Abstract
An insufficient future liver remnant (FLR) is associated with post-hepatectomy liver failure. Associating liver partition and portal vein ligation for stage hepatectomy (ALPPS) has been shown to be effective for the induction of rapid FLR hypertrophy so as to improve the resectability in patients with insufficient FLR. We hereby report our experience of this novel approach for a 6-year-old patient with hepatoblastoma. Computed tomography showed a hepatoblastoma measuring 12.5 cm × 9.9 cm × 11.7 cm in the right liver (Couinaud segment IV, V and VIII). Volumetric assessment of the FLR i.e., left lateral section was 112.6 mL i.e., 21.2% of the estimated total liver volume. In view of the small-for-size FLR, ALPPS was contemplated. An anterior approach was adopted for the in-situ parenchymal split without mobilisation of the right liver. FLR volumetry on the seventh postoperative day was 160.7 mL, which represented a 46.1% gain in volume, and a FLR/ESLV ratio of 30.2%. A right trisectionectomy was performed on the eighth postoperative day. Postoperative recovery was uneventful. Patient was discharged on day 16 after the first operation. To our knowledge, this was the first report that showed the applicability of ALPPS to a paediatric patient.
Keywords: Associating liver partition and portal vein ligation for stage hepatectomy, Hepatectomy, Portal vein, Hepatoblastoma, In-situ split
Core tip: Associating liver partition and portal vein ligation for stage hepatectomy (ALPPS) is a novel surgical approach that was first reported in 2012. This surgical approach has revolutionized the management of patients with resectable liver tumors and inadequate future liver remnant volume. Nonetheless, the global preliminary experience is so far limited to the use in adult patients with small future liver remnant. With the favorable outcome in adult patients reported so far, we have adopted this technique to a young patient with a right liver hepatoblastoma and small left lateral section. To our knowledge, this is the first report that showed the feasibility of ALPPS in a pediatric patient.
INTRODUCTION
Hepatectomy remains an important curative treatment for both primary and secondary malignant liver tumors. However, postoperative liver failure (PLF) remains the commonest cause of death after major hepatectomy in spite of the recent advancement in operative techniques and perioperative care. An insufficient future liver remnant (FLR) is associated with PLF. The conventional approach is to perform portal vein embolization to induce FLR hypertrophy which normally requires 4-8 wk before proceeding to hepatectomy. However, disease progression while waiting for sufficient hypertrophy could result in drop-out from receiving curative resection. Associating liver partition and portal vein ligation for stage hepatectomy (ALPPS) has been recently advocated to induce rapid FLR hypertrophy that significantly shortens the time for the second stage hepatectomy[1,2]. We report our experience of this approach for a child with hepatoblastoma.
CASE REPORT
A 6-year old girl presented with one-week history of abdominal distension and malaise. Physical examination revealed hepatomegaly. Her body weight and height was 16.9 kg and 116 cm respectively. The serum alpha-fetoprotein (AFP) level at the time of diagnosis was 399035 ng/mL. Hepatitis serology was negative. Computed tomography revealed a 12.5 cm × 9.9 cm × 11.7 cm mass lesion occupying Couinaud segment IV, V and VIII. Tumor biopsy confirmed hepatoblastoma. Four cycles of systemic chemotherapy using cisplatin, vincristine and 5-FU were given for 8 wk. However, serum AFP level was elevated to 477880 ng/mL despite chemotherapy and she was then assessed for resection.
Her liver function tests were normal. A right trisectionectomy was deemed necessary for complete tumor clearance. However, volumetric measurement of the FLR i.e., left lateral section (LLS) was only 112.6 mL (Figure 1). The estimated total liver volume (ESLV)[3] was 531.9 mL with FLR/ESLV ratio of 21.2%. Given the recent exposure to hepatotoxic chemotherapy, the FLR was considered small-for-size after major hepatectomy and would render the patient at risk of PLF. On the other hand, induction of FLR hypertrophy via right portal vein embolization was failed as the fine-caliber right portal vein of this child was not accessible by the percutaneous approach. Hence, ALPPS was performed.
Figure 1.
