Abstract
Background
Persons with end-stage renal disease (ESRD) on hemodialysis carry an exceptionally high burden of cardiovascular disease. Angiotensin-converting enzyme inhibitors (ACEIs) are recommended for patients on dialysis, but there are few data regarding their effectiveness in ESRD.
Methods
We conducted a secondary analysis of results of the HEMO study, a randomized trial of dialysis dose and membrane flux in patients on maintenance hemodialysis. We focused on the nonrandomized exposure of ACEI use, using proportional hazards regression and a propensity score analysis. The primary outcome was all-cause mortality. Secondary outcomes examined in the present analysis were cardiovascular hospitalization, heart failure hospitalization, and the composite outcomes of death or cardiovascular hospitalization and death or heart failure hospitalization.
Results
In multivariable-adjusted analyses, there were no significant associations among ACEI use and mortality (hazard ratio 0.97, 95% CI 0.82–1.14), cardiovascular hospitalization, and either composite outcome. Angiotensin-converting enzyme inhibitor use was associated with a higher risk of heart failure hospitalization (hazard ratio 1.41, 95% CI 1.11–1.80). In the propensity score–matched cohort, ACEI use was not significantly associated with any outcomes, including heart failure hospitalization.
Conclusions
In a well-characterized cohort of patients on maintenance hemodialysis, ACEI use was not significantly associated with mortality or cardiovascular morbidity. The higher risk of heart failure hospitalization associated with ACEI use may not only reflect residual confounding but also highlights gaps in evidence when applying treatments proven effective in the general population to patients with ESRD. Our results underscore the need for definitive trials in ESRD to inform the treatment of cardiovascular disease.
Angiotensin-converting enzyme inhibitors (ACEIs) have been shown to reduce mortality and cardiovascular morbidity in a variety of clinical scenarios, such as postacute myocardial infarction or in patients with heart failure or left ventricular dysfunction.1–3 Persons with end-stage renal disease (ESRD) on dialysis carry an exceptionally high burden of cardiovascular disease, with 45% of all deaths attributed to cardiovascular causes.4 Although current national clinical practice guidelines5 recommend the use of ACEIs in patients on maintenance dialysis, there are few data regarding their effectiveness for cardiovascular disease prevention in this population because randomized clinical trials of ACEIs systematically excluded patients with ESRD.
Given the uncertainty surrounding the effectiveness of ACEIs in patients on maintenance hemodialysis, we conducted a secondary analysis of data from the HEMO study.6 The HEMO study data have several advantages over previous observational studies, in that the data contain exceptionally detailed clinical information, allowing for improved case-mix adjustment, and clinical outcomes were rigorously adjudicated using standardized criteria rather than determined by administrative codes. We hypothesized that subjects receiving ACEIs at study entry would have lower risks of mortality and cardiovascular morbidity compared with subjects who did not receive this class of medication.
Methods
Study population
Details of the HEMO study protocol have been published previously.6,7 Briefly, the HEMO study was a randomized clinical trial of 1,846 prevalent hemodialysis patients between 18 and 80 years old from 15 US clinical centers composed of 72 dialysis units. Subjects were enrolled between March 1995 and October 2000 and randomly assigned in a 2 × 2 factorial design to standard or high equilibrated Kt/V urea and low- or high-flux dialyzers. Subjects were followed up until death or the administrative end of study (December 2001). When studying the end point of death, we censored subjects at time of kidney transplant only because the HEMO study continued to collect survival information even after transfer to a nonparticipating clinical center. However, when studying end points that included hospitalization, we censored subjects at the time of kidney transplant and transfer to a nonparticipating clinical center because information regarding hospitalization was not collected after patient transfer to nonparticipating clinical centers in the HEMO study.
Medication use
In the HEMO study, use of the following classes of medications was ascertained from the hemodialysis chart or from the patient: ACEIs, angiotensin II receptor blockers (ARBs), β-blockers, calcium-channel blockers, α-1 antagonists (eg, terazosin), minoxidil, adrenergic stimulants (eg, clonidine), erythropoietin, aspirin, warfarin, nitrates, and vitamin D replacement (either oral or intravenous). Dose was not recorded. Although both ARBs and ACEIs inhibit the renin-angiotensin-aldosterone system, these 2 classes of medications may have different associations with outcomes. We were unable to analyze ARB users separately because very few subjects were using ARBs at the time of the HEMO study (n = 26). We, therefore, excluded subjects taking ARBs at study entry for our primary analyses (final total n = 1820). We conducted additional sensitivity analyses that included the 26 subjects who were using ARBs along with ACEI users in the analysis.
