Abstract
OBJECTIVES
To describe the longitudinal patterns and the within- and across-facility differences in hospice use and in-hospital deaths between long-term nursing home decedent residents with and without dementia.
DESIGN
Retrospective analyses of secondary datasets for CY2003–2007.
SETTING
Nursing homes in the USA.
PARTICIPANTS
A total of 1,261,726 decedents in 16,347 nursing homes were included in CY2003–2007 trend analysis and 236,619 decedents in 15,098 nursing homes in CY2007 were included in the within- and across-facility analyses.
MEASUREMENTS
Hospice use in the last 100 days of life, and in-hospital deaths were outcome measures. Dementia was defined as having a diagnosis of Alzheimer’s disease (AD) and/or dementia other than AD, based on the Minimum Data Set (MDS) health assessments.
RESULTS
Overall hospice use increased from 25.6% in 2003 to 35.7% in 2007. During this time, hospice use for decedents with dementia increased from 25.1% to 36.5%, compared to an increase from 26.5% to 34.4% for decedents without dementia. The rate of in-hospital deaths remained virtually unchanged. Within the same facility, decedents with dementia were significantly more likely to use hospice (OR=1.07, 95% CI: 1.04–1.11) and less likely to die in a hospital (OR=0.76, 95% CI: 0.74–0.78). Decedents in nursing homes with higher dementia prevalence, regardless of individual dementia status, were more likely to use hospice (OR=1.67, 95% CI: 1.22–2.27).
CONCLUSION
Nursing homes appear to provide less aggressive end of life care to decedents with dementia compared to others. Although significantly more decedent residents with dementia now receive hospice care at the end of life, the quality evaluation and monitoring of hospice programs have not been systematically conducted, and additional research in this area is warranted.
Keywords: hospice, hospitalization, place of death, in-hospital deaths, dementia
INTRODUCTION
Dementia prevalence in US nursing homes is widespread and increasing. In 2010, almost 60% of residents had a diagnosis of Alzheimer’s disease or other dementia.1 With the aging of the baby boomers this rate is expected to increase.2, 3 At the same time, nursing homes have become an increasingly important end-of-life (EOL) care setting in the United States, especially for people with dementia. While 28% of non-traumatic deaths among people aged 65 years and older occur in a nursing home, about 67% of those aged 65 years and older, with a diagnosis of dementia, die in a nursing home.4 As the proportion of deaths occurring in nursing homes increases, so do the concerns about EOL care quality in this setting.
Recently, Mukamel and colleagues proposed two EOL quality measures for nursing homes: hospice use and place of death (dying in a hospital or a nursing home).5 Studies have suggested that nursing home residents enrolled in hospice had a reduced likelihood of being hospitalized at the EOL, and were more likely to get better pain management and less likely to have physical restraints and feeding tubes.6–9 It has also been suggested that residents with dementia who received hospice services had experienced better EOL care quality as reported by their family members.10–13 Compared to hospice care, aggressive treatment at the EOL may be detrimental. Many terminally ill residents die in hospitals shortly after being transferred from nursing homes.14 Between 40 to 70% of such hospitalizations are thought to be inappropriate or potentially avoidable.15–17
Prior studies have documented wide variations with regard to hospice use and EOL hospitalizations across US nursing homes, including state-level variations,18 urban-rural differences,19 and racial disparities.20 To date, however, there has been no study specifically focusing on differences in the provision of EOL care to nursing home decedents with and without dementia. Differences in EOL care may be attributed to differential within-facility treatment provided to decedents with and without dementia residing in the same facility. However, such differences may also reflect across-facility variations resulting from different practice patterns in facilities that have distinctly different proportions of residents with and without dementia. In this study we: 1) compare patterns of hospice use and in-hospital deaths among decedents with and without dementia in US nursing homes; 2) examine whether there are within-facility differences in hospice use and in-hospital deaths between decedents with and without dementia residing in the same nursing home; and 3) determine whether there are across-facility differences in hospice use and in-hospital deaths across nursing homes with different prevalence of dementia.
METHODS
Data & Sample
The study population included all long-term care decedent residents who died in US Medicare and/or Medicaid certified facilities or in a hospital within 8 days of being transferred there during CY2003–2007. We employed the Minimum Data Set V2.0 (MDS), which contains individual level information on socio-demographics, physical and mental health status, diagnoses, and treatments, collected at regular intervals. The MDS data were linked to the Medicare beneficiary file to identify residents who died, to hospice claims to identify hospice enrollment, and to hospital claims to define hospital admissions. We also used the LTCFocUS.org website (http://ltcfocus.org/about.aspx) to identify information on facility-level characteristics.
Data from 2003 to 2007 were used to describe the trend for hospice use and in-hospital deaths. Data from CY2007 were used to examine the within-facility and across-facility differences in hospice use and in-hospital deaths between decedents with and without dementia.
In each nursing home, decedent residents were selected based on the following criteria. 1) They were long-term care residents, defined as those who stayed in a nursing home longer than three months or whose nursing home stay was not paid by Medicare. Residents who were hospitalized and returned to nursing home on Medicare were also included in the study as they were long-term care residents before their hospitalization. Rehabilitative or post-acute residents were excluded because typically these residents are admitted into nursing homes with an expectation of being discharged back into community, and death, while it occurs, is not an expected outcome. 2) They were 65 years of age and older. Nursing home residents younger than 65 years are different from the elderly with regard to their health status and treatments. 3) They had at least one comprehensive assessment (admission, annual or significant status change). We used a decedent’s last MDS assessment as the primary source of covariates for the two study outcomes. If the last assessment for a decedent was a quarterly assessment, we imputed a set of information from a prior comprehensive assessment. 4) They were not in coma. 5) They did not transfer to another nursing facility after the last MDS assessment. 6) They did not enroll in managed care in the last month of life, as Medicare inpatient claims are often incomplete for such individuals.
