Abstract
Tedizolid phosphate: a second-generation oxazolidinone for acute bacterial skin and skin structure infections
INTRODUCTION
Between 2001 and 2003, acute bacterial skin and skin structure infections (ABSSSIs) accounted for more than 11 million ambulatory care visits, with a visit rate of 410.7 per 10,000 persons.1 As a broader term, ABSSSI encompasses the following (Table 1):2–4
Cellulitis/erysipelas
Wound infection
Major cutaneous abscess
Table 1.
Characteristics of ABSSSIs
| Cellulitis/erysipelas | |
| Wound infection |
|
| Cutaneous abscess |
This infection is characteristically identified by a measurable lesion (based on edema, redness, and induration) of at least 75 cm2 with systemic signs of infection and/or lymphadenopathy.2–4 For major abscesses and wound infections, the area of erythema or induration must also extend 5 cm or more from the peripheral margin of the lesion.3,4 A common contributing pathogen in this setting is Staphylococcus aureus, particularly methicillin-resistant S. aureus (MRSA).1,4 Several pharmacological options, including oxazolidinones, are available for use (Table 2).5,6
Table 2.
Examples of Antibacterial Drugs Used Against MRSA5
| Class | Drug |
|---|---|
| Beta-lactam | Ceftaroline |
| Folate antagonist | Trimethoprim-sulfamethoxazole |
| Glycolipopeptide | Telavancin |
| Glycopeptide | Vancomycin |
| Lincosamide | Clindamycin |
| Lipopeptide | Daptomycin |
| Oxazolidinone | Linezolid |
| Streptogramin | Quinupristin-dalfopristin |
| Tetracycline | Minocycline |
In 2000, linezolid (Zyvox, Pfizer) became the first oxazolidinone approved by the Food and Drug Administration (FDA). Its mechanism of action entails inhibition of bacterial protein synthesis by binding 23S ribosomal RNA within the 50S subunit. Indications for use include the management of skin and skin structure infections (complicated and uncomplicated), community-acquired pneumonia, nosocomial pneumonia, and vancomycin-resistant Enterococcus faecium infections. Linezolid is bacteriostatic against staphylococci and enterococci, and bactericidal against streptococci strains. Conveniently dosed at 600 mg twice daily, it can be administered intravenously or orally in a 1:1 ratio. Notable warnings and precautions are serotonin syndrome, myelosuppression, and postmarketing reports of hypoglycemia with concomitant use of antihyperglycemic agents.6
Since its release, however, there have been reports of MRSA strains resistant to linezolid due to the acquisition of a natural resistance gene known as cfr (chloramphenicol-florfenicol resistance). As a result, Cfr methyltransferase is expressed and alters the 23S rRNA component of the ribosomal subunit in bacteria.7,8 Introducing a unique challenge for the management of multidrug-resistant gram-positive organisms, new drug developments have been explored.
In June 2014, the FDA approved tedizolid phosphate (Sivextro, Cubist Pharmaceuticals) as a second-generation oxazolidinone with potentially four- to 16-fold potency against MRSA when compared with linezolid.9–11 Favorable results from clinical trials have led to its indication for the treatment of ABSSSIs in adult patients with susceptible bacteria.11 This article reviews the information available to date on this product in relation to safety and efficacy.
CHEMICAL STRUCTURE
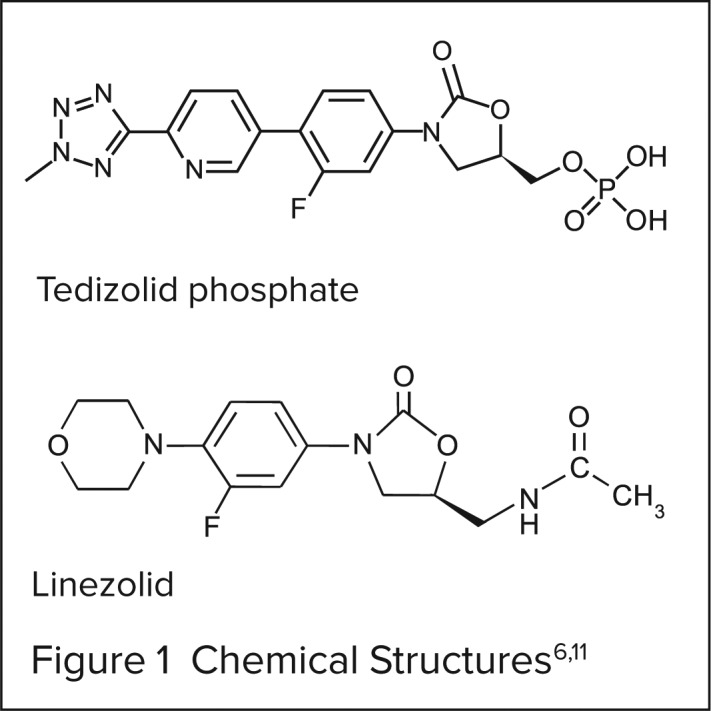
The full chemical name of tedizolid is (5R)-3-{3-fluoro-4-[6-(2-methyl-2H-tetrazol-5-yl)pyridine-3-yl]phenyl}-5-(hydroxymethyl)-1,3-oxazolidin-2-one.9 Figure 1 illustrates the chemical structures of tedizolid phosphate and linezolid.
