Abstract
Ulcerative colitis and Crohn’s disease are the major phenotypes of the idiopathic inflammatory bowel disease (IBD), which afflicts millions of individuals throughout the world with debilitating symptoms, impairing function and quality of life. Current medications are aimed at reducing the symptoms or suppressing exacerbations. However, patients require life-long medications, and this can lead to drug dependency, loss of response together with adverse side effects. Indeed, drug side effects become additional morbidity factor in many patients on long-term medications. Nonetheless, the efficacy of anti-tumour necrosis factors (TNF)-α biologics has validated the role of inflammatory cytokines notably TNF-α in the exacerbation of IBD. However, inflammatory cytokines are released by patients’ own cellular elements including myeloid lineage leucocytes, which in patients with IBD are elevated with activation behaviour and prolonged survival. Accordingly, these leucocytes appear logical targets of therapy and can be depleted by adsorptive granulocyte/monocyte apheresis (GMA) with an Adacolumn. Based on this background, recently GMA has been applied to treat patients with IBD in Japan and in the European Union countries. Efficacy rates have been impressive as well as disappointing. In fact the clinical response to GMA seems to define the patients’ disease course, response to medications, duration of active disease, and severity at entry. The best responders have been first episode cases (up to 100%) followed by steroid naïve and patients with a short duration of active disease prior to GMA. Patients with deep ulcers together with extensive loss of the mucosal tissue and cases with a long duration of IBD refractory to existing medications are not likely to benefit from GMA. It is clinically interesting that patients who respond to GMA have a good long-term disease course by avoiding drugs including corticosteroids in the early stage of their IBD. Additionally, GMA is very much favoured by patients for its good safety profile. GMA in 21st century reminds us of phlebotomy as a major medical practice at the time of Hippocrates. However, in patients with IBD, there is a scope for removing from the body the sources of pro-inflammatory cytokines and achieve disease remission. The bottom line is that by introducing GMA at an early stage following the onset of IBD or before patients develop extensive mucosal damage and become refractory to medications, many patients should respond to GMA and avoid pharmacologics. This should fulfill the desire to treat without drugs.
Keywords: Inflammatory bowel disease, Myeloid lineage leucocytes, Adsorptive granulocytes/monocytes apheresis, Corticosteroid sparing effect, Complement activation fragments, Treating inflammatory bowel disease without drugs
Core tip: The efficacy of anti-tumour necrosis factor-α biologics has validated the role of inflammatory cytokines in the exacerbation of inflammatory bowel disease (IBD). However, inflammatory cytokines are released by patients’ own cellular elements including myeloid lineage leucocytes, which in patients with IBD are elevated with activation behaviour. Accordingly, these leucocytes appear logical targets of therapy and can be depleted by adsorptive granulocyte/monocyte apheresis (GMA). Therefore, in patients with IBD, there is a scope for removing from the body the sources of pro-inflammatory cytokines, and this should fulfill the desire to treat without drugs. Therefore, by introducing GMA at an early stage following the onset of IBD or before patients develop extensive mucosal damage, many patients should respond to GMA and avoid pharmacologics.
INFLAMMATORY BOWEL DISEASE
The idiopathic inflammatory bowel disease (IBD), which includes ulcerative colitis (UC) and Crohn’s diseases (CD) is an immune disorder characterized by inflammation of the gastrointestinal tract in genetically susceptible individuals when exposed to environmental risk factors[1]. Therefore, IBD has long been thought to have a genetic basis and involves response of the immune mechanisms to certain environmental agent(s). The development of IBD among monozygotic twins and an increased incidence in countries undergoing rapid Westernization highlight the relevance of genetic predisposition together with environmental factors in disease pathogenesis and incidence[2]. What all these mean is that in patients with IBD, the intestinal immune profile becomes dysregulated showing exaggerated response to triggers that would have been insignificant in an individual without genetic susceptibility factor.
However, it is clinically relevant to bear in mind that whereas UC is confined to the colon and the rectum (large intestine), CD may affect any part of the gut from the mouth to the perianal region. Most commonly CD affects the distal ileum and the colon; up to 65% of CD patients present with small intestinal involvement. Both UC and CD are debilitating chronic health disorders that afflict millions of individuals throughout the world with symptoms, which impair function and quality of life.
Further, the human intestine is host to thousands of bacterial species, collectively referred to as the intestinal microbiota or microflora[3]. While it is understood that the presence of this microbiota is essential for human health, this relationship may become unbalanced, and translate into development of UC or CD[3,4]. Accordingly, both clinical and experimental observations indicate that IBD flare-ups are triggered by a combined loss of the so-called intestinal barrier function and a dysregulated immune response to the intestinal microbiota[3,5].
A multitude of clinical manifestations represent the expression of IBD. These include diarrhoea, rectal bleeding, abdominal discomfort, fever, anaemia, and weight loss. Both UC and CD tend to run a remitting-relapsing course affected by diverse factors mentioned above. The severity of UC is often presented by a clinical activity index (CAI), which is described by several authors[6-9]. Another, but complementary parameter is endoscopic activity index (EI), which is a true reflection of mucosal damage or otherwise mucosal remission[10] calculated according to Rachmilewitz[6] or the Mayo scoring method[7]. Further, disease activity in CD, which is the other phenotype of IBD is assessed by the well known CD activity index (CDAI)[11]. A CDAI of < 150 reflects remission. The authors of this review (Tanaka T, Ohmori T, Sawada K, Yamamoto T, Hanai H) are gastroenterologists and routinely evaluate patients by both CAI and endoscopy/colonoscopy with greater reliance on endoscopic evaluation[10]. Therefore, in this article, our endeavours were supported by the diagnostic power of colonoscopy to identify patients with an active flare of IBD who were identified as the most likely responders to selective, but therapeutic removal of circulating myeloid linage leucocytes (granulocytes and monocytes/macrophages) by extracorporeal adsorption as a non-pharmacologic treatment intervention. This strategy is known as GMA, which stands for adsorptive granulocyte and monocyte apheresis, described later. In Figure 1 colonoscopic photographs from the colonic mucosa of a healthy human subject and from patients with UC are presented. The mucosa is the surface through, which nutrients and water from the food in the intestine are absorbed into the blood stream. Accordingly, healthy mucosa has a well developed vascular network for adequate absorption of water and nutrients. However, in patients with IBD, the vascular patterns may become invisible or lost due to inflammation or ulcers, seen in Figure 1. As the mucosal layer is involved in the absorption of nutrients and water from the gut, during severely active IBD, absorption of nutrients and water is seriously impaired. Extensive and deep ulcers together with near total loss of the mucosal tissue are not uncommon in patients with severe IBD even in the presence of conventional medications. This condition is debilitating, the patients may suffer from weight loss. For example unabsorbed food and water will pass as watery diarrhoea, or bloody diarrhoea (due to bleeding ulcers). Patients with deep ulcers and extensive loss of the mucosal tissue are not likely to respond to any drug based medication or even to therapeutic depletion of myeloid leucocytes by GMA, they have fulminant UC (disease persists in the presence of optimal medication) and often must opt for resection of the affected gut segment. Needless to say that only an initial diagnostic colonoscopy can identify such patients as non-responders to drug based interventions so that the patient can opt for surgical intervention at an early stage. This should significantly shorten morbidity time and help to avoid futile use of medical resources.
Figure 1.
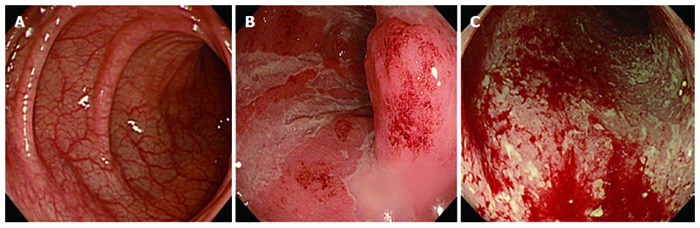
Colonoscopy images. A: Colonoscopy showing normal mucosa with visible vascular patterns in a healthy, non-inflammatory bowel disease (IBD) individual; B: During strong inflammation in a patient with IBD, visible vascular patterns are lost; C: Inflammation can lead to ulcerated mucosa and contact bleeding. Both mucosal inflammation and ulcers lead to inadequate absorption of water and nutrients from the gut. The affected patients may lose weight and become anaemic due to bloody diarrhoea, which if untreated can be very debilitating.
THERAPEUTIC OPTIONS FOR PATIENTS WITH IBD
However, currently available medications aid in the induction and maintenance of remission by targeting various points along the disordered immune pathway implicated in IBD flare ups[12-17]. Despite these seemingly advances, knowledge on the precise cause of IBD is inadequate at present. Accordingly, up to now drug therapy has been empirical rather than based on a sound understanding of disease aetiology. While drug therapy initially appears effective in the majority of patients, it comes at the cost of serious side effects[18-20], which add to the disease complexity. First-line medications for exacerbation of IBD include 5-aminosalicylic acid or sulphasalazine in combination with a corticosteroid together with azathioprine (or 6-mercaptopurine) and nutritional support for some patients[6,16,17]. Treatment failure in patients with severe disease has often been an indication for surgical intervention in many steroid refractory patients[14,21] although in recent years, cyclosporin A (CsA) has been introduced for corticosteroid refractory UC[8,9,15]. Despite being moderately effective in this clinical setting in reducing surgery rate, there remain serious concerns over long-term efficacy and toxicity of CsA[20]. The development of new anti-tumour necrosis factor (TNF)-α antibodies like infliximab and adalimumab represent progress, but there is concern about safety and long term efficacy of biologics. However, this is not to say that drugs have no place in the treatment of IBD. In fact, no one can deny the role of medicines in the elimination of most diseases that our ancestors were left defenseless against. Instead, in this review, our endeavour has been to present clinical evidence and therapeutic outcomes supporting the idea that many patients with IBD can be treated without drugs, but by targeted apheresis.
CYTOKINES AND INFLAMMATORY BOWEL DISEASE
As stated above, the precise cause of IBD is not fully understood at present, and currently available medications do not eradicate the fundamental cause. Therefore, it should be logical to identify known exacerbating factors as therapeutic targets. In line with this thinking, patients with active IBD show elevated cytokine expression, aberrant antigen-antibody complexes, T-cell anomalies, and an increased numbers of granulocytes and monocytes/macrophages (myeloid lineage leucocytes)[22,23], which show activation behaviour[24,25], and prolonged survival[26]. The interaction between neutrophils and macrophages is thought to induce a state of chronic inflammation, which contributes to the perpetuation of IBD. Additionally, the chronic nature of IBD means that afflicted individuals need life-long drug therapy and this can lead to refractoriness[18] and drug-related adverse side effects[19]. However, it is now widely known that IBD is exacerbated and perpetuated by the so-called inflammatory cytokines including TNF-α, interleukin (IL)-1β, IL-23 and others[27-29]. Accordingly, patients with active IBD respond to anti-cytokine antibodies, notably, to anti-TNF-α biologics[30,31] albeit having known serious side effects[32-34]. Nonetheless, the clinical response to anti-TNF biologics has validated the role of this cytokine as an exacerbating factor in dysregulated immune profile. Further cytokines like TNF-α, IL-1β and others are produced by patients’ own cellular elements, notably by the myeloid lineage leucocytes[24,25,35,36]. Hence, elevated circulating myeloid lineage leucocytes appear logical targets of therapy by selective leucocytapheresis we introduced as GMA above. In this article, we have reviewed the latest developments in therapeutic leucocytapheresis to treat IBD with the Adacolumn GMA.
EVOLUTION OF APHERESIS AS A THERAPEUTIC PRACTICE
The word “apheresis” means to take away or to remove, clean from disease causing elements. In the modern time, apheresis means an extracorporeal medical technique for selective removal of components of the blood to achieve a therapeutic effect. Thus apheresis is an extracorporeal therapy. In classical sense, the most basic practice in apheresis involves passing of a patient’s blood through a medical device where removal of components takes place; it is a kind of bloodletting. In the early 20th century, dialysis[37], and centrifugation[38] were introduced for selective depletion of soluble elements[37] or blood cells[38] to achieve therapeutic effects. Even in today’s biologic based therapy targeting a pathologic cytokine, chemokine or an adhesion molecule, apheresis is considered as a non-drug strategy to manage diseases for which there is no effective drug based medication like removing toxic substances from the plasma, which threaten well-being[39,40]. Strategies that selectively remove plasma components or blood cells as therapeutic interventions have generally been safe, and not associated with any major side effect in a significant number of patients[39-41]. Recently, apheresis has been considered as an effective alternative to drug therapy or as an adjunct to conventional medications to enhance drug efficacy with potential to reduce standard medication dosage like the GMA trials in patients with IBD where corticosteroids were avoided or were tapered to a minimum[41-44].
