Abstract
AIM: To compare the outcome of the surgical management of left-sided and right-sided diverticular disease.
METHODS: The medical records of 77 patients who were surgically treated for diverticular disease between 1999 and 2010 in a tertiary referral hospital were retrospectively reviewed. The study population was limited to cases wherein the surgical specimen was confirmed as diverticulosis by pathology. Right-sided diverticula were classified as those arising from the cecum, ascending colon, and transverse colon, and those from the descending colon, sigmoid colon, and rectum were classified as left-sided diverticulosis. To assess the changing trend of occurrence of diverticulosis, data were compared with two previous studies of 51 patients.
RESULTS: The proportion of left-sided disease cases was significantly increased compared to the results of our previous studies in 1994 and 2001, (27.5% vs 48.1%, P < 0.05). Moreover, no differences in gender, body mass index, multiplicity of the diverticula, fever, or leukocytosis were noted between patients with right-sided and left-sided disease. However, patients with right-sided disease were significantly younger (50.9 year vs 64.0 year, P < 0.01). Furthermore, left-sided disease was significantly associated with a higher incidence of complicated diverticulitis (89.2% vs 57.5%, P < 0.01), combined resection due to extensive inflammation (21.6% vs 5.0%, P < 0.05), operative complications (51.4% vs 27.5%, P < 0.05), and in-hospital mortality (10.8% vs 0%, P < 0.05), along with longer post-operative hospitalization duration (21.3 ± 10.2 d vs 10.6 ± 8.1 d, P < 0.05).
CONCLUSION: Compared with right-sided diverticular disease, the incidence of left-sided disease in Korea has increased since 2001 and is associated with worse surgical outcomes.
Keywords: Colonic diverticulosis, Diverticular bleeding, Diverticulitis, Poor surgical outcome, Left-sided diverticulitis
Core tip: In Asian countries, including South Korea, diverticulosis is relatively rare and usually detected on the right side of the colon. In the present study, the outcome of the surgical management of left-sided and right-sided diverticular disease was assessed. The results demonstrate that the incidence of left-sided diverticular disease in South Korea is increasing. Furthermore, left-sided disease is generally more severe than right-sided disease and associated with worse surgical outcomes.
INTRODUCTION
Diverticulosis is prevalent in Western countries, and primarily involves multiple pseudo-diverticula, with secondary causes, in the sigmoid colon on the left side[1]. However, diverticula are less common in Asian populations, including Koreans, and develop 10-20 years earlier than in Western populations. These diverticula usually occur as single, congenital, true forms involving the right colon around the appendix[2,3]. The incidence of diverticulosis has recently increased in Asian populations, nearing that of Western countries[4,5], which may be due to a more westernized diet, aging population, increase in colonoscopic screening, and better diagnostic methods.
Although colonic diverticulosis is usually asymptomatic, 10%-20% of patients develop diverticulitis[6]. Patients with uncomplicated diverticulitis generally respond well to outpatient, conservative treatment, such as oral antibiotics. However, surgical treatment may be required for recurrent cases, those with recurrent diverticular bleeding, and for diverticulitis complicated by abscess formation, perforation, intestinal obstruction, or fistula formation[7]. Western countries have developed guidelines for the management of diverticulosis, primarily for left-sided disease, and have recommended the use of surgical techniques, such as colostomy and multistep resection. Percutaneous abscess drainage and elective surgical techniques, including laparoscopy, have also been used[8]. However, no clear guidelines have been established for right-sided disease, and it is not known whether the guidelines for left-sided disease can also be applied.
Studies evaluating the incidence of colonic diverticulosis in South Korea have largely focused on right-sided disease and included relatively small numbers of subjects[9-11]. Previous studies by our group reported in 1994 and 2001 also revealed a relatively high incidence of right-sided diverticulosis[12,13]. Therefore, to provide a more thorough and current assessment, the present study compared the outcomes of surgical management of right-sided and left-sided diverticular diseases and related these findings to those of our previous studies.