Outcomes
Our primary outcome of interest was all-cause mortality. We also examined the association of ACEI use with hospitalization. Specifically, we examined cardiovascular hospitalization (defined as hospitalization for ischemic heart disease, heart failure, arrhythmias, other cardiac conditions, hypertension, and peripheral vascular disease). Given the particular indication of ACEIs for the treatment of heart failure,2,8,9 we examined heart failure hospitalization separately. To account for issues of competing risks, we analyzed the composite outcomes of all-cause mortality or cardiovascular hospitalization and all-cause mortality or heart failure hospitalization. We conducted an additional sensitivity analysis that excluded heart failure hospitalization from cardiovascular hospitalizations.
All deaths were reported to the data coordinating center within 6 weeks of the event, and the cause of death was adjudicated by the outcomes committee after review of the medical records. All hospitalizations were reported to the data coordinating center within 2 weeks of the event, and assignments of causes of hospitalization were based on review of the discharge summary and/or telephone call to the attending physician.
Statistical methods
Baseline characteristics for the cohort are described as mean (SD) for continuous variables or as frequencies for categorical variables. We compared differences between groups by baseline ACEI use using the Student t test or χ2 test as appropriate. We also reported standardized differences among ACEI users and ACEI nonusers. Standardized differences for continuous variables are calculated by taking the difference in means between ACEI users and ACEI nonusers for a given variable and dividing it by the average SD for the 2 groups; standardized differences for dichotomous variables are calculated in an analogous manner.10 It has been suggested that a standardized difference of >10% represents meaningful imbalance between treatment groups.10,11
We analyzed the association of ACEI use with all-cause mortality using bivariable- and multivariable-adjusted Cox proportional hazards regression. In multivariable-adjusted models we included the following covariates assessed at study entry: age; sex; race (black vs nonblack); years on dialysis (in quartiles); residual urea clearance adjusted for total body water (in tertiles); marital status (married or partnered vs not); Quetélet (body mass) index (kg/m2); serum potassium (mmol/L); serum albumin (g/dL); predialysis systolic blood pressure (mm Hg, as a linear and quadratic term); whether the patient had been sick in the week before the visit (yes vs no); and the following comorbid conditions (present vs absent): ischemic heart disease, arrhythmias, heart failure, other cardiac disease, diabetes mellitus, cerebrovascular disease, peripheral vascular disease, musculoskeletal disease, nonvascular nervous system disease, gastrointestinal disease, hepatic disease, ophthalmological disease, and malignancy. We adjusted for baseline use of the following classes of medications: β-blockers, calcium-channel blockers, minoxidil, adrenergic stimulants, nitrates, aspirin, and warfarin use. We chose these covariates because several were shown to be significant independent predictors of mortality in the HEMO study,6 whereas others were significantly (P < .1) associated with ACEI use and/or outcomes. All analyses were stratified by clinical center to account for potential differences in baseline hazard functions in different clinical centers.
We tested for effect modification by including a multiplicative interaction term with ACEI use by age (dichotomized at the median of 60 years); race (black vs nonblack); and a history of heart failure, diabetes mellitus, or ischemic heart disease.
To minimize potential confounding by indication given the nonrandomized nature of our analysis, we also conducted a companion propensity score analysis.12 We used logistic regression to calculate the probability of ACEI use vs ACEI nonuse at study entry using the same variables included in the multivariable-adjusted models. Our propensity score had a concordance statistic (corresponding to the area under the receiver operating characteristic curve) of 0.703. We used a greedy match algorithm13 to pair ACEI users with ACEI nonusers in a 1:1 ratio whose difference in propensity score was <0.03, as has been done previously.14 To avoid the center effect, we only matched subjects who were within the same clinical center. We were able to match 408 ACEI users (89.1%) to 408 ACEI nonusers using this algorithm. We also conducted Cox proportional hazards regression in the propensity score–matched cohort, including an adjustment for age, sex, and race. To account for matching, we stratified the analysis by matched pairs.
