Abstract
Perfluoro-n-octane (PFO) is commonly used in vitreoretinal surgery. In this case report, we present a 35-year-old patient with retained PFO up to 9 years after par plana vitrectomy. Post-operatively, PFO bubbles occupied 15% of the anterior chamber (AC). Follow-up over 9 years, consistently showed a quiet AC, normal intraocular pressure and endothelial cell counts remained stable. Until date, the patient has been under observation and there have been no ocular symptoms or side-effects. Residual PFO that inadvertently remains in the AC can be well- tolerated, without side-effects for up to 9 years.
Keywords: Anterior Chamber, Perfluoro-n-octane, Vitreo-retinal Surgery
INTRODUCTION
Perfluorocarbon liquids (PFCLs) are a mainstay of vitreoretinal surgery because of their high specific gravity, low viscosity, optical clarity and immiscibility in water, which permit surgical tissue manipulation. PFCLs are an adjunct in vitreoretinal surgery for complex retinal detachment repair as they displace subretinal fluid and blood anteriorly (thus limiting the need for a posterior drainage retinotomy), unfold the retina in giant retinal tear cases and provide countertraction and retinal stabilization during membrane peeling in eyes with proliferative vitreoretinopathy.
Multiple agents have been used and approved in different countries, including perfluoro-n-octane (PFO), perfluoroperhydrophenanthrene (vitreon) and perfluorodecalin. PFO is primarily used in North America. PFCLs have a specific gravity of 1.9; therefore, they have a higher density than water. This property allows them to sink into the retina and displace any subretinal fluid anteriorly. If there is no significant traction on the retina, the PFCLs will push the retina flat onto the eye wall.
When compared with other available perfluorocarbons, PFO has the most visible interface, which aids complete intraoperative removal. PFO also has the lowest viscosity of PFCLs (0.69 centistokes at 25°C for PFO and 8.03 centistokes for perfluoropherhydrophenanthrene), offering less resistance to injection and aspiration through microsurgical instruments and has the highest vapor pressure, allowing more complete evaporation of residual PFO from the retinal surface after fluid-air exchange. Despite these characteristics, inadvertent post-operative retention of PFO occurs in approximately 1-3.5% of eyes.
CASE REPORT
An otherwise healthy 24-year-old male who was status post-Lasik with a history of high myopia in both eyes presented to the emergency room at King Khaled Eye Specialist Hospital, Saudi Arabia on June 2002 with a history of a sudden drop of vision in the right eye with onset 3 weeks prior to presentation. On examination, his visual acuity was 20/40 and 20/20 for the right and left eyes, respectively. Intraocular pressure (IOP) was within the normal (13 mmHg) limits in both eyes.
Anterior segment examination of both eyes was within normal limits. Fundus examination of the right eye indicated an inferior rhegmatogenous retinal detachment with multiple peripheral breaks and macula off. Fundus examination of the left eye showed localized inferotemporal retinal detachment with peripheral breaks.
Patient was diagnosed with rhegmatogenous retinal detachment, macula off with multiple peripheral breaks in the right eye and localized retinal detachment with multiple peripheral breaks in the left eye.
A pars plana vitrectomy, air-fluid exchange with perfluoropropane (C3F8) 15% flush and a scleral buckle were performed on the right eye. Indirect laser treatment and retinal cryopexy were performed on the left eye. The post-operative period was unremarkable and the patient was doing well with a flat retina in both eyes.
On a follow-up visit in early September 2002, a new horseshoe tear had formed behind the buckle at the 12:00 meridian, which required laser treatment in the periphery of the tear. On the following two follow-up visits (at 2 weeks and 1 month) after the procedure, the retina was flat.
In January 2003, the patient presented to the emergency at King Khalid Eye Specialist Hospital with a visual complaint of a veil in front of the right eye with onset 3 days prior to presentation. On examination, visual acuity was 20/200 in the right eye and 20/20 in the left eye. IOP was 12 mmHg in the right eye and 15 mmHg in the left eye. Anterior segment examination indicated a trace posterior subcapsular cataract (PSC) in the right eye and the left eye was unremarkable. On fundus examination of the right eye, there was subretinal fluid extending from 6:00 to 7:00 meridian with macula on, the remainder of the exam was normal. Fundus examination of the left eye was unremarkable.
Patient was diagnosed with recurrent macula-on retinal detachment in the right eye. Pars plana vitrectomy, PFCL injection removal, air-fluid exchange, C3F8 10% flush and endolaser were performed in the right eye. The post-operative period was unremarkable and the retina was flat bilaterally.
Anterior segment examination of both eyes was only significant for PFO bubbles occupying approximately 15% of the anterior chamber (AC) [Figure 1] and a PSC in the right eye. Patient continued follow-up with the vitreoretinal division at King Khaled Eye Specialist Hospital for 9 years at 6-month intervals and his last visit was on December 2012; the patient was doing well at all post-operative visits. Currently, his visual acuity is 20/60 with glasses in the right eye and 20/20 in the left eye.