In total, 1,261,726 decedents in 16,347 facilities were included in CY2003–2007 trend analysis. A total of 236,619 decedents in 15,098 nursing facilities in CY2007 were included in the analyses examining the differences in EOL care between decedents with and without dementia, within and across facilities.
Dependent Variables
We used two EOL care measures as dependent variables: hospice use and in-hospital deaths. Hospice use was defined as receiving nursing home hospice care in the last 100 days of life. In-hospital deaths included two possible situations: a resident was hospitalized and died in the hospital or a resident was hospitalized and transferred to a hospital-based hospice where death occurred.
Key Independent Variables of Interest
The key independent variable for the within-facility analyses was whether a decedent had a diagnosis of Alzheimer’s disease (AD) and/or dementia other than AD on the last or last full MDS health assessment. The key independent variable of interest for the across-facility analyses was the prevalence of dementia at the facility level. It was defined as the proportion of all long-term care residents, decedents and survivors, who had a dementia diagnosis in 2007.
Covariates
To identify the covariates, we relied on the risk adjustment models developed by Mukamel for nursing home hospice use and in-hospital deaths.5 Because our study focused specifically on decedents with dementia, we also included as a covariate whether care was received in an Alzheimer’s/dementia special care unit. We grouped the resident-level characteristics into five categories. Demographic characteristics included age, gender, race/ethnicity, marital status and education. Health and functional status characteristics included activities of daily living (ADL) self performance, active disease diagnoses, infections, pressure and/or sepsis ulcers, and weight change. In the category of treatments, we included chemotherapy, feeding tube use, dialysis, chemotherapy, oxygen therapy, tracheotomy therapy, and ventilator/respirator. With regard to advance directives, do not hospitalize (DNH) and do not resuscitate (DNR) orders were included. We also included the length of stay in the last nursing home. This variable was dichotomized into less than or equal to one year and longer than one year. For each dependent variable, a separate set of covariates was employed.
We included several facility-level characteristics in the across-facility analyses, which prior studies have shown to be associated with the outcomes of interest.19, 21, 22 These included presence of a physician’s assistant (PA) or nurse practitioner (NP), proportion of residents whose primary payer source was Medicare, proportion of residents whose primary payer source was Medicaid, facility ownership, hospital based or not, number of beds, registered nurse (RN) hours per resident per day, and certified nurse aid (CNA) and licensed practical nurse (LPN) hours per resident per day.
Analytical Approach
To examine the time trend for hospice use and in-hospital deaths from 2003 to 2007, we calculated: 1) the proportion of decedents who enrolled in hospice within 100 days of death in each year; and 2) the proportion of decedents who died in a hospital in each year. For each year, Chi-square tests were used to compare the rates of hospice use and in-hospital deaths between decedents with and without dementia. We also compared individual characteristics between those with and without dementia. We used student T-test for continuous variables, and Chi-square test for categorical variables.
To examine the within-facility differences, we fit logistic regression models with facility fixed-effects. The estimated coefficients of the individual dementia diagnosis were used to test the within-facility differences. To examine the across-facility differences, we fit logistic regression models with facility random-effects. The estimated coefficients of the facility-level dementia prevalence were used to test the across-facility differences.
RESULTS
Time Trends for Hospice Use and In-hospital Deaths From 2003 to 2007
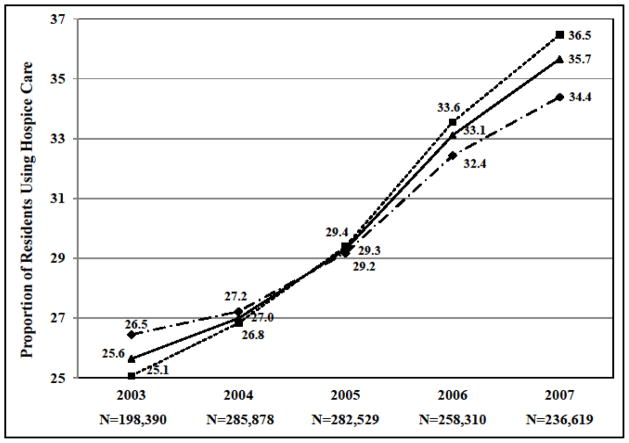
The time trends for hospice use and in-hospital deaths for all decedents, with and without dementia, are depicted in Figures 1 and 2. The rate of hospice use had increased each year, from 25.6% in 2003, to 35.7% in 2007 (Figure 1). Prior to 2005, a higher percentage of decedents without dementia used hospice care compared to those with dementia. After 2005, this trend had reversed to a higher percentage of decedents with dementia having used hospice compared to those without dementia.
Figure 1.
Hospice Use among Nursing Home Decedents from 2003 to 2007.
 Without Dementia
Without Dementia
 With Dementia
With Dementia
 Overall
Overall
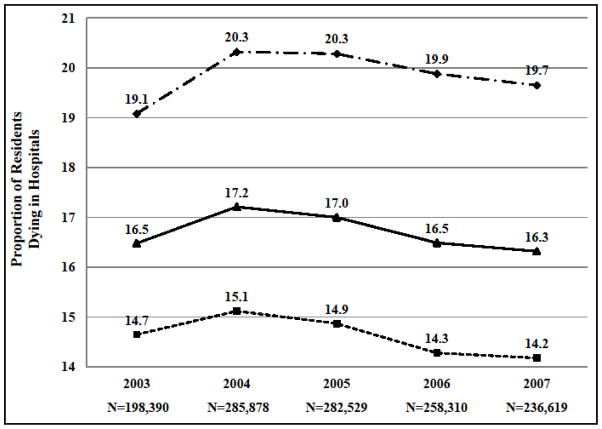
Figure 2.