MATERIALS AND METHODS
Patient selection
Patients who were surgically treated with open colectomy for symptomatic diverticular disease at the Department of Surgery in Seoul National University Hospital from November 1999 to July 2010 were retrospectively investigated. The medical records were reviewed to collect data concerning patient characteristics, disease complications, operative procedures, morbidity, and mortality. The study population was limited to cases where diverticulosis (with or without inflammation) was confirmed by pathology from a surgical specimen. Diverticula arising from the cecum, ascending colon, and transverse colon were classified as right-sided, and those from the descending colon, sigmoid colon, and rectum were classified as left-sided diverticulosis. Colonic diverticulitis was categorized into three groups according to the clinical manifestations: diverticular bleeding, uncomplicated diverticulitis, and complicated diverticulitis. Complicated diverticulitis was further divided into four grades of severity according to the Hinchey classification system[14]. This study was approved by the Institutional Review Board of the Seoul National University Hospital (IRB No. H-1104-025-357).
Statistical analysis
All analyses were performed with SPSS version 18.0 for Windows (SPSS Inc., Chicago, IL, United States). Statistical analysis of nominal variables was performed with the χ2 test or Fisher’s exact test, where appropriate. Student’s t-tests were used to analyze continuous variables. P-values less than 0.05 were considered to indicate statistically significant differences.
RESULTS
Gender and age distribution of patients
A total of 77 patients were treated for symptomatic diverticular disease during the study period, including 49 men and 28 women with a mean age of 57.2 years (range: 19-87 years). The largest number of patients was in the 60-69 years age group (18; 23.4%) (Figure 1).
Figure 1.
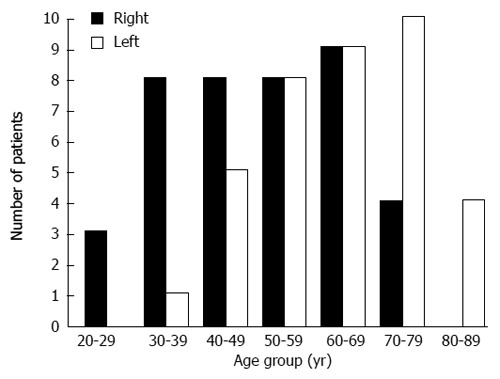
Incidence of colonic diverticular disease according to age group. The mean age of the patients was 57.2 years (range: 19-87 years). After the patients were divided into age groups with 10-year intervals, the 60-69 years age group had the largest number of patients (n = 18, 23.4%).
Symptoms and signs
Nine patients (9; 11.7%) had diverticular bleeding without clinically significant inflammation and 68 (68; 88.3%) had diverticulitis. Fifty-six cases (56; 72.7%) were classified as complicated diverticulitis. The most common surgical indication was colonic perforation (26; 33.8%), treated by emergency operation. Intraperitoneal abscess was the second most common indication (17; 22.1%), for which preoperative percutaneous drainage was performed in six cases (6; 35.3%). Recurrent abdominal pain occurred in 14 patients (14; 18.2%) with symptom duration ranging from 3-74 mo. Seven of these patients were operated on for a second attack, five patients were operated on for a third attack, and two were operated on for more than four attacks. Additional indications included lower gastrointestinal bleeding (9; 11.7%) and sigmoidovesical intraperitoneal fistulae (7; 9.1%). Four preoperatively undiagnosed abdominal masses (4; 5.2%), previously misdiagnosed as colon cancer or locally invasive bladder cancer, were eventually diagnosed as diverticulitis by pathologic examinations.
Comparison of right- and left-sided diverticulosis
Right-sided diverticulosis (40; 51.9%) was slightly more common than left-sided diverticulosis (37; 48.1%). The sigmoid colon was the most frequently involved site (35; 45.5%), followed by the ascending colon (22; 28.5%), cecum (18; 23.4%), descending colon (1; 1.3%), and upper rectum (1; 1.3%). Compared with the combined results of our previous studies in which 27.5% of cases had left-sided diverticulosis, the proportion of patients with left-sided disease was significantly higher in the present study (P < 0.01) (Table 1). The age of patients with left-sided disease was significantly older than for right-sided disease (P < 0.01), but there were no significant differences between the right- and left-sided disease groups in terms of gender, body mass index, multiplicity of diverticula, fever, or leukocytosis (Table 2). All nine patients who had diverticular bleeding had right-side diverticulosis, whereas complicated diverticulitis was more commonly associated (33/37; 89.2%) with left-sided disease (P < 0.01) (Table 2).
