Abstract
Decentralization of HIV care is promoted to improve access to antiretroviral therapy in sub-Saharan Africa. This study describes care transitions among HIV-infected persons in Northern Tanzania during a period of rapid decentralization of HIV Care and Treatment Centers (CTCs) from hospitals to local health centers.
Between November 2008 and June 2009, 492 HIV-infected patients in established care at two referral hospitals in Moshi, Tanzania, and 262 persons newly diagnosed with HIV were selected for participation in a prospective cohort study entitled Coping with HIV/AIDS in Tanzania. Clinical records and participant self-reports, collected between June and November 2012, were used to describe retention in care and transitions between CTCs during the study period.
After a mean follow-up period of 3.5 years, 10 percent of participants had died, 9 percent were lost to follow-up, and 11 percent had moved. Of the remaining participants enrolled from CTCs, more than 90 percent reported at least one CTC visit during the previous six months, with 98 percent still in care at the CTC at which they were enrolled. Nearly 3 out of 4 newly diagnosed clients listed a referral hospital as their primary CTC. Fewer than 10 percent of participants ever sought care at another CTC in the study area; nearly 90 percent of those in care bypassed their closest CTC. Administrative data from all facilities in the study area indicate that new clients, even after the scale-up from 8 CTCs in 2006 to 21 CTCs in 2008, disproportionately selected established CTCs, and client volume at newly approved facilities was highly variable.
Despite the decentralization of HIV care and treatment in this setting, many patients continue to bypass their closest CTC to seek care at established facilities. Patient preferences for HIV care, which may inform optimal resource utilization, are largely unknown and warrant further investigation.
Keywords: HIV/AIDS, antiretroviral therapy, decentralization, treatment retention, Tanzania
BACKGROUND
Access to antiretroviral therapy (ART) in low- and middle-income countries (LMIC) has improved dramatically over the past decade (World Health Organization, 2013), facilitated in part by the decentralization and scale-up of the number of health facilities providing ART (El-Sadr et al., 2012; TACAIDS, 2012).
Decentralization of HIV care has been pursued by numerous sub-Saharan African (SSA) countries (see, e.g., Fayorsey et al., 2013; Pfeiffer et al., 2010; Topp et al., 2013; Uebel, Joubert, Wouters, Mollentze, & van Rensburg, 2013; World Health Organization, 2013) and is advocated by the President’s Emergency Plan for AIDS Relief (PEPFAR) as a means of expanding coverage, co-utilizing services for HIV and other illnesses, and improving engagement and retention in care (PEPFAR, 2009; Gilks et al., 2006; Mulamba et al., 2010). While several implementation studies (Mutemwa et al., 2013; Topp et al., 2013; Uebel et al., 2013) described efficiency gains due to decentralization and integration of HIV care with care for other conditions, little is known about changes in patients’ care-seeking behaviors in response to the availability of additional treatment options.
In 2008, near the beginning of a marked expansion of HIV care and treatment in Tanzania, the Coping with HIV/AIDS in Tanzania (CHAT) study prospectively enrolled cohorts of patients with established HIV infection and persons newly diagnosed with HIV, with the aims of identifying predictors of HIV treatment adherence and health outcomes in a SSA setting. Analyses of study participants’ transitions between HIV care and treatment centers (CTCs) during the 3.5 year study period provide a unique opportunity to assess the effects of HIV care and treatment decentralization on care-seeking behaviors.
