Abstract
Background
We hypothesize that a deficient premotor-motor inhibitory network contributes to the unwanted involuntary movements in dystonia.
Methods
We studied nine controls and nine patients with writer’s cramp (WC). Dorsal premotor-motor cortical inhibition (dPMI) was tested by applying conditioning transcranial magnetic stimulation (TMS) to the dorsal premotor cortex and then a test pulse to the ipsilateral motor cortex at an interval of 6ms. We used an H-reflex in flexor carpi radialis paired with TMS over the premotor cortex to assess for spinal cord excitability change. Finally, we interrupted a choice reaction time task with TMS over dorsal premotor cortex to assess performance in a non-dystonic task.
Results
Our results showed that WC patients exhibited dPMI at rest (88.5%, the ratio of conditioned to unconditioned test pulse) in contrast to our controls who did not show dPMI (109.6%) (p=0.0198). This difference between patients and controls persisted during contraction (100% vs. 112%) and pen-holding (95.6% vs. 111%). The H-reflex in the arm was not modulated by the premotor cortex stimulation. WC patients made more errors and the error rate improved with TMS over the premotor cortex.
Conclusions
These results suggest that abnormal premotor-motor interactions may play a role in the pathophysiology of focal dystonia. dPMI was not modulated by task in either group, but was constantly greater in the patients. The significance of the increased inhibition is likely to be compensatory. It appears to be a robust finding and, in combination with other features, could be further explored as a biomarker.
Keywords: TMS, Dystonia, Motor cortex
INTRODUCTION
Dystonia is characterized by abnormal postures and twisting movements, which can lead to significant disability in activities of daily living. In adults, dystonia is typically focal in its presentation with the most common involvement in the eyes, neck or limbs.1 Focal limb dystonia can be task-specific as in writer’s cramp (WC)—where the motor system functions normally for a majority of motor tasks but abnormal muscle contractions of the hand and forearm cause an abnormal cramping posture during writing.
This task-specific dysfunction suggests an abnormality originating when pairing a motor task with a particular effector limb. The dorsal premotor cortex has been a suggested location for this transformation to occur.2 fMRI data suggest that the dorsal premotor cortex is aberrantly overactive during a mental imagery task in WC patients;3 and although others have found deficient left dorsal premotor cortex activation4—there appears to be consistent aberrant signal seen in WC patients in the premotor cortex compared to controls. Inhibiting activity in the dorsal premotor cortex is associated with improvement in writing ability in WC patients.5 Our group previously investigated dorsal premotor-motor cortical inhibition (dPMI) during a phasic movement in normal subjects and WC patients.6 The normal subjects showed no dPMI at rest or with movement. Unexpectedly, we found enhanced dPMI in WC patients in a surround muscle at rest with abolition of dPMI during a phasic movement, suggesting that dPMI might be an abnormal mechanism for the failure of surround inhibition in the patients.6
To further understand whether the enhancement of dPMI at rest is part of a compensatory response suppressing dystonic posture or plays an active pathophysiologic role in the generation of the dystonic movements in WC patients, we studied a simple tonic movement and a task-specific tonic posture (holding a pen). In addition, as there are direct projections from the premotor cortex to the spinal cord,7 we paired premotor transcranial magnetic stimulation (TMS) with an H reflex in the arm to assess for spinal cord excitability change to pinpoint the origin of the inhibition (e.g. cortical vs. spinal). As the premotor cortex is a potential therapeutic site for intervention, we looked at WC patients’ performance in a non-dystonic task and then interrupted the activity of the premotor cortex in a choice reaction time task to look for improvement or impairment in performance in this motor task. Finally, the diagnosis of focal dystonia is made clinically as there is no clear biomarker as yet identified. Given this information gap, we sought to analyze dPMI as a potential biomarker as this will be helpful in reducing diagnostic confusion, aiding with inclusion in clinical trials and providing an objective measure during intervention trials.
METHODS
Patients
We studied 9 WC right-handed patients (7 men) and 9 age-matched, right-handed healthy volunteers (6 men) with mean ages 55 years (48–71 years) and 51 years (24–72 years), respectively. The WC patients were all affected on their dominant side (right) and one WC patient had bilateral WC. WC patients were studied at least 3 months after the last botulinum toxin treatment. We also studied an additional 9 healthy volunteers (mean age 27 years) in the H reflex experiment. All subjects met all inclusion criteria and signed an informed consent. The study was approved by the National Institutes of Health Institutional Review Board.
