Abstract
Photodynamic therapy (PDT) has been used for treatment of various intraocular tumors including choroidal hemangioma, vasoproliferative tumor, amelanotic choroidal melanoma and choroidal neovascular membrane due to choroidal osteoma. This case report documents the effect of PDT for a presumed acquired retinal astrocytoma. A 42-year-old female with a juxtapapillary acquired astrocytoma was treated with a single session of PDT using standard parameters. The tumor showed dramatic regression over 6 months into a fibrotic scar. It remained regressed and stable with 20/20 vision after 51 months of follow-up. We believe that PDT can be used as a primary treatment for acquired retinal astrocytoma.
Keywords: Astrocytoma, Photodynamic Therapy, Retinal Astrocytoma
INTRODUCTION
Acquired retinal astrocytoma is a benign glial intraretinal tumor.1 It is considered the retinal equivalent of low-grade brain astrocytomas. Despite its benign cytology, it can show progressive growth and behave as a locally aggressive malignant tumor. The clinical course can be complicated with exudative retinal detachment, vitreous hemorrhage, neovascular glaucoma and a blind, painful eye, ultimately leading to enucleation.2,3]
The management of acquired astrocytoma remains controversial. External beam radiotherapy,2 laser photocoagulation,4 cryotherapy, plaque radiotherapy and pars plana vitrectomy and endoresection5 were previously proposed as the treatment options to avoid enucleation.3 However, these treatments have been ineffective in many patients.2,3,4 Over time, some studies revealed success with verteporfin photodynamic therapy (PDT) in the treatment of acquired retinal astrocytomas.6,7,8 In this case report, we present a patient with symptomatic, presumed acquired retinal astrocytoma - without evidence of tuberous sclerosis - that showed dramatic regression after a single session of PDT.
CASE REPORT
A 42-year-old female noted decreased visual acuity in her right eye for 1 month. The visual acuity was counting fingers at one meter in the right eye and 20/20 in the left eye. Anterior segment examination was normal in both eyes. The fundus was unremarkable in the left eye. In the right eye, there was a juxtapapillary, amelanotic, yellow-white lesion with circinate exudation, exudative inferior hemiretinal (including fovea) detachment and overlying marginal retinal hemorrhages [Figure 1a]. The lesion was 3.6 mm in thickness and had a basal diameter of 3 mm. Optical coherence tomography (OCT) imaging through the fovea demonstrated a serous retinal detachment [Figure 1b]. OCT through the lesion showed preservation of the linear configuration of the retinal pigment epithelial layer with deep optical shadowing, suggesting a tumor of retinal and not choroidal origin [Figure 1c]. Fluorescein angiography revealed early hypofluorescence with scarce intrinsic vascularity [Figure 1d] and diffuse late-phase hyperfluorescence with subretinal fluorescein leakage [Figure 1e]. Ultrasonography disclosed a solid, pedunculated lesion inferior to the optic disc with medium internal reflectivity and inferior exudative retinal detachment [Figure 1f]. There was no systemic evidence of tuberous sclerosis or neurofibromatosis.
Figure 1.
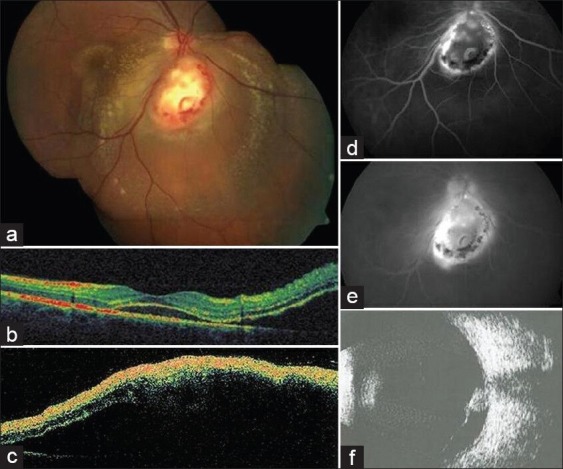
Before photodynamic therapy: (a) Color fundus photograph shows a juxtapapillary, yellow-white retinal lesion with circinate exudation and exudative retinal detachment. (b) Optical coherence tomography (OCT) through the fovea demonstrates serous foveal detachment. (c) OCT through lesion shows preservation of the linear configuration of the retinal pigment epithelial layer with deep optical shadowing, suggesting a tumor of retinal origin. (d) Early hypofluorescence with scarce intrinsic vascularity. (e) Diffuse late-phase hyperfluorescence with subretinal fluorescein leakage and note the lack of typical small, well-defined fine blood vessels over the tumor in the early vascular filling phases. (f) Ultrasonography reveals a non-calcified, pedunculated retinal mass with acoustic solidity and inferior retinal detachment
Patient was diagnosed with presumed acquired retinal astrocytoma. With informed consent from the patient, the tumor was treated with a single session of PDT using standard treatment parameters (50 J/cm2 light dose, 600 mW/cm2 power and 83 s duration). An intravenous injection of 6 mg/m2 body surface area verteporfin over 10 min was performed then laser with emission wavelength of 689 nm was delivered to the entire tumor in one spot (5400 microns), avoiding the optic disc as much as possible.