Figure 1.
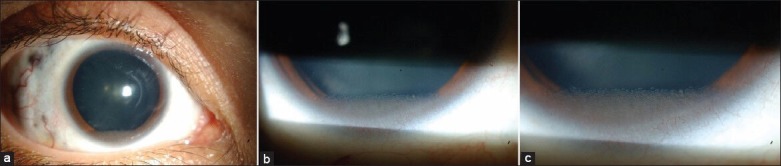
(a-c) Slit lamp photos of the anterior segment of the right eye at different magnifications showing perfluoro-n-octane bubbles in the anterior chamber 9 years after vitreoretinal surgery (May 2007)
The patient refused any intervention for the cataract in the right eye as he is currently satisfied with his vision [Figure 2]. The retained PFO in the AC remained stable for the entire follow-up over 9 years. Posterior segment examination, on all post-operative visits from 2003 to 2012, revealed the retina was flat in both eyes [Figure 3]. The endothelial cell count was 3500 cells/mm2 in 2007 and 3100 cells/mm² in 2012.
Figure 2.
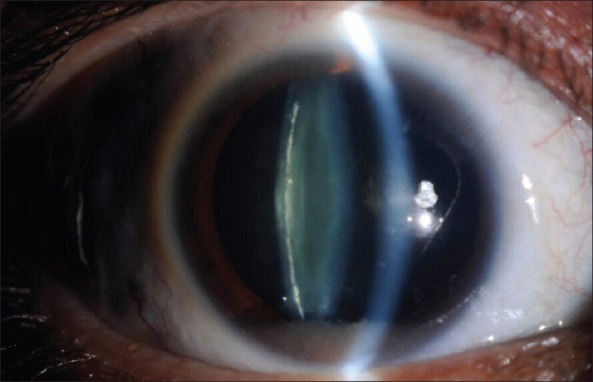
Posterior subcapsular cataract in the right eye (December 2012)
Figure 3.
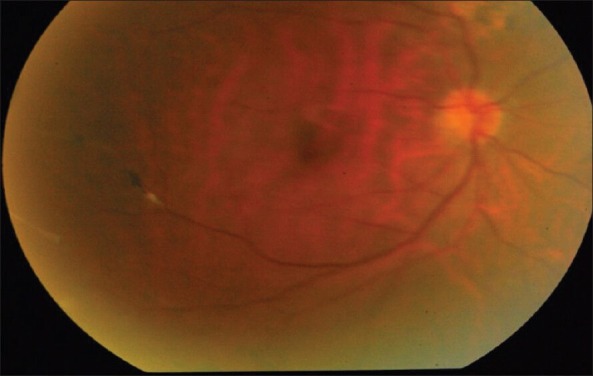
Fundus photo of the right eye showing a flat retina. The mild hazy view is due to the cataract in this eye (December 2012)
DISCUSSION
In this case report of retained PFO over 9 years, we found no significant ocular effect. The safety of PFO as a post-operative tamponade was investigated a decade ago by Chang et al.1 Intravitreal PFO retained for up to 48 h in the rabbit eye did not cause clinical, electrophysiologic or microscopic evidence of toxicity.1 However, minute amounts of PFO (approximately 0.1 ml) remained in the rabbit eye for longer periods led to the deposition of white precipitates (appearing at 3-5 weeks).1 Histopathology of the white precipitates indicated macrophages containing intracellular vacuoles.1 Long-term (up to 2 months) placement of PFO revealed similar findings with the accumulation of cells at the interface of PFO and compressed cortical vitreous (earliest appearance at 2 weeks).1 Macrophages were present in all rabbit eyes containing these vacuoles on the inner retinal surface and evidence of progressive epiretinal membrane formation was noted.1
The safety of retained PFO has been previously studied. Elsing et al.2 reported five cases with retained (PFO) liquid after retinal reattachment surgery. They2 concluded that if a significant volume of PFO is retained in an eye, PFO mechanically compresses residual vitreous, causing deposition of white proteinaceous deposits as early as the third post-operative week, with macrophage incursion.2 Elsing et al.2 concluded that young eyes, eyes with considerable residual vitreous gel and eyes with 0.25 ml or greater of retained PFO are likely at higher risk for developing this inflammatory response. Eyes that develop persistent inflammation, secondary membrane formation or recurrent RD should undergo reoperation for removal of this material. In our case, there was no inflammatory response, perhaps due to a low volume of retained PFO. Hence, we elected observation instead of surgical intervention.