In-hospital Deaths among Nursing Home Decedents from 2003 to 2007.
 Without Dementia
Without Dementia
 With Dementia
With Dementia
 Overall
Overall
The rate of in-hospital deaths in nursing homes remained virtually unchanged from 2003 to 2007, as shown in Figure 2. During this time period, the rate of in-hospital deaths among decedents with dementia was significantly and consistently lower than among decedents without dementia.
Characteristics of the Study Nursing Homes and Population in 2007
Among the decedent residents, 60.9% had a dementia diagnosis in 2007 (Table 1). Overall, 35.7% of the decedents used hospice care in the last 100 days of life, and 16.3% of the decedents died in a hospital.
Table 1.
Study Population Characteristics: 2007 Nursing Home Decedent Residents
| With dementia | Without dementia | Overall | |
|---|---|---|---|
|
| |||
| N=143,980 (60.9%) | N=92,639 (39.1%) | N=236,619 | |
| Mean(SD)/% | Mean(SD)/% | Mean(SD)/% | |
| Dependent variables | |||
| Hospice care a | 36.5 | 34.4 | 35.7 |
| In-hospital deaths a | 14.2 | 19.7 | 16.3 |
| Resident characteristics | |||
| Demographics | |||
| Age a | 87.43(7.31) | 85.22(8.62) | 86.57(7.92) |
| Gender=female a | 71.9 | 66.9 | 69.9 |
| Race=white a | 87.2 | 87 | 87.1 |
| Married a | 21.2 | 20.5 | 20.9 |
| Education a | |||
| No schooling | 0.9 | 1.1 | 0.9 |
| Less than college | 66.8 | 69.7 | 68 |
| College and higher | 16.1 | 18.1 | 16.9 |
| Unknown | 16.2 | 11.1 | 14.2 |
| Length of stay in a nursing home a | |||
| < 90 days | 3.3 | 7.9 | 5.1 |
| 90 days – 1 year | 13.9 | 20.8 | 16.6 |
| > 1 year | 82.8 | 71.3 | 78.3 |
| Health and functioning status | |||
| Activities of daily living self performance(0–28) a | 22.24(6.68) | 19.61(7.80) | 21.21(7.25) |
| Diabetes a | 27 | 34.2 | 29.9 |
| Congestive heart failure a | 28 | 36.2 | 31.2 |
| Number of cardiovascular diseases a | 1.75(1.27) | 1.83(1.29) | 1.78(1.28) |
| Asthma or COPD, or both a,c | 20.4 | 27.8 | 23.3 |
| Emphysema/COPD a,c | 19.1 | 26.2 | 21.9 |
| Cancer a | 9.7 | 17.3 | 12.7 |
| Tuberculosis | 0.02 | 0.03 | 0.02 |
| HIV infection a | 0.03 | 0.07 | 0.05 |
| Pressure ulcer or stasis ulcer, stage 2 or higher a,d | 14.5 | 15.8 | 15 |
| Pressure ulcer: at least stage 3 a,d | 7.4 | 7.5 | 7.4 |
| Hip fracture in last 180 days a | 2.8 | 2.6 | 2.7 |
| Other fracture in last 180 days a | 2.9 | 3.7 | 3.2 |
| End-stage diagnosis a | 11.4 | 13.1 | 12 |
| Swallowing problem a | 41.6 | 30.7 | 37.2 |
| Weight loss b | 23.5 | 23 | 23.3 |
| Weight gain a | 6.6 | 7.5 | 6.9 |
| Treatments | |||
| Feeding tube | 8.9 | 8.7 | 8.8 |
| Dialysis a | 0.9 | 3.2 | 1.8 |
| Chemotherapy a | 0.4 | 0.9 | 0.6 |
| Oxygen therapy a | 23.4 | 36.4 | 28.6 |
| Suctioning a | 1.4 | 2.2 | 1.7 |
| Tracheotomy care a | 0.4 | 1.5 | 0.8 |
| Ventilator/respirator a | 0.3 | 1 | 0.6 |
| Alzheimer’s/dementia special care a | 10.9 | 1.7 | 7.2 |
| Advance directives | |||
| Do not resuscitate a | 75 | 67.2 | 71.9 |
| Do not hospitalize a | 7.9 | 5.9 | 7.1 |
| Facility characteristics | N=15,098 | ||
| Prevalence of dementia among long-term care residents | 50.2%(14.5%) | ||
| Presence of a physician’s assistant or nurse practitioner | 31.1 | ||
| % of Medicare | 14.7%(13.7%) | ||
| % of Medicaid | 61.2%(21.1%) | ||
| Hospital based | 5.6 | ||
| For-profit (ownership) | 67.7 | ||
| Number of beds | 110 (65) | ||
| Registered nurse hours per resident per day | 0.34 (0.46) | ||
| Certified nurse aid & licensed practiced nurse hours per resident per day | 3.01 (1.09) | ||
P<0.001, tests between residents with and without dementia.
P<0.01.
Asthma or COPD, or both is a covariate in the model for in-hospital death; emphysema/COPD is a covariate in the model for hospice use.
Pressure ulcer or stasis ulcer, stage 2 or higher is a covariate in the model for in-hospital deaths; pressure ulcer: at least stage 3 is a covariate in the model for hospice use.
COPD: chronic obstructive pulmonary disease.
