Abstract
Background and Objectives
Cryolipolysis is a noninvasive and well-tolerated treatment for reduction of localized subcutaneous fat. Although several studies demonstrate the safety and efficacy of this procedure, volumetric fat reduction from this treatment has not been quantified. This prospective study investigated the change in volume of fat after cryolipolysis treatment using three-dimensional (3D) photography.
Materials and Methods
A prospective study of subjects treated with cryolipolysis on the flank (love handle) was performed at Massachusetts General Hospital. Volume measurements were performed with a Canfield Scientific Vectra three-dimensional camera and software to evaluate the amount of post procedure volume change. Clinical outcomes were assessed with caliper measurements, subject surveys, and blinded physician assessment of photographs.
Results
Eleven subjects were enrolled in this study. Each subject underwent a single cycle of cryolipolysis to one flank. The untreated flank served as an internal control. The follow up time after treatment was two months. The mean amount of calculated absolute fat volume loss using 3D photography from baseline to 2 months follow up visit was 56.2 ± 25.6 from the treatment site and 16.6 ± 17.6 cc from the control (p < 0.0001). A mean absolute difference of 39.6 cc between the treated and untreated sides was calculated at 2 months post-treatment. Comparison of caliper measurements from baseline to 2 months post-treatment demonstrated significant reduction of the treated flank from 45.6 ± 5.8 mm at baseline to 38.6 ±4.6 mm at 2 months post-treatment (p<0.001). The untreated flank did not show significant reduction with caliper measurements demonstrating 45.3 ± 5.0 mm at baseline and 44.6 ± 5.1 mm at 2 months post-treatment (p=0.360). No unexpected side effects or adverse events were reported. Post-treatment satisfaction surveys demonstrated 82% of subjects were satisfied with the results.
Conclusions
Cryolipolysis is a safe, well-tolerated and effective noninvasive fat removal methodology that on average leads to 39.6 cc of fat loss at 2 months after a single treatment cycle.
Keywords: fat removal, noninvasive, volume of fat, imaging, cold induced fat loss
Introduction
Body-sculpting and fat removal procedures are becoming increasingly more popular. Although diet, exercise and bariatric surgery may be effective in controlling obesity, cosmetic procedures may still be necessary to remove localized adiposity in difficult to lose locations, such as the flanks and abdomen. Liposuction is the most frequently used method for excess local fat removal, but it is considered to be an invasive surgical procedure with significant risks including pain, infection, prolonged recovery, scarring, hematoma, deep vein thrombosis/pulmonary embolism and anesthesia-related complications.1,2 These risks and associated downtime have led patients to seek out alternatives such as noninvasive body contouring. Currently available noninvasive fat removal methods include low-level laser therapy, radiofrequency, ultrasound, infrared light and cryolipolysis.3
Cryolipolysis (CoolSculpting, Zeltiq, Pleasanton, CA) is a novel method of selective removal of fat with cooling. This technique is based on the concept that fat cells are more sensitive to cold than the surrounding tissue. Prior studies and observations have demonstrated that cold exposure can induce selective damage to the subcutaneous fat via induction of panniculitis, resulting in reduction in the superficial fat layer of the skin.4,5 The initial preclinical animal studies using a swine model showed that controlled local skin surface cooling leads to selective loss in the fat layer without damaging the overlying skin. Histologic analysis demonstrated approximately 80% loss of the upper fat layer of the skin or 40% of total fat layer thickness at 3.5 months after treatment. 6 Since initial approval by the U.S. Food and Drug Administration (FDA) in 2010 for reduction of focal adiposity of the flanks, several studies have demonstrated the safety and efficacy of cryolipolysis.7 In one clinical study, 10 subjects had a 20.4% reduction in fat thickness as measured by ultrasound of the flank 2 months and 25.5% at 6 months after a single treatment. 8 Another study looking at efficacy of cryolipolysis in Chinese patients, demonstrated an average loss of 14.67% in flat layer at 2 months post-treatment using caliper measurements.9 A larger, retrospective study demonstrated 25% reduction in fat layer thickness at 3 months based on caliper measurements.10
Although several studies have been published on efficacy, safety and subject satisfaction, there is no study quantifying numerical fat volume loss in the treated area following cryolipolysis. This study investigated the quantification of fat volume loss with cryolipolysis technique using three-dimensional imaging technology. To our knowledge this is the first published study to date to assess volume changes and quantification after noninvasive fat removal in comparison to an internal control. In addition, secondary study endpoints included evaluation of efficacy using caliper measurements and blinded investigator evaluations of clinical photographs. Subject satisfaction, tolerance, and safety were also assessed.