We tested the proportionality assumption with log-negative-log plots. We calculated hazard ratios (HRs) and 95% CI from model parameter estimates and SEs, respectively. We considered 2-tailed P values <.05 statistically significant. All analyses were conducted with SAS Enterprise Guide 4.2 (Cary, NC).
Dr Chang was supported by an American Heart Association fellowship award; Dr Chertow was supported by NIH K24 DK085446. The authors are solely responsible for the design and conduct of this study, all study analyses, the drafting and editing of the manuscript, and its final contents.
Results
At study entry, 458 subjects (25.2%) were using ACEIs. In the unmatched sample, 12 of the 31 covariates had standardized differences that exceeded 10% (Table I). Angiotensin-converting enzyme inhibitor users tended to be younger; had a higher prevalence of heart failure, diabetes mellitus, and musculoskeletal disease; and were more often sick in the week previous to the baseline visit. Angiotensin-converting enzyme inhibitor users also had higher predialysis systolic blood pressure, higher baseline serum potassium, and slightly more residual kidney function. After propensity score matching, standardized differences in the matched cohort were all <6% (Table I).
Table I.
Baseline characteristics of the HEMO study cohort before and after propensity score matching
| Baseline characteristics | Before propensity score matching
|
After propensity score matching
|
||||||
|---|---|---|---|---|---|---|---|---|
| ACEI nonuser n = 1362 |
ACEI user n = 458 |
P | Std Diff (%) | ACEI nonuser n = 408 |
ACEI user n = 408 |
P | Std Diff (%) | |
| Age, y | 58.2 (13.8) | 56.0 (14.8) | .004 | 15.4 | 57.1 (14.4) | 56.6 (14.6) | .6 | 3.4 |
| Female sex | 56.2 | 55.5 | .8 | 1.0 | 55.4 | 55.2 | .9 | 0.3 |
| Black race | 63.4 | 60.7 | .3 | 3.9 | 61.8 | 60.1 | .6 | 2.5 |
| Duration of dialysis, y | 3.9 (4.4) | 3.5 (4.2) | .1 | 9.3 | 3.7 (4.5) | 3.6 (4.3) | .9 | 2.3 |
| Married/partnered | 37.7 | 42.6 | .06 | 7.1 | 43.4 | 41.7 | .6 | 2.4 |
| Body mass index, kg/m2 | 25.6 (5.3) | 24.8 (5.2) | .003 | 15.2 | 25.1 (4.9) | 25.1 (5.2) | .9 | 0.3 |
| History of | ||||||||
| Ischemic heart disease | 39.0 | 38.9 | .96 | 0.1 | 41.9 | 40.9 | .8 | 1.4 |
| Arrhythmias | 30.6 | 31.2 | .8 | 0.9 | 31.9 | 32.4 | .9 | 0.8 |
| Heart failure | 35.8 | 50.0 | <.0001 | 20.5 | 47.6 | 45.8 | .6 | 2.6 |
| Other heart conditions | 61.8 | 65.9 | .1 | 6.0 | 69.1 | 65.4 | .3 | 5.6 |
| Cerebrovascular disease | 18.7 | 22.3 | .1 | 6.3 | 21.3 | 21.8 | .9 | 0.9 |
| Peripheral vascular disease | 24.7 | 27.5 | .2 | 4.5 | 26.2 | 27.5 | .7 | 2.1 |
| Diabetes mellitus | 42.7 | 49.3 | .01 | 9.4 | 47.3 | 49.3 | .6 | 2.8 |