Compared to nursing home decedents without dementia, decedents with dementia tended to be older, more likely to be female, white, married, and less likely to have had some college or higher education. Decedents with dementia had worse functional status (i.e., a higher score in ADLs self performance) than decedents without dementia, and were more likely to have had a hip fracture in the last 180 days, swallowing problems, and weight loss. On the other hand, compared to decedents without dementia, those with a dementia diagnosis were less likely to have had the following conditions and symptoms: diabetes, congestive heart failure, asthma and/or COPD, cancer, HIV infection, pressure and/or stasis ulcer, fractures other than hip fracture in the last 180 days, end-stage diagnosis, and weight gain. Those with dementia also had fewer cardiovascular diseases, were less likely to have had dialysis, chemotherapy, oxygen therapy, suctioning, tracheotomy care, or be on a ventilator/respirator. However, decedents with dementia were more likely to have received care in dementia special care units, and were more likely to have had DNR and DNH orders compared to decedents without dementia.
At the facility level, the average prevalence of dementia among all long-term care residents, (decedents and survivors), was 50.2% (SD=14.5%). Overall, 67.7% of study nursing homes were for-profit, 5.6% were hospital based, and the average number of beds was 110. Among all study nursing homes, 31.1% had a PA or NP. The average RN hours per resident per day was 0.34 (SD=0.46), and CNA and LPN hours was 3.01 (SD=1.09). In an average nursing home, 61.2% (SD=21.1%) of residents were Medicaid and 14.7% (SD=13.7%) were Medicare.
Within-Facility Differences in Hospice Use and In-Hospital Deaths
Table 2 shows the results for the within-facility analyses of hospice use and in-hospital deaths. After controlling for individual characteristics and facility fixed-effects, decedents with dementia had 7% higher odds of using hospice than those without dementia (OR=1.07, 95% CI: 1.04–1.11). Resident characteristics associated with marginally higher odds of hospice use included being female, white, married, having a higher ADLs score, cancer, end-stage diagnosis, weight loss, and pressure ulcers. Decedents with congestive heart failure, or those who had stayed in their last nursing home longer than one year, were less likely to use hospice. Treatments that decedents received before death, including dialysis, tracheotomy care, and ventilator/respiratory care were also related to lower odds of using hospice. Decedents in Alzheimer’s/dementia special care units or those who used oxygen therapy were more likely to use hospice care.
Table 2.
Estimates of Fixed-Effects Model: Within-Facility Differences in Hospice Use and In-hospital Deaths
| Hospice (n=109,219) | In-hospital Deaths (n=173,836) | |||
|---|---|---|---|---|
|
| ||||
| OR | [95% CI] | OR | [95% CI] | |
| Dementia | 1.07 a | 1.04–1.11 | 0.76 a | 0.74–0.78 |
| Female | 1.14 a | 1.10–1.19 | 0.93 a | 0.90–0.96 |
| Age | 0.84 | 0.59–1.21 | 0.74 | 0.54–1.04 |
| Age squared | 1.00 | 1.00–1.01 | 1.00 | 1.00–1.01 |
| Age cubed | 1.00 | 1.00–1.00 | 1.00 | 1.00–1.00 |
| Race=white | 1.27 a | 1.20–1.34 | ||
| Education (referent= no schooling) | ||||
| Less than college | 1.08 | 0.91–1.28 | ||
| College and higher | 1.10 | 0.92–1.30 | ||
| Unknown | 0.96 | 0.80–1.14 | ||
| Married | 1.05 c | 1.01–1.09 | ||
| Length of stay in a nursing home (referent= < 1 year) | ||||
| > 1 year | 0.86 a | 0.83–0.89 | ||
| ADLs self performance | 1.03 a | 1.02–1.03 | ||
| Congestive heart failure | 0.95 b | 0.92–0.99 | ||
| Diabetes | 1.19 a | 1.16–1.22 | ||
| Number of cardiovascular diseases | 1.09 a | 1.08–1.10 | ||
| Asthma or COPD, or both | 1.11 a | 1.08–1.14 | ||
| Emphysema/COPD | 0.97 | 0.93–1.00 | ||
| Cancer | 1.78 a | 1.70–1.87 | ||
| Tuberculosis | 1.34 | 0.64–2.81 | ||
| HIV infection | 1.45 | 0.73–2.87 | ||
| Pressure ulcer or stasis ulcer: stage 2 or higher | 0.73 a | 0.70–0.75 | ||
| Pressure ulcer: at least stage 3 | 1.15 a | 1.09–1.22 | ||
| Hip fracture in last 180 days | 0.93 | 0.86–1.02 | 0.95 | 0.88–1.03 |
| Other fracture in last 180 days | 1.09 c | 1.01–1.17 | ||
| End-stage diagnosis | 8.12 a | 7.66–8.61 | ||
| Swallowing problem | 0.97 | 0.94–1.01 | ||
| Weight loss | 1.38 a | 1.33–1.42 | ||
| Weight gain | 0.96 | 0.90–1.01 | ||
| Feeding tube | 1.13 a | 1.08–1.18 | ||
| Dialysis | 0.61 a | 0.54–0.69 | 1.64 a | 1.52–1.79 |
| Chemotherapy | 0.84 | 0.69–1.01 | ||
| Oxygen therapy | 1.12 a | 1.08–1.17 | ||
| Radiation | 1.06 | 0.74–1.53 | 0.62 b | 0.46–0.85 |
| Suctioning | 0.86 | 0.73–1.01 | ||
| Tracheotomy care | 0.59 a | 0.46–0.77 | 0.57 a | 0.48–0.68 |
| Ventilator/respirator | 0.46 a | 0.34–0.62 | 1.08 | 0.88–1.32 |
| Alzheimer’s/dementia special care | 1.11 b | 1.04–1.18 | 0.89 b | 0.84–0.95 |
| Do not resuscitate | 0.49 a | 0.48–0.51 | ||
| Do not hospitalize | 0.28 a | 0.26–0.31 | ||
P<0.001.
P<0.01.
P<0.05.
ADLs: activities of daily living. COPD: chronic obstructive pulmonary disease.
Some observations were dropped from the analyses due to missing values, or a lack of within facility variation in outcome variables.
