Abstract
Importance
Single measures of blood pressure (BP) levels are associated with the development of atherosclerosis; however, long-term patterns in BP and their impact on CVD risk are poorly characterized.
Objective
To identify common BP trajectories throughout early adulthood and to determine their association with presence of coronary artery calcification (CAC) during middle age.
Design
We used data from the CARDIA study from baseline in 1985-1986 through 25 years of follow-up (2010-2011).
Setting
Prospective cohort study
Participants
CARDIA participants were Black and White men and women aged 18-30 years at baseline.
Exposures
We examined systolic BP, diastolic BP, and mid-BP [calculated as (SBP+DBP)/2 and an important marker of CHD risk among younger populations] at baseline and years 2, 5, 7, 10, 15, 20, and 25. Latent mixture modeling was used to identify trajectories in SBP, DBP and mid-BP over time.
Main Outcome Measure
Coronary artery calcification greater than or equal to Agatston score of 100 Agatston units at year 25.
Results
Among 4,681 participants, we identified 5 distinct mid-BP trajectories: Low-Stable (22% [95% CI 19.9-23.7], n=987), Moderate-Stable (42% [40.3-44.3], n=2,085), Moderate-Increasing (12% [10.4-14.0], n=489), Elevated-Stable (19% [17.1-20.0], n=903) and Elevated-Increasing (5% [4.0-5.5], n=217). As compared to the Low-Stable group, trajectories with elevated BP levels had greater odds of having CAC >100. Adjusted odds ratios (95% CI) were 1.44 (0.83-2.49) for Moderate-Stable, 1.86 (0.91-3.82) for Moderate-Increasing, 2.28 (1.24-3.70) for Elevated-Stable, and 3.70 (1.66-8.20) for Elevated-Increasing groups. The adjusted prevalence of CAC ≥ 100 was 5.8% in the Low-Stable group. These ORs represent an absolute increase of 2.7%, 5%, 6.3% and 12.9% for the prevalence of CAC ≥100 for the Moderate-Stable, Moderate-Increasing, Elevated Stable and Elevated Increasing groups respectively as compared to the Low-Stable Group. Associations were not altered after adjustment for baseline and year 25 BP. Findings were similar for trajectories of isolated systolic BP trajectories, but were attenuated for diastolic BP trajectories.
Conclusions and Relevance
BP trajectories throughout young adulthood vary and higher BP trajectories were associated with an increased risk of CAC in middle age. Long-term trajectories in BP may assist in more accurate identification of individuals with subclinical atherosclerosis.
Keywords: blood pressure, calcium, epidemiology, risk factors
Blood pressure (BP) represents a major modifiable risk factor for cardiovascular disease (CVD). Current risk prediction models only take into account BP level at the time of risk prediction, usually in middle or older age, and do not consider the potential impact of BP levels experienced earlier in life or the changes in BP levels over time. Time-averaged and cumulative BP among adults have also been shown to predict CVD risk among several large prospective investigations .1,2,3,4 For nearly everyone, at least in populations which consume large amounts of salt5, systolic BP increases with age and these increases during middle age have been associated with CVD risk.6,7 It was recently demonstrated that changes in BP throughout middle and older age are significantly associated with the lifetime risk for CVD, and the larger the changes the greater the lifetime risk.8 However, the patterns of BP change may differ among individuals; thus, a life-course perspective when evaluating the effects of BP is essential. Long-term BP trajectory patterns from young adulthood to middle age and their impact on CVD risk remain unknown. Therefore, the aims of this study are (1) to identify subgroups of individuals with similar trajectories in BP from young adulthood through middle age, (2) to characterize those participants and BP trajectories, and (3) to determine the independent association of BP trajectories from young adulthood to middle age with the presence of subclinical CVD as measured by coronary artery calcification (CAC) during middle age. We hypothesized that there exist multiple trajectory patterns within the CARDIA population and that in comparison to a trajectory in which individuals maintain ideal BP levels throughout young adulthood, a portion of the population will experience higher levels of BP and/or faster rates of increase in BP which will be associated with increased subclinical atherosclerosis in year 25.
Methods
The Coronary Artery Risk Development in Young Adults (CARDIA) study is a prospective cohort study designed to investigate the development of cardiovascular risk and disease. In 1985-1986, 5,115 Black and White men and women aged 18-30 years of age were recruited from four urban sites across the United States including Birmingham, AL; Chicago, IL; Minneapolis, MN; and Oakland, CA). CARDIA participants have been followed for over 25 years with detailed demographic and clinical data, including self-reported anthropometric and laboratory measures, and assessment for subclinical atherosclerosis. Race was determined by self-report at year 0 and verified at year 2. Participant data have been collected across 8 examination cycles including baseline and at years 2, 5, 7, 10, 15, 20, and 25. Retention rates have been high throughout the 25 years of follow-up (90%, 86%, 81%, 77%, 74%, 72% and 72%, respectively). A more thorough description of the study design and conduct has been previously published.9-11 The study was approved by the institutional review board at all study sites and all participants signed an informed consent. The current analyses include CARDIA participants with BP measures available at 3 or more examinations.
Blood pressure was measured at each of the 8 CARDIA exam cycles. At each exam, trained technicians used either a random zero sphygmomanometer (Y0-Y20) or OmROn sphygmomanometer (Y20-Y25) to measure participants' blood pressure. Resting systolic and diastolic blood pressure was measured three times at 1-minute intervals. We used the average of the second and third blood pressure measurements. In our main analysis we examined trajectories in systolic blood pressure and mid-BP, defined as the mean of the systolic and diastolic BP measurements. In addition to SBP, Mid-BP was chosen a priori because it has been shown to have the greatest predictive utility for CVD compared with other single measures of BP (systolic blood pressure [SBP] or diastolic blood pressure [DBP], pulse pressure or mean arterial pressure).12,13 In addition, mid-BP allowed us to take into account the effects of both systolic and diastolic blood pressure jointly. This is of particular importance among this younger CARDIA population, as diastolic blood pressure has been shown to play a larger role in CHD risk among the young to middle age adults.14-17 Separate trajectories in systolic and diastolic blood pressures were also examined.