Table 1.
Diverticular disease distribution n (%)
Table 2.
Clinical characteristics according to the site of diverticular disease n (%)
| Variables | Right (n = 40) | Left (n = 37) | P value |
| Age (yr)1 | 50.9 ± 15.0 | 64.0 ± 14.0 | < 0.01 |
| Gender (M/F) | 29/11 | 20/17 | 0.09 |
| Disease category | < 0.01 | ||
| Diverticular bleeding | 9 (22.5) | 0 (0) | |
| Uncomplicated diverticulitis | 8 (20.0) | 4 (10.8) | |
| Complicated diverticulitis | 23 (57.5) | 33 (89.2) | |
| Smoking | 14 (35.9) | 8 (21.6) | 0.19 |
| Alcohol consumption | 21 (52.5) | 7 (18.9) | < 0.01 |
| BMI1 | 23.8 ± 2.5 | 23.2 ± 3.0 | 0.35 |
| Fever | 14 (35.0) | 8 (21.6) | 0.19 |
| Leukocytosis | 14 (35.0) | 17 (45.9) | 0.33 |
| Multiple sites | 22 (55.0) | 28 (75.7) | 0.06 |
Date are expressed as mean ± SD. BMI: Body mass index.
Classification of surgical operations
Hemicolectomy (n = 24) was more commonly performed for right-sided disease, followed in frequency by ileocecal resection (n = 13) and subtotal colectomy for bleeding (n = 2). Hartmann’s operation (n = 19) was frequently performed for left-sided disease, and in 18 cases, colonic anastomosis was possible after sigmoid colectomy. Left-sided diverticulosis was significantly associated with longer postoperative hospitalization, combined resection of the small intestine or bladder, operative complications, and higher mortality (all P < 0.05) (Table 3).
Table 3.
Postoperative outcomes according to the site of diverticular disease n (%)
| Variables | Right (n = 40) | Left (n = 37) | P value |
| Operation time (min)1 | 122.4 ± 41.6 | 141.9 ± 51.1 | 0.07 |
| Combined resection | 2 (5.0) | 8 (21.6) | 0.04 |
| Postoperative hospital stay (d)1 | 10.6 ± 8.1 | 21.3 ± 10.2 | 0.01 |
| Complications | 11 (27.5) | 19 (51.4) | 0.03 |
| Mortality | 0 (0) | 4 (10.8) | < 0.05 |
Date are expressed as mean ± SD.
Surgery for diverticular bleeding
All nine cases of colonic resection due to diverticular bleeding without inflammation involved patients who had right-sided diverticulosis. The surgical indications included recurrent bleeding in six cases, hemodynamic instability due to massive bleeding in two cases, and the need for continuous transfusion in one case. The mean age was 64.2 years (range: 43-74 year), which was slightly higher than that of the diverticulitis group (mean: 56.3 year). Seven cases were surgically treated with right hemicolectomy, and two patients underwent subtotal colectomy, as the bleeding site could not be identified. The mean duration of postoperative hospitalization was 9.2 d (range: 4-20 d). There were no mortalities among these patients, with three postoperative complications noted: pneumonia, wound infection, and re-bleeding.
Surgery for diverticulitis according to the Hinchey classification
Cases of complicated diverticulitis were classified by severity according to the Hinchey classification (Table 4). Eight of 68 patients were immunocompromised due to immunosuppressive therapy after kidney transplantation, chemotherapy, hematological cancer, or long-term steroid use (Table 5). Although the incidence of postoperative morbidity in the immunocompromised patients was not significantly different from that in the immunocompetent patients, the mortality rate was significantly higher (P < 0.01). Death in all of the immunocompromised patients was associated with perforated diverticulitis.
Table 4.