However, today’s selective removal of constituents of circulating blood to achieve a therapeutic effect by apheresis is reminiscent of the rather crude technique of bloodletting (phlebotomy) and its therapeutic application at the time of Hippocrates (460-377 BC) in Ancient Greece. Bloodletting was widely practiced as a major therapeutic intervention in the Ancient civilization of Egypt from where it expanded to Ancient Greece and other parts of the world. The perception then was that disease reflected presence of disease-causing substances in the blood and bloodletting was to expel the pathologic agents. Bloodletting was routinely and extensively practiced for diseases like inflammation, fever, hypertension, and other undiagnosed diseases, its most high profile patient was the first US president, George Washington (reviewed in ref[45]). Bloodletting as a major medical practice was subsequently popularized by Claudius Galen (129-203 AC), a Greek physician who practiced in Rome and became a well respected authority in medicine for over 1500 years. In the late 19th century, bloodletting under a more modern name, phlebotomy was popularly used to treat conditions like haemochromatosis, polycythaemia vera and others. It may just be the folly of the past, but it is difficult to imagine that this procedure would have been so widely practiced for such a long time if it had not been associated with efficacy.
Even in this era of modern medicine and if we consider IBD, and innovations in biologic therapy, it is clinically relevant to bear in mind that drug therapy by its very nature, involves adding a foreign substance or substances to the body system and although initially may be effective, but potentially can lead to the disease becoming drug dependent or drug refractory (body’ reaction to a foreign substance). Hence, a therapeutic strategy based on a non-drug intervention, a correction or support of body’s natural processes like GMA[41-53], if effective has an unrivalled advantage over drug based medication.
TARGET LEUCOCYTES FOR THERAPEUTIC GMA
For an extracorporeal intervention like GMA to be a novel non-drug therapeutic option, it should selectively deplete leucocytes, which in patients with IBD are thought to contribute to the disease pathogenesis. For example, patients with active IBD are found to have compromised lymphocytes[42,47,54] in the presence of elevated and activated granulocytes and monocytes/macrophages[46,48] seen in Figure 2. Additionally, certain sub-populations of lymphocytes like the CD4(+)CD25(+) phenotype, known as the regulatory T-cells (Treg) have essential immunoregulatory function and therefore, are indispensable to the host[55-61]. Based on these understandings, the Adacolumn for GMA is designed to spare lymphocytes, seen in Figure 3, and boost Treg phenotype[48,61]. The column is filled with specially designed cellulose acetate beads of 2mm in diameter as leucocytapheresis carriers[22]. As shown in Figure 3, the carriers remove from blood in the Adacolumn most of the granulocytes, monocytes/macrophages together with a significant fraction of platelets[23,48]. Surprisingly, the procedure has been associated with a sustained increase in absolute lymphocyte counts following a course of GMA[22]. The increase in lymphocyte counts includes the Treg phenotype, CD4(+)CD25(+)[61]. The mechanisms for sparing lymphocytes are briefly described here and illustrated in Figure 4. Patients with IBD may have immune complexes (IC) in their plasma[23,62,63]. Cellulose acetate adsorbs immunoglobulin G (IgG) and IC from the plasma[23,62,63]. Upon adsorption, the binding sites on IgG and IC become available for the fragment crystallizable gamma (Fcγ) receptors (FcγRs) on myeloid lineage leucocytes[23,62,63]. Further, cellulose acetate with adsorbed IgG and IC generates complement activation fragments including C3a and C5a[23,63]. The opsonins C3b/C3bi and others derived from the complement activation fragments also adsorb onto the carriers and serve as the binding sites for the leucocyte complement receptors, CR1, CR2, CR3 (Mac-1, CD11b/CD18). Hence, leucocyte adsorption to the GMA carriers in the Adacolumn is governed by the opsonins, FcγRs and the leucocytes complement receptors[23]. The expressions of these sets of receptors are common features of myeloid lineage leucocytes. Lymphocytes are not known to express complement receptors except on small subsets of B, T and natural killer (NK) cells. Similarly, FcγRs are not widely expressed on lymphocytes except on small populations of CD19+B cells and CD56+NK cells[62]. These basic phenomena proceed well on the carriers and lend GMA selectivity (Figure 4). Further, to our knowledge, there is no published data showing elevated peripheral lymphocytes in patients with active IBD and in one of the best controlled studies on lymphocytapheresis in IBD, Lerebours et al[64] selectively depleted circulating lymphocytes in patients with CD. At the end of an 18-mo follow-up, the clinical outcome in the lymphocytapheresis group was 21% inferior to that of the control group. This well planed controlled clinical trial[64] rules out therapeutic benefit from removing lymphocytes in patients with IBD.
Figure 2.
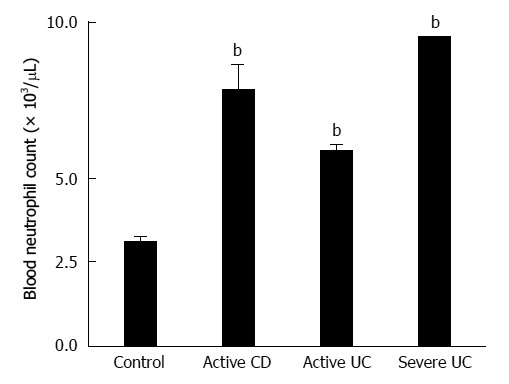
Blood neutrophil (granulocyte) counts in healthy controls and patients with inflammatory bowel disease. This figure shows a very marked elevation of neutrophils during active inflammatory bowel disease (IBD). Additionally, in patients with IBD, neutrophils show activation behaviour and increased survival time in the circulation[26,36] as well as within the mucosal tissue[25]. bP < 0.01 vs control group. UC: Ulcerative colitis; CD: Crohn’s disease.
Figure 3.
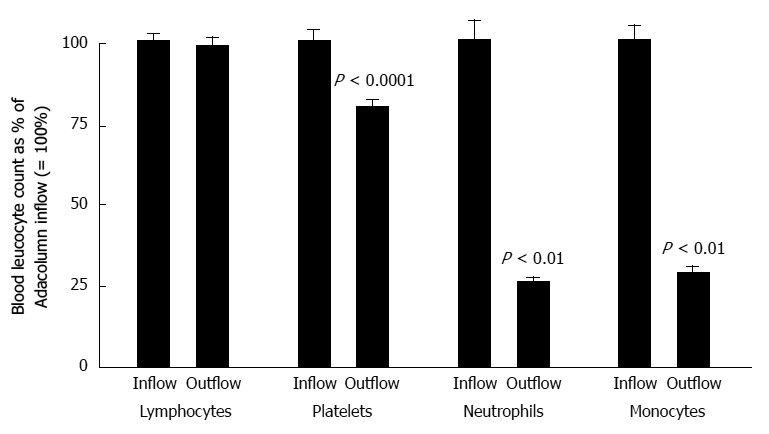
Selective depletion of myeloid lineage cells (neutrophils, monocytes and platelets) by adsorptive granulocyte and monocyte apheresis with the Adacolumn in patients with inflammatory bowel disease. In each case, the column inflow count was expressed as 100% and the column outflow count (return to patient) was expressed as a percentage of the inflow count taken 30 min (peak fall) during a 60-min granulocyte and monocyte apheresis (GMA) session. The data serve as a solid basis for the argument that GMA selectively depletes granulocytes, monocytes/macrophages together with a significant fraction of platelets, but spares lymphocytes[22,23,48,117].
Figure 4.
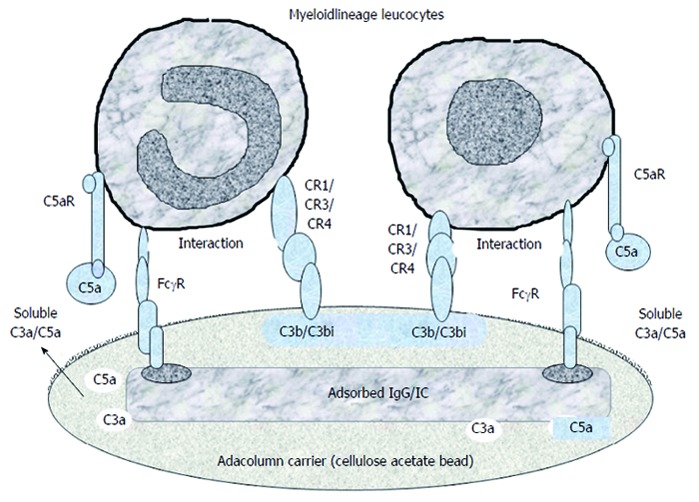
A tentative illustration of the mechanisms, which mediate the selective adhesion of myeloid lineage leucocytes to the granulocyte and monocyte apheresis cellulose acetate carriers. The first event is adhesion of plasma immunoglobulin (IgG) and immune complexes (IC) to the carriers, which serve as the binding sites for the fragment crystallizable gamma receptor (FcγR) on myeloid leucocytes. Then complement activation (helped by IgG and IC) generates C3a, C5a, C3b/C3bi fragments. Of these C3b/C3bi (opsonins) adsorb onto the carriers and serve as the binding sites for the complement receptors (CR) on myeloid leucocytes. Adhesion of leucocytes results in the release of interleukin-1 receptor antagonis, hepatocyte growth factor, soluble tumour necrosis factor receptors, all with therapeutic effects (Figure 13). Modified from Reference[23].
CLINICAL EFFICACY RATES FOR GMA IN UC PATIENTS
Hitherto, a large number of articles mostly from Japan[65-77], and Europe[78-91], but also from the United States[92-96] have described the efficacy of GMA in patients with IBD. The clinical application of GMA with the Adacolumn began following a pioneering multicentre clinical trial by Shimoyama et al[41] described below under steroid sparing effects of GMA. Since then, GMA has been widely applied in Japan and in the European Union (EU) countries to treat patients with IBD. Efficacy rates have been both striking[42-44] as well as disappointing[92,93], reflecting patients’ diverse demographic features prior to GMA. Further, the authors of this review regularly apply GMA to treat patients with IBD for longer than a decade. Based on our experience, the best responders are first episode cases who are often drug naïve and have a short duration of IBD[52], followed by steroid naïve patients[42,50,53,75]. Efficacy rate in first episode cases has been as high as 100%[52] and in steroid naïve cases over an 85%[42,50]. Likewise, recently, Yokoyama et al[74] reported that the most appropriate time to apply GMA therapy in patients with UC was immediately after a clinical relapse. The authors found that the best responders were those with a short duration of active disease[74]. However, patients with deep mucosal lesions and extensive loss of the mucosal tissue at the lesion sites[52,53,82,93] together with those who have a long duration of active UC and exposure to multiple conventional drugs including corticosteroids when the UC has become refractory to medications are not likely to benefit from GMA[49,52,92,93]. These are clinically relevant findings because patients who responded to GMA have a better long-term clinical outcome by avoiding corticosteroids during their first active UC phase[70], while knowing GMA non-responders should help to save medical cost by avoiding futile application of GMA. Figure 5 shows clinical remission rates in typical cohorts of patients with active UC. As shown, the remission rate for patients with the first UC episode has been 100%[52]. All these first episode cases were steroid naïve with a short (< 4 mo) duration of UC. GMA non-responder patients had deep ulcers with near total loss of the mucosal tissue at the lesion sites, a long duration of UC, and exposure to multiple drugs[49,52]; a few were candidates for colectomy[49,52]. Further, sustainability of GMA induced remission has been good[50,53,69,75,87]. Patients who relapse respond well to another course of GMA therapy[87]. Regarding remission rates, Tanaka et al[49] reported an efficacy of 73.8% based on CAI in a cohort of 61 steroid naive patients. Similar efficacy rate has been reported by Hanai et al[50].
Figure 5.