Subclinical coronary atherosclerosis was quantified using coronary artery calcification (CAC) measured at the year 25 examination. Calcified coronary artery plaque measurement was done with an electrocardiographically gated multidector computed tomography (CT) scanner with a standard phantom for calibration using a standardized protocol18 with published accuracy, comparability and reproducibility.19,20 Briefly, scans were obtained and image analysts blinded to participant characteristics calculated a total coronary artery calcium score using a modified Agatston method,21 with select overreading by a physician expert in cardiovascular imaging. Our outcome in this study was the presence of CAC greater than or equal to Agatston score of 100 Agatston units. CAC ≥ 100 has been identified as a marker of risk for high risk of coronary events22 and has been used often in previous consensus statements.23,24 In addition, we examined CAC >0 in sensitivity analyses.
Statistical Analyses
Blood pressure trajectories were modeled among all 4,681 CARDIA participants with BP measured at 3 or more exams. Only 3,442 participants with CAC data available at year 25 were included in the models examining the association between blood pressure and CAC >100. We used latent class models to identify subgroups within the CARDIA cohort that share a similar underlying trajectory in BP. These models were fit using SAS Proc Traj.25-27 See statistical appendix for more details on the trajectory modeling process. In order to estimate the association of trajectory group on subclinical atherosclerosis, trajectory group membership was included as an independent variable in a logistic regression model examining predictors of the presence of CAC Agatston score ≥ 100 at Exam Year 25. The adjusted model included baseline age, race, sex, highest level of education, antihypertensive medication use at each exam, mg/dL of total cholesterol per year, cumulative number of years with diabetes, cumulative number of years as a current smoker, and BMI at both baseline and Y25. As in other studies, in order to account for the uncertainty in BP trajectory group assignment the posterior probability of group membership we generated 20 multiple imputations of trajectory membership using the posterior probabilities.28 We then fit the logistic regression model for each of the 20 data sets and combined our results across the multiple imputations. Model calibration was examined using the Hosmer-Lemeshow goodness-of fit chi-square statistic. We compared the predictive utility of trajectory group as compared to other longitudinal BP measures (single baseline BP measurements, multiple BP measurements [baseline and Y25] and cumulative BP [mm Hg × years]) using the logistic C-statistic and the discrimination (D statistic)29of the models for each of these BP measures individually and jointly. The D-statistic represents the difference in the average of event probabilities between the groups which experience the event and those who do not. The Wilcoxon test was used to detect significant location shifts and differences in the distributions of the predicted event probabilities. In order to quantify how the model reclassifies individuals with the addition of trajectory group, we calculated the Integrated Discrimination Improvement (IDI) index by calculating the difference in the D-statistics (discrimination slopes) between the models including only baseline BP or year 25 BP and those including trajectory group. All analyses were completed in SAS version 9.3. P-values < 0.05 were considered statistically significant.
Results
The CARDIA cohort enrolled 5,115 individuals. Trajectories in mid-blood pressure were examined among 4,681 CARDIA participants with three or more BP measurements. Of these, 3,442 participants had CAC available at year 25. Five discrete trajectories in mid-BP from young adulthood to middle age were identified (Figure 1): 21.8%, 95% CI: 19.9%-23.7% (n=987) of participants maintained low BP throughout follow-up (we refer to these participants as the, “Low-Stable group.”), 42.3%, 95% CI: 40.3%-44.3% (n=2,085) of participants experienced moderate BP levels (Moderate-Stable group), 12.2%, 95% CI: 10.4%-14.0% (n=489) started at moderate levels and experienced a rapid increase in BP starting at an average age of 35 years (Moderate-Increasing group), 19.0%, 95% CI: 17.1%-20.0% (n=903) had relatively elevated BP levels throughout (Elevated-Stable group), and 4.8%, 95% CI: 4.0%-5.5% (n=217) had high BP levels (Elevated-Increasing group).
Figure 1. Trajectories in Mid-Blood Pressure in the Coronary Artery Risk Development in Young Adults (CARDIA) Study.
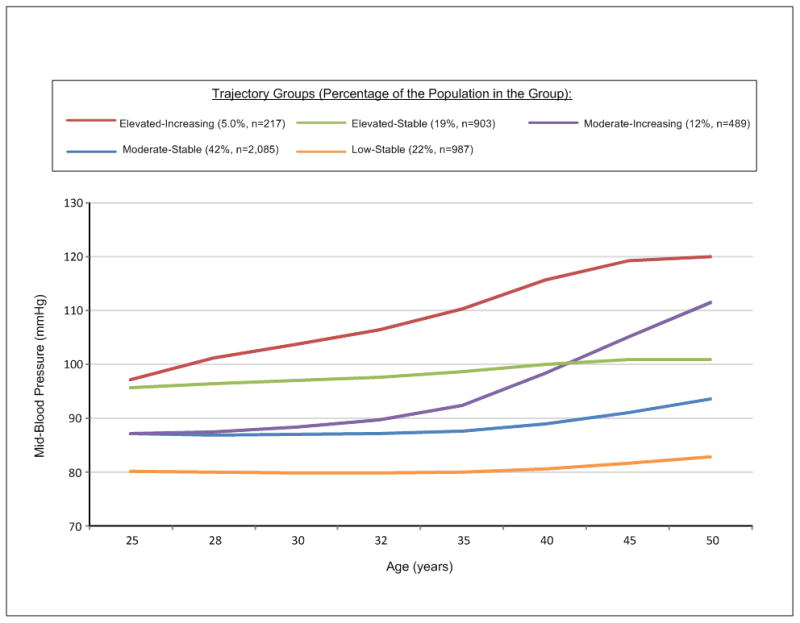
Trajectory classes identified for mid-blood pressure; their pattern by age and the percentage (number) of CARDIA participants in each class.