METHODS
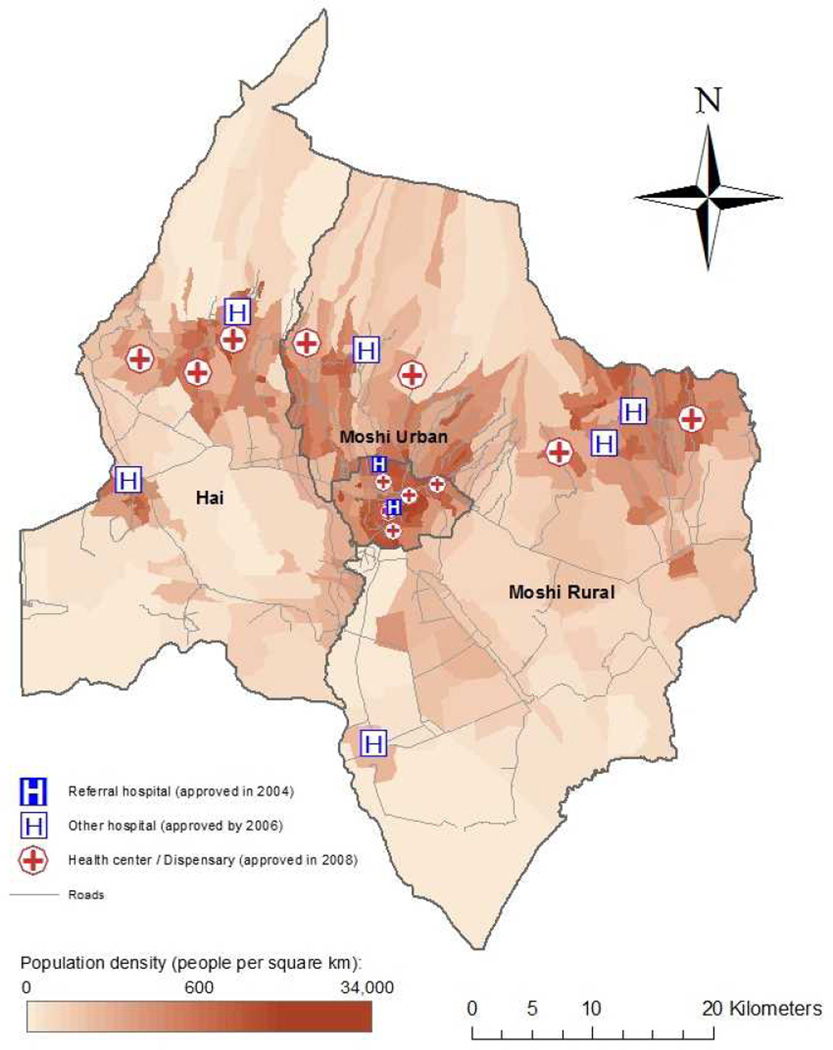
CHAT is an observational cohort study designed to explore the relationships between psychosocial characteristics, treatment adherence, and health outcomes among HIV-positive individuals in Tanzania (Pence et al., 2012). The study was conducted in three districts in Kilimanjaro Region, Tanzania. During the past decade, the study area experienced a significant increase in the number of health facilities providing HIV care and treatment services. In 2004, only one zonal referral hospital and one regional public hospital, both in the Region’s capital, were operating as CTCs; by 2008, the number of CTCs had increased to 21 (Figure 1.)
Figure 1.
HIV care and treatment centers (CTCs) in the CHAT study area
Note: Two proximal health center-based CTCs in Moshi Urban are indistinguishable in the figure.
Sample selection
Between November 2008 and June 2009, CHAT recruited 492 patients with established HIV infection from the region’s two referral hospitals and 262 newly diagnosed individuals from four urban voluntary counseling and testing sites. Participants were ages 18–65 years at enrollment and had no plans to leave the study area. The detailed CHAT sampling and enrollment approach has been described previously (Pence et al., 2012) and is summarized in a supplemental online appendix.
Data collection
Surveys addressing varied domains, including demographic characteristics, HIV knowledge and risk behaviors, physical and mental health, and HIV medication adherence were administered twice annually by trained research interviewers in participants’ native language, Kiswahili (Pence et al., 2012). At the 3.5 year follow-up assessment, participants were also asked to list all CTCs ever attended and to identify their primary CTC. GPS coordinates were obtained for all study area CTCs; participants’ residences were linked to village centroids (OpenMicroData, 2013).
Ethical considerations
Study activities were approved by the Institutional Review Boards of Duke University, Kilimanjaro Christian Medical College and the National Institute for Medical Research in Tanzania.
Analysis
Student t-tests and chi-squared statistics were used to assess the statistical significance of differences between participants in established care and those newly diagnosed at enrollment. Distances from village centroids to study area CTCs were calculated using the shortest possible route along a known road network, plus straight line distances from each endpoint to the nearest road (ESRI, Redlands, CA).
RESULTS
Participants’ demographic and clinical characteristics are summarized in Table 1. At baseline, nearly two-thirds of participants had experienced a WHO stage 3 or 4 event; the majority had a nadir CD4+ count below 200 cells/mm3; 82 percent of those in established care were on ART. More than half of the participants came from rural areas. On average, patients reported travelling more than 15km and spent more than 1 hour getting to the CTC.
Table 1.