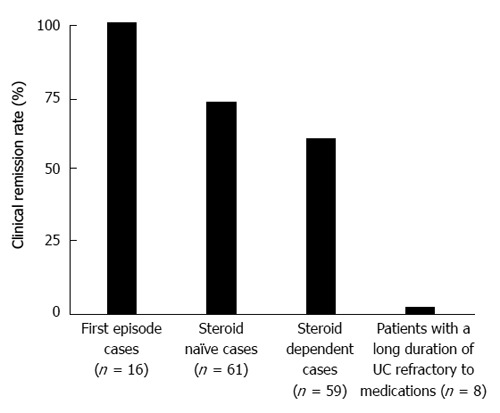
Clinical remission rates in typical cohorts of patients with active ulcerative colitis. The remission rate for patients with the first ulcerative colitis (UC) episode was 100%. All these first episode cases were steroid naïve with a short (< 4 mo) duration of UC; both steroid naïve and short disease duration are granulocyte and monocyte apheresis (GMA)-responder features. Accordingly, the remission rate in corticosteroid naïve cohort looks better than for steroid dependent cohort. GMA non-responder patients had deep ulcers with near total loss of the mucosal tissue at the lesion sites, a long duration of UC, and exposure to multiple drugs; a few were candidates for colectomy[42,49,52].
GMA SPARES CORTICOSTEROID
In the first pivotal study by Shimoyama et al[41] mentioned above, the steroid sparing effect of GMA was unequivocally demonstrated. In a multicentre setting[22,41], 105 patients with active UC while on prednisolone (PSL) were randomly assigned to GMA (n = 53) or to PSL (n = 52). As seen on Figure 6, at entry, in the PSL group, the steroid dose was increased to induce remission, while patients in the GMA group received GMA, at one session per week over five consecutive weeks as remission induction therapy. As seen on the figure, PSL dose was then tapered in line with disease improvement or remission. At the end of the trial, 21 patients (44.2%) in the PSL group and 31 patients (58.5%) in the GMA group were in remission. The results of this study suggested that GMA has significantly better efficacy as compared with the conventional corticosteroid and can spare patients from steroids. Likewise, in a later study by Hanai et al[44], the authors randomly assigned 69 patients with corticosteroid dependent moderately severe UC (at the time of relapse) to GMA (n = 46) or to PSL (n = 23). At entry, the mean dose of PSL was 12 mg per day per patient in both groups. As remission induction therapy, in the GMA group, patients were given up to an 11 treatment sessions over 10 wk, while in the PSL group, the mean dose of PSL was increased to 30 mg per day per patient. At week 12, an 83% of the patients in the GMA group were in clinical remission vs 65% of the patients in the PSL group. Further, during the 12 wk of treatment, the cumulative amount of PSL received per patient was 1157 mg in the GMA and 1938 mg in the PSL group. This study provided further support for GMA as an effective adjunct to standard drug therapy of moderately severe UC with significant corticosteroid sparing effect. They reported steroid related adverse side effects in a significant number of patients, while for GMA, side effects were flushing and transient lightheadedness in a small number of patients.
Figure 6.
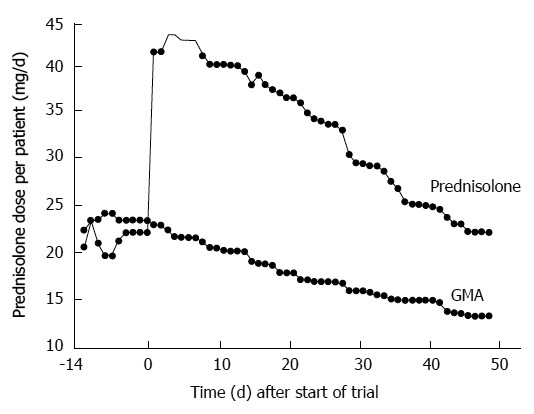
Steroid sparing effect of granulocyte and monocyte apheresis. In this trial, 105 patients with active ulcerative colitis while on the corticosteroid prednisolone (PSL) were randomly assigned to granulocyte and monocyte apheresis (GMA) (n = 53) or to PSL (n = 52). In the PSL group, the steroid dose was increased at entry to induce remission, while patients in the GMA group received GMA, at one session per week over five consecutive weeks. PSL dose was then tapered in line with disease improvement or remission. At the end of the trial, 21 patients (44.2%) in the PSL group and 31 patients (58.5%) in the GMA group were in remission. Therefore, GMA showed significantly better efficacy than PSL and spared patients from steroids[22,41,44].
GMA FOR CHILDREN OR ADOLESCENTS WITH UC
In children and adolescents with IBD, conventional drugs like salicylates, thiopurines, corticosteroids or the new anti-TNF-α biologics may adversely affect the patients’ growth and development. Therefore, GMA as a non-drug therapeutic intervention, if effective in this clinical setting is unrivalled by any currently known drug based medication. With this in mind, Tomomasa et al[76] were the first to apply GMA to children who had active UC. In that study, 12 children, age 5 to 15 years, all with active UC refractory to corticosteroids were given one GMA session per week for 5-10 consecutive weeks. In 8 patients, clinical symptoms improved after two GMA sessions. Normal body temperature, stool frequency, and disappearance of blood in stool were seen after 24.3 ± 11.5 d. The endoscopic index improved from 2.6 ± 0.3 to 0.4 ± 0.2. One patient who initially responded developed bloody diarrhoea later and 2 cases remained unchanged. The dose of steroid was tapered during GMA therapy by 50%. No serious adverse effect was observed. This study showed that GMA was effective and well tolerated in children with active UC refractory to corticosteroids.
Very recently, Tanaka et al[75] reported good efficacy and safety outcomes for GMA in children and adolescents with active IBD, all corticosteroid naïve, which is a GMA responder feature. In a single centre setting, a total of 24 consecutive children and adolescents, age 11-19 years were given mesalazine or sulphasalazine as a first-line medication. Seventeen patients relapsed or did not respond to the first-line medications, and received GMA at 2 sessions in the first week, and then weekly, up to an 11 sessions. Patients who achieved a decrease of at least 5 points in the CAI score were to continue with GMA, while non-responders were to receive 0.5 to 1.0 mg/kg per day PSL plus additional GMA sessions similar to GMA responder cases. At entry and week 12, patients were clinically and endoscopically evaluated, allowing each patient to serve as her or his own control. In this study, 7 patients achieved remission with the first-line medications and did not receive GMA. Five patients did not respond to the first 5 GMA sessions and received PSL plus GMA, while 12 patients responded to the first 5 GMA sessions and received additional sessions. At entry, the average CAI was 14.1 ± 0.4, range 11-17, and the average endoscopic index was 9.2 ± 0.3, range 7-11. The corresponding values at week 12 were 2.1 ± 0.2, range 1-4 and 2.4 ± 0.2, range 1-4. PSL was tapered to 0 mg within 3 mo in the 5 cases who did receive PSL in combination with GMA. This study is the closest one can expect to clinical practice rather than to clinical trial. With the strategy they applied, all 24 consecutive patients achieved clinical remission, most with endoscopic remission as well[75]. The authors’ conclusion states that in growing patients with active UC refractory to first-line medications, GMA induced clinical remission and mucosal healing, while in non-responders to GMA monotherapy, addition of a low dose PSL enhanced the efficacy of GMA and tapering of the PSL dose soon after remission was not associated with UC relapse. Avoiding corticosteroid at an early stage of UC should ensure better long-term clinical course[70,75].
GMA IN PATIENTS WITH CD
So far, this review has focused mainly on the efficacy of GMA in patients with active UC. This is because IBD in the colon or in the rectum is strongly affected by neutrophils[50,54], while the role of myeloid lineage leucocytes in the small intestinal IBD lesions has not been defined yet. Nonetheless the majority of CD patients have colonic lesions, and therefore, GMA seems to produce significant efficacy in most patients with active CD[85,97,98]. Additionally, as described for UC, patients with severe CD refractory to currently available pharmacologicals may not respond well to GMA[93]. Perhaps most IBD physicians in the West are not fully aware that unlike Europe where there is no striking difference in the prevalence of UC and CD, in Japan, the prevalence of UC is more than 3 times higher than that of CD. Accordingly, the first Adacolumn multicenter study in Japan that led to reimbursement approval was in patients with active UC[22,41]. This is why most GMA papers from Japan are on studies in patients with UC. However, subsequently, a clinical trial in patients with CD refractory to conventional medications was undertaken[98], and led to reimbursement approval for patients with CD in Japan. However, the first study in CD was reported by Matsui et al[97], on 7 patients who were refractory to standard medications, each patient received 5 GMA sessions over 5 consecutive weeks. Five of 7 patients achieved remission. It is clinically relevant to mention here that the only 2 GMA non-responders in Matsui’s study had primarily small intestinal lesions. Subsequently, Fukuda et al[98] reported an efficacy rate of 52% by applying 5 GMA sessions to each of 21 patients with severe CD. However, it is imperative to elaborate that the patients Fukuda et al[98] included had received conventional medications including 2 wk of optimum nutritional therapy (a routine treatment for CD in Japan) and only patients who remained with a high CDAI score received GMA. Therefore, 52% remission rate in a cohort of patients with severe and medication refractory CD was very encouraging. Further, Domènech et al[85], treated 12 steroid dependent patients with CD. The remission rate was 70%. Finally, Muratov et al[79] treated 7 patients with CD who had relapsed while on optimum conventional medication and a few on biologics. The median CDAI decreased from 290 at weeks 1 to 184 at week 7 and to 128.5 (remission level) at 12 mo. It is clear from the aforementioned reports that up to now, only very complicated and severe cases of CD have received GMA therapy.
EFFECTIVE DOSAGE OF GMA
The evolution of modern medicine has relied on the outcomes of clinical trials to determine the dosage of drugs with maximum efficacy margin and minimum adverse side effect. Fortunately for GMA, which is a non-drug treatment strategy, reliance on clinical trial outcomes has been less demanding or at least lack of it has not caused serious concern partly because of its good safety profile, and partly for the fact that GMA removes from the body instead of adding to it. Accordingly, unlike drugs, loss of efficacy, dependence and refractoriness are not likely. Nonetheless, it is a basic requirement to know the most effective frequency and the number of GMA sessions for patients with mild, moderate or severe IBD as this can help to save time and cost. The reality is that up to now GMA treatment has been an empirical practice. Some institutes administer 2 GMA sessions per week in the first 2-3 wk and then 1 session per week up to 10 or 11 sessions[50,52]. Hanai et al[50] reported that although patients with steroid naïve UC responded well to 5 GMA sessions, steroid refractory patients with severe UC responded better to 10 sessions. In contrast, Suzuki et al[42,52] administer 2 GMA sessions per week and cease when CAI decreases to 4 or less (clinical remission level); patients who do not improve after several sessions are classified as non-responders[52]. These treatment regimens are all contrary to the initial clinical trials in which 5 GMA sessions over five consecutive weeks were applied[22,41]. Regarding duration of one GMA session, Kanke et al[66] found that 90 min was significantly better than the routinely applied 60 min per GMA session. Likewise, Yoshimura et al[73] increased the processed blood volume from the conventional 1800 mL per GMA session to over 3000 mL per session. In this study, the efficacy rate in the higher processed blood volume group was significantly greater than in the 1800 mL per session group[73]. In a prospective multicentre study, Sakuraba et al[99] found that intensive GMA at 2 sessions per week induced remission in shorter time and at a significantly higher rate when compared to weekly GMA. The authors assigned 112 patients with moderately active UC to 2 groups. Group 1 patients received one GMA session per week, while group 2 patients received 2 sessions per week, up to 10 sessions in both groups. The remission rate in group 1 was 46.7%, while in group 2 was 73.1%. Further, the mean time to remission was 28.1 d, in group 1 and 16.3 d in group 2. In spite of these outcomes, there is evidence to suggest that the efficacy of GMA is time dependent. Recently, Yamamoto et al[100] administered one GMA session per day over 5 consecutive days. There was no safety concern, but the efficacy rate was very much less than in the 5 GMA sessions reported by Shimoyama et al[41]. As reviewed above, in patients with active IBD, large numbers of myeloid lineage leucocytes in the colonic mucosa are seen in biopsies[49,53] or by measuring a specific neutrophil protein[101]. The infiltrated neutrophils may take several weeks to clear in spite of CAI showing clinical remission[102]. Additionally, the immunomodulatory actions of GMA are time dependent. In line with this assertion, in rheumatoid arthritis patients, there was a sustained increase in CD4+ T-lymphocytes up to 12 wk following the last GMA session[22]. Similarly, there was a striking down-modulation of the inflammatory chemokine receptor CXCR3 on leucocytes several weeks after the last GMA session[23]. Clearly further investigations are warranted for establishing the optimum frequency and duration of GMA session.
