Abstract
Objective
To assess cognitive functioning in children with type 1 diabetes (T1D) and examine whether glycemic history influences cognitive function.
Research Design and Methods
Neuropsychological evaluation of 216 children (healthy controls, n = 72; T1D, n = 144) ages 4-10yrs across five DirecNet sites. Cognitive domains included IQ, Executive Functions, Learning and Memory, and Processing Speed. Behavioral, mood, parental IQ data and T1D glycemic history since diagnosis were collected.
Results
The cohorts did not differ in age, gender or parent IQ. Median T1D duration was 2.5yrs and average onset age was 4yrs. After covarying age, gender, and parental IQ, the IQ and the Executive Functions domain scores trended lower (both p = .02, not statistically significant adjusting for multiple comparisons) with T1D relative to controls. Children with T1D were rated by parents as having more depressive and somatic symptoms (p < 0.001). Learning and memory (p = 0.46) and processing speed (p = 0.25) were similar. Trends in the data supported that the degree of hyperglycemia was associated with Executive Functions, and to a lesser extent, Child IQ and Learning and Memory.
Conclusions
Differences in cognition are subtle in young children with T1D within 2 years of onset. Longitudinal evaluations will help determine whether these findings change or become more pronounced with time.
Keywords: cognition, early onset, T1DM, hyperglycemia, hypoglycemia, children
Young children with type 1diabetes are particularly prone to experiencing extreme fluctuations in glucose levels at a time when the developing brain is undergoing wide ranging maturational changes (Giedd & Rapoport, 2010). White matter proliferation, neuronal pruning and refining of neuronal networks are all actively occurring in childhood (Bullmore & Sporns, 2012). Several studies assessing cognition in youth with early onset diabetes (EOD) have shown worse outcomes across a variety of cognitive domains, principally IQ (Northam et al., 1998; Rovet, Ehrlich, & Hoppe, 1987), executive functions (Bjorgaas, Gimse, Vik, & Sand, 1997; Flykanaka-Gantenbein, 2004; Lin, Northam, Rankins, Werther, & Cameron, 2010; Ly, Anderson, McNamara, Davis, & Jones, 2011), learning and memory (Gaudieri, Chen, Greer, & Holmes, 2008; Lin et al., 2010), and processing speed (Lin et al., 2010; Northam et al., 2001; Ryan, Vega, & Drash, 1985).
Many, but not all studies of adults and children with childhood-onset type 1diabetes (T1D) have documented an association between severe hypoglycemia (with seizures or loss of consciousness) and either poorer cognitive outcomes (Blasetti et al., 2011; Hershey, Craft, Bhargava, & White, 1997; Hershey, Lillie, Sadler, & White, 2003, 2004; Hershey et al., 2005; Lin et al., 2010; Naguib, Kulinskaya, Lomax, & Garralda, 2009; Northam et al., 2001; Perantie et al., 2008; Rovet & Ehrlich, 1999)or brain changes (Ferguson et al., 2003; Haumont, Dorchy, & Pelc, 1979; Hyllienmark, Maltez, Dandenell, Luvigsson, & Brismar, 2005; Musen et al., 2006; Northam et al., 2009; Perantie et al., 2011; Perantie et al., 2007; Perros, Deary, Sellar, Best, & Frier, 1997). There is preliminary evidence to suggest that this association can be detected quite early in young children and youth with recent onset diabetes (Aye et al., 2011). On the other hand, results from the Diabetes Control and Complications Trial (DCCT) long-term follow-up study showed no effect of severe hypoglycemia history on cognitive function in adults with T1D, even in the youngest age subgroup (ages 13-18 at study entry), who were carefully followed for an average of 18 years (The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group, 2007). However, the DCCT cohort may not be entirely representative of the T1D population. For example, approximately 83% of DCCT participants had no severe hypoglycemic episodes in their past, and, due to exclusion criteria, no subject had more than two severe episodes in the two years prior to enrollment or evidence of hypoglycemia unawareness.
Chronic hyperglycemia exposure may also affect the brain, targeting both grey and white matter. Compared to hypoglycemia, however, there is less information on the effects of hyperglycemia on the developing brain. Greater hyperglycemia exposure has been associated with abnormal grey and white matter volumes (Perantie et al., 2011; Perantie et al., 2007), decrements in processing speed (Jacobson et al., 2011) and verbal intelligence (Perantie et al., 2008).
This study was designed to investigate cognitive effects of T1D in young children (4 to <10 years old) as compared with healthy controls, and to characterize the influence of intensity and frequency of fluctuations in glucose levels (glycemic excursions) on cognitive functioning in children with T1D. Novel aspects of this study include capture of a young cohort with relatively recent disease duration, careful control of possible influencing factors including parental IQ and mood status, as well as concurrent collection and analysis of neuroimaging data including DTI and whole brain morphometry using voxel-based morphometry (VBM). The neuroimaging results are reported in full elsewhere (Barnea-Goraly N et al., 2013; Marzelli et al., 2013)
Our cohort offers unique insights to the earliest impact of dysglycemia on cognition. We hypothesized that cognitive differences would be observed in all key domains: IQ, executive functions, memory, and processing speed. We hypothesized further that degree of cognitive differences would be associated with level of dysglycemia.
Research Design and Methods
This study was conducted across the five clinical centers of the Diabetes Research in Children Network (DirecNet) after review and approval by local Institutional Review Boards and the NIH-designated Data Safety Monitoring Board (DSMB). Parents or guardians provided written informed consent, and children of appropriate age (as per local Institutional Review Board) also provided assent. These data represent a portion of baseline evaluation conducted as part of a larger longitudinal study that includes neuroimaging. Children between 4 and < 10 years of age with T1D diagnosed prior to age 8 and healthy control participants were recruited. Eligibility criteria for the T1D participants included onset of T1D after 6 months of age and use of daily insulin therapy for at least 1 month. For all participants exclusion criteria were as follows: preterm birth prior to 34 weeks gestation, low birth weight (less than 2000 grams), intellectual or learning disability (based on parent-report), prior inpatient psychiatric treatment or any neurologic disease not related to diabetes. Control participants included siblings and community volunteers. Recruitment was monitored and suspended as needed in order to achieve a balance (within 10%) of T1D participants and control participants by the following age groups (4-<5, 5-<6, 6-<7, 7-<8, 8-<9, and 9-<10 years) and by gender. Eligibility criteria for the healthy controls included HbA1c < 6.0% (42 mmol/mol), fasting blood glucose (BG) < 110mg/dL, and for siblings of T1D participants, documented negative pancreatic autoantibodies (ICA, anti-insulin, anti-GAD). Target sample sizes after adjusting for attrition and missing data were 140 participants with T1D and 70 healthy controls to detect an effect size of 0.5 for each cognitive domain.