Figure 1.
CLINICAL PHARMACOLOGY
Tedizolid phosphate is a prodrug that is converted by plasma phosphatases to microbiologically active tedizolid in vivo. It interacts with the bacterial 23S ribosome initiation complex and binds to the 50S subunit to prevent the formation of the 70S complex. As a result, tedizolid inhibits bacterial translation and protein synthesis.9,10
MICROBIOLOGICAL ACTIVITY
Tedizolid has activity against clinically relevant gram-positive pathogens such as MRSA, methicillin-susceptible S. aureus (MSSA), Streptococcus pyogenes, Streptococcus agalactiae, enterococci, and coagulase-negative staphylococci (Table 3). In addition, this drug has demonstrated activity against linezolid-resistant staphylococci (Table 4).10–13
Table 3.
Spectrum of Activity for Tedizolid11
| Aerobic and facultative gram-positive bacteria |
|
| Aerobic and facultative anaerobic gram-positive bacteria |
|
Table 4.
Comparison of Tedizolid vs. Linezolid-Resistant Staphylococci13
| MIC Range (mg/L) | Resistant Strains | ||
|---|---|---|---|
| Coagulase-negative staphylococci | Tedizolid | 0.06 to 16 | — |
| Linezolid | 8 to > 128 | 100 | |
| Staphylococcus aureus | Tedizolid | 0.5 | — |
| Linezolid | 8 to 16 | 100 |
Specific to S. aureus strains in vitro, tedizolid had a minimum inhibitory concentration (MIC) range of 0.125 to 0.5 mcg/mL. Further evaluation showed that 95% of MRSA isolates and 72% of MSSA isolates had a MIC of 0.25 mcg/mL or less.12 For penicillin-resistant streptococcus pneumoniae, in vitro susceptibility results showed a MIC of 0.125 to 0.25 mcg/mL and MIC50 (the MIC at which 50% of the isolates were inhibited) of 0.25 mcg/mL. When considering MIC90 (the MIC at which 90% of the isolates were inhibited), tedizolid was four times more potent than linezolid, with values of 0.25 mcg/mL and 1 mcg/mL, respectively.14
PHARMACODYNAMICS AND PHARMACOKINETICS
Using a neutropenic murine S. aureus pneumonia model, the mean free drug area under the curve (fAUC) over 24 hours divided by the MIC, or fAUC/MIC ratio, associated with a bacteriostatic endpoint was comparable between tedizolid and linezolid: 20 versus 19, respectively. The average fAUC/MIC ratio for a bactericidal or 1-log unit kill endpoint was about two-fold higher when compared with bacteriostatic endpoints, with no difference between treatment groups (tedizolid, 34.6, and linezolid, 46.1, respectively; P = 0.334).15 Moreover, tedizolid has been shown to be bacteriostatic at 24 hours and bactericidal by day 3 of treatment in S. aureus isolates.16
A prospective, open-label, multiple-dose study evaluated the pharmacokinetics of tedizolid phosphate 200 mg by mouth (PO) once daily for three days. A total of 20 healthy adult patients completed the study, with an average age of 28 ± 9 years and weight of 82.4 ± 12.5 kg. There was no difference in drug concentrations obtained immediately prior to the third dose and at 24 hours (P = 0.947), indicating steady-state concentrations. Plasma pharmacokinetic data obtained from bronchoalveolar samples on day 3 revealed a maximum drug concentration (Cmax) of 2.4 ± 0.4 mcg/mL, time to Cmax (Tmax) of two hours (range: 0.5 to 4 hours), terminal half-life (t½) of 9.2 ± 2 hours, and protein binding of 89.44 ± 1.58%. This study also described higher concentrations in the epithelial lining fluid and alveolar macrophages compared to free plasma concentrations, suggesting extensive penetration into both extracellular and intracellular pulmonary compartments.17
Sahre et al. evaluated a single 600-mg oral dose of tedizolid phosphate in 12 healthy volunteers. Pharmacokinetic analysis of drug in plasma reported a Cmax of 5.4 ± 1.5 mg/L, Tmax of 2.4 ± 1.1 hours, t½ of 8.1 hours (range: 5.9 to 12.8 hours), and protein binding of 87.3 ± 1.3%. It was also found that tedizolid freely distributes into adipose and muscle tissue following the single dose, with similar levels detected in free plasma concentrations.18
Active tedizolid had a mean total clearance (CL) of 8.28 L/hr and distribution clearance (CLd) of 2.95 L/hr. A central compartment volume (V1) of 71.4 L and peripheral compartment volume (V2) of 27.9 L were reported.10