TREATMENT COST
In a comprehensive study, Panés et al[78] estimated the treatment cost for patients with UC in the EU countries for conventional medications and GMA. The average annual cost per patient treated with conventional medications was estimated to be 6740€, while the cost for GMA was 6959€, which is very close to the conventional medications. In contrast, for steroid-dependent patients, the average annual cost was 6059€ for conventional medications and 11436€ for GMA. Further, this study found that the efficacy rate in patients who achieved clinical remission with GMA was 22.5% higher than for conventional therapy. The authors concluded that incorporating GMA in the therapeutic management of patients with moderate-to-severe UC, GMA is cost-effective and the extra cost is compromised by GMA’s safety profile when compared with drug therapy.
GMA REDUCES MUCOSAL CONCENTRATION OF MYELOID LINEAGE LEUCOCYTES
As reviewed above, one pathologic feature of active IBD is presence of a large number of granulocytes and monocytes/macrophages in the colonic mucosa[49,53]. In clinical settings, GMA is applied as an extracorporeal procedure to reduce the excess and activated myeloid lineage leucocytes from patients’ systemic circulation. One could logically argue that removal of the leucocytes from the circulating blood should lead to depletion of these cells in the colonic mucosa where they are believed to exacerbate and perpetuate IBD[25,27,36]. Figure 7 shows typical immunohistochemical images taken from colonic biopsy specimens in a patient with total colitis in active stage and following GMA induced remission. The figure shows that the colonic mucosal tissue is densely infiltrated by myeloid lineage leucocytes with the formation of crypt abscess and GMA has reduced the concentration of these leucocytes in the mucosa. It is relevant to mention here that the images seen in Figure 7 are typical for IBD lesions in the large intestine because similar images are uncommon in biopsies from small intestinal IBD lesions found in most patients with CD. It might be equally true to say that CD patients with the active IBD lesions confined to the small intestine may not be the right candidates for GMA therapy[97].
Figure 7.
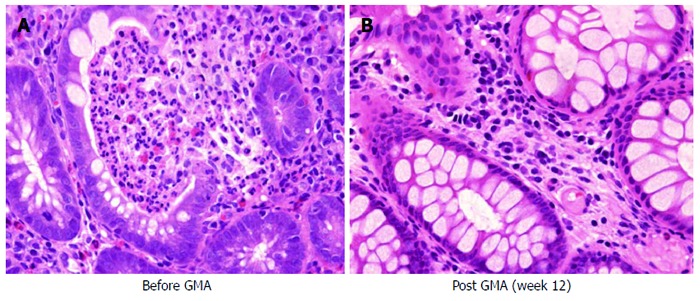
Typical immunohistochemical images taken from colonic biopsy specimens in a patient with total colitis in active stage (A) and following remission (B). This figure shows that the mucosal tissue is densely infiltrated by myeloid lineage leucocytes and granulocyte and monocyte apheresis has reduced the concentration of these leucocytes in the mucosa. The specimens seen in this figure are from a 60-year-old male with moderately severe ulcerative colitis and corticosteroid naive, baseline clinical activity index, 13.
COLONOSCOPIC FEATURES OF GMA RESPONDER AND NON-RESPONDER PATIENTS
As reviewed above, several studies have reported that any patient with a fair level of intact colonic mucosa is a potential responder to GMA. With this in mind, in the authors’ hospitals, all patients receive endoscopic evaluations and the evaluation is used to treat or not to treat a patient by GMA. However, as stated above, by applying GMA at an early stage[70], most first episode cases respond[52], and we do not have many drug refractory patients with badly damaged mucosal tissue. Even patients with a near equal CAI score may have very different mucosal damage status, indicating that CAI per se does not reflect the full extent of mucosal damage in patients with IBD[49]. Figure 8 shows typical colonoscopy features of patients who may respond well to GMA and be spared from drug based medications. These two cases were from a subgroup of patients who were identified as responders by colonoscopy. These cases were steroid naïve with severe UC based on clinical evaluation (CAI > 14) without endoscopy, nonetheless good responders to GMA because, firstly, the mucosal tissue was preserved and secondly, the patients were not exposed to multiple drugs prior to GMA. The photographs show complete restoration of the mucosal vascular patterns post GMA. Almost all such cases readily respond to GMA. Without colonoscopy, clinical evaluation would have identified these patients as having severe UC, a potential candidate for steroid therapy. However, such responders to GMA without corticosteroids should have good long-term clinical course[70].
Figure 8.
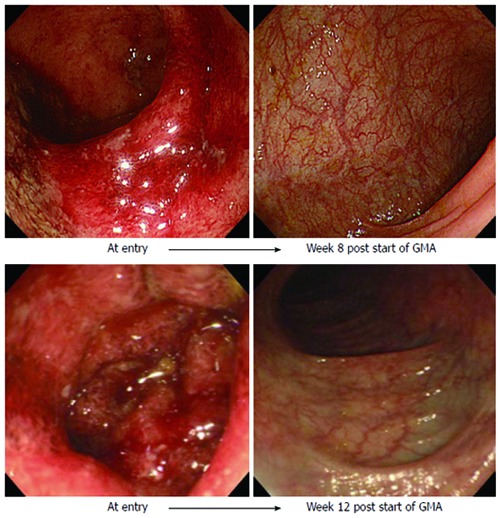
Typical endoscopic features of patients who may respond well to granulocyte and monocyte apheresis and be spared from drug based medications. These cases were from a subgroup of patients who have been identified as good responders by colonoscopy. These patients were steroid naïve with severe ulcerative colitis (clinical activity indices > 14), yet good responders to granulocyte and monocyte apheresis (GMA), firstly because the mucosal tissue was preserved and secondly, the patients were corticosteroid naïve at the time of relapse. The photographs show complete restoration of the mucosal vascular patterns at post GMA.
In contrast, Figure 9 shows colonoscopic features of GMA non-responder patients. Here, colonoscopy photographs from two typical GMA non-responder patients at entry and at week 12 are presented. The colonoscopy images at entry revealed deep and extensive colonic lesions with virtually no mucosal tissue left at the lesion sites. However, no patient with the entry mucosal damage seen in this figure is likely to show any significant fall in CAI, a few may have fulminant UC, candidates for surgery.
Figure 9.
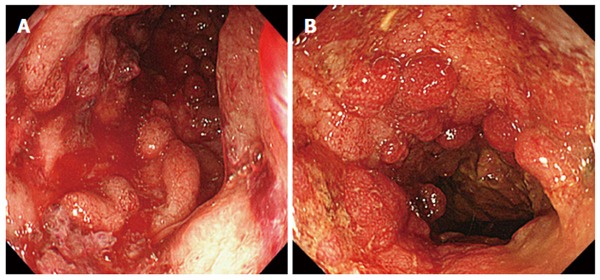
Colonoscopy images showing deep and extensive colonic lesions together with inflammatory polyps and contact bleeding. Typical colonoscopic images from patients with severely damaged mucosal tissue (A), granulocyte/monocyte apheresis non-responders (B). However, most patients with the entry mucosal damage seen in this figure are medication refractory and unlikely to respond to granulocyte and monocyte apheresis, some opt for colectomy.
TREATMENT OF PYODERMA GANGRENOSUM ASSOCIATED WITH IBD
Pyoderma gangrenosum (PG)-like skin lesions are seen in up to 2% of patients with IBD and can be a major cause of pathological and psychological morbidity[103]. It is interesting that PG and psoriatic skin lesions are reported to be good responders to GMA[103-107]. To our knowledge, most treated cases have responded well and yet, it all happened by chance[103]. A patient with IBD associated PG was treated for IBD, but the response of pyoderma lesions was more striking than anything expected from GMA. The young patient had very stressful deep refractory lesions over a long period of time (Figure 10). The lesions fully remitted after 10 GMA sessions[103]. Subsequently, other authors independently reported cases of pyoderma or psoriatic skin lesions responding well to GMA[104-107]. The mechanism associated with the efficacy of GMA in these conditions is not very clear, but the chemokine receptor, CXCR3 is known to have an active role in the initiation and perpetuation of inflammatory skin lesions and is strongly down-modulated by GMA[23]. This action of GMA, if duplicated by follow-up studies can serve as a major break-through in our efforts to understand the mechanisms of clinical efficacy of GMA in these clinical settings.
Figure 10.
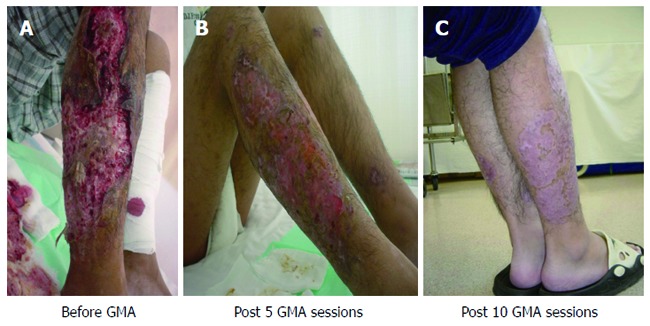
Pyoderma gangrenosum lesions. Pyoderma gangrenosum lesions associated with Crohn’s disease (A), partially re-epithelialized after 5 granulocyte and monocyte apheresis (GMA), sessions (B), fully re-epithelialized after 10 GMA sessions (C)[103].
SPECIFIC IMMUNOLOGICAL EFFECTS
The CD14+CD16+ monocyte phenotype is known to be pro-inflammatory as a major source of TNF[108] and shows dramatic expansion in inflammatory conditions. Accordingly, Hanai et al[109] reported elevated CD14+CD16+ monocytes in patients with IBD and a very marked depletion of these TNF-producing monocytes by GMA. This monocyte sub-set was depleted to levels seen in healthy persons[109]. In Figure 11, typical effect of GMA is shown by flow cytometry. This action of GMA should significantly alleviate inflammation in patients with dysregulated immune profile. Additionally, as reviewed above, GMA has been associated with a sustained increase in circulating lymphocytes[20] including the CD4(+)CD25(+) Treg phenotype[61]. In spite of this, the clinical efficacy associated with a course of GMA is unlikely to reflect its effects on peripheral leucocytes per se. It is inferred that additional mechanisms of actions might follow a course of GMA. As seen in Figure 4, leucocytes that bear the FcγR and complement receptors adhere to the GMA carriers[23,62]. The adsorbed leucocytes release an array of substances both toxic and non-toxic, but anti-inflammatory as well, which reach the patients’ circulation via the column outflow that returns to patients. Among these, cytokines, C3a and C5a are of short half-life and may not reach the patients’ circulation in fully active form. Hanai et al[110] reported a significant increase in the column outflow blood levels of soluble TNF receptors I and II known to neutralize TNF without invoking TNF-like actions[111].
Figure 11.
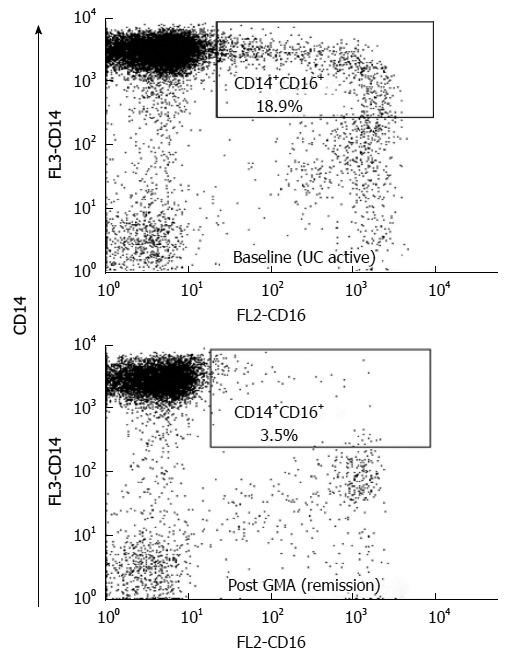
Typical flow cytometry outputs. Flow cytometry showing immunophenotyping of elevated pro-inflammatory CD14(+)CD16(+)DR(++) monocytes in a patient with inflammatory bowel disease and depletion of these tumour necrosis factor-producing leucocytes by granulocyte and monocyte apheresis (GMA). In this patient, an 18.9% of monocytes were identified as CD14+CD16+ phenotype in active ulcerative colitis (UC) stage and this was reduced to just 3.5% when the patient achieved remission following a course of GMA therapy. Normal level is < 8%[109].