| Musculoskeletal disease | 45.3 | 39.1 | .02 | 8.9 | 42.7 | 40.7 | .6 | 2.9 |
| Nonvascular nervous system disease | 37.0 | 37.6 | .8 | 0.9 | 38.7 | 37.8 | .8 | 1.3 |
| Gastrointestinal disease | 36.6 | 37.6 | .7 | 1.5 | 36.3 | 38.7 | .5 | 3.5 |
| Hepatic disease | 17.6 | 16.8 | .7 | 1.5 | 18.4 | 17.7 | .8 | 1.3 |
| Malignancy | 9.2 | 8.1 | .5 | 2.8 | 9.8 | 8.6 | .5 | 2.9 |
| Ophthalmologic disease | 27.5 | 32.1 | .06 | 7.1 | 31.6 | 31.9 | .9 | 0.5 |
| Sick in past 7 d | 22.2 | 28.6 | .005 | 10.4 | 24.5 | 28.2 | .2 | 5.9 |
| Predialysis systolic blood pressure, mm Hg | 150 (22) | 158 (22) | <.0001 | 36.3 | 156 (22) | 156 (22) | .9 | 0.9 |
| Serum potassium, mEq/L | 4.8 (0.8) | 5.0 (0.8) | .0003 | 25.0 | 4.9 (0.8) | 4.9 (0.7) | .9 | 1.0 |
| Serum albumin, g/dL | 3.6 (0.36) | 3.6 (0.37) | .0003 | 2.8 | 3.6 (0.35) | 3.6 (0.37) | >.99 | 0.0 |
| Residual urea clearance adjusted to Watson’s V, mL/min per 35 L | 0.2 (0.4) | 0.3 (0.6) | .005 | 19.9 | 0.2 (0.4) | 0.3 (0.4) | .7 | 2.7 |
| Other baseline medication use | ||||||||
| β-Blockers | 27.9 | 35.2 | .003 | 11.9 | 34.8 | 34.1 | .8 | 1.0 |
| Calcium-channel blockers | 46.8 | 55.5 | .001 | 13.4 | 56.4 | 53.7 | .4 | 3.8 |
| Minoxidil | 1.1 | 3.1 | .004 | 11.4 | 2.5 | 2.9 | .7 | 1.7 |
| Adrenergic agonists | 2.4 | 5.0 | .005 | 12.7 | 4.7 | 3.9 | .6 | 2.8 |
| Nitrates | 16.1 | 20.3 | .04 | 7.7 | 19.6 | 21.3 | .5 | 3.0 |
| Aspirin | 25.9 | 33.4 | .002 | 12.1 | 31.9 | 33.3 | .7 | 2.1 |
| Coumadin | 8.7 | 10.5 | .3 | 4.8 | 11.8 | 10.5 | .6 | 2.9 |
Values are percentages or mean (SD). P value was calculated using χ2 test or t tests as appropriate. Std Diff, Standardized difference.
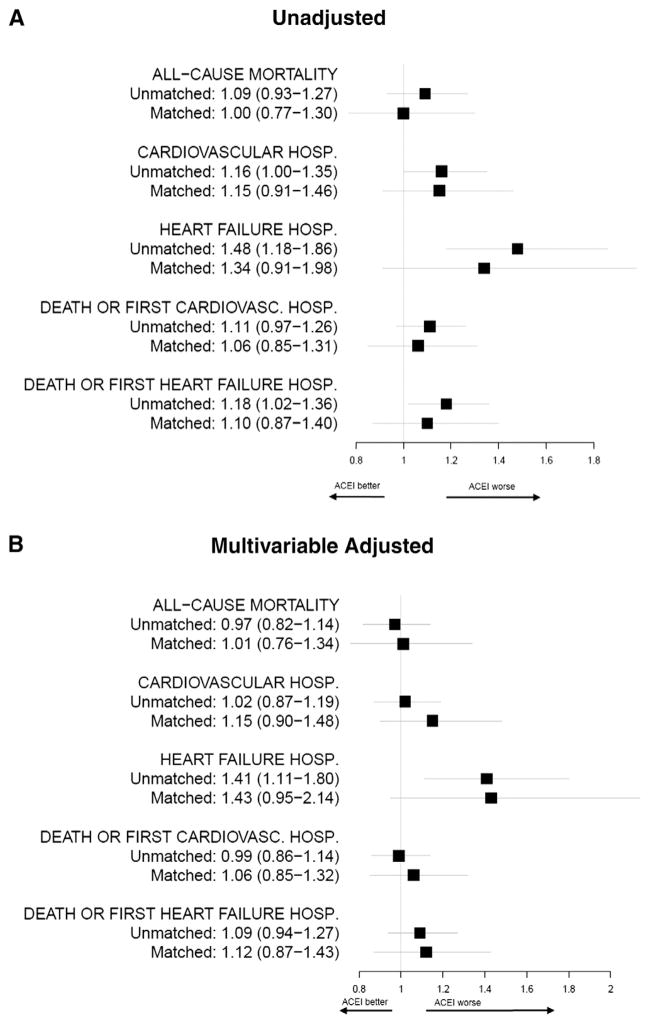
During a median of 2.5 years (interquartile range 1.3–4.3) of follow-up, there were 866 deaths. Nine hundred fifty-two subjects reached the end point of cardiovascular hospitalizations, and 362 subjects reached the end point of heart failure hospitalizations in the unmatched cohort. Using bivariable- and multivariable-adjusted Cox proportional hazards regression, we found no significant association of ACEI use with all-cause mortality, cardiovascular hospitalization, or with the composite end point of death or cardiovascular hospitalization (Figure 1A and B). However, ACEI use was associated with a 48% (95% CI 18%–86%) higher risk of heart failure hospitalization, which persisted even after multivariable adjustment. Age; race; or a prior history of heart failure, diabetes mellitus, or ischemic heart disease did not modify the association of ACEI use and heart failure hospitalization or any of the other outcomes investigated (P interaction >.05 in all cases).