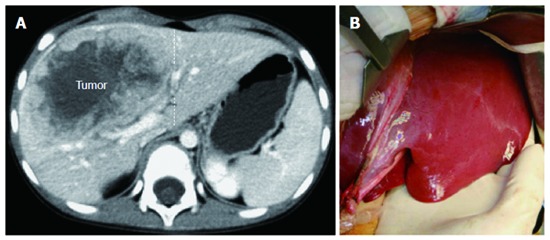
Cross-sectional imaging (A) and operative view (B) of the spatial relationship between the liver mass and the small left lateral section.
In the first part of ALPPS on 24th October 2013, right portal vein ligation and in-situ liver split was performed. The right hepatic artery and left hepatic vessels were safeguarded. An ‘‘anterior approach’’ was adopted for the in-situ split procedure without mobilization of the right liver. Parenchymal split was performed by Cavitron ultrasonic surgical aspirator (Valleylab, Boulder, CO). The segment IV portal pedicles and bile ducts were divided until the left hilar plate was exposed (Figure 2). The parenchymal split was continued until segment IV turned dusky in color that signified complete ‘‘deportalization’’. A methylene blue test was performed to exclude bile leakage from the transection surface. No drain was placed nor any plastic bag wrapping of the right liver was performed. Postoperative recovery was uneventful. FLR volumetry on the seventh postoperative day was 160.7 mL, which represented a 46.1% gain in volume, and a FLR/ESLV ratio of 30.2% (Figure 3).
Figure 2.
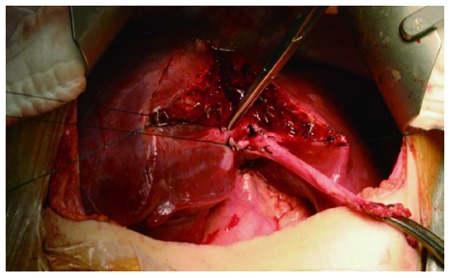
Right portal vein ligation and in-situ split between segment 4 and left lateral section. A main branch of segment 4 portal pedicle was slung and later divided.
Figure 3.
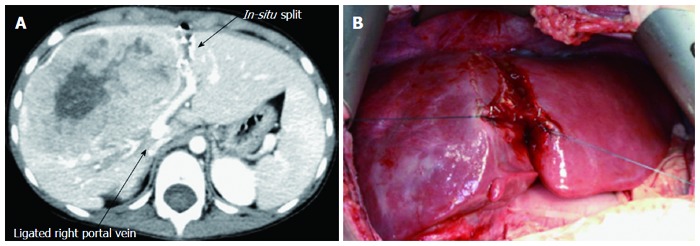
Volumetric changes induced by associating liver partition and portal vein ligation for stage hepatectomy. A: Cross-sectional imaging on seventh postoperative day after in-situ split shows significant left lateral section hypertrophy; B: The operative view shows the dusky-looking segment 4 and the hypertrophied left lateral section.
The second part of ALPPS entailed a completion right trisectionectomy on the eighth postoperative day. Minimal adhesion was encountered at the liver hilum or at the liver surface. The right liver was mobilized after division of the right hepatic artery, right biliary pedicle, right and middle hepatic vein. By this manner, the chance of iatrogenic tumor rupture during forceful mobilization of the right liver was much reduced. The liver function test returned to normal levels five days later. No postoperative morbidity occurred. Histological examination confirmed hepatoblastoma with clear resection margin. Immunohistochemical staining of liver parenchyma for Ki-67 showed the proliferation index of right liver and LLS to be 2% and 20% (Figure 4) respectively. Patient returned home on day 16 after the first operation. Her serum AFP declined to 4011 ng/mL at 8 wk after the operation.
Figure 4.
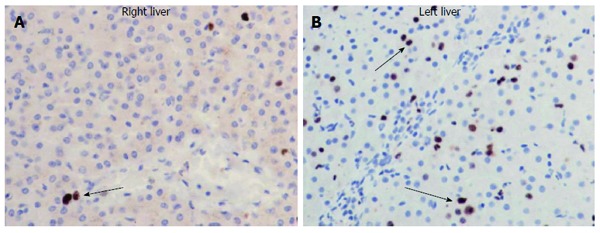
Immunohistochemical staining for Ki-67 (brown nuclei) showed the significant difference in cellular proliferative activity between the right liver (A) and left lateral section (B) after associating liver partition and portal vein ligation (arrows) for stage hepatectomy.