In summary, according to the prescribing information, peak plasma concentrations are attained within approximately three hours after oral tedizolid therapy and one hour following a tedizolid infusion. The absolute bioavailability is approximately 91% for both formulations, with a reported 70% to 90% plasma protein binding capacity. The volume of distribution at steady state for a single intravenous (IV) dose is on average 67 to 80 L. Tedizolid seems to be an unlikely substrate of the CYP450 enzymes. However, a majority of the compound is hepatically eliminated.11 Table 5 compares the pharmacokinetic parameters of tedizolid phosphate and linezolid.
Table 5.
Mean (Standard Deviation) Pharmacokinetic Parameters
| Tedizolid Phosphate11 (200 mg PO once daily) | Linezolid6 (600 mg PO twice daily) | |
|---|---|---|
| Cmax (mg/L) | 2.2 ± 0.6 | 21.2 ± 5.78 |
| Tmax (hours) | 3.5 (1.0 to 6.0) † | 1.03 ± 0.62 |
| T½ (hours) | 12 | 5.4 ± 2.06 |
| Clearance (L/hr) | 8.4 ± 2.1 | 4.8 ± 1.74 |
| AUC (mcg*hr/mL) | 25.6 ± 8.4 | 138 ± 42.1 |
Median (range)
PIVOTAL CLINICAL TRIALS
Phase 2 Trial
Prokocimer et al. conducted a randomized, double-blind, dose-ranging study involving tedizolid phosphate at 12 U.S. sites. Eligible patients had to be 18 to 75 years old with complicated skin and skin structure infection (cSSSI) and a suspected or confirmed gram-positive pathogen. Types of infections included were deep extensive cellulitis, abscesses, and surgical or post-traumatic wounds.10 The main difference between cSSSI and ABSSSI is a distinguishing factor of lesion size present with the latter.
Patients were randomized in a 1:1:1 ratio to receive 200, 300, or 400 mg of oral tedizolid phosphate daily for five to seven days. The primary objective was clinical response rates in each group at the test-of-cure visit in the clinically evaluable (CE) and clinical modified-intent-to-treat (cMITT) populations. A total of 188 patients were included in the modified intent-to-treat (MITT) and cMITT analysis (200-mg group, n = 63; 300-mg group, n = 63; 400-mg group, n=62). The most common pathogen isolated was S. aureus (90.3%), with a majority identified as MRSA strains (80.6%). Patients were treated for an average of 6.4 days. The clinical response rates were similar in all dosing arms: MITT, 87.8%; CE, 95.7%; microbiologically evaluable, 96.2%. Data trends were also similar irrespective of lesion type or size and infection severity.10
Phase 3 Trials
ESTABLISH-1
The efficacy and safety of tedizolid phosphate versus linezolid in ABSSSI were evaluated in a multicenter, randomized, double-blind, double-dummy, noninferiority, phase 3 trial. Patients had to be 18 years of age or older with cellulitis/erysipelas, major cutaneous abscess, or wound infection. Along with erythema and a total lesion size of at least 75 cm2, patients also had to have at least one local, regional, or systemic sign of infection and a documented or suspected gram-positive bacterium. Patients were excluded if they had an uncomplicated ABSSSI, a vascular catheter site– associated ABSSSI, thrombophlebitis, or surgery other than clean surgery; if they received any other topical or systemic antibiotics with similar spectrum of activity within 96 hours of the first dose of study drug; or if they previously failed therapy at the same infection site. Eligible patients were randomized on a 1:1 basis to receive either tedizolid phosphate 200 mg PO once daily for six days or linezolid 600 mg PO twice daily for 10 days. The primary endpoint was an early clinical response at the 48- to 72-hour assessment in the intent-to-treat (ITT) analysis group. A treatment responder was defined as a patient who was afebrile; had no growth in lesion area, width, or length from baseline; did not receive other antimicrobial therapy identified by the exclusion criteria; and did not die of any cause.12
