0.8 (0.5, 1.4) | 0.6 (0.3, 1.1) | 0.6 (0.3, 1.2) | 0.5 (0.3, 1.1) | 0.5 (0.2, 1.02) | 0.5 (0.2, 1.04) |
| 100% reduction | 0.7 (0.5, 1.04) | 0.7 (0.5, 1.1) | 0.8 (0.6, 1.1) | 0.8 (0.5, 1.3) | 0.7 (0.4, 1.3) | 0.8 (0.5, 1.5) | 0.3 (0.1, 0.7) | 0.3 (0.1, 0.7) | 0.3 (0.1, 0.9) |
| Recurrent/persistent disorder at Wave 2 (among those with current or lifetime history diagnosis at Wave 1) | |||||||||
| Reduction in daily smoking | |||||||||
| 0 to (+/−) 9% change | Ref | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. | Ref. |
| 10–49% reduction | 1.2 (0.9, 1.6) | 1.3 (0.9, 1.7) | 1.3 (0.95, 1.7) | 1.1 (0.8, 1.4) | 1.1 (0.8, 1.4) | 1.1 (0.8, 1.4) | 1.2 (0.8, 2.0) | 1.1 (0.7, 1.9) | 1.0 (0.6, 1.8) |
| 50–99% reduction | 0.9 (0.7, 1.2) | 0.9 (0.7, 1.3) | 0.9 (0.7, 1.3) | 0.7 (0.5, 0.9) | 0.7 (0.5, 1.02) | 0.7 (0.5, 1.1) | 0.8 (0.5, 1.4) | 0.8 (0.4, 1.5) | 0.9 (0.5, 1.7) |
| 100% reduction | 0.6 (0.4, 0.8) | 0.6 (0.4, 0.9) | 0.6 (0.4, 0.9) | 0.6 (0.4, 0.8) | 0.6 (0.4, 0.9) | 0.7 (0.5, 0.99) | 0.3 (0.1, 0.6) | 0.3 (0.1, 0.8) | 0.5 (0.2, 1.1) |
Mood/anxiety disorder: No lifetime history at Wave 1: N=2,938 (448 incident cases, 2490 with no diagnosis at Wave 2); Current or lifetime history diagnosis at Wave 1: N=1,915 (805 recurrent/persistent cases, 1110 with no diagnosis at Wave 2). When adjusting for propensity scores, sample sizes decreased slightly due to some missing data for included covariates: No lifetime history at Wave 1: N = 2845; Current or lifetime history diagnosis at Wave 1: N = 1883.
Alcohol use disorder: No lifetime history at Wave 1: N=2554 (183 incident cases, 2371 with no diagnosis at Wave 2); Current or lifetime history diagnosis at Wave 1: N=2299 (572 recurrent/persistent cases, 1727 with no diagnosis at Wave 2). When adjusting for propensity scores, sample sizes decreased slightly due to some missing data for included covariates: No lifetime history at Wave 1: N = 2488; Current or lifetime history diagnosis at Wave 1: N = 2240.
Drug use disorder: No lifetime history at Wave 1: N=3760 (89 incident cases, 3671 with no diagnosis at Wave 2); Current or lifetime history diagnosis at Wave 1: N=1093 (153 recurrent/persistent cases, 940 with no diagnosis at Wave 2). When adjusting for propensity scores, sample sizes decreased slightly due to some missing data for included covariates: No lifetime history at Wave 1: N = 3662; Current or lifetime history diagnosis at Wave 1: N = 1066.
Model 3 additionally adjusts for other outcome comorbidities at Wave 2 (e.g., the model predicting presence of alcohol use disorder at Wave 2 adjusts for lifetime history diagnosis or past 12 months drug use disorder and mood/anxiety disorders at Wave 2).
Although our “treatment” variable (levels of smoking reduction) appears ordinal, the proportional odds assumption was not met using ordinal logistic regression. Therefore, we used multinomial logistic regression to estimate the propensity for each level of treatment given our observed variables listed above. There was considerable overlap of the distributions of the multiple propensity scores, as is recommended. We also checked for balance of the covariates among the four treatment groups after adjusting for three of the four propensity scores. Prior to adjusting for propensity scores, 23 of the covariates differed significantly among the smoking reduction groups. After adjusting for the multiple propensity scores (i.e., propensity for 10–49% smoking reduction, propensity for 50–99% reduction, and propensity for 100% smoking reduction), no covariates differed significantly among the smoking reduction groups. To estimate the effect of level of smoking reduction on Wave 2 status of the diagnoses of interest, we used logistic regression to model the likelihood of Wave 2 diagnoses as a function of level of smoking reduction and the three multiple propensity scores. Then we further adjusted for Wave 2 status of the other mood/anxiety and substance use disorders as appropriate. For example, when examining Wave 2 alcohol use disorder as an outcome, we also included the presence of drug use disorder and mood/anxiety disorder at Wave 2 (in last 12 months at Wave 2 or prior to last 12 months) as covariates in the model. Analyses were performed using SAS-callable SUDAAN version 9.0.1, a software program that uses Taylor series linearization to adjust for design effects of complex sample surveys like the NESARC (Shah et al. 2002). Wave 2 stratum, PSU, and weights were applied to the models. Estimates in Table 2 with 95% confidence intervals that do not include the null value are significant at alpha= .05.