DISCUSSION
Liver resection remains an important curative treatment for both primary and secondary malignant liver tumors. Resectability is determined by both tumor factors and preoperative liver function status. In patients with large tumors, or centrally locating tumors, extended liver resection is often required for oncological clearance with adequate resection margin. However, this frequently gives rise to situation when the FLR could be too small to sustain postoperative essential hepatic function leading to PLF, a condition that remains the most common cause of mortality after major hepatectomy. Recently, a large-scale study of 301 patients by Kishi et al[4] showed the potential hazardous consequence of small FLR. In this study, the incidence of mortality due to liver failure was significantly higher in patients with FLR < 20% total liver volume than those with FLR ≥ 20% total liver volume. In order to prevent PLF, Makuuchi et al[5] proposed the use of portal vein embolization (PVE) to augment the FLR volume in the early 1990s. Since then, PVE or portal vein ligation (PVL) has become a standard procedure to prepare patients with insufficient FLR before extended hepatectomy. In a meta-analysis of 37 studies on 1088 patients, PVE with various methods of embolization induced a mean volumetric increment by 8%-27% over a period of 2-6 wk[6]. Alternatively, PVL achieved a FLR volumetric increment by 38%-53% over a period of 4-8 wk[7-9]. Nonetheless, a major drawback of PVE or PVL is that sufficient volume could only be gained over ‘weeks’ and the chance of tumor progression during this waiting period remains substantial.
In March 2012, Schnitzbauer et al[1] reported a novel strategy on inducing FLR hypertrophy by right portal vein ligation combined with in-situ liver split in 25 patients with malignant liver tumors. A procedure that was later termed as ALPPS[2]. This study showed that FLR volume could be rapidly increased by 74% over an interval of 9 d. Given the significant augmentation of FLR within a short period of time, there was no incidence of tumor progression in the interval and all patients were able to undergo the second staged hepatectomy. Such positive findings were reproduced in another study by Alvarez et al[10] which showed an actual volume gain of 303 mL in an interval of 6 d followed by a 100% R0 resection rate. It was postulated that the rapid hypertrophic effect observed was largely attributed to the in-situ split procedure that led to complete segment IV deportalization and hence, prevented formation of vascular collaterals between the left and right liver that could otherwise undermine the completeness of right portal vein occlusion alone.
Nonetheless, this operative approach is not without risk and has been criticized for the high incidence of bile leakage and sepsis after in-situ split. However, it was conceivable that clear identification and control before ligation of intraparenchymal bile ducts offered by the judicious use of ultrasonic dissector, and the use of methylene blue test in our operative technique may help to lower the incidence of biliary complications associated with ALPPS[11].
The reason for applying ALPPS in this child was compelling as her last dose of chemotherapy was already terminated for over 4 wk prior to surgery in order to allow her recovery from the toxicity of chemotherapy. Any further delay of 4-8 wk to nurture FLR hypertrophy as in conventional PVE or PVL would put her at risk of tumor progression, from resectable to unresectable disease. In view of a speedy FLR hypertrophy within a short period of time, it was considered worthwhile to perform ALPPS for this child. To our knowledge, this was the first report that showed the applicability of ALPPS to a pediatric patient.
COMMENTS
Case characteristics
A young child with huge liver mass.
Clinical diagnosis
A right liver hepatoblastoma.
Differential diagnosis
With a high rising serum alpha-fetoprotein level, another possibility is hepatocellular carcinoma.
Laboratory diagnosis
The serum alpha-fetoprotein was 399035 ng/mL at the time of diagnosis.
Imaging diagnosis
Computed tomography showed a 12.5 cm × 9.9 cm × 11.7 cm tumor in right liver.
Pathological diagnosis
Histology confirmed hepatoblastoma. Liver biopsy of the right liver and left lateral section showed Ki-67 to be 2% and 20% respectively, suggestive of increased cellular proliferation in the liver remnant.
Term explanation
Associating liver partition and portal vein ligation for stage hepatectomy (ALPPS) is the synonym for right portal vein ligation and in-situ liver split.
Experiences and lessons
Induction of liver hypertrophy is a feasible approach for paediatric patient with insufficient future liver remnant (FLR). The clinical experience with ALPPS in adult patients is transferrable to paediatric patient.
Peer review
The rapid FLR hypertrophy is related to complete portal flow diversion to the left lateral section by the in-situ split resulting in enhanced cellular proliferation.
