Abstract
This ethnography of family caregiving explored why peristomal skin complications are both common and undertreated among colorectal cancer (CRC) survivors with intestinal ostomies. We sought to identify factors that hinder or facilitate prompt detection and treatment of ostomy and skin problems. We collected data through in-depth interviews with 31 cancer survivors and their family caregivers, fieldwork, structured assessments, and medical records review. We analyzed data using qualitative theme and matrix analyses. We found that survivors who received help changing the skin barrier around their stoma had fewer obstacles to detection and treatment of peristomal skin complications. Half of the survivors received unpaid help with ostomy care. All such help came from spouses. Married couples who collaborated in ostomy care reported that having assistance in placing the ostomy appliance helped with preventing leaks, detecting skin changes, and modifying ostomy care routines. Survivors who struggled to manage ostomy care independently reported more obstacles to alleviating and seeking treatment for skin problems. Nurses who encounter CRC survivors with ostomies can improve treatment of peristomal skin problems by asking patients and caregivers about ostomy care and skin problems, examining the peristomal area, and facilitating routine checkups with a wound, ostomy and continence nurse.
Keywords: surgical stomas, family caregivers, ethnography, colorectal neoplasms, long-term survivors
Introduction
Although there are 11.4 million cancer survivors in the United States, health care providers have limited evidence and guidelines on how to assess and care for survivors who are living with long-term and late effects of cancer and its treatment (Bober et al., 2009; Maddams et al., 2009; Forman et al., 2003). Cancer survivorship experiences in old age are particularly important to document given that sixty percent of cancer survivors are over age 65, and 14% have lived for more than 20 years since their initial diagnosis (Horner et al., 2009). In this report, we focus on the specific challenges of colorectal cancer (CRC) survivors with intestinal stomas (ostomies). The proportion of CRC survivors aged 65 and over who are living with permanent ostomies is not well documented; however, patients with colon cancer are much less likely to receive a permanent ostomy than patients with rectal cancer. During the years 2002-2004, 52% of rectal cancer patients in the U.S. received permanent ostomies as a result of their proctectomy surgery (Ricciardi et al., 2011).
People with intestinal ostomies have many ostomy equipment options. Equipment includes a skin barrier, which adheres to the abdominal skin, and a collection pouch, which connects to the skin barrier and contains the stool. Managing an intestinal ostomy requires pouch emptying from one to many times a day. People who have colostomies need to empty the pouch once or twice a day. People who have ileostomies need to empty their pouch more frequently, from a few to many times a day. Less frequently, the skin barrier or entire appliance needs to be removed from the skin and changed. Ostomy care requires time, consistent routines, the ability to see the stoma (which may be obscured by a large abdomen or a peristomal hernia), manual dexterity, and stamina. Contact with ostomy output can lead to skin complications and can result from a retracted stoma, the location of the stoma on a patient's abdomen, or a variety of problems relating to managing the ostomy equipment. Good ostomy care can prevent leaks, rashes, skin breakdown, and the need for frequent skin barrier changes, while poor ostomy care can result in more frequent skin barrier changes and increasingly complex peristomal skin care.
Skin rashes and breakdown are a pervasive problem among individuals living with colostomies and ileostomies (Hellman & Lago, 1990). The most common problem is irritant dermatitis from contact with ostomy output, which creates a less resilient skin barrier and can lead to more serious complications (Nybaek et al., 2010). A recent review estimated the prevalence of peristomal skin problems at between 10.2% and 43% (Salvadalena, 2008). The lifetime cumulative probability of skin problems among long-term colostomates and ileostomates is estimated at 17.4% and 34%, respectively (Leong et al., 1994; Londono-Schimmer et al., 1994). Although early treatment and education can mitigate complicated wound care, peristomal skin problems are frequently unrecognized, underreported, and untreated (Hellman & Lago, 1990; Richbourg et al., 2007), even in populations with ready access to wound, ostomy, continence (WOC) nurses. (Herlufsen et al., 2006; Lyon et al., 2000) Approximately half of CRC survivors with ostomies may have a skin disorder, yet many will not seek professional care when the skin irritation is at an early stage. In this ethnographic study of family caregiving for CRC survivors with ostomies, we explored how long-term CRC survivors manage their ostomy care. We sought to identify the factors that hinder or facilitate prompt detection and treatment of ostomy and skin care problems, with the goal of improving care and quality of life for this vulnerable group of cancer survivors.