Further, GMA-related suppression of inflammatory cytokines (TNF-α, IL-1β, IL-6 and IL-8) released by peripheral leucocytes has been reported[112]. In in-vitro settings, exposure of human blood to the GMA carriers caused the release of significant amounts of IL-1 receptor antagonist (IL-1ra) and hepatocyte growth factor (HGF)[113], seen in Figure 12. The release of these substances (albeit very small) should proceed inside the Adacolumn during GMA in clinical settings and reach the patients’ circulation via the column outflow line. IL-1ra is known to control intestinal inflammation[114], while HGF is believed to promote epithelial cell regeneration, an essential step in ulcer healing[115]. Further, examinations of mucosal biopsy specimens suggested that GMA suppresses cytokine profiles within the mucosa[79,116]. A wary reader may wonder why this is possible with a system that impacts peripheral blood leucocyte counts. One answer could be that GMA reduces the number of leucocytes that are destined for the mucosa, partially by depleting them (Figure 3) and partially by down-modulating the adhesion receptors on the remaining leucocytes[117]. Muratov et al[79] found a marked decrease in tissue interferon (IFN)-γ or TNF-α positive leucocytes in clinical responders after GMA. In parallel, significantly lower levels of IFN-γ producing leucocytes were detected in peripheral blood. IFN-γ positive T-cells in pretreatment biopsies completely disappeared or decreased in post-treatment biopsies sampled 2 wk after the last GMA session in responders and appeared to predict the maintenance of long-term remission, up to 12 mo. However, our view is that the impact of GMA on the CD4(+)CD25(+) Treg[61] reviewed above is potentially very interesting in patients with dysregulated immune behaviour in whom, the immune system is in a state of exuberant activity. In Figure 13, the immunological actions of GMA in patients with IBD are summarized based on published findings. In addition to adsorption of elevated and activated myeloid lineage leucocytes to the GMA carriers, the column outflow blood is a potential source of anti-inflammatory substances.
Figure 12.
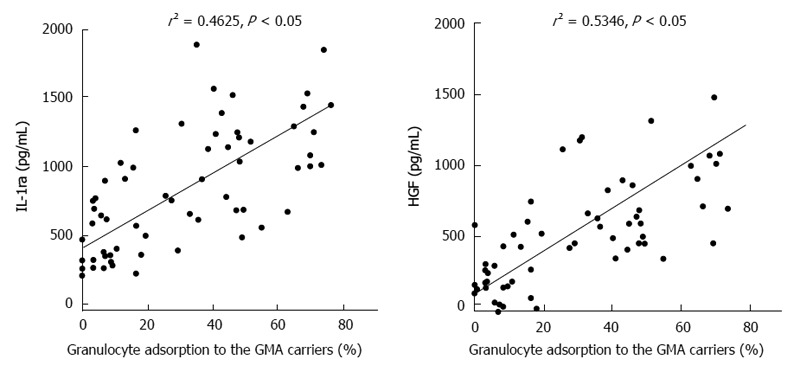
Adsorption dependent release of interleukin-1 receptor antagonist, and hepatocyte growth factor from myeloid lineage leucocytes (granulocytes and monocytes) in in-vitro setting. Hepatocyte growth factor (HGF) is known to promote ulcer healing and cell regeneration, while interleukin-1 receptor antagonist (IL-1ra) is strongly anti-inflammatory[113]. GMA: Granulocyte and monocyte apheresis.
Figure 13.
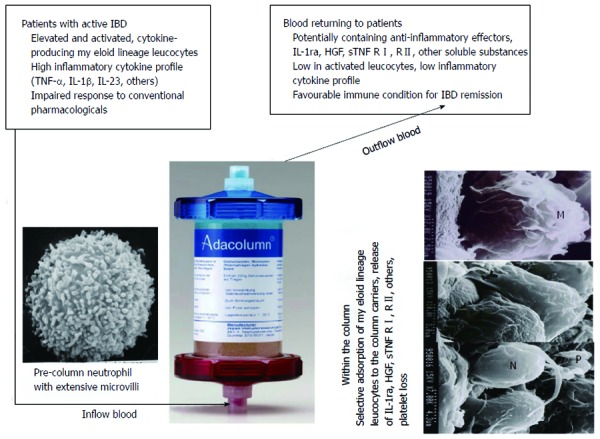
An idealistic view of the events attributed to therapeutic granulocyte and monocyte apheresis with the Adacolumn in patients with inflammatory bowel disease. Scanning photomicrographs of leucocytes adsorbed onto a granulocyte and monocyte apheresis (GMA) carrier and the basic events, which follow on the surface of the carriers during GMA in clinical setting (see Figure 4 as well). Normal, non-activated and non-adherent neutrophils and monocytes/macrophages express extensive surface microvilli. The villi bear various receptors like tumour necrosis factor (TNF) receptors, and L selectin, which are shed upon adsorption of the cells to the carriers. Further as seen, adsorbed leucocytes undergo extensive release reaction. Up to now, interleukin-1 receptor antagonist (IL-1ra), hepatocyte growth factor (HGF), IL-10 and soluble TNF receptors have been measured. During GMA, the blood, which returns to patients via the column outflow line may be likened to a biologic cocktail containing a large number of soluble substances released by the adherent leucocytes. The adsorptive nature of GMA is thought to be the most intriguing feature of this non-pharmacological treatment intervention. M: Monocyte; N: Neutrophil; P: Platelet; IBD: Inflammatory bowel disease.
PUTTING EVERYTHING TOGETHER
IBD is a debilitating chronic, life-long health disorder, affecting millions of individuals with symptoms, which impair function and quality of life. The aetiology of IBD is not precisely understood at present, and therefore, hitherto drug therapy has been empirical rather than based on a sound understanding of disease mechanism(s). This empirical approach to medication might be a major factor for refractoriness and adverse drug effects. Indeed, adverse drug side effects become additional morbidity factors in many patients on long-term medications. Although, the fundamental cause(s) of IBD is not well known, but the exacerbating factors like TNF-α and other inflammatory cytokines are known and have been targeted. Bearing in mind that inflammatory cytokines are generated by the patients’ own cellular elements including myeloid lineage leucocytes, it seems logical to apply GMA and deplete the elevated and activated myeloid lineage leucocytes. When the elevated cytokine producing leucocytes are depleted, the patients’ immune system should be able to adjust itself to a more normal function or at least drug efficacy could be better. As GMA removes from the body instead of adding, it has not been associated with dependency, refractoriness, and safety concern. However, lets’ not forget that efficacy outcomes with GMA in patients with IBD have been impressive as well as disappointing. A review of the clinical experience indicates that GMA responders and non-responders define patients’ past disease course, severity and response to medications. This is to say that IBD patients present with diverse clinical and endoscopic disease severity levels, long or short duration of IBD, and a history of exposure to medication (or otherwise). Hence, their clinical response to medical interventions or to GMA can be complete remission, partial response or no response at all. Regarding GMA, it has been found that first episode cases together with steroid naïve and patients with a short duration of active IBD, but without extensive loss of the mucosal tissue respond well and are spared from additional pharmacologic interventions. Additionally, GMA responder patients have good long-term disease course. Therefore, if this strategy is adhered to at an early stage during the development of IBD, there should be fewer drug-refractory or cases with badly damaged mucosal tissue that are medication or GMA non-responders. GMA is not a rescue therapy in patients in whom drug therapy has failed, while disease severity is worsening, but rather to minimize the number of patients who need such intervention. Centuries ago, bloodletting was a major medical practice to cure disease because of lack of today’s medicines, while today, GMA therapy reflects advance in our knowledge of immune behaviour in IBD and a desire to treat without drugs.
Footnotes
P- Reviewer: Guslandi M, Ingle SB, Yamamoto S S- Editor: Gou SX L- Editor: A E- Editor: Wang CH
References
- 1.Selby W. The natural history of ulcerative colitis. Baillieres Clin Gastroenterol. 1997;11:53–64. doi: 10.1016/s0950-3528(97)90053-1. [DOI] [PubMed] [Google Scholar]
- 2.Loftus CG, Loftus EV Jr, Harmsen WS, Zinsmeister AR, Tremaine WJ, Melton LJ, Sandborn WJ. Update on the incidence and prevalence of Crohn’s disease and ulcerative colitis in Olmsted County, Minnesota, 1940-2000. Inflamm Bowel Dis. 2007;13:254–261. doi: 10.1002/ibd.20029. [DOI] [PubMed] [Google Scholar]
- 3.Neish AS. Microbes in gastrointestinal health and disease. Gastroenterology. 2009;136:65–80. doi: 10.1053/j.gastro.2008.10.080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Uronis JM, Arthur JC, Keku T, Fodor A, Carroll IM, Cruz ML, Appleyard CB, Jobin C. Gut microbial diversity is reduced by the probiotic VSL#3 and correlates with decreased TNBS-induced colitis. Inflamm Bowel Dis. 2011;17:289–297. doi: 10.1002/ibd.21366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xavier RJ, Podolsky DK. Unravelling the pathogenesis of inflammatory bowel disease. Nature. 2007;448:427–434. doi: 10.1038/nature06005. [DOI] [PubMed] [Google Scholar]
- 6.Rachmilewitz D. Coated mesalazine (5-aminosalicylic acid) versus sulphasalazine in the treatment of active ulcerative colitis: a randomised trial. BMJ. 1989;298:82–86. doi: 10.1136/bmj.298.6666.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis. A randomized study. N Engl J Med. 1987;317:1625–1629. doi: 10.1056/NEJM198712243172603. [DOI] [PubMed] [Google Scholar]
- 8.Lichtiger S, Present DH, Kornbluth A, Gelernt I, Bauer J, Galler G, Michelassi F, Hanauer S. Cyclosporine in severe ulcerative colitis refractory to steroid therapy. N Engl J Med. 1994;330:1841–1845. doi: 10.1056/NEJM199406303302601. [DOI] [PubMed] [Google Scholar]
- 9.Sandborn WJ, Tremaine WJ, Schroeder KW, Steiner BL, Batts KP, Lawson GM. Cyclosporine enemas for treatment-resistant, mildly to moderately active, left-sided ulcerative colitis. Am J Gastroenterol. 1993;88:640–645. [PubMed] [Google Scholar]
- 10.Travis SP, Higgins PD, Orchard T, Van Der Woude CJ, Panaccione R, Bitton A, O’Morain C, Panés J, Sturm A, Reinisch W, et al. Review article: defining remission in ulcerative colitis. Aliment Pharmacol Ther. 2011;34:113–124. doi: 10.1111/j.1365-2036.2011.04701.x. [DOI] [PubMed] [Google Scholar]
- 11.Best WR, Becktel JM, Singleton JW, Kern F. Development of a Crohn’s disease activity index. National Cooperative Crohn’s Disease Study. Gastroenterology. 1976;70:439–444. [PubMed] [Google Scholar]
- 12.Truelove SC, Jewell DP. Intensive intravenous regimen for severe attacks of ulcerative colitis. Lancet. 1974;1:1067–1070. doi: 10.1016/s0140-6736(74)90552-2. [DOI] [PubMed] [Google Scholar]
- 13.Hanauer SB. Medical therapy for ulcerative colitis 2004. Gastroenterology. 2004;126:1582–1592. doi: 10.1053/j.gastro.2004.02.071. [DOI] [PubMed] [Google Scholar]
- 14.Hyde GM, Thillainayagam AV, Jewell DP. Intravenous cyclosporin as rescue therapy in severe ulcerative colitis: time for a reappraisal? Eur J Gastroenterol Hepatol. 1998;10:411–413. doi: 10.1097/00042737-199805000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Hanauer SB. Can cyclosporine go it alone in severe ulcerative colitis? Curr Gastroenterol Rep. 2001;3:455–456. [PubMed] [Google Scholar]
