Abstract
Background and objectives
The Statewide Sharing variance to the national kidney allocation policy allocates kidneys not used within the procuring donor service area (DSA), first within the state, before the kidneys are offered regionally and nationally. Tennessee and Florida implemented this variance. Known geographic differences exist between the 58 DSAs, in direct violation of the Final Rule stipulated by the US Department of Health and Human Services. This study examined the effect of Statewide Sharing on geographic allocation disparity over time between DSAs within Tennessee and Florida and compared them with geographic disparity between the DSAs within a state for all states with more than one DSA (California, New York, North Carolina, Ohio, Pennsylvania, Texas, and Wisconsin).
Design, setting, participants, & measurements
A retrospective analysis from 1987 to 2009 was conducted using Organ Procurement and Transplant Network data. Five previously used indicators for geographic allocation disparity were applied: deceased-donor kidney transplant rates, waiting time to transplantation, cumulative dialysis time at transplantation, 5-year graft survival, and cold ischemic time.
Results
Transplant rates, waiting time, dialysis time, and graft survival varied greatly between deceased-donor kidney recipients in DSAs in all states in 1987. After implementation of Statewide Sharing in 1992, disparity indicators decreased by 41%, 36%, 31%, and 9%, respectively, in Tennessee and by 28%, 62%, 34%, and 19%, respectively in Florida, such that the geographic allocation disparity in Tennessee and Florida almost completely disappeared. Statewide kidney allocations incurred 7.5 and 5 fewer hours of cold ischemic time in Tennessee and Florida, respectively. Geographic disparity between DSAs in all the other states worsened or improved to a lesser degree.
Conclusions
As sweeping changes to the kidney allocation system are being discussed to alleviate geographic disparity—changes that are untested run the risk of unintended consequences—more limited changes, such as Statewide Sharing, should be further studied and considered.
Keywords: renal transplantation, transplant outcomes, kidney donation
Introduction
Kidney transplantation is an effective treatment for patients with ESRD. In 2011, nearly 17,000 kidney transplants were performed in the United States, but 94,000 patients remained on the waiting list (1,2). This discrepancy has led to an increase in waiting time to kidney transplantation from 3.3 years in 2000 to 4.72 years by 2009, increasing the cumulative time on dialysis and the mortality rate while awaiting a transplant (3–5). Furthermore, there is disparity in waiting time for a kidney transplant depending on where a patient is located geographically. This violates the “Final Rule,” a mandate by the US Department of Health and Human Services from 1998 stipulating that the allocation of kidneys within the United States achieve geographic parity for all waitlisted patients (3,4,6). The current United Network for Organ Sharing (UNOS) kidney allocation system allocates a procured kidney to the procuring donor service area (DSA) before regional and national allocation. Several strategies to reduce geographic disparities have been proposed (7–11). A variance called Statewide Sharing was granted by UNOS to Tennessee (entailing two DSAs) in November 1992 and to Florida (entailing four DSAs) in June 1991 (12). Statewide Sharing first offers a procured kidney to the procuring DSA but then allocates the kidney to the other DSAs within the state before regional and national allocation (12). As UNOS considers new allocation policies, understanding the effects of implementation of Statewide Sharing on geographic disparity may be instructive. Therefore, we analyzed those effects on the geographic allocation disparity between the DSAs within Tennessee and Florida over time and compared them with findings in states that followed the national UNOS allocation policy instead.
Materials and Methods
Geographic disparity between DSAs was analyzed for all states that entail more than one complete DSA. These states included California, Florida, North Carolina, New York, Ohio, Pennsylvania, Tennessee, Texas, and Wisconsin. States with fewer than two complete DSAs were excluded from the analysis because two or more DSAs are needed to assess disparity.
Data Sources
After approval by the Northwestern University Institutional Review Board, data were obtained from the Organ Procurement and Transplant Network Standard Transplant Analysis and Research for adult (>18 years) kidney transplant candidates and deceased-donor kidney transplant recipients. The primary cohort includes all transplant recipients who received a deceased-donor kidney transplant during the study period (1987–2009). Two additional cohorts were included to test the robustness of our conclusions. One adjusted for transplant kidney quality using the Kidney Donor Risk Index (KDRI) by ensuring an equal percentage of randomly selected waitlisted patients in all DSAs in the following four subgroups: KDRI scores of 0–0.75, 0.76–1.5, 1.6–2.25, and >2.25. The other cohort, referred to as the additional exclusion cohort, excluded paybacks, and no HLA mismatch kidney candidates in the analysis.
Geographic disparity was measured by five indicators that have previously been identified in the transplant literature as suitable indicators of geographic allocation disparity: (1) mean transplant rate, (2) median waiting time, (3) median cumulative time on dialysis, (4) 5-year graft survival, and (5) cold ischemic time (CIT) as an indicator of allocation efficiency (13–17). The annual transplant rate was calculated as the mean number of transplant candidates per transplant. The waiting time to transplant was calculated for each recipient, and the median was calculated for each DSA. For all nonpreemptive kidney transplant recipients, the time on dialysis was calculated as the time between onset of dialysis and transplantation, and the median cumulative time on dialysis was calculated for each DSA. Five-year graft survival was calculated using unadjusted Kaplan–Meier analysis.
Statistical Analyses
The five disparity indicators (hereafter referred to as the allocation disparity indicators) were assessed from 1987 to 2009. Furthermore, comparative analysis was performed between the 5-year time period preceding the Statewide Sharing variance (1987–1991) and the time period afterward (1992–2009) using time-series analyses. In addition, Tennessee was compared with the three other states that entail two complete DSAs (North Carolina, Pennsylvania, Wisconsin), and Florida was compared with the three other states that entail four DSAs (California, New York, Ohio).
Data were summarized using descriptive statistics (mean, median, SD, frequency, and proportions). Chi-squared tests were used to compare for significant differences across transplant recipient populations in the four respective states (Tennessee, North Carolina, Pennsylvania, and Wisconsin; Florida, California, New York, and Ohio) (Table 1). Significant differences in 5-year graft survival before and after the variance were studied by comparing hazard ratios from a multivariable Cox regression model, adjusted for transplant recipient characteristics, listed in Table 1. Significant differences in the geographic allocation disparity indicators before and recently after Statewide Sharing implementation (Table 2) were tested using chi-squared tests, t tests, and Wilcoxon two-sample tests. All analyses were conducted using SAS software, version 9.3 (SAS Institute, Cary, NC).
Table 1.