Figure 1.
A and B, Forest plots showing the association of ACEI use versus ACEI nonuse on clinical outcomes in the unmatched and propensity score–matched cohorts. Values shown are HRs (95% CIs). A, Results from unadjusted analyses. B, Results in the unmatched cohort adjusted for age; sex; race (black vs nonblack); years on dialysis (in quartiles); residual urea clearance adjusted for total body water (in tertiles); marital status (married or partnered vs not); Quetélet (body mass) index (kg/m2); serum potassium (mmol/L); serum albumin (g/dL); predialysis systolic blood pressure (mm Hg, as a linear and quadratic term); whether the patient had been sick in the week before the visit; ischemic heart disease; arrhythmias; heart failure; other cardiac disease; diabetes mellitus; cerebrovascular disease; peripheral vascular disease; musculoskeletal disease; nonvascular nervous system disease; gastrointestinal disease; hepatic disease; ophthalmological disease; malignancy; and baseline use of β-blockers, calcium-channel blockers, minoxidil, adrenergic stimulants, nitrates, aspirin, and warfarin use. In the propensity score–matched cohort, results were adjusted for age, sex, and black race. HOSP, Hospitalization. Cardiovascular hospitalization includes ischemic heart disease, heart failure, arrhythmia, other cardiac conditions, hypertension, and peripheral vascular disease.
In the propensity score–matched cohort, there were 409 deaths; 446 subjects reached the end point of cardiovascular hospitalizations, and 188 subjects reached the end point of heart failure hospitalizations. Similar to results from the unmatched cohort, ACEI use was not significantly associated with any of the clinical outcomes in the propensity score–matched cohort (Figure 1A and B). Notably, the association of ACEI use with higher risk of heart failure hospitalization no longer met statistical significance.
Our results did not materially change in sensitivity analyses that included ARB users along with ACEI users (data not shown). Analyses of cardiovascular hospitalizations that excluded heart failure hospitalizations showed no significant association with ACEI use in the unmatched and matched cohorts (data not shown).
Discussion
Our analysis demonstrated that, in a well-characterized cohort of patients on maintenance hemodialysis, ACEI use was not significantly associated with mortality or cardiovascular hospitalization. Our results are generally consistent with several previous retrospective cohort studies that used data from the United States Renal Data System.15–20 The major strength of our present analysis is that, in contrast to the previous studies, the carefully collected data in the HEMO study allowed us to improve our case-mix adjustment and classification of clinical outcomes.
Our results contrast with 2 studies in patients on maintenance dialysis showing an association between ACEI and lower mortality. Winkelmayer et al21 showed that ACEI use and ARB use were associated with a 30% (95% CI 2%–50%) reduction in 1-year mortality. Similarly, Berger et al22 demonstrated a 42% (95% CI 23%–58%) lower risk of 30-day mortality associated with ACEI use; longer term follow-up in this cohort has not been published. However, both of these studies differed from the present analysis in that they were conducted in patients who had recently experienced an acute myocardial infarction. Moreover, the study by Winkelmayer et al was conducted in low-income elderly patients who had an exceptionally high 1-year mortality of 63.6%. By comparison, the 1-year mortality in the HEMO study was 16.6%.6
Our results are consistent with the only placebo-controlled, randomized trial of ACEIs in patients on hemodialysis examining cardiovascular events whose results have been published to date.23 The FOSIDIAL study randomized 397 patients on maintenance hemodialysis with left ventricular hypertrophy to receive fosinopril or placebo for 2 years. Treatment with fosinopril did not significantly change the composite outcome of cardiovascular death or cardiovascular events (HR 0.93, 95% CI 0.68–1.26). However, as the FOSIDIAL authors acknowledged, the trial was underpowered because the actual event rate of 32.7% was much lower than the anticipated event rate of 50% over 2 years of follow-up.