Results
A slight majority of the daily smokers included in the analysis was male (52.2%) and a large majority was Caucasian (76.9%). Additional characteristics are presented in Table 1. The average number of cigarettes per day at Wave 1 was 18.9 (95% confidence interval [CI] 18.5–19.3; median 19.3, inter-quartile range 9.8–19.8). Forty-one percent of daily smokers underwent minimal or no change (+/− 9% change) in number of cigarettes smoked daily from Wave 1 to Wave 2, 20.1% had a 10–49% reduction in the number of cigarettes smoked daily, 19.5% had a 50–99% reduction, and 19.2% quit smoking. The quit rate was much higher for smokers who consumed fewer cigarettes at Wave 1 compared to those who consumed more cigarettes (1–5 cigarettes/day 48.4%, 6–10 cigarettes/day 29.0%, 11–20 cigarettes/day 13.7%, 21–30 cigarettes/day 13.3%, >30 cigarettes/day 12.0%; chi-square = 22.8, p<.001).
Table 1.
Demographics of smokers who had smoked daily in the past year at Wave 1 (N=4,853)
| Variable | n (Weighted %) |
|---|---|
| Gender | |
| Female | 2,620 (47.8) |
| Male | 2,223 (52.2) |
| Race/ethnicity | |
| Caucasian | 3,173 (76.9) |
| African American | 857 (9.5) |
| Hispanic | 604 (8.0) |
| Asian/Native Hawaiian/Pacific Islander | 82 (2.1) |
| Native American | 137 (3.5) |
| Age | |
| 18–29 years old | 1,060 (24.2) |
| 30–44 years old | 1,656 (34.4) |
| 45–64 years old | 1,711 (33.6) |
| ≥ 65 years old | 426 (7.9) |
| Income | |
| ≥ $40,000 | 1,912 (46.0) |
| $15,000 - $39,999 | 1,852 (36.9) |
| < $15,000 | 1,089 (17.1) |
| Education | |
| < High school | 943 (19.2) |
| High school diploma/GED | 1,734 (37.1) |
| Some college | 1,572 (31.9) |
| Bachelor’s degree or more | 604 (11.8) |
| Marital status | |
| Married/Living together | 2,214 (56.8) |
| Not married | 1,187 (22.1) |
| Divorced/Widowed/Separated | 1,452 (21.1) |
| Change in daily smoking | |
| 0 to (+/−) 9% change | 1,912 (41.2) |
| 10–49% reduction | 994 (20.1) |
| 50–99% reduction | 986 (19.5) |
| 100 % reduction | 961 (19.2) |
At Wave 1, 38.8% of daily smokers had history (i.e., current or lifetime history) of mood/anxiety disorder, 50.0% had history of alcohol use disorder, and 24.2% had history of drug use disorder. Among those with history of the disorders at Wave 1, by Wave 2, 40.6% had recurrent/persistent mood/anxiety disorder, 25.1% had recurrent/persistent alcohol use disorder, and 14.8% had recurrent/persistent drug use disorder. Among the groups that did not have current or lifetime history of the diagnosis of interest at Wave 1, 14.3% had new onset of mood/anxiety disorder at Wave 2, 7.0% had new onset of alcohol use disorder at Wave 2 and 2.6% had new onset of drug use disorder at Wave 2.
Figures 1, 2, and 3 show the percent of respondents with current mood/anxiety, alcohol use disorder, and drug use disorders at Wave 2 by change in number of cigarettes smoked daily from Wave 1 to Wave 2, stratified by status of the diagnosis of interest at Wave 1.
Figure 2.
Prevalence of alcohol use disorder within the past 12 months at Wave 2, by smoking reduction from Wave 1 to Wave 2, stratified by status of alcohol abuse/dependence at Wave 1. Circles represent prevalence estimates, and lines represent 95% confidence intervals.
In bivariate logistic regression models (Model 1 in Table 2), among smokers with no lifetime history of the diagnosis of interest at Wave 1, those who quit smoking were much less likely to have new onset of drug use disorder at Wave 2 (odds ratio [OR] 0.3, 95% CI 0.1–0.7). Quitting smoking was not significantly associated with new onset of mood/anxiety disorder or alcohol use disorder at Wave 2. Among smokers with current or lifetime history diagnosis at Wave 1, quitting smoking was associated with a decreased likelihood of recurrent/persistent mood/anxiety disorder (OR 0.6, 95% CI 0.4–0.8), alcohol use disorder (OR 0.6, 95% CI 0.4–0.8), and drug use disorder (OR 0.3, 95% CI 0.1–0.6) at Wave 2. Reducing daily smoking by 50–99% was also associated with a decreased risk of recurrent/persistent alcohol use disorder at Wave 2 (OR 0.7, 95% CI 0.5–0.9).
Models adjusting for the multiple propensity scores (i.e., propensity for 10–49%, 50–99%, and 100% smoking reduction) and additionally for Wave 2 comorbidities are also shown in Table 2 (Models 2 and 3, respectively). Among smokers with no lifetime history of the diagnosis of interest, there was no significant association between reducing smoking and new onset of mood/anxiety disorder or new onset of alcohol use disorder at Wave 2. However, quitting smoking was associated with a decreased risk of new onset of drug use disorder at Wave 2 (adjusting for propensity scores: adjusted odds ratio [aOR] 0.3, 95% CI 0.1–0.7; further adjusting for history of alcohol and mood disorders at Wave 2: aOR 0.3, 95% CI 0.1–0.9).