Our ethnographic approach is informed by a social ecology theory, which encompasses the physical, cognitive, and emotional work of caregiving in contrast to psychologically-oriented studies that frame caregiving as a form of stress (Brown & Stetz, 1999; Thomas & Morris, 2002). Social-ecological theorists argue that to understand the individual, one must consider the larger social system in which one operates. Social ecology has informed classic and recent qualitative and quantitative studies in gerontology and allows researchers to conceptualize the relationship between the individual and his/her physical and social environment (Lawton et al., 1978; Mendes de Leon et al., 2001; Strauss et al., 1984; Izal et al., 2005; Brandt & Pope, 1997; Putnam, 2002; Kahana, 1982).
Methods
All research activities for this study were approved by the Institutional Review Boards (IRBs) at Kaiser Permanente Northwest (KPNW) and Kaiser Permanente Northern California (KPNC).
Recruitment
Participants were members of an integrated health care delivery system, Kaiser Permanente, in its Northern California (KPNC) and Northwest (KPNW) regions. Participants were identified by searching tumor registries and administrative databases. We identified all long-term CRC survivors with ostomies (5+ years post-diagnosis) living within 100 miles of our research offices in Portland, OR and Oakland, CA. These individuals (N=307) were first invited to participate by mail, and then contacted by telephone for an eligibility screening interview, which confirmed that 105 survivors had a permanent ostomy, were receiving at least one hour of unpaid caregiving per week, and had no cognitive, speech, or hearing impairments that would preclude their participation in an in-depth interview. After recruiting survivors, we contacted and recruited their main informal caregivers. Of the 105 eligible survivor/caregiver pairs, 31 (29.5%) were enrolled. The remaining 70% declined to participate for a variety of reasons including caregivers’ schedule, failing health, or lack of interest. Six families who enrolled in the initial phase of the study were subsequently invited to participate in extended participant observation fieldwork, a naturalistic observation method used by cultural anthropologists that allows for informal conversations, observation of everyday activities, and increased rapport between researchers and study participants. (Dewalt et al., 1998; Creswell, 2007).
Measures
All participants completed a baseline interview with open-ended and fixed-choice questions on ostomy care, caregiving activities, and social and demographic characteristics. Medical records data were used to ascertain specific details of each survivor's cancer history and past use of medical care.
Data Collection
Three experienced ethnographers with PhD-level training in medical anthropology (CM) or sociology (AA, PL) collected the data. An additional ethnographer (CB) with a psychology background and extensive interviewing experience was trained and supervised by the study Principal Investigator (CM).
For baseline interviews, two-person teams interviewed cancer survivors and caregivers in their homes (in all but one case). Interviews were audio recorded and lasted approximately one hour. Interview questions explored caregiving activities, caregiving relationships, ostomy care routines, and ostomy-related problems. For ethnographic observation, we purposely selected six families to represent a range of health or caregiving situations. Each family was followed by one researcher, who spent 2 to 4 hours at a time directly observing ostomy care, daily routines, transportation out of the house, valued social activities, and health care visits. Data were recorded as fieldnotes after the visit. Interactions and stories from multiple family members and caregivers were documented in order to afford a more nuanced understanding of caregiving as it relates to ostomy care. Repeated visits with families also allowed ethnographers to follow up on questions from previous visits and during informal interviews with participants. Families were followed for an average of five months, with an average of 6.3 observation points per family.