Postoperative outcomes of diverticulitis according to Hinchey’s criteria n (%)
| No peritonitis (n = 43) | Peritonitis (n = 25) | P value | |
| Right/left | 25/18 | 6/19 | 0.01 |
| Emergency | 4 (9.3) | 24 (96.0) | < 0.01 |
| Two-stage operation | 1 (2.3) | 20 (80.0) | < 0.01 |
| Operation time (min)1 | 125.1 ± 46.3 | 144.8 ± 44.2 | 0.09 |
| Complications | 8 (18.6) | 19 (76.0) | < 0.01 |
| Mortality | 0 (0) | 4 (16.0) | 0.02 |
Date are expressed as mean ± SD. The no peritonitis group includes patients with uncomplicated diverticulitis or complicated diverticulitis classified as Hinchey grade 1 or 2. The peritonitis group includes patients with complicated diverticulitis classified as Hinchey grade 3 and 4.
Table 5.
Postoperative outcomes of diverticulitis according to the preoperative immune status n (%)
| Immunocompetent (n = 60) | Immunocompromised (n = 8) | P value | |
| Right/left | 29/31 | 2/6 | 0.28 |
| Symptom duration (d)1 | 238.2 ± 66.3 | 7.0 ± 1.8 | < 0.01 |
| Hinchey grade 3, 4 | 19 (31.7) | 6 (75.0) | 0.04 |
| Emergency operation | 22 (36.7) | 6 (75) | 0.06 |
| Two-stage operation | 14 (23.3) | 7 (87.5) | < 0.01 |
| Complications | 22 (36.7) | 5 (62.5) | 0.25 |
| Mortality | 0 (0) | 4 (50.0) | < 0.01 |
Date are expressed as mean ± SD.
DISCUSSION
Autopsy and radiologic findings indicate that colonic diverticulosis is present in 35%-50% of the population in Western countries, rarely in the right side, and most commonly involving the sigmoid colon[15-17]. Although diverticulosis is relatively rare in Asian countries, usually detected in the right side of the colon, the incidence in patients undergoing colonoscopy is increasing (12.1%-9.7%)[4,18]. In most cases, right-sided diverticula are congenitally formed as a result of the out-pouching of the whole layer of the weakened intestinal wall[19]. In contrast, left-sided disease is usually associated with secondary causes, including diet, constipation, increased colonic pressure, defecation habits, and irritable bowel syndrome. Consequently, left-sided diverticulosis more commonly occurs in older patients in South Korea[20,21], as indicated by the present study.
Diverticulosis without inflammation is usually asymptomatic, though right-sided diverticulosis is associated with massive bleeding due to the presence of a relatively thinner intestinal wall[22]. Diverticular bleeding is the most common cause (30%-40%) of lower gastrointestinal bleeding among the elderly, particularly with comorbidities[23]. It rarely occurs as a complication of diverticulitis. Although more than 80% of cases of diverticular bleeding spontaneously resolve with conservative treatment, surgical treatment may be required for recurrent bleeding, hemodynamic instability due to massive bleeding, and require continuous transfusion[24]. The risk for postoperative recurrent bleeding following a segmental resection for a localized bleeding site is reported to be approximately 14%[25,26]. If the bleeding site cannot be localized, a subtotal colectomy can be indicated. In the present study, one patient underwent a subtotal colectomy because of re-bleeding 18 d after a right hemicolectomy was performed for bleeding identified in the ascending colon by preoperative colonoscopy.
The indications for colectomy after conservative treatment of acute diverticulitis should be based on the clinical manifestations rather than the number of recurrences, in accordance with the guidelines of the American Society of Colorectal Surgery[8]. The clinical manifestations of diverticulitis include fever, abdominal pain, and tenderness. In some cases, a tender abdominal mass, colonic obstruction, and diffuse peritonitis may be present[7]. However, in a case of complicated diverticulitis with fistula, adhesion, or abscess, surgical intervention is recommended even if conservative treatment is temporarily successful, as long-term resolution of the disease is unlikely. The symptoms of colonic diverticulitis differ according to the location of the involved site, and right-sided diverticulitis is often difficult to distinguish from acute appendicitis[27]. Although there are no surgical guidelines for the management of right-sided disease, right hemicolectomy or ileocecal resection is usually performed, depending on the extent and severity of the diverticulitis.