Associations were more numerous between smoking reduction and decreased risk of recurrent/persistent diagnoses at Wave 2, even after adjustment for propensity scores and Wave 2 comorbidities (Models 2 and 3 in Table 2). Among smokers with current or lifetime history of diagnosis of mood/anxiety disorders at Wave 1, quitting smoking was associated with a decreased risk of recurrent/persistent mood/anxiety disorder at Wave 2 (adjusting for propensity scores: aOR 0.6, 95% CI 0.4–0.9; further adjusting for history of alcohol and drug disorders at Wave 2: aOR 0.6, 95% CI 0.4–0.9). Among smokers with current or lifetime history of diagnosis of alcohol use disorder at Wave 1, quitting smoking was associated with a decreased risk of recurrent/persistent alcohol use disorder at Wave 2 (adjusting for propensity scores: adjusted odds ratio [aOR] 0.6, 95% CI 0.4–0.9; further adjusting for history of alcohol and mood disorders at Wave 2: aOR 0.7, 95% CI 0.5–0.99). Finally, among smokers with current or lifetime history of diagnosis of drug use disorder at Wave 1, quitting smoking was associated with a decreased risk of recurrent/persistent drug use disorder at Wave 2 after adjusting for propensity scores (aOR 0.3, 95% CI 0.1–0.8), but lost significance when additionally adjusting for Wave 2 history of alcohol use disorder and mood/anxiety disorder (but results still trended in the protective direction, aOR 0.5, 95% CI 0.2–1.1).
At Wave 1, among those with either current (within the past 12 months) or lifetime history (prior to past 12 months) diagnosis, 64.7% had a current diagnosis for mood/anxiety disorder, 33.7% had a current diagnosis for alcohol use disorder, and 23.0% had a current diagnosis for drug use disorder. To examine if there were similar associations between smoking cessation and persistent versus recurrent cases at Wave 2, we further stratified the final models by those with current diagnosis at Wave 1 (to examine persistent cases at Wave 2) versus those with lifetime history at Wave 1 (to examine recurrent cases at Wave 2). Results showed that the protective effects of smoking cessation on Wave 2 status of diagnosis appeared slightly stronger for persistent cases than recurrent cases of mood/anxiety disorder (aOR 0.5, 95% CI 0.3–0.8 and aOR 0.9, 95% CI 0.5–1.8, respectively) and alcohol use disorder (aOR 0.5, 95% CI 0.3–0.96 and aOR 95% CI 0.8, 0.4–1.4, respectively). However, confidence intervals were wide and still overlapping between the two groups. The effects of cessation appeared similar for persistent and recurrent cases of drug disorder at Wave 2 (aOR 0.4, 95% CI 0.1–1.9 and aOR 0.4, 95% CI 0.1–1.4, respectively). It should be noted that stratifying models by current or lifetime diagnosis further decreased sample size and thus the power to find statistically significant effects. Results are not presented for smoking reduction categories because these findings were not statistically significant.
Discussion
We examined the effect of reducing or quitting smoking following a 3 year interval on the development of mood/anxiety. We found that among smokers with a prior history of a mood or anxiety disorder, smoking cessation is associated with a lower likelihood of recurrence/persistence of mood and anxiety disorders. If we interpret the smoking- mood/anxiety comorbidity as smokers “treating” their mood and anxiety disorder by smoking, our results support existing studies that found smokers are not at increased risk of mental health problems when they quit smoking (Leistikow & Shipley, 1999; Tsoh et al. 2000; Hall et al. 2006; Klungsoyr et al. 2006; McFall et al. 2006; Munafò et al. 2008; Prochaska et al. 2008; Shahab & West, 2009; Hajek et al. 2010; Torres et al. 2010; Shahab, 2012; Donald et al. 2013; Mathew et al. 2013; Morissette et al. 2012). Additionally, we use a nationally representative sample for generalizability and the propensity score regression adjustment approach to correct for observed differences among smokers with different levels of smoking reduction in order to support causal inferences about the mental health outcomes that follow smoking reduction.
As illustrated by our Figures and odds ratios, mental health status improves when smoking is reduced by 50–99% though statistical significance is not quite reached. Given the reduction of sample size that comes with examining different levels of smoking reduction and mental health outcomes, it may be that we are underpowered to reach statistical significance with regards to the psychological outcomes that accompany smoking reduction.