Materials and Methods
This was a prospective, site randomized clinical trial approved by the Partners Human Research Committee at Massachusetts General Hospital. Eleven subjects were enrolled and treated with a single cycle of cryolipolysis to one flank (Coolsculpting, ZELTIQ Aesthics, Pleasanton, CA) between December 2012 and July 2013. Side of treatment was randomized. All treatments were performed using the Ez App 6.3 applicator. Each treated flank was exposed to CIF 41.6 (−73mW/cm2) for 60 minutes. The untreated side served as an internal control for each subject and was later treated at the conclusion of the study as a courtesy to all subjects who completed the study. Baseline and follow up 3D photographs, weight, and caliper measurements were taken for each subject. Side effects and satisfaction data were collected with subject surveys by a trained clinician. Clinical outcomes including safety, caliper measurements, weight, photographs and subject surveys were collected at 10 minutes, 48–72 hours, 1 week, 2 weeks, 3 weeks, and 2 months after treatment. Two months was chosen as the end time point of the study because previously published studies demonstrated efficacy and significant improvement in body contouring at 2 months post treatment.8,9
The treatment site was identified, assessed and marked by a single, unblinded investigator. Prior to treatment, weight, photographs and caliper measurement of the marked areas on flanks were obtained. The area on the flank where caliper measurements were taken from was marked by a transparent paper and aligned using landmarks such as nevi or scars on follow up visits to ensure reproducibility of measurement sites at each visit.
The primary study endpoint of treatment efficacy was assessed by quantitative volume measurements with a Canfield Scientific Vectra three-dimensional (3D) camera and software (Canfield Scientific Inc, Fairfield, New Jersey). Photographs were taken at fixed angles and posture at each visit to ensure standardization at the same position in both pre-treatment and post-treatment photographs. Subjects were given standardized disposable underwear to minimize its effects on the skin and fat, and to avoid distraction to the blinded evaluators. Three-dimensional images were taken of the subjects in sagittal (left and right sides) and coronal (front and back sides) views at the baseline and at completion of the study. The abdominal region was exposed, and the subject was instructed to remain still while the camera captured an image. Images taken at baseline and the last follow up (2 months) were imported into Mirror Analysis 3D software (Canfield Scientific Inc, Fairfield, New Jersey) and registered using anatomical landmarks (pigmented lesions, umbilicus, etc.) away from the treated area for proper alignment. The registered images were aligned to a grid, with the x-axis aligned to the AP plane, z-axis aligned to the L-R plane, and y-axis aligned to the S-I plane. Using the grid as a guide, a 64 cm2 square region corresponding to the size of the treated area was selected on the baseline model, and projected onto the follow up model for volume calculations. Three-dimensional color schematic representation of volume changes between baseline and post-treatment photographs were also used to define the area of interest for measurements (Figure 5). The volume between the area of interest on the aligned baseline and 2 month follow up photographs was calculated to be the volume change. All volume measurements were recorded in milliliters. This process was repeated four times by two independent researchers, and the average volume change was calculated. The quantitative volume measurements were compared to caliper measurements and to evaluations by blinded dermatologists of clinical photographs to assess for correlation.
Figure 5.