Participants
A total of 144 participants with T1D and 72 healthy controls participated in the study. Average age was 7 years for both groups (range 4.0 to < 10 years). The T1D and control groups had similar gender distributions, parent education and income levels (Table 2). The T1D cohort had a median duration of diabetes of 2.5 years, ranging from 0.1 to 7.9 years. Among children with T1D 16% (n = 23) had a history of at least one episode of severe hypoglycemia and 36% (n = 51) had a history of diabetic ketoacidosis (DKA), mostly at the time of diagnosis.
Table 2.
Demographics by Group
| T1D participants (N = 144) | Control participants (N = 72) | |
|---|---|---|
| Age (years) | ||
| mean ± SD | 6.96 ± 1.68 | 6.92 ± 1.79 |
| Range | 4.00 to 9.99 | 4.06 to 9.97 |
| Female | 66 (46%) | 34 (47%) |
| Race/Ethnicity | ||
| White | 117 (81%) | 62 (86%) |
| Hispanic or Latino | 10 (7%) | 4 (6%) |
| African American | 6 (4%) | 4 (6%) |
| Asian | 2 (1%) | 0 |
| More than one race | 9 (6%) | 2 (3%) |
| BMI percentile median (25th, 75th percentile) | 72% (58%, 87%) | 61% (35%, 82%) |
| Diabetes duration (years) | ||
| median (25th, 75th percentile) | 2.5 (1.2, 4.4) | NA |
| Range | 0.1 to 7.9 | |
| Age at onset (yrs) mean ± SD | 4.1 ± 1.9 | NA |
| Range | 0.9 - 8.0 | |
| Severe Hypoglycemia History a N (%) | 23 (16%) | NA |
| HbA1c (%) (mmol/mol) at enrollment | ||
| mean ± SD | 7.9 ± 0.9 (63 ± 10) | 5.2 ± 0.2 (33 ± 2) |
| Range | 6.3 to 10.2 (45 to 88) | 4.7 to 5.8 (28 to 40) |
| Parent History of Diabetesb N (%) | 21 (15%) | 9 (13%) |
| Relative with Diabetesc N (%) | NA | 31 (43%) |
| Sibling of a Type 1 Diabetes Subject in Study N(%) | NA | 18 (25%) |
| Parent Education Leveld N (%) | ||
| < 12th Grade | 1 (< 1%) | 1 (1%) |
| 12th Grade | 20 (14%) | 4 (6%) |
| Associates | 23 (16%) | 7 (10%) |
| Bachelors | 45 (31%) | 24 (33%) |
| Masters | 36 (25%) | 24 (33%) |
| Professional | 19 (13%) | 12 (17%) |
| Parent Income levele N (%) | N = 134 | N = 66 |
| Less than $25,000 | 11 (8%) | 2 (3%) |
| $25,000 to $49,999 | 23 (17%) | 10 (15%) |
| $50,000 to $99,999 | 51 (38%) | 24 (36%) |
| $100,000 to $199,999 | 34 (25%) | 22 (33%) |
| $200,000 or more | 15 (11%) | 8 (12%) |
| Verbal IQ f | ||
| mean ± SD | 108 ± 14 | 112 ± 12 |
| Range | 74 to 150 | 86 to 147 |
| Performace IQ f | ||
| mean ± SD | 109 ± 15 | 112 ± 15 |
| Range | 73 to 143 | 84 to 148 |
Includes 18 participants with one episode, 3 with two, 1 with three and 1 with five episodes.
Among 21 T1D participants, 11 reported T1D and 10 reported T2D; among 9 HC participants, 4 reported T1D and 5 reported T2D. Excludes 3 T1D participants for whom the biological parents’ information was not available.
Only HC participants were asked if they had relative with T1D. Eight participants reported T1D siblings who are not in the study, 3 reported parent, 1 reported grandparent and 1 reported first-cousin with T1D.
Highest of primary and secondary care givers.
Excludes 10 T1D and 6 HC participants who selected ‘do not know’ or ‘do not want to answer’.
1 HC subject has missing IQ test
Glycemic control
For the T1D participants, available HbA1c levels were obtained from medical records. History of severe hypoglycemia since the time of diagnosis was obtained from parent report. Severe hypoglycemia was defined as requiring assistance of another person to actively administer carbohydrate, glucagon, or other resuscitative actions due to altered consciousness. T1D participants wore a continuous glucose monitor (CGM) to collect a minimum of 72 hours of glycemic data with at least 24 hours of overnight data collection. For those participants who were using a CGM for routine management of their diabetes, the CGM data were collected from their own CGM. For those not using a CGM for management purposes, an iPro2 (Medtronic MiniMed, Inc., Northridge, CA) or DexCom SEVEN Plus (DexCom, Inc., San Diego, CA) was provided to the participant at no cost. The study devices were blinded, meaning that the participant did not have access to the CGM results in real time. The median (interquartile range) of CGM use was 93 (83, 107) hours during daytime (6 am – 10 pm), and 48 (42, 56) hours during nighttime.
Neurocognitive testing
An age-appropriate neurocognitive battery was administered by trained personnel certified by the DirecNet neurocognitive core (T. Hershey and A. Cato). Standard neuropsychological age-specific measures and behavioral questionnaires were used to derive cognitive, mood, and behavioral domains of interest. Domains assessed in the children included IQ, Executive Functions, Learning and Memory, Processing Speed, parent-reported executive functioning, externalizing behavior, and internalizing mood symptoms (Table 1). The assignment of tasks to each cognitive domain was based on clinical experience. A parent/guardian also completed an abbreviated IQ measure. On an a priori basis, the cognitive domains were considered primary outcomes; the parent-reported measures of mood and behavior were considered secondary outcomes; and parent IQ was selected as a planned covariate.
Table 1.