We also found that among smokers with pre-existing alcohol use disorder (current or lifetime at Wave 1), a recurrence or continuation of their alcohol use disorder was less likely if they quit smoking by Wave 2. In addition, smokers with no history of pre-existing disorder (for outcome of interest) who stopped smoking during the 3 years after the initial assessment were significantly less likely to meet criteria for a past 12 month diagnosis of drug use disorder compared with smokers who continued to smoke the same amount; effect on alcohol use disorder or mood and anxiety disorders trended in the same direction but were not statistically significant. In other words, the risk of incident cases of disorders known to co-occur with smoking was significantly reduced for drug use disorders. Studies over the last 30 years consistently agree that substance use problems and cigarette consumption are correlated; up to 90% of patients in substance abuse treatment settings are smokers (Anthony & Echeagaray-Wagner, 2000; Dawson, 2000; Chiolero et al. 2006). Still, the combined treatment of tobacco smoking and other addiction remains modest (Schroeder & Morris, 2010; Guydish et al. 2011). Despite mounting scientific evidence suggesting otherwise, cessation of both substances (whether heavy alcohol or illicit drug use) and cigarette smoking is often assumed to be too challenging (Romberger & Grant, 2004; Ziedonis et al. 2006). In contrast to this assumption, we found that among smokers with alcohol disorders, smoking cessation is associated with a reduction in the risk of recurrence or persistence of alcohol disorder, with evidence of no risk of relapse; findings trended near significance for drug use disorders. Likewise, smokers without a prior history of drug use disorder did not have a first onset of drug use disorder when they quit their smoking. Previous research has similarly found that former smokers have a higher mental and physical quality of life than those dependent on nicotine (Miller et al. 2000; Bonard et al. 2001; Degenhardt & Hall, 2001; Mulder et al. 2001; Hemmingsson et al. 2008). Thus, the current study along with previous research findings bode well for smokers who quit because it is unlikely that most smokers will spiral into drug addiction problems when they quit smoking.
A limitation of the study is the absence of information on the timing of the events of interest during the 3- year follow-up interval between assessments. Therefore, it might be that some smokers stopped drinking or using drugs (or reduced their use enough that threshold diagnosis was no longer met) before they quit smoking. The sequence of abstinence before smoking cessation would corroborate past findings that document the remission of alcohol use disorder increases the chances of smoking cessation (Breslau et al. 1996). Or, it may be that smoking cessation potentiates a reduction in concurrent substance use behaviors. Importantly, our findings give further support to the notion that persons with both alcohol or other drugs and tobacco use can quit smoking without risking an escalation of problem alcohol and drug use.
Similarly, the direction of the relationship between smoking cessation and recurrence/persistence of mood and anxiety disorders during the 3 year follow-up interval is difficult to disentangle. Existing studies have indicated that the association between cigarette smoking and psychiatric disorders is due to shared antecedent factors (Dierker et al. 2002; Ferguson et al. 2003; McCabe et al. 2004). Related, our findings provide further evidence that smoking and mental health problems are linked. Causation can go in both directions. Specifically, persons who quit smoking may subsequently have a lower likelihood of current depression or anxiety. Conversely, those with remission of the co-morbid disorder may have an easier time quitting smoking. Specifically, individuals may have had better control of their psychiatric illness which in turn also spontaneously triggered smoking cessation versus smoking cessation prompting a remission of the psychiatric illness.
Other limitations should be mentioned. We used propensity scores to adjust for observed differences among smokers with different levels of smoking reduction. However, when calculating the propensity scores we were limited to use of variables collected in the NESARC survey. Therefore, there could be unobserved confounders for which we could not control, such as lifestyle factors that are associated with both likelihood of successful smoking cessation and mental health outcomes but are not included in the NESARC survey. Yet the NESARC provides a rich set of baseline variables and we believe that the most important confounders are included. In addition, we relied on participants’ self-report and our analyses are subject to potential biases introduced by retrospective recall and accuracy of memory. There is some attrition between assessments. Moreover, it may be that individuals under-reported recurrent cigarette smoking and/or psychiatric symptoms because of multiple assessments or interviewer rapport for the respondents that were interviewed by the same interviewer in both NESARC waves. Or, we may not have the correct timeframe to truly capture major psychiatric illnesses which are episodic in nature.
The considerable strengths of this study deserve mention as well. The very large sample size allowed us to estimate incident and persistent cases of disorders of interest separately. Each type of outcome has important scientific and public health implications. The longitudinal nature of the study, with a relatively short follow-up interval---three years--- allowed us to measure change in cigarette consumption and it potential effect on conditions that tend to co-occur with it. A study of change in the purported independent variables in relation to the hypothesized outcomes offers a strong epidemiologic design that brings us closer to the understanding of etiologic pathways. Study findings provide new and important epidemiologic insights into the association between smoking reduction, mental health problems, and alcohol and drug disorders.. Contrary to the widely held assumption that smoking cessation might lead to increases psychiatric symptoms and/or alcohol or drug use, we find no increase and instead find a significant decrease in risk of new cases of drug use disorder. Among smokers with prior comorbid disorders, quitting was associated with reduced risk for mood/anxiety disorders and alcohol disorder. Smokers have a high prevalence of alcohol or drug use disorder and mood/anxiety disorders (Kalman et al. 2005; Lawrence et al. 2009); therefore, the finding that quitting smoking is associated with improved mental health is important news. Smokers can be more compelled to quit with new knowledge that positive behavioral and psychological outcomes can accompany smoking cessation.
Acknowledgements
This publication was made possible by Grant Numbers UL1 RR024992 and KL2 RR024994 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH), and NIH Roadmap for Medical Research and by K02DA021237 from the NIH. Other support includes an ACS IRG-58-010-54 from the American Cancer Society, NIH Career Development Award, (NIDA, K01DA025733) and NIDA, R01 DA032843 awarded to Dr. Cavazos-Rehg, and an NIH Midcareer Investigator Award awarded to Dr. Bierut (K02 DA021237), R01 DA031288 awarded to Dr. Grucza.