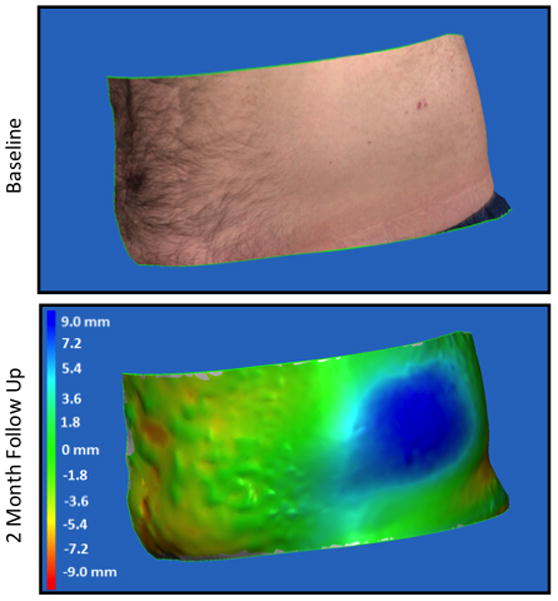
Three-dimensional colorimetric map colorimetric map of volume change in treated side. Cool colors represent volume loss and warmer colors represent volume gain as distance in mm between flanks. Green represents no change in volume
The secondary endpoints of the study were treatment efficacy and side effect assessment at 10 minutes, 48–72 hours, 1 week, 2 weeks, 3 weeks, and 2 months after treatment. Secondary measurements of efficacy included caliper measurements and blinded investigator evaluations. All subjects had caliper measurements at the treated and control sites at baseline and at 2 months. Landmarks and photographs were used to ensure the same area in the treated and untreated sides were used for caliper measurements. Care was taken to position subject at the exact same position during each measurement and the same properly trained investigator did all the caliper measurements for the entire study to ensure consistency. Weights were measured at baseline and at the 2 months post-treatment study visit using the same scale. Blinded investigator assessment of treatment efficacy was conducted by assessment of photographs by three independent dermatologists. Subject satisfaction survey served as a marker for objective measurement of efficacy. Overall subject satisfaction was assessed at the end of the study at 2 months post-treatment
Side effects were recorded by subject surveys at different time points after treatment. In addition a physician recorded the erythema, edema, bruising, bleeding, scaring, blistering, and crusting in the treated area. These parameters where surveyed and observed at 10 minutes, 48–72 hours, 1 week, 2 weeks, 3 weeks, and 2 months after treatment.
The D’Agostino & Pearson omnibus normality test demonstrated that the data was normally distributed. Therefore parametric statistical tests were performed. The caliper measurements at baseline and 2 month follow up were analyzed using a paired two sample T-test. Volume loss measured by three-dimensional imaging in the treated and control sides was directly compared with a one-tailed two sample T-test assuming unequal variances.
Results
Eleven subjects were treated (55% female, 45% male; mean age 37.6 ± 8.4). The average Body Mass Index (BMI) was 27.1 ± 2.0 (range 22.5–29.1) (Table 1). Subjects were randomized to have either the right or left flank treated (64% and 46% respectively). Each subject had only a single treatment. At baseline the treated and control flanks had similar average caliper measurements that were not statistically significant (p=0.8) (Table 1).
Table 1.