Neurocognitive Test Battery: Domains and Measures
| Cognitive Domain | Measurea | Test | Batteryb |
|---|---|---|---|
| IQ | scaled scoree | Block design | WPPSI3 / WASI |
| scaled scoree | Similarities | ||
| scaled scoree | Vocabulary | ||
| scaled scoree | Matrix reasoning | ||
| Executive Functions | Detectability | CPT2 | Connor's |
| Total Correct | Auditory Attn | NEPSYII | |
| Total Correct | Concept Formation | WJIII Cognitive | |
| Total Correct | Numbers | CMS | |
| Learning & Memory | Total items recalled | Word Listsc | CMS |
| Total items recalled | Dot Locationsc | CMS | |
| Processing Speed | standard scored | Visual Match I / II | WJIII Cognitive |
| Decision Speed | WJIII Cognitive |
| Mood/Behavior | Measure | Scale | Battery |
|---|---|---|---|
| Executive functioning | Raw score | Global Executive Composite | BRIEF Parent |
| Externalizing symptoms | T score | Externalizing | BASCII PRS |
| Internalizing symptoms | T score | Internalizing | BASCII PRS |
| Covariate | Measure | Test | Battery |
|---|---|---|---|
| Parent IQ | scaled scoree | Vocabulary | WASI |
| scaled scoree | Matrix Reasoning |
z score was calculated for each measure using mean and SD from the current study pooling all participants (N=214). For domains with more than one test, the average was taken giving equal weight to each z score.
Abbreviations: CMS – Children's Memory Scale (Cohen, 1997); CPT – Continuous Performance Test (Connors, 1994); NEPSYII – Neuropsychological Battery for Children, Second Edition (Korkman, Kirk, & Kemp, 2007); WJIII Cognitive – Woodcock-Johnson Test of Cognitive Abilities, Third Edition (Woodcock, McGrew, & Mather, 2001); WPPSI3–Wechsler Preschool and Primary Scales of Intelligence, Third Edition (Wechsler, 2002); WASI-Wechsler Adult Scale of Intelligence (Wechsler, 1999); BRIEF – Behavior Rating Inventory of Executive Functions (Gioia, Isquith, Guy, & Kenworthy, 2000); BASCII PRS – Behavior Assessment System for Children, Second Edition Parent Rating Scales (Reynolds & Kamphaus, 2004).
Same version given regardless of age.
Age-based standard score from WJIII Cognitive normative update (NU) sample
Age-based scaled score derived from Wechsler normative sample
For T1D participants, at the time of neurocognitive testing BG concentrations needed to be between 70 and 300 mg/dL. During testing they were monitored for symptoms of hypoglycemia and BG levels were assessed at least twice at regular, planned intervals, by fingerstick on a home glucose meter. Insulin or food was given to titrate BG levels as needed. Ketones were evaluated in cases of BG > 300 mg/dL and if positive, testing was postponed. Testing was also suspended if BG dropped < 70, and resumed only when BG again read within 70-300 mg/dl. Test protocols were double scored at a centralized location (Washington University in St. Louis), and the results were then analyzed at the DirecNet Coordinating Center (Jaeb Center for Health Research, Tampa, FL).
Statistical Methods
A z-score was calculated for each measure using mean and SD from the current study pooling all participants (N = 214) (Manschot et al., 2006; van den Berg et al., 2010). The calculations were based on ranks using van der Waerden scores to account for some skewness in the distributions. For domains with more than one measure, the composite z-score was taken as an average giving equal weight to each z-score. Domain scores were omitted in participants who did not complete all sub-domain measures. Repeated measures least squares regression models were used to account for the possibility that outcomes from siblings may be correlated. These models compared children with versus without T1D on each of the domains and subdomain measures adjusting for age, gender, and parent IQ. The parent-reported child depression score was used as an additional covariate for subdomain analyses as presence of depressive symptoms can have a deleterious effect on cognition (Murrough, Iacoviello, Neumeister, Charney, & Iosifescu, 2011).
Primary outcome domains were pre-defined as Delayed Memory, Executive Functions, Processing Speed and IQ. Secondary outcomes included parent ratings of executive functioning, externalizing behavior symptoms and internalizing mood symptoms. Upon inspection of the data, a ceiling effect was observed for the Delayed Memory domain. This domain was therefore replaced with the domain of Learning and Memory using subdomain measures that did not exhibit any ceiling effect in the results. Because this was not a pre-specified domain, it is considered a secondary outcome in this analysis. All p-values presented in this manuscript are nominal p-values without correction for multiple comparisons. For the four primary domains, the Hochberg step up approach (Hochberg, 1988) was used to adjust the threshold defining statistical significance to account for multiple comparisons. No formal correction for multiple comparisons was made for the other secondary domains. Effect sizes were calculated for individual subdomains based on the estimated difference and standard error from a regression model adjusting for the factors mentioned above. Subdomain analyses were considered secondary and p-values were only calculated for the composite domains to mitigate the problem of multiple comparisons.
Within the T1D cohort, additional exploratory analyses were performed using variables specific to diabetes to characterize the influence of glycemic excursions on cognitive functioning. Hyperglycemia exposure was estimated by creating a hyperglycemic index from all available HbA1c measurements, calculating the incremental area under the curve (AUC) above an HbA1c level of 6.0% (42 mmol/mol) using the trapezoid rule. The median (interquartile range) for total number of HbA1c measurements was 11 (6, 18) overall and 4 (4, 6) measurements per year. CGM indices (mean glucose, % readings in target range, % readings in hypoglycemic range, coefficient of variation [CV]) were calculated giving equal weight to each of the 24 hours of the day (Diabetes Research in Children Network Study Group, 2007). Other diabetes-specific variables included age of onset, duration of diabetes, and presence or absence of severe hypoglycemia history. Spearman partial correlations were conducted between these variables and each of the cognitive domains, adjusting for age, gender and parent IQ. No formal correction was made for the large number of statistical comparisons arising from combinations of each of these factors with the cognitive data. P-values above 0.01 were not considered statistically significant.
Results
Primary Outcomes
Covarying for age, gender, and parent IQ, there were trends for children with T1D to score lower than age-matched controls in the domains of IQ and Executive Functions (both p = .02, not statistically significant adjusting for multiple comparisons). There was no significant difference between groups for Processing Speed (p = .25, Table 3).
Table 3.
Comparison of T1D and HC participants on cognition, behavior and mood.
| N | T1D participants Mean ± SD | N | Control participants Mean ± SD | p-valuea | |
|---|---|---|---|---|---|
| Z- Scores | |||||
| IQb | 144 | −0.09 ± 1.01 | 70 | +0.19 ± 0.89 | 0.02a |
| Executive Functionsb | 135 | –0.07 ± 0.96 | 70 | +0.14 ± 1.00 | 0.02a |
| Learning and Memoryb | 142 | –0.01 ± 0.97 | 71 | +0.03 ± 1.01 | 0.46a |
| Processing Speedb | 140 | +0.04 ± 1.02 | 72 | –0.07 ± 0.89 | 0.25a |
| BRIEF (Behavior Rating Inventory of Executive Function by Parent)c | 140 | +0.06 ± 0.92 | 68 | –0.12 ± 1.08 | 0.26a |
| Externalizing (Behavior Assessment by Parent)c | 144 | +0.03 ± 0.96 | 70 | –0.07 ± 1.01 | 0.73a |
| Internalizing (Behavior Assessment by Parent)c | 144 | +0.19 ± 0.90 | 69 | –0.40 ± 1.02 | <0.001a |
Nominal p-value uncorrected for multiple comparisons. Obtained from repeated measures least squares regression models, adjusted for siblings from same family, age, gender, and parent IQ.