A multicenter study by Scott et al.3 evaluated 555 patients (555 eyes), 15 months of age or older who had undergone pars plana vitrectomy for complex retinal detachment associated with proliferative vitreoretinopathy with intraoperative PFO. They3 found 41 (7.4%) eyes with retained PFO and concluded that it was not a significant predictor of either recurrent retinal detachment or visual outcome.3 These conclusions are consistent with our case where the patient has had an uneventful course and satisfied with his vision for almost a decade despite the retained PFO (and cataract).
In a comparison of ease of removal intraoperatively and safety and efficacy of PFO versus perfluoroperhydrophenanthrene (vitreon), Loewenstein et al.,4 reported that vitreon was retained in 8.4% eyes and PFO in 4% of the eyes. There were no cases of macular epiretinal membranes, cystoid macular edema, or uveitis in patients with retained vitreon or PFO.4 The outcomes from both studies3,4 indicate observation may be the more prudent course in many cases of retained PFO.
However, there are cases where surgical intervention is warranted. For example, a 65-year-old male with secondary open angle glaucoma due to retained PFO after vitreoretinal surgery has been previously reported.5 In another case, PFCLs and silicone oil were left in the eye at the end of the surgery.6 The authors concluded that (PFCLs) are surgical tools and should be completely removed from the eye at the end of the surgery. PFCLs and silicone oil tend to emulsify together, forming an opaque fluid containing both silicone oil and dispersed PFCL bubbles.6
Pradeep et al.7 reported a case of 55-year-old lady complaining of decreased vision in the left eye with pain and redness for 3 months with a history of cataract surgery with an unspecified PFCL to aid in the removal of a dropped nucleus intraoperatively. They7 concluded that retained PFCL can cause late onset fibrinous inflammation after a quiescent period, but surgical intervention may lead to good visual outcome. In the current case, the eye has remained quiet for 9 years and late onset reaction may occur, yet we do not believe this potential scenario, warrants the risks associated with surgery at this time.
In our case, this patient has retained PFO in the AC and has been extensively evaluated every 6 months over 9 years. We performed visual acuity testing, slit lamp examination of the anterior segment looking for signs of inflammation, IOP measurement and fundus examination. Endothelial microscopy has been performed twice first in 2007 and again in 2012. Every parameter to date has been normal without signs of ocular toxicity.
To the best of our knowledge, this is the longest documented follow-up for a case with retained PFO in a human eye.
CONCLUSION
Inadvertent retention of PFO in the AC may be well-tolerated, without side-effects for up to 9 years. However, some evidence of harmful effects from animal studies and isolated case reports has been reported. Hence, we recommend that in similar cases, the patient be followed regularly with extensive ophthalmic evaluation to rule out any signs of ocular toxicity.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Chang S, Sparrow JR, Iwamoto T, Gershbein A, Ross R, Ortiz R. Experimental studies of tolerance to intravitreal perfluoro-n-octane liquid. Retina. 1991;11:367–74. [PubMed] [Google Scholar]
- 2.Elsing SH, Fekrat S, Green WR, Chang S, Wajer SD, Haller JA. Clinicopathologic findings in eyes with retained perfluoro-n-octane liquid. Ophthalmology. 2001;108:45–8. doi: 10.1016/s0161-6420(00)00481-4. [DOI] [PubMed] [Google Scholar]
- 3.Scott IU, Flynn HW, Jr, Murray TG, Feuer WJ, Perfluoron Study Group. Outcomes of surgery for retinal detachment associated with proliferative vitreoretinopathy using perfluoro-n-octane: A multicenter study. Am J Ophthalmol. 2003;136:454–63. doi: 10.1016/s0002-9394(03)00241-1. [DOI] [PubMed] [Google Scholar]
- 4.Loewenstein A, Humayun MS, de Juan E, Jr, Campochiaro PA, Haller JA. Perfluoroperhydrophenanthrene versus perfluoro-n-octane in vitreoretinal surgery. Ophthalmology. 2000;107:1078–82. doi: 10.1016/s0161-6420(00)00095-6. [DOI] [PubMed] [Google Scholar]
- 5.Toffoli D, Arbour JD, Harasymowycz P. Retained perfluoron postvitreoretinal surgery causing secondary open-angle glaucoma. Can J Ophthalmol. 2008;43:372. doi: 10.3129/i08-047. [DOI] [PubMed] [Google Scholar]
- 6.Ciardella AP, Langton K, Chang S. Intraocular dispersion of liquids in silicone oil. Am J Ophthalmol. 2003;136:365–7. doi: 10.1016/s0002-9394(03)00221-6. [DOI] [PubMed] [Google Scholar]
- 7.Pradeep S, Chhablani JK, Patel B, Rani P. Delayed inflammation associated with retained perfluorocarbon liquid. Indian J Ophthalmol. 2011;59:396–8. doi: 10.4103/0301-4738.83623. [DOI] [PMC free article] [PubMed] [Google Scholar]