After controlling for individual characteristics and facility fixed-effects, the odds of dying in a hospital were 24% lower for decedents with dementia compared to other decedents residing in the same nursing facility (OR=0.76, 95%CI: 0.74–0.78). Resident characteristics related to marginally higher odds of dying in a hospital included diabetes, cardiovascular diseases, asthma and/or COPD, and fractures other than hip fracture in the last 180 days. Being female, and having stage 2 or higher pressure and/or stasis ulcers were associated with lower odds of dying in a hospital. Decedents who received Alzheimer’s/dementia special care, radiation, or tracheotomy care were less likely to die in a hospital, while those with feeding tube or dialysis care were more like to die in a hospital. Having a DNR or a DNH order was associated with a significantly lower odds of dying in a hospital (DNR: OR=0.49, 95% CI: 0.48–0.51; DNH: OR=0.28, 95% CI: 0.26–0.31).
Across-Facility Differences in Hospice Use and In-hospital Deaths
The results of across-facility analyses for hospice use and in-hospital deaths are depicted in Table 3. For each standard deviation increase (14.5%) in facility-level prevalence of dementia, the odds of hospice use for decedent residents increased by 7.7% (OR=1.67). Other facility factors associated with higher odds of using hospice included having a PA or NP, for-profit ownership, and more CNA and LPN hours per resident per day. In facilities with a higher proportion of residents whose primary payer source was Medicaid, or that were hospital-based, decedents were less likely to use hospice care.
Table 3.
Estimates of Random-Effects Model: Across-Facility Differences in Hospice Use and In-hospital Deaths
| Hospice (n=125,342) | In-hospital Deaths (n=179,715) | |||
|---|---|---|---|---|
| OR | [95% CI] | OR | [95% CI] | |
| Prevalence of dementia among long-term care residents | 1.67 | 1.22–2.27 | 0.92 | 0.80–1.06 |
| Resident characteristics | ||||
| Dementia | 1.09 a | 1.05–1.13 | 0.76 a | 0.74–0.78 |
| Female | 1.16 a | 1.12–1.20 | 0.93 a | 0.90–0.95 |
| Age | 0.86 | 0.6 –1.24 | 0.70 c | 0.50–0.98 |
| Age squared | 1.00 | 1.00–1.01 | 1.01 c | 1.00–1.01 |
| Age cubed | 1.00 | 1.00 –1.00 | 1.00 b | 1.00–1.00 |
| Race=white | 1.21 a | 1.15–1.28 | ||
| Education (referent= no schooling) | ||||
| Less than college | 1.05 | 0.89 –1.25 | ||
| College and higher | 1.08 | 0.90 –1.29 | ||
| Unknown | 0.92 | 0.77–1.10 | ||
| Married | 1.04 a | 1.00–1.08 | ||
| Length of stay in a nursing home (referent= < 1 year) | ||||
| > 1 year | 0.87 a | 0.84 –0.90 | ||
| ADLs self performance | 1.03 a | 1.02–1.03 | ||
| Diabetes | 1.20 a | 1.17–1.24 | ||
| Congestive heart failure | 0.95 b | 0.92–0.98 | ||
| Number of cardiovascular diseases | 1.09 a | 1.07–1.10 | ||
| Asthma or COPD, or both | 0.97 | 0.93–1.01 | ||
| Emphysema/COPD | ||||
| Cancer | 1.74 a | 1.66–1.82 | ||
| Tuberculosis | 1.28 | 0.62–2.66 | ||
| HIV infection | 1.53 | 0.78–3.00 | ||
| Pressure ulcer or stasis ulcer, stage 2 or higher | 0.74 a | 0.71–0.76 | ||
| Pressure ulcer: at least stage 3 | 1.17 a | 1.11–1.24 | ||
| Hip fracture in last 180 days | 0.93 | 0.85–1.02 | 0.96 | 0.88–1.04 |
| Other fracture in last 180 days | 1.07 | 0.99–1.15 | ||
| End-stage diagnosis | 8.10 a | 7.66–8.56 | ||
| Swallowing problem | 0.98 | 0.95–1.01 | ||
| Weight loss | 1.38 a | 1.33–1.43 | ||
| Weight gain | 0.95 | 0.90–1.01 | ||
| Feeding tube | 1.21 a | 1.16–1.27 | ||
| Dialysis | 0.60 a | 0.53–0.68 | 1.72 a | 1.59–1.87 |
| Chemotherapy | 0.82 c | 0.68–0.99 | ||
| Oxygen therapy | 1.11 a | 1.07–1.15 | ||
| Radiation | 1.09 | 0.76–1.57 | 0.68 c | 0.50–0.92 |
| Suctioning | 0.85 c | 0.72–0.99 | ||
| Tracheotomy care | 0.57 a | 0.44–0.74 | 0.57 a | 0.48–0.68 |
| Ventilator/respirator | 0.44 a | 0.32–0.60 | 1.06 | 0.86–1.30 |
| Alzheimer’s/dementia special care | 1.12 a | 1.06–1.19 | 0.84 a | 0.79–0.89 |
| Do not resuscitate | 0.48 a | 0.46–0.49 | ||
| Do not hospitalize | 0.30 a | 0.27–0.33 | ||
| Facility characteristics | ||||
| Presence of a PA or NP | 1.32 a | 1.22–1.43 | 0.87 a | 0.84–0.90 |
| % of Medicare | 0.89 | 0.56–1.42 | 2.18 a | 1.77–2.69 |
| % of Medicaid | 0.25 a | 0.19–0.32 | 2.96 a | 2.62–3.34 |
| Hospital based | 0.37 a | 0.30–0.45 | 0.91 | 0.83–1.00 |
| For-profit (ownership) | 1.74 a | 1.58–1.90 | 1.00 | 0.96–1.05 |
| Number of beds | 1.00 c | 1.00–1.00 | 1.00 c | 1.00–1.00 |
| RN hours per resident per day | 0.52 a | 0.44–0.62 | 0.84 a | 0.78–0.90 |
| CNA & LPN hours per resident per day | 1.15 a | 1.10–1.20 | 0.96 a | 0.94–0.98 |
P<0.001.