CHAT sample characteristics at baseline (N=754)
| In established care | Newly diagnosed 1 | ||
|---|---|---|---|
| Number of participants | 492 | 262 | |
| Client charactistics | Percent or mean (sd) |
Percent or mean (sd) |
p-value |
| Female gender | 68.1 % | 68.7 % | 0.863 |
| Age (years) | 41.8 (8.8) | 37.4 (9.0) | <0.001 |
| Married | 36.8 % | 37.8 % | 0.787 |
| Nadir CD4+ count < 200 cells/mm3 | 63.0 % | 50.0 % | 0.107 |
| 200 to < 350 cells/mm3 | 24.3 % | 26.7 % | |
| 350 to < 500 cells/mm3 | 8.9 % | 15.0 % | |
| 500+ cells/mm3 | 3.8 % | 8.3 % | |
| WHO stage 3 or 4 | 64.4 % | 60.0 % | 0.404 |
| Years since HIV diagnosis | 2.0 (1.7) | 0.0 (0.0) | <0.001 |
| On antiretroviral therapy | 82.4 % | 10.3 % | <0.001 |
| Rural residence | 57.6 % | 62.5 % | 0.206 |
| Time spent getting to the CTC (minutes) | 80.9 (46.9) | ||
| Patient-reported distance to CTC (km) | 15.7 (12.5) | ||
| Cost of getting to and from CTC (TSH) 2 | 1749.2 (1352.0) |
Of newly diagnosed participants, 38% were enrolled immediately, 49 percent within one week of diagnosis; 13% more than one week after diagnosis.
In 2008, the exchange rate of US Dollar to Tanzania shilling was approximately 1:1,200.
After 3.5 years of follow-up, nearly 3 out of 4 newly diagnosed clients listed a referral hospital as their primary CTC, and 98 percent of participants enrolled at the two referral hospitals still considered these hospitals to be their primary CTC (Table 2). Only 5 percent of CHAT participants ever sought care at another facility in the study area.
Table 2.
HIV care and treatment among CHAT participants after 3.5 years of follow-up (N=525)
| Participants enrolled from | ||||
|---|---|---|---|---|
| Referral hospital 1 |
Referral hospital 2 |
Newly diagnosed |
Total | |
| N (%) | N (%) | N (%) | N (%) | |
| N at baseline | 223 | 269 | 262 | 754 |
| Died | 7 (3%) | 26 (10%) | 42 (16%) | 75 (10%) |
| Lost to follow-up | 8 (4%) | 16 (6%) | 46 (18%) | 70 (9%) |
| Moved during the study period 1 | 24 (11%) | 24 (9%) | 36 (14%) | 84 (11%) |
| N at follow-up 2 | 184 | 203 | 138 | 525 |
| At least 1 CTC visit in the past 6 months | 166 (90%) | 190 (94%) | 111 (80%) | 467 (89%) |
| Primary care location after 3.5 years | ||||
| Referral hospital 1 | 181 (98%) | 1 (0%) | 8 (6%) | 190 (36%) |
| Referral hospital 2 | 0 (0%) | 198 (98%) | 94 (68%) | 292 (56%) |
| Other hospital | 0 (0%) | 1 (0%) | 3 (2%) | 4 (1%) |
| Health center | 2 (1%) | 2 (1%) | 16 (12%) | 20 (4%) |
| Out of the study area | 1 (1%) | 1 (0%) | 7 (5%) | 9 (2%) |
| Never sought care at a CTC | 0 (0%) | 0 (0%) | 10 (7%) | 10 (2%) |
| Total # of CTCs ever attended | ||||
| 1 | 165 (90%) | 176 (87%) | 104 (75%) | 445 (85%) |
| 2 | 17 (9%) | 26 (13%) | 23 (17%) | 66 (13%) |
| 3 | 2 (1%) | 1 (0%) | 1 (1%) | 4 (1%) |
| # of CTCs in the study area ever attended | ||||
| None | - | - | 13 (9%) | 13 (2%) |
| 1 | 171 (93%) | 188 (93%) | 112 (81%) | 471 (90%) |
| 2 | 12 (7%) | 15 (7%) | 13 (9%) | 40 (8%) |
| 3 | 1 (1%) | 0 (0%) | 0 (0%) | 1 (0%) |
84 participants who moved during the study period were excluded from analyses of treatment locations at follow-up because many of these participants moved out of the study area, and patients may have moved for their HIV care.
All subsequent percentages refer to CHAT participants observed at both baseline and follow-up who did not move during the study period.
Many patients bypassed multiple closer facilities for care at their self-identified primary CTC (Table 3). For both urban and rural participants the distance to their primary CTC was more than twice the distance to their closest CTC. One of 10 rural patients and 12 percent of urban patients sought care at their closest CTC; half of rural participants and two thirds of urban participants were in care at their respective closest hospital-based CTCs. Only 2 percent were in care at their nearest health center.
Table 3.