Higher scores are better.
Higher scores are worse.
Secondary Outcomes
Learning and memory (p = .46) did not differ between the groups. Parents reported more internalizing problems in children with T1D (p < .001). Level of externalizing problems (p = .73), parent-reported executive functioning problems (p = .26) did not differ between the groups.
Sub-domain analyses
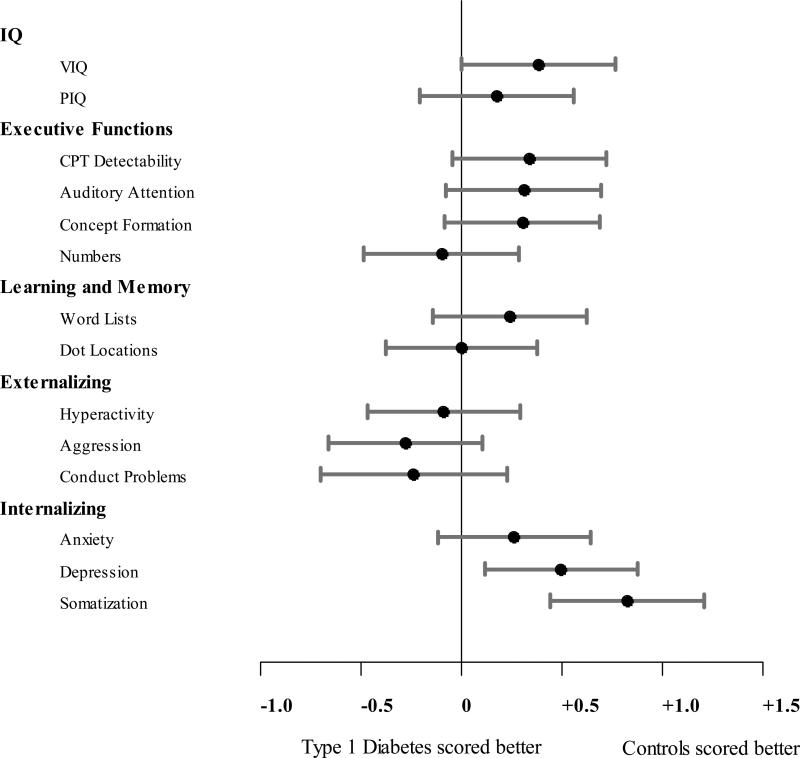
Within the internalizing domain, parents of children with T1D reported higher levels on sub-domains of depression, somatization, and anxiety (Figure 1). Subsequent sub-domain analyses included level of parent-reported child depression as an additional covariate to ensure that changes in cognitive function were not impacted by degree of depressive symptoms. Within the executive functions domain, additionally covarying for depression, all sub-domain measures but one (CMS Numbers) differed between the groups. In children with T1D, scores trended lower on measures of visual sustained attention (effect size = 0.34), auditory sustained attention (effect size = 0.31) and novel concept formation (effect size = 0.30). Scores also trended lower in children with T1D for both verbal (effect size = .38) and performance IQ (effect size = .17) as well as verbal (effect size = 0.24) but not visual learning and memory (effect size = −0.001).
Relationship to glycemic variables
Within the T1D group, children with a history of DKA and severe hypoglycemia (DKA & SH, N = 12) trended as having lower scores on the IQ measure (p = 0.06) relative to those with no history of either DKA or SH (Table 4). Trends were also observed across several indices in the direction of a deleterious effect of hyperglycemia on IQ, Executive Functions, and Learning and Memory. Trends included the hyperglycemic index based on all HbA1c values. Chronic hyperglycemia indexed by averaged A1c AUC above 6.0% (see methods) was associated with lower Child IQ (p = 0.05) and Learning and Memory (p = 0.05) domain scores (Table 5). From the CGM data, T1D cases with a higher percentage of euglycemia (glucose values between 71 and 180 mg/dL) had higher scores within the Executive Functions domain (p = 0.01) (Table 6). Trends included that hyperglycemia was associated with lower scores on the Executive Functions domain, such that the percentage of time blood glucose values were above 180 mg/dL was associated with a lower Executive Functions domain score (p = 0.04). A final trend was that a higher mean glucose score was associated with a lower Executive Functions domain score (p = 0.03).
Table 4.
Cognitive outcomes by DKA and severe hypoglycemia.
| N | Child IQ mean ± SD | Executive Functions mean ± SD | Learning and Memory mean ± SD | Processing Speed mean ± SD | |
|---|---|---|---|---|---|
| Z- Scores | |||||
| Non-Diabetic | 72 | +0.19 ± 0.89 | +0.14 ± 1.00 | +0.03 ± 1.01 | −0.07 ± 0.89 |
| T1D | 144 | –0.09 ± 1.01 | –0.07 ± 0.96 | –0.01 ± 0.97 | +0.04 ± 1.02 |
| DKA history | |||||
| Severe | 13 | –0.33 ± 0.88 | –0.16 ± 0.64 | –0.31 ± 0.73 | +0.07 ± 0.98 |
| Moderate | 38 | –0.30 ± 0.81 | –0.25 ± 0.84 | +0.02 ± 0.96 | –0.09 ± 1.05 |
| None | 91 | +0.06 ± 1.07 | +0.03 ± 1.03 | +0.03 ± 0.99 | +0.10 ± 1.03 |
| p-valuea | 0.37 | 0.64 | 0.47 | 0.58 | |
| SH history | |||||
| Seizure/Coma | 12 | –0.49 ± 0.92 | –0.43 ± 0.56 | –0.39 ± 0.64 | –0.42 ± 0.86 |
| SH without seizure/coma | 11 | –0.39 ± 0.77 | –0.19 ± 1.01 | +0.45 ± 0.77 | +0.34 ± 0.96 |
| None | 121 | –0.03 ± 1.03 | –0.03 ± 0.99 | –0.02 ± 1.00 | +0.05 ± 1.04 |
| p-valuea | 0.37 | 0.24 | 0.20 | 0.24 | |
| DKA & SH combination | |||||
| DKA & SH | 12 | –0.69 ± 0.84 | –0.26 ± 0.83 | +0.13 ± 0.68 | +0.02 ± 1.24 |
| DKA only | 39 | –0.19 ± 0.79 | –0.22 ± 0.80 | –0.11 ± 0.97 | –0.08 ± 0.98 |
| SH only | 11 | –0.17 ± 0.78 | –0.37 ± 0.82 | –0.07 ± 0.95 | –0.10 ± 0.66 |
| No DKA/SH | 80 | +0.09 ± 1.10 | +0.09 ± 1.05 | +0.05 ± 1.00 | +0.13 ± 1.07 |
| p-valuea | 0.06 | 0.19 | 0.80 | 0.99 | |
p-value from generalized least square regression models, adjusted for age, gender and parent IQ, diabetes duration and incremental AUC above HbA1c level of 6.0%. Statistical comparison is made between the two most extreme groups (i.e., severe vs. none for DKA history, seizure/coma vs. none for SH history, DKA & SH vs. No DKA/SH for combination).