Although Welch et al[28] recommended a one-stage operation with resection of the involved site, a two-stage operation with Hartmann’s procedure is performed if severe contamination of the peritoneum is present. This was the technique of choice in 19 cases in the present study, whereas primary anastomosis was possible after colonic resection in the remaining cases. Left-sided disease frequently required a multi-stage operation and was more often associated with postoperative morbidity and mortality than right-sided diverticular disease, likely due to the progression of the disease to a more complicated form. It has been argued that the higher complication rate and recurrence in younger patients is a result of delayed diagnosis[29]. However, it has also been suggested that this increased disease severity warrants a more aggressive surgical treatment[30]. In the present study, surgical procedures did not vary according to patient age or gender, or location of the diverticulosis. However, among immunocompromised patients, diverticulitis manifested as colonic perforation in 40% of cases, of which the majority required an emergency operation, which is consistent with previous reports[31-33]. The rapid progression of diverticulitis due to impaired control of inflammation is likely to be responsible for the high mortality rate[34]. Therefore, a two-stage operation with resection of the involved site is preferred over a primary anastomosis.
A limitation of the present study is that it was of a retrospective design. In addition, the patients were operated on at a tertiary referral hospital and were therefore likely to have therapeutically nonresponsive diverticulitis. Thus, the conclusions of this study may not apply to the general population. However, to the best of our knowledge, this is the only study comparing the surgical outcomes of right-sided and left-sided colonic diverticular disease from a single institute.
In conclusion, the proportion of left-sided diverticulosis is increasing in South Korea. Because left-sided colonic diverticular disease is associated with older age and with more complicated disease expression with worse outcomes, surgeons should be particularly attentive in assessing surgical indications.
ACKNOWLEDGMENTS
The authors are indebted to Patrick Barron, Professor Emeritus, Tokyo Medical University and Adjunct Professor, Seoul National University Bundang Hospital for his pro bono editing of this manuscript.
COMMENTS
Background
In Western countries, diverticula primarily occur as multiple pseudo-diverticula with secondary causes in the sigmoid colon on the left side. However, in Korean and other Asian populations, diverticula usually occur as a single, congenital, true form involving the right colon around the appendix. Furthermore, these right-sided diverticula develop 10-20 years earlier than those in Western populations.
Research frontiers
Recent work has indicated an increasing incidence of diverticulosis in Asian populations. This increase may be due to westernization of diet, aging of the population, increase in colonoscopic screening, and better diagnostic methods. As a result, the formerly rare condition has become more common, with incidence rates similar to those found in Western countries.
Innovations and breakthroughs
Surgeons should be particularly attentive in assessing surgical indications for left-sided colonic diverticular disease, as the results indicate an association with advanced age and more complicated disease expression.
Applications
Korean and Western patients with diverticulosis may demonstrate different disease outcomes due to ethnic or dietary factors. Although further study is needed to elucidate the role of these factors, the results of this study demonstrate that the incidence of diverticulitis is increasing in South Korea.
Terminology
Diverticulitis is used to describe the inflammation of a diverticulum or diverticula, which is commonly accompanied by gross or microscopic perforation. Diverticulosis refers to the presence of noninflamed diverticula.
Peer review
This is a retrospective review of surgically treated diverticular disease in a tertiary referral hospital in South Korea. The study compares the incidence of right- and left-sided disease in a Korean population, and compares the results with previous studies to demonstrate an increase in the incidence over the past two decades.