Data Analysis
Transcribed interviews, fieldnotes, and analysis documents were managed with QSR International's NVIVO8 qualitative data analysis software. (Richards, 1999) Our investigator team—consisting of ethnographers (CM, AA, PL), a cancer nursing researcher (MG), a surgical oncologist (RK), and a health economist (MH)—discussed topics that arose in the interviews (e.g., social, caregiving, health system, and clinical issues) on a weekly basis. We used inductive theme analysis techniques (Strauss & Corbin, 1990; Luborsky, 1994) to develop codes focusing on themes relating to caregiving, and applied these to all baseline data. We conducted additional analyses focused on peristomal skin irritation by reviewing coded data and searching the entire dataset for sections containing the words skin, rash, red, sore, and irritation (as well as variants of those words). Using matrix analysis to understand patterns across families in our sample, (Knafl & Ayres, 1996) we identified barriers to and facilitators of detecting and reporting peristomal skin problems in this population. Given the small sample size in this study, we were only able to explore dimensions of variability that were central to the study aims and design: the interactions within caregiving relationships, caregiving activities, and ostomy-related health and well-being. Further explorations of differences in outcomes by gender, educational level, or ostomy type (colostomy or ileostomy) were beyond the scope of this study.
Results
Sample Description
Before we report our results, we will briefly describe our sample. Our sample of survivors and their caregivers represent diverse living situations and caregiving relationships, as described in Tables 1 and 2. All survivors were receiving at least one hour per week of unpaid assistance due to a health problem or functional impairment. Survivors were receiving varied types of assistance, including personal care, help with household tasks, and help with instrumental activities such as driving, managing finances, or health care (Table 1 describes survivors’ impairment levels). Of the 31 survivors, 15 received no help with ostomy care, 11 received help with ostomy care and other activities, and 5 received only ostomy care assistance, with no other form of informal or paid caregiving.
Table 1. Sample description.
| Variable | Frequency (percent) | |
|---|---|---|
|
| ||
| Patient N=31 | Caregiver N=31 | |
|
| ||
| Age | ||
| 45-70 | 10 (32.3) | 16 (51.6) |
| 71-84 | 15 (46.9) | 10 (32.3) |
| 85 + | 6 (19.4) | 2 (6.5) |
|
| ||
| Female | 17 (55%) | 22 (71%) |
|
| ||
| Household Income | NA | |
| Up to $30K | 6(19.4) | |
| $30,001 to $50K | 7 (22.6) | |
| $50,001 to $75K | 7 (22.6) | |
| Over $75 K | 5 (16.1) | |
| Missing | 6 (19.4) | |
|
| ||
| Education | ||
| HS/GED, vocational | 13(41.9) | 5 (16.1) |
| school, or less | 11 (35.5) | 17 (54.8) |
| Some college | 6 (19.4) | 5 (16.1) |
| Some graduate school | 1 (3.2) | 4 (12.9) |
| Missing | ||
|
| ||
| White or Caucasian | 27 (87.1) | 26 (83.8) |
|
| ||
| Impairment Level | N/A | |
| Needs ADL help1 | 18 (58.1) | |
| Needs IADL and/or ostomy care help | 13 (41.9) | |
|
| ||
| Type of ostomy | N/A | |
| Colostomy | 27 (87.1) | |
| Ileostomy | 4 (12.9) | |
ADL = Activity of daily living (i.e. bathing or dressing); IADL = Instrumental activity of daily living (i.e. driving or preparing meals).
Table 2. Household and caregiving situation of study participants.
| Variable | Frequency (percent) N=31 |
|---|---|
|
| |
| Household Status | |
| Lives with spouse | 21 (67.7) |
| Lives alone | 5 (12.9) |
| Lives with non-spouse caregiver | 5 (16.1) |
|
| |
| Caregiver's Relation to Patient | |
| Spouse | 21 (67.7) |
| Child | 2 (6.5) |
| Other Relative | 6 (19.4) |
| Not related | 2 (6.5) |
Factors that Hinder or Facilitate Detection and Treatment: Who Sees the Peristomal Skin?