In general trajectory groups tracked with BP at age 25 and experienced small, steady increases in systolic and diastolic BP, as well as the proportion of participants on antihypertensive medications, however; two groups (the Moderated-Increasing and Elevated-Increasing groups) experienced large and more rapid increases in blood pressure over time (Table 1). The Moderated-Increasing and Elevated-Increasing groups experienced the largest increases in systolic BP (mean increases were 30.2 mm Hg and 21.2 mm Hg, respectively) and diastolic BP (20.9 mm Hg and 11.5 mm Hg, respectively).
Table 1. Average Systolic and Diastolic Blood Pressure and Percentage on Medication at Each Study Exam by Mid-BP Trajectory Group: The Coronary Artery Risk Development in Young Adults Study.
| Low-Stable Group | Moderate-Stable Group | Moderate-Increasing Group | Elevated-Stable Group | Elevated-Increasing Group | |
|---|---|---|---|---|---|
| N=987 | N=2,085 | N=489 | N=903 | N=217 | |
| Average SBP, mm Hg (SD) | |||||
|
| |||||
| Year 0 | 100.5 (7.3) | 109.0 (7.9) | 111.3 (8.5) | 120.4 (8.8) | 125.0 (12.0) |
| Year 2 | 98.0 (7.0) | 106.4 (7.8) | 109.2 (8.1) | 117.5 (8.5) | 123.6 (12.3) |
| Year 5 | 96.9 (6.6) | 105.9 (7.5) | 109.7 (8.3) | 117.8 (8.6) | 129.7 (14.7) |
| Year 7 | 97.3 (7.1) | 106.4 (7.3) | 111.9 (9.3) | 118.9 (8.8) | 134.5 (16.7) |
| Year 10 | 97.8 (6.5) | 107.7 (7.5) | 115.3 (10.4) | 120.4 (9.3) | 135.3 (18.5) |
| Year 15 | 99.1 (6.9) | 109.9 (8.2) | 124.2 (13.4) | 122.7 (11.7) | 144.4 (18.5) |
| Year 20 | 101.8 (7.4) | 113.3 (8.9) | 132.4 (15.0) | 122.4 (10.5) | 142.1 (16.2) |
| Year 25 | 104.2 (8.5) | 118.0 (10.4) | 141.5 (14.4) | 122.6 (10.4) | 146.2 (18.8) |
| Average DBP, mm Hg, (SD) | |||||
|
| |||||
| Year 0 | 61.7 (7.7) | 67.6 (7.6) | 68.5 (8.9) | 75.8 (8.3) | 80.3 (11.2) |
| Year 2 | 60.1 (7.3) | 66.4 (7.4) | 67.4 (8.2) | 75.0 (8.6) | 80.1 (11.1) |
| Year 5 | 60.5 (6.9) | 67.9 (7.2) | 70.2 (8.3) | 77.5 (7.8) | 86.3 (12.2) |
| Year 7 | 60.5 (6.9) | 67.6 (6.8) | 71.2 (9.0) | 77.4 (8.5) | 88.0 (12.2) |
| Year 10 | 63.0 (6.4) | 70.7 (6.9) | 76.6 (8.7) | 80.5 (7.9) | 90.4 (11.6) |
| Year 15 | 64.1 (7.0) | 72.3 (7.4) | 81.7 (10.7) | 81.7 (9.3) | 96.1 (13.8) |
| Year 20 | 61.4 (6.5) | 70.6 (7.3) | 84.8 (9.3) | 77.3 (8.4) | 91.3 (11.0) |
| Year 25 | 63.8 (6.9) | 74.1 (7.7) | 89.4 (8.6) | 77.3 (7.9) | 91.8 (12.2) |
| Participants on Medication No. (%) | |||||
|
| |||||
| Year 0 | 1 (0.1) | 6 (0.3) | 3 (0.6) | 13 (1.4) | 13 (6.0) |
| Year 2 | 1 (0.1) | 3 (0.1) | 2 (0.4) | 18 (2.0) | 14 (6.5) |
| Year 5 | 0 (0.0) | 2 (0.1) | 5 (1.0) | 32 (3.5) | 31 (14.3) |
| Year 7 | 1 (0.1) | 2 (0.1) | 6 (1.2) | 39 (4.3) | 33 (15.2) |
| Year 10 | 0 (0.0) | 11 (0.5) | 12 (2.5) | 64 (7.1) | 48 (22.1) |
| Year 15 | 4 (0.4) | 48 (2.3) | 35 (7.2) | 142 (15.7) | 63 (29.0) |
| Year 20 | 14 (1.4) | 164 (7.9) | 110 (22.5) | 238 (26.4) | 91 (41.9) |
| Year 25 | 31 (3.1) | 286 (13.7) | 185 (37.8) | 323 (35.8) | 110 (50.7) |
Individuals in the Low-Stable group were the most likely to be female, white, more highly educated and more likely to have fewer concurrent cardiovascular risk factors (Table 2). African Americans were more likely to experience rapid increases in BP, with the Moderate-Increasing group having the largest proportion of African American women and the Elevated-Increasing group having the largest proportion of African American men. In addition, these rapid increases in BP were associated with higher rates of smoking and occurred alongside increases in BMI (avg BMI increased by 7.4-7.6 among Increasing and High groups but only by 4.5-5.7 among the other groups with more stable BP levels).