- 16.O’Keefe SJ. Nutrition and gastrointestinal disease. Scand J Gastroenterol Suppl. 1996;220:52–59. doi: 10.3109/00365529609094750. [DOI] [PubMed] [Google Scholar]
- 17.Kozuch PL, Hanauer SB. Treatment of inflammatory bowel disease: a review of medical therapy. World J Gastroenterol. 2008;14:354–377. doi: 10.3748/wjg.14.354. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Taffet SL, Das KM. Sulfasalazine. Adverse effects and desensitization. Dig Dis Sci. 1983;28:833–842. doi: 10.1007/BF01296907. [DOI] [PubMed] [Google Scholar]
- 19.Present DH. How to do without steroids in inflammatory bowel disease. Inflamm Bowel Dis. 2000;6:48–57; discussion 58. doi: 10.1097/00054725-200002000-00009. [DOI] [PubMed] [Google Scholar]
- 20.Serkova NJ, Christians U, Benet LZ. Biochemical mechanisms of cyclosporine neurotoxicity. Mol Interv. 2004;4:97–107. doi: 10.1124/mi.4.2.7. [DOI] [PubMed] [Google Scholar]
- 21.Kornbluth A, Marion JF, Salomon P, Janowitz HD. How effective is current medical therapy for severe ulcerative and Crohn’s colitis? An analytic review of selected trials. J Clin Gastroenterol. 1995;20:280–284. doi: 10.1097/00004836-199506000-00004. [DOI] [PubMed] [Google Scholar]
- 22.Saniabadi AR, Hanai H, Takeuchi K, Umemura K, Nakashima M, Adachi T, Shima C, Bjarnason I, Lofberg R. Adacolumn, an adsorptive carrier based granulocyte and monocyte apheresis device for the treatment of inflammatory and refractory diseases associated with leukocytes. Ther Apher Dial. 2003;7:48–59. doi: 10.1046/j.1526-0968.2003.00012.x. [DOI] [PubMed] [Google Scholar]
- 23.Saniabadi AR, Hanai H, Suzuki Y, Ohmori T, Sawada K, Yoshimura N, Saito Y, Takeda Y, Umemura K, Kondo K, et al. Adacolumn for selective leukocytapheresis as a non-pharmacological treatment for patients with disorders of the immune system: an adjunct or an alternative to drug therapy? J Clin Apher. 2005;20:171–184. doi: 10.1002/jca.20046. [DOI] [PubMed] [Google Scholar]
- 24.Lefkowitz DL, Mills K, Lefkowitz SS, Bollen A, Moguilevsky N. Neutrophil-macrophage interaction: a paradigm for chronic inflammation. Med Hypotheses. 1995;44:58–62. doi: 10.1016/0306-9877(95)90303-8. [DOI] [PubMed] [Google Scholar]
- 25.McCarthy DA, Rampton DS, Liu YC. Peripheral blood neutrophils in inflammatory bowel disease: morphological evidence of in vivo activation in active disease. Clin Exp Immunol. 1991;86:489–493. doi: 10.1111/j.1365-2249.1991.tb02958.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Brannigan AE, O’Connell PR, Hurley H, O’Neill A, Brady HR, Fitzpatrick JM, Watson RW. Neutrophil apoptosis is delayed in patients with inflammatory bowel disease. Shock. 2000;13:361–366. doi: 10.1097/00024382-200005000-00003. [DOI] [PubMed] [Google Scholar]
- 27.Schreiber S, Nikolaus S, Hampe J, Hämling J, Koop I, Groessner B, Lochs H, Raedler A. Tumour necrosis factor alpha and interleukin 1beta in relapse of Crohn’s disease. Lancet. 1999;353:459–461. doi: 10.1016/S0140-6736(98)03339-X. [DOI] [PubMed] [Google Scholar]
- 28.Papadakis KA, Targan SR. Role of cytokines in the pathogenesis of inflammatory bowel disease. Annu Rev Med. 2000;51:289–298. doi: 10.1146/annurev.med.51.1.289. [DOI] [PubMed] [Google Scholar]
- 29.Neurath MF. IL-23: a master regulator in Crohn disease. Nat Med. 2007;13:26–28. doi: 10.1038/nm0107-26. [DOI] [PubMed] [Google Scholar]
- 30.van Dullemen HM, van Deventer SJ, Hommes DW, Bijl HA, Jansen J, Tytgat GN, Woody J. Treatment of Crohn’s disease with anti-tumor necrosis factor chimeric monoclonal antibody (cA2) Gastroenterology. 1995;109:129–135. doi: 10.1016/0016-5085(95)90277-5. [DOI] [PubMed] [Google Scholar]
- 31.Rutgeerts P, Sandborn WJ, Feagan BG, Reinisch W, Olson A, Johanns J, Travers S, Rachmilewitz D, Hanauer SB, Lichtenstein GR, et al. Infliximab for induction and maintenance therapy for ulcerative colitis. N Engl J Med. 2005;353:2462–2476. doi: 10.1056/NEJMoa050516. [DOI] [PubMed] [Google Scholar]
- 32.Brown SL, Greene MH, Gershon SK, Edwards ET, Braun MM. Tumor necrosis factor antagonist therapy and lymphoma development: twenty-six cases reported to the Food and Drug Administration. Arthritis Rheum. 2002;46:3151–3158. doi: 10.1002/art.10679. [DOI] [PubMed] [Google Scholar]
- 33.Moustou AE, Matekovits A, Dessinioti C, Antoniou C, Sfikakis PP, Stratigos AJ. Cutaneous side effects of anti-tumor necrosis factor biologic therapy: a clinical review. J Am Acad Dermatol. 2009;61:486–504. doi: 10.1016/j.jaad.2008.10.060. [DOI] [PubMed] [Google Scholar]
- 34.Aaltonen KJ, Virkki LM, Malmivaara A, Konttinen YT, Nordström DC, Blom M. Systematic review and meta-analysis of the efficacy and safety of existing TNF blocking agents in treatment of rheumatoid arthritis. PLoS One. 2012;7:e30275. doi: 10.1371/journal.pone.0030275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Cassatella MA. The production of cytokines by polymorphonuclear neutrophils. Immunol Today. 1995;16:21–26. doi: 10.1016/0167-5699(95)80066-2. [DOI] [PubMed] [Google Scholar]
- 36.Nikolaus S, Bauditz J, Gionchetti P, Witt C, Lochs H, Schreiber S. Increased secretion of pro-inflammatory cytokines by circulating polymorphonuclear neutrophils and regulation by interleukin 10 during intestinal inflammation. Gut. 1998;42:470–476. doi: 10.1136/gut.42.4.470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Abel JJ, Rowntree LG, Turner BB. On the removal of diffusable substances from the circulating blood by means of dialysis. Transactions of the Association of American Physicians, 1913. Transfus Sci. 1990;11:164–165. [PubMed] [Google Scholar]
- 38.Goldfinger D, Capostagno V, Lowe C, Sacks HJ, Gatti RA. Use of long-term leukapheresis in the treatment of chronic lymphocytic leukemia. Transfusion. 1980;20:450–454. doi: 10.1046/j.1537-2995.1980.20480260279.x. [DOI] [PubMed] [Google Scholar]
- 39.Lazarus HM, Cohen SB, Clegg DO, Menitove JE, Sorin SB, Hinkle S, Markenson JA, Saal S, Goodnough LT, Fleischmann RM. Selective in vivo removal of rheumatoid factor by an extracorporeal treatment device in rheumatoid arthritis patients. Transfusion. 1991;31:122–128. doi: 10.1046/j.1537-2995.1991.31291142942.x. [DOI] [PubMed] [Google Scholar]
- 40.Eshleman JR, Silberstein LE. The development of selective plasmapheresis as a means for specific therapeutic intervention. Transfusion. 1991;31:96–98. doi: 10.1046/j.1537-2995.1991.31291142958.x. [DOI] [PubMed] [Google Scholar]
- 41.Shimoyama T, Sawada K, Hiwatashi N, Sawada T, Matsueda K, Munakata A, Asakura H, Tanaka T, Kasukawa R, Kimura K, et al. Safety and efficacy of granulocyte and monocyte adsorption apheresis in patients with active ulcerative colitis: a multicenter study. J Clin Apher. 2001;16:1–9. doi: 10.1002/jca.1000. [DOI] [PubMed] [Google Scholar]
- 42.Suzuki Y, Yoshimura N, Saniabadi AR, Saito Y. Selective granulocyte and monocyte adsorptive apheresis as a first-line treatment for steroid naïve patients with active ulcerative colitis: a prospective uncontrolled study. Dig Dis Sci. 2004;49:565–571. doi: 10.1023/b:ddas.0000026299.43792.ae. [DOI] [PubMed] [Google Scholar]
- 43.Cohen RD. Treating ulcerative colitis without medications--”look mom, no drugs!”. Gastroenterology. 2005;128:235–236. doi: 10.1053/j.gastro.2004.11.024. [DOI] [PubMed] [Google Scholar]
- 44.Hanai H, Watanabe F, Yamada M, Sato Y, Takeuchi K, Iida T, Tozawa K, Tanaka T, Maruyama Y, Matsushita I, et al. Adsorptive granulocyte and monocyte apheresis versus prednisolone in patients with corticosteroid-dependent moderately severe ulcerative colitis. Digestion. 2004;70:36–44. doi: 10.1159/000080079. [DOI] [PubMed] [Google Scholar]
- 45.Saniabadi AR, Hanai H. Therapeutic apheresis from the early civilizations to the twenty-first century. Gastroenterol Clin Biol. 2010;34:645–648. doi: 10.1016/j.gcb.2010.09.003. [DOI] [PubMed] [Google Scholar]
- 46.Hanai H, Watanabe F, Saniabadi AR, Matsushitai I, Takeuchi K, Iida T. Therapeutic efficacy of granulocyte and monocyte adsorption apheresis in severe active ulcerative colitis. Dig Dis Sci. 2002;47:2349–2353. doi: 10.1023/a:1020159932758. [DOI] [PubMed] [Google Scholar]
- 47.Aoki H, Nakamura K, Yoshimatsu Y, Tsuda Y, Irie M, Fukuda K, Hosoe N, Takada N, Shirai K, Suzuki Y. Adacolumn selective leukocyte adsorption apheresis in patients with active ulcerative colitis: clinical efficacy, effects on plasma IL-8, and expression of Toll-like receptor 2 on granulocytes. Dig Dis Sci. 2007;52:1427–1433. doi: 10.1007/s10620-006-9406-8. [DOI] [PubMed] [Google Scholar]
- 48.Saniabadi AR, Hanai H, Fukunaga K, Sawada K, Shima C, Bjarnason I, Lofberg R. Therapeutic leukocytapheresis for inflammatory bowel disease. Transfus Apher Sci. 2007;37:191–200. doi: 10.1016/j.transci.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 49.Tanaka T, Okanobu H, Kuga Y, Yoshifuku Y, Fujino H, Miwata T, Moriya T, Nishida T, Oya T. Clinical and endoscopic features of responders and non-responders to adsorptive leucocytapheresis: a report based on 120 patients with active ulcerative colitis. Gastroenterol Clin Biol. 2010;34:687–695. doi: 10.1016/j.gcb.2010.08.007. [DOI] [PubMed] [Google Scholar]
- 50.Hanai H, Watanabe F, Takeuchi K, Iida T, Yamada M, Iwaoka Y, Saniabadi A, Matsushita I, Sato Y, Tozawa K, et al. Leukocyte adsorptive apheresis for the treatment of active ulcerative colitis: a prospective, uncontrolled, pilot study. Clin Gastroenterol Hepatol. 2003;1:28–35. doi: 10.1053/jcgh.2003.50005. [DOI] [PubMed] [Google Scholar]
- 51.Hanai H. Positions of selective leukocytapheresis in the medical therapy of ulcerative colitis. World J Gastroenterol. 2006;12:7568–7577. doi: 10.3748/wjg.v12.i47.7568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Suzuki Y, Yoshimura N, Fukuda K, Shirai K, Saito Y, Saniabadi AR. A retrospective search for predictors of clinical response to selective granulocyte and monocyte apheresis in patients with ulcerative colitis. Dig Dis Sci. 2006;51:2031–2038. doi: 10.1007/s10620-006-9199-9. [DOI] [PubMed] [Google Scholar]