Demographics and baseline clinical characteristics
| Variable | Mean ± SD |
|---|---|
|
| |
| Age (yrs) | 37.6 ± 8.4 (range 27–53) |
| Sex | |
| Females (n,%) | 6(55%) |
| Male(n,%) | 5 (45%) |
| BMI(kg/m2) | 27.1 ±2.0 (range 22.5–29.1) |
| Side treated, right (n,%) | |
| Right | 4 (36%) |
| Left | 7 (64%) |
| Caliper measurement (mm) | |
| Treated side | 45.8 ± 5.0 (range 33–53) |
| Untreated side | 45.1 ±5.0 (range 38–52) |
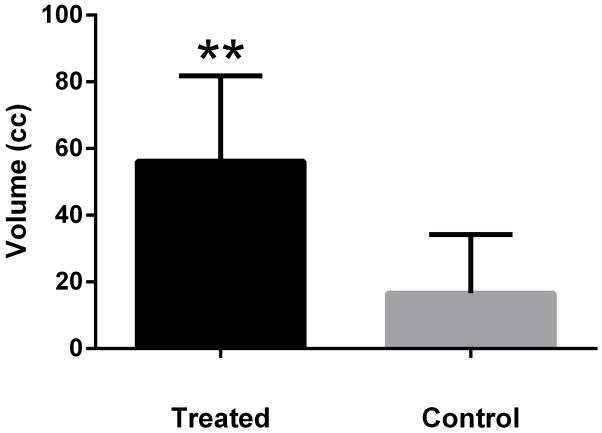
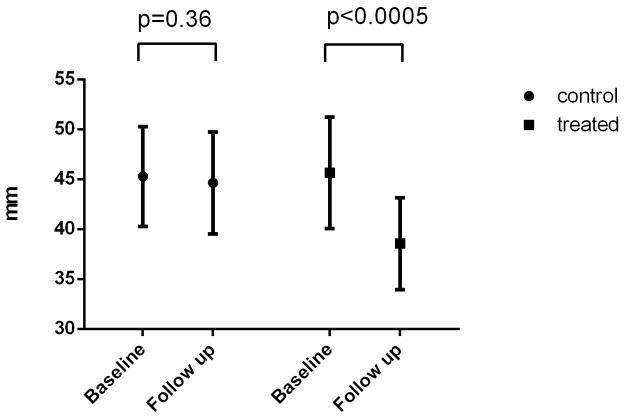
The mean amount of volume loss in the treated flank at 2 months post-treatment was 56.2 ± 25.6 cc versus 16.6 ± 17.6 cc in the untreated flank (p<0.0001). Overall the mean absolute difference in volume loss between treated and untreated flanks at 2 months after treatment was 39.5 cc (Figure 1). These numbers correlated with the caliper measurements which showed significant reduction of the treated flank from 45.6 ± 5.8 mm at baseline to 38.6 ±4.6 mm at 2 month follow (p<0.001). The untreated flank did not show significant reduction with caliper measurements demonstrating 45.3 ± 5.0 mm at baseline and 44.6 ± 5.1 mm at 2 months post treatment (p=0.360). The average reduction in fat thickness based on the caliper measurements was 14.9% in the treated flank and 0.7% in the untreated flank (Figure 2).
Figure 1.
Quantification of volume loss. Three-dimensional imaging system software was used to quantify volume loss for treated and control (untreated) sites from baseline to 2 month follow up. **p<0.0001
Figure 2.
Caliper measurements of treated and control (untreated) at baseline and at 2 months post-treatment follow up.
Three independent blinded dermatologists evaluated the clinical efficacy of the treatments by analyzing baseline and 2 months post-treatment standardized photographs for all subjects. Blinded evaluators were able to choose the treated side in 79% of subjects.
All subjects reported erythema and edema followed by reduction in sensation ten minutes after treatment at the site of applicator. The reported decreased sensation persisted at 3 weeks post treatment in 73% subjects and 18% at 2 months post-treatment. Fifty-five percent of subjects reported pain in the treated areas 10 minutes after treatment with 36% reporting mild pain and 18% reporting moderate. No one reported pain or erythema in the treated area at 1-week and 2-weeks post treatment, respectively (Table 2). No subject required pain medication during or after treatment. There were no occurrences of extended pain, blistering, scarring, bleeding, crusting, hyper- or hypopigmentation. At the end of the study 82% of subjects were satisfied with the treatment results. Of the 82% of satisfied subjects, all said they would have the procedure again, and that they would recommend the treatment to a friend. The number one reason why subjects liked the treatment was that it was noninvasive.
Table 2.