Table 2. Demographic Characteristics and Risk Factors of Participants by Mid-BP Trajectory Group: The Coronary Artery Risk Development in Young Adults Study.
| Low-Stable Group | Moderate-Stable Group | Moderate-Increasing Group | Elevated-Stable Group | Elevated-Increasing Group | ||
|---|---|---|---|---|---|---|
| N=987 | N=2,085 | N=489 | N=903 | N=217 | p-value | |
| Demographic Characteristics | ||||||
| Age at Baseline (SD) | 25.1(3.7) | 24.9 (3.6) | 24.9 (3.7) | 24.9 (3.6) | 25.1 (3.6) | 0.57 |
| Female, % | 78.8 | 55.1 | 60.1 | 29.7 | 38.2 | <0.001 |
| Race, % | <0.001 | |||||
| Black | 29.4 | 49.3 | 69.9 | 56.8 | 79.3 | |
| White | 70.6 | 50.7 | 30.1 | 43.2 | 20.7 | |
| Education, % | ||||||
| High School or Less | 34.5 | 42.6 | 44.2 | 47.6 | 61.3 | <0.001 |
| Some College | 15.7 | 19.9 | 26.4 | 24.0 | 21.2 | <0.001 |
| College Graduate | 24.4 | 19.9 | 17.6 | 16.1 | 9.2 | <0.001 |
| Graduate School | 25.4 | 17.6 | 11.9 | 12.3 | 8.3 | <0.001 |
| Cardiovascular Risk Factors, % | ||||||
| Current Smoker at Y0 | 29.0 | 29.4 | 31.8 | 27.7 | 37.5 | 0.055 |
| Current Smoker at Y25 | 12.8 | 16.6 | 22.9 | 16.8 | 28.2 | <0.001 |
| Total Cholesterol at Y0 (SD) | 173.3 (32.0) | 176.0 (32.1) | 178.4 (33.9) | 181.7 (35.5) | 183.7 (36.3) | <0.001 |
| Total Cholesterol at Y25 (SD)* | 194.2 (34.4) | 192.8 (36.4) | 194.8 (38.0) | 186.4 (38.7) | 196.4 (42.4) | 0.0112 |
| Diabetes at Y0 | 0.3 | 0.5 | 0.8 | 1.0 | 1.8 | 0.048 |
| Diabetes at Y25 | 5.2 | 12.1 | 17.7 | 23.4 | 35.9 | <0.001 |
| Avg. BMI at Y0 (SD) | 22.4 (3.5) | 24.2 (4.6) | 25.6 (5.3) | 26.2 (5.9) | 27.6 (6.6) | <0.001 |
| Avg. BMI at Y25 (SD) | 26.9 (5.7) | 29.9 (6.6) | 33.2 (7.6) | 31.8 (7.8) | 35.0 (8.9) | <0.001 |
| Mean Coronary Artery Calcification Score, (SD) | 16.9 (91.0) | 32.4 (159.4) | 44.4 (172.1) | 87.2 (288.9) | 190.5 (638.8) | <0.0001 |
The prevalence of CAC ≥100 varied from 4.0% in the Low-Stable BP trajectory group up to 25.4% in the Elevated-Increasing BP trajectory group. Within each trajectory group, individuals on antihypertensive medications had a higher prevalence of CAC as compared to individuals within the same trajectory group but not on antihypertensive medications. Even among groups that started at similar baseline BP levels, for example the Moderate-Stable and Moderate-Increasing groups, participants who experienced steeper increases in BP had a higher prevalence of CAC >100, 7.9% vs 10.1%, respectively (p for trend was <0.0001). In comparison to individuals in the Low-Stable group, those in trajectory groups with patterns of higher mid-BP had increasingly greater odds of having CAC ≥ 100. Adjustment for individual demographic characteristics and education only slightly attenuated the odds ratios. Additional adjustment for other cardiovascular risk factors and blood pressure medication resulted in larger attenuations of the odds ratios for the higher risk groups especially the Elevated-Stable and Elevated-Increasing groups. Elevated BP trajectory groups were independently associated with CAC≥100 at year 25 (Table 3) even after adjustment for demographic characteristics, other CV risk factors, and anti-hypertensive medication in model 1. Adjusted odds ratios (95% CI) were 1.44 (0.83-2.49) for Moderate-Stable, 1.86 (0.91-3.82) for Moderate-Increasing, 2.28 (1.24-4.18) for Elevated-Stable, and 3.70 (1.66-8.20) for Elevated-Increasing groups. The adjusted prevalence of CAC ≥ 100 was 5.8% in the Low-Stable group. These ORs represent an absolute increase of 2.7%, 5%, 6.3% and 12.9% for the prevalence of CAC ≥100 for the Moderate-Stable, Moderate-Increasing, Elevated Stable and Elevated Increasing groups respectively as compared to the Low-Stable Group. Findings were similar for the outcome of CAC > 0 (eTable 1). In sensitivity analyses, the BP trajectory patterns were similar and their association with CAC ≥100 was essentially unchanged when restricted to individuals who were not on BP medication at any time during follow-up (n=3507).
Table 3. Adjusted Odds Ratios and 95% Confidence Intervals of the Association of Blood Pressure Trajectory Groups with Coronary Artery Atherosclerosis ≥ 100.