Footnotes
P- Reviewer: Afshar S, Bali C, O’Dwyer PJ S- Editor: Qi Y L- Editor: A E- Editor: Zhang DN
References
- 1.Schuler JG, Bayley J. Diverticulitis of the cecum. Surg Gynecol Obstet. 1983;156:743–748. [PubMed] [Google Scholar]
- 2.Connell AM. Pathogenesis of diverticular disease of the colon. Adv Intern Med. 1977;22:377–395. [PubMed] [Google Scholar]
- 3.Almy TP, Howell DA. Medical progress. Diverticular disease of the colon. N Engl J Med. 1980;302:324–331. doi: 10.1056/NEJM198002073020605. [DOI] [PubMed] [Google Scholar]
- 4.Song JH, Kim YS, Lee JH, Ok KS, Ryu SH, Lee JH, Moon JS. Clinical characteristics of colonic diverticulosis in Korea: a prospective study. Korean J Intern Med. 2010;25:140–146. doi: 10.3904/kjim.2010.25.2.140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cho EY, Choi CS, Kim JW, Kweon JH, Kim TH, Seo GS, Jo HJ, Choi SC, Nah YH. [Primary duodenal choriocarcinoma presenting as massive intestinal bleeding and metastasis to brain] Korean J Gastroenterol. 2006;48:128–131. [PubMed] [Google Scholar]
- 6.Ferzoco LB, Raptopoulos V, Silen W. Acute diverticulitis. N Engl J Med. 1998;338:1521–1526. doi: 10.1056/NEJM199805213382107. [DOI] [PubMed] [Google Scholar]
- 7.Jacobs DO. Clinical practice. Diverticulitis. N Engl J Med. 2007;357:2057–2066. doi: 10.1056/NEJMcp073228. [DOI] [PubMed] [Google Scholar]
- 8.Rafferty J, Shellito P, Hyman NH, Buie WD. Practice parameters for sigmoid diverticulitis. Dis Colon Rectum. 2006;49:939–944. doi: 10.1007/s10350-006-0578-2. [DOI] [PubMed] [Google Scholar]
- 9.Choi MH, Hwang JK, Kim JH. Operative treatment of the colonic diverticular disease. J Korean Surg Soc. 2003;65:534–540. [Google Scholar]
- 10.Kim KY, Kim IK, Jung SW, Park KH, Park YJ. Analysis on the surgical treatment of colonic diverticulitis. J Korean Surg Soc. 2007;73:36–41. [Google Scholar]
- 11.Moon BC, Kim HS. Developmental pattern and treatment in colon diverticular disease. J Korean Soc Coloproctol. 2007;23:305–311. [Google Scholar]
- 12.Chung HD, Park KJ, Heo SC, Kang SB. Surgical treatment for diverticular disease of the colon. J Korean Soc Coloproctol. 2001;17:243–250. [Google Scholar]
- 13.Min SG, Park JG, Choe KJ, Kim JP. Surgical management of diverticular disease of the colon. J Korean Soc Coloproctol. 1994;10:303–311. [Google Scholar]
- 14.Hinchey EJ, Schaal PG, Richards GK. Treatment of perforated diverticular disease of the colon. Adv Surg. 1978;12:85–109. [PubMed] [Google Scholar]
- 15.Hughes LE. Postmortem survey of diverticular disease of the colon. II. The muscular abnormality of the sigmoid colon. Gut. 1969;10:344–351. doi: 10.1136/gut.10.5.344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Miangolarra CJ. Diverticulitis of the right colon: an important surgical problem. Ann Surg. 1961;153:861–870. doi: 10.1097/00000658-196106000-00006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Nakaji S, Danjo K, Munakata A, Sugawara K, MacAuley D, Kernohan G, Baxter D. Comparison of etiology of right-sided diverticula in Japan with that of left-sided diverticula in the West. Int J Colorectal Dis. 2002;17:365–373. doi: 10.1007/s00384-002-0403-x. [DOI] [PubMed] [Google Scholar]
- 18.Lee KM, Paik CN, Chung WC, Jung SH, Chang UI, Yang JM. Clinical significance of colonic diverticulosis associated with bowel symptoms and colon polyp. J Korean Med Sci. 2010;25:1323–1329. doi: 10.3346/jkms.2010.25.9.1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rodkey GV, Welch CE. Diverticulitis of the colon: evolution in concept and therapy. Surg Clin North Am. 1965;45:1231–1243. doi: 10.1016/s0039-6109(16)37690-3. [DOI] [PubMed] [Google Scholar]