- 53.Tanaka T, Okanobu H, Yoshimi S, Murakami E, Kogame A, Imagawa H, Numata Y, Kuga Y, Moriya T, Ohya T, et al. In patients with ulcerative colitis, adsorptive depletion of granulocytes and monocytes impacts mucosal level of neutrophils and clinically is most effective in steroid naïve patients. Dig Liver Dis. 2008;40:731–736. doi: 10.1016/j.dld.2008.02.012. [DOI] [PubMed] [Google Scholar]
- 54.Heimann TM, Aufses AH. The role of peripheral lymphocytes in the prediction of recurrence in Crohn’s disease. Surg Gynecol Obstet. 1985;160:295–298. [PubMed] [Google Scholar]
- 55.Powrie F, Read S, Mottet C, Uhlig H, Maloy K. Control of immune pathology by regulatory T cells. Novartis Found Symp. 2003;252:92–98; discussion 98-105, 106-114. [PubMed] [Google Scholar]
- 56.Maul J, Loddenkemper C, Mundt P, Berg E, Giese T, Stallmach A, Zeitz M, Duchmann R. Peripheral and intestinal regulatory CD4+ CD25(high) T cells in inflammatory bowel disease. Gastroenterology. 2005;128:1868–1878. doi: 10.1053/j.gastro.2005.03.043. [DOI] [PubMed] [Google Scholar]
- 57.Uhlig HH, Powrie F. The role of mucosal T lymphocytes in regulating intestinal inflammation. Springer Semin Immunopathol. 2005;27:167–180. doi: 10.1007/s00281-005-0206-6. [DOI] [PubMed] [Google Scholar]
- 58.Liu H, Hu B, Xu D, Liew FY. CD4+CD25+ regulatory T cells cure murine colitis: the role of IL-10, TGF-beta, and CTLA4. J Immunol. 2003;171:5012–5017. doi: 10.4049/jimmunol.171.10.5012. [DOI] [PubMed] [Google Scholar]
- 59.Huber S, Schramm C, Lehr HA, Mann A, Schmitt S, Becker C, Protschka M, Galle PR, Neurath MF, Blessing M. Cutting edge: TGF-beta signaling is required for the in vivo expansion and immunosuppressive capacity of regulatory CD4+CD25+ T cells. J Immunol. 2004;173:6526–6531. doi: 10.4049/jimmunol.173.11.6526. [DOI] [PubMed] [Google Scholar]
- 60.Kanai T, Watanabe M. Clinical application of human CD4+ CD25+ regulatory T cells for the treatment of inflammatory bowel diseases. Expert Opin Biol Ther. 2005;5:451–462. doi: 10.1517/14712598.5.4.451. [DOI] [PubMed] [Google Scholar]
- 61.Yokoyama Y, Fukunaga K, Fukuda Y, Tozawa K, Kamikozuru K, Ohnishi K, Kusaka T, Kosaka T, Hida N, Ohda Y, et al. Demonstration of low-regulatory CD25High+CD4+ and high-pro-inflammatory CD28-CD4+ T-Cell subsets in patients with ulcerative colitis: modified by selective granulocyte and monocyte adsorption apheresis. Dig Dis Sci. 2007;52:2725–2731. doi: 10.1007/s10620-006-9560-z. [DOI] [PubMed] [Google Scholar]
- 62.Hiraishi K, Takeda Y, Shiobara N, Shibusawa H, Jimma F, Kashiwagi N, Saniabadi AR, Adachi M. Studies on the mechanisms of leukocyte adhesion to cellulose acetate beads: an in vitro model to assess the efficacy of cellulose acetate carrier-based granulocyte and monocyte adsorptive apheresis. Ther Apher Dial. 2003;7:334–340. doi: 10.1046/j.1526-0968.2003.00049.x. [DOI] [PubMed] [Google Scholar]
- 63.D’Arrigo C, Candal-Couto JJ, Greer M, Veale DJ, Woof JM. Human neutrophil Fc receptor-mediated adhesion under flow: a hollow fibre model of intravascular arrest. Clin Exp Immunol. 1995;100:173–179. doi: 10.1111/j.1365-2249.1995.tb03620.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lerebours E, Bussel A, Modigliani R, Bastit D, Florent C, Rabian C, René E, Soulé JC. Treatment of Crohn’s disease by lymphocyte apheresis: a randomized controlled trial. Groupe d’Etudes Thérapeutiques des Affections Inflammatoires Digestives. Gastroenterology. 1994;107:357–361. doi: 10.1016/0016-5085(94)90159-7. [DOI] [PubMed] [Google Scholar]
- 65.Kanai T, Hibi T, Watanabe M. The logics of leukocytapheresis as a natural biological therapy for inflammatory bowel disease. Expert Opin Biol Ther. 2006;6:453–466. doi: 10.1517/14712598.6.5.453. [DOI] [PubMed] [Google Scholar]
- 66.Kanke K, Nakano M, Hiraishi H, Terano A. Clinical evaluation of granulocyte/monocyte apheresis therapy for active ulcerative colitis. Dig Liver Dis. 2004;36:811–817. doi: 10.1016/j.dld.2004.08.004. [DOI] [PubMed] [Google Scholar]
- 67.Yamamoto T, Umegae S, Matsumoto K. Mucosal healing in patients with ulcerative colitis during a course of selective leukocytapheresis therapy: a prospective cohort study. Inflamm Bowel Dis. 2010;16:1905–1911. doi: 10.1002/ibd.21260. [DOI] [PubMed] [Google Scholar]
- 68.Takayama T, Kanai T, Matsuoka K, Okamoto S, Sujino T, Mikami Y, Hisamatsu T, Yajima T, Iwao Y, Ogata H, et al. Long-term prognosis of patients with ulcerative colitis treated with cytapheresis therapy. J Crohns Colitis. 2013;7:e49–e54. doi: 10.1016/j.crohns.2012.05.005. [DOI] [PubMed] [Google Scholar]
- 69.Hibi T, Sameshima Y, Sekiguchi Y, Hisatome Y, Maruyama F, Moriwaki K, Shima C, Saniabadi AR, Matsumoto T. Treating ulcerative colitis by Adacolumn therapeutic leucocytapheresis: clinical efficacy and safety based on surveillance of 656 patients in 53 centres in Japan. Dig Liver Dis. 2009;41:570–577. doi: 10.1016/j.dld.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 70.Yamamoto T, Umegae S, Matsumoto K. Long-term clinical impact of early introduction of granulocyte and monocyte adsorptive apheresis in new onset, moderately active, extensive ulcerative colitis. J Crohns Colitis. 2012;6:750–755. doi: 10.1016/j.crohns.2011.12.009. [DOI] [PubMed] [Google Scholar]
- 71.Kato S, Hosomi E, Amano F, Kobayashi T, Kani K, Yamamoto R, Ogawa T, Matsuda A, Sato Y, Izaki S, et al. The efficacy of intensive granulocyte and monocyte adsorption apheresis in a patient with Crohn’s disease complicated by extensive subcutaneous aseptic neutrophilic abscesses. J Crohns Colitis. 2012;6:787–791. doi: 10.1016/j.crohns.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 72.Yamamoto T, Saniabadi AR, Maruyama Y, Umegae S, Matsumoto K. Factors affecting clinical and endoscopic efficacies of selective leucocytapheresis for ulcerative colitis. Dig Liver Dis. 2007;39:626–633. doi: 10.1016/j.dld.2007.04.007. [DOI] [PubMed] [Google Scholar]
- 73.Yoshimura N, Tadami T, Kawaguchi T, Sako M, Yoshimoto H, Yamaka T, Takazoe M. Processed blood volume impacts clinical efficacy in patients with ulcerative colitis undergoing adsorptive depletion of myeloid lineage leucocytes. J Gastroenterol. 2012;47:49–55. doi: 10.1007/s00535-011-0464-0. [DOI] [PubMed] [Google Scholar]
- 74.Yokoyama Y, Kawai M, Fukunaga K, Kamikozuru K, Nagase K, Nogami K, Kono T, Ohda Y, Iimuro M, Hida N, et al. Looking for predictive factors of clinical response to adsorptive granulocyte and monocyte apheresis in patients with ulcerative colitis: markers of response to GMA. BMC Gastroenterol. 2013;13:27. doi: 10.1186/1471-230X-13-27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Tanaka T, Sugiyama S, Goishi H, Kajihara T, Akagi M, Miura T. Treatment of children and adolescents with ulcerative colitis by adsorptive depletion of myeloid lineage leucocytes as monotherapy or in combination with low dose prednisolone after failure of first-line medications. BMC Gastroenterol. 2013;13:130. doi: 10.1186/1471-230X-13-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Tomomasa T, Kobayashi A, Kaneko H, Mika S, Maisawa S, Chino Y, Syou H, Yoden A, Fujino J, Tanikawa M, et al. Granulocyte adsorptive apheresis for pediatric patients with ulcerative colitis. Dig Dis Sci. 2003;48:750–754. doi: 10.1023/a:1022892927121. [DOI] [PubMed] [Google Scholar]
- 77.Tominaga K, Nakano M, Hoshino M, Kanke K, Hiraishi H. Efficacy, safety and cost analyses in ulcerative colitis patients undergoing granulocyte and monocyte adsorption or receiving prednisolone. BMC Gastroenterol. 2013;13:41. doi: 10.1186/1471-230X-13-41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Panés J, Guilera M, Ginard D, Hinojosa J, González-Carro P, González-Lara V, Varea V, Domènech E, Badia X. Treatment cost of ulcerative colitis is apheresis with Adacolumn cost-effective? Dig Liver Dis. 2007;39:617–625. doi: 10.1016/j.dld.2007.03.007. [DOI] [PubMed] [Google Scholar]
- 79.Muratov V, Lundahl J, Ulfgren AK, Elvin K, Fehrman I, Ahlborg N, Ost A, Hittel N, Saniabadi A, Löfberg R. Down-regulation of interferon-gamma parallels clinical response to selective leukocyte apheresis in patients with inflammatory bowel disease: a 12-month follow-up study. Int J Colorectal Dis. 2006;21:493–504. doi: 10.1007/s00384-005-0069-2. [DOI] [PubMed] [Google Scholar]
- 80.Ruuska T, Wewer V, Lindgren F, Malmborg P, Lindquist M, Marthinsen L, Browaldh L, Casswall T, Kalliomäki M, Grönlund J. Granulocyte-monocyte adsorptive apheresis in pediatric inflammatory bowel disease: results, practical issues, safety, and future perspectives. Inflamm Bowel Dis. 2009;15:1049–1054. doi: 10.1002/ibd.20859. [DOI] [PubMed] [Google Scholar]
- 81.Bresci G, Parisi G, Mazzoni A, Scatena F, Capria A. Granulocytapheresis versus methylprednisolone in patients with acute ulcerative colitis: 12-month follow up. J Gastroenterol Hepatol. 2008;23:1678–1682. doi: 10.1111/j.1440-1746.2008.05595.x. [DOI] [PubMed] [Google Scholar]
- 82.Kruis W, Dignass A, Steinhagen-Thiessen E, Morgenstern J, Mössner J, Schreiber S, Vecchi M, Malesci A, Reinshagen M, Löfberg R. Open label trial of granulocyte apheresis suggests therapeutic efficacy in chronically active steroid refractory ulcerative colitis. World J Gastroenterol. 2005;11:7001–7006. doi: 10.3748/wjg.v11.i44.7001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Bresci G, Parisi G, Mazzoni A, Scatena F, Capria A. Treatment of patients with acute ulcerative colitis: conventional corticosteroid therapy (MP) versus granulocytapheresis (GMA): a pilot study. Dig Liver Dis. 2007;39:430–434. doi: 10.1016/j.dld.2007.01.001. [DOI] [PubMed] [Google Scholar]
- 84.Caprilli R, D’Ovidio V. Leukocytapheresis as promising therapy for inflammatory bowel disease. Dig Liver Dis. 2007;39:435–437. doi: 10.1016/j.dld.2007.02.003. [DOI] [PubMed] [Google Scholar]