Side Effects After Cryolipolysis Treatment
| Side Effects | 10 min | 1 week | 2 weeks | 3 weeks | 2 months |
|---|---|---|---|---|---|
| Erythema | 100% | 9% | 0% | 0% | 0% |
| Edema | 100% | 18% | 9% | 0% | 0% |
| Decreased Sensation | 100% | 73% | 73% | 73% | 18% |
| Pain | 55% | 0% | 0% | 0% | 0% |
Discussion
To our knowledge this study is the first clinical study quantifying volumetric reduction of fat following cryolipolysis. Three-dimensional imaging has been used in the past for quantification of autologous fat grafting in the midface, demonstrating mean absolute volume augmentation of 3.3 cc.12 This was the first study to quantify volume after fat grafting and to show that three-dimensional imaging can reliably be used to analyze volume changes even in single digit range.12 We preformed a similar study quantifying the volume change after cryolipolysis. We provide strong and definitive objective and quantitative data of significant volume loss, which occurs after cryolipolysis of the flank at 2 months following a single treatment. The mean amount of calculated absolute fat volume loss from treated flank was 56.2 cc and untreated flank was 16.6 cc, which was highly statistically significant (P < 0.0001), giving a mean absolute difference of 39.6 cc between the treated and untreated sides. This data suggests that after a single cryolipolysis treatment there is on average about 40 cc of fat volume loss at 2 months post-treatment using the Ez App 6.3 applicator. Undoubtedly in comparison to invasive fat removal procedures such as liposuction, 40 cc is a minimal fat volume loss, but still significant enough for subjects to be satisfied with the clinical improvement and for blinded physicians to identify the treated side. Subjects repeatedly voiced their satisfaction with the noninvasive nature and minimal downtime of the procedure.
The loss of volume in the untreated flank could be explained by factors such as weight changes and limitations of the software used to calculate the volume and the location of the area of interest. Even though subjects were asked to keep their normal lifestyle and diet we did not control for weight in our study and based on the analysis of the mean weight at baseline (179.5lb) and 2 months follow up (177.2lb), there was statistically significant average weight loss of 1.3% from baseline (p=0.05). Figure 3 shows the weight at baseline and at 2 months post-treatment for each subject. Subject five lost 9lbs during the duration of the study and 3D quantitative volume analysis of her images demonstrated volume loss of 108 cc in the treated flank and 45 cc in the control (untreated) flank. This was the highest volume of change in the control side. In addition, subject 4 gained 3lbs during the duration of the study and his control flank demonstrated gain of volume of 17.5 cc. He was the only subject in our study who gained volume in the control flank. Despite volume gain in the control flank, he still had volume loss of 53.6 cc in the treated flank (Figures 4 and 5). One investigator performing the blinded evaluation of this subject’s photograph did note the volume increase in the untreated site.
Figure 3.
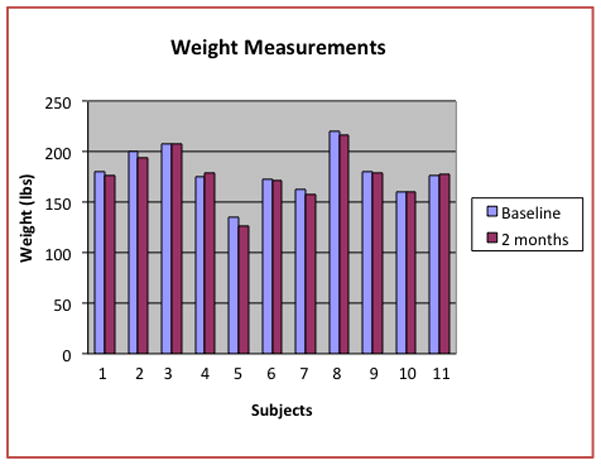
Weight measurements of all subjects at baseline and at 2 month follow up.
Figure 4.
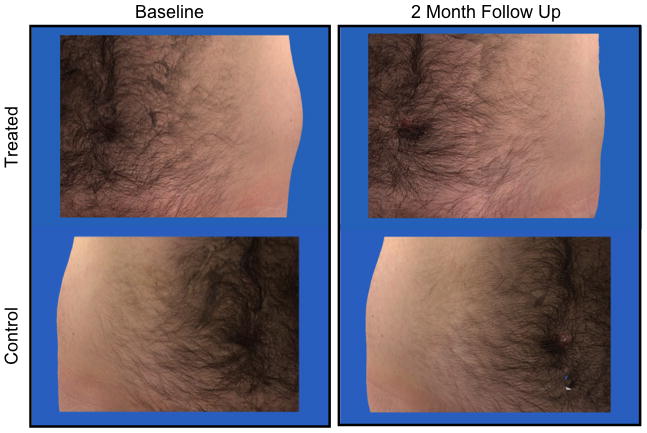
Flanks (love handles) at baseline and at 2 month follow up after a single treatment. The left flank was treated and the right flank was a control (untreated).