Following PDT, the visual acuity decreased to hand motion due to dense vitreous hemorrhage that developed during the 1st week after treatment [Figure 2a]. The vitreous hemorrhage cleared spontaneously in 2 months [Figure 2b–d]. Thereafter, the visual acuity gradually improved to 20/40 with complete regression of the tumor into a fibrotic scar-like tissue at 6 months, 20/25 with complete resolution of lipid exudation and exudative retinal detachment at 14 months and 20/20 at 2 years [Figure 3]. At 51 months follow-up, visual acuity remained stable with complete tumor atrophy and no recurrence.
Figure 2.
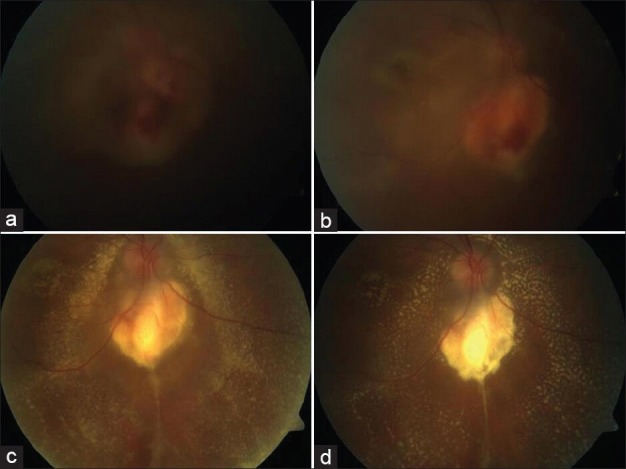
Regression of tumor after photodynamic therapy at: (a) 1 week, (b) 1 months, (c) 2 months and (d) 3 months
Figure 3.
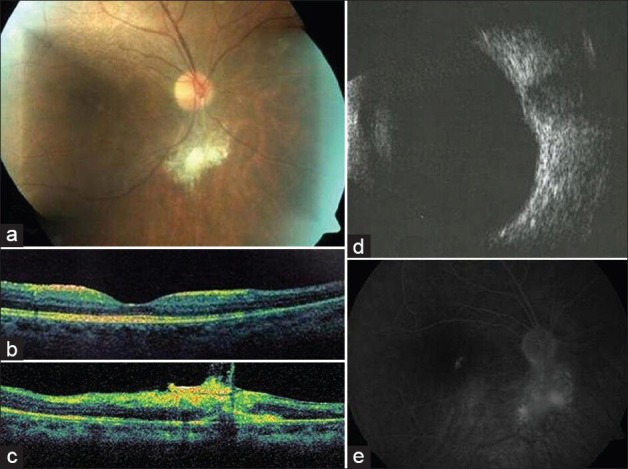
2 years after photodynamic therapy: (a) Marked regression of the tumor. (b) Optical coherence tomography (OCT)(fovea) shows disappearance of the serous retinal detachment. (c) OCT (lesion) precisely demonstrates the intraretinal location of the tumor with overlying epiretinal membrane. (d) Ultrasonography discloses minimal elevation due to residual scar. (e) Late phase angiography showing hyperfluorescence with staining of the residual, intraretinal fibrotic tissue
DISCUSSION
Benign retinal astrocytic lesions include reactive retinal gliosis, astrocytic hamartoma and acquired astrocytoma.1,7 Retinal gliosis usually occurs after trauma, inflammation, or infection. Astrocytic hamartoma is typically stable, diagnosed in early childhood and is often associated with tuberous sclerosis or neurofibromatosis.1 In contrast, acquired astrocytoma is a sporadic tumor that occurs in relatively older individuals, is not associated with tuberous sclerosis and is often symptomatic and progressive.1,3 Thus, any delay in the diagnosis and treatment may result in poor visual outcomes and increased ocular morbidity.