Transplant recipient characteristics by state
| Characteristics | TN | NC | PA | WI | P Valuea | FL | CA | NY | OH | P Valuea |
|---|---|---|---|---|---|---|---|---|---|---|
| Patients (n) | 4658 | 4903 | 14,329 | 4733 | 10,863 | 20,581 | 11,298 | 7374 | ||
| No. of DSAs | 2 | 2 | 2 | 2 | 4 | 4 | 4 | 4 | ||
| Blood type | ||||||||||
| A | 39.6 | 38.2 | 39.3 | 42.0 | 0.83 | 36.6 | 36.4 | 35.1 | 38.4 | 0.89 |
| AB | 5.6 | 5.3 | 5.5 | 6.2 | 0.94 | 5.1 | 5.6 | 6.4 | 5.6 | 0.85 |
| B | 11.8 | 12.4 | 12.6 | 12.8 | 0.98 | 12.9 | 13.3 | 13.0 | 11.9 | 0.94 |
| O | 43.0 | 44.1 | 42.7 | 38.9 | 0.67 | 45.4 | 44.8 | 45.5 | 44.1 | 0.99 |
| Age at transplant | ||||||||||
| 0–17 yr | 3.7 | 4.1 | 4.1 | 2.4 | 0.45 | 3.8 | 6.5 | 5.1 | 3.6 | 0.08 |
| 18–39 yr | 28.8 | 28.2 | 23.2 | 22.7 | 0.08 | 23.7 | 27.2 | 25.4 | 25.6 | 0.65 |
| 40–64 yr | 60.2 | 59.2 | 57.6 | 63.0 | 0.66 | 57.2 | 55.3 | 57.3 | 60.8 | 0.73 |
| ≥65 yr | 7.4 | 8.5 | 15.0 | 12.0 | <0.001 | 15.3 | 10.9 | 12.2 | 10.0 | 0.09 |
| Men | 62.2 | 59.2 | 62.1 | 60.8 | 0.84 | 61.2 | 59.7 | 60.5 | 61.8 | 0.97 |
| Race | ||||||||||
| Non-Hispanic White | 57.5 | 40.7 | 63.8 | 68.9 | <0.001 | 51.4 | 35.0 | 47.0 | 62.6 | <0.001 |
| Non-Hispanic black | 40.5 | 55.1 | 29.1 | 19.9 | <0.001 | 30.9 | 15.2 | 32.1 | 33.5 | <0.001 |
| Hispanic | 0.9 | 1.3 | 3.6 | 4.8 | 0.001 | 13.8 | 30.8 | 13.4 | 1.8 | <0.001 |
| Asian | 0.8 | 1.5 | 2.7 | 4.9 | 0.001 | 2.7 | 15.6 | 5.9 | 1.6 | <0.001 |
| Other | 0.3 | 1.3 | 0.8 | 1.6 | 0.20 | 1.2 | 3.3 | 1.5 | 0.5 | 0.01 |
| Panel reactive antibodies | ||||||||||
| 0–19 | 81.1 | 83.9 | 85.6 | 83.4 | 0.86 | 89.1 | 88.3 | 86.5 | 85.6 | 0.95 |
| 20–79 | 12.9 | 11.6 | 9.6 | 11.4 | 0.31 | 8.7 | 8.2 | 9.8 | 11.0 | 0.54 |
| 80–100 | 6.0 | 4.5 | 4.8 | 5.2 | 0.80 | 2.3 | 3.4 | 3.7 | 3.4 | 0.62 |
| Primary diagnosis | ||||||||||
| Diabetes | 13.2 | 15.4 | 15.1 | 17.0 | 0.59 | 15.5 | 13.9 | 14.9 | 17.5 | 0.53 |
| Glomerulosclerosis | 5.8 | 9.8 | 7.1 | 10.0 | 0.05 | 9.7 | 9.4 | 7.2 | 8.9 | 0.50 |
| Hypertension | 23.4 | 18.2 | 16.6 | 10.9 | <0.001 | 19.3 | 12.7 | 17.1 | 13.8 | 0.01 |
| Polycystic kidneys | 5.9 | 5.1 | 6.2 | 7.9 | 0.42 | 8.0 | 4.5 | 6.1 | 6.6 | 0.06 |
| Graft failure | 6.1 | 5.1 | 5.0 | 7.5 | 0.24 | 3.6 | 5.1 | 5.7 | 5.5 | 0.47 |
| Other | 45.5 | 46.4 | 50.1 | 46.6 | 0.56 | 43.8 | 54.4 | 49.1 | 47.6 | 0.05 |
| Primary insurance | ||||||||||
| Medicare | 58.2 | 58.9 | 32.5 | 51.3 | <0.001 | 56.5 | 40.9 | 42.4 | 43.8 | 0.003 |
| Private | 32.5 | 34.7 | 4.8 | 6.1 | 0.33 | 38.0 | 40.1 | 40.6 | 47.5 | 0.37 |
| Medicaid | 4.8 | 5.2 | 58.2 | 38.0 | <0.001 | 3.9 | 15.7 | 15.5 | 7.7 | <0.001 |
| Other | 4.5 | 1.2 | 4.5 | 4.6 | 0.07 | 1.7 | 3.4 | 1.5 | 1.0 | 0.09 |
| Some college | 51.6 | 52.8 | 49.9 | 55.9 | 0.50 | 56.8 | 56.1 | 54.9 | 55.1 | 0.98 |
| Pre-emptive listing | 35.4 | 37.0 | 29.8 | 31.4 | 0.08 | 38.6 | 28.5 | 30.5 | 28.0 | 0.01 |
Unless otherwise noted, values are percentages. Patient characteristics of all transplant recipients who underwent transplantation within Tennessee (TN), North Carolina (NC), Pennsylvania (PA), Wisconsin (WI), Florida (FL), California (CA), New York (NY), and Ohio (OH) are listed for the study period (1987–2009). In 1991 and 1992, respectively, TN and FL implemented the Statewide Sharing variance. The P value illustrates the magnitude of difference between the states for a specific patient characteristic. DSA, donor service area.
A chi-squared test was used to calculate P values to determine significant differences across the four respective states.
Table 2.