Distances from participants' homes to HIV care and treatment centers, 2012 (N=502)
| Rural | Urban | ||
|---|---|---|---|
| # of participants1 | 265 | 237 | |
| # of active CTCs in the study area | 13 | 8 | |
| Estimated distance to the primary CTC (km) | 20.5 (11.6) | 5.5 (7.4) | <0.001 |
| Estimated distance to the closest CTC (km) | 9.5 (6.6) | 2.5 (4.2) | <0.001 |
| % of patients seeking care at: | |||
| Closest HIV CTC | 10.2 % | 12.7 % | 0.384 |
| Closest hospital-based CTC | 46.0 % | 66.7 % | <0.001 |
| Closest health center-based CTC | 1.5 % | 2.1 % | 0.613 |
| # of urban CTCs bypassed for care | 2.9 (2.2) | 3.0 (2.3) | 0.713 |
| # of rural CTCs bypassed for care | 1.6 (1.8) | 0.2 (0.9) | <0.001 |
| Total # of CTCs bypassed for care | 4.5 (3.2) | 3.1 (2.6) | <0.001 |
Excludes 10 participants who never sought care at a CTC, 9 participants whose primary CTC is outside the study area, and 4 participants with missing data on residence or CTC location
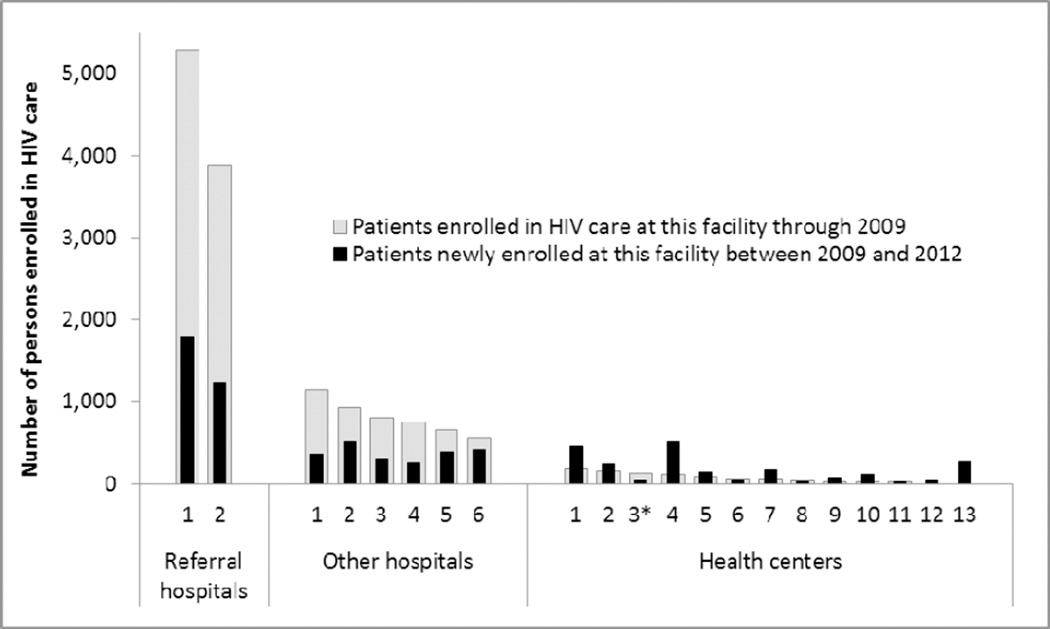
Administrative data from the study area also suggest limited utilization of many newly approved CTCs. Between 2009 and 2012, 3,291 new clients enrolled at the two referral hospitals (1,645 per facility); 2,435 at six other hospitals (406 per facility); and 2,332 at fourteen health centers (167 per facility; Figure 2). The variation in client enrollment at newly approved facilities was high.
Figure 2.
Patient enrollment before and after CTC scale-up in the study area, 2009 through 2012
Source: Administrative data for the CHAT study area; sequential numbers identify individual CTCs in each category (referral hospitals; other hospitals; health centers), sorted by cumulative patient enrollment through September 2009. The cumulative number of clients ever enrolled at CTCs in the study area increased from 14,865 in 2009 to 22,874 in 2012. Correlation between pre- and post-2009 volumes: rho=0.9526; R2=0.9075.
*2011 data were used due to missing 2012 data for one facility.
DISCUSSION
This study describes treatment retention and care transitions among a cohort of HIV infected adults during a period of rapid HIV care and treatment scale-up in Northern Tanzania. After 3.5 years of follow-up, despite a near tripling of the number of CTCs in the study area, 98 percent of patients enrolled from the two referral hospitals remained in care at these facilities, and nearly three quarters of newly diagnosed study participants made a referral hospital their primary CTC. Despite concerted efforts to decentralize HIV care and treatment to smaller, local facilities, many patients continued to bypass their closest CTC, and the number of clients enrolled at newly approved CTCs was low and varied greatly across facilities.