| No. of Participants with CAC ≥ 100 at Year 25 (%) | Unadjusted | Model 1 | Model 2 | Model 3 | |
|---|---|---|---|---|---|
| Mid-BP Trajectory Group | |||||
| Low-Stable | 28 (4.0%) | 1.00 | 1.00 | 1.00 | 1.00 |
| Moderate-Stable | 109 (7.9%) | 1.94 (1.18-3.20) | 1.44 (0.83-2.49) | 1.56 (0.88-2.78) | 1.53 (0.84-2.79) |
| Moderate-Increasing | 38 (10.1%) | 2.57 (1.44-4.59) | 1.86 (0.91-3.82) | 2.11 (0.98-4.53) | 2.07 (0.76-5.62) |
| Elevated-Stable | 102 (17.4%) | 4.79 (2.92-7.85) | 2.28 (1.24-4.18) | 2.77 (1.34-5.74) | 2.48 (1.24-4.98) |
| Elevated-Increasing | 32 (25.4%) | 8.02 (4.50-14.29) | 3.70 (1.66-8.20) | 4.87 (1.34-12.63) | 4.12 (1.45-11.71) |
| SBP Trajectory Group | |||||
| Low-Stable | 33 (4.2%) | 1.00 | 1.00 | 1.00 | 1.00 |
| Moderate-Stable | 117 (8.2%) | 2.22 (1.44-3.41) | 1.56 (96-2.53) | 1.67 (1.00-2.77) | 1.54 (0.92-2.58) |
| Moderate-Increasing | 25 (9.1%) | 2.36(1.33-4.18) | 1.71 (0.82-3.54) | 1.90 (0.88-4.10) | 1.53 (0.56-4.22) |
| Elevated-Stable | 107 (18.5%) | 4.78 (3.07-7.45) | 2.16 (1.23-3.83) | 2.50 (1.25-4.98) | 2.11 (1.12-3.99) |
| Elevated-Increasing | 27 (30.3%) | 10.91 (5.89-20.21) | 5.24 (2.21-12.44) | 6.44 (2.37-17.53) | 4.78 (1.67-13.68) |
| DBP Trajectory Group | |||||
| Low-Stable | 33 (4.7%) | 1.00 | 1.00 | 1.00 | 1.00 |
| Moderate-Stable | 118 (8.3%) | 1.87 (1.22-2.86) | 1.48 (0.89-2.47) | 1.55 (0.90-2.65) | 1.57 (0.91-2.71) |
| Moderate-Increasing | 38 (11.3%) | 2.47 (1.46-4.17) | 1.77 (0.88-3.57) | 1.87 (0.89-3.93) | 1.97 (0.77-5.03) |
| Elevated-Stable | 97 (16.2%) | 3.92 (2.54-6.04) | 1.93 (1.11-3.36) | 2.16 (1.12-4.16) | 2.09 (1.13-3.89) |
| Elevated-Increasing | 23 (21.1%) | 5.49 (3.00-10.07) | 1.98 (0.86-4.54) | 2.28 (0.87-6.00) | 2.20 (0.81-6.01) |
Model 1 = age, race, sex, highest level of education, antihypertensive medication use at each exam, mg/dL of total cholesterol per year, cumulative number of years with diabetes, cumulative number of years as a current smoker, and BMI at both baseline and Y25
Model 2 = Model 1 + baseline systolic and diastolic blood pressure
Model 3 = Model 1 + year 25 systolic and diastolic blood pressure
Odds ratios for CAC for different trajectory groups was not significantly altered even with additional adjustment for baseline systolic and diastolic blood pressure (model 2) or year 25 systolic and diastolic blood pressure (model 3). All models fit the data well with Hosmer-Lemeshow chi-square statistics with a p-value >0.05. The average predicted probability of having CAC ≥ 100 under the adjusted model including trajectory group for the group of CARDIA participants with CAC ≥ 100 was 25.3% as compared to those who did not have CAC ≥ 100, predicted probability of 8.1%. The discrimination of the model and its ability to correctly identify individuals with CAC ≥ 100 was similar as compared to models with either baseline or year 25 BP alone. The C-statistic for the unadjusted model was 0.66 which increased to 0.84 in models 1, 2 and 3. Similarly, the D-statistic for the adjusted model of trajectory groups was only slightly higher (0.172) as compared to models of baseline BP and Y25 BP (D-statistic 0.167 and 0.169, respectively; p-value <0.001); however, the IDI was only 0.5 and 0.3, respectively.
Overall patterns were similar when we examined the trajectories of systolic and diastolic blood pressure separately (Figure 2A and AB and eTables 2-6). Five discrete trajectory groups were identified for long-term patterns in systolic BP: 24.6%, 95% CI: 22.5%-26.8% (n=1113) of participants maintained low SBP throughout follow-up (we refer to these participants as the, “Low-Stable group.”), 44.1%, 95% CI: 42.1%-46.1% (n=2,167) of participants experienced moderate SBP levels (Moderate-Stable group), 9.8%, 95% CI: 7.9%-10.7% (n=363) started at moderate levels and experienced a rapid increase in SBP starting at an average age of 35 years (Moderate-Increasing group), 18.8%, 95% CI: 16.6%-21.0% (n=884) had relatively elevated SBP levels throughout (Elevated-Stable group), and 3.3%, 95% CI: 2.6%-4.0% (n=154) had high SBP levels (Elevated-Increasing group). SBP trajectory groups had increasing prevalence of CAC ≥ 100 with increasing SBP trajectory group ranging from e Figure 3. After adjustment for demographic, long-term CV risk factors and BP medication, these SBP trajectory groups were significantly associated with the prevalence of CAC >100; ORs were 1.56 (0.96-2.53) for the Moderate-Stable group, 1.71 (0.82-3.54) for the Moderate-Increasing group, 2.16 (1.23-3.83) for the Elevated-Stable Group, and 5.24 for the Elevated-Increasing group as compared to the Low-Stable group (Table 3). The adjusted prevalence of CAC ≥ 100 at year 25 was 6.4% among the Low-Stable group and increased by 2.5%, 3.3%, 5.9%, and 14.3% for the Moderate-Stable, Moderate-Increasing, Elevated-Stable and Elevated-Increasing groups.
Figure 2. Trajectories in Systolic and Diastolic Blood Pressure in the Coronary Artery Risk Development in Young Adults (CARDIA) Study.
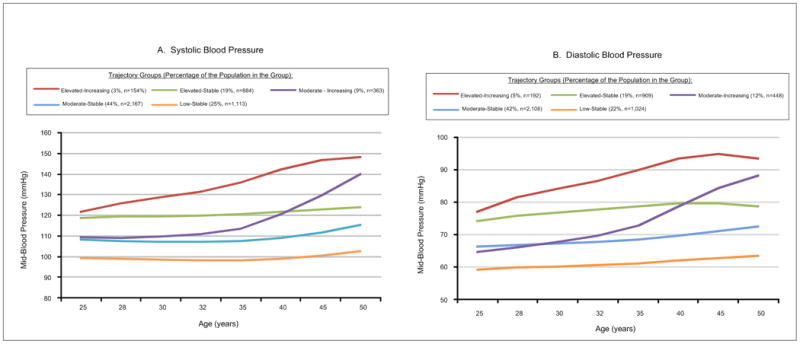
Trajectory classes identified for systolic [A] and diastolic [B] blood pressure; their pattern by age and the percentage (number) of CARDIA participants in each class.