Table 5.
Cognitive outcomes by diabetes history among T1D subjectsa
| Child IQ | Executive Functions | Learning and Memory | Processing Speed | |
|---|---|---|---|---|
| Averaged A1c AUC above 6.0% | ||||
| Correlation | −0.17 | −0.15 | −0.17 | +0.04 |
| p-value | 0.05 | 0.10 | 0.05 | 0.63 |
| N | 140 | 131 | 138 | 136 |
| Diabetes Duration | ||||
| Correlation | −0.06 | −0.02 | +0.07 | −0.12 |
| p-value | 0.47 | 0.78 | 0.41 | 0.16 |
| N | 140 | 131 | 138 | 136 |
| Age at onset (yrs) | ||||
| Correlation | +0.05 | +0.04 | −0.04 | +0.09 |
| p-value | 0.54 | 0.67 | 0.64 | 0.30 |
| N | 140 | 131 | 138 | 136 |
Results from Spearman partial correlations controlling for age, gender, and parent IQ.
Table 6.
Cognitive outcomes by glycemic indices measured by CGM data among T1D subjectsa
| Child IQ | Executive Functions | Learning and Memory | Processing Speed | |
|---|---|---|---|---|
| % Glucose in Target Range (71-180 mg/dL) | ||||
| Correlation | +0.13 | +0.22 | +0.01 | −0.09 |
| p-value | 0.13 | 0.01 | 0.91 | 0.32 |
| N | 140 | 131 | 138 | 136 |
| % Glucose in Hypoglycemia (<70 mg/dL) | ||||
| Correlation | −0.09 | +0.04 | +0.08 | −0.04 |
| p-value | 0.29 | 0.62 | 0.34 | 0.66 |
| N | 140 | 131 | 138 | 136 |
| % Glucose in Hyperglycemia (above 180 mg/dL) | ||||
| Correlation | −0.09 | −0.19 | −0.02 | +0.10 |
| p-value | 0.31 | 0.04 | 0.79 | 0.27 |
| N | 140 | 131 | 138 | 136 |
| Glucose Coefficient of Variation (SD/mean) | ||||
| Correlation | −0.12 | +0.02 | +0.05 | −0.05 |
| p-value | 0.16 | 0.86 | 0.60 | 0.59 |
| N | 140 | 131 | 138 | 136 |
| Mean Glucose | ||||
| Correlation | −0.10 | −0.20 | −0.05 | +0.07 |
| p-value | 0.26 | 0.03 | 0.58 | 0.45 |
| N | 140 | 131 | 138 | 136 |
Results from Spearman partial correlations controlling for age, gender, and parent IQ.
Discussion
In this cohort of young children with T1D, trends towards cognitive differences were observed relative to controls in the areas of intellectual ability and executive functions (both p = .02) after accounting for parent IQ and level of parent-reported depression. These findings are subtle and did not meet our threshold for statistical significance. The clinical significance of the findings is uncertain, given the modest effects. Nonetheless, the findings are in keeping with Aye et al. (Aye et al., 2011). Together, results suggest that cognitive differences may emerge in young children with T1D, even after relatively short disease duration. Mood differences were identified in the form of more somatic, depressive, and anxious symptoms. The mood differences observed in this young cohort are consistent with extant literature, particularly during the time around diagnosis (Kovacs, Goldston, Obrosky, & Bonar, 1997).
One could surmise that we did not find more pronounced cognitive differences because of the high functioning nature of our cohort. Baseline IQ findings in the Lin et al. 2010 study, however, were quite similar (Average FSIQ of 108 for T1D patients and 110 for Controls). That said, it is possible that cognitive differences might be identified earlier or in a more pronounced fashion in the overall population of children with type 1 diabetes. An additional possibility is that our test battery was not sufficiently sensitive to detect cognitive differences. Tests in wide clinical use were selected for this protocol. It is possible that use of tasks from the experimental or cognitive literature (e.g., Hershey's spatial delayed memory task) might have yielded more robust findings.
In keeping with the benefits of euglycemia on the developing brain, T1D youth in this cohort who spent more time in euglycemia performed better on measures of executive functions. Further, trends in the data suggested a deleterious effect of hyperglycemia on executive functions. Overall, however, associations between dysglycemia and cognition did not meet our threshold for statistical significance. We suspect that the relationship between cognitive findings and glycemic variables may become more easily detectable after longer disease duration or in children of an older age. Indeed, in other prospective studies in which a relationship between glycemic variables and cognitive functions were reported, the cohorts included older children. Northam et al. (Northam, Anderson, Werther, Warne, & Andrewes, 1999), who studied children at the time of diagnosis and 2 years following disease onset, found significant relationships between cognitive findings (executive functions of auditory attention, working memory; and verbal and visual learning and memory) and both chronic hyperglycemia and recurrent severe hypoglycemia. It is important to note, however, that these associations were confined to the older children in the cohort within the age range of 7 to 14. Likewise, Hershey et al. (Hershey et al., 2005) reported a relationship between repeated (≥ 3 episodes) severe hypoglycemia and spatial memory performance. This combined cohort consisted of an older age group, ages 6-18. Hershey and colleagues reported the finding once more in a prospective study (Perantie et al., 2008) with a cohort ranging in age from 5 to 16 with similar findings of relationship between spatial memory and hypoglycemia. In these reports, findings were most pronounced in older children with early diabetes onset (< 5 years) and longer disease duration.