Study design
dPMI
Disposable surface silver-silver chloride EMG electrodes were placed on the right first dorsal interosseous muscle (FDI) in a bipolar montage. Resting motor threshold (RMT) was determined over the primary motor cortex corresponding to the right first dorsal interosseous muscle (FDI). The coil over the dorsal premotor cortex (dPM) was placed 8% of the nasion-inion distance (~2 cm) anterior and 1cm medial to the “hotspot” for FDI, ipsilateral and confirmed with a neuronavigation system (Brainsight™, Rogue Research Inc., Montreal, Quebec, Canada, Figure 1). With both coils in place, the RMT and active motor threshold (AMT) during a 10% maximum voluntary contraction of the FDI, as measured by force transducer, were determined to the nearest 1% of maximal stimulator output. The EMG signal was amplified using a conventional EMG machine (Nicolet Viking) with bandpass between 10 and 2000 Hz and digitized at 5kHz.
Figure 1.
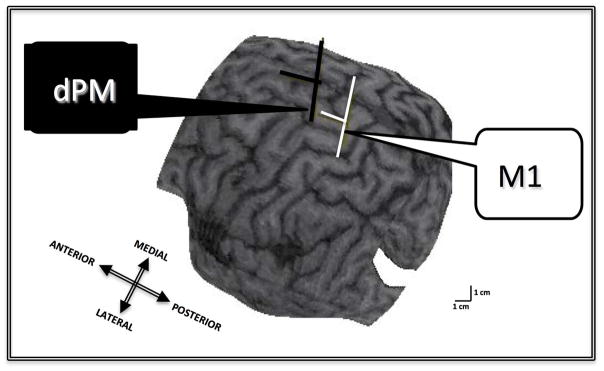
Brainsight™-derived image from representative subject showing the localization of the coil placement over the left dorsal premotor cortex (dPM) and the primary motor cortex (M1) for the hand representation. The T-shaped symbol represents the computer-generated trajectory of the TMS pulse from the scalp to the cortex.
The Magstim Bistim2 (Magstim Co., Whitland, Dyfed, UK), connected to two custom figure-8 coils with an inner loop diameter of 35mm, was used. One coil was placed over the FDI M1 “hot spot”, tangential to the scalp with the handle pointing backwards and laterally at a 45-degree angle away from midline. The second coil over dPM was oriented to produce currents in an anterior to posterior direction as in Beck et al.6 The coils slightly overlapped with the dPM coil flush on the scalp and the M1 coil slightly elevated.
At least 12 MEPs were collected in each of six conditions. The stimuli with each condition block were delivered at a random interval between 3 and 9 seconds. The conditions were performed in the following order: rest, isometric FDI contraction, and pen-holding task. We performed them in this order to stabilize the subject’s hand and wrist at rest within a plexiglass platform holding the force transducer for the first two conditions. Further, we wanted to prevent dystonic contractions so began with the least task-specific movement and then progressed to the writing posture. The isometric FDI condition consisted of the subject contracting FDI at 10% MVC, with his/her wrist stabilized with a Velcro strap to hold in place in the platform. The pen-holding task consisted of the subject holding a pen in their right hand and maintaining that posture throughout the testing. For this condition, the hand and wrist were removed from the plexiglass platform. To ensure, a consistent posture, the WC subjects were instructed to hold the pen to a dot on a paper at all times. The WC subjects were able to perform all conditions, including the isometric contraction and pen-holding task, without dystonic posturing. The interstimulus interval (ISI) was 6msec between the conditioning dPM pulse and the M1 test pulse with dPM pulse intensity at 0.9AMT and M1 pulse intensity at 1.2RMT. In the two movement conditions, the TMS stimulator intensity was adjusted to produce MEP amplitudes approximately equal to amplitudes in the rest condition.