- 85.Domènech E, Hinojosa J, Esteve-Comas M, Gomollón F, Herrera JM, Bastida G, Obrador A, Ruiz R, Saro C, Gassull MA. Granulocyteaphaeresis in steroid-dependent inflammatory bowel disease: a prospective, open, pilot study. Aliment Pharmacol Ther. 2004;20:1347–1352. doi: 10.1111/j.1365-2036.2004.02288.x. [DOI] [PubMed] [Google Scholar]
- 86.Maiden L, Takeuchi K, Baur R, Bjarnason I, O’Donohue J, Forgacs I, Chung-Faye G, Sanderson J, Bjarnason I. Selective white cell apheresis reduces relapse rates in patients with IBD at significant risk of clinical relapse. Inflamm Bowel Dis. 2008;14:1413–1418. doi: 10.1002/ibd.20505. [DOI] [PubMed] [Google Scholar]
- 87.Lindberg A, Eberhardson M, Karlsson M, Karlén P. Long-term follow-up with Granulocyte and Monocyte Apheresis re-treatment in patients with chronically active inflammatory bowel disease. BMC Gastroenterol. 2010;10:73. doi: 10.1186/1471-230X-10-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Cabriada JL, Domènech E, Ibargoyen N, Hernández V, Clofent J, Ginard D, Gutiérrez-Ibarluzea I, Hinojosa J. Leukocytapheresis for steroid-dependent ulcerative colitis in clinical practice: results of a nationwide Spanish registry. J Gastroenterol. 2012;47:359–365. doi: 10.1007/s00535-011-0499-2. [DOI] [PubMed] [Google Scholar]
- 89.Dignass AU, Eriksson A, Kilander A, Pukitis A, Rhodes JM, Vavricka S. Clinical trial: five or ten cycles of granulocyte-monocyte apheresis show equivalent efficacy and safety in ulcerative colitis. Aliment Pharmacol Ther. 2010;31:1286–1295. doi: 10.1111/j.1365-2036.2010.04295.x. [DOI] [PubMed] [Google Scholar]
- 90.Bresci G, Romano A, Mazzoni A, Scatena F, Altomare E, Capria A, Sacco R. Feasibility and safety of granulocytapheresis in Crohn’s disease: a prospective cohort study. Gastroenterol Clin Biol. 2010;34:682–686. doi: 10.1016/j.gcb.2010.09.009. [DOI] [PubMed] [Google Scholar]
- 91.Sacco R, Romano A, Mazzoni A, Bertini M, Federici G, Metrangolo S, Parisi G, Nencini C, Giampietro C, Bertoni M, et al. Granulocytapheresis in steroid-dependent and steroid-resistant patients with inflammatory bowel disease: a prospective observational study. J Crohns Colitis. 2013;7:e692–e697. doi: 10.1016/j.crohns.2013.06.012. [DOI] [PubMed] [Google Scholar]
- 92.Sands BE, Sandborn WJ, Feagan B, Löfberg R, Hibi T, Wang T, Gustofson LM, Wong CJ, Vandervoort MK, Hanauer S. A randomized, double-blind, sham-controlled study of granulocyte/monocyte apheresis for active ulcerative colitis. Gastroenterology. 2008;135:400–409. doi: 10.1053/j.gastro.2008.04.023. [DOI] [PubMed] [Google Scholar]
- 93.Sands BE, Katz S, Wolf DC, Feagan BG, Wang T, Gustofson LM, Wong C, Vandervoort MK, Hanauer S. A randomised, double-blind, sham-controlled study of granulocyte/monocyte apheresis for moderate to severe Crohn’s disease. Gut. 2013;62:1288–1294. doi: 10.1136/gutjnl-2011-300995. [DOI] [PubMed] [Google Scholar]
- 94.Schwartz D, Ferguson JR. Current pharmacologic treatment paradigms for inflammatory bowel disease and the potential role of granulocyte/monocyte apheresis. Curr Med Res Opin. 2007;23:2715–2728. doi: 10.1185/030079907x233241. [DOI] [PubMed] [Google Scholar]
- 95.Abreu MT, Plevy S, Sands BE, Weinstein R. Selective leukocyte apheresis for the treatment of inflammatory bowel disease. J Clin Gastroenterol. 2007;41:874–888. doi: 10.1097/MCG.0b013e3180479435. [DOI] [PubMed] [Google Scholar]
- 96.Sandborn WJ. Preliminary data on the use of apheresis in inflammatory bowel disease. Inflamm Bowel Dis. 2006;12 Suppl 1:S15–S21. doi: 10.1097/01.mib.0000195387.26892.22. [DOI] [PubMed] [Google Scholar]
- 97.Matsui T, Nishimura T, Matake H, Ohta T, Sakurai T, Yao T. Granulocytapheresis for Crohn’s disease: a report on seven refractory patients. Am J Gastroenterol. 2003;98:511–512. doi: 10.1111/j.1572-0241.2003.07251.x. [DOI] [PubMed] [Google Scholar]
- 98.Fukuda Y, Matsui T, Suzuki Y, Kanke K, Matsumoto T, Takazoe M, Matsumoto T, Motoya S, Honma T, Sawada K, et al. Adsorptive granulocyte and monocyte apheresis for refractory Crohn’s disease: an open multicenter prospective study. J Gastroenterol. 2004;39:1158–1164. doi: 10.1007/s00535-004-1465-z. [DOI] [PubMed] [Google Scholar]
- 99.Sakuraba A, Motoya S, Watanabe K, Nishishita M, Kanke K, Matsui T, Suzuki Y, Oshima T, Kunisaki R, Matsumoto T, et al. An open-label prospective randomized multicenter study shows very rapid remission of ulcerative colitis by intensive granulocyte and monocyte adsorptive apheresis as compared with routine weekly treatment. Am J Gastroenterol. 2009;104:2990–2995. doi: 10.1038/ajg.2009.453. [DOI] [PubMed] [Google Scholar]
- 100.Yamamoto T, Umegae S, Matsumoto K. Daily granulocyte and monocyte adsorptive apheresis in patients with active ulcerative colitis: a prospective safety and feasibility study. J Gastroenterol. 2011;46:1003–1009. doi: 10.1007/s00535-011-0428-4. [DOI] [PubMed] [Google Scholar]
- 101.Tibble JA, Sigthorsson G, Bridger S, Fagerhol MK, Bjarnason I. Surrogate markers of intestinal inflammation are predictive of relapse in patients with inflammatory bowel disease. Gastroenterology. 2000;119:15–22. doi: 10.1053/gast.2000.8523. [DOI] [PubMed] [Google Scholar]
- 102.Hanai H, Takeuchi K, Iida T, Kashiwagi N, Saniabadi AR, Matsushita I, Sato Y, Kasuga N, Nakamura T. Relationship between fecal calprotectin, intestinal inflammation, and peripheral blood neutrophils in patients with active ulcerative colitis. Dig Dis Sci. 2004;49:1438–1443. doi: 10.1023/b:ddas.0000042243.47279.87. [DOI] [PubMed] [Google Scholar]
- 103.Ohmori T, Yamagiwa A, Nakamura I, Nishikawa K, Saniabadi AR. Treatment of pyoderma gangrenosum associated with Crohn’s disease. Am J Gastroenterol. 2003;98:2101–2102. doi: 10.1111/j.1572-0241.2003.07657.x. [DOI] [PubMed] [Google Scholar]
- 104.Kanekura T, Maruyama I, Kanzaki T. Granulocyte and monocyte adsorption apheresis for pyoderma gangrenosum. J Am Acad Dermatol. 2002;47:320–321. doi: 10.1067/mjd.2002.120597. [DOI] [PubMed] [Google Scholar]
- 105.Kanekura T, Yoshii N, Yonezawa T, Kawabata H, Saruwatari H, Kanzaki T. Treatment of pustular psoriasis with granulocyte and monocyte adsorption apheresis. J Am Acad Dermatol. 2003;49:329–332. doi: 10.1067/s0190-9622(03)00795-3. [DOI] [PubMed] [Google Scholar]
- 106.Seishima M, Mizutani Y, Shibuya Y, Nagasawa C, Aoki T. Efficacy of granulocyte and monocyte adsorption apheresis for pustular psoriasis. Ther Apher Dial. 2008;12:13–18. doi: 10.1111/j.1744-9987.2007.00536.x. [DOI] [PubMed] [Google Scholar]
- 107.Ikeda S, Takahashi H, Suga Y, Eto H, Etoh T, Okuma K, Takahashi K, Kanbara T, Seishima M, Morita A, et al. Therapeutic depletion of myeloid lineage leukocytes in patients with generalized pustular psoriasis indicates a major role for neutrophils in the immunopathogenesis of psoriasis. J Am Acad Dermatol. 2013;68:609–617. doi: 10.1016/j.jaad.2012.09.037. [DOI] [PubMed] [Google Scholar]
- 108.Belge KU, Dayyani F, Horelt A, Siedlar M, Frankenberger M, Frankenberger B, Espevik T, Ziegler-Heitbrock L. The proinflammatory CD14+CD16+DR++ monocytes are a major source of TNF. J Immunol. 2002;168:3536–3542. doi: 10.4049/jimmunol.168.7.3536. [DOI] [PubMed] [Google Scholar]
- 109.Hanai H, Iida T, Takeuchi K, Watanabe F, Yamada M, Kikuyama M, Maruyama Y, Iwaoka Y, Hirayama K, Nagata S, et al. Adsorptive depletion of elevated proinflammatory CD14+CD16+DR++ monocytes in patients with inflammatory bowel disease. Am J Gastroenterol. 2008;103:1210–1216. doi: 10.1111/j.1572-0241.2007.01714.x. [DOI] [PubMed] [Google Scholar]
- 110.Hanai H, Watanabe F, Yamada M, Sato Y, Takeuchi K, Iida T, Tozawa K, Tanaka T, Maruyama Y, Matsushita I, et al. Correlation of serum soluble TNF-alpha receptors I and II levels with disease activity in patients with ulcerative colitis. Am J Gastroenterol. 2004;99:1532–1538. doi: 10.1111/j.1572-0241.2004.30432.x. [DOI] [PubMed] [Google Scholar]
- 111.Mohler KM, Torrance DS, Smith CA, Goodwin RG, Stremler KE, Fung VP, Madani H, Widmer MB. Soluble tumor necrosis factor (TNF) receptors are effective therapeutic agents in lethal endotoxemia and function simultaneously as both TNF carriers and TNF antagonists. J Immunol. 1993;151:1548–1561. [PubMed] [Google Scholar]
- 112.Hanai H, Iida T, Yamada M, Sato Y, Takeuchi K, Tanaka T, Kondo K, Kikuyama M, Maruyama Y, Iwaoka Y, et al. Effects of adacolumn selective leukocytapheresis on plasma cytokines during active disease in patients with active ulcerative colitis. World J Gastroenterol. 2006;12:3393–3399. doi: 10.3748/wjg.v12.i21.3393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Takeda Y, Shiobara N, Saniabadi AR, Adachi M, Hiraishi K. Adhesion dependent release of hepatocyte growth factor and interleukin-1 receptor antagonist from human blood granulocytes and monocytes: evidence for the involvement of plasma IgG, complement C3 and beta2 integrin. Inflamm Res. 2004;53:277–283. doi: 10.1007/s00011-004-1253-5. [DOI] [PubMed] [Google Scholar]
- 114.Dinarello CA, Thompson RC. Blocking IL-1: interleukin 1 receptor antagonist in vivo and in vitro. Immunol Today. 1991;12:404–410. doi: 10.1016/0167-5699(91)90142-G. [DOI] [PubMed] [Google Scholar]
- 115.Tahara Y, Ido A, Yamamoto S, Miyata Y, Uto H, Hori T, Hayashi K, Tsubouchi H. Hepatocyte growth factor facilitates colonic mucosal repair in experimental ulcerative colitis in rats. J Pharmacol Exp Ther. 2003;307:146–151. doi: 10.1124/jpet.103.054106. [DOI] [PubMed] [Google Scholar]
- 116.Yamamoto T, Saniabadi AR, Umegae S, Matsumoto K. Impact of selective leukocytapheresis on mucosal inflammation and ulcerative colitis: cytokine profiles and endoscopic findings. Inflamm Bowel Dis. 2006;12:719–726. doi: 10.1097/00054725-200608000-00008. [DOI] [PubMed] [Google Scholar]
- 117.Hanai H, Takeda Y, Eberhardson M, Gruber R, Saniabadi AR, Winqvist O, Lofberg R. The mode of actions of the Adacolumn therapeutic leucocytapheresis in patients with inflammatory bowel disease: a concise review. Clin Exp Immunol. 2011;163:50–58. doi: 10.1111/j.1365-2249.2010.04279.x. [DOI] [PMC free article] [PubMed] [Google Scholar]