The geographic allocation disparity before and after the implementation of the Statewide Sharing variance in Tennessee and Florida—a comparison with other two and four DSA states
| No. of DSAs/State | Transplant Rate | Waiting Time (yr) | Time on Dialysis (yr) | 5-Year Graft Survival (%)a | ||||
|---|---|---|---|---|---|---|---|---|
| Before | Recently after | Before | Recently after | Before | Recently after | Before | Recently after | |
| TN | ||||||||
| 1 | 4.63 | 6.63 | 0.69 | 1.42 | 1.69 | 2.83 | 34.5 | 81.8b |
| 2 | 3.94 | 5.61 | 0.47 | 1.47 | 2.62 | 2.93 | 38.8 | 83.4b |
| Disparity ratio | 2.02 | 1.19b | 1.74 | 1.11b | 1.58 | 1.09b | 1.12 | 1.02 |
| NC | ||||||||
| 1 | 3.68 | 4.88 | 0.78 | 1.20 | 1.38 | 3.08 | 28.7 | 89.3 |
| 2 | 5.19 | 8.60 | 0.58 | 2.82 | 1.74 | 4.41 | 31.6 | 82.0b |
| Disparity ratio | 1.38 | 2.00 | 1.59 | 2.49 | 1.32 | 1.45 | 1.10 | 1.09 |
| PA | ||||||||
| 1 | 3.65 | 7.79 | 0.79 | 1.71 | 2.02 | 3.16 | 43.3 | 78.8b |
| 2 | 2.69 | 4.82 | 0.47 | 1.11 | 1.48 | 2.64 | 33.2 | 71.8b |
| Disparity ratio | 1.54 | 1.66 | 1.64 | 1.53 | 1.39 | 1.20 | 1.31 | 1.10 |
| WI | ||||||||
| 1 | 3.18 | 7.27 | 0.47 | 2.01 | 1.28 | 3.11 | 30.1 | 89.7 |
| 2 | 4.61 | 3.54 | 0.47 | 0.83 | 1.01 | 2.09 | 43.3 | 81.8 |
| Disparity ratio | 1.73 | 2.04 | 1.19 | 2.46b | 1.40 | 1.50 | 1.44 | 1.10 |
| FL | ||||||||
| 1 | 2.87 | 4.50 | 0.44 | 1.15 | 1.40 | 2.82 | 29.5 | 85.0b |
| 2 | 2.83 | 6.11 | 0.20 | 1.26 | 1.82 | 3.24 | 38.2 | 87.6b |
| 3 | 4.13 | 5.51 | 0.74 | 1.39 | 2.35 | 3.18 | 38.1 | 84.4b |
| 4 | 1.98 | 4.37 | 0.23 | 1.22 | 1.63 | 2.90 | 36.9 | 87.4b |
| Disparity ratio | 2.01 | 1.44b | 3.86 | 1.45b | 1.89 | 1.25b | 1.29 | 1.04 |
| CA | ||||||||
| 1 | 5.18 | 22.06 | 0.43 | 2.70 | 1.42 | 5.00 | 39.5 | 88.0b |
| 2 | 4.97 | 9.16 | 0.18 | 1.62 | 1.16 | 3.94 | 29.6 | 88.6 |
| 3 | 3.76 | 11.4 | 0.65 | 2.94 | 1.87 | 6.17 | 44.4 | 86.6b |
| 4 | 3.16 | 7.21 | 0.65 | 2.44 | 2.03 | 3.88 | 38.2 | 82.5b |
| Disparity ratio | 2.01 | 3.16 | 4.52 | 2.13 | 1.90 | 1.60 | 1.50 | 1.07 |
| NY | ||||||||
| 1 | 6.81 | 5.66 | 0.45 | 1.44 | 1.41 | 2.51 | 60.5 | 91.4 |
| 2 | 3.35 | 10.15 | 0.71 | 2.89 | 2.04 | 4.47 | 33.9 | 82.2 |
| 3 | 6.62 | 9.50 | 0.98 | 2.45 | 2.95 | 5.64 | 38.8 | 76.5b |
| 4 | 4.18 | 7.40 | 0.78 | 2.26 | 1.60 | 3.16 | 42.9 | 80.3 |
| Disparity ratio | 2.49 | 1.99 | 3.28 | 2.17 | 2.50 | 2.27 | 1.78 | 1.19 |
| OH | ||||||||
| 1 | 6.35 | 10.68 | 1.05 | 2.80 | 2.06 | 4.55 | 33.4 | 83.9 |
| 2 | 5.62 | 4.01 | 0.51 | 1.02 | 1.44 | 2.71 | 26.7 | 76.0b |
| 3 | 7.37 | 5.00 | 0.34 | 1.48 | 1.18 | 2.90 | 30.6 | 78.9b |
| 4 | 3.48 | 9.06 | 0.35 | 1.83 | 1.75 | 3.40 | 36.9 | 82.5 |
| Disparity ratio | 2.76 | 2.91 | 4.50 | 3.07 | 1.83 | 1.71 | 1.38 | 1.10 |
| TX | ||||||||
| 1 | 2.12 | 6.15 | 0.25 | 1.50 | 1.44 | 3.19 | 31.9 | 80.3 |
| 2 | 2.73 | 19.9 | 0.35 | 3.42 | 1.44 | 5.24 | 44.0 | 82.6b |
| 3 | 2.51 | 5.46 | 0.30 | 1.46 | 1.78 | 3.28 | 37.9 | 86.4 |
| Disparity ratio | 1.37 | 3.51b | 2.24 | 2.49 | 1.32 | 1.67 | 1.38 | 1.08 |
The change of geographic allocation disparity over time, comparing a 5-year interval prior (1987–1991) to implementation of the Statewide Sharing variance with a recent 5-year time-period (2005–2009). The Statewide Sharing variance was implemented in Florida and Tennessee in 1991 and 1992. The extent of the existing disparity between donor service areas (DSAs) within a state is measured by the disparity ratio. A disparity ratio that equals 1.0 suggests that no geographic disparity exists, while geographic disparity between DSAs increases as the disparity ratio rises above 1.0. Transplant rate calculated as the mean number of transplant candidates per transplant in the period. Waiting time calculated as the median waiting time to transplantation in the period. Time on dialysis is calculated as the median cumulative dialysis time before transplantation in the period. “Before” denotes 1987–1991; “recently after” refers to 2005–2009. DSA, donor service area; TN, Tennessee; NC, North Carolina; PA, Pennsylvania; WI, Wisconsin; FL, Florida; CA, California; NY, New York; OH, Ohio; TX, Texas.
Five-year graft survival significance is adjusted for age, sex, race, panel reactive antibody, diagnosis, insurance, and educational attainment.
Significant difference in disparity ratio between before and recently after implementation of Statewide Sharing variance (P<0.05).
Allocation Disparity Ratio.
The magnitude of change for each geographic allocation disparity indicator before and after Statewide Sharing within a state was calculated as an allocation disparity ratio. The ratio is calculated between the highest and the lowest values for each disparity indicator among the DSAs in a given state. An allocation disparity ratio of 1.0 suggests that there is no geographic disparity between the DSAs within the state, while a rising disparity ratio (>1.0) indicates more geographic disparity.
Time-series models comparing changes in the allocation disparity ratios among the states pre- and post-Statewide Sharing were estimated for Tennessee and Florida. The following equation presents the statistical model:
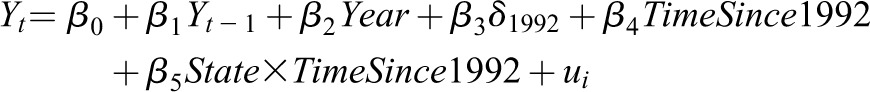 |
 represents the allocation disparity ratio in year t,
represents the allocation disparity ratio in year t,  is the disparity indicator in the previous year,
is the disparity indicator in the previous year,  is a binary indicator for the year 1992, and
is a binary indicator for the year 1992, and  is the number of years elapsed since 1992.
is the number of years elapsed since 1992.  is the interaction of a binary indicator for either Tennessee or Florida and
is the interaction of a binary indicator for either Tennessee or Florida and  . Finally,
. Finally,  is the random effect specific to state i. A significant, negative coefficient (β5) indicates that Tennessee or Florida has had annually smaller increases (or greater decreases) in disparity relative to the mean since 1992 (variance enactment).
is the random effect specific to state i. A significant, negative coefficient (β5) indicates that Tennessee or Florida has had annually smaller increases (or greater decreases) in disparity relative to the mean since 1992 (variance enactment).
CIT.
The change in mean CIT for kidneys procured and used for kidney transplantation anywhere in the United States over time was calculated and used as a proxy for allocation efficiency, with shorter CIT suggesting greater allocation efficiency.
Results
The following numbers of patients were included: 92,711 in the primary cohort, 68,365 in the KDRI-controlled cohort, and 77,003 in the additional exclusions cohort. Table 1 presents demographic and patient characteristics of the primary cohort by state. Supplemental Tables A1 and A2 provide the number of patients in each DSA for all cohorts and a detailed outline of the KDRI-controlled cohort. Kidney transplant recipients in Tennessee were less likely to be older than age 65 years, Hispanic, or Asian; less likely to be experiencing glomerulosclerosis; and more likely to experience hypertension compared with transplant recipients in North Carolina, Pennsylvania, and Wisconsin. Transplant recipients in Florida were significantly more likely to have hypertension, to be Medicare insured (but not Medicaid insured), and be listed preemptively for transplant than recipients in California, New York, and Ohio.