Footnotes
Financial Disclosures
LB is listed as an inventor on Issued U.S. Patent 8,080,371,”Markers for Addiction” covering the use of certain SNPs in determining the diagnosis, prognosis, and treatment of addiction. DKH had a grant from Nabi Biopharmaceuticals to test a nicotine immunotherapy.
References
- Adhikari B, Kahende J, Malarcher A, Pechacek T, Tong V. Smoking-attributable mortality, years of potential life lost, and productivity losses—United States, 2000–2004. Morbidity and Mortality Weekly Report. 2008;57:1226–1228. [PubMed] [Google Scholar]
- Anthony JC, Echeagaray-Wagner F. Epidemiologic analysis of alcohol and tobacco use - patterns of co-occurring consumption and dependence in the United States. Alcohol Research and Health. 2000;24:201–208. [PMC free article] [PubMed] [Google Scholar]
- Asher MK, Martin RA, Rohsenow DJ, MacKinnon SV, Traficante R, Monti PM. Perceived barriers to quitting smoking among alcohol dependent patients in treatment. Journal of Substance Abuse Treatment. 2003;24:169–174. doi: 10.1016/s0740-5472(02)00354-9. [DOI] [PubMed] [Google Scholar]
- Baca CT, Yahne CE. Smoking cessation during substance abuse treatment: what you need to know. Journal of Substance Abuse Treatment. 2009;36:205–219. doi: 10.1016/j.jsat.2008.06.003. [DOI] [PubMed] [Google Scholar]
- Becoña E, Vázquez FL, del Carmen Míguez M. Smoking cessation and anxiety in a clinical sample. Personality and Individual Differences. 2002;32:489–494. [Google Scholar]
- Bock BC, Goldstein MG, Marcus BH. Depression following smoking cessation in women. Journal of Substance Abuse. 1996;8:137–144. doi: 10.1016/s0899-3289(96)90151-0. [DOI] [PubMed] [Google Scholar]
- Borrelli B, Niaura R, Keuthen NJ, Goldstein MJ, DePue JD, Murphy C, Abrams DB. Development of major depressive disorder during smoking-cessation treatment. The Journal of Clinical Psychiatry. 1996;57:534–538. doi: 10.4088/jcp.v57n1106. [DOI] [PubMed] [Google Scholar]
- Breslau N, Peterson E, Schultz L, Andreski P, Chilcoat H. Are smokers with alcohol disorders less likely to quit? American Journal of Public Health. 1996;86:985–990. doi: 10.2105/ajph.86.7.985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brookhart MA, Schneeweiss S, Rothman KJ, Glynn RJ, Avorn J, Stürmer T. Variable selection for propensity score models. American Journal of Epidemiology. 2006;163:1149–1156. doi: 10.1093/aje/kwj149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown RA, Lewinsohn PM, Seeley JR, Wagner EF. Cigarette smoking, major depression, and other psychiatric disorders among adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 1996;35:1602–1610. doi: 10.1097/00004583-199612000-00011. [DOI] [PubMed] [Google Scholar]
- Burgess ES, Brown RA, Kahler CW, Niaura R, Abrams DB, Goldstein MG, Miller IW. Patterns of change in depressive symptoms during smoking cessation: who's at risk for relapse? Journal of Consulting and Clinical Psychology. 2002;70:356–361. doi: 10.1037//0022-006X.70.2.356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen CM, Yi H, Dawson DA, Stinson FS, Grant BF. Alcohol use and alcohol use disorders in the United States, a 3-year follow-up: main findings from the 2004–2005 Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Alcohol Epidemiologic Data Reference Manual. 2010:8. [Google Scholar]
- Chen CM, Yi H, Falk DE, Stinson FS, Dawson DA, Grant BF. Alcohol use and alcohol use disorders in the United States: main findings from the 2001–2002 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Alcohol Epidemiologic Data Reference Manual. 2006:8. [Google Scholar]
- Chiolero A, Wietlisbach V, Ruffieux C, Paccaud F, Cornuz J. Clustering of risk behaviors with cigarette consumption: a population-based survey. Preventive Medicine. 2006;42:348–353. doi: 10.1016/j.ypmed.2006.01.011. [DOI] [PubMed] [Google Scholar]
- Cooney JL, Cooney NL, Pilkey DT, Kranzler HRA, Oncken C. Effects of nicotine deprivation on urges to drink and smoke in alcoholic smokers. Addiction. 2003;98:913–921. doi: 10.1046/j.1360-0443.2003.00337.x. [DOI] [PubMed] [Google Scholar]
- Covey LS, Glassman AH, Stetner F. Depression and depressive symptoms in smoking cessation. Comprehensive Psychiatry. 1990;31:350–354. doi: 10.1016/0010-440x(90)90042-q. [DOI] [PubMed] [Google Scholar]
- Covey LS, Glassman AH, Stetner F. Major depression following smoking cessation. The American Journal of Psychiatry. 1997;154:263–265. doi: 10.1176/ajp.154.2.263. [DOI] [PubMed] [Google Scholar]