A total of 667 patients were randomized to tedizolid phosphate (n = 332) or linezolid (n = 335). The median age was 43 years (range: 18 to 100 years). A majority of patients had cellulitis/erysipelas (41.1%) versus major cutaneous abscess (29.7%) or wound infections (29.25%). S. aureus was the most common pathogen detected, with MRSA isolated in both tedizolid phosphate (42.1%) and linezolid (43.1%) groups. Treatment response rates were similar at the 48- to 72-hour assessment in those taking tedizolid phosphate (79.5%; 95% confidence interval [CI], 74.8 to 83.7%) and linezolid (79.4%; 95% CI, 74.7 to 83.6%). Noninferiority was achieved with an absolute treatment difference of 0.1% (95% CI, −6.1 to 6.2%). Sustained clinical success rates at the end of treatment using the ITT data were comparable between the tedizolid phosphate (69.3%; 95% CI, 64 to 74.2%) and linezolid (79.1%; 95% CI, 66.8 to 76.7%) groups (absolute treatment difference, −2.6%; 95% CI, −9.6 to 4.2%). Similar trends were noted in clinical responses assessed by investigators.12
ESTABLISH-2
A subsequent randomized, double-blind, parallel-group, noninferiority phase 3 trial evaluated the use of IV tedizolid phosphate or linezolid with an option to switch to oral therapy. Patients had to be 12 years of age or older with a minimum lesion area of 75 cm2, a documented or suspected gram-positive infection, and at least one regional or systemic sign of infection. The margin of abscess or wound, if present, had to extend 5 cm or more from the abscess and wound, induration, erythema, or edema. Exclusion criteria were analogous to the ESTABLISH-1 trial. Eligible patients received randomly, in a 1:1 ratio, IV tedizolid phosphate 200 mg once daily for six days or IV linezolid 600 mg twice daily for 10 days. Patients who received at least two doses of therapy were eligible to switch to oral therapy if they met at least two of the following criteria: no increase in lesion size compared with baseline, temperature of 37.7°C or less, or absence of worsening signs and symptoms of the affected area. Additional therapy to broaden coverage for gram-negative or anaerobic bacteria was permitted for wound infections at the discretion of the investigator. The primary outcome was early clinical response 48 to 72 hours following the initiation of treatment. Treatment responders were defined as patients who had a 20% or more reduction in the primary lesion from baseline, did not receive any other systemic antibiotic therapy with overlapping gram-positive activity, and did not die from any cause within 72 hours of receiving the first dose of study drug.19
A total of 666 patients received either tedizolid phosphate (n = 332) or linezolid (n = 334). There was no difference in baseline characteristics between the groups. The median age of patients receiving tedizolid phosphate was 46 years (range: 17 to 86). Cellulitis or erysipelas accounted for a majority of the ABSSSIs (tedizolid phosphate, n = 166, 50%; linezolid, n = 168, 50%). Other reported infections included major cutaneous abscess (tedizolid phosphate, n = 68, 20%; linezolid, n = 68, 20%) and infected wounds (tedizolid phosphate, n = 98, 30%; and linezolid, n = 98, 29%). Approximately 59.5% of the study population had at least one gram-positive organism identified at baseline (tedizolid phosphate, n = 197, 59%; linezolid, n = 202, 60%). At 81.5%, S. aureus was the most common organism identified (tedizolid phosphate, n = 158, 80%; linezolid, n = 167, 83%), with 27.5% being MRSA isolates and 54% MSSA isolates. Other gram-positive bacteria identified were beta-hemolytic streptococci, Streptococcus agninosus group, and Enterococcus faecalis. The mean time to switch to oral therapy was similar between groups (tedizolid phosphate, 1.7 ± 1.18 days; linezolid, 1.8 ± 1.35 days, P = 0.99). There were also no statistically significant differences in the mean durations of IV treatment, which for the U.S. were 2.2 ± 2.17 days and 2.0 ± 2.03 days with tedizolid phosphate and linezolid, respectively. However, there was a disparity between patients managed outside the U.S., suggesting different clinical practices overseas. Only 18% of patients received IV study drug for the entire treatment duration. Early clinical response at 48 to 72 hours was achieved in 85% (n = 283) of patients receiving tedizolid phosphate and 83% (n = 276) of patients receiving linezolid therapy. Thus, non-inferiority was attained with an absolute difference of 2.6% (95% CI, −3.0 to 8.2).19
SAFETY PROFILE
Adverse Events