Geographic Allocation Disparity Measured by Indicator Ratios for the Primary Cohort
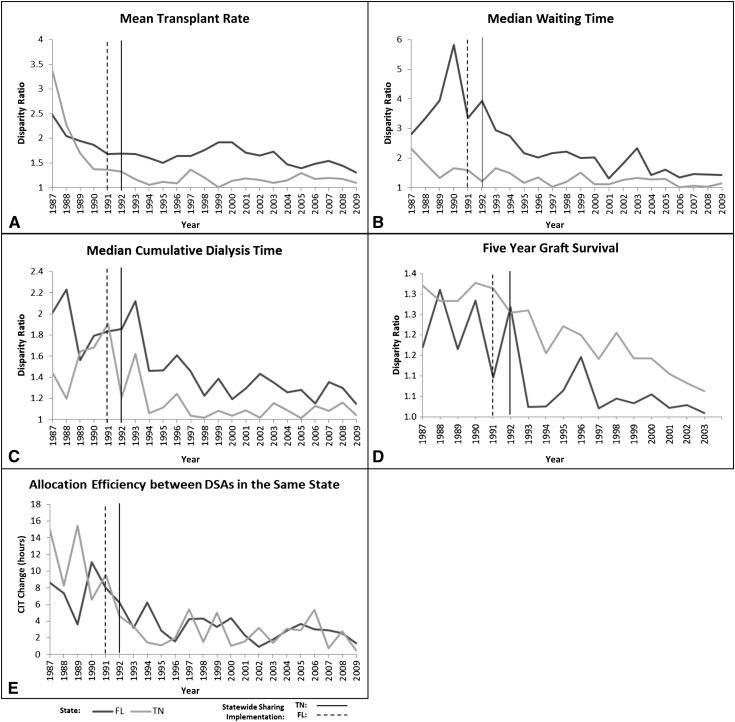
Figure 1 demonstrates change in geographic disparity between DSA within one state, measured by the disparity ratio between 1987 and 2009. In Tennessee, the disparity ratio dropped from 3.39 in 1987 to 1.10 in 2009 for transplant rates, from 2.31 to 1.15 for waiting time, from 1.45 to 1.04 for dialysis time, and from 1.22 to 1.03 for 5-year graft survival. In addition, the average difference in CIT between kidneys transplanted locally and those transplanted within the state dropped from 15.0 hours in 1987 to 0.49 hours in 2009. A drop in disparity for all disparity indicators by 1995 was sustained thereafter. In Florida, the implementation of Statewide Sharing resulted in the more gradual decrease: from 2.48 to 1.30 for transplant rates, from 2.81 to 1.42 for waiting time, from 2.01 to 1.15 for dialysis time, and from 1.29 to 1.04 for 5-year graft survival. The average difference in CIT between kidneys transplanted locally and those transplanted within the state dropped from 8.62 hours in 1987 to 1.36 hours in 2009. Since 2005, the decrease in allocation disparity ratios was sustained in Florida (Figure 1).
Figure 1.
Improvement of geographic allocation disparity in Tennessee and Florida over time between 1987 and 2009. Florida (FL) and Tennessee (TN) implemented Statewide Sharing variances in 1991 and 1992, respectively (dotted and solid vertical line). Geographic disparity is measured for four disparity indicators (transplant rate, waiting time, dialysis time, and 5-year graft survival) using an allocation disparity ratio. Geographic disparity improves as the allocation disparity ratio nears 1.0. A disparity ratio of 1.0 suggests that there is no geographic disparity between DSAs within a state. Panel E illustrates allocation efficiency by demonstrating the drop in cold ischemic time (CIT) difference between locally transplanted kidneys and those transplanted statewide. DSA, donor service area.
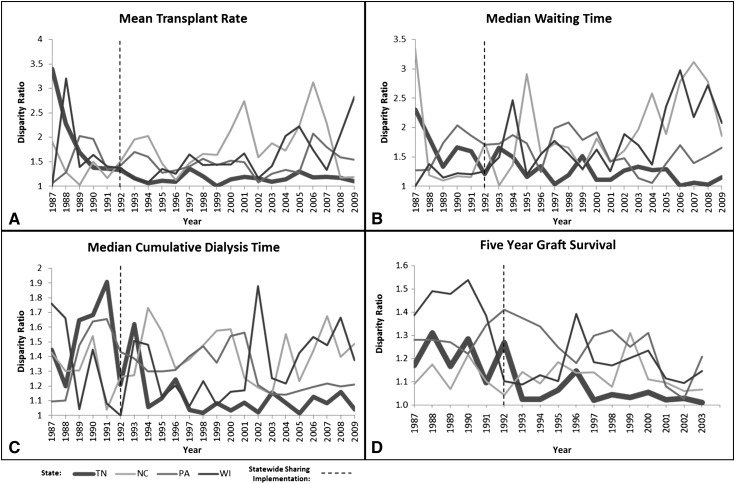
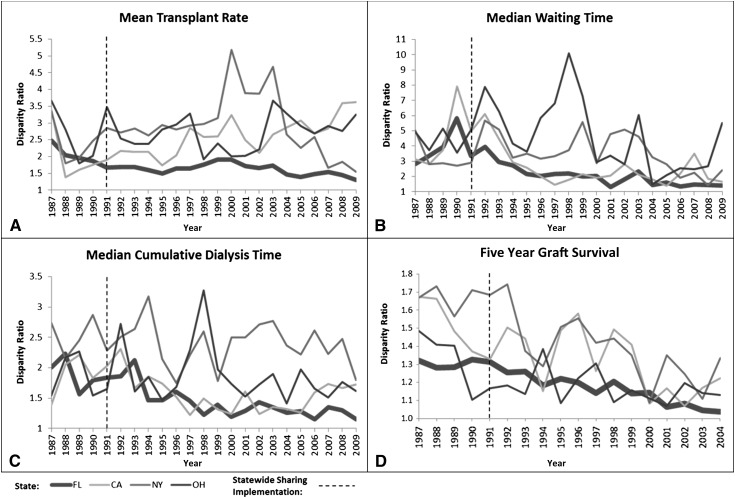
After implementation of Statewide Sharing, Tennessee and Florida had significantly less variation in the disparity ratios (see Figure 2 for Tennessee compared with North Carolina, Pennsylvania and Wisconsin and Figure 3 for Florida compared with California, New York, and Ohio). States that did not implement Statewide Sharing had limited decrease or even an increase in their disparity ratios over time.
Figure 2.
Changes of geographic allocation disparity in states with two DSAs between 1987–2009. Tennessee (TN) implemented Statewide Sharing variance in 1992. North Carolina (NC), Pennsylvania (PA), and Wisconsin (WI) have not implemented Statewide Sharing variance. Geographic disparity is measured for four disparity indicators (transplant rate, waiting time, dialysis time, and 5-year graft survival) using an allocation disparity ratio. Geographic disparity improves as the allocation disparity ratio nears 1.0. A disparity ratio of 1.0 suggests that there is no geographic disparity between DSAs within a state.