We found an increased risk of heart failure hospitalization associated with ACEI use in the unmatched cohort. Our results contrast with previous studies using data from the United States Renal Data System showing no significant association of ACEI use with heart failure hospitalization.19,24 Given the reported beneficial effects of ACEIs in ESRD on regression of left ventricular hypertrophy25 and reduced vascular stiffness,26 we suspect that these results could have either arisen from chance because we did not adjust for multiple comparisons or from residual confounding not addressed by multivariable adjustment. Notably, analyses with the propensity score–matched cohort did not show a statistically significant association of ACEI use with heart failure hospitalization, although the effect estimates were similar to the unmatched cohort. Propensity score matching may have better accounted for residual confounding, but the lack of statistical significance could also be attributed to the slightly smaller sample size and number of events contained within the matched cohort.
Current clinical guidelines recommend ACEIs and ARBs interchangeably for patients on hemodialysis.5 However, ARBs are not removed by hemodialysis, whereas most ACEIs are removed to a variable extent27; and there is evidence that these 2 classes of medications may have different effects on clinical outcomes. In a recent analysis of data from the Dialysis Outcomes and Practice Patterns Study,28 ARB use was associated with a lower risk of all-cause mortality compared with patients not taking ARBs (relative risk 0.93, P = .05); but no significant association with mortality was seen with ACEI use (relative risk 1.00, P = .89). In a recent randomized clinical trial, Cice et al29 showed that among patients on maintenance hemodialysis with low ejection fraction and clinical heart failure, treatment with an ARB versus placebo in addition to an ACEI-based medication regimen reduced all-cause mortality by 49% (95% CI 18%–68%). In the HEMO study, very few subjects were taking ARBs at study entry, precluding separate analyses for these subjects, with or without concomitant ACEIs.
The HEMO study data had many advantages over other cohorts used in previous observational analyses, but there were also several limitations. First, as with any observational study of comparative effectiveness, subjects were not randomly assigned to receive ACEIs or not. Therefore, despite our use of multivariable adjustment and propensity score–matching techniques to reduce confounding by indication, unmeasured factors could still result in residual confounding. Second, because we did not have detailed information on when medications were initiated or discontinued, we could not analyze longitudinal medication use and were unable to construct a “new user” cohort.30 By analyzing prevalent ACEI users, we could not adjust for subjects’ characteristics at the time of ACEI initiation. Third, we did not have information on doses or individual medications within each class, although we would not expect substantial differences between specific types of ACEIs on clinical outcomes. Finally, although the HEMO study cohort appears similar to the US prevalent hemodialysis population in most measured characteristics, the generalizability of the HEMO study data might be restricted by its nature as a randomized clinical trial.
In summary, our analysis did not demonstrate an association of ACEI use with cardiovascular morbidity and mortality. Given the observational nature of our analysis, our results should not be used as justification for withholding of treatment with ACEIs in ESRD. Rather, our analysis highlights gaps in the evidence when applying treatment strategies effective in the non-ESRD population to patients on maintenance hemodialysis. Our results also underscore the need for definitive randomized clinical trials in patients on dialysis to inform the treatment of hypertension and other cardiovascular diseases.
Footnotes
Disclosures
The HEMO study was conducted by the HEMO Study Investigators and supported by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). The data from the HEMO study reported here were supplied by the NIDDK Central Repositories. This manuscript was not prepared in collaboration with Investigators of the HEMO study and does not necessarily reflect the opinions or views of the HEMO study, the NIDDK Central Repositories, or the NIDDK.