With longer disease duration, a larger variety of cognitive differences have been reported by Northam and by Hershey, among others, including the domains of verbal intellectual ability, working memory, and processing speed. After 12 years of disease duration, risk factors of EOD, severe hypoglycemia and poor metabolic control (hyperglycemia) were found to be additive, particularly for verbal IQ subtests and executive functioning tasks (Lin et al., 2010). These previous findings related to verbal IQ are particularly interesting in light of trends towards lower verbal IQ and lower verbal learning and memory functioning in our cohort of young children with T1D.
It is possible that early CNS insult in the form of either severe DKA or SH (with seizure/coma) could have a delayed impact on cognition such that with time, the disparity in cognitive scores could grow larger. Likewise, individuals with less severe CNS insult but with glycemic dysregulation may show cumulative impact over time or delayed onset of cognitive deficits. A clinical correlate is noted in young children treated with cranial radiation therapy (RT). The cumulative impact of RT and chemotherapy on young children's cognitive outcomes emerges over time as revealed in the late effects literature (Yeates, Ris, Taylor, & Pennington, 2010).
One purported mechanism to explain these conclusions is that damage to white matter development and proliferation results in neurocognitive deficits. Likewise, CNS insult to children with EOD may have a delayed, progressive and cumulative impact on cognition over time. Concurrent baseline neuroimaging analysis performed by our DirecNet study group with this cohort supports the hypothesis that white matter disruption has occurred at this early stage in disease progression. Using DTI, white matter integrity differences were found such that in our cohort, children with T1D had reduced axial diffusivity (AD) in multiple widespread brain regions when compared with controls. Within the T1D group, earlier onset of diabetes, longer disease duration, and higher HbA1c values significantly influenced white matter findings (Barnea-Goraly N et al., 2013). In addition, our group used whole brain structural analysis (VBM) to reveal group differences in this young cohort including decreased gray matter volume (GMV) in several posterior regions and increased GMV in regions within the temporal and prefrontal cortices. Again, dysglycemia was significantly related to the observed brain structure differences (Marzelli et al., 2013).
In summary, cognitive differences are subtle in young children with T1D at relatively short disease duration (2.5 years on average). These results lead us to hypothesize that the identified trends towards group differences are likely related to the impact of glycemic variability on the developing brain, and over time, the effects become more pronounced and thus, more easily detected. Longitudinal follow up of this cohort will better characterize any association of these cognitive changes with dysglycemia.
Important next steps in our cohort of young children are to determine whether these differences become more pronounced over time and to determine whether stronger relationships emerge between observed cognitive differences and glycemic variables. Further, cognitive testing along with concurrent neuroimaging studies over time will help reveal if dynamic changes in brain systems, such as perturbations in white matter proliferation during this time frame, relate to the observed cognitive findings in children with T1D.
Figure 1. Estimated effect sizes for cognitive subdomains.
The dot represents the point estimate and the width of the bars represents a 99% confidence interval. The confidence intervals are not otherwise corrected for multiple comparisons. For the domains of Executive Functions, IQ, and Learning and Memory, effect sizes to the right of the vertical line indicate that the control group scored higher. For Externalizing and Internalizing domains, scores are reversed such that effect sizes to the right of the vertical line indicate that the control group had less symptoms.
Acknowledgements
We would like to thank all the participants and their families for their participation. This research was supported by funding from Jaeb Center for Health Research and the NIH (DIRECNET U01 HD41890, HD41890-10, HD41906-10, HD41908-10, HD41915, HD41918, HD56526) and UL1 RR024992. A.Cato, N. Mauras, C. Kollman, P. Cheng, R. Beck, K. Ruedy, J. Ambrosino and T. Aye, have no relevant conflict of interest to disclose. T. Hershey reports receiving payment for consultancy for an NIH grant review, payment from Washington University as a faculty member, and payment for work on the Scientific Advisory board for the Tourette Syndrome Association. She also reports money paid to her institution from the NIH for a pending grant. A. Reiss reports money paid to his institution from the NIH for a pending grant. A. Conrad reports receiving payment from the University of Iowa for time conducting evaluations. N. White reports receiving payment for consultancy from Novo Nordisk and Daiichi Sankyo.
Prior presentation of study data occurred at the American Diabetes Association meeting in Philadelphia in June, 2012. The information in this manuscript has never been published either electronically or in print.
Footnotes
The DirecNet Study Group: Clinical Centers: (Personnel are listed as (PI) for Principal Investigator, (I) for co-Investigator and (C) for Coordinators.) Department of Pediatrics, University of Iowa Carver College of Medicine, Iowa City, IA: Eva Tsalikian, MD (PI); Michael J. Tansey, MD (I); Julie Coffey, MSN (C); Joanne Cabbage (C); Sara Salamati (C); Nemours Children's Clinic, Jacksonville, FL: Nelly Mauras, MD (PI); Larry A. Fox, MD (I); Allison Cato, PhD; (I); Kim Englert, RN, BSN, CDE (C); Kaitlin Sikes, ARNP, MSN (C); Tina Ewen (C); Division of Pediatric Endocrinology and Diabetes, Stanford University, Stanford, CA: Bruce A. Buckingham, MD (PI); Darrell M. Wilson, MD (I); Tandy Aye, MD (I); Kimberly Caswell, ARNP (C); Department of Pediatrics, Yale University School of Medicine, New Haven, CT: Stuart A. Weinzimer, MD (PI); William V. Tamborlane, MD (I); Amy Steffen, BS (C); Kate Weyman, MSN (C); Melinda Zgorski, BSN (C) ; Washington University in St. Louis, St. Louis, MO: Neil H. White, MD, CDE (PI); Ana Maria Arbelaez, MD, (I); Lucy Levandoski, PA-C (C); Angie Starnes, RN, BSN, CDE (C), Tamara Hershey, PhD (I); Coordinating Center: Jaeb Center for Health Research, Tampa, FL: Roy W. Beck, MD, PhD; Katrina J. Ruedy, MSPH; Craig Kollman, PhD; Peiyao Cheng, MPH; Beth Stevens; Image Coordinating Center: Allan L. Reiss, MD; Naama Barnea-Goraly, MD; Matthew J. Marzelli, BS; Paul M. Mazaika, PhD; Cognitive Core: Tamara Hershey, PhD; Colleen Considine; Aiden Bondurant; Michaela Cuneo; Emily Bihun; Sarah June Grafeman, PhD.