While patients’ familiarity with existing care providers may have played a role in limiting care transitions, a variety of characteristics, including concerns regarding quality of care, confidentiality, patient-provider interactions, cost, and the availability of medications, laboratory tests, and other services (T. Heckman et al., 1998; Ickovics & Meade, 2002; Meredith, Orlando, Humphrey, Camp, & Sherbourne, 2001; R. Whetten et al., 2006), influence patients’ decisions to engage and remain in care at specific facilities.
A recent Cochrane review (Kredo, Ford, Adeniyi, & Garner, 2013) provided no evidence that decentralization from hospitals to more peripheral health facilities led to worse health outcomes, and in some settings loss to care was reduced. However, experiences from both wealthier and poorer nations suggest that the quality of HIV care varies greatly across diverse HIV treatment clinics (Halm, Lee, & Chassin, 2002; T. G. Heckman et al., 1998; Hogg et al., 1998; Shapiro et al., 1999). While some studies indicate that comparable quality can be provided at primary health facilities (Boyer et al., 2012; Fayorsey et al., 2013; Hansudewechakul et al., 2012; McGuire et al., 2012), others document a lack of laboratory facilities, medication shortages and limited drug options (Labhardt et al., 2012; Nyogea et al., 2012; Pasquet et al., 2010). Further, while some aspects of localized care, such as community-based support and increased tracing of defaulters, may appeal to some patients, others may perceive these activities as intrusive or stigmatizing (Humphreys et al., 2010).
While this study cannot ascertain the reasons for patients’ treatment decisions, low rates of care transitions to smaller CTCs have significant implications for the cost-effectiveness of decentralization efforts and the potential success of further decentralization of HIV care. The push for decentralization of HIV care to rural areas in the United States in the 1990s was not as successful as hoped, largely due to concerns about the quality of care, confidentiality, and stigma (McKinney, 2002; Nguyen & Whetten, 2003; Reif, Golin, & Smith, 2005; K. Whetten & Pence, 2013; K. Whetten, Reif, Whetten, & Murphy-McMillan, 2008). Similar concerns affect care in rural areas of low and middle-income countries (Kahabuka, Kvåle, Moland, & Hinderaker, 2011; Kahabuka, Moland, Kvåle, & Hinderaker, 2012; Tran & Nguyen, 2012).
We acknowledge several limitations of this study. Rates of care transitions in this study may not be representative of all HIV patients in the area; no information was available on care locations among those who dropped out of the study; and treatment patterns may differ for different populations, including by gender. Further, the findings may not be generalizable to other areas that experienced similar scale-up of HIV care and treatment.
CONCLUSION
Despite intense efforts to scale-up and decentralize HIV care, many patients continue to bypass their closest HIV CTC to seek care at larger established facilities. With the effectiveness and cost-effectiveness of decentralization depending greatly on the ability of new CTCs to attract and retain a sufficiently large client base, further evidence is needed to understand the characteristics of care and treatment delivery that influence patients’ care-seeking behaviors.
Supplementary Material
Acknowledgements
Funding. This publication was made possible by Grant Number 5R01MH078756 from the National Institute of Mental Health, and supported by the Duke University Center for AIDS Research (CFAR), an NIH funded program (5P30 AI064518). KL2 RR024127-04 provided salary support for Dr. Reddy. The contents of this publication are solely the responsibility of the authors and do not necessarily represent the official views of the National Institute of Mental Health or the National Institutes of Health.
We acknowledge the support provided by the Regional Medical Officer of the Kilimanjaro Region, Dr. Mtumwa Mwako.
Contributor Information
Jan Ostermann, Email: jan.ostermann@gmail.com.
Kathryn Whetten, Email: katewhetten@gmail.com.
Elizabeth Reddy, Email: elizabeth.reddy@duke.edu.
Brian Pence, Email: bpence@unc.edu.
Andrew Weinhold, Email: andrew.weinhold@gmail.com.
Dafrosa Itemba, Email: dafrosakoku@gmail.com.
Venance Maro, Email: venmaro@ymail.com.
Eligy Mosille, Email: eligymosille@yahoo.com.
Nathan Thielman, Email: n.thielman@duke.edu.