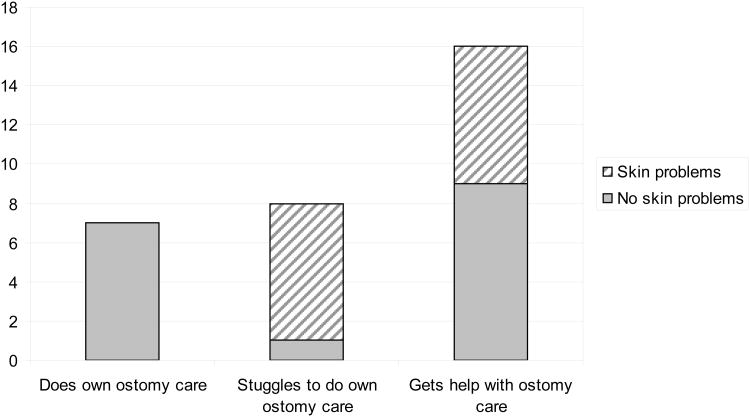
Our ethnographic study among CRC survivors and their caregivers sought to identify factors that hinder or facilitate the prompt detection and treatment of peristomal skin complications. One facilitator of prompt detection and treatment is having a caregiver who regularly sees the peristomal skin when the skin barrier is removed. Among the 15 survivors who received no help with ostomy care, eight reported no difficulties with ostomy care while seven others struggled and experienced problems such as leaks, poor placement of the skin barrier, anxiety about ostomy care or fatigue from ostomy care tasks. Of the 16 survivors receiving assistance with ostomy care, seven reported skin problems and all but one reported getting help with skin barrier changes (see Figure 1).
Figure 1. Ostomy care and detected peristomal skin problems (N=31).
Inability to see one's stoma or peristomal skin was the main reason for needing help with ostomy care. Some patients had failing eyesight that made it difficult to see and evaluate their skin, even if they could do their ostomy care by touch. Others had increased abdominal girth or skin folds that made it difficult or impossible to see their stoma. Several patients had hernias adjacent to the stoma that blocked their line-of-sight. Patients who cannot see their stoma or peristomal skin likely have more difficulty applying the skin barrier and appliance correctly, which in turn can cause leakage of ostomy output and subsequent skin problems.
Our analysis identified specific caregiving activities that facilitate the detection, reporting, and treatment of peristomal skin problems as well as challenges that make independent ostomy care difficult. They hinge on routine visual inspection of the stoma and peristomal skin area. Elements of ostomy care, such as emptying the bag, can take place multiple times a day. However, only removal of the skin barrier allows for inspection of the peristomal area. This can happen every several days to once a week. Who actually sees a patient's stoma and peristomal skin varies considerably. Informal caregivers who do not assist with skin barrier and appliance changes do not see the stoma or the skin around it, and therefore are unable to recognize when there is a problem. Even when caregivers observe intimate activities such as bathing and dressing, they cannot see the peristomal area when it is covered by the skin barrier and ostomy pouch.
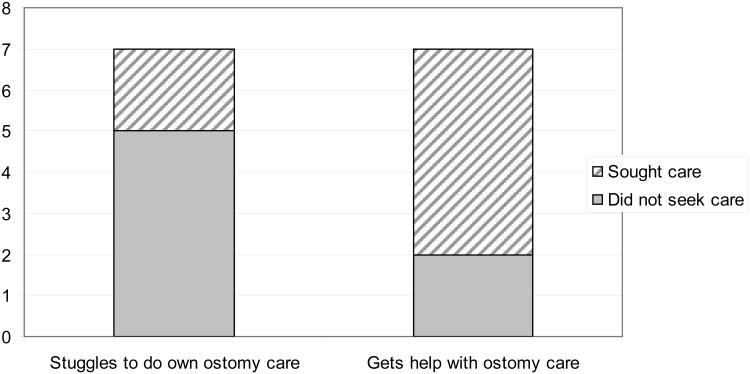
When caregivers participated in changing the appliance and revealing the peristomal skin, they gained an understanding of what normal or abnormal peristomal skin looks like. These caregivers helped by doing things that decreased skin irritation, such as thoroughly cleaning peristomal skin, allowing the area to dry, and applying powder, paste or medication before replacing the skin barrier and appliance. They also initiated health care intervention— such as seeking assistance from the WOC nurse, primary care clinician, or dermatologist—to evaluate peristomal skin and ostomy equipment problems. Figure 2 shows that among the 14 participants who reported peristomal skin problems, a higher proportion sought health care for their problem when their informal caregiver assisted with skin barrier and equipment changes. Examples are presented in Table 3.