- 20.Kim JS, Cha SG, Kim YT, Yoon YB, Song IS, Choi KW, Kim CY, Cho JM, Choi BI. The prevalence and clinical features of diverticular disease of the colon. Korean J Gastroenterol. 1993;25:305–314. [Google Scholar]
- 21.Kim HU, Kim YH, Choe WH, Kim JH, Youk CM, Lee JU, Shim SG, Son HJ, Rhee PL, Kim JJ, et al. [Clinical characteristics of colonic diverticulitis in Koreans] Korean J Gastroenterol. 2003;42:363–368. [PubMed] [Google Scholar]
- 22.Wong SK, Ho YH, Leong AP, Seow-Choen F. Clinical behavior of complicated right-sided and left-sided diverticulosis. Dis Colon Rectum. 1997;40:344–348. doi: 10.1007/BF02050427. [DOI] [PubMed] [Google Scholar]
- 23.Zuccaro G. Management of the adult patient with acute lower gastrointestinal bleeding. American College of Gastroenterology. Practice Parameters Committee. Am J Gastroenterol. 1998;93:1202–1208. doi: 10.1111/j.1572-0241.1998.00395.x. [DOI] [PubMed] [Google Scholar]
- 24.Chen CY, Wu CC, Jao SW, Pai L, Hsiao CW. Colonic diverticular bleeding with comorbid diseases may need elective colectomy. J Gastrointest Surg. 2009;13:516–520. doi: 10.1007/s11605-008-0731-4. [DOI] [PubMed] [Google Scholar]
- 25.Parkes BM, Obeid FN, Sorensen VJ, Horst HM, Fath JJ. The management of massive lower gastrointestinal bleeding. Am Surg. 1993;59:676–678. [PubMed] [Google Scholar]
- 26.McGuire HH. Bleeding colonic diverticula. A reappraisal of natural history and management. Ann Surg. 1994;220:653–656. doi: 10.1097/00000658-199411000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lee IK, Kim SH, Lee YS, Kim HJ, Lee SK, Kang WK, Ahn CH, Oh ST, Jeon HM, Kim JG, et al. Diverticulitis of the right colon: tips for preoperative diagnosis and treatment strategy. J Korean Soc Coloproctol. 2007;23:223–231. [Google Scholar]
- 28.Welch CE, Allen AW, Donaldson GA. An appraisal of resection of the colon for diverticulitis of the sigmoid. Ann Surg. 1953;138:332–343. doi: 10.1097/00000658-195313830-00005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Vignati PV, Welch JP, Cohen JL. Long-term management of diverticulitis in young patients. Dis Colon Rectum. 1995;38:627–629. doi: 10.1007/BF02054123. [DOI] [PubMed] [Google Scholar]
- 30.Minardi AJ, Johnson LW, Sehon JK, Zibari GB, McDonald JC. Diverticulitis in the young patient. Am Surg. 2001;67:458–461. [PubMed] [Google Scholar]
- 31.Perkins JD, Shield CF, Chang FC, Farha GJ. Acute diverticulitis. Comparison of treatment in immunocompromised and nonimmunocompromised patients. Am J Surg. 1984;148:745–748. doi: 10.1016/0002-9610(84)90429-x. [DOI] [PubMed] [Google Scholar]
- 32.Tyau ES, Prystowsky JB, Joehl RJ, Nahrwold DL. Acute diverticulitis. A complicated problem in the immunocompromised patient. Arch Surg. 1991;126:855–858; discussion 858-859. doi: 10.1001/archsurg.1991.01410310065009. [DOI] [PubMed] [Google Scholar]
- 33.Lederman ED, Conti DJ, Lempert N, Singh TP, Lee EC. Complicated diverticulitis following renal transplantation. Dis Colon Rectum. 1998;41:613–618. doi: 10.1007/BF02235270. [DOI] [PubMed] [Google Scholar]
- 34.Hall J, Hammerich K, Roberts P. New paradigms in the management of diverticular disease. Curr Probl Surg. 2010;47:680–735. doi: 10.1067/j.cpsurg.2010.04.005. [DOI] [PubMed] [Google Scholar]