References
- 1.CONSENSUS Trial Study Group. Effects of enalapril on mortality in severe congestive heart failure. Results of the Cooperative North Scandinavian Enalapril Survival Study (CONSENSUS). The CONSENSUS Trial Study Group. N Engl J Med. 1987;316:1429–35. doi: 10.1056/NEJM198706043162301. [DOI] [PubMed] [Google Scholar]
- 2.SOLVD Investigators. Effect of enalapril on survival in patients with reduced left ventricular ejection fractions and congestive heart failure. The SOLVD investigators. N Engl J Med. 1991;325:293–302. doi: 10.1056/NEJM199108013250501. [DOI] [PubMed] [Google Scholar]
- 3.Indications for ACE inhibitors in the early treatment of acute myocardial infarction: systematic overview of individual data from 100 000 patients in randomized trials. Circulation. 1998;97:2202–12. doi: 10.1161/01.cir.97.22.2202. [DOI] [PubMed] [Google Scholar]
- 4.U.S. Renal Data System. USRDS 2010 annual data report: atlas of chronic kidney disease and end-stage renal disease in the United States. Bethesda, MD: National Institutes of Health NIDDK; 2010. [Google Scholar]
- 5.K/DOQI clinical practice guidelines for cardiovascular disease in dialysis patients. Am J Kidney Dis. 2005;45:S1–S153. [PubMed] [Google Scholar]
- 6.Eknoyan G, Beck GJ, Cheung AK, et al. Effect of dialysis dose and membrane flux in maintenance hemodialysis. N Engl J Med. 2002;347:2010–9. doi: 10.1056/NEJMoa021583. [DOI] [PubMed] [Google Scholar]
- 7.Greene T, Beck GJ, Gassman JJ, et al. Design and statistical issues of the hemodialysis (HEMO) study. Control Clin Trials. 2000;21:502–25. doi: 10.1016/s0197-2456(00)00062-3. [DOI] [PubMed] [Google Scholar]
- 8.Cohn JN, Tognoni G. A randomized trial of the angiotensin-receptor blocker valsartan in chronic heart failure. N Engl J Med. 2001;345:1667–75. doi: 10.1056/NEJMoa010713. [DOI] [PubMed] [Google Scholar]
- 9.Pfeffer MA, Swedberg K, Granger CB, et al. Effects of candesartan on mortality and morbidity in patients with chronic heart failure: the CHARM-Overall programme. Lancet. 2003;362:759–66. doi: 10.1016/s0140-6736(03)14282-1. [DOI] [PubMed] [Google Scholar]
- 10.Austin PC, Mamdani MM. A comparison of propensity score methods: a case-study estimating the effectiveness of post-AMI statin use. Stat Med. 2006;25:2084–106. doi: 10.1002/sim.2328. [DOI] [PubMed] [Google Scholar]
- 11.Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083–107. doi: 10.1002/sim.3697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55. [Google Scholar]
- 13.Kosanke J, Bergstralh E. GMATCH macro: Match 1 or more controls to cases using the greedy algorithm. Mayo Clinic College of Medicine; 2004. [Last accessed October 1, 2010]. Available at: http://mayoresearch.mayo.edu/mayo/research/biostat/sasmacros.cfm. [Google Scholar]
- 14.Isakova T, Gutierrez OM, Chang Y, et al. Phosphorus binders and survival on hemodialysis. J Am Soc Nephrol. 2009;20:388–96. doi: 10.1681/ASN.2008060609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Griffith TF, Chua BS, Allen AS, et al. Characteristics of treated hypertension in incident hemodialysis and peritoneal dialysis patients. Am J Kidney Dis. 2003;42:1260–9. doi: 10.1053/j.ajkd.2003.08.028. [DOI] [PubMed] [Google Scholar]
- 16.Kestenbaum B, Gillen DL, Sherrard DJ, et al. Calcium channel blocker use and mortality among patients with end-stage renal disease. Kidney Int. 2002;61:2157–64. doi: 10.1046/j.1523-1755.2002.00355.x. [DOI] [PubMed] [Google Scholar]
- 17.Foley RN, Herzog CA, Collins AJ. Blood pressure and long-term mortality in United States hemodialysis patients: USRDS Waves 3 and 4 Study. Kidney Int. 2002;62:1784–90. doi: 10.1046/j.1523-1755.2002.00636.x. [DOI] [PubMed] [Google Scholar]