Figure 3.
Changes of geographic allocation disparity in states with four DSAs between 1987–2009. Florida (FL) adopted Statewide Sharing variance in 1991. California (CA), New York (NY), and Ohio (OH) have not implemented Statewide Sharing variance. Geographic disparity is measured for four disparity indicators (transplant rate, waiting time, dialysis time, and 5-year graft survival) using an allocation disparity ratio. Geographic disparity improves as the allocation disparity ratio nears 1.0. A disparity ratio of 1.0 suggests that there is no geographic disparity between DSAs within a state.
Table 2 illustrates a comparative analysis of the geographic disparity before (1987–1991) and recently after (2005–2009) implementation of Statewide Sharing for each disparity indicator for transplant recipients in the primary cohort. Table 3 displays annual changes in allocation disparity ratios after Statewide Sharing (1992–2009) that were estimated by using the preceding equation. The findings were as follows.
Table 3.
Geographic allocation disparity: annual changes in disparity ratios due to implementation of Statewide Sharing variance
| State | Transplant Rate | Waiting Time | Time on Dialysis | Five-Year Graft Survivala |
|---|---|---|---|---|
| TN | −0.003b (−0.028 to 0.022) | −0.019b (−0.043 to 0.005) | −0.012b (−0.024 to 0.000) | −0.012 (−0.022 to −0.002) |
| Baselinec | 0.031 (Reference) | 0.030 (Reference) | 0.008 (Reference) | −0.003 (Reference) |
| FL | −0.031b (−0.064 to 0.002) | −0.117 (−0.193 to −0.041) | −0.030b (−0.052 to −0.008) | −0.017 (−0.031 to −0.003) |
| Baselined | 0.016 (Reference) | −0.057 (Reference) | −0.006 (Reference) | −0.010 (Reference) |
95% confidence intervals in parentheses. The annualized change of geographic allocation disparity ratios since enactment of Statewide Sharing variance (1992–2009) was calculated via time series regression. The coefficients and SE of the annual changes in Tennessee and Florida are provided (β2+β4+β5). The baseline denotes the mean change of geographic allocation disparity ratios for other comparable states (β2+β4). A negative annual change indicates an improvement in disparity since 1992. A positive annual change indicates worsening disparity since 1992. Transplant rate calculated as the mean number of transplant candidates per transplant in the period. Waiting time calculated as the median waiting time to transplantation in the period. Time on dialysis is calculated as the median cumulative dialysis time prior to transplantation in the period.
Five-year graft survival significance is adjusted for age, sex, race, panel reactive antibody, diagnosis, insurance, and educational attainment.
Significantly different annual change of geographic disparity from baseline (P<0.05).
Baseline includes North Carolina, Pennsylvania, and Wisconsin.
Baseline includes California, New York, Ohio, and Texas.
Transplant Rate.
The disparity ratio of transplant rates developed to 1.19 in Tennessee recent Statewide Sharing compared with 1.99 in North Carolina, 1.66 in Pennsylvania and 2.04 in Wisconsin (P<0.05). Only Tennessee experienced a decrease in the disparity ratio, which was sustained over time. Similarly, the disparity ratio developed to 1.43 in Florida recent Statewide Sharing compared with 3.16 in California, 1.99 in New York, and 2.91 in Ohio. After implementation of Statewide Sharing, the change in transplant rate disparity, β5, was statistically significant (P<0.05) and negative for both Tennessee and Florida, indicating that both states had a decrease in disparity relative to other states since implementation of the variance.
Waiting Time.
The disparity ratio of waiting time at transplantation developed to 1.11 in Tennessee, 2.49 in North Carolina, 1.53 in Pennsylvania, and 2.46 in Wisconsin. All states except Pennsylvania had a significant annual change for the waiting time disparity ratio, with only Tennessee experiencing improved disparity over time. Similarly, the disparity ratio developed to 1.45 in Florida, 2.13 in California, 2.17 in New York, and 3.07 in Ohio. After Statewide Sharing, the change in waiting time disparity, β5, was statistically significant (P<0.05) and negative for Tennessee.
Time on Dialysis.
The disparity ratio of cumulative time on dialysis before transplantation developed to 1.09 in Tennessee, 1.45 in North Carolina, 1.19 in Pennsylvania, and 1.50 in Wisconsin. Similarly, the disparity ratio developed to 1.25 in Florida, 1.60 in California, 2.27 in NY, and 1.71 in Ohio. After Statewide Sharing, β5 was statistically significant (P<0.05) and negative for both Tennessee and Florida.
5-Year Graft Survival.
The disparity ratio of 5-year graft survival developed to 1.03 in Tennessee, 1.07 in North Carolina, 1.14 in Pennsylvania, and 1.15 in Wisconsin. The disparity ratio developed to 1.04 in Florida compared with 1.09 in California, 1.21 in New York, and 1.13 in Ohio. After Statewide Sharing, neither Tennessee nor Florida experienced statistically significant decreases in disparity relative to other states (β5<0; P>0.05).
CIT.
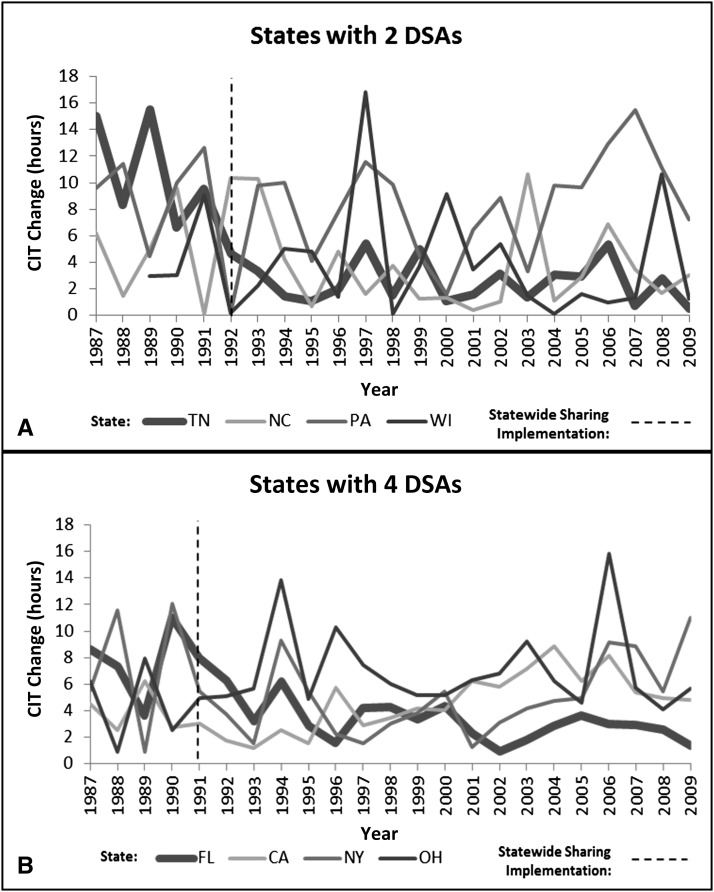
CITs, as a proxy for allocation efficiency, are shown in Table 4 for each state in the time before and recently after implementation of Statewide Sharing (2005–2009). The CIT for Tennessee decreased by 7.5 hours, increased by 0.7 hour in North Carolina and 3.3 hours in Pennsylvania, and decreased by 1.1 hours in Wisconsin. It was reduced by 5.0 hours in Florida, increased by 3.9 hours in California, increased by 0.8 hour in New York, and increased by 2.7 in Ohio. Texas had a 1.7-hour reduction in CIT. Figure 4 illustrates the difference in CIT reduction between kidneys transplanted locally and those transplanted within their state. CIT differences in Tennessee and Florida dropped after implementation of Statewide Sharing and were significantly less than those in other states by 2009.