References
- Aye T, Reiss AL, Kesler S, Hoang S, Drobny J, Park Y, Buckingham BA. The Feasibility of Detecting Neuropsychologic and Neuroanatomic Effects of Type 1 Diabetes in Young Children. Diabetes Care. 2011;34(7):1458–1462. doi: 10.2337/dc10-2164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnea-Goraly N, Raman M, Mazaika P, Marzelli M, Hershery T, Weinzimer SA, Reiss AL. Alterations in white matter structure in young children with type 1 diabetes mellitus. Diabetes Care. 2013 doi: 10.2337/dc13-1388. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bjorgaas M, Gimse R, Vik T, Sand T. Cognitive function in type 1 diabetic children with and without episodes of severe hypoglycaemia. Acta Paediatrica. 1997;86:148–153. doi: 10.1111/j.1651-2227.1997.tb08856.x. [DOI] [PubMed] [Google Scholar]
- Blasetti A, Chiuri RM, Tocco AM, Giulio CD, Mattei PA, Ballone E, Verrotti A. The Effect of Recurrent Severe Hypoglycemia on Cognitive Performance in Children With Type 1 Diabetes: A Meta-analysis. Journal of Child Neurology. 2011;26(11):1383–1391. doi: 10.1177/0883073811406730. [DOI] [PubMed] [Google Scholar]
- Bullmore E, Sporns O. The economy of brain network organization. Nature Reviews Neuroscience. 2012;13(5):336–349. doi: 10.1038/nrn3214. [DOI] [PubMed] [Google Scholar]
- Cohen MJ. CMS: Children's Memory Scale. The Psychological Corporation; 1997. [Google Scholar]
- Connors CK. CPT: The Conners Continuous Performance Test. Multi-Health Systems; Toronto, Canada: 1994. [Google Scholar]
- Diabetes Research in Children Network Study Group Continuous Glucose Monitoring in Children with Type 1 diabetes. Journal of Pediatrics. 2007;151(4):388–393. doi: 10.1016/j.jpeds.2007.03.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ferguson SC, Blane A, Perros P, McCrimmon RJ, Best JJ, Wardlaw J, Frier BM. Cognitive Ability and Brain Structure in Type 1 Diabetes: Relation to Microangiopathy and Preceding Severe Hypoglycemia. Diabetes. 2003;52:149–156. doi: 10.2337/diabetes.52.1.149. [DOI] [PubMed] [Google Scholar]
- Flykanaka-Gantenbein C. Hypoglycemia in Childhood: Long-Term Effects. Pediatric Endocrinology Reviews. 2004;1(Suppl 3):530–536. [PubMed] [Google Scholar]
- Gaudieri PA, Chen R, Greer TF, Holmes CS. Cognitive Function in Children with Type 1 Diabetes: A meta-analysis. Diabetes Care. 2008;31(9):1892–1897. doi: 10.2337/dc07-2132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giedd JN, Rapoport JL. Structural MRI of Pediatric Brain Development: What Have We Learned and Where Are We Going? Neuron. 2010;67(5):728–734. doi: 10.1016/j.neuron.2010.08.040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gioia GA, Isquith PK, Guy SC, Kenworthy L. Behavior Rating Inventory of Executive Function. PAR, Inc.; Lutz, FL: 2000. [Google Scholar]
- Haumont D, Dorchy H, Pelc S. EEG abnormalities in diabetic children: influence of hypoglycemia and vascular complications. Clinical Pediatrics. 1979;18:750–753. doi: 10.1177/000992287901801205. [DOI] [PubMed] [Google Scholar]
- Hershey T, Craft S, Bhargava N, White NH. Memory and Insulin Dependent Diabetes Mellitus (IDDM): Effects of Childhood Onset and Severe Hypoglycemia. Journal of the International Neuropsychological Society. 1997;3(6):509–520. [PubMed] [Google Scholar]
- Hershey T, Lillie R, Sadler M, White NH. Severe Hypoglycemia and Long-Term Spatial Memory in Children with Type 1 Diabetes Mellitus: A Retrospective Study. Journal of the International Neuropsychological Society. 2003;9(5):740–750. doi: 10.1017/S1355617703950077. [DOI] [PubMed] [Google Scholar]
- Hershey T, Lillie R, Sadler M, White NH. A prospective study of severe hypoglycemia and long-term spatial memory in children with type 1 diabetes. Pediatric Diabetes. 2004;5:63–71. doi: 10.1111/j.1399-543X.2004.00045.x. [DOI] [PubMed] [Google Scholar]
- Hershey T, Perantie DC, Warren SL, Zimmerman EC, Sadler M, White NH. Frequency and Timing of Severe Hypoglycemia Affects Spatial Memory in Children with Type 1 Diabetes. Diabetes Care. 2005;10:2372–2377. doi: 10.2337/diacare.28.10.2372. [DOI] [PubMed] [Google Scholar]
- Hochberg Y. A sharper Bonferroni procedure for multiple tests of significance. Biometrika. 1988;75:800–802. [Google Scholar]
- Hyllienmark L, Maltez J, Dandenell A, Luvigsson J, Brismar T. EEG abnormalities with and without relation to severe hypoglycemi in adolescents with type 1 diabetes. Diabetologia. 2005;48:412–419. doi: 10.1007/s00125-004-1666-2. [DOI] [PubMed] [Google Scholar]
- Jacobson AM, Ryan CM, Cleary PA, Waberski BH, Weinger K, Musen G, DCCT/EDIC Research Group Biomedical risk factors for decreased cognitive functioning in type 1 diabetes: an 18 year follow-up of the Diabetes Control and Complications Trial (DCCT) cohort. Diabetologia. 2011;54(2):245–255. doi: 10.1007/s00125-010-1883-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korkman M, Kirk U, Kemp S. NEPSY-II: Neuropsychological Battery for Children. Second Edition. Harcourt Assessment; San Antonio, TX: 2007. [Google Scholar]
- Kovacs M, Goldston D, Obrosky DS, Bonar LK. Psychiatric Disorders in Youths With IDDM: Rates and Risk Factors. Diabetes Care. 1997;20(1):36–44. doi: 10.2337/diacare.20.1.36. [DOI] [PubMed] [Google Scholar]
- Lin A, Northam EA, Rankins D, Werther GA, Cameron FJ. Neuropsychological profiles of young people with type 1 diabetes 12 yr after disease onset. Pediatric Diabetes. 2010;11:235–243. doi: 10.1111/j.1399-5448.2009.00588.x. [DOI] [PubMed] [Google Scholar]