Figure 2. Health care seeking for reported peristomal skin problems (N=14).
Table 3. Collaboration in skin barrier/appliance changes facilitates detection of peristomal skin problems: examples.
|
Who Receives Assistance with Ostomy Care?
Spouses were the only caregivers in our study who actively provided unpaid help with ostomy care, although several daughters had provided sporadic help to parents in the past or expressed willingness to do so in the future. Some participants viewed receiving or giving help with ostomy care as disgusting, embarrassing, or as a reflection of the survivor's incompetence for self-care. As one survivor stated, “I just dread the day that anybody would have to take care of me [in that way].” Several non-spousal caregivers described cooperating in ostomy care as a reversal of the child-parent role, creating strain for both care recipients and caregivers.
For some participants, their physical environment, housing, or finances hindered receiving assistance with ostomy care. A small or inconvenient bathroom arrangement made it hard for some to receive help. More significantly, survivors whose informal caregiver did not live with them faced multiple barriers to receiving assistance with ostomy care. The frequency of ostomy care tasks would require informal caregivers to change their employment or living arrangements in order to be available to help their loved ones. Alternatively, paid caregiving was unaffordable or unacceptable for some families. Finally, survivors living alone were reluctant to move to a relative's house or to an assisted living setting in order to receive help with ostomy care.
A small number of participants without spouses had significant functional impairments, ostomy care difficulties, and serious peristomal skin problems. They sought no help with ostomy care because they perceived no acceptable option for obtaining such help. (Table 4 provides descriptions of two such cases.)
Table 4. Barriers to receiving assistance with ostomy care from non-spouse caregivers: examples.
|
Sixteen of the 21 spouse pairs collaborated in ostomy care. Couples who collaborated in ostomy care tended to frame this work as part of caring for each other and an aspect of their marriage commitment. These couples had established intimate, caring routines for cooperating in ostomy care. One wife who diligently cared for her husband's ostomy-related needs described caregiving as the final act in a wonderful marriage to her terminally ill spouse. One husband created protective “gaskets” out of t-shirt material in order to prevent skin irritation around his wife's ostomy. A wife talked about helping her husband change his skin barrier, saying, “It feels comfortable.”
The five spouse pairs who did not collaborate in ostomy care did not feel comfortable about doing ostomy care together. One couple's relationship deteriorated after the husband's cancer surgery. The wife was disgusted by her husband's wounds and his ostomy care and became panic-stricken when she accidentally poked his stoma and made it bleed. Despite her husband's obvious struggles to manage ostomy care independently, she subsequently refused to help him. In another family, a husband caregiver, whose wife had very limited physical functioning, reported being depressed by the demands of caregiving. Outbursts of anger and frustration characterized his caregiving activities. Sometimes when a paid caregiver was unavailable to change his wife's appliance, he took off her equipment and used an adult diaper instead of going through the work to replace the skin barrier and pouch. The wife was stuck in a cycle of applying a cream to the peristomal area to treat irritation, having problems keeping her skin barrier on because of the cream, and then wearing diapers which only increased the contact between her skin and ostomy output.
These examples show how relationship history and the meaning attributed to ostomy care influence assistance with this task. Disgust, aversion, and anxiety are powerful barriers to providing assistance with ostomy care in family settings, yet some couples who cooperate in ostomy care do frame their actions in the context of an ongoing, positive relationship.