It is important to notice that quantitative volumetric measurements using standardized 3D photos are also subject to errors, since the region of interest and landmarks are subjectively assigned. In this study, this was minimized by having two independent evaluators and four repetitive measures of each area for statistical analysis. Our data confirms the reliability of quantitative volume measurements using three-dimensional imaging. The quantification of volume change in the control site, which was not statistically significant, also supports the conclusion that the change of average weight during the study (average of 2lb loss over 2 months) cannot account for the calculated loss of volume in the treated side. However, it could account for the small and statistically insignificant volume loss in the untreated side. In addition, despite our careful efforts to ensure consistency of photographic technique and measurements, body position changes due to breathing and slight differences in alignment may have contributed to minimal volume variation observed in untreated and treated sides. Because of this, the difference between the average loss in the treated and untreated sides (39.5 cc) is a more accurate representation of the amount of fat loss that would not be due to these aforementioned limitations.
Volume loss measured through 3D image analysis is an effective modality to measure fat loss as it correlated with caliper measurements which is a standard method used in the literature to demonstrate effectiveness. Caliper measurements at baseline and 2 month follow up showed significant loss in the treated flank (7mm, p<0.001) but not in the untreated flank (0.7mm, p=0.36). The average reduction in fat thickness based on the caliper measurements was 14.9% in the treated flank and 0.7% in the untreated flank (Figure 2). This is very consistent with previously reported 13.4% reduction at the love handles in Chinese subjects at 2 months post single cryolipolysis treatment.9
In addition, blinded investigator performed evaluation showed 79 % efficacy in identifying the correct treated side using baseline and 2 months post-treatment standardized photographs. Although this number is slightly lower than previously reported correct identification of the treated site in 82% of subjects by blinded evaluators, this may be because the photographs used for blinded evaluations in our study were taken at 2 months post-treatment versus 3 months and 6 months at other studies.10,11
Assessing efficacy of noninvasive fat removal relies on the measurements currently used, which include ultrasound, caliper measurements, two-dimensional photographic comparisons, tape measurements, and magnetic resonance imaging (MRI). Blind analysis of pre and post-treatment 2D photographs are commonly used for fat removal studies, but it is not a reliable method to evaluate efficacy. Changes in position, light and even subject’s underwear can easily distract the evaluators. All of these factors were carefully controlled in this study by using a systematic analysis of 3D images. Other imaging systems such as ultrasound (US) and MRI can also evaluate subcutaneous fat quantitatively. US images, however, are also prone to technical errors as the pressure of the probe into the skin is controlled by the operator and therefore, subject to human mistakes or bias. Only MRI can reliably show subcutaneous fat change, however costs are also a limitation of its use.
Despite the availability of the aforementioned tools, their efficacy as an assessment measure has also been questioned, highlighting the need for highly accurate and standardized method for measurement of fat loss.13 Although more studies are needed to prove the reliability and accuracy of using three-dimensional imaging as an assessment tool for measurement of fat volume changes, our study clearly shows that it can be used as a more practical and reliable quantitative assessment tool.
In terms of subject satisfaction, our data found that 82% of the subjects were satisfied with the results, and that they would have the treatment again, recommending it to a friend. The number one reason they liked the treatment was that it was noninvasive. This correlates with the trend that more patients are seeking minimally invasive techniques with very little down time, despite the fact that the volume loss is not as significant as invasive techniques, such as liposuction.