Table 4.
Changes in cold ischemic time and type of allocation (local, state, regional, national) before and after Statewide Sharing
| State | Local | State | Regionala | National | CIT: Change from “Before” to “Recently after” (h) | ||||
|---|---|---|---|---|---|---|---|---|---|
| Allocation (%) | Mean CIT (h) | Allocation (%) | Mean CIT (h) | Allocation (%) | Mean CIT (h) | Allocation (%) | Mean CIT (h) | ||
| TN | |||||||||
| Before | 59.1 | 18.5 | 2.2 | 28.5 | 12.8 | 25.9 | 25.9 | 29.4 | 7.5 |
| Recently after | 56.7 | 16.1 | 13.1 | 18.6 | 8.3 | 26.6 | 21.8 | 24.8 | |
| NC | |||||||||
| Before | 57.6 | 20.4 | 1.8 | 23.3 | 16.4 | 24.8 | 24.2 | 31.6 | −0.7 |
| Recently after | 69.7 | 20.8 | 3.1 | 24.4 | 4.8 | 21.5 | 22.4 | 24.5 | |
| PA | |||||||||
| Before | 85.5 | 25.4 | 2.2 | 33.4 | 2.9 | 30.1 | 9.3 | 31.5 | −3.3 |
| Recently after | 79.2 | 16.4 | 1.6 | 27.6 | 4.4 | 24.8 | 14.7 | 25.1 | |
| WI | |||||||||
| Before | 86.9 | 26.0 | 1.5 | 30.3 | 0.7 | 35.1 | 10.9 | 33.2 | 1.1 |
| Recently after | 82.9 | 14.5 | 0.8 | 17.5 | 3.9 | 21.7 | 12.5 | 24.8 | |
| FL | |||||||||
| Before | 52.9 | 22.7 | 6.7 | 30.4 | 16.4 | 33.3 | 24.1 | 35.6 | 5.0 |
| Recently after | 70.6 | 20.3 | 6.8 | 23.0 | 2.7 | 23.8 | 19.9 | 25.3 | |
| CA | |||||||||
| Before | 76.1 | 27.1 | 6.1 | 29.1 | 12.0 | 21.0 | 5.8 | 32.4 | −3.9 |
| Recently after | 73.7 | 14.3 | 5.5 | 20.2 | 3.1 | 17.5 | 17.6 | 26.3 | |
| NY | |||||||||
| Before | 86.8 | 25.5 | 3.1 | 32.6 | 0.7 | 23.8 | 9.4 | 32.2 | −0.8 |
| Recently after | 77.1 | 16.9 | 4.4 | 24.7 | 0.0 | – | 18.5 | 24.1 | |
| OH | |||||||||
| Before | 84.0 | 22.4 | 2.2 | 27.0 | 3.4 | 27.4 | 10.4 | 29.8 | −2.7 |
| Recently after | 70.3 | 13.6 | 3.1 | 20.8 | 3.3 | 21.4 | 23.3 | 24.1 | |
| TX | |||||||||
| Before | 88.0 | 20.7 | 4.0 | 26.5 | 0.5 | 26.1 | 7.4 | 29.6 | 1.7 |
| Recently after | 74.4 | 18.0 | 4.6 | 22.2 | 0.7 | 16.4 | 20.4 | 24.8 | |
Florida and Tennessee implemented Statewide Sharing in 1991 and 1992, respectively. To clarify the distribution of kidneys used, the percentage distributed locally, by state, regionally, and nationally are provided also. Negative CIT changes indicate an increase in CIT over time. Allocation: percentage of kidneys procured by the donor service area, transplanted locally, statewide, regionally, and nationally. CIT, cold ischemic time; TN, Tennessee; NC, North Carolina; PA, Pennsylvania; WI, Wisconsin; FL, Florida; CA, California; NY OH, Ohio; TX, Texas.
Regional allocation includes all kidneys allocated to the United Network of Organ Sharing region of procurement, excluding kidneys allocated within the state of procurement.
Figure 4.
Allocation efficiency between DSAs within states with two and four DSAs (1987–2009). Florida (FL) and Tennessee (TN) adopted Statewide Sharing variance in 1991 and 1992, respectively. Tennessee and Florida are compared with states that entail the same number of DSAs that did not implement Statewide Sharing. Allocation efficiency is measured as the additional time required to allocate a deceased-donor kidney for transplantation within the state of procurement when local allocation is not possible. CA, California; NC, North Carolina; NY, New York; OH, Ohio; PA, Pennsylvania; WI, Wisconsin.
Kidney Retention
Kidney retention is summarized in Table 4. The percentage of kidneys procured and retained in Tennessee (i.e., local and state allocations) increased after implementation of Statewide Sharing from 61.3% to 69.8%. The percentage of kidneys procured within Tennessee and shared outside of Tennessee (i.e., regional and national allocations) after implementation was 30.1%, compared with the other two-DSA states, where it was 27.2% in North Carolina, 19.1% in Pennsylvania, and 16.4% in Wisconsin. The percentage of kidneys procured in Tennessee but transplanted outside Tennessee remained the highest compared with the other two DSA states.
In Florida, kidneys procured in one of the four DSAs within Florida, transplanted outside of the procuring DSA but retained within Florida (i.e., state allocations) was stable (6.7% versus 6.8%) while local allocation within the procuring DSA increased significantly, from 52.9% to 70.6%. The percentage procured and retained in Florida (i.e., local and state allocations) increased after implementation of Statewide Sharing from 59.6% to 77.4%. The percentage procured within Florida and shared outside of Florida after implementation was 22.6%, compared with the other four-DSA states, where it was 20.7% in California, 18.5% in New York, and 26.6% in Ohio.
States with Three DSAs
Only Texas entails three DSAs. Texas did not implement the Statewide Sharing and over time the allocation disparity between the DSAs within Texas increased for transplant rate, waiting time to transplantation, and time on dialysis (Tables 2 and 3), but the difference in CIT between the three DSAs decreased by 1.7 hours (Table 4). Over time, statewide retention of procured kidneys declined from 92.1% to 79.0%.
Adjusted Cohort Analysis
The geographic disparity is illustrated by disparity ratios in Table 5 for the KDRI Controlled and Primary cohorts. For the KDRI controlled cohort, waiting time disparity improved significantly in Tennessee (P<0.05) relative to other states, and disparity in time on dialysis improved for both Tennessee and Florida relative to other states (P<0.05). Additional analysis adjusting for panel reactive antibodies, HLA (including zero HLA mismatch), and payback kidneys did not alter the findings (not reported).
Table 5.