REFERENCES
- Asenso-Okyere WK, Anum A, Osei-Akoto I, Adukonu A. Cost recovery in Ghana: are there any changes in health care seeking behaviour? Health Policy Plan. 1998;13:181–188. doi: 10.1093/heapol/13.2.181. [DOI] [PubMed] [Google Scholar]
- Boyer S, Protopopescu C, Marcellin F, Carrieri MP, Koulla-Shiro S, Moatti JP, Spire B. Performance of HIV care decentralization from the patient's perspective: health-related quality of life and perceived quality of services in Cameroon. Health Policy Plan. 2012;27(4):301–315. doi: 10.1093/heapol/czr039. [DOI] [PubMed] [Google Scholar]
- El-Sadr WM, Holmes CB, Mugyenyi P, Thirumurthy H, Ellerbrock T, Ferris R, Whiteside A. Scale-up of HIV treatment through PEPFAR: a historic public health achievement. J Acquir Immune Defic Syndr. 2012;603(Suppl):S96–S104. doi: 10.1097/QAI.0b013e31825eb27b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fayorsey RN, Saito S, Carter RJ, Gusmao E, Frederix K, Koech-Keter E, Abrams EJ. Decentralization of pediatric HIV care and treatment in five sub-Saharan African countries. J Acquir Immune Defic Syndr. 2013;62(5):e124–e130. doi: 10.1097/QAI.0b013e3182869558. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilks CF, Crowley S, Ekpini R, Gove S, Perriens J, Souteyrand Y, De Cock KM. The WHO public-health approach to antiretroviral treatment against HIV in resource-limited settings. Lancet. 2006;368:505–510. doi: 10.1016/S0140-6736(06)69158-7. [DOI] [PubMed] [Google Scholar]
- Haddad S, Fournier P. Quality, cost and utilization of health services in developing countries. A longitudinal study in Zaire. Soc Sci Med. 1995;40:743–753. doi: 10.1016/0277-9536(94)00134-f. [DOI] [PubMed] [Google Scholar]
- Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med. 2002;137(6):511–520. doi: 10.7326/0003-4819-137-6-200209170-00012. [DOI] [PubMed] [Google Scholar]
- Hansudewechakul R, Naiwatanakul T, Katana A, Faikratok W, Lolekha R, Thainuea V, McConnell MS. Successful clinical outcomes following decentralization of tertiary paediatric HIV care to a community-based paediatric antiretroviral treatment network, Chiangrai, Thailand, 2002 to 2008. J Int AIDS Soc. 2012;15(2):17358. doi: 10.7448/IAS.15.2.17358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heckman T, Somlai A, Peters J, Walker J, Otto-Salaj L, Galdabini C, Kelly J. Barriers to care among persons living with HIV/AIDS in urban and rural areas. AIDS Care. 1998;10(3):365–375. doi: 10.1080/713612410. [DOI] [PubMed] [Google Scholar]
- Heckman TG, Somlai AM, Peters J, Walker J, Otto-Salaj L, Galdabini CA, Kelly JA. Barriers to care among persons living with HIV/AIDS in urban and rural areas. AIDS Care. 1998;10(3):365–375. doi: 10.1080/713612410. [DOI] [PubMed] [Google Scholar]
- Hogg RS, Raboud J, Bigham M, Montaner JS, O'Shaughnessy M, Schechter MT. Relation between hospital HIV/AIDS caseload and mortality among persons with HIV/AIDS in Canada. Clin Invest Med. 1998;21(1):27–32. [PubMed] [Google Scholar]
- Humphreys C, Wright J, Walley J, Mamvura C, Bailey K, Ntshalintshali S, et al. Nurse led, primary care based antiretroviral treatment versus hospital care: a controlled prospective study in Swaziland. BMC Health Serv Res. 2010;10:229. doi: 10.1186/1472-6963-10-229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ickovics JR, Meade CS. Adherence to HAART among patients with HIV: Breakthroughs and barriers. AIDS Care. 2002;14(3) doi: 10.1080/09540120220123685. [DOI] [PubMed] [Google Scholar]
- Jacobsen K, Ansumana R, Abdirahman H, Bockarie A, Bangura U, Meehan KA, et al. Considerations in the selection of healthcare providers for mothers and children in Bo, Sierra Leone: reputation, cost and location. International Health. 2012;4:307–313. doi: 10.1016/j.inhe.2012.09.004. [DOI] [PubMed] [Google Scholar]
- Kahabuka C, Kvåle G, Moland KM, Hinderaker SG. Why caretakers bypass Primary Health Care facilities for child care - a case from rural Tanzania. BMC Health Serv Res. 2011;11:315. doi: 10.1186/1472-6963-11-315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kahabuka C, Moland KM, Kvåle G, Hinderaker SG. Unfulfilled expectations to services offered at primary health care facilities: Experiences of caretakers of underfive children in rural Tanzania. BMC Health Serv Res. 2012;12(158) doi: 10.1186/1472-6963-12-158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein T. Selecting therapies in Benin: making choices between informal, formal, private and public health services. Africa Spectrum. 2007:461–481. [Google Scholar]