The diagnosis of acquired retinal astrocytoma depends on the clinical finding and imaging results.1 It appears as a yellow-white nodular lesion within the sensory retina. It is typically located in the macular or juxtapapillary region. Fluorescein angiography typically shows small, well-defined fine blood vessels in the tumor in the early vascular filling phases and rather intense, diffuse late staining. Ultrasonography reveals a non-calcified, nodular mass with high internal reflectivity. OCT can be used to document the intraretinal location of the tumor and its highly reflective features. Fine needle aspiration may be required in establishing the correct diagnosis in atypical cases.7
The differential diagnosis of acquired retinal astrocytoma includes choroidal melanoma, solitary idiopathic choroiditis, retinoblastoma and retinal hemangioblastoma.1 The tumor reported in the current case was located in the sensory retina. The confirmation of the retinal location with OCT (especially images from follow-up such as Figure 2c) aided in differentiate it from a tumor of choroidal origin. Furthermore, the color of the tumor was yellow-white and it was hypofluorescent without any evidence of small, well-defined capillaries in the early phase of angiography. In contrast, retinal hemangioblastoma is typically a reddish-pink tumor of the fundus and shows rapid hyperfluorescence in the arterial phase of the fluorescein angiography. Finally, retinoblastoma of comparable size to our case does not usually cause such lipid exudation and exudative retinal detachment. The pedunculated architecture with acoustic solidity and lack of calcification in B-scan ultrasonography also favors the diagnosis of presumed acquired astrocytoma. Despite its atypical features in fluorescein angiography and lack of histopathologic confirmation, our case presumably represents an example for an acquired retinal astrocytoma.1,3,8 We believe that the presence of lipid exudation and exudative retinal detachment is consistent with the aggressive behaviour.8
PDT has been used for treatment of various intraocular tumors, including choroidal hemangioma,9 osteoma,10 melanoma,11 exudative changes over nevus/combined hamartoma,12,13 retinal capillary hemangioma14 and retinal vasoproliferative tumors.15 Due to the poor response of acquired astrocytoma to laser photocoagulation and radiotherapy, recent studies have focused on PDT to avoid enucleation in the management of this lesion.6,7,8 In 2006, Mennel et al.6 reported the first successful treatment with PDT of a symptomatic retinal astrocytic hamartoma associated with tuberous sclerosis. They demonstrated complete resolution of subretinal fluid, disappearance of tumor vessels and improved vision after one session (166 s) of PDT. In 2008, Shields et al.7 described the use of PDT for a pigmented variant of acquired astrocytoma in an 18-year-old female with no history of tuberous sclerosis. They showed minimal involution of the tumor, but complete resolution of macular exudation, edema and subretinal fluid with improvement of visual acuity following one session of PDT with standard parameters. Eskelin et al.8 reported similar outcome in two cases with symptomatic, locally aggressive astrocytomas. They used PDT successfully as a secondary treatment (after failure with prior laser photocoagulation) for a juxtapapillary astrocytoma in a 34-year-old male with tuberous sclerosis and as a primary treatment for a macular astrocytoma in a 68-year-old man without tuberous sclerosis. Following one session of PDT with standard parameters, they observed regression of tumors and complete resolution of exudative retinal detachment in both patients. In our case, a pronounced effect on the symptomatic, juxtapapillary, presumed acquired retinal astrocytoma was obtained with a single session of PDT. The vitreous hemorrhage after PDT presumably occurred due to the rupture of superficial vessels over the tumor.
CONCLUSION
Our paper demonstrates dramatic regression of a symptomatic, juxtapapillary, presumed acquired retinal astrocytoma with complete resolution of exudative retinal detachment and lipid exudation after one session of PDT. Thus, PDT can be considered as a first-line treatment in cases with acquired retinal astrocytoma.