- Ly TT, Anderson M, McNamara KA, Davis EA, Jones TW. Neurocognitive Outcomes in Young Adults With Early-Onset Type 1 Diabetes: A prospective follow-up study. Diabetes Care. 2011;34(10):2192–2197. doi: 10.2337/dc11-0697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Manschot SM, Brands AMA, van der Grond J, Kessels RPC, Algra A, Kappelle LJ, Biessels GJ. Brain Magnetic Resonance Imaging Correlates of Impaired Cognition in Patients With Type 2 Diabetes. Diabetes. 2006;55(4):1106–1113. doi: 10.2337/diabetes.55.04.06.db05-1323. [DOI] [PubMed] [Google Scholar]
- Marzelli M, Barnea-Goraly N, Mazaika PK, Hershey T, Tsalikian E, Tamborlane W, Reiss AL. Neuroanatomical correlates of dysglycemia in young children with type 1 diabetes mellitus Diabetes. 2013 doi: 10.2337/db13-0179. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murrough JW, Iacoviello B, Neumeister A, Charney DS, Iosifescu DV. Cognitive dysfunction in depression: Neurocircuitry and new therapeutic strategies. Neurobiology of Learning and Memory. 2011;96(4):553–563. doi: 10.1016/j.nlm.2011.06.006. [DOI] [PubMed] [Google Scholar]
- Musen G, Lyoo IK, Sparks CR, Weinger K, Hwang J, Ryan CM, Jacobson AM. Effects of Type 1 Diabetes on Gray Matter Density as Measured by Voxel-Based Morphometry. Diabetes. 2006;55:326–333. doi: 10.2337/diabetes.55.02.06.db05-0520. [DOI] [PubMed] [Google Scholar]
- Naguib JM, Kulinskaya E, Lomax CL, Garralda ME. Neuro-cognitive Performance in Children with Type 1 Diabetes- A Meta-analysis. Journal of Pediatric Psychology. 2009;34(3):271–282. doi: 10.1093/jpepsy/jsn074. [DOI] [PubMed] [Google Scholar]
- Northam EA, Anderson PJ, Jacobs R, Hughes M, Warne GL, Werther GA. Neuropsychological Profiles of Children With Type 1 Diabetes 6 Years After Disease Onset. Diabetes Care. 2001;24:1541–1546. doi: 10.2337/diacare.24.9.1541. [DOI] [PubMed] [Google Scholar]
- Northam EA, Anderson PJ, Werther GA, Warne GL, Adler RG, Andrewes D. Neuropsychological Complications of IDDM in Children 2 Years After Disease Onset. Diabetes Care. 1998;21:379–384. doi: 10.2337/diacare.21.3.379. [DOI] [PubMed] [Google Scholar]
- Northam EA, Anderson PJ, Werther GA, Warne GL, Andrewes D. Predictors of Change in the Neuropsychological Profiles of Children with Type 1 Diabetes 2 Years after Disease Onset. Diabetes Care. 1999;22:1438–1444. doi: 10.2337/diacare.22.9.1438. [DOI] [PubMed] [Google Scholar]
- Northam EA, Rankins D, Lin A, Wellard RM, Pell GS, Finch SJ, Cameron FJ. Central Nervous System Function in Youth With Type 1 Diabetes 12 Years After Disease Onset. Diabetes Care. 2009;32(3):445–450. doi: 10.2337/dc08-1657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perantie DC, Koller JM, Weaver PM, Lugar HM, Black KJ, White NH, Hershey T. Prospectively Determined Impact of Type 1 Diabetes on Brain Volume During Development. Diabetes. 2011;60(11):3006–3014. doi: 10.2337/db11-0589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perantie DC, Lim A, Wu J, Weaver P, Warren SL, Sadler M, Hershey T. Effects of prior hypoglycemia and hyperglycemia on cognition in children with type 1 diabetes mellitus. Pediatric Diabetes. 2008;9(2):87–95. doi: 10.1111/j.1399-5448.2007.00274.x. [DOI] [PubMed] [Google Scholar]
- Perantie DC, Wu J, Koller JM, Lim A, Warren SL, Black KJ, Hershey T. Regional Brain Volume Differences Associated with Hyperglycemia and Severe Hypoglycemia in Youth with Type 1 Diabetes. Diabetes Care. 2007;30(9):2331–2337. doi: 10.2337/dc07-0351. [DOI] [PubMed] [Google Scholar]
- Perros P, Deary IJ, Sellar RJ, Best JJ, Frier BM. Brain Abnormalities Demonstrated by Magnetic Resonance Imaging in Adult IDDM Patients with and without a History of Recurrent Severe Hypoglycemia. Diabetes Care. 1997;20:1013–1018. doi: 10.2337/diacare.20.6.1013. [DOI] [PubMed] [Google Scholar]
- Reynolds CR, Kamphaus RW. Behavior Assessment System for Children, Second Edition Parent Rating Scales. American Guidance Service; Circle Pines, MN: 2004. [Google Scholar]
- Rovet JF, Ehrlich RM. The Effect of Hypoglycemic Seizures on Cognitive Function in Children with Diabetes: A 7-Year Prospective Study. Journal of Pediatrics. 1999;134(4):503–506. doi: 10.1016/s0022-3476(99)70211-8. [DOI] [PubMed] [Google Scholar]
- Rovet JF, Ehrlich RM, Hoppe M. Intellectual Deficits Associated With Early Onset of Insulin-Dependent Diabetes Mellitus in Children. Diabetes Care. 1987;10(4):510–515. doi: 10.2337/diacare.10.4.510. [DOI] [PubMed] [Google Scholar]
- Ryan C, Vega A, Drash A. Cognitive Deficits in Adolescents Who Developed Diabetes Early in Life. Pediatrics. 1985;75:921–927. [PubMed] [Google Scholar]
- The Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group Long-Term Effect of Diabetes and Its Treatment on Cognitive Function. New England Journal of Medicine. 2007;356(18):1842–1852. doi: 10.1056/NEJMoa066397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van den Berg E, Reijmer YD, de Bresser J, Kessels RPC, Kappelle LJ, Biessels GJ, Utrecht Diabetic Encephalopathy Study Group A 4 year follow-up study of cognitive functioning in patients with type 2 diabetes mellitus. Diabetologia. 2010;53(1):58–65. doi: 10.1007/s00125-009-1571-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wechsler D. Wechsler Adult Scale of Intelligence. The Psychological Corporation: Harcourt Brace & Company; New York, NY: 1999. [Google Scholar]
- Wechsler D. Wechsler Preschool and Primary Scale of Intelligence. Third Edition. Psychological Corporation; San Antonio, TX: 2002. [Google Scholar]
- Woodcock RW, McGrew KS, Mather N. Woodcock-Johnson Test of Cognitive Abilites. Third Edition. Riverside Publishing; Itasca, IL: 2001. [Google Scholar]
- Yeates KO, Ris MD, Taylor HG, Pennington BF, editors. Research, Theory, and Practice. Second Edition Guilford Press; 2010. Pediatric Neuropsychology. [Google Scholar]