- Knippenberg R, Nafo FT, Osseni R, Camara YB, Abassi EA, Soucat A. Increasing client’s power to scale up health services for the poor: the Bamako initiative in West Africa; background paper to the World Development Report. Washington: World Bank; 2003. [Google Scholar]
- Kredo T, Ford N, Adeniyi F, Garner P. Decentralising HIV treatment in lower- and middle-income countries (Review) The Cochrane Library. 2013:1–78. doi: 10.1002/14651858.CD009987.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kruk ME, Mbaruku G, McCord CW, Moran M, Rockers PC, Galea S. Bypassing primary care facilities for childbirth: a population-based study in rural Tanzania. Health Policy Plan. 2009;24:279–288. doi: 10.1093/heapol/czp011. [DOI] [PubMed] [Google Scholar]
- Labhardt ND, Sello M, Lejone T, Ehmer J, Mokhantso M, Lynen L, Pfeiffer K. Adoption of new HIV treatment guidelines and drug substitutions within first-line as a measure of quality of care in rural Lesotho: health centers and hospitals compared. Trop Med Int Health. 2012 doi: 10.1111/j.1365-3156.2012.03051.x. [DOI] [PubMed] [Google Scholar]
- Leonard KL, Mliga GR, Mariam DH. Bypassing health centers in Tanzania: revealed preferences for quality. Journal of African Economies. 2002;11:441–471. [Google Scholar]
- McGuire M, Pinoges L, Kanapathipillai R, Munyenyembe T, Huckabee M, Makombe S, Pujades-Rodriguez M. Treatment initiation, program attrition and patient treatment outcomes associated with scale-up and decentralization of HIV care in rural Malawi. PLoS One. 2012;7(10):e38044. doi: 10.1371/journal.pone.0038044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKinney M. Variations in rural AIDS epidemiology and service delivery models in the United States. Journal of Rural Health. 2002;18(3):455–466. doi: 10.1111/j.1748-0361.2002.tb00910.x. [DOI] [PubMed] [Google Scholar]
- Meredith LS, Orlando M, Humphrey N, Camp P, Sherbourne C. Are Better Ratings of the Patient-Provider Relationship Associated With Higher Quality Care for Depression? Med Care. 2001;39(4):349–360. doi: 10.1097/00005650-200104000-00006. [DOI] [PubMed] [Google Scholar]
- Mulamba D, Fullem A, Hirschhorn L, Allers C, Oser R, Rau B. Decentralizing Antiretroviral Treatment Services at Primary Health Care Facilities: A Guide to Expanding Access and Care in Resource-Limited, Generalized HIV Epidemic Settings. Arlington, VA: USAID; 2010. [Google Scholar]
- Mutemwa R, Mayhew S, Colombini M, Busza J, Kivunaga J, Ndwiga C. Experiences of health care providers with integrated HIV and reproductive health services in Kenya: a qualitative study. BMC Health Serv Res. 2013;13:18. doi: 10.1186/1472-6963-13-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nguyen T, Whetten K. Is Anybody Out There? Integrating HIV Services in Rural Regions. Public Health Reports. 2003;118(1):3–9. doi: 10.1093/phr/118.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nyogea D, Tanner M, Geubbels E, Hennings L, Stoeckle M, Mwaigomole G. Supply chain management in peripheral care and treatment centres (CTCs) in rural Tanzania: situational assessment; Paper presented at the 19th International AIDS Conference; Washington, DC. 2012. http://www.iasociety.org/Abstracts/A200744042.aspx. [Google Scholar]
- OpenMicroData. Tanzania: shapefiles for EAs, villages, districts and regions, 2002. 2013 Retrieved from: http://openmicrodata.wordpress.com/2010/12/16/tanzania-shapefiles-for-eas-villages-districts-and-regions/
- Pasquet A, Messou E, Gabillard D, Minga A, Depoulosky A, et al. Impact of Drug Stock-Outs on Death and Retention to Care among HIV-Infected Patients on Combination Antiretroviral Therapy in Abidjan, Côte d'Ivoire. PLoS One. 2010;5(10) doi: 10.1371/journal.pone.0013414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pence BW, Shirey K, Whetten K, Agala B, Itemba D, Adams J, Shao J. Prevalence of psychological trauma and association with current health and functioning in a sample of HIV-infected and HIV-uninfected Tanzanian adults. PLoS One. 2012;7(5):e36304. doi: 10.1371/journal.pone.0036304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- PEPFAR. [Cited: Feb 22, 2012];The United States President's Emergency Plan for AIDS Relief. Five-Year Strategy. 2009 http://www.pepfar.gov/strategy/document/133251.htm.