Tedizolid phosphate was well tolerated following the oral administration of a once-daily 200-mg dose for three days. No serious adverse events (AEs) were reported; the most commonly reported AEs were mild bradycardia (n = 2), headache (n = 1), and nausea (n = 1).17
In the ESTABLISH-1 trial, the most common AEs associated with tedizolid phosphate were gastrointestinal in nature (nausea, vomiting, and diarrhea), although they occurred at a lesser incidence than with linezolid (15.7% for tedizolid phosphate vs. 24.8% for linezolid). Headaches were also reported (6.3% for tedizolid phosphate vs. 5.1% for linezolid). The rates of serious AEs were low in both arms. However, alanine aminotransferase elevations greater than or equal to twice the baseline or upper limit of normal were noted in 24 patients (4.1% for tedizolid phosphate vs. 3.5% for linezolid). Patients continued therapy regardless of this abnormality and there were no implications of hepatic dysfunction or toxicity. Other laboratory data revealed that patients who received tedizolid phosphate (2.3%) had a lower incidence of abnormal platelet counts compared with linezolid (4.9%). Platelet counts normalized without medical intervention.12
Gastrointestinal effects (nausea, vomiting, and diarrhea) and headaches were also seen with tedizolid phosphate in the ESTABLISH-2 trial; however, there were no statistically significant differences when compared with linezolid. Nine percent of patients in the tedizolid phosphate group and 13% of patients in the linezolid group had a platelet count below the lower limit of normal (less than 150 × 109/L; P = 0.071). A smaller percentage of patients had an absolute neutrophil count below the lower limit of normal (less than 1.6 × 109/L) with tedizolid phosphate (nine of 305 patients, 3%) compared with linezolid (21 of 299 patients, 7%; P = 0.024).19
Warnings and Precautions
Due to a lack of efficacy and safety data in the setting of neutropenia, clinicians should consider alternative therapies when managing a patient with neutropenia and ABSSSIs.11
Special Populations
Tedizolid phosphate is classified as pregnancy category C. Animal data have shown the potential to induce toxic effects on fetal development. In rats, tedizolid was excreted in breast milk.11
DOSAGE AND ADMINISTRATION
Based on the findings of the dose-ranging study conducted by Prokocimer et al., the recommended dose for tedizolid phosphate in adult patients (18 years of age or older) is 200 mg once daily either orally or intravenously for six days. Dosage adjustments are not necessary for patients with hepatic impairment, renal impairment, or undergoing hemodialysis.10,11
The IV solution is prepared from a sterile, lyophilized powder, single-use 200-mg vial. It must be reconstituted with 0.9% sodium chloride injection, USP, and administered as an infusion over one hour; it is not to be given as an IV push or bolus.11
DRUG–DRUG AND DRUG–FOOD INTERACTIONS
Tedizolid (200 mg daily) has a 50% inhibitory concentration (IC50) of 8.7 µM and 5.7 µM for monoamine oxidase (MAO)-A and MAO-B, respectively. Linezolid (600 mg twice daily), on the other hand, seemed to have a higher overall IC50 for these enzymes (MAO-A = 46 µM, MAOB = 2.1 µM). These data show that tedizolid is a seemingly weak, reversible inhibitor of MAO in vitro.20
A tyramine sensitivity study was conducted in 30 healthy patients to determine the concentration of tyramine needed to increase systolic blood pressure by 30 mmHg or greater (TYR30). As a result, a geometric mean tyramine sensitivity ratio (placebo TYR30 divided by tedizolid phosphate TYR30) of 1.33 was identified (90% CI, 1.05 to 1.69). Of note, a ratio of two or more was deemed to be clinically relevant. Although tedizolid phosphate was generally well tolerated, at least 25 of 30 patients experienced palpitations, a known AE in tyramine-based studies. This study also concluded that 550 mg or more of tyramine is needed to observe a 30 mmHg increase in systolic blood pressure with tedizolid phosphate. It is therefore unlikely to see clinically relevant pressor effects in patients taking a tyramine-rich meal while receiving tedizolid phosphate therapy.20