In summary, we have identified specific caregiving activities—skin barrier and appliance changes—that facilitate detection and treatment of peristomal skin problems. We additionally have illustrated psychosocial factors that can hinder or facilitate these activities. Table 5 summarizes our findings in terms of the factors that hinder or facilitate detection and reporting of peristomal skin problems among long-term CRC survivors in community settings.
Table 5. Detecting and reporting peristomal skin problems: Barriers and Facilitators.
| Barriers | Facilitators |
|---|---|
|
| |
|
|
Discussion
Half of the cancer survivors in our sample received some form of unpaid help with ostomy care and all of that help came from spouses. Spouses most frequently helped with changing the skin barrier or appliance. They assured correct placement and a good seal around the stoma to provide skin protection and they watched for skin changes. Survivors who receive help changing the skin barrier and appliance have fewer obstacles to prompt detection and treatment of peristomal skin problems. Survivors who were not managing ostomy care competently on their own and who did not have a caregiver who was willing to help with these intimate tasks seemed at highest risk for developing untreated skin problems.
Our findings suggest underlying causes for the pervasive untreated peristomal skin problems which have been assessed quantitatively in previous studies. (Hellman & Lago, 1990; Knafl & Ayres, 1996; Salvadalena, 2008; Leong et al., 1994; Londono-Schimmer et al., 1994; Pittman et al., 2008; Richbourg et al., 2007; Lyon et al., 2000; Herlufsen et al., 2006). As social-ecological theory would predict, we found that ostomy problems can manifest when a survivor's capacity for independent ostomy care does not fit the resources of family and household environments—a concept known as “person-environment fit” (Izal et al., 2005; Lawton et al., 1991; Kahana, 1982). We also identified barriers and facilitators to closing gaps in this person-environment fit. Weaknesses of this study include a relatively small sample size, few ileostomy patients (making comparison by type of ostomy difficult), lack of direct examination of patients’ peristomal skin or ostomy, and no formal assessment of competence at ostomy care. There was also little representation of ethnic and racial diversity. Additionally, we only interviewed individuals who were receiving informal caregiving at home. Other populations of CRC survivors with ostomies (such as those who have no caregiving needs, those who have no available caregivers, or those who live in nursing homes or other care facilities) may face different barriers and facilitators to detecting, reporting and seeking care for peristomal skin complications. Future research that focuses on these populations would add to our understanding of why peristomal skin problems go unreported. Strengths of this study relate to the depth of information gathered through interviewing and fieldwork, attention to informal caregiver perspectives, and a sample of families with a wide range of care needs.
Given how few people with peristomal skin complications seek medical care, we suggest several simple steps that any health care provider can take to improve patient care. First, directly ask patients about their ostomy care routines. Four simple questions are highlighted in Table 6. Second, involve caregivers in appointments when appropriate and ask caregivers for their input about ostomy care and skin problems. Third, refer any patients with ostomy care or skin problems to a nurse trained in ostomy care. Keep a list of such nurses and resources in your area, and consult the Wound Ostomy and Continence Nurses’ Society for more information (www.wocn.org). Fourth, organize your practice to enable direct examination of the patient's peristomal skin. Ask patients to bring a change of equipment or have some supplies available. Patients will need extra time in the exam room or in a bathroom to re-apply their equipment. Finally, given the prevalence of peristomal skin and ostomy management problems, annual check-ups with a WOC nurse may be warranted.
Table 6. Medical history questions about peristomal skin and ostomy care routines.
|
Acknowledgments
Support for this study was provided by Grant No. 1R21 CA129887 from the National Cancer Institute. We thank the study participants for their candor and patience in teaching us about life with an ostomy. We also thank Jennifer Schneider, Gail Morgan, Jeanne Reinhardt and Jill Pope for their assistance in preparing this manuscript. We presented an earlier version of the manuscript at the American Psychosocial Oncology Society meeting in New Orleans, LA in February 2010.
Support: Grant No. 1R21 CA129887 from the National Cancer Institute.