P<0.01.
P<0.05.
ADLs: activities of daily living. COPD: chronic obstructive pulmonary disease. PA: physician’s assistant. NP: nurse practitioner. RN: registered nurse. CNA: certified nurse aid. LPN: licensed practical nurse.
Some observations were dropped from the analyses due to missing values in the variables included in the models.
The facility-level prevalence of dementia was not significantly associated with the decedents’ risk of dying in a hospital. Residents were less likely to die in a hospital if they resided in a facility with a PA or NP, or received more RN or CNA and LPN hours per resident per day. Individuals in facilities with higher proportion of residents whose primary payer source was Medicare or Medicaid had higher odds of dying in a hospital.
DISCUSSION
Consistent with other studies,23, 24 we found a significant increase in hospice use among decedent nursing home residents between 2003 to 2007 (25.6% to 35.7%). While prior to 2005, decedent residents with dementia were less likely to use hospice than those without dementia, after 2005 the trend reversed, and decedents with dementia had substantially higher use of hospice services prior to death. At the same time, the rate of in-hospital deaths remained virtually unchanged from 2003 to 2007, with the rate among decedents with dementia being consistently lower compared to decedents without dementia.
We also found that in 2007 decedent residents with dementia received substantially different patterns of care with regard to hospice use and in-hospital deaths, compared to residents in the same facilities, but without a diagnosis of dementia. The former were significantly more likely to receive hospice care prior to death and less likely to die in a hospital. The higher use of hospice services associated with dementia was evident not only within facilities, but also across facilities. Decedents, regardless of dementia status, in nursing homes with a higher prevalence of dementia were more likely to use hospice care. However, the risk of in-hospital deaths was not significantly different across facilities with different prevalence of dementia.
While providing explanations for the phenomena we observe is beyond the scope of this paper, we offer several plausible scenarios. The increasing recognition of dementia as a terminal illness, and the ongoing advocacy efforts to improve EOL care for patients with dementia, may have been the driving force behind the changing patterns of nursing home care provided to this group of residents. For example, in 2005 the Alzheimer’s Association launched the Campaign for Quality Residential Care in order to improve the quality of care for residents with dementia in assisted living and nursing home facilities. One phase of this campaign focused specifically on improving EOL care for residents with dementia, including increasing hospice use and decreasing the inappropriate or avoidable aggressive care.25 As nursing homes with higher proportion of dementia residents experience the benefits of hospice for their decedent residents with dementia, they may be more likely to refer other EOL decedents to hospice as well. Such nursing home behavior would be consistent with our findings for across-facility differences in hospice use. A recent study showed that decedents’ hospice use is associated with nursing home EOL care practices, after controlling for individual and facility characteristics26.
While an increase in hospice use may indicate improvements in EOL quality of care, some concerns about hospice use in nursing homes remain. First, despite the growth in hospice use, rate among decedent residents with dementia remains quite low. Partially, this may be due to the difficulty in providing acute prognosis of life expectancy of 6 or fewer months, as required by Medicare, for residents with dementia. As demonstrated in one study, only 1% of newly admitted nursing home residents with dementia received a life expectancy prognosis of six months or shorter, yet 71% died within six months.27 Because nursing home residents have quite unpredictable disease trajectories, particularly those with dementia, it has been suggested that bundled benefit of palliative care and restorative care for nursing home residents may be more effective to achieve better quality of EOL care than continuing to rely on hospice referral.28, 29 By removing the eligibility criterion of a prognosis of six months or shorter life expectancy, the bundled benefit may be able to provide the much needed access to palliative care for all residents, particularly for those at the EOL. Another remaining concern with hospice provision in nursing homes has been that the quality of hospice care remains largely unknown. Limited existing evidence with regard to hospice care suggested some concerns about its quality for people with dementia.30 Overall, the significant increase in the use of hospice care in nursing homes has been a result of the substantial growth in hospice providers, particularly for-profit providers.23
Between 2000 and 2007, the number of for-profit hospices doubled while the number of nonprofit remained the same.31 It was suggested that the care of patients with dementia may be more profitable for hospice providers.30 Indeed, more decedent residents with dementia had been enrolled in for-profit compared to non-profit hospices, and these residents stayed in hospice longer. At the same time nursing home decedent residents with dementia who receive hospice care, have fewer visits per day by skilled personnel, compared to hospice recipients without dementia.30 Future research is needed to evaluate the quality of hospice care provided to nursing home decedent residents with and without dementia.
Although we did not observe a longitudinal change in the pattern of in-hospital deaths for decedents with and without dementia, the within-facility differences suggest that nursing homes provide less aggressive treatment to decedents with dementia, both with regard to hospice use and EOL hospital transfers. Although it is evident that hospitalizing terminally ill nursing home residents may result in adverse outcomes, nursing homes continue to transfer dying residents to hospitals, but they are less likely to do so for decedent residents with dementia compared to those without dementia. Knowing a resident’s treatment preferences with regard to hospitalizations is an important predictor of such transfers at the EOL. Our findings demonstrate that the odds of dying in a hospital for decedents having a DNH order was 72% lower compared to those without a DNH. However, DNH orders are uncommon in nursing homes, for all residents and those with dementia as well.32, 33 In our study, only 7.9% of decedents with dementia and 5.9% of decedents without dementia had a DNH order.