Geographic allocation disparity by cohort: annual changes in disparity ratios due to implementation of Statewide Sharing variance
| State | Transplant Rate | Waiting Time | Time on Dialysis | Five-Year Graft Survivala |
|---|---|---|---|---|
| Primary cohortb | ||||
| TN | −0.003c (−0.028 to 0.022) | −0.019c (−0.043 to 0.005) | −0.012c (−0.024 to 0.000) | −0.012 (−0.022 to −0.002) |
| Baselined | 0.031 (Reference) | 0.030 (Reference) | 0.008 (Reference) | −0.003 (Reference) |
| FL | −0.031c (−0.064 to 0.002) | −0.117 (−0.193 to −0.041) | −0.030c (−0.052 to -0.008) | −0.017 (−0.031 to −0.003) |
| Baselinee | 0.016 (Reference) | −0.057 (Reference) | −0.006 (Reference) | −0.010 (Reference) |
| Controlled-KDRI cohortf | ||||
| TN | −0.019 (−0.041 to 0.003) | −0.017c (−0.048 to 0.014) | −0.010c (−0.024 to 0.004) | −0.021 (−0.037 to −0.005) |
| Baselined | 0.002 (Reference) | 0.039 (Reference) | 0.006 (Reference) | −0.008 (Reference) |
| FL | −0.114 (−0.187 to −0.041) | −0.144 (−0.254 to −0.034) | −0.046c (−0.071 to −0.021) | −0.031 (−0.053 to −0.009) |
| Baselinee | −0.067 (Reference) | −0.059 (Reference) | −0.015 (Reference) | −0.021 (Reference) |
95% confidence intervals in parentheses. The annualized change of geographic allocation disparity ratios since enactment of Statewide Sharing (1992–2009) was calculated via time series regression. The coefficients and standard errors of the annual changes in Tennessee and Florida are provided (β2+β4+β5). The baseline denotes the mean change of geographic allocation disparity ratios for other comparable states (β2+β4). A negative annual change indicates an improvement in disparity since 1992. A positive annual change indicates worsening disparity since 1992. Transplant rate calculated as the mean number of transplant candidates per transplant in the period. Waiting time calculated as the median waiting time to transplantation in the period. Time on dialysis is calculated as the median cumulative dialysis time before transplantation in the period. TN, Tennessee; FL, Florida; KDRI, Kidney Donor Risk Index.
Five-year graft survival significance is adjusted for age, sex, race, panel reactive antibody, diagnosis, insurance, and educational attainment.
Primary: All adult deceased-donor kidney transplant recipients.
Significantly different annual change of geographic disparity from baseline (P<0.05).
Baseline includes North Carolina, Pennsylvania, and Wisconsin.
Baseline includes California, New York, Ohio, and Texas.
Controlled analyses for kidney quality.
Discussion
The two states that adopted the Statewide Sharing variance experienced significant reduction in allocation disparity while disparities in states that followed the national allocation policy worsened or showed inconsistent improvement between 1987 and 2009. We used five disparity indicators described in the transplant literature to assess geographic disparity (13–17). While each indicator is compelling, we considered them all. Waiting time to transplant is the most commonly cited metric of geographic disparity (4,14,15), but transplant rates were proposed by the Institute of Medicine as a superior metric (13). If little disparity existed between the DSAs within a state, the disparity indicators would be similar across all DSAs; however, our data demonstrate otherwise.
Our study shows that the only sustained reductions in allocation disparities occurred in Tennessee and Florida, where kidneys not used within the procuring DSA were first allocated to other DSAs within the state before being allocated regionally and, then, nationally (12). The strength of this analysis is that actual observations rather than predictive models were used.
After implementation of Statewide Sharing, Tennessee and Florida in-state kidney retention increased by 8.5% and 17.8%, respectively. More kidneys procured in Tennessee were allocated from the procuring DSA to a nonprocuring DSA in Tennessee for transplantation. In contrast, in Florida, more procured kidneys were transplanted locally within the DSA. The increase in retention of procured kidneys within Tennessee and Florida reduced the number of kidneys eligible for out-of-state kidney allocation and may raise concern that the implementation of Statewide Sharing reduced kidney retention within the procuring DSA (18). However, Tennessee and Florida had the highest and second highest percentage of out-of-state kidney allocation compared with other two and four DSA states. Hence, Statewide Sharing did not disproportionately affect available kidneys to the other states.
Although our data demonstrate reduction in geographic allocation disparities, the reasons remain speculative. One might be the improved coordination of organ allocation between the DSAs within a state, as inter-DSA relationships are typically closer. The reduction in the initial allocation disparity was faster in Tennessee, which entails only two DSAs compared with Florida, which has four DSAs. The development of close relationships and streamlining of the allocation process between two DSAs probably occurs rapidly with fewer DSAs. Thus, further understanding of the effect of Statewide Sharing on the behavior of DSAs is necessary. Tennessee and Florida not only reduced the difference in CIT for locally versus statewide transplanted kidneys within their states but also significantly decreased CIT over time; in comparison, the other states increased their CIT over time or reduced their CIT to a much lesser extent. This is noteworthy because the introduction of statewide allocation before the regional and national allocation might introduce inefficiency and, therefore, might increase CIT. Our data, however, demonstrate that the implementation of Statewide Sharing did not occur at the cost of allocation efficiency.
It is also important to note that Tennessee and Florida are markedly different, beyond the fact that one state has only two DSAs and the other has four. Recipient demographic characteristics were also found to vary considerably across the states. This supports that the effect of Statewide Sharing on allocation disparity is independent of state and patient characteristics. In addition, recently presented patient-level analyses have demonstrated that the implementation of Statewide Sharing increased the rate of transplantation for highly sensitized patients (19,20).
Other attempts have been made to resolve the geographic disparities, in response to the 1998 Department of Health and Human Services Final Rule mandating geographic allocation equality (6–11). However, Statewide Sharing is the only UNOS policy variance for which actual evidence supports its ability to reduce geographic disparity. These findings are timely because UNOS engages in discussions to restructure and reorganize the kidney allocation system with a goal of reducing geographic disparities. Instead of more sweeping changes currently proposed to address geographic disparities (7–11), local changes, such as Statewide Sharing, need to be considered, especially because more extensive changes, such as redefining regions, may have unintended consequences. The authors do not suggest that Statewide Sharing is a solution to the national problem of geographic disparity but rather that small changes to kidney allocation can decrease the geographic disparity that UNOS is poised to resolve. These results and experiential evidence should supplement any policy discussion, especially because UNOS has tasked organ-specific allocation committees to define and develop metrics and strategies to reduce geographic disparities in organ transplantation, scrutinizing existing geographic disparities in kidney allocation (21).
Our study has some limitations. First, this study investigated geographic disparity from a DSA perspective. Future study may extend this analysis to study the effect of the variance on different patient blood types or subgroups. Second, overall graft survival has improved significantly during the study period, making inferences between statewide sharing and improved graft survival challenging. However, our adjusted analyses for kidney quality (KDRI), panel reactive antibodies, and HLA still support the findings that Statewide Sharing can successfully alleviate the allocation disparities among DSAs within a state.
One may propose eliminating statewide disparity by having a single DSA in multiple DSA states. While plausible, this strategy does not resolve disparities across states. Sharing arrangements between DSAs improved the existing geographic disparity over time, and such arrangements might not have to be limited to states only.