- Crum RM, La Flair L, Storr CL, Green KM, Stuart EA, Alvanzo AA, Lazareck S, Bolton JM, Robinson J, Sareen J, Mojtabai R. Reports of drinking to self-medicate anxiety symptoms: longitudinal assessment for subgroups of individuals with alcohol dependence. Depression and Anxiety. 2013;30:174–183. doi: 10.1002/da.22024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dawson DA. Drinking as a risk factor for sustained smoking. Drug and Alcohol Dependence. 2000;59:235–249. doi: 10.1016/s0376-8716(99)00130-1. [DOI] [PubMed] [Google Scholar]
- Dierker LC, Avenevoli S, Stolar M, Merikangas KR. Smoking and depression: an examination of mechanisms of comorbidity. The American Journal of Psychiatry. 2002;159:947–953. doi: 10.1176/appi.ajp.159.6.947. [DOI] [PubMed] [Google Scholar]
- Donald S, Chartrand H, Bolton JM. The relationship between nicotine cessation and mental disorders in a nationally representative sample. Journal of Psychiatric Research. 2013;47:1673–1679. doi: 10.1016/j.jpsychires.2013.05.011. [DOI] [PubMed] [Google Scholar]
- Ferguson D, Goodwin RD, Horwood LJ. Major depression and cigarette smoking: results of a 21-year longitudinal study. Psychological Medicine. 2003;33:1357–1367. doi: 10.1017/s0033291703008596. [DOI] [PubMed] [Google Scholar]
- Flach SD, Diener A. Eliciting patients' preferences for cigarette and alcohol cessation: an application of conjoint analysis. Addictive Behaviors. 2004;29:791–799. doi: 10.1016/j.addbeh.2004.02.008. [DOI] [PubMed] [Google Scholar]
- Glassman AH, Covey LS, Stetner F, Rivelli S. Smoking cessation and the course of major depression: a follow-up study. Lancet. 2001;357:1929–1932. doi: 10.1016/S0140-6736(00)05064-9. [DOI] [PubMed] [Google Scholar]
- Grant BF, Moore TC, Shepard J, Kaplan K. National Institute on Alcohol Abuse and Alcoholism. Bethesda, MD: 2003. Source and accuracy statement: Wave 1 National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) [Google Scholar]
- Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2004;61:361–368. doi: 10.1001/archpsyc.61.4.361. [DOI] [PubMed] [Google Scholar]
- Guydish J, Passalacqua E, Tajima B, Chan M, Chun J, Bostrom A. Smoking prevalence in addiction treatment: a review. Nicotine and Tobacco Research. 2011;13:401–411. doi: 10.1093/ntr/ntr048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hajek P, Taylor T, McRobbie H. The effect of stopping smoking on perceived stress levels. Addiction. 2010;105:1466–1471. doi: 10.1111/j.1360-0443.2010.02979.x. [DOI] [PubMed] [Google Scholar]
- Hall SM, Muñoz RF, Reus VI, Sees KL. Nicotine, negative affect, and depression. Journal of Consulting and Clinical Psychology. 1993;61:761–767. doi: 10.1037//0022-006x.61.5.761. [DOI] [PubMed] [Google Scholar]
- Hall SM, Tsoh JY, Prochaska JJ, Eisendrath S, Rossi JS, Redding CA, Rosen AB, Meisner M, Humfleet GL, Gorecki JA. Treatment for cigarette smoking among depressed mental health outpatients: a randomized clinical trial. American Journal of Public Health. 2006;96:1808–1814. doi: 10.2105/AJPH.2005.080382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes JR. Depression during tobacco abstinence. Nicotine & Tobacco Research. 2007;9:443–446. doi: 10.1080/14622200701243185. [DOI] [PubMed] [Google Scholar]
- Hughes JR. Smoking and suicide: a brief overview. Drug and Alcohol Dependence. 2008;98:169–178. doi: 10.1016/j.drugalcdep.2008.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Imbens GW. The role of the propensity score in estimating dose-response functions. Biometrika. 2000;87:706–710. [Google Scholar]
- Kalman D, Morissette SB, George TP. Co-morbidity of smoking in patients with psychiatric and substance use disorders. American Journal of Addictions. 2005;14:106–123. doi: 10.1080/10550490590924728. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Killen JD, Fortmann SP, Schatzberg A, Hayward C, Varady A. Onset of major depression during treatment for nicotine dependence. Addictive Behaviors. 2003;28:61–470. doi: 10.1016/s0306-4603(01)00266-0. [DOI] [PubMed] [Google Scholar]
- Klungsoyr O, Nygard JF, Sorensen T, Sandanger I. Cigarette smoking and incidence of first depressive episode: an 11-year, population-based follow-up study. American Journal of Epidemiology. 2006;163:421–432. doi: 10.1093/aje/kwj058. [DOI] [PubMed] [Google Scholar]
- Kohn CS, Tsoh JY, Weisner CM. Changes in smoking status among substance abusers: baseline characteristics and abstinence from alcohol and drugs at 12-month follow-up. Drug and Alcohol Dependence. 2003;69:61–71. doi: 10.1016/s0376-8716(02)00256-9. [DOI] [PubMed] [Google Scholar]
- Launiainen T, Broms U, Keskitalo-Vuokko K, Pitkäniemi J, Pelander A, Kaprio J, Ojanperä I. Nicotine, alcohol, and drug findings in young adults in a population-based postmortem database. Nicotine and Tobacco Research. 2011;13:763–771. doi: 10.1093/ntr/ntr069. [DOI] [PubMed] [Google Scholar]