Five discrete trajectory groups were identified for long-term patterns in diastolic BP: 22.5%, 95% CI: 20.5%-24.6% (n=1024) of participants maintained low DBP throughout follow-up (Low-Stable group), 42.6%, 95% CI: 40.4%-44.8% (n=2,108) of participants experienced moderate DBP levels (Moderate-Stable group), 11.4% 95% CI: 9.6%-13.2% (n=448) started at moderate levels and experienced a rapid increase in DBP starting at an average age of 35 years (Moderate-Increasing group), 19.2%, 95% CI: 17.2%-21.2% (n=909) had relatively elevated DBP levels throughout (Elevated-Stable group), and 4.4%, 95% CI: 3.6%-5.1% (n=192) had high DBP levels (Elevated-Increasing group). The adjusted associations (Table 3) for diastolic blood pressure trajectory groups were less strongly associated with CAC≥100. Systolic and diastolic trajectory groups were moderately to highly correlated with mid-BP trajectory groups (Pearson correlation coefficient of 0.83 for DBP and 0.63 for SBP); but only moderately correlated with each other with a correlation coefficient of 0.5.
Discussion
In this study we found that there were heterogeneous trajectories in mid-BP over 25 years from young adulthood to middle age. We identified five unique trajectories in mid-BP and systolic BP that were significantly associated with the presence of subclinical atherosclerosis later in middle age. CARDIA participants who exhibited elevated BP levels throughout and those that experienced increases in BP levels over time had the greatest odds of having CAC ≥ 100. Importantly, the majority of these participants had BP levels within the range of prehypertension. While not significant, even individuals in the Moderate-Stable group who on average maintained BP levels within recommended clinical ranges, but were not in the group exhibiting the lowest levels of BP (Low-Stable group), tended to have almost twice the odds of having CAC≥100. Membership in a trajectory group with elevated BP represented an independent predictor of CAC beyond either baseline blood pressure in young adulthood or year 25 blood pressure during middle age and may help to identify individuals with prevalent levels of CAC that have been shown to be associated with increased CVD risk.
Over 33% of US adults have hypertension30; however, much of our understanding of BP levels comes from cross-sectional data. Many longitudinal studies that have examined changes in BP over time often only had fewer than 5 years of follow-up and focused mainly on elderly individuals. BP levels in mid-life have been shown to predict stroke risk31 and cardiovascular mortality over 25 years later32, and may be more strongly associated with CHD mortality than BP levels measured at a time closer in proximity to the time of event .33Additionally, although BP lowering due to pharmacological treatment may be achieved quickly, measures of cardiovascular function (e.g. left ventricular hypertrophy, increased LV mass, and degree of carotid stenosis) tend tends to remain abnormal after exposure to long-term periods of elevated BP.34-37
The findings from this current study provide a unique insight into long-term patterns of BP change and highlight the fact that within the CARDIA population there are heterogeneous patterns in BP trajectories. Latent class modeling, as used in these current analyses, has allowed identification of different patterns of BP change as separate trajectory groups, thus providing a more realistic understanding of lifetime trends in BP compared with population mean levels. Among CARDIA participants, Pletcher and colleagues previously demonstrated that cumulative years of prehypertension prior to age 35 was associated with prevalent coronary calcium in middle-age.4 This current study extends those findings to demonstrate that not only is cumulative prehypertension important, but that certain populations such as African Americans and smokers are more likely to experience rapid increases in blood pressure during middle age placing them at higher risk. Consistent with our long-term findings, recent data from the UK have also demonstrated important heterogeneity in short-term BP trajectories in mid-life.38 Our findings further suggest that these trajectory groups provide important additional information regarding the presence of significant levels of subclinical atherosclerosis, which has been shown to be a strong indicator of future cardiovascular risk.22 This understanding of the effect of change or timing of change in BP on subclinical atherosclerosis may be important for risk stratification in the future.
The strengths and limitations of this investigation are worth note. This study applied innovative statistical methods to examine patterns BP in a large, well-characterized cohort of Black and White Americans. The longitudinal nature of CARDIA and phenotyping at each of the 8 exams provides detailed long-term patterns of blood pressure. Although CARDIA is a racially and geographically diverse cohort, the trajectory groups identified may not be generalizable to other populations. Not all CARDIA participants had blood pressure information available at all exam periods. However, missing BP is unlikely to have altered our findings as the mean number of BP measurements was 7 and did not differ by trajectory group. In sensitivity analyses, BP was imputed at each exam for all surviving CARDIA participants. Using these imputed BPs trajectory group assignment was consistent and did not result in any changes in the association between trajectory group and CAC. In addition, CARDIA participants were aged 18 to 30 years at baseline, thus we have no information on BP patterns prior to their entry into CARDIA. Coronary artery calcification at year 25 was missing for 28% of CARDIA participants. Participants who did not attend more recent exams were more likely to be African American, lower SES and have a greater burden of CV risk factors; nevertheless, these subgroups are well-represented in CARDIA attendees and by adjusting for these risk factors CAC is assumed to be missing at random and thus are results are unlikely to be biased.
Although BP has been a well-known risk factor for CVD for decades, these findings suggest that an individual's long-term patterns of change in BP starting in early adulthood may provide additional information about their risk for the development of coronary calcium. In particular, prehypertension at a young age followed by chronic exposure to blood pressure levels in the prehypertension range or higher was strongly associated with CAC > 100. Additional research is needed to examine the utility of specific BP trajectories in risk prediction for clinical CVD events and to explore the impact of lifestyle modification, treatment, and timing of intervention on lifetime trajectories in BP and outcomes.
Supplementary Material
Acknowledgments
The Coronary Artery Risk Development in Young Adults Study (CARDIA) is conducted and supported by the National Heart, Lung, and Blood Institute (NHLBI) in collaboration with the University of Alabama at Birmingham (HHSN268201300025C & HHSN268201300026C), Northwestern University (HHSN268201300027C), University of Minnesota (HHSN268201300028C), Kaiser Foundation Research Institute (HHSN268201300029C), and Johns Hopkins University School of Medicine (HHSN268200900041C). CARDIA is also partially supported by the Intramural Research Program of the National Institute on Aging (NIA) and an intra-agency agreement between NIA and NHLBI (AG0005).