ACKNOWLEGMENTS
We thank Nurgün Demir for her assistance in collecting the data of the patient for this study. Samuray Tuncer, MD had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Shields JA, Shields CL. Intraocular tumors. In: Shields JA, Shields CL, editors. An Atlas and Textbook. 2nd ed. Philadelphia: Lippincott Williams and Wilkins; 2008. pp. 406–27. [Google Scholar]
- 2.Reeser FH, Aaberg TM, Van Horn DL. Astrocytic hamartoma of the retina not associated with tuberous sclerosis. Am J Ophthalmol. 1978;86:688–98. doi: 10.1016/0002-9394(78)90192-7. [DOI] [PubMed] [Google Scholar]
- 3.Shields JA, Eagle RC, Jr, Shields CL, Marr BP. Aggressive retinal astrocytomas in 4 patients with tuberous sclerosis complex. Arch Ophthalmol. 2005;123:856–63. doi: 10.1001/archopht.123.6.856. [DOI] [PubMed] [Google Scholar]
- 4.Bloom SM, Mahl CF. Photocoagulation for serous detachment of the macula secondary to retinal astrocytoma. Retina. 1991;11:416–22. doi: 10.1097/00006982-199111040-00009. [DOI] [PubMed] [Google Scholar]
- 5.Vilaplana D, Castilla M, Poposki V, Alameda F, Shields CL. Acquired retinal astrocytoma managed with endoresection. Retina. 2006;26:1081–2. doi: 10.1097/01.iae.0000254888.63519.3c. [DOI] [PubMed] [Google Scholar]
- 6.Mennel S, Hausmann N, Meyer CH, Peter S. Photodynamic therapy for exudative hamartoma in tuberous sclerosis. Arch Ophthalmol. 2006;124:597–9. doi: 10.1001/archopht.124.4.597. [DOI] [PubMed] [Google Scholar]
- 7.Shields CL, Materin MA, Marr BP, Krepostman J, Shields JA. Resolution of exudative retinal detachment from retinal astrocytoma following photodynamic therapy. Arch Ophthalmol. 2008;126:273–4. doi: 10.1001/archophthalmol.2007.54. [DOI] [PubMed] [Google Scholar]
- 8.Eskelin S, Tommila P, Palosaari T, Kivelä T. Photodynamic therapy with verteporfin to induce regression of aggressive retinal astrocytomas. Acta Ophthalmol. 2008;86:794–9. doi: 10.1111/j.1755-3768.2007.01151.x. [DOI] [PubMed] [Google Scholar]
- 9.Blasi MA, Tiberti AC, Scupola A, Balestrazzi A, Colangelo E, Valente P, et al. Photodynamic therapy with verteporfin for symptomatic circumscribed choroidal hemangioma: Five-year outcomes. Ophthalmology. 2010;117:1630–7. doi: 10.1016/j.ophtha.2009.12.033. [DOI] [PubMed] [Google Scholar]
- 10.Shields CL, Materin MA, Mehta S, Foxman BT, Shields JA. Regression of extrafoveal choroidal osteoma following photodynamic therapy. Arch Ophthalmol. 2008;126:135–7. doi: 10.1001/archopht.126.1.135. [DOI] [PubMed] [Google Scholar]
- 11.Tuncer S, Kir N, Shields CL. Dramatic regression of amelanotic choroidal melanoma with PDT following poor response to brachytherapy. Ophthalmic Surg Lasers Imaging. 2012;43:e38–40. doi: 10.3928/15428877-20120426-01. [DOI] [PubMed] [Google Scholar]
- 12.Rundle P, Rennie I. Management of symptomatic choroidal naevi with photodynamic therapy. Eye (Lond) 2007;21:1531–3. doi: 10.1038/sj.eye.6702623. [DOI] [PubMed] [Google Scholar]
- 13.Cilliers H, Harper CA. Photodynamic therapy with verteporfin for vascular leakage from a combined hamartoma of the retina and retinal pigment epithelium. Clin Experiment Ophthalmol. 2006;34:186–8. doi: 10.1111/j.1442-9071.2006.01150.x. [DOI] [PubMed] [Google Scholar]
- 14.Schmidt-Erfurth UM, Kusserow C, Barbazetto IA, Laqua H. Benefits and complications of photodynamic therapy of papillary capillary hemangiomas. Ophthalmology. 2002;109:1256–66. doi: 10.1016/s0161-6420(02)01059-x. [DOI] [PubMed] [Google Scholar]
- 15.Blasi MA, Scupola A, Tiberti AC, Sasso P, Balestrazzi E. Photodynamic therapy for vasoproliferative retinal tumors. Retina. 2006;26:404–9. doi: 10.1097/01.iae.0000238554.61165.fd. [DOI] [PubMed] [Google Scholar]