Footnotes
P- Reviewer: Hashimoto N, Kayadibi H S- Editor: Qi Y L- Editor: A E- Editor: Liu XM
References
- 1.Schnitzbauer AA, Lang SA, Goessmann H, Nadalin S, Baumgart J, Farkas SA, Fichtner-Feigl S, Lorf T, Goralcyk A, Hörbelt R, et al. Right portal vein ligation combined with in situ splitting induces rapid left lateral liver lobe hypertrophy enabling 2-staged extended right hepatic resection in small-for-size settings. Ann Surg. 2012;255:405–414. doi: 10.1097/SLA.0b013e31824856f5. [DOI] [PubMed] [Google Scholar]
- 2.de Santibañes E, Clavien PA. Playing Play-Doh to prevent postoperative liver failure: the “ALPPS” approach. Ann Surg. 2012;255:415–417. doi: 10.1097/SLA.0b013e318248577d. [DOI] [PubMed] [Google Scholar]
- 3.Urata K, Kawasaki S, Matsunami H, Hashikura Y, Ikegami T, Ishizone S, Momose Y, Komiyama A, Makuuchi M. Calculation of child and adult standard liver volume for liver transplantation. Hepatology. 1995;21:1317–1321. [PubMed] [Google Scholar]
- 4.Kishi Y, Abdalla EK, Chun YS, Zorzi D, Madoff DC, Wallace MJ, Curley SA, Vauthey JN. Three hundred and one consecutive extended right hepatectomies: evaluation of outcome based on systematic liver volumetry. Ann Surg. 2009;250:540–548. doi: 10.1097/SLA.0b013e3181b674df. [DOI] [PubMed] [Google Scholar]
- 5.Makuuchi M, Thai BL, Takayasu K, Takayama T, Kosuge T, Gunvén P, Yamazaki S, Hasegawa H, Ozaki H. Preoperative portal embolization to increase safety of major hepatectomy for hilar bile duct carcinoma: a preliminary report. Surgery. 1990;107:521–527. [PubMed] [Google Scholar]
- 6.Abulkhir A, Limongelli P, Healey AJ, Damrah O, Tait P, Jackson J, Habib N, Jiao LR. Preoperative portal vein embolization for major liver resection: a meta-analysis. Ann Surg. 2008;247:49–57. doi: 10.1097/SLA.0b013e31815f6e5b. [DOI] [PubMed] [Google Scholar]
- 7.Capussotti L, Muratore A, Baracchi F, Lelong B, Ferrero A, Regge D, Delpero JR. Portal vein ligation as an efficient method of increasing the future liver remnant volume in the surgical treatment of colorectal metastases. Arch Surg. 2008;143:978–982; discussion 982. doi: 10.1001/archsurg.143.10.978. [DOI] [PubMed] [Google Scholar]
- 8.Aussilhou B, Lesurtel M, Sauvanet A, Farges O, Dokmak S, Goasguen N, Sibert A, Vilgrain V, Belghiti J. Right portal vein ligation is as efficient as portal vein embolization to induce hypertrophy of the left liver remnant. J Gastrointest Surg. 2008;12:297–303. doi: 10.1007/s11605-007-0410-x. [DOI] [PubMed] [Google Scholar]
- 9.Kianmanesh R, Farges O, Abdalla EK, Sauvanet A, Ruszniewski P, Belghiti J. Right portal vein ligation: a new planned two-step all-surgical approach for complete resection of primary gastrointestinal tumors with multiple bilateral liver metastases. J Am Coll Surg. 2003;197:164–170. doi: 10.1016/S1072-7515(03)00334-X. [DOI] [PubMed] [Google Scholar]
- 10.Alvarez FA, Ardiles V, Sanchez Claria R, Pekolj J, de Santibañes E. Associating liver partition and portal vein ligation for staged hepatectomy (ALPPS): tips and tricks. J Gastrointest Surg. 2013;17:814–821. doi: 10.1007/s11605-012-2092-2. [DOI] [PubMed] [Google Scholar]
- 11.Lam CM, Lo CM, Liu CL, Fan ST. Biliary complications during liver resection. World J Surg. 2001;25:1273–1276. doi: 10.1007/s00268-001-0109-1. [DOI] [PubMed] [Google Scholar]