This manuscript has been reviewed by CARDIA for scientific content. The funding agencies had no other role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication. Norrina Allen, PhD conducted the data analysis. She had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Conflicts of Interest: There were no conflicts of interest reported.
References
- 1.Vasan RS, Massaro JM, Wilson PW, et al. Antecedent blood pressure and risk of cardiovascular disease: the Framingham Heart Study. Circ. 2002;105(1):48–53. doi: 10.1161/hc0102.101774. [DOI] [PubMed] [Google Scholar]
- 2.Lee DS, Massaro JM, Wang TJ, et al. Antecedent blood pressure, body mass index, and the risk of incident heart failure in later life. Hypertension. 2007;50(5):869–876. doi: 10.1161/HYPERTENSIONAHA.107.095380. [DOI] [PubMed] [Google Scholar]
- 3.Stewart R, Xue QL, Masaki K, et al. Change in blood pressure and incident dementia: a 32-year prospective study. Hypertension. 2009;54(2):233–240. doi: 10.1161/HYPERTENSIONAHA.109.128744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pletcher MJ, Bibbins-Domingo K, Lewis CE, et al. Prehypertension during young adulthood and coronary calcium later in life. Annals of internal medicine. 2008;149(2):91–99. doi: 10.7326/0003-4819-149-2-200807150-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stamler J, Elliott P, Dennis B, et al. INTERMAP: background, aims, design, methods, and descriptive statistics (nondietary) Journal of human hypertension. 2003;17(9):591–608. doi: 10.1038/sj.jhh.1001603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Franklin SS, Gustin Wt, Wong ND, et al. Hemodynamic patterns of age-related changes in blood pressure. The Framingham Heart Study. Circulation. 1997;96(1):308–315. doi: 10.1161/01.cir.96.1.308. [DOI] [PubMed] [Google Scholar]
- 7.Neaton JD, Blackburn H, Jacobs D, et al. Serum cholesterol level and mortality findings for men screened in the Multiple Risk Factor Intervention Trial. Multiple Risk Factor Intervention Trial Research Group. Archives of internal medicine. 1992;152(7):1490–1500. [PubMed] [Google Scholar]
- 8.Allen N, Berry JD, Ning H, Van Horn L, Dyer A, Lloyd-Jones DM. Impact of blood pressure and blood pressure change during middle age on the remaining lifetime risk for cardiovascular disease: the cardiovascular lifetime risk pooling project. Circulation. 2012;125(1):37–44. doi: 10.1161/CIRCULATIONAHA.110.002774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Friedman GD, Cutter GR, Donahue RP, et al. CARDIA: study design, recruitment, and some characteristics of the examined subjects. Journal of clinical epidemiology. 1988;41(11):1105–1116. doi: 10.1016/0895-4356(88)90080-7. [DOI] [PubMed] [Google Scholar]
- 10.Cutter GR, Burke GL, Dyer AR, et al. Cardiovascular risk factors in young adults. The CARDIA baseline monograph. Controlled clinical trials. 1991;12(1 Suppl):1S–77S. doi: 10.1016/0197-2456(91)90002-4. [DOI] [PubMed] [Google Scholar]
- 11.Hughes GH, Cutter G, Donahue R, et al. Recruitment in the Coronary Artery Disease Risk Development in Young Adults (Cardia) Study. Controlled clinical trials. 1987;8(4 Suppl):68S–73S. doi: 10.1016/0197-2456(87)90008-0. [DOI] [PubMed] [Google Scholar]
- 12.Mosley WJ, 2nd, Greenland P, Garside DB, Lloyd-Jones DM. Predictive utility of pulse pressure and other blood pressure measures for cardiovascular outcomes. Hypertension. 2007;49(6):1256–1264. doi: 10.1161/HYPERTENSIONAHA.106.083592. [DOI] [PubMed] [Google Scholar]
- 13.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360(9349):1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 14.Franklin SS. The importance of diastolic blood pressure in predicting cardiovascular risk. JASH. 2007;1(1):82–93. doi: 10.1016/j.jash.2006.11.004. [DOI] [PubMed] [Google Scholar]
- 15.Lichtenstein MJ, Shipley MJ, Rose G. Systolic and diastolic blood pressures as predictors of coronary heart disease mortality in the Whitehall study. British medical journal. 1985;291(6490):243–245. doi: 10.1136/bmj.291.6490.243. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Tverdal A. Systolic and diastolic blood pressures as predictors of coronary heart disease in middle aged Norwegian men. British medical journal. 1987 Mar 14;294(6573):671–673. doi: 10.1136/bmj.294.6573.671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Franklin SS, Larson MG, Khan SA, et al. Does the relation of blood pressure to coronary heart disease risk change with aging? The Framingham Heart Study. Circ. 2001;103(9):1245–1249. doi: 10.1161/01.cir.103.9.1245. [DOI] [PubMed] [Google Scholar]
- 18.Carr JJ, Nelson JC, Wong ND, et al. Calcified coronary artery plaque measurement with cardiac CT in population-based studies: standardized protocol of Multi-Ethnic Study of Atherosclerosis (MESA) and Coronary Artery Risk Development in Young Adults (CARDIA) study. Radiology. 2005;234(1):35–43. doi: 10.1148/radiol.2341040439. [DOI] [PubMed] [Google Scholar]
- 19.Carr JJ, Crouse JR, 3rd, Goff DC, Jr, D'Agostino RB, Jr, Peterson NP, Burke GL. Evaluation of subsecond gated helical CT for quantification of coronary artery calcium and comparison with electron beam CT. AJR. American journal of roentgenology. 2000;174(4):915–921. doi: 10.2214/ajr.174.4.1740915. [DOI] [PubMed] [Google Scholar]