Several study limitations should be noted. First, potential omitted variable bias, which exists in any study, may also be present in our study. However, we used the MDS dataset which provides a considerably richer selection of variables of interest than typically found in administrative databases. Second, the potential under-diagnosis of dementia may bias the results34. If dementia is under-diagnosed in the MDS health assessments, some decedent residents who were categorized as not having dementia might have actually had the disease. However, if this is the case, the actual effect size of the within-facility differences would be greater than what we have found. For the across-facility differences, we cannot predict the direction of the potential bias, because we do not have any evidence as to whether the under-diagnosis of dementia problem varies across facilities. Third, we do not adjust for the complexity or the duration of dementia and that could potentially bias the results, but we have no reason to believe that there is a biased distribution of residents with more advanced dementia across facilities.
In conclusion, this study found that nursing home decedent residents with dementia were more likely to use hospice and less likely to die in a hospital, suggesting that decedents with dementia may receive less aggressive EOL care. Future studies are needed to better understand the mechanism underlying the differences in hospice use and in-hospital deaths between decedent residents with and without dementia, and to evaluate the quality of hospice care provided to all nursing home decedent residents, and in particular to those with dementia.
Acknowledgments
This work was supported by the National Institute of Nursing Research [NR010727 to Helena Temkin-Greener], and was presented at 2012 Academy Health Annual Research Meeting and 2012 American Public Health Association Annual Meeting.
We gratefully acknowledge funding support from the National Institute of Nursing Research grant NR010727.
Sponsor’s Role: The funding institution had no role in the design, methods, data collection, analysis, or preparation of manuscript or in the decision to submit the manuscript for publication.
Footnotes
Conflict of Interest Checklist:
| Elements of Financial/Personal Conflicts | *Author 1 Q Li | Author 2 NT Zheng | Author 3 H Temkin-Greener | |||
|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | |
| Employment or Affiliation | x | x | x | |||
| Grants/Funds | x | x | x | |||
| Honoraria | x | x | x | |||
| Speaker Forum | x | x | x | |||
| Consultant | x | x | x | |||
| Stocks | x | x | x | |||
| Royalties | x | x | x | |||
| Expert Testimony | x | x | x | |||
| Board Member | x | x | x | |||
| Patents | x | x | x | |||
| Personal Relationship | x | x | x | |||
*Authors can be listed by abbreviations of their names
For “yes”, provide a brief explanation:____________________
Author Contributions: Qinghua Li: Study concept and design, data management, analysis and interpretation, preparation of manuscript. Nan Tracy Zheng: Data management, preparation of manuscript. Helena Temkin-Greener: Study concept and design, acquisition of data, interpretation of data analysis, preparation of manuscript.
References
- 1.Centers for Medicare and Medicaid Services. [Accessed 06/03/2011];MDS Active Resident Information Report (online) Available from: https://www.cms.gov/MDSPubQIandResRep/04_activeresreport.asp?date=32&isSubmitted=res2.
- 2.Knight BG, Sayegh P. Mental health and aging in the 21st century. Journal of Aging & Social Policy. 2011;23(3):228. doi: 10.1080/08959420.2011.579494. [DOI] [PubMed] [Google Scholar]
- 3.Ferri CP, Prince M, Brayne C, et al. Global prevalence of dementia: a Delphi consensus study. The Lancet. 2006;366(9503):2112–2117. doi: 10.1016/S0140-6736(05)67889-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mitchell SL, Teno JM, Miller SC, et al. A National Study of the Location of Death for Older Persons with Dementia. Journal of the American Geriatrics Society. 2005;53(2):299–305. doi: 10.1111/j.1532-5415.2005.53118.x. [DOI] [PubMed] [Google Scholar]
- 5.Mukamel DB, Caprio T, Ahn R, et al. End-of-Life Quality-of-Care Measures for Nursing Homes: Place of Death and Hospice. Journal of Palliative Medicine. 2012;15(4):438–446. doi: 10.1089/jpm.2011.0345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Miller SC, Mor V, Wu N, et al. Does receipt of hospice care in nursing homes improve the management of pain at the end of life? Journal of the American Geriatrics Society. 2002;50(3):507–515. doi: 10.1046/j.1532-5415.2002.50118.x. [DOI] [PubMed] [Google Scholar]
- 7.Miller SC, Gozalo P, Mor V. Outcomes and Utlization for Hospice and Non-hospice Nursing Facility Decedents. Office of Disability, Aging and Long-Term Care Policy; US: 2000. [Google Scholar]
- 8.Miller SC, Mor V, Teno JM. Hospice enrollment and pain assessment and management in nursing homes. Journal of Pain and Symptom Management. 2003;26(3):791–799. doi: 10.1016/s0885-3924(03)00284-7. [DOI] [PubMed] [Google Scholar]
- 9.Miller SC, Gozalo P, Mor V. Hospice enrollment and hospitalization of dying nursing home patients. The American journal of medicine. 2001;111(1):38–44. doi: 10.1016/s0002-9343(01)00747-1. [DOI] [PubMed] [Google Scholar]