- Lawrence D, Mitrou F, Zubrick SR. Smoking and mental illness: results from population surveys in Australia and the United States. BMC Public Health. 2009;9:285. doi: 10.1186/1471-2458-9-285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leistikow BN, Shipley MJ. Might stopping smoking reduce injury death risks? A meta-analysis of randomized, controlled trials. Preventive Medicine. 1999;28:255–259. doi: 10.1006/pmed.1998.0412. [DOI] [PubMed] [Google Scholar]
- Lewinsohn PM, Rohde P, Brown RA. Level of current and past adolescent cigarette smoking as predictors of future substance use disorders in young adulthood. Addiction. 1999;94:913–921. doi: 10.1046/j.1360-0443.1999.94691313.x. [DOI] [PubMed] [Google Scholar]
- Mathew AR, Robinson JD, Norton PJ, Cinciripini PM, Brown RA, Blalock JA. Affective trajectories before and after a quit attempt in smokers with current depressive disorders. Nicotine and Tobacco Research. 2013 Mar 18; doi: 10.1093/ntr/ntt036. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCabe RE, Chudzik SM, Antony MM, Young L, Swinson RP, Zolvensky MJ. Smoking behaviors across anxiety disorders. Journal of Anxiety Disorders. 2004;18:7–18. doi: 10.1016/j.janxdis.2003.07.003. [DOI] [PubMed] [Google Scholar]
- McFall M, Atkins DC, Yoshimoto D, Thompson CE, Kanter E, Malte CA, Saxon AJ. Integrating tobacco cessation treatment into mental health care for patients with posttraumatic stress disorder. The American Journal on Addictions. 2006;15:336–344. doi: 10.1080/10550490600859892. [DOI] [PubMed] [Google Scholar]
- Morissette SB, Gulliver SB, Kamholz BW, Spiegel DA, Tiffany ST, Barlow DH. Transdermal nicotine during cue reactivity in adult smokers with and without anxiety disorders. Psychology of Addictive Behaviors. 2012;26:507–518. doi: 10.1037/a0028828. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Munafò MRB, Hitsman B, Rende R, Metcalfe C, Niaura R. Effects of progression to cigarette smoking on depressed mood in adolescents: evidence from the National Longitudinal Study of Adolescent Health. Addiction. 2008;103:162–171. doi: 10.1111/j.1360-0443.2007.02052.x. [DOI] [PubMed] [Google Scholar]
- Myers MG, Kelly JF. Cigarette smoking among adolescents with alcohol and other drug use problems. Alcohol Research and Health. 2006;29:221–227. [PMC free article] [PubMed] [Google Scholar]
- Patten CA, Rummans TA, Croghan IT, Hurt RD, Hays JT. Development of depression during placebo-controlled trials of bupropion for smoking cessation: case reports. The Journal of Clinical Psychiatry. 1990;60:436–441. doi: 10.4088/jcp.v60n0703. [DOI] [PubMed] [Google Scholar]
- Pirie K, Peto R, Reeves GK, Green J, Beral V. The 21st century hazards of smoking and benefits of stopping: a prospective study of one million women in the UK. Lancet. 2013;381:133–141. doi: 10.1016/S0140-6736(12)61720-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JJ, Delucchi K, Hall SM. A meta-analysis of smoking cessation interventions with individuals in substance abuse treatment or recovery. Journal of Consulting and Clinical Psychology. 2004a;72:1144–1156. doi: 10.1037/0022-006X.72.6.1144. [DOI] [PubMed] [Google Scholar]
- Prochaska JJ, Hall SM, Tsoh JY, Eisendrath S, Rossi JS, Redding CA, Rosen AB, Meisner M, Humfleet GL, Gorecki JA. Treating tobacco dependence in clinically depressed smokers: effect of smoking cessation on mental health functioning. American Journal of Public Health. 2008;98:446–448. doi: 10.2105/AJPH.2006.101147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prochaska JJ, Rossi JS, Redding CA, Rosen AB, Tsoh JY, Humfleet GL, Eisendrath SJ, Meisner MR, Hall SM. Depressed smokers and stage of change: implications for treatment interventions. Drug and Alcohol Dependence. 2004b;76:143–151. doi: 10.1016/j.drugalcdep.2004.04.017. [DOI] [PubMed] [Google Scholar]
- Ramsey SE, Brown RA, Strong DR, Stuart GL, Weinstock MC, Myers MG. Cigarette smoking and substance use among adolescents in psychiatric treatment. Journal of Child and Adolescent Substance Abuse. 2005;14:1–13. [Google Scholar]
- Rohsenow DJ, Colby SM, Martin RA, Monti PM. Nicotine and other substance interaction expectancies questionnaire: relationship of expectancies to substance use. Addictive Behaviors. 2005;30:629–641. doi: 10.1016/j.addbeh.2005.01.001. [DOI] [PubMed] [Google Scholar]
- Romberger DJ, Grant K. Alcohol consumption and smoking status: the role of smoking cessation. Biomedicine and Pharmacotherapy. 2004;58:77–83. doi: 10.1016/j.biopha.2003.12.002. [DOI] [PubMed] [Google Scholar]
- Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- Ruan WJ, Goldstein RB, Chou SP, Smith SM, Saha TD, Pickering RP, Dawson DA, Huang B, Stinson FS, Grant BF. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample. Drug and Alcohol Depenence. 2008;92:27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schroeder SA, Morris CD. Confronting a neglected epidemic: tobacco cessation for persons with mental illnesses and substance abuse problems. Annual Review of Public Health. 2010;31:297–314. doi: 10.1146/annurev.publhealth.012809.103701. [DOI] [PubMed] [Google Scholar]
- Seidner AL, Burling TA, Gaither DE, Thomas RG. Substance-dependent inpatients who accept smoking treatment. Journal of Substance Abuse. 1996;8:33–44. doi: 10.1016/s0899-3289(96)90067-x. [DOI] [PubMed] [Google Scholar]
- Shah BV, Branwell G, Bieler GS. The SUDAAN User's Manual, Release 7.5. Research Triangle Park, NC; 2002. Research Triangle Institute. [Google Scholar]
- Shahab L, West R. Do ex-smokers report feeling happier following cessation? Evidence from a cross-sectional survey. Nicotine & Tobacco Research. 2009;11:553–557. doi: 10.1093/ntr/ntp031. [DOI] [PubMed] [Google Scholar]
- Shahab L, West R. Differences in happiness between smokers, ex-smokers and never smokers: cross-sectional findings from a national household survey. Drug and Alcohol Dependence. 2012;121:38–44. doi: 10.1016/j.drugalcdep.2011.08.011. [DOI] [PubMed] [Google Scholar]
- Shiffman S. Relapse following smoking cessation: a situational analysis. Journal of Consulting and Clinical Psychology. 1982;50:71–86. doi: 10.1037//0022-006x.50.1.71. [DOI] [PubMed] [Google Scholar]
- Spreeuwenberg MD, Bartak A, Croon MA, Hagenaars JA, Busschbach JJ, Andrea H, Twisk J, Stijnen T. The multiple propensity score as control for bias in the comparison of more than two treatment arms: an introduction from a case study in mental health. Medical Care. 2010;48:166–174. doi: 10.1097/MLR.0b013e3181c1328f. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Alcohol abuse and smoking - dual recoveries. Alcohol Health and Research World. 1996;20:124–127. [PMC free article] [PubMed] [Google Scholar]
- Stage KB, Glassman AH, Covey LS. Depression after smoking cessation: case reports. The Journal of Clinical Psychiatry. 1996;57:467–469. doi: 10.4088/jcp.v57n1005. [DOI] [PubMed] [Google Scholar]
- Stuyt EB. Recovery rates after treatment for alcohol/drug dependence: tobacco users vs. non-tobacco users. The American Journal on Addictions. 1997;6:159–167. [PubMed] [Google Scholar]
- Tobias M, Templeton R, Collings S. How much do mental disorders contribute to New Zealand's tobacco epidemic? Tobacco Control. 2008;17:347–350. doi: 10.1136/tc.2008.026005. [DOI] [PubMed] [Google Scholar]
- Torres LD, Barrera AZ, Delucchi K, Penilla C, Pérez-Stable EJ, Muñoz RF. Quitting smoking does not increase the risk of major depressive episodes among users of Internet smoking cessation interventions. Psychological Medicine. 2010;40:441–449. doi: 10.1017/S0033291709990560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trends in current cigarette smoking among high school students and adults, United States, 1965–2011. [Accessed 7 Dec 2012];Centers for Disease Control and Prevention. http://www.cdc.gov/tobacco/data_statistics/tables/trends/cig_smoking/
- Tsoh JY, Humfleet GL, Munoz RF, Reus VI, Hartz DT, Hall SM. Development of major depression after treatment for smoking cessation. The American Journal of Psychiatry. 2000;157:368–374. doi: 10.1176/appi.ajp.157.3.368. [DOI] [PubMed] [Google Scholar]
- Upadhyaya HP, Deas D, Brady KT, Kruesi M. Cigarette smoking and psychiatric comorbidity in children and adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41:1294–1305. doi: 10.1097/00004583-200211000-00010. [DOI] [PubMed] [Google Scholar]
- Viswanath K, Herbst RS, Land SR, Leischow SJ, Shields PG. Tobacco and cancer: an American Association for Cancer Research policy statement. Cancer Research. 2010;70:3419–3430. doi: 10.1158/0008-5472.CAN-10-1087. [DOI] [PubMed] [Google Scholar]
- West R, Hajek P. What happens to anxiety levels on giving up smoking? American Journal of Psychiatry. 1997;154:1589–1592. doi: 10.1176/ajp.154.11.1589. [DOI] [PubMed] [Google Scholar]
- Zanutto E, Lu B, Hornik R. Using propensity score subclassification for multiple treatment doses to evaluate a national antidrug media campaign. Journal of Educational and Behavioral Statistics. 2005;30:59–73. [Google Scholar]
- Ziedonis DM, Guydish J, Williams J, Steinberg M, Foulds J. Barriers and solutions to addressing tobacco dependence in addiction treatment programs. Alcohol Research and Health. 2006;29:228–235. [PMC free article] [PubMed] [Google Scholar]