Statistics
The results of the experimental tests were entered into a computerized database. Outcome measures (i.e., peak-to-peak amplitude change) were compared using a two-group repeated measures analysis of variance using PROC MIXED in SAS version 9.3. P values less than 0.05 were considered significant. To test the hypothesis that there is enhanced dPMI at rest, measurements of normalized MEPs (conditioning plus test/test alone) recorded from FDI at rest were compared between control and dystonia groups. To test the secondary hypothesis that abnormal dPMI would be task-dependent, we compared the measurement of normalized MEPs recorded from FDI during FDI contraction and during the pen-holding task using appropriately constructed contrasts in effects within PROC MIXED. We used an autoregressive correlation structure to account for the condition ordering.
H reflex
In order to determine if the conditioning stimuli over dPM affects spinal motor neuron pool excitability in the normal motor system, we recorded H reflexes from flexor carpi radialis (FCR) in 9 healthy subjects. The reflex was assessed by low-intensity electrical stimulation of median nerve at the elbow. Given a cortical ISI of 6msec, the ISI between cortical conditioning pulse and median nerve stimulation was adjusted for H reflex latency in each subject. Once the optimal ISI had been calculated, we also looked at ISI −2msec, −1msec, +1msec, and +2msec around the ISI.
Statistics
The results of the experimental tests were entered into a computerized database. To test the hypothesis that there is no difference between H reflex measures with and without premotor conditioning in the six conditions, we used a PROC MIXED in SAS v. 9.3 to compare the Mmax as well as the percent of the control H reflex amplitude.
Choice Reaction Time Task
Subjects were seated in a comfortable chair, facing a computer screen with their heads stabilized in position. The subjects placed their right hand on the desk and had their legs uncrossed beneath the desk. Disposable surface EMG electrodes were placed on the right FDI and ipsilateral soleus in a bipolar montage. The Magstim Bistim2 (Magstim Co., Whitland, Dyfed, UK), connected to a custom figure-8 coil with an inner loop diameter of 35mm, was used.
The subjects were asked to respond to a shape on the computer screen. The particular shape instructed the subject to either press a button with their right hand or to press a foot pedal with their right foot. Based on the methods described by Schluter et al.,8 the shapes were presented for 100ms with a 4 sec interval between trials. Practice sessions without a dPM pulse were conducted prior to beginning the experimental trials. The subjects were reminded to do the task as accurately and quickly as possible. One control subject and one WC patient were not able to learn the task accurately and did not complete this experiment. TMS over the dPM was given at 70% of stimulator output at an interval of 140msec from the cue-onset—as this interval showed the maximal disruption of response times in controls in a similar paradigm.8 Five blocks of 20 trials were conducted with half of the trials without stimulation, leaving a total of 200 dPM TMS pulses for the entire experimental session. EMG data were recorded from FDI and SOL prior to and during the task to ensure that the dPM stimulation did not elicit a MEP and to record any dystonic discharges in the affected limb during the task. The primary outcome measure was the change from baseline (without conditioning dPM pulse) in the time to button press or foot pedal press. This change in reaction time was compared between the FHD and control groups. In addition, the accuracy of response choice was also recorded.
Statistics
Outcome measures were compared using a two-group repeated measures analysis of variance using appropriately constructed contrasts in effects within PROC MIXED. To test the hypothesis that the abnormality of task-specificity in WC is due to abnormal premotor cortex activity, we compared measurements of the change in reaction times due to dPM TMS in the WC group vs. the control group. We also explored the change in reaction times for hand vs. leg movements both within the WC and control groups as well as between groups. We used a generalized linear mixed model logistic regression analysis to compare error rates between WC patients and controls.