- 10.Teno JM, Gozalo PL, Lee IC, et al. Does Hospice Improve Quality of Care for Persons Dying from Dementia? Journal of the American Geriatrics Society. 2011 doi: 10.1111/j.1532-5415.2011.03505.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miller SC, Lima JC, Mitchell SL. Influence of Hospice on Nursing Home Residents with Advanced Dementia Who Received Medicare-Skilled Nursing Facility Care Near the End of Life. Journal of the American Geriatrics Society. 2012;60(11):2035–2041. doi: 10.1111/j.1532-5415.2012.04204.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kiely DK, Givens JL, Shaffer ML, et al. Hospice Use and Outcomes in Nursing Home Residents with Advanced Dementia. Journal of the American Geriatrics Society. 2010;58:12–2291. doi: 10.1111/j.1532-5415.2010.03185.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Mitchell SL, Kiely DK, Miller SC, et al. Hospice care for patients with dementia. Journal of Pain and Symptom Management. 2007;34(1):7–16. doi: 10.1016/j.jpainsymman.2007.01.003. [DOI] [PubMed] [Google Scholar]
- 14.Smith WR, Kellerman A, Brown JS. The impact of nursing home transfer policies at the end of life on a public acute care hospital. Journal of the American Geriatrics Society. 1995;43(9):1052. doi: 10.1111/j.1532-5415.1995.tb05573.x. [DOI] [PubMed] [Google Scholar]
- 15.Saliba D, Kington R, Buchanan J, et al. Appropriateness of the decision to transfer nursing facility residents to the hospital. J Am Geriatr Soc. 2000;48(2):154–163. doi: 10.1111/j.1532-5415.2000.tb03906.x. [DOI] [PubMed] [Google Scholar]
- 16.Zinn JS, Aaronson WE, Rosko MD. Variations in the outcomes of care provided in Pennsylvania nursing homes: Facility and environmental correlates. Medical Care. 1993;31(6):475. doi: 10.1097/00005650-199306000-00001. [DOI] [PubMed] [Google Scholar]
- 17.Ouslander JG, Lamb G, Perloe M, et al. Potentially avoidable hospitalizations of nursing home residents: Frequency, causes, and costs. J Am Geriatr Soc. 2010;58(4):627–635. doi: 10.1111/j.1532-5415.2010.02768.x. [DOI] [PubMed] [Google Scholar]
- 18.Gozalo P, Teno JM, Mitchell SL, et al. End-of-Life Transitions among Nursing Home Residents with Cognitive Issues. New England Journal of Medicine. 2011;365(13):1212–1221. doi: 10.1056/NEJMsa1100347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Temkin-Greener H, Zheng NT, Mukamel DB. Rural–Urban Differences in End-of-Life Nursing Home Care: Facility and Environmental Factors. The Gerontologist. 2012 doi: 10.1093/geront/gnr143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Zheng NT, Mukamel DB, Caprio T, et al. Racial Disparities in In-hospital Death and Hospice Use Among Nursing Home Residents at the End of Life. Medical care. 2011;49(11):992. doi: 10.1097/MLR.0b013e318236384e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cai S, Mukamel DB, Veazie P, et al. Hospitalizations in nursing homes: Does payer source matter? Evidence from New York State. Medical Care Research and Review. 2011;68(5):559–578. doi: 10.1177/1077558711399581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Teno JM, Gozalo P, Mitchell SL, et al. Terminal Hospitalizations of Nursing Home Residents: Does Facility Increasing the Rate of Do Not Resuscitate Orders Reduce Them? Journal of Pain and Symptom Management. 2011;41(6):1040–1047. doi: 10.1016/j.jpainsymman.2010.07.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Miller SC, Lima J, Gozalo PL, et al. The growth of hospice care in US nursing homes. Journal of the American Geriatrics Society. 2010;58(8):1481–1488. doi: 10.1111/j.1532-5415.2010.02968.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Miller SC, Lima JC, Mitchell SL. Hospice Care for Persons With Dementia: The Growth of Access in US Nursing Homes. American Journal of Alzheimer’s Disease and Other Dementias. 2010;25(8):666–673. doi: 10.1177/1533317510385809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Alzheimer’s Association. Dementia Care Practice Recommendations for Assisted Living Residences and Nursing Homes, Phase 3, End-of-Life Care. 2008. [Google Scholar]
- 26.Zheng NT, Mukamel DB, Caprio TV, et al. Hospice Utilization in Nursing Homes: Association With Facility End-of-Life Care Practices. The Gerontologist. 2012 doi: 10.1093/geront/gns153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mitchell SL, Kiely DK, Hamel MB. Dying with advanced dementia in the nursing home. Archives of internal medicine. 2004;164(3):321. doi: 10.1001/archinte.164.3.321. [DOI] [PubMed] [Google Scholar]
- 28.Meier DE, Lim B, Carlson MDA. Raising The Standard: Palliative Care In Nursing Homes. Health Affairs. 2010;29(1):136–140. doi: 10.1377/hlthaff.2009.0912. [DOI] [PubMed] [Google Scholar]
- 29.Huskamp, Stevenson DG, Chernew ME, et al. A new Medicare end-of-life benefit for nursing home residents. Health Affairs. 2010;29(1):130–135. doi: 10.1377/hlthaff.2009.0523. [DOI] [PubMed] [Google Scholar]
- 30.Wachterman, Marcantonio, Davis, et al. Association of Hospice Agency Profit Status With Patient Diagnosis, Location of Care, and Length of Stay. JAMA: The Journal of the American Medical Association. 2011;305(5):472–479. doi: 10.1001/jama.2011.70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Miller SC U.S. Senate. Report to the Congress: Reforming the delivery system. Medicare Payment Advisory Commission; 2008. [Google Scholar]
- 32.Lamberg JL, Person CJ, Kiely DK, et al. Decisions to hospitalize nursing home residents dying with advanced dementia. Journal of the American Geriatrics Society. 2005;53(8):1396–1401. doi: 10.1111/j.1532-5415.2005.53426.x. [DOI] [PubMed] [Google Scholar]
- 33.Mitchell SL, Teno JM, Intrator O, et al. Decisions to Forgo Hospitalization in Advanced Dementia: A Nationwide Study. Journal of the American Geriatrics Society. 2007;55(3):432–438. doi: 10.1111/j.1532-5415.2007.01086.x. [DOI] [PubMed] [Google Scholar]
- 34.Vincent M, Orna I, Mark U, et al. BMC Health Services Research. Temporal and Geographic variation in the validity and internal consistency of the Nursing Home Resident Assessment Minimum Data Set 2.0; p. 11. [DOI] [PMC free article] [PubMed] [Google Scholar]