- 20.Detrano RC, Anderson M, Nelson J, et al. Coronary calcium measurements: effect of CT scanner type and calcium measure on rescan reproducibility--MESA study. Radiology. 2005;236(2):477–484. doi: 10.1148/radiol.2362040513. [DOI] [PubMed] [Google Scholar]
- 21.Agatston AS, Janowitz WR, Hildner FJ, Zusmer NR, Viamonte M, Jr, Detrano R. Quantification of coronary artery calcium using ultrafast computed tomography. Journal of the American College of Cardiology. 1990;15(4):827–832. doi: 10.1016/0735-1097(90)90282-t. [DOI] [PubMed] [Google Scholar]
- 22.Detrano R, Guerci AD, Carr JJ, et al. Coronary calcium as a predictor of coronary events in four racial or ethnic groups. The New England journal of medicine. 2008;358(13):1336–1345. doi: 10.1056/NEJMoa072100. [DOI] [PubMed] [Google Scholar]
- 23.Greenland P, Bonow RO, Brundage BH, et al. ACCF/AHA 2007 clinical expert consensus document on coronary artery calcium scoring by computed tomography in global cardiovascular risk assessment and in evaluation of patients with chest pain: a report of the American College of Cardiology Foundation Clinical Expert Consensus Task Force (ACCF/AHA Writing Committee to Update the 2000 Expert Consensus Document on Electron Beam Computed Tomography) developed in collaboration with the Society of Atherosclerosis Imaging and Prevention and the Society of Cardiovascular Computed Tomography. Journal of the American College of Cardiology. 2007;49(3):378–402. doi: 10.1016/j.jacc.2006.10.001. [DOI] [PubMed] [Google Scholar]
- 24.Budoff MJ, Achenbach S, Blumenthal RS, et al. Assessment of coronary artery disease by cardiac computed tomography: a scientific statement from the American Heart Association Committee on Cardiovascular Imaging and Intervention, Council on Cardiovascular Radiology and Intervention, and Committee on Cardiac Imaging, Council on Clinical Cardiology. Circulation. 2006;114(16):1761–1791. doi: 10.1161/CIRCULATIONAHA.106.178458. [DOI] [PubMed] [Google Scholar]
- 25.Jones BL, Nagin D, Roeder K. A SAS Procedure Based on Mixture Models for Estimating Developmental Trajectories. Sociological Methods & Research. 2001;29:374–393. [Google Scholar]
- 26.Nagin DS, Odgers CL. Group-based trajectory modeling in clinical research. Annual review of clinical psychology. 2010;6:109–138. doi: 10.1146/annurev.clinpsy.121208.131413. [DOI] [PubMed] [Google Scholar]
- 27.Nagin DS, Odgers CL. Group-Based Trajectory Modeling (Nearly) Two Decades Later. Journal of quantitative criminology. 2010;26(4):445–453. doi: 10.1007/s10940-010-9113-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Siddique J, Chung JY, Brown CH, Miranda J. Comparative effectiveness of medication versus cognitive-behavioral therapy in a randomized controlled trial of low-income young minority women with depression. Journal of consulting and clinical psychology. 2012;80(6):995–1006. doi: 10.1037/a0030452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tjur T. Coefficients of Determination in Logistic Regression Models - A New Proposal:The Coefficient of Discrimination. The American Statistician. 2009;63(4):366–372. [Google Scholar]
- 30.Go AS, Mozaffarian D, Roger VL, et al. Heart Disease and Stroke Statistics--2013 Update A Report From the American Heart Association. Circulation. 2012;127:e6–e245. doi: 10.1161/CIR.0b013e31828124ad. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Seshadri S, Wolf PA, Beiser A, et al. Elevated midlife blood pressure increases stroke risk in elderly persons: the Framingham Study. Archives of internal medicine. 2001;161(19):2343–2350. doi: 10.1001/archinte.161.19.2343. [DOI] [PubMed] [Google Scholar]
- 32.Miura K, Daviglus ML, Dyer AR, et al. Relationship of blood pressure to 25-year mortality due to coronary heart disease, cardiovascular diseases, and all causes in young adult men: the Chicago Heart Association Detection Project in Industry. Archives of internal medicine. 2001;161(12):1501–1508. doi: 10.1001/archinte.161.12.1501. [DOI] [PubMed] [Google Scholar]
- 33.Boshuizen HC, Lanti M, Menotti A, et al. Effects of past and recent blood pressure and cholesterol level on coronary heart disease and stroke mortality, accounting for measurement error. AJE. 2007;165(4):398–409. doi: 10.1093/aje/kwk021. [DOI] [PubMed] [Google Scholar]
- 34.Wolf PA, D'Agostino RB, Belanger AJ, Kannel WB. Probability of stroke: a risk profile from the Framingham Study. Stroke; a journal of cerebral circulation. 1991 Mar;22(3):312–318. doi: 10.1161/01.str.22.3.312. [DOI] [PubMed] [Google Scholar]
- 35.Kannel WB, Wolf P, Dawber TR. Hypertension and cardiac impairments increase stroke risk. Geriatrics. 1978;33(9):71–77. 81–73. [PubMed] [Google Scholar]
- 36.Bikkina M, Levy D, Evans JC, et al. Left ventricular mass and risk of stroke in an elderly cohort. The Framingham Heart Study. JAMA. 1994;272(1):33–36. [PubMed] [Google Scholar]
- 37.Wilson PW, Hoeg JM, D'Agostino RB, et al. Cumulative effects of high cholesterol levels, high blood pressure, and cigarette smoking on carotid stenosis. NEJM. 1997;337(8):516–522. doi: 10.1056/NEJM199708213370802. [DOI] [PubMed] [Google Scholar]
- 38.Wills AK, Lawlor DA, Muniz-Terrera G, et al. Population heterogeneity in trajectories of midlife blood pressure. Epidemiology. 2012;23(2):203–211. doi: 10.1097/EDE.0b013e3182456567. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