References
- Bober SL, Recklitis CJ, Campbell EG, Park ER, Kutner JS, Najita JS, et al. Caring for cancer survivors: a survey of primary care physicians. Cancer. 2009;115:4409–4418. doi: 10.1002/cncr.24590. [DOI] [PubMed] [Google Scholar]
- Brandt EN, Jr, Pope AM. Enabling America: Assessing the Role of Rehabilitation Science and Engineering. Washington, DC: National Academy Press; 1997. Models of disability and rehabilitation; pp. 62–80. [PubMed] [Google Scholar]
- Brown M, Stetz K. The labor of caregiving: a theoretical model of caregiving during potentially fatal illness. Qual Health Res. 1999;9:182–197. doi: 10.1177/104973299129121776. [DOI] [PubMed] [Google Scholar]
- Creswell J. Qualitative Inquiry & Research Design: Choosing among Five Approaches. Thousand Oaks CA: Sage Publications; 2007. [Google Scholar]
- Dewalt K, Dewalt B, Wyland C. Participant observation - 1998. In: Bernard HR, editor. Handbook of Methods in Cultural Anthropology. Walnut Creek, CA: Altamira Press; 1998. pp. 259–300. [Google Scholar]
- Forman D, Stockton D, Moller H, Quinn M, Babb P, De AR, et al. Cancer prevalence in the UK: results from the EUROPREVAL study. Ann Oncol. 2003;14:648–654. doi: 10.1093/annonc/mdg169. [DOI] [PubMed] [Google Scholar]
- Hellman J, Lago CP. Dermatologic complications in colostomy and ileostomy patients. Int J Dermatol. 1990;29:129–133. doi: 10.1111/j.1365-4362.1990.tb04085.x. [DOI] [PubMed] [Google Scholar]
- Herlufsen P, Olsen AG, Carlsen B, Nybaek H, Karlsmark T, Laursen TN, et al. Study of peristomal skin disorders in patients with permanent stomas. Br J Nurs. 2006;15:854–862. doi: 10.12968/bjon.2006.15.16.21848. [DOI] [PubMed] [Google Scholar]
- Horner M, Ries L, Krapcho M, Neyman N, Aminou R, Howlader N, et al. SEER Cancer Statistics Review, 1975-2006. 2009 HTTP://seer.cancer.gov/csr/1975_2006/ [On-line]. Available: HTTP://seer.cancer.gov/csr/1975_2006/
- Izal M, Montorio I, Marquez M, Losada A. Caregivers' expectations and care receivers' competence Lawton's ecological model of adaptation and aging revisited. Arch Gerontol Geriatr. 2005;41:129–140. doi: 10.1016/j.archger.2005.01.001. [DOI] [PubMed] [Google Scholar]
- Kahana E. A congruence model of person-environment interaction. In: Lawton MP, Windley PG, Byerts TO, editors. Aging and the Environment: Theoretical Approaches. New York: Springer; 1982. pp. 97–121. [Google Scholar]
- Knafl K, Ayres L. Managing Large Qualitative Data Sets in Family Research. Journal of Family Nursing. 1996;2:350–365. [Google Scholar]
- Lawton M, Brody E, Turner-Massey P. The relationships of environmental factors to changes in well-being. Gerontologist. 1978;18:133–137. doi: 10.1093/geront/18.2.133. [DOI] [PubMed] [Google Scholar]
- Lawton M, Moss M, Kleban M, Glicksman A, Rovine M. A two-factor model of caregiving appraisal and psychological well-being. J Gerontol. 1991;46:181–189. doi: 10.1093/geronj/46.4.p181. [DOI] [PubMed] [Google Scholar]
- Leong AP, Londono-Schimmer EE, Phillips RK. Life-table analysis of stomal complications following ileostomy. Br J Surg. 1994;81:727–729. doi: 10.1002/bjs.1800810536. [DOI] [PubMed] [Google Scholar]