Biomarker Analysis
The results of the dPMI measures from this study and our published results from Beck et al.6 of dPMI rest values obtained in abductor pollicis brevis (APB) were combined to increase the number of subjects analyzed (n=19 in each group). We constructed a receiver operating characteristics (ROC) curve, a plot of sensitivity vs. 1-specificity across the range of possible dPMI values at rest in hand muscles (combined data for FDI and APB).9
RESULTS
dPMI
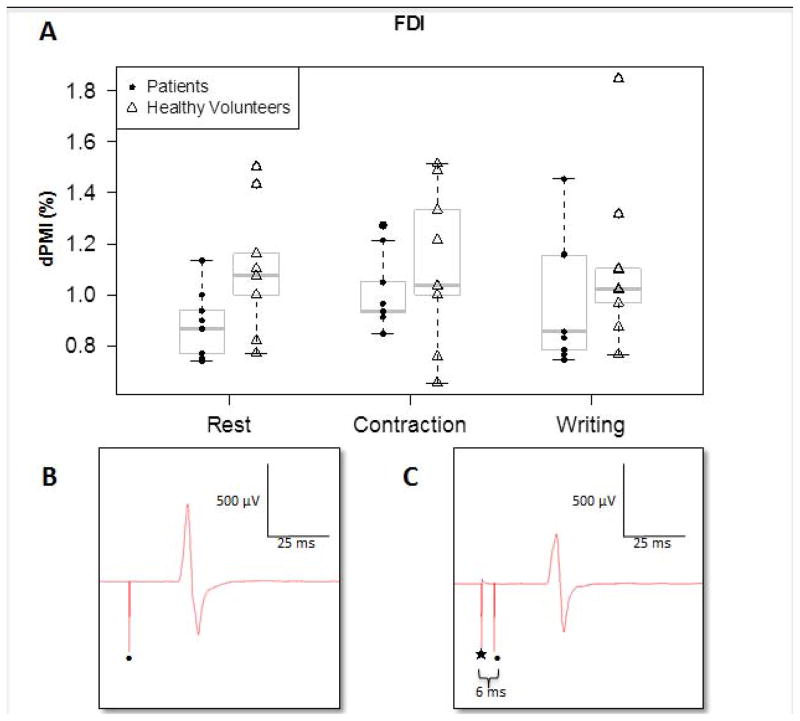
We compared the peak-to-peak MEP amplitude in all conditions in WC patients and healthy controls and present the ratio of dPM conditioned MEP amplitudes to unconditioned MEP amplitudes, with anything less than one representing an inhibitory conditioning influence from the premotor cortex. Each subject had three repeated measures (conditions). In order to compare arms and account for within subject correlation on the measures, a two-way repeated measures ANOVA was performed using PROC MIXED in SAS ver. 9.3; the correlation structure was taken to be auto-regressive because treatment order was fixed. Interaction between condition and arm was not significant (p = 0.85), condition was not significant (p = 0.75), but arms differed significantly (p = 0.007). A contrast comparing patients to controls estimates patients to be 0.16 %dPMI lower than controls on average across conditions (se = 0.051). Illustrated in Figure 2. WC patients exhibited dPMI at rest (88.5%, the ratio of conditioned to unconditioned test pulse) in contrast to controls who did not show dPMI at rest (109.6%). The difference between patients and controls persisted during contraction (100% vs. 112%) and pen-holding (95.6% vs. 111%) as well.
Figure 2.
A) Boxplots of group and individual data showing enhanced dPMI at rest, with contraction and during pen-holding task in WC patient group (*p=0.007). B) Representative MEP tracing from WC patient in test condition (• artifact from test stimulus). C) MEP tracing from same patient during dPM conditioning (| artifact from conditioning stimulus, • artifact from test stimulus) with smaller MEP peak-to-peak amplitude—showing inhibitory conditioning from dorsal premotor cortex to motor cortex.
H reflex
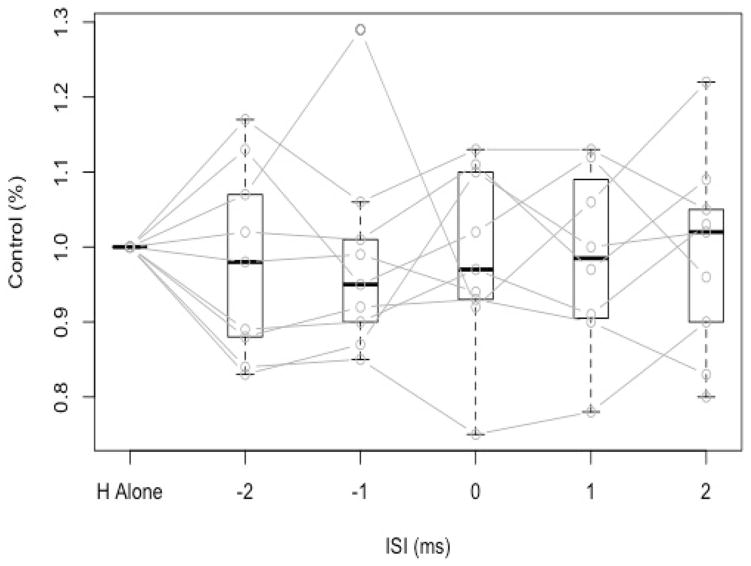
We used the following formula to calculate the ISI between premotor stimulation and H reflex stimulation: ISI= (6ms + MEP latency) − H latency. The mean ISI was 4.67 msec (STD 2.50). When comparing the H reflex alone with the premotor conditioning pulse, there was no significant difference in H reflex amplitude (p=0.9836) (Figure 3). We also looked at ISI intervals at 2 msec before and after the calculated ISI in order to fully capture any conditioning influence of the premotor stimulation. There were no significant differences seen (Figure 3).
Figure 3.
Boxplots of group and individual data showing no difference premotor conditioned H reflex from H reflex alone—without conditioning (p=0.9836).
Choice Reaction Time Task
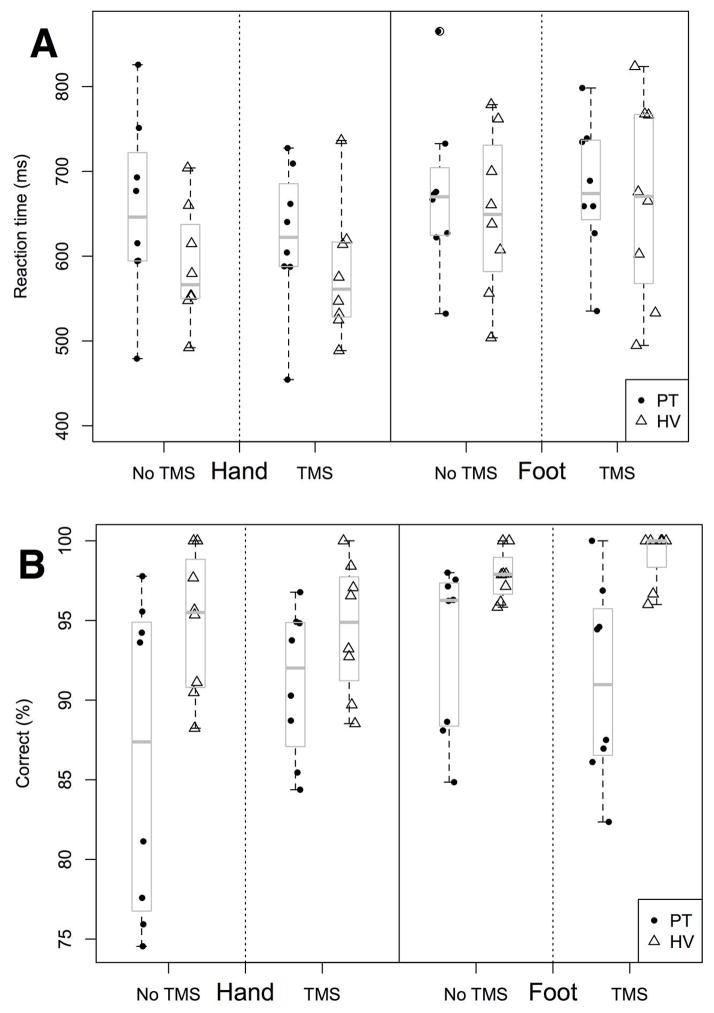
WC patients showed a trend toward a longer reaction time 680 msec (SD 120) vs. 577 msec (SD 72) in healthy controls in the hand (p=0.1046). dPM TMS did not influence the reaction time in patients (653 msec, SD 107) or in controls (582 msec, SD 80). Patients and controls both had longer reaction times in the foot compared to the hand but did not differ between groups, 691 msec (SD 96) and 678 msec (SD 80). As in the hand, TMS did not influence reaction time in the foot significantly (682 msec (SD 103) in patients and 684 msec (SD 98) in controls) (Figure 4A). Patients did show an increase in errors in their choice responses and this difference was improved by TMS (p=0.0084). In addition, WC patients were more likely to make an error in the hand than in the foot response (p=0.0003) (Figure 4B).
Figure 4.
A) Boxplots of group and individual data showing trend toward longer choice reaction time in the hand (p=0.1046). B) Boxplots of group and individual data showing significantly more errors in WC patients than in healthy controls (p=0.0084).
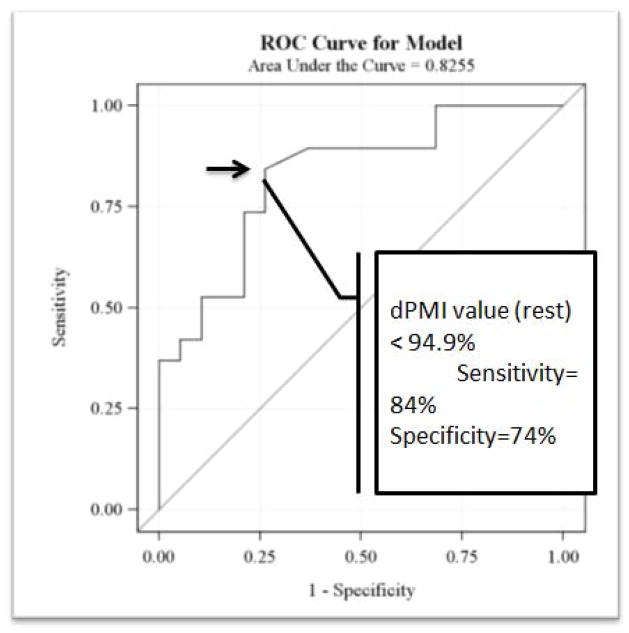
Biomarker Analysis
We found that the lower the dPMI rest value (i.e., enhanced inhibition), the greater the increased specificity that the value was from the WC patient group. The area under the curve (AUC) was 0.825. The receiver operating curve was constructed and the shoulder/cut-off value was at a dPMI level of 94.9% which has a sensitivity of 84% and specificity of 74% (Figure 5).
Figure 5.
Receiver Operating Characteristics Curve for dPMI at rest.
DISCUSSION
These results confirm our prior results that dPMI is enhanced in WC patients at rest—and extends those findings to show that abnormal premotor-motor cortex interactions in dystonia patients persist during tonic movement as well as during a task-specific movement. While with movement, WC patients do not show dPMI (100% in isometric contraction) or limited dPMI in the pen-holding task (95.6%), healthy controls show continued facilitation at 112% and 111%, respectively. In addition, the inhibitory influence from the premotor cortex appears to be supraspinal in nature as there was no change in the H-reflex with premotor conditioning stimulation in healthy controls. This enhanced inhibition in WC patients at rest has to be considered in the background where the characteristic physiologic abnormality seen is a loss of inhibition.10 One possibility is that the enhanced inhibition from premotor to motor cortex is compensatory (e.g., a reaction to abnormal excitation). This compensation, when working, may help to prevent abnormal muscle contractions. We did not see the modulation of dPMI in a task-dependent manner--although there was a trend toward less dPMI with movement but patients still differed significantly from controls during movement suggesting that loss of the enhanced dPMI may play a role in abnormal contractions with movement and that the abnormal movements are suppressed at rest due to the relatively enhanced dPMI. Additionally, we found that TMS over the premotor cortex reduced errors in a choice reaction time task. This is consistent with previous studies showing that rTMS over the premotor cortex improves WC symptoms and supports the idea that enhanced dPMI is a compensatory process that can be further enhanced by noninvasive techniques.5, 11 The alternative possibility that enhanced dPMI is part of the primary pathophysiologic abnormality in writer’s cramp is less well supported by current evidence.
While writer’s cramp is a motor abnormality in its presentation, WC patients may have sensory and cognitive impairments found on detailed testing. Impairment in temporal discrimination between tactile stimuli has been shown both in the affected limb as well in the unaffected limb in WC patients.12 Higher level sensory processing such as in studies looking at time-dependent features of movement have been found abnormal in WC patients—with increased timing errors found in the patient group.13 As these cognitive and sensory changes are seen independent of the affected limb or independent of performing the abnormal motor task, they have been considered to be possible endophenotypes of focal dystonia.14 Similarly, we found in our WC patients, in a non-dystonic task, there was a trend toward a longer choice reaction time as well as significantly more errors made in the dystonia group. Administering TMS to the premotor cortex decreased the error rate in dystonia patients, suggesting a role for motor planning abnormalities in the generation of the increased error rate. Again, whether this impaired motor function in a non-dystonic task is due to compensation (e.g., enhanced dPMI) or due to an underlying endophenotypic abnormality in sensorimotor integration is a more general sense is not entirely clear; however, it is interesting that interrupting the area where enhanced inhibition is found, improved accuracy in the WC patients. If it is due to compensation, there may be unintended consequences in “normal” movement that need to be considered when further enhancing inhibition in the premotor cortex as a therapeutic strategy.
Abnormal premotor-motor interactions may play a role in the pathophysiology of focal dystonia, primarily or as compensation. This abnormality is robust. Given our small sample size, dPMI at rest as a biomarker is unlikely to be employed on its own; however, its usefulness as a biomarker may increase in combination with other markers such as abnormal tactile discrimination, yielding a “panel” of physiologic tests that would improve the diagnostic certainty in focal dystonia.12 The premotor cortex is a therapeutic target that may enhance a compensatory response; however, this should be balanced by any potential worsening of non-dystonic motor performance. The role of dPMI now needs to be assessed in other focal dystonias to see if this is a common pathway that is disturbed in dystonia rather than simply as a marker of task-specificity.
Acknowledgments
We would like to thank Ronald Schrader, PhD for his statistical expertise. We would like to thank Drs. Bill Shuttleworth and Leslie Morrison for thoughtful review and discussion of prior drafts of this manuscript.
Funding Source:
The project was supported (in part or in full) by the National Center for Research Resources and the National Center for Advancing Translational Sciences of the National Institutes of Health through Grant Number KL2 TR000089 and Grant Number UL1 TR000041. The project was also supported through NIH/NINDS Intramural Funds.
AUTHOR ROLES
Dr. Pirio Richardson: 1) Research project: A. Conception, B. Organization C. Execution; 2) Statistical analysis: A. Design, B. Execution, C. Review and Critique; 3) Manuscript: A. Writing of the first draft, B. Review and Critique.
Dr. Beck: 1) Research project: C. Execution; 2) Statistical analysis: C. Review and Critique; 3) Manuscript: B. Review and Critique.
Dr. Bliem: 1) Research project: C. Execution; 2) Statistical analysis: C. Review and Critique; 3) Manuscript: B. Review and Critique.
Dr. Hallett: 1) Research project: A. Conception; 2) Statistical analysis: A. Design, C. Review and Critique; 3) Manuscript: B. Review and Critique.
FULL FINANCIAL DISCLOSURES OF ALL AUTHORS FOR THE PAST YEAR
Dr. Pirio Richardson
|
Stock Ownership in medically-related fields: None |
Intellectual Property Rights: None |
|
Consultancies: None |
Expert Testimony: None |
|
Advisory Boards: None |
Employment: University of New Mexico, New Mexico VA Healthcare System |
|
Partnerships: None |
Contracts: None |
|
Honoraria: None |
Royalties: None |
|
Grants: 8KL2TR000089 (NIH-NCRR) U54NS065701 (NIH/NINDS/ORDR) NS065701 (NIH/NINDS/ORDR) |
Other: None |
Dr. Beck
|
Stock Ownership in medically-related fields: None |
Intellectual Property Rights: None |
|
Consultancies: None |
Expert Testimony: None |
|
Advisory Boards: None |
Employment: University of Freiburg, Freiburg im Breisgau, Germany |
|
Partnerships: None |
Contracts: None |
|
Honoraria: None |
Royalties: None |
|
Grants: None |
Other: None |
Dr. Bliem
|
Stock Ownership in medically-related fields: None |
Intellectual Property Rights: None |
|
Consultancies: None |
Expert Testimony: None |
|
Advisory Boards: None |
Employment: European Patent Office |
|
Partnerships: None |
Contracts: None |
|
Honoraria: None |
Royalties: None |
|
Grants: None |
Other: None |
Dr. Hallett
|
Stock Ownership in medically-related fields: None |
Intellectual Property Rights: National Institutes of Health |
|
Consultancies: None |
Expert Testimony: None |
|
Advisory Boards: None |
Employment: National Institute of Neurological Diseases and Stroke |
|
Partnerships: None |
Contracts: None |
|
Honoraria: None |
Royalties: Cambridge University Press Oxford University Press Wiley-Blackwell Springer Lippincott Williams & Wilkins Elsevier |
|
Grants: None |
Other: Neurotoxin Institute BCN Peptides provided drug to NIH for a clinical trial for the treatment of blepharospasm. Manhattan Pharmaceuticals provided some funds to NIH for a clinical trial in essential tremor. |
Footnotes
The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Financial Disclosure/Conflict of Interest:
Dr. Pirio Richardson reports no disclosures.
Dr. Beck reports no disclosures.
Dr. Bliem reports no disclosures.
Dr. Hallett reports no disclosures.
References
- 1.Batla A, Stamelou M, Bhatia KP. Treatment of focal dystonia. Curr Treat Options Neurol. 2012;14(3):213–29. doi: 10.1007/s11940-012-0169-6. [DOI] [PubMed] [Google Scholar]
- 2.Rijntjes M, Dettmers C, Buchel C, et al. A blueprint for movement: functional and anatomical representations in the human motor system. J Neurosci. 1999;19(18):8043–8048. doi: 10.1523/JNEUROSCI.19-18-08043.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Delnooz CCS, Helmich RC, Medendorp WP, et al. Writer’s cramp: Increased dorsal premotor activity during intended writing. Hum Brain Mapp. 2013;34(3):613–25. doi: 10.1002/hbm.21464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Castrop F, Dresel C, Hennenlotter A, et al. Basal ganglia-premotor dysfunction during movement imagination in writer’s cramp. Mov Disord. 2012;27(11):1432–1439. doi: 10.1002/mds.24944. [DOI] [PubMed] [Google Scholar]
- 5.Veugen LC, Hoffland BS, Stegeman DF, et al. Inhibition of the dorsal premotor cortex does not repair surround inhibition in writer’s cramp patients. Exp Brain Res. 2013;225(1):85–92. doi: 10.1007/s00221-012-3350-y. [DOI] [PubMed] [Google Scholar]
- 6.Beck S, Houdayer EP, Pirio Richardson S, et al. The role of inhibition from the left dorsal premotor cortex in right-sided focal hand dystonia. Brain Stim. 2009;2(4):208–14. doi: 10.1016/j.brs.2009.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chouinard P, Paus T. The primary motor and premotor areas of the human cerebral cortex. Neuroscientist. 2006;12(2):143–152. doi: 10.1177/1073858405284255. [DOI] [PubMed] [Google Scholar]
- 8.Schluter ND, Rushworth MF, Passingham RE, et al. Temporary interference in human lateral premotor cortex suggests dominance for the selection of movements: a study using transcranial magnetic stimulation. Brain. 1998;121:785–799. doi: 10.1093/brain/121.5.785. [DOI] [PubMed] [Google Scholar]
- 9.Agresti A. Categorical data analysis. 2. New Jersey: John Wiley & Sons; 2002. pp. 228–230. [Google Scholar]
- 10.Hallett M. Neurophysiology of dystonia: the role of inhibition. Neurobiol Dis. 2011;42(2):177–184. doi: 10.1016/j.nbd.2010.08.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Huang YZ, Lu CS, Rothwell JC, et al. Modulation of the disturbed motor network in dystonia by multisession suppression of premotor cortex. PloS One. 7(10):e47574. doi: 10.1371/journal.pone.0047574. Epub 2012 Oct 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Tinazzi M, Fiorio M, Fiaschi A, et al. Sensory functions in dystonia: insights from behavioral studies. Mov Disord. 2009;24:1427–36. doi: 10.1002/mds.22490. [DOI] [PubMed] [Google Scholar]
- 13.Avanzino L, Martino D, Martino I, et al. Temporal expectation in focal hand dystonia. Brain. 2013;136(Pt 2):444–54. doi: 10.1093/brain/aws328. [DOI] [PubMed] [Google Scholar]
- 14.Bradley D, Whelan R, Walsh R, et al. Comparing endophenotypes in adult-onset primary torsion dystonia. Mov Disord. 2010;25:84–90. doi: 10.1002/mds.22889. [DOI] [PubMed] [Google Scholar]