Abstract
Previous research has documented bidirectional relationships between trauma exposure and posttraumatic stress (PTS), such that individuals who are exposed to more traumatic events are at increased risk of developing PTS, and more severe PTS is associated with more subsequent trauma exposure. However, the empirical literature is limited by a lack of longitudinal studies that include continuous measures of PTS, differentiate between assaultive (e.g., sexual assault, being help up or mugged) and non-assaultive (e.g., serious illness, natural disaster) trauma, and focus on urban contexts. The purpose of this study was to fill these gaps through testing three-wave cross-lagged panel models of exposure to assaultive and non-assaultive traumatic events and PTS among a large sample of urban-dwelling adults (N = 1360; 84.4% non-Hispanic Black). In the model including assaultive trauma, more Wave 2 assaultive events were associated with significantly higher Wave 3 PTS. In contrast, in the model including non-assaultive trauma, higher Wave 1 and Wave 2 PTS were associated with more non-assaultive events at Waves 2 and 3, respectively. Taken together, the findings suggest a cycle of adversity wherein urban residents who have experienced assaultive trauma are at risk of more severe PTS, which in turn increases risk for exposure to non-assaultive trauma. This cycle could be tested directly in future studies through models including both types of events. Additional research on the mechanisms that underlie the pathways between PTS and traumatic events could also have implications for policy and practice.
Keywords: Posttraumatic stress, trauma exposure, cross-lagged model, non-Hispanic Blacks, urban environment
Literature Review
Posttraumatic stress disorder (PTSD) is a common, debilitating mental disorder that develops in some persons following exposure to traumatic events and is characterized by traumatic intrusions, avoidance of traumatic reminders, and hyperarousal symptoms (APA, 2000). The lifetime prevalence of PTSD is 7.3 % in the general population and 9.1% among persons exposed to traumatic events (Roberts, Gilman, Breslau, Breslau, & Koenen, 2011). The prevalence of PTSD is even higher among those living in low socioeconomic urban areas (e.g., Breslau et al., 1998; Liebschutz et al., 2007), possibly due to increased exposure to assaultive violence (e.g., Breslau et al., 1998). For as many as 42% of individuals who develop PTSD, the disorder becomes chronic, with symptoms persisting years after exposure to the index trauma (e.g., Cougle, Resnick, & Kilpatrick, 2013). One possible explanation for chronic PTSD is that posttraumatic stress (PTS) symptoms heighten risk for further traumatic events that, in turn, perpetuate or exacerbate PTS over time. The current study explored this possibility by investigating bidirectional relationships between trauma exposure and posttraumatic stress among a large, predominantly non-Hispanic Black sample, living in urban Detroit.
Research to date has provided strong evidence for bidirectional relationships between trauma exposure and PTS. Supporting the pathway from trauma exposure to PTS, cross-sectional studies consistently have identified exposure to multiple traumatic events as a risk factor for PTSD (e.g., Schumm, Briggs-Phillips, & Hobfoll, 2006; Walsh et al., 2012). A substantial body of literature also suggests that individuals exposed to prior traumatic events are at greater risk of PTSD following a subsequent trauma (e.g., Brewin, Andrews & Valentine, 2000; Ozer, Best, Lipsey & Weiss, 2003). Stress sensitization, whereby an individual who is exposed to early stressors is more vulnerable to developing psychopathology when exposed to later stressors, is one potential theoretical explanation for this differential susceptibility to PTSD (e.g., McLaughlin, Conron, Koenen, & Gilman, 2010). For example, it has been postulated that exposure to stressors, particularly early in life, may alter the stress response system such that these systems are primed to respond in ways that increase risk for PTSD after exposure to later stressors (Yehuda et al., 2010).
There is also evidence that more severe PTS predicts exposure to subsequent traumatic events, particularly those characterized by assaultive violence, such as sexual or physical assault. For example, PTS symptoms have been found to prospectively predict interpersonal revictimization among women with a history of intimate partner violence (IPV) (e.g., Cougle, Resnick, & Kilpatrick, 2009). An additional prospective study of college women found that sexual revictimization was more likely among participants with higher PTS (Sandberg, Matorin, & Lynn, 1999).
A substantial body of literature on revictimization has provided insight into the possible mechanisms underlying the pathway from PTS to subsequent trauma exposure. For example, hyperarousal symptoms are theorized to desensitize trauma survivors to an internal sense of threat, leading to impairment in the ability to distinguish between true and false threats in the environment (e.g., Messman-Moore & Long, 2003). Supporting this notion, cross-sectional studies have found PTS symptoms to mediate associations between child abuse and adult rape (Messman-Moore, Ward, & Brown, 2009), with hyperarousal symptoms specifically accounting for linkages (e.g., Risser, Hetzel-Riggin, Thomsen, & McCanne, 2006). Hyperarousal symptoms are also thought to trigger avoidance, that is, voluntary or involuntary attempts to self-regulate negative affect that can be observable (e.g., substance use, sexual risk-taking) or private (e.g., distraction, numbing) in nature (Marx, Heidt, & Gold, 2005). Although such efforts could temporarily relieve hyperarousal symptoms, they further impede threat detection abilities and thereby augment revictimization risk. Empirical findings documenting positive associations between emotion dysregulation and impaired risk detection (Walsh, DiLillo, & Messman-Moore, 2012), and as well as between substance abuse and PTS (e.g., Kilpatrick et al., 2003), lend support for this proposition. Reexperiencing symptoms (e.g., intrusive thoughts) have also been posited to undermine threat detection and adaptive coping abilities (Messman-Moore & Long, 2003). Along these lines, a recent study found that, among victims of IPV, reexperiencing symptoms predicted revictimization, an effect that was partially mediated by victims’ own psychological IPV behavior (Kujipers, van der Knapp, & Winkel, 2012).
Although studies to date have provided ample evidence for bidirectional relationships between trauma exposure and PTS, the extant research is limited in at least five ways. First, the majority of studies have not tested the PTS to traumatic events and traumatic events to PTS pathways simultaneously, making it unclear whether they operate together within the same sample and to what effect. Second, longitudinal data is needed to explore the temporal dynamics between PTS and trauma exposure. To our knowledge, no studies to date have drawn on longitudinal data to test a cross-lagged model of trauma exposure and PTS.
Third, with few exceptions (e.g., Gabert-Quillen et al., 2012), the majority of studies on this topic have investigated PTSD dichotomously, focusing on the presence or absence of the disorder, rather than exploring associations between trauma exposure and a continuous measure of PTS. This is a significant limitation given that continuous measures allow for optimal exploration of levels of PTS over time. Among participants who consistently do or do not meet diagnostic criteria for PTSD, variation in PTS could have important implications for adaptive functioning (e.g., Pietrzak, Goldstein, Southwick, & Grant, 2011). The literature on revictimization also suggests the importance of examining symptom clusters within PTSD separately, as they could be differentially associated with subsequent trauma exposure.
Fourth, few studies have differentiated between assaultive and non-assaultive trauma. In the current study, we define assaultive trauma as actual or threatened violations of bodily integrity that are interpersonal in nature, including rape, physical assault, or being held captive, tortured or kidnapped. We include both direct experiences, wherein the person was a victim of or witness to the assault, and indirect experiences, wherein the person’s close friend or family member was the victim, as both could theoretically affect the person’s sense of safety and trust in his or her environment. In contrast, we define non-assaultive trauma as actual or threatened violations of bodily integrity that are not inherently interpersonal in nature, including motor vehicle accidents, natural disasters, and life-threatening illnesses. Again, we included both direct and indirect experiences of such events in our definition.