Cryolipolysis appears to be safe and well tolerated. No subjects reported persistent pain, blistering, scarring, erythema, or edema. All subjects were pain free by 1 week post-treatment. All subjects reported reduction in sensation at the treatment site 10 minutes post treatment. This resolved for all but 1 subject, who reported mild reduction in sensation at 2 months post treatment.
In conclusion, cryolipolysis is a well tolerated, safe and effective noninvasive fat removal technique. There is on average about 40cc of fat volume loss after a single treatment of the flank at 2 months post-treatment.
References
- 1.Alderman AK, Collins ED, Streu R, et al. Benchmarking outcomes in plastic surgery: national complication rates for abdominoplasty and breast augmentation. Plast Reconstr Surg. 2009;124:2127–33. doi: 10.1097/PRS.0b013e3181bf8378. [DOI] [PubMed] [Google Scholar]
- 2.Desrosiers AE, 3rd, Grant RT, Breitbart AS. Don’t try this at home: liposuction in the kitchen by an unqualified practitioner leads to disastrous complications. Plast Reconstr Surg. 2004;113:460–1. doi: 10.1097/01.PRS.0000100616.87383.2E. [DOI] [PubMed] [Google Scholar]
- 3.Jalian HR, Avram MM. Body contouring: the skinny on noninvasive fat removal. Semin Cutan Med Surg. 2012;31:121–5. doi: 10.1016/j.sder.2012.02.004. [DOI] [PubMed] [Google Scholar]
- 4.Epstein EH, Jr, Oren ME. Popsicle panniculitis. N Engl J Med. 1970;282:966–7. doi: 10.1056/NEJM197004232821709. [DOI] [PubMed] [Google Scholar]
- 5.Beacham BE, Cooper PH, Buchanan CS, Weary PE. Equestrian cold panniculitis in women. Arch Dermatol. 1980;116:1025–7. [PubMed] [Google Scholar]
- 6.Manstein D, Laubach H, Watanabe K, Farinelli W, Zurakowski D, Anderson RR. Selective cryolysis: a novel method of non-invasive fat removal. Lasers Surg Med. 2008;40:595–604. doi: 10.1002/lsm.20719. [DOI] [PubMed] [Google Scholar]
- 7.Avram MM, Harry RS. Cryolipolysis for subcutaneous fat layer reduction. Lasers Surg Med. 2009;41:703–8. doi: 10.1002/lsm.20864. [DOI] [PubMed] [Google Scholar]
- 8.Coleman SR, Sachdeva K, Egbert BM, Preciado J, Allison J. Clinical efficacy of noninvasive cryolipolysis and its effects on peripheral nerves. Aesthetic Plast Surg. 2009;33:482–8. doi: 10.1007/s00266-008-9286-8. [DOI] [PubMed] [Google Scholar]
- 9.Shek SY, Chan NP, Chan HH. Non-invasive cryolipolysis for body contouring in Chinese--a first commercial experience. Lasers Surg Med. 2012;44:125–30. doi: 10.1002/lsm.21145. [DOI] [PubMed] [Google Scholar]
- 10.Dierickx CC, Mazer JM, Sand M, Koenig S, Arigon V. Safety, tolerance, and patient satisfaction with noninvasive cryolipolysis. Dermatol Surg. 2013;39:1209–16. doi: 10.1111/dsu.12238. [DOI] [PubMed] [Google Scholar]
- 11.Kaminer MWR, Newman J, et al. Visible cosmetic improvement with cryolipolysis: Photographic evidence. Annual Meeting of the American Society for Dermatologic Surgery; Phoenix, AZ. 2009. [Google Scholar]
- 12.Meier JD, Glasgold RA, Glasgold MJ. Autologous fat grafting: long-term evidence of its efficacy in midfacial rejuvenation. Arch Facial Plast Surg. 2009;11:24–8. doi: 10.1001/archfacial.2008.518. [DOI] [PubMed] [Google Scholar]
- 13.Zachary CB, Saedi N, Allison J. The geometric model and fat reduction. J Drugs Dermatol. 2013;12:27–34. [PubMed] [Google Scholar]