Finally, the current study focuses only on two states (Tennessee, Florida). We have performed additional analyses (not shown) suggesting that preferred partnerships among a small number of DSAs in close geographic proximity across the nation can alleviate existing geographic disparities between DSAs, without loss in transplant volume or quality or loss of locally procured organs (22).
Our study provides compelling evidence for supporting Statewide Sharing as a model to alleviate geographic allocation disparity. Small and incremental changes to the current kidney allocation system ought to be seriously considered as a means to reduce geographic allocation disparity between DSAs in the United States.
Disclosures
The authors are not part of a state with Statewide Sharing.
Supplementary Material
Acknowledgments
The authors would like to thank the members of the Northwestern University Transplant Outcomes Research Collaborative (NUTORC) and four anonymous reviewers for their opinions and suggestions for this work.
This work is funded by National Science Foundation award CMMI-1131568, Agency for Healthcare Research and Quality Health Services Research Dissertation Award R36 HS021078-01, and NUTORC.
The content of this work is the responsibility of the authors alone and does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products, or organizations imply endorsement by the US Government.
Footnotes
Published online ahead of print. Publication date available at www.cjasn.org.
This article contains supplemental material online at http://cjasn.asnjournals.org/lookup/suppl/doi:10.2215/CJN.05350513/-/DCSupplemental.
References
- 1.Organ Procurement and Transplantation Network: US transplants performed: January 1, 1988–August 31, 2012, November 14, 2012. Available at: http://optn.transplant.hrsa.gov/latestData/step2.asp? Accessed November 20, 2012
- 2.Organ Procurement and Transplantation Network: Current U.S. Waiting List. November 14, 2012. Available at: http://optn.transplant.hrsa.gov/latestData/step2.asp? Accessed November 20, 2012
- 3.Davis AE, Mehrotra S, McElroy LM, Friedewald JJ, Skaro AI, Lapin B, Kang R, Holl JL, Abecassis MM, Ladner DP: The extent and predictors of waiting time geographic disparity in kidney transplantation in the United States [published online ahead of print December 27, 2013]. Transplantation 10.1097/01.tp.0000438623.89310.dc [DOI] [PubMed] [Google Scholar]
- 4.Davis A, Mehrotra S, Friedewald J, Skaro A, McElroy L, Kang R, Wang E, Holl J, Abecassis M, Ladner D: The causes and consequences of kidney transplantation waiting time inequity across the United States [abstract]. Presented at American Society of Transplant Surgeons Winter Symposium 2013, Miami Beach, FL, January 31–February 3, 2013 [Google Scholar]
- 5.Davis A, Mehrotra S, Ladner D, Kilambi V, Friedewald J: Has geographic inequity in kidney transplantation changed since the final rule, technical report, Evanston, IL, Department of Industrial Engineering and Management Sciences, Northwestern University, 2013 [Google Scholar]
- 6.USDepartment of Health and Human Services : Organ Procurement and Transplantation Network, Final Rule (40 CFR Part 121). Fed Regist 63: 16296–16338, 1998 [PubMed] [Google Scholar]
- 7.Davis A, Mehrotra S, Friedewald J, Ladner D: Characteristics of a Simulation Model of the National Kidney Transplantation System. In: Proceedings of the 2013 Winter Simulation Conference, edited by Pasupathy R, Kim S-H, Tolk A, Hill R, Kuhl ME. Piscataway, NJ, Institute of Electrical and Electronics Engineers, 2013, pp 2320–2329 [Google Scholar]
- 8.OPTN/UNOS Kidney Transplantation Committee: Report to the Board of Directors. June 2011. Available at: http://optn.transplant.hrsa.gov/CommitteeReports/board_main_KidneyTransplantationCommittee_7_1_2011_10_38.pdf Accessed November 23, 2012
- 9.Stahl JE, Kong N, Shechter SM, Schaefer AJ, Roberts MS: A methodological framework for optimally reorganizing liver transplant regions. Med Decis Making 25: 35–46, 2005 [DOI] [PubMed] [Google Scholar]
- 10.Kong N, Schaefer AJ, Hunsaker B, Roberts MS: Maximizing the efficiency of the US liver allocation systems through region design. Manage Sci 2010 [Google Scholar]
- 11.Gentry S, Axelrod D, Dzebiaahvili N, Lentine K, Schnitzler M, Segev D: Designing geographic allocation regions for equitable access to liver transplant. Presented at INFORMS Healthcare 2011, Montreal, Quebec, Canada; June 20–22, 2011 [Google Scholar]
- 12.US Department of Health and Human Services, Organ Procurement and Transplant Network: Catalogue of all current OPTN member variances. April 2010
- 13.Institute of Medicine : Organ Procurement and Transplantation: Assessing Current Policies and the Potential Impact of the DHHS Final Rule, Washington, DC, National Academy Press, 1999 [PubMed] [Google Scholar]
- 14.Mathur AK, Ashby VB, Sands RL, Wolfe RA: Geographic variation in end-stage renal disease incidence and access to deceased donor kidney allocation. Am J Transplant 10: 1069–1080 [DOI] [PubMed] [Google Scholar]
- 15.Danovitch GM, Cohen B, Smits JMA: Waiting time or wasted time? The case for using time on dialysis to determine waiting time in the allocation of cadaveric kidneys. Am J Transplant 2: 891–893, 2002 [DOI] [PubMed] [Google Scholar]
- 16.Organ Procurement and Transplantation Network: At-a-glance proposal to substantially revise the national kidney allocation system. Available at: http://optn.transplant.hrsa.gov/PublicComment/pubcommentPropSub_311.pdf Accessed November 10, 2012
- 17.Wolfe RA, McCullough KP, Schaubel DE, Kalbfleisch JD, Murray S, Stegall MD, Leichtman AB: Calculating life years from transplant (LYFT): Methods for kidney and kidney-pancreas candidates. Am J Transplant 8(4 Pt 2): 997–1011, 2008 [DOI] [PubMed] [Google Scholar]
- 18.Davis D, Wolitz R: A staff working and discussion paper: the ethics of organ allocation. The President’s Council on Bioethics. 2006. Available at: https://bioethicsarchive.georgetown.edu/pcbe/background/davispaper.html Accessed November 17, 2012
- 19.Hale DA, Moore DE, Shaffer D: Allocation inequities caused by mandatory assignment of kidneys based on BDR matching [abstract]. Presented at the American Transplant Congress 2012, Boston, MA, June 2-6, 2014 [Google Scholar]
- 20.Hale DA, Moore DE, Shaffer D: Allocation variance induced inequities of deceased donor kidney allocation [abstract]. Am J Transplant 11[Suppl S2]: 34, 2011. 21114653 [Google Scholar]
- 21.Organ Procurement and Transplantation Network: Executive summary of the minutes of the OPTN/UNOS Board of Directors Meeting. November 13, 2012. Available at: http://optn.transplant.hrsa.gov/SharedContentDocuments/ExecutiveSummary_1112.pdf Accessed May 16, 2013.
- 22.Davis A, Ladner D, Friedewald J, Mehrotra S, Daskin M, Skaro A, Abecassis M: Demonstrating geographic equity in kidney organ allocation—satisfying the final rule at last [abstract]. Presented at American Society of Nephrology Kidney Week 2011, Philadelphia, PA, November 8–13, 2011. J Am Soc Nephrol 11[Suppl S22]: 74A, 2011
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.