- 18.Ishani A, Herzog CA, Collins AJ, et al. Cardiac medications and their association with cardiovascular events in incident dialysis patients: cause or effect? Kidney Int. 2004;65:1017–25. doi: 10.1111/j.1523-1755.2004.00473.x. [DOI] [PubMed] [Google Scholar]
- 19.Abbott KC, Trespalacios FC, Agodoa LY, et al. Beta-blocker use in long-term dialysis patients: association with hospitalized heart failure and mortality. Arch Intern Med. 2004;164:2465–71. doi: 10.1001/archinte.164.22.2465. [DOI] [PubMed] [Google Scholar]
- 20.Trespalacios FC, Taylor AJ, Agodoa LY, et al. Incident acute coronary syndromes in chronic dialysis patients in the United States. Kidney International. 2002;62:1799–805. doi: 10.1046/j.1523-1755.2002.00638.x. [DOI] [PubMed] [Google Scholar]
- 21.Winkelmayer WC, Charytan DM, Levin R, et al. Poor short-term survival and low use of cardiovascular medications in elderly dialysis patients after acute myocardial infarction. Am J Kidney Dis. 2006;47:301–8. doi: 10.1053/j.ajkd.2005.10.009. [DOI] [PubMed] [Google Scholar]
- 22.Berger AK, Duval S, Krumholz HM. Aspirin, beta-blocker, and angiotensin-converting enzyme inhibitor therapy in patients with end-stage renal disease and an acute myocardial infarction. J Am Coll Cardiol. 2003;42:201–8. doi: 10.1016/s0735-1097(03)00572-2. [DOI] [PubMed] [Google Scholar]
- 23.Zannad F, Kessler M, Lehert P, et al. Prevention of cardiovascular events in end-stage renal disease: results of a randomized trial of fosinopril and implications for future studies. Kidney Int. 2006;70:1318–24. doi: 10.1038/sj.ki.5001657. [DOI] [PubMed] [Google Scholar]
- 24.Trespalacios FC, Taylor AJ, Agodoa LY, et al. Heart failure as a cause for hospitalization in chronic dialysis patients. Am J Kidney Dis. 2003;41:1267–77. doi: 10.1016/s0272-6386(03)00359-7. [DOI] [PubMed] [Google Scholar]
- 25.Cannella G, Paoletti E, Delfino R, et al. Prolonged therapy with ACE inhibitors induces a regression of left ventricular hypertrophy of dialyzed uremic patients independently from hypotensive effects. Am J Kidney Dis. 1997;30:659–64. doi: 10.1016/s0272-6386(97)90490-x. [DOI] [PubMed] [Google Scholar]
- 26.Tycho Vuurmans JL, Boer WH, Bos WJ, et al. Contribution of volume overload and angiotensin II to the increased pulse wave velocity of hemodialysis patients. J Am Soc Nephrol. 2002;13:177–83. doi: 10.1681/ASN.V131177. [DOI] [PubMed] [Google Scholar]
- 27.Inrig JK. Intradialytic hypertension: a less-recognized cardiovascular complication of hemodialysis. Am J Kidney Dis. 2010;55:580–9. doi: 10.1053/j.ajkd.2009.08.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Lopes AA, Bragg-Gresham JL, Ramirez SPB, et al. Prescription of antihypertensive agents to haemodialysis patients: time trends and associations with patient characteristics, country and survival in the DOPPS. Nephrol Dial Transplant. 2009;24:2809–16. doi: 10.1093/ndt/gfp212. [DOI] [PubMed] [Google Scholar]
- 29.Cice G, Di Benedetto A, D’Isa S, et al. Effects of telmisartan added to angiotensin-converting enzyme inhibitors on mortality and morbidity in hemodialysis patients with chronic heart failure: a double-blind, placebo-controlled trial. J Am Coll Cardiol. 2010;56:1701–8. doi: 10.1016/j.jacc.2010.03.105. [DOI] [PubMed] [Google Scholar]
- 30.Ray WA. Evaluating medication effects outside of clinical trials: new-user designs. Am J Epidemiol. 2003;158:915–20. doi: 10.1093/aje/kwg231. [DOI] [PubMed] [Google Scholar]