Although PTS has been more consistently associated with assaultive trauma (e.g., Cougle et al., 2009; Krause et al., 2006), at least one prospective study found that individuals with chronic PTSD were more likely to experience both assaultive and non-assaultive traumatic events when re-assessed two years later (Cougle, Resnick, & Kilpatrick, 2013). Assaultive and non-assaultive trauma could also differ in their impact on PTS. For example, a study of women in an urban environment found higher PTS severity and longer symptom duration for women who had experienced assaultive trauma, versus non-assaultive, trauma (Gill, Page, Sharps, & Campbell, 2008).
Lastly, few studies on this topic have included non-Hispanic Black residents from urban environments. This is a significant limitation given the increased risk of assaultive violence among this population (e.g., Breslau et al., 1998), which could perhaps yield stronger associations between trauma exposure and PTS. Conversely, linkages between trauma and PTS could be attenuated in an urban context because pervasive exposure to violence may initiate cognitive processes associated with normalization of violent stimuli that in turn may operate to mitigate the negative psychological effects of violence (Ng-Mak, Salzinger, Feldman, & Stueve, 2002).
The Current Study
In the current study, we addressed these limitations by 1) testing longitudinal cross-lagged models of PTS and trauma exposure; 2) including a continuous measure of PTS; 3) running separate models for assaultive and non-assaultive trauma; and 4) drawing upon a sample of predominantly non-Hispanic Black residents of urban Detroit. Based on the literature to date, we hypothesized significant cross-lagged paths such that individuals who reported exposure to more traumatic events at one wave would report higher PTS at subsequent waves, and individuals with higher PTS at one wave would report exposure to more traumatic events at subsequent waves. No a priori hypotheses were made about whether the magnitude of these pathways would vary between models with assaultive and non-assaultive traumatic events given the lack of available data on this topic.
Methods
Participants and Procedure
Data were drawn from the Detroit Neighborhood Health Study (DNHS), a longitudinal study of predominantly non-Hispanic Black adults (18 years or older) living in Detroit, Michigan. Baseline telephone surveys were conducted by contacting households within the city limits of Detroit and randomly selecting one adult from each household to participate. Participants were selected using a dual-frame probability design, through use of telephone numbers obtained from the United States Postal Service Sequence Files, as well as a list-assisted random-digit-dial frame. Individuals without listed numbers or with only a cell phone were recruited by mail. Additional detail on the baseline sampling methodology of DNHS can be found elsewhere (e.g., Uddin et al., 2010). Wave 1 (W1) of the study was conducted between 2008 and 2009, and a total of 1547 participants completed the survey, with an overall response rate among eligible persons of 53.0%. Approximately a year after W1, participants were re-contacted for the Wave 2 (W2) assessment. A total of 1054 participants completed the W2 survey (68.1% retention rate). Wave 3 (W3) occurred approximately a year after W2, and 965 participants from the baseline sample participated (62.5% retention rate). A total of 847 participants completed all three waves, yielding an overall retention rate of 54.8%. At each wave, participants completed a structured telephone survey, which lasted an average of 40 minutes and included a measure of PTS and an inventory of traumatic events. Informed consent was obtained at the beginning of each survey, and participants were offered $25 for their participation in each interview. The Institutional Review Board of the University of Michigan approved the study.
Because we were interested in the impact of trauma exposure over time, we selected participants who reported at least one lifetime traumatic event and therefore completed the inventory of PTS at W1 (n = 1360). The majority of the participants (84.4%) identified as non-Hispanic Black, 9.9% as non-Hispanic White, and 1.8% as Hispanic; 57.4% were female. On average, participants were 50.60 years old (SD = 16.57; range: 18–92) at W1. At W1, 25.8% were married, whereas 24.2% were separated or divorced, 11.9% widowed, and 38.1% single and never married. Participants also reported on their income and employment status at W1: 28.2% reported an income under $15,000, and 56.9% were unemployed. The number of years since participants’ “worst” trauma ranged from 0 to 89 (M = 14.29, SD =13.75). There were no significant differences in W1 PTS or trauma exposure by years since “worst” trauma.
Measures
Traumatic Events
At W1, participants completed a 20-item trauma inventory of lifetime traumatic events (Breslau et al., 1998). At W2 and W3, participants completed the inventory in reference to the time since the last interview. From the 20-item inventory, we selected eight items indicative of assaultive trauma and seven of non-assaultive trauma, as defined in the current study (Table 1). Five items were excluded from this categorization because they were not clearly assaultive or non-assaultive. First, we excluded “experienced combat or exposure to a war zone in the military or as a civilian” because such experiences could entail both assaultive and non-assaultive trauma and the participants did not detail their specific war-related experiences. Second, the item “unexpectedly discovered a dead body” was excluded because it did not specify whether the death was due to assaultive violence (e.g., murder) or non-assaultive trauma (e.g., an accident). The same rationale was behind our decision to exclude two additional items: “witnessed someone being killed or seriously injured” and “the sudden, unexpected death of someone close.” Finally, an item wherein participants indicated whether they had experienced another traumatic event not on the inventory was excluded because participants endorsing this item were not asked to specify the nature of the event. The total number of assaultive events and non-assaultive events endorsed at each wave were included as count variables
Table 1.
Number and Percentage of Participants Reporting Each Traumatic Event (N = 1360)
| Wave 1 | Wave 2 | Wave 3 | |
|---|---|---|---|
| Assaultive Trauma | |||
| Been raped | 216 (15.9%) | 32 (3.4%) | 24 (2.8%) |
| Experienced another kind of sexual assault or unwanted sexual contact as a result of force, threat of harm, or manipulation | 293 (21.5%) | 14 (1.5%) | 15 (1.8%) |
| Been shot or stabbed | 217 (16.0%) | 19 (2.0%) | 16 (1.9%) |
| Been mugged, held up, or threatened with a weapon | 519 (38.3%) | 52 (5.5%) | 39 (4.6%) |
| Been held captive, tortured or kidnapped | 429 (31.6%) | 50 (5.3%) | 46 (5.4%) |
| Been badly beaten up | 105 (7.7%) | 22 (2.3%) | 24 (2.8%) |
| Learned that a close friend or relative was raped or sexually assaulted | 212 (15.7%) | 11 (1.2%) | 12 (1.4%) |
| Learned that a close friend or relative was seriously physically attacked | 177 (13.0%) | 2 (0.2%) | 1 (0.1%) |
| Any Assaultive Trauma | 983 (72.3%) | 138 (14.7%) | 129 (15.1%) |
| Non Assaultive Trauma | |||
| Been in a serious car or motor vehicle crash | 172 (12.7%) | 5 (0.5%) | 7 (0.8%) |
| Experienced any other kind of serious accident or injury | 410 (30.3%) | 43 (4.6%) | 50 (5.9%) |
| Experienced a natural disaster (e.g., fire, flood, earthquake) in which you were hurt or your property was damaged | 162 (12.0%) | 2 (0.2%) | 3 (0.4%) |
| Been diagnosed with a life-threatening illness or had a serious operation | 1091 (80.4%) | 357 (38.1%) | 328 (38.5%) |
| Had a child of yours diagnosed as having a life- threatening illness | 386 (28.5%) | 133 (14.1%) | 133 (15.7%) |
| Learned that a close friend or relative was seriously injured in a motor vehicle crash | 76 (5.6%) | 1 (0.1%) | 0 (0.0%) |
| Learned that a close friend or relative was seriously injured in any other accident | 532 (39.2%) | 31 (3.3%) | 30 (3.5%) |
| Any Non-Assaultive Trauma | 1091 (80.2%) | 194 (21.7%) | 191 (22.3%) |
Note. Values based on raw data.