- Londono-Schimmer EE, Leong AP, Phillips RK. Life table analysis of stomal complications following colostomy. Dis Colon Rectum. 1994;37:916–920. doi: 10.1007/BF02052598. [DOI] [PubMed] [Google Scholar]
- Luborsky M. The identification and analysis of themes and patterns. In: Gubrium GF, Sankar A, editors. Qualitative Methods in Aging Research. New York: Sage Publications; 1994. pp. 189–210. [Google Scholar]
- Lyon CC, Smith AJ, Griffiths CE, Beck MH. The spectrum of skin disorders in abdominal stoma patients. Br J Dermatol. 2000;143:1248–1260. doi: 10.1046/j.1365-2133.2000.03896.x. [DOI] [PubMed] [Google Scholar]
- Maddams J, Brewster D, Gavin A, Steward J, Elliott J, Utley M, et al. Cancer prevalence in the United Kingdom: estimates for 2008. Br J Cancer. 2009;101:541–547. doi: 10.1038/sj.bjc.6605148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mendes de Leon C, Gold D, Glass T, Kaplan L, George L. Disability as a function of social networks and support in elderly African Americans and Whites: the Duke EPESE 1986--1992. J Gerontol B Psychol Sci Soc Sci. 2001;56:S179–S190. doi: 10.1093/geronb/56.3.s179. [DOI] [PubMed] [Google Scholar]
- Nybaek H, Knudsen DB, Laursen TN, Karlsmark T, Jemec GB. Quality of life assessment among patients with peristomal skin disease. Eur J Gastroenterol Hepatol. 2010;22:139–143. doi: 10.1097/MEG.0b013e32832ca054. [DOI] [PubMed] [Google Scholar]
- Pittman J, Rawl SM, Schmidt CM, Grant M, Ko CY, Wendel C, et al. Demographic and clinical factors related to ostomy complications and quality of life in veterans with an ostomy. Journal of Wound, Ostomy & Continence Nursing. 2008;35:493–503. doi: 10.1097/01.WON.0000335961.68113.cb. [DOI] [PubMed] [Google Scholar]
- Putnam M. Linking aging theory and disability models: increasing the potential to explore aging with physical impairment. Gerontologist. 2002;42:799–806. doi: 10.1093/geront/42.6.799. [DOI] [PubMed] [Google Scholar]
- Ricciardi R, Roberts PL, Read TE, Baxter NN, Marcello PW, Schoetz DJ. Presence of specialty surgeons reduces the likelihood of colostomy after proctectomy for rectal cancer. Dis Colon Rectum. 2011;54:207–213. doi: 10.1007/DCR.0b013e3181fb8903. [DOI] [PubMed] [Google Scholar]
- Richards L. Using NVivo in qualitative research. London & Los Angeles: Sage; 1999. [Google Scholar]
- Richbourg L, Thorpe JM, Rapp CG. Difficulties experienced by the ostomate after hospital discharge. Journal of Wound, Ostomy & Continence Nursing. 2007;34:70–79. doi: 10.1097/00152192-200701000-00011. [DOI] [PubMed] [Google Scholar]
- Salvadalena G. Incidence of complications of the stoma and peristomal skin among individuals with colostomy, ileostomy, and urostomy: a systematic review 10. Journal of Wound, Ostomy & Continence Nursing. 2008;35:596–609. doi: 10.1097/01.WON.0000341473.86932.89. [DOI] [PubMed] [Google Scholar]
- Strauss A, Corbin J. Basics of qualitative research: Grounded theory procedures and techniques. Newbury Park CA: Sage; 1990. [Google Scholar]
- Strauss A, Corbin J, Fagerhaugh S, Glaser B, Maines D, Suczek B, et al. Chronic Illness and the Quality of Life. 2nd. St. Louis, MO: Mosby; 1984. [Google Scholar]
- Thomas C, Morris S. Informal carers in cancer contexts. Eur J Cancer Care (Engl) 2002;11:178–182. doi: 10.1046/j.1365-2354.2002.00336.x. [DOI] [PubMed] [Google Scholar]