- Pfeiffer J, Montoya P, Baptista AJ, Karagianis M, Pugas Mde M, Micek M, Gloyd S. Integration of HIV/AIDS services into African primary health care: lessons learned for health system strengthening in Mozambique - a case study. J Int AIDS Soc. 2010;13:3. doi: 10.1186/1758-2652-13-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reif S, Golin C, Smith S. Barriers to Accessing HIV Care in North Carolina: Rural and Urban Differences. AIDS Care. 2005;17(5) doi: 10.1080/09540120412331319750. [DOI] [PubMed] [Google Scholar]
- Shapiro MF, Morton SC, McCaffrey DF, Senterfitt JW, Fleishman JA, Perlman JF, Bozzette SA. Variations in the care of HIV-infected adults in the United States: results from the HIV Cost and Services Utilization Study. JAMA. 1999;281(24):2305–2315. doi: 10.1001/jama.281.24.2305. [DOI] [PubMed] [Google Scholar]
- Shorter MM, Ostermann J, Crump JA, Tribble AC, Itemba DK, Mgonja A, Thielman NM. Characteristics of HIV voluntary counseling and testing clients before and during care and treatment scale-up in Moshi, Tanzania. J Acquir Immune Defic Syndr. 2009;52(5):648–654. doi: 10.1097/QAI.0b013e3181b31a6a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- TACAIDS. UNGASS Country Progress Reporting - Tanzania Mainland. 2012 Retrieved 30-Mar-2012, from http://www.unaids.org/en/dataanalysis/knowyourresponse/countryprogressreports/2012countries/ce_TZ_Narrative_Report[1].pdf.
- TACAIDS, Zanzibar AIDS Commission, National Bureau of Statistics, Office of the Chief Government Statistician, & ICF International. HIV/AIDS and Malaria Indicator Survey 2011–12. Dar es Salaam, Tanzania: Tanzania Commission for AIDS, ZAC, NBS, OCGS, and ICF International; 2013. [Google Scholar]
- Tembon AC. Health care provider choice: the North West Province of Cameroon. Int J Health Plan Manage. 1996;11:53–67. doi: 10.1002/(SICI)1099-1751(199601)11:1<53::AID-HPM413>3.0.CO;2-A. [DOI] [PubMed] [Google Scholar]
- The United Republic of Tanzania. 2012 Population and housing census. Population distribution by administrative areas. Dar es Salaam and Zanzibar, Tanzania: National Bureau of Statistics, Ministry of Finance, Office of Chief Government Statistician; 2013. [Google Scholar]
- Thielman NM, Ostermann J, Whetten K, Whetten R, Itemba DK, Maro V, Reddy E. Reduced Adherence to Antiretroviral Therapy among HIV-infected Tanzanians Seeking Cure from the Loliondo Healer. J Acquir Immune Defic Syndr, forthcoming. 2013 doi: 10.1097/01.qai.0000437619.23031.83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Topp SM, Chipukuma JM, Chiko MM, Matongo E, Bolton-Moore C, Reid SE. Integrating HIV treatment with primary care outpatient services: opportunities and challenges from a scaled-up model in Zambia. Health Policy Plan. 2013;28(4):347–357. doi: 10.1093/heapol/czs065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tran B, Nguyen N. Patient satisfaction with HIV/AIDS care and treatment in the decentralization of services delivery in Vietnam. PLoS One. 2012;7(10) doi: 10.1371/journal.pone.0046680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Uebel KE, Joubert G, Wouters E, Mollentze WF, van Rensburg DH. Integrating HIV care into primary care services: quantifying progress of an intervention in South Africa. PLoS One. 2013;8(1):e54266. doi: 10.1371/journal.pone.0054266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whetten K, Pence BW. You’re the First One I’ve Told: Faces of HIV in the Deep South. New Jersey: Rutgers University Press; 2013. [Google Scholar]
- Whetten K, Reif S, Whetten R, Murphy-McMillan LK. Trauma, Mental Health, Distrust, and Stigma Among HIV-Positive Persons: Implications for Effective Care. Psychosomatic Medicine. 2008;70(5):531–538. doi: 10.1097/PSY.0b013e31817749dc. [DOI] [PubMed] [Google Scholar]
- Whetten R, Whetten K, Pence BW, Reif S, Conover C, Bouis S. Does distance affect utilization of substance abuse and mental health services in the presence of transportation services? AIDS Care. 2006;181(Suppl):S27–S34. doi: 10.1080/09540120600839397. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Global update on HIV treatment 2013: results, impact and opportunities. Geneva, Switzerland: 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.