Posttraumatic stress
PTS was assessed using an interview version of the PTSD Checklist-Civilian Version (PCL-C; Weathers & Ford, 1996). The PCL-C includes 17 items, representing criteria B (re-experiencing: five items, e.g., “repeated, disturbing thoughts or memories about the event”), C (avoidance: two items, e.g., ““avoiding activities or situations because they reminded you of the stressful experience”; and emotional numbing: five items, e.g., “loss of interest in things you used to enjoy”), and D (hyperarousal: five items, e.g., “trouble falling and staying asleep”) from the Diagnostic and Statistical Manual of Mental Disorders (4th ed.; DSM-IV, American Psychological Association [APA], 1994). At each assessment, participants asked to respond based on the event reported as the “worst” at W1 and, at W2 and W3, were reminded of the which event they had reported. Participants indicated the degree to which they had been bothered by each symptom as a result of the event from 1 = Not at all to 5 = Extremely. Responses are typically summed to yield a symptom severity score, and scores above 44 are indicative of probable PTSD in normative samples (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996). Whereas the items on the PCL-C are typically asked in reference to the past month, the timeframe was modified for the current study. At W1, participants were asked the extent they were ever bothered by each symptom, and at W2 and W3, the extent they were bothered since the prior interview. The PCL-C has previously been shown to have excellent internal consistency and substantial agreement with PTSD diagnosis and symptom ratings (e.g., Blanchard et al., 1996; Weathers, Litz, Herman, Huska, & Keane, 1993). Clinical in-person interviews with a random subsample of 51 DNHS participants generally supported the reliability and validity of PTSD diagnoses based on meeting criteria on the reexperiencing, avoidance/numbing, and hyperarousal subscales of the PCL-C, as well as the additional criteria (via items assessing feelings of helplessness and hopelessness during the event, duration of symptoms, and significant distress and functional impairment), relative to the gold-standard Clinician-Administered PTSD Scale for DSM-IV (CAPS) (for additional details, see Uddin et al., 2010). Specifically, the PCL-C had a specificity of 0.97, positive predictive value of 0.80, negative predictive value of 0.72, and an area under the receiver-operating characteristic (ROC) curve of 0.76. Notably, however, the sensitivity of the PCL-C was only 0.24, implying that the prevalence of PTSD based on the PCL-C was conservative in the study. The internal consistency of the PCL-C in this study was α= .93 at W1, .94 at W2, and .97 at W3.
Data Analysis
Descriptive statistics for all study variables, as well as attrition and missing value analysis, were conducted in SPSS 20.0 (IBM Corp., 2011). All subsequent analyses were conducted in Mplus 7.1 (Muthén & Muthén, 1998–2012). Maximum likelihood (ML) estimation with robust standard errors, via the MLR estimator, was used to handle missing data and non-normality. Longitudinal measurement models for PTS were tested, and goodness of fit was evaluated using the Root Mean Square Error of Approximation (RMSEA) and its 90% confidence interval (CI), and the Comparative Fit Index (CFI). The following criteria were used to determine acceptable model fit (Hu & Bentler, 1999): RMSEA and its 90% CI upper limit close to or below 0.06, and CFI close to or above .95. Comparative fit of nested measurement models was evaluated with chi-square difference tests (χ2diff), using scaling factors to account for the use of MLR (Santorra & Bentler, 2001), and change in CFI, with changes ≥ .01 indicating worse fit (Cheung & Rensvold, 2002). Next, the hypothesized cross-lagged panel models between trauma exposure and PTS were conducted, with separate models for assaultive events and non-assaultive events. Trauma counts (i.e., the number of events on the trauma inventory endorsed) were modeled as single indicators of standard-normal latent variables with means set at 0 and variances set at 1, which permitted use of MLR (Kline, 2005). Because count variables were used, RMSEA and CFI were unavailable as indicators of model fit, and chi-square tests were only available for the count outcomes. Therefore, these values are not reported in the results. The cross-lagged models were replicated for each PCL-C symptom cluster summary score. In the symptom cluster models, each summary score was included as an observed variable; that is, individual items for each cluster were not loaded onto a latent symptom cluster variable. We note here that analyzing each cluster separately contradicts our use of latent posttraumatic stress variables in the prior models. Specifically, latent variable models carry the assumption that each indicator is interchangeable, with each being a reflection of the latent variable and measurement error (c.f., Jarvis, Mackenzie, & Podsakoff, 2003). This contrasts with our approach to looking at each indicator separately, which assumes that they might relate differently to other variables in the model. Despite this contradiction, we felt that analyses of different symptom clusters could provide important insights into how each relates to assaultive and non-assaultive trauma exposure. Additionally, these analyses were motivated by findings demonstrating differential relations between the symptom clusters and trauma exposure (e.g., Kujipers et al., 2012; Risser et al., 2006).
Results
Descriptive Analyses
Table 1 includes the frequency of each of the 15 traumatic events at each wave. Means and standard deviations of the PCL-C total severity score, PCL-C symptom cluster subscale scores, and counts of assaultive and non-assaultive events endorsed at each wave are provided in Table 2. Based on the symptom severity score cut-off of 44, 20.9% had probable PTSD at W1, 15.7% at W2, and 14.7% at W3.
Table 2.
Descriptive Data for Variables Included in Analyses (N = 1360)
| Wave 1
|
Wave 2
|
Wave 3
|
||||
|---|---|---|---|---|---|---|
| M (SD) | Range | M (SD) | Range | M (SD) | Range | |
| PTS Symptom Cluster Scores | ||||||
| Reexperiencing | 2.22 (1.05) | 1.0 – 5.0 | 2.01 (1.01) | 1.0 – 5.0 | 1.98 (1.02) | 1.0 – 5.0 |
| Avoidance | 2.10 (1.26) | 1.0 – 5.0 | 1.93 (1.14) | 1.0 – 5.0 | 1.88 (1.10) | 1.0 – 5.0 |
| Numbing | 1.75 (.92) | 1.0 – 5.0 | 1.59 (.85) | 1.0 – 4.8 | 1.60 (.81) | 1.0 – 5.0 |
| Hyperarousal | 2.00 (1.01) | 1.0 – 5.0 | 1.87 (.95) | 1.0 – 5.0 | 1.85 (.95) | 1.0 – 5.0 |
| Counts of Traumatic Events | ||||||
| Assaultive events | 1.81 (1.69) | 0 – 8 | .21 (.59) | 0 – 5 | .21 (.55) | 0 – 4 |
| Non-assaultive events | 1.86 (1.49) | 0 – 7 | .28 (.61) | 0 – 5 | .29 (.62) | 0 – 4 |
Note. Values based on raw data.
Bonferroni-corrected independent-samples t-tests and chi-square tests detected no significant differences in demographic characteristics between the 1360 participants who reported at least one lifetime trauma at W1 and the 187 who did not meet this inclusion criterion. For the 1360 included participants, the overall rate of missing data at the item level was 14.7%. Average missing rates for 20 trauma inventory items at each wave were as follows: 0.2% at W1, 30.8% at W2, and 37.2% at W3. For the PCL-C items, average missing rates at each wave were 0.9% at W1, 61.2% at W2, and 65.6% at W3. For the 1052 participants who provided any W2 data, average rates of missingness for W2 trauma and PCL-C items were 0.04% and 45.0%, respectively. For the 965 participants who provided any W3 data, average rates of missingness for W3 trauma and W3 PCL-C items were 0.2% and 46.6%, respectively. Given the high rates of missingness for W2 and W3 PCL-C, we ran additional independent-samples t-tests and Mann Whitney tests to examine whether participants missing PCL-C items at each time point differed in their levels PCL-C of and W1 total counts of traumatic events, respectively. We found that participants missing W2 PCL-C items had significantly lower W1 PCL-C (t(894.47) = 4.78, p < .001, equal variances not assumed) and reported significantly fewer W1 traumatic events (Z = −5.72, p < .001). The same was true for participants missing W3 PCL-C items: t(820) = 3.62, p < .001 and Z = −5.92, p < .001.
Posttraumatic Stress: Longitudinal Measurement Model
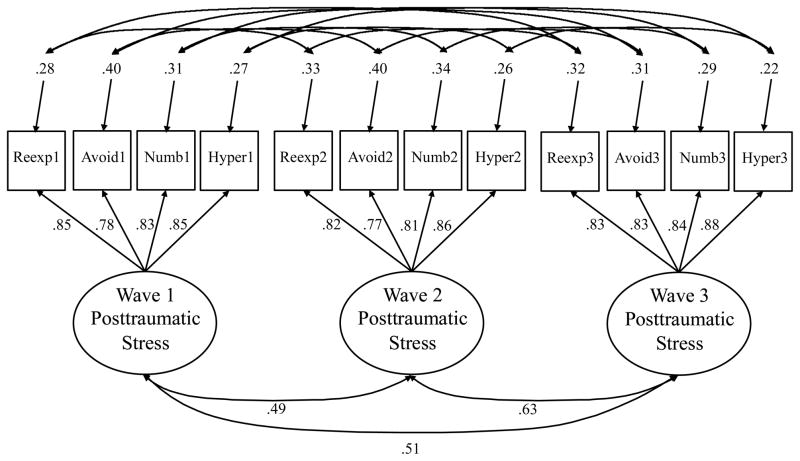
Based on previous research suggesting a four-factor structure of PTSD (e.g., King, Leskin, King, & Weathers, 1998), mean scores for items on the re-experiencing, avoidance, emotional numbing, and hyperarousal subscales were included as indicators of a PTSD latent variable in the measurement model (Figure 1). As shown, correlated errors between assessments of each PCL-C subscale at each wave were included. A baseline model that allowed for free estimation of factor loadings and intercepts, and that constrained the variance of the PTSD latent variable at each wave at 1.0, had acceptable fit with the data, χ2(39) = 141.43, p < .001, RMSEA = .04 (90% CI [.04, .05]), CFI = .98. A second model constrained factor loadings to equality at each wave and the variance of the PTSD latent variable at Wave 1 only at 1.0, and allowed for free estimation of the variances of the PTSD latent variable at Waves 2 and 3. This model also had acceptable fit with the data, χ2(45) = 147.36, p < .001, RMSEA = .04 (90% CI [.03, .05]), CFI = .98. The second model did not produce a statistically significant reduction in model fit, χ2diff (6) = 5.75, p = .45, and the change in CFI was < .01. Therefore, we concluded that the factor loadings were time invariant. The standardized parameter estimates of this solution, which was used in all subsequent models, are presented in Figure 1 (all factor loading and factor correlation ps < .001).
Figure 1.
Final longitudinal measurement model of posttraumatic stress symptoms. Standardized parameter estimates provided (all ps < .001). For clarity, correlated error estimates are not presented (range = .03–.32). Reexp = Reexperiencing; Avoid = Avoidance; Numb = Numbing; Hyper = Hyperarousal.
Cross-Lagged Models
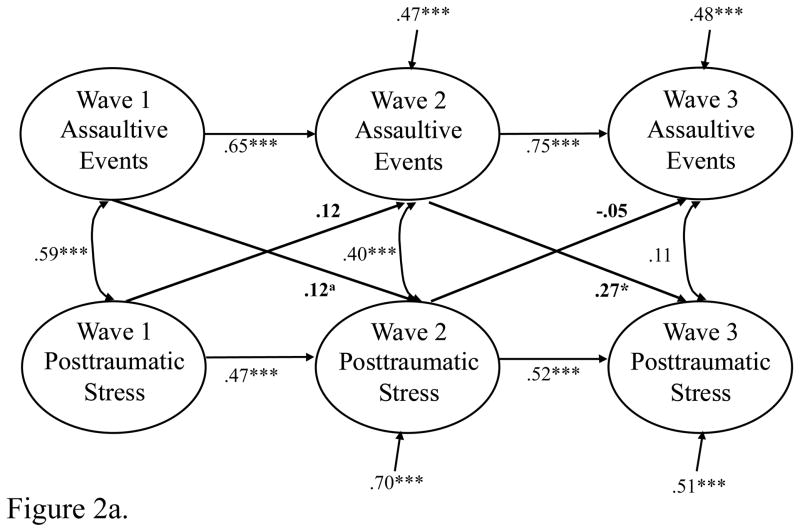
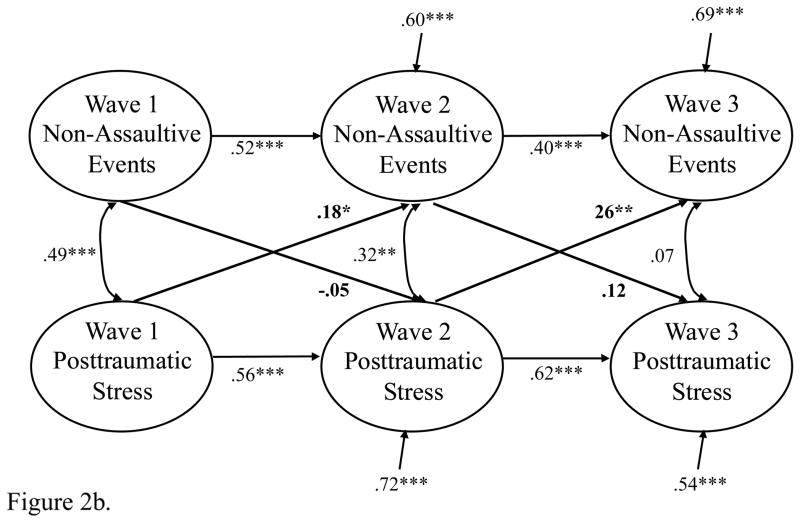
The results of the cross-lagged models are shown in Figures 2a–2b. Standardized coefficients for the cross-lagged paths, as well as standard errors and 95% confidence intervals, are also listed in Table 3 as rough indicators of effect size. For the assaultive traumatic events model, the path from W1 assaultive events to W2 PTS was marginally significant, whereas the path from W2 assaultive events to W3 PTS was statistically significant. In both cases, exposure to more assaultive events at one wave was associated with higher PTS at the subsequent wave. Neither of the paths from PTS to subsequent assaultive events reached statistical significance. For the non-assaultive traumatic events model, neither of the paths from non-assaultive events to PTS was significant. Both paths from PTS to subsequent non-assaultive events were significant, however, such that higher PTS at one wave was associated with significantly more non-assaultive events reported at the subsequent wave. In Figures 2a–2b standardized disturbances of endogenous variables, are provided as indicators of effect size. The percent of variance explained ranged from 28% to 53%. Notably, all of the standardized disturbances were statistically significant, meaning that there was significant residual variance in each endogenous variable.
Figure 2.
Figure 2a. Results of model including assaultive traumatic events. Cross-lagged paths and coefficients are in boldface for clarity. ap < .10, *p < .05, ***p < .001.
Figure 2b. Results of model including non-assaultive events. Cross-lagged paths and coefficients are in boldface for clarity. *p < .05, **p < .01, ***p < .001.
Table 3.
Coefficients for Cross-Lagged Paths for Models Predicting Total Posttraumatic Stress and Symptom Clusters (N= 1360)
| Posttraumatic Stress Est. (SE) [95% CI] |
Reexperiencing Est. (SE) [95% CI] |
Avoidance Est. (SE) [95% CI] |
Numbing Est. (SE) [95% CI] |
Hyperarousal Est. (SE) [95% CI] |
|
|---|---|---|---|---|---|
| Assaultive Trauma | |||||
| W1 Trauma → W2 Symptoms | .12 (.07) [−.02, .27] a | .15 (.07) [.02, .29] * | .19 (.07) [.05, .32] ** | .11 (.06) [< .01, .22] * | .20 (.06) [.07, .32] ** |
| W2 Trauma → W3 Symptoms | .27 (.11) [.06, .47] * | .31 (.11) [.10, .52] * | .39 (.09) [.22, .55] *** | .31 (.08) [.16, .45] *** | .30 (.08) [.15, .45] *** |
| W1 Symptoms → W2 Trauma | .12 (.09) [−.06, .30] | .10 (.09) [−.09, .28] | .12 (.07) [−.02, .25] a | .14 (.07) [< .01, .28] * | .07 (.07) [−.07, .22] |
| W2 Symptoms → W3 Trauma | −.05 (.10) [−.24, .14] | −.07 (.09) [−.25, .11] | −.02 (.10) [−.21, .17] | .03 (.08) [−.13, .18] | −.05 (.09) [−.22, 12] |
| Non-Assaultive Trauma | |||||
| W1 Trauma → W2 Symptoms | −.05 (.08) [−.21, .11] | −.02 (.08) [−.18, .15] | .03 (.03) [−.02, .08] | .04 (.06) [−.09, .16] | −.01 (.08) [−.17, .15] |
| W2 Trauma → W3 Symptoms | .12 (.11) [−.09, .32] | .20 (.11) [−.01, .41] a | .30 (.08) [.14, .46] *** | .23 (.09) [.06, .41] ** | .16 (.09) [−.02, .34] |
| W1 Symptoms → W2 Trauma | .18 (.07) [.04, .32] * | .22 (.08) [.08, .37] ** | .18 (.06) [.06, .29] ** | .18 (.06) [.06, .31] ** | .19 (.07) [.06, .32] ** |
| W2 Symptoms → W3 Trauma | .26 (.07) [.11, .40] ** | .21 (.07) [.07, .35] ** | .22 (.07) [.08, .36] ** | .22 (.07) [.09, .36] *** | .24 (.08) [.09, .38] *** |
Note. Values in boldface represent different patterns of significance in symptom cluster analyses, as compared to the posttraumatic stress latent variable analyses. Values in italics represent different magnitude of the coefficients, as compared to the posttraumatic stress latent variable analyses.
p < .10,
p < .05,
p < .01,
p < .001.
We could not directly assess whether observed differences in the cross-lagged paths between the assaultive and non-assaultive models were statistically significant because the two types of traumatic events were not included in the same model. To provide some insight into the magnitude of observed differences, we inspected the 95% CIs of the paths in the two models. For each cross-lagged path, the 95% CIs overlapped between the two models, suggesting – but not explicitly demonstrating – that the observed differences were not statistically significant. We note here that, in supplementary analyses, we tried to run a model including both assaultive and non-assaultive events. However, this model would not run with our data, despite the use of several strategies to facilitate model convergence (e.g., Montecarlo integration, increasing the number of iterations; Muthén & Muthén, 1998–2012).
The cross-lagged models were replicated with each symptom cluster summary score. Standardized coefficients, standard errors, and 95% CIs for the cross-lagged paths in these models are listed in Table 3. As shown, the patterns of statistical significance were generally consistent with the PTS models, although there were some exceptions (listed in boldface): 1) the paths from W1 assaultive events to all symptom clusters at W2 were statistically significant; 2) the paths from W1 avoidance and emotional numbing to W2 assaultive events were statistically significant; and 3) the paths from W2 non-assaultive events to W3 avoidance and emotional numbing were statistically significant. Despite these exceptions, we noted that the direction of all but three paths (listed in italics) was consistent across the four symptom clusters, that any differences in the magnitude between the paths were small, and that all 95% confidence intervals were overlapping. Because the different symptom clusters were not included in a single model, we could not determine whether any observed differences were statistically significant.
Supplementary Analysis: Indirect Paths from W1 Trauma to W2 PTS
In reviewing the results of the cross-lagged models, we noted that none of the direct paths from W1 traumatic events to W2 PTS reached statistical significance (although this pathway was significant in the assaultive events model for each symptom cluster). We speculated that this could be due in part to the temporal nature of the data. That is, the W1 assessment of traumatic events included lifetime events, some of which might have occurred well before participants enrolled in the study. Such events might not be directly contributing to W2 PTS, but instead, might be indirectly influencing W2 PTS through either W1 PTS or W2 traumatic events. To test this possibility, we ran models testing these two indirect pathways. In these models, the covariance between W1 traumatic events and W1 PTS was converted to a directional path from the former to the latter. The same was done for the path between W2 traumatic events and W2 PTS. The indirect path through W1 PTS was computed as the product of a) the direct path from W1 trauma to W1 PTS and b) the direct path from W1 PTS to W2 PTS. The indirect path through W2 trauma was computed as the product of a) the direct path from W1 trauma to W2 trauma and b) the direct path from W2 trauma to W2 PTS (Muthén, 2011). Additionally, we computed total effects from W1 trauma to W2 PTS as the sum of the direct effect and two indirect effects. Table 4 lists the unstandardized coefficients, standard errors, and 95% confidence intervals for the direct, indirect, and total effects. Notably, the two indirect paths were statistically significant in the assaultive events and non-assaultive events models.
Table 4.
Results of Models Testing Indirect Effects from Wave 1 Trauma Exposure to Wave 2 Posttraumatic Stress. (N = 1360)
| Assaultive Traumatic Events Estimate (SE) [95% CI] |
Non-Assaultive Traumatic Events Estimate (SE) [95% CI] |
|
|---|---|---|
| Direct Effect | −.22 (.14) [−.49, .05] | −.24 (.12) [−.47, −.01] * |
| Indirect Effect 1: Trauma 1 → PTS1 → PTS2 | .27 (.05) [.17, .36] *** | .25 (.04) [.17, .32] *** |
| Indirect Effect 2: Trauma 1 → Trauma 2 → PTS2 | .36 (.11) [.13, .58] ** | .18 (.07) [.04, .32] * |
| Total Effect | .40 (.07) [.26, .55] *** | .19 (.08) [.05, .34] * |
Note. Each indirect effect was computed as product of the two direct pathways within it. Each total effect was computed as the sum of the direct effect and two indirect effects. Unstandardized coefficients are presented.
p < .05,
p < .01,
p < .001.
Discussion
The purpose of this study was to explore longitudinal and bidirectional relationships between counts of assaultive and non-assaultive traumatic events and a continuous measure of PTS among a sample of primarily non-Hispanic Black adults living in urban Detroit. The results of cross-lagged panel models suggested that exposure to assaultive events has a long-term influence on PTS symptomatology. Exposure to more lifetime assaultive traumatic events, reported at W1, was marginally associated with higher W2 PTS. Exposure to more assaultive events between W1 and W2, reported at W2, was significantly associated with higher PTS at W3. Higher PTS at one wave, in turn, was associated with exposure to more non-assaultive traumatic events at the subsequent wave. These findings suggest a cycle of adversity in which urban residents who have been exposed to assaultive trauma are at increased risk of more severe and chronic PTS symptoms, which in turn increase risk for exposure to non-assaultive traumatic events.
It is important to note, however, that this cycle of adversity was not directly examined in the current study. A model that included both assaultive and non-assaultive events modeled as count variables did not run with our data, despite the use of several strategies to facilitate model convergence. Therefore, we were unable to assess indirect paths from assaultive to non-assaultive events through PTS. We were also unable to determine whether the patterns of statistical significance in the cross-lagged paths held after controlling for within-wave covariances between assaultive and non-assaultive events, which at the bivariate level ranged from .54 to .93. Finally, we were unable to compare whether observed differences in the cross-lagged paths between the models were statistically significant. We noted, however, that the 95% confidence intervals for respective cross-lagged coefficients overlapped between the two models. Although this observation suggests that the pathways did not differ between the assaultive and non-assaultive models, it is not a direct test of statistical significance and we believe that the differences in the magnitude of the paths are still noteworthy.
We replicated the analysis for all PTS symptoms with separate analyses for the four PTSD symptom clusters and noted some points of divergence. In the assaultive trauma models, more W1 assaultive events were associated with significantly higher levels of each symptom cluster at W2. Additionally, W1 emotional numbing was significantly associated with exposure to more W2 assaultive events, which is consistent with previous findings linking emotion dysregulation and impaired risk detection (e.g., Walsh et al., 2012). In the non-assaultive trauma models, more W2 non-assaultive events were significantly associated with higher levels of avoidance and emotional numbing at W3. Again, because these models were not nested, we could not directly test for whether observed differences were statistically significant. We noted that the magnitude of differences among the coefficients was small, all respective 95% confidence intervals were overlapping, and paths were consistently in the same direction. Nonetheless, the findings provided some evidence of differential relationships between the symptom clusters and trauma exposure. Further exploration of these differences, as well as the mechanisms underlying the cross-lagged paths for each symptom cluster, would be interesting directions for future study.
In interpreting the results, we noted that in no case were lifetime traumatic events significantly associated with W2 PTS, although this path was marginally significant in the assaultive events model. Because we were interested in the long-term influence of lifetime trauma on PTS, we ran supplementary analysis assessing indirect pathways from lifetime trauma to W2 PTS through W1 PTS and W2 traumatic events. Both indirect pathways were statistically significance in the assaultive and non-assaultive events models. These results suggest that exposure to lifetime traumatic events – both assaultive and non-assaultive – exert a long-term influence on PTS by increasing risk for more proximal PTS and exposure to additional trauma.
The results of the study contribute to the literature in three ways. First, the longitudinal design of the study allowed for exploration of bidirectional pathways both prospectively and simultaneously. By modeling the pathways prospectively, we were able to provide stronger evidence for the directionality of the relationships (i.e., that PTS leads to trauma exposure, and vice versa) than previous cross-sectional studies. By testing both pathways simultaneously through cross-lagged models, we were able to investigate the magnitude of each pathway, while controlling for the other pathway, again strengthening the results. Additionally, the inclusion of a continuous measure of PTS and counts of traumatic events, rather than dichotomous variables, allowed for a more fine-tuned investigation of how levels of one construct related to levels of the other over time. The study design overall provided more definitive evidence for bidirectional pathways between PTS and trauma exposure, and the results of the study are consistent with prior research documenting clear associations between levels of trauma exposure and PTS (e.g., Breslau, Chilcoat, Kessler, & Davis, 1999), as well as studies showing that PTS increases the likelihood of future trauma exposure (e.g., Cougle et al., 2009).
Second, the inventory of trauma exposure allowed for exploration of whether the magnitude of the cross-lagged paths varied by whether the traumatic events were assaultive (e.g., rape, being mugged or held up) or non-assaultive (e.g., serious illness, natural disaster). This is in contrast to the majority of previous studies, which have not differentiated between assaultive and non-assaultive trauma. Although we could not explicitly test whether observed differences reached statistical significance, the results provided some evidence that assaultive events are more strongly associated with subsequent PTS than non-assaultive events, which is consistent with previous findings (Breslau et al., 1998). The results also suggest that PTS symptoms might lead to more non-assaultive, versus assaultive, traumatic events. These findings are inconsistent with previous research and theory suggesting that PTS might render individuals more vulnerable to assaultive events, particularly those that are interpersonal in nature and over which an individual may exert more control.
Third, the study is focused on a sample of predominantly non-Hispanic Black adults living in an urban context, which is in contrast to the majority of previous studies that have investigated relationships between PTS and trauma exposure and is of particular importance given the high risk of assaultive violence among this population. Even within samples at increased risk of victimization and PTS, there is heterogeneity in exposure and psychological responses. Future studies that delve into the factors that render individuals within these groups vulnerable would therefore be of value.
Implications
The evidence for bidirectional paths between trauma exposure and PTS here underscores the need for greater attention to the interplay between these constructs in shaping longitudinal patterns of psychological symptoms. Further longitudinal studies could more explicitly test the cycle of adversity suggested by the results through testing models that include both assaultive and non-assaultive events and indirect pathways from the former to the latter through PTS. Future studies that explore the mechanisms underlying the paths between trauma and PTS would also be significant contributions to the literature. Investigations that include constructs that have been proposed as contributing to revictimization, including emotion dysregulation, impaired threat detection, and risk behavior, would be of particular value (e.g., Messman-Moore & Long, 2003; Marx et al., 2005). Such studies could perhaps provide more information on whether the different PTS symptom clusters differentially relate to trauma exposure. Studies that gather more detailed information regarding traumatic events, for example the extent to which events are within or outside of individual control, would shed additional light on these pathways. Further studies could also explore moderators; for example, perhaps the association between traumatic events and PTS is weaker for individuals with higher social support and community involvement, or who are involved in treatment.
Further research on factors that mediate and moderate relationship between PTS and trauma exposure would inform policy and clinical interventions, for example by demonstrating individual and community capacities that buffer against trauma exposure and prevent revictimization. In the absence of such findings, the results of the current findings merely provide support for existing empirically supported interventions to reduce PTS (e.g., Ponniah & Hollan, 2009), and trauma exposure in urban contexts (e.g., Center for Disease Control, 2011). However, given the extent of trauma exposure in this community sample and that PTS in this context was associated with increased risk of a range of traumatic events, we echo the call of Messman-Moore and Long (2003) for researchers, providers, and policymakers to take an ecological perspective on retraumatization that accounts for multiple levels of influence (e.g., individual, interpersonal, societal) on cycles of violence.
Limitations
Several limitations to the study are worth noting. Although the checklist of traumatic events allowed for assessment of a wide range of experiences, we lacked in-depth information about the events reported and all events were given equal weight. There is intra-category variability for traumatic events assessed via checklist like the one used in this study (Dohrenwend, 2006), and we were unable to determine how much assaultive versus non-assaultive events were influenced by individual characteristics. For example, some of the non-assaultive events (e.g., motor vehicle accident) could be due in part to engagement in risk behavior (e.g., substance use) to ameliorate negative emotions resulting from PTS. It is also likely that variations in characteristics of traumatic events, such as their severity, duration, and appraisal, could influence subsequent PTS symptoms. Likewise, PTS could be could differentially related to various aspects of subsequent trauma exposure. As such, further studies that include more precise assessments of traumatic events are needed to deepen our understanding over how trauma and PTS relate over time. Participants’ reports of traumatic events might also have been biased by their current symptoms, such that those suffering from higher PTS might have been likely to report more events (e.g., Roemer, Litz, Orsillo, Ehlich, & Friedman, 1998). Retrospective bias could inflate correlations between PTS and traumatic events within each wave, and possibly longitudinal associations as well. The low sensitivity of the modified PCL-C as a diagnostic instrument of lifetime PTSD, relative to the CAPS, in the larger study is an additional limitation. Notably, however, the PCL-C was not used as the basis for a categorical indicator of PTSD in the current study, but rather as a continuous measure of PTS symptoms. Additionally, it is unclear how conservative estimates of participants’ symptomatology would affect associations with trauma exposure.
The focus of the study was also limited to trauma exposure, rather than a wider range of events that could shape, and be shaped by, PTS symptomatology. Future studies that incorporate more general stressors (e.g., relationship tensions, employment difficulties) in addition to trauma, for example, could better reflect relationships between accumulated adversity and PTS. As mentioned previously, we also lacked measures assessing constructs that could tap into the mechanisms through which PTS could influence subsequent trauma exposure, such as impairments in threat detection, emotion dysregulation, or risk behaviors. Further studies that include more waves of data could also use a latent difference score approach to model mean level change in PTS and trauma exposure over time (c.f., King et al., 2006).
In addition, participants who did not report any lifetime traumatic events at W1 were not included in the analysis, which might have inflated associations between PTS and subsequent trauma exposure. These excluded participants did not complete W1 assessments of lifetime PTS, and it did not make sense conceptually to estimate their W1 PTS using maximum likelihood (since these values would not be missing at random) or set their W1 PTS to zero (which would carry the flawed assumption that they had no W1 PTS-like symptoms). Another noteworthy limitation was that rates of missingness at the W2 and W3 were high, particularly on the measure of PTS. Moreover, participants who completed W2 and W3 assessments of PTS had significantly higher baseline PTS and trauma exposure than those did not. Although the use of maximum likelihood allowed us to include participants with missing data, it is possible that this approach did not capture unmeasured differences between the two groups that could have biased our results. One possibility is that some of the participants missing follow-up assessments could not recall the event they reported as the “worst” at baseline, despite being reminded of which event they had reported, and therefore could not report on PTS linked to that event. It is also possible that some participants refused to report on PTS linked to their “worst” W1 event, but completed other measures in the study, including the inventory of traumatic events. Notably, none of the interviewers provided participant comments on why they did not complete subsequent assessments of PTS, nor did they provide any insight into this pattern. A more general limitation of the study was having all assessments linked to the “worst” event. Although this method allowed for consistency in measurement over time (e.g., versus linking subsequent assessments to a different traumatic event), it does not fit with a conceptualization of PTSD as a set of symptoms that could be connected to multiple traumatic events. The measure of PTS was also based on the DSM-IV, rather than the DSM-5, diagnostic criteria for PTSD. The scale items did not reflected updated wording of symptoms, and the three additional symptoms were not assessed. It is possible that these alterations could have affected the results and therefore replication with updated measures is needed.
Replication across other urban environments is also needed given that the participants were all from the same metropolitan area. An additional consideration is that the sample was, on average, middle-aged (M = 52.47 years old, SD = 16.06, range: 18–92). Persons aged 12 to 24 years are at highest risk of violence exposure (Truman & Planty, 2012), and only 6.0% of the sample was 24 or younger at baseline. It is possible that the relatively low incidence of assaultive events in the current study could render associations between PTS and assaultive trauma weaker than in a study focusing on younger adults. Additionally, the associations could be inflated due to the strong influence of the environment for individuals living in a high-poverty, urban context. That is, environmental factors, such as neighborhood violence, poor housing quality, and lack of access to adequate healthcare, could increase the risk of both traumatic events and PTS, perhaps strengthening the relationship between them. This could be especially true for non-assaultive traumatic events, which were reported somewhat more often than assaultive events in the current study.
Despite these limitations, the results of the study further our understanding of the processes that lead to chronic PTS. In the sample of trauma survivors from a predominantly non-Hispanic Black urban context, we found that past-year exposure to assaultive events was associated with significantly greater PTS at follow-up. Higher PTS, in turn, was significantly associated with further exposure to more non-assaultive traumatic events. The findings suggest that individuals suffering from PTS might paradoxically live in contexts that put them at higher risk of exposure to non-assaultive traumatic events. Further exposure to assaultive events, in contrast, heightens risk for worsening PTS. Future research that explores the mechanisms underlying these pathways would provide important insights for policy and practice.
Acknowledgments
This research was supported by grants from the National Institute for Drug Abuse (R01 DA022720) and National Institute of Mental Health (T32 MH013043). We acknowledge Allison Aiello, Derek Wildman, and the rest of the DNHS research group.
Contributor Information
Sarah R. Lowe, Columbia University
Kate Walsh, Columbia University.
Monica Uddin, Wayne State University.
Sandro Galea, Columbia University.
Karestan C. Koenen, Columbia University
References
- American Psychological Association. Diagnostic and statistical manual of mental disorders. 4. Washington, DC: Author; 1994. [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behavioral Research and Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Breslau N, Chilcoat HD, Kessler RC, Davis GC. Previous exposure to trauma and PTSD effects of subsequent trauma: Results from the Detroit Area Survey of Trauma. American Journal of Psychiatry. 1999;156:902–907. doi: 10.1176/ajp.156.6.902. Retrieved from http://archpsyc.jamanetwork.com/journal.aspx. [DOI] [PubMed] [Google Scholar]
- Breslau N, Kessler RC, Chilcoat HD, Schultz LR, Davis GC, Andreski P. Trauma and posttraumatic stress disorder in the community. Archives of General Psychiatry. 1998;55:626–632. doi: 10.1001/archpsyc.55.7.626. [DOI] [PubMed] [Google Scholar]
- Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. Journal of Consulting & Clinical Psychology. 2000;68:748–766. doi: 10.1037/0022-006X.68.5.748. [DOI] [PubMed] [Google Scholar]
- Center for Disease Control. Youth violence: Prevention strategies. 2011 Retrieved from: http://www.cdc.gov/violenceprevention/youthviolence/prevention.html.
- Cheung GW, Resnvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Structural Equation Modeling. 2002;9:233–255. doi: 10.1207/S15328007SEM0902_5. [DOI] [Google Scholar]
- Cohen J. Statistical power analysis in the behavioral sciences. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]
- Cougle JR, Resnick H, Kilpatrick DG. Factors associated with chronicity of posttraumatic stress disorder: A prospective analysis of a national sample of women. Psychological Trauma: Theory, Research, Practice, and Policy. 2013;5:43–49. doi: 10.1037/a0025954. [DOI] [Google Scholar]
- Cougle JR, Resnick H, Kilpatrick DG. A prospective examination of PTSD symptoms as risk factors for subsequent exposure to potentially traumatic events among women. Journal of Abnormal Psychology. 2009;118:405–411. doi: 10.1037/a0015370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dohrenwend BP. Inventorying stressful life events as risk factors for psychopathology. Psychological Bulletin. 2006;132:477–495. doi: 10.1037/0033-2909.132.3.477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gabert-Quillen CA, Irish Leah A, Siedjeski E, Fallon W, Spoonster E, Delahanty DL. The impact of social support on the relationship between trauma history and posttraumatic stress disorder symptoms in motor vehicle accident victims. International Journal of Stress Management. 2012;19:69–79. doi: 10.1037/a0026488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gill JM, Page GG, Sharps P, Campbell JC. Experiences of traumatic events and associations with PTSD and depression development in urban health care-seeking women. Journal of Urban Health. 2008;85:693–706. doi: 10.1007/s11524-008-9290-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hu L, Bentler P. Cutoff criteria for fit indexes in covariance structure: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. doi: 10.1080/10705519909540118. [DOI] [Google Scholar]
- IBM Corp. IBM SPSS Statistics for Windows. Version 20.0. Armonk, NY: IBM Corp; 2011. [Google Scholar]
- Jarvis CB, MacKenzie SB, Podsakoff PM. A critical review of construct indicators and measurement model misspecification in marketing and consumer research. Journal of Consumer Research. 2003;30:199–218. doi: 10.1086/376806. [DOI] [Google Scholar]
- Kessler RC, Sonnega A, Bromet E, Hughes M, Nelson CB. Posttraumatic stress disorder in the National Comorbidity Survey. Archives of General Psychiatry. 1995;52:1048–1060. doi: 10.1001/archpsyc.1995.03950240066012. [DOI] [PubMed] [Google Scholar]
- Kline RB. Principles and practice of structural equation modeling. 2. New York, NY: Guilford; 2005. [Google Scholar]
- Kilpatrick DG, Ruggiero KJ, Acierno R, Saunders BE, Resnick HS, Best CL. Violence and risk of PTSD, major depression, substance abuse/dependence, and comorbidity: Results from the National Survey of Adolescents. Journal of Consulting and Clinical Psychology. 2003;71:692–700. doi: 10.1037/0022-006X.71.4.692. [DOI] [PubMed] [Google Scholar]
- King DW, Leskin GA, King LA, Weathers FW. Confirmatory factor analysis of the Clinician-Administered PTSD Scale: Evidence for dimensionality of posttraumatic stress disorder. Psychological Assessment. 1998;10:90–96. doi: 10.1037//1040-3590.10.2.90. [DOI] [Google Scholar]
- King LA, King DW, McArdle JJ, Saxe GN, Doron-LaMarca S, Orazem RJ. Latent difference score approach to longitudinal trauma research. Journal of Traumatic Stress. 2006;19:771–785. doi: 10.1002/jts.20188. [DOI] [PubMed] [Google Scholar]
- Kujipers KF, van der Knapp LM, Winkel FW. PTSD symptoms as risk factors for intimate partner violence revictimization and the mediating role of victims’ violent behavior. Journal of Traumatic Stress. 2012;25:179–186. doi: 10.1002/jts.21676. [DOI] [PubMed] [Google Scholar]
- Liebschutz J, Saitz R, Brower V, Keane TM, Lloyd-Travaglini C, Averbuch T, Samet JH. PTSD in urban primary care: High prevalence and low physician recognition. Journal of General Internal Medicine. 2007;22:719–726. doi: 10.1007/s11606-007-0161-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marx BP, Heidt JM, Gold SD. Perceived uncontrollability and unpredictability, self-regulation, and sexual sevictimization. Review Of General Psychology. 2005;9:67–90. doi: 10.1037/1089-2680.9.1.67. [DOI] [Google Scholar]
- McLaughlin KA, Conron KJ, Koenen KC, Gilman SE. Childhood adversity, adult stressful life events, and risk of past-year psychiatric disorder: a test of the stress sensitization hypothesis in a population-based sample of adults. Psychological Medicine. 2010;40:1647–1658. doi: 10.1017/S0033291709992121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Messman-Moore TL, Long PJ. The role of childhood sexual abuse sequelae in the sexual revictimization of women: An empirical review and theoretical reformulation. Clinical Psychology Review. 2003;23:537–571. doi: 10.1016/S0272-7358(02)00203-9. [DOI] [PubMed] [Google Scholar]
- Messman-Moore TL, Ward RM, Brown AL. Substance use and PTSD symptoms impact the likelihood of rape and revictimization in college women. Journal of Interpersonal Violence. 2009;24:499–521. doi: 10.1177/0886260508317199. [DOI] [PubMed] [Google Scholar]
- Muthén B. Applications of causally defined direct and indirect effects in mediation analysis using SEM in Mplus. 2011 Manuscript submitted for publication. Retrieved from http://www.statmodel.com/download/causalmediation.pdf.
- Múthen L, Múthen B. Mplus user’s guide. Version 7. Los Angeles, CA: Múthen & Múthen; 1998–2012. [Google Scholar]
- Ng-Mak DS, Salzinger S, Feldman RS, Stueve CA. Normalization of violence among inner-city youth: A formulation for research. American Journal of Orthopsychiatry. 2002;72:92–101. doi: 10.1037/0002-9432.72.1.92. [DOI] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TI, Weiss DS. Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Bulletin. 2003;129:52–73. doi: 10.1037/0033-2909.129.1.52. [DOI] [PubMed] [Google Scholar]
- Pietrzak RH, Goldstein RB, Southwick SM, Grant BF. Medical comorbidity of full and partial posttraumatic stress disorder in U.S. adults: Results from Wave 2 of the National Epidemiologic Survey on Alcohol and Related Conditions. Psychosomatic Medicine. 2011;73:697–707. doi: 10.1097/PSY.0b013e3182303775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ponniah K, Hollon SD. Empirically supported psychological treatments for adult acute stress disorder and posttraumatic stress disorder: A review. Depression and Anxiety. 2009;26:1086–1109. doi: 10.1002/da.20635. [DOI] [PubMed] [Google Scholar]
- Risser HJ, Hetzel-Riggin MD, Thomsen CJ, McCanne TR. PTSD as a mediator of sexual revictimization: The role of reexperiencing, avoidance, and arousal symptoms. Journal of Traumatic Stress. 2006;19:687–698. doi: 10.1002/jts.20156. [DOI] [PubMed] [Google Scholar]
- Roberts AL, Gilman SE, Breslau J, Breslau N, Koenen KC. Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological Medicine. 2011;41:71–83. doi: 10.1017/S0033291710000401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roemer L, Litz BT, Orsillo SM, Ehlich PJ, Friedman MJ. Increases in retrospective accounts of war-zone exposure over time: The role of PTSD symptom severity. Journal of Traumatic Stress. 1998;11:597–605. doi: 10.1023/A:1024469116047. [DOI] [PubMed] [Google Scholar]
- Sandberg DA, Matorin AI, Lynn SJ. Dissociation, posttraumatic stress symptomatology, and sexual revictimization: A prospective examination of mediator and moderator analysis. Journal of Traumatic Stress. 1999;12:127–138. doi: 10.1023/A:1024702501224. [DOI] [PubMed] [Google Scholar]
- Santorra A, Bentler PM. A scaled difference chi-square test statistic for moment structure analysis. Psychometrika. 2001;66:507–514. doi: 10.1007/BF02296192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schumm JA, Briggs-Phillips M, Hobfoll SE. Cumulative interpersonal traumas and social support as risk and resiliency factors in predicting PTSD and depression among inner-city women. Journal of Traumatic Stress. 2006;19:825–836. doi: 10.1002/jts.20159. [DOI] [PubMed] [Google Scholar]
- Truman JL, Planty M. Criminal victimization, 2011. Washington, DC: United States Department of Justice; 2012. Retrieved from www.ojp.usdoj.gov. [Google Scholar]
- Uddin M, Aiello A, Wildman DE, Koenen KC, Pawelec G, de los Santos R, Goldmann E, Galea S. Epigenetic and immune function profiles associated with posttraumatic stress disorder. Proceedings of the National Academy of Sciences. 2010;107:9470–9475. doi: 10.1073/pnas.0910794107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh K, Danielson CK, McCauley J, Saunders BE, Kilpatrick DG, Resnick HS. National prevalence of PTSD among sexually revictimized adolescent, college, and adult women. Archives of General Psychiatry. 2012;69:935–942. doi: 10.1001/archgenpsychiatry.2012.132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh K, DiLillo D, Messman-Moore TL. Lifetime sexual victimization and poor risk perception: Does emotion dysregulation account for the links? Journal of Interpersonal Violence. 2012;27:3054–3071. doi: 10.1177/0886260512441081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Ford J. Psychometric properties of the PTSD checklist (PCL-C, PCL-S, PCL-M, PCL-PR) In: Stamm BH, editor. Measurement of stress, trauma, and adaptation. Lutherville, MD: Sidran; 1996. [Google Scholar]
- Weathers F, Litz B, Herman D, Huska J, Keane T. The PTSD checklist (PCL): Reliability, validity, and diagnostic utility. Presented to the meeting of the International Society of Traumatic Stress Studies.Oct, 1993. [Google Scholar]
- Yehuda R, Flory JD, Pratchett LC, Buxbaum J, Ising M, Holsboer F. Putative biological mechanisms for the association between early life adversity and the subsequent development of PTSD. Psychopharmacology. 2010;212:405–17. doi: 10.1007/s00213-010-1969-6. [DOI] [PubMed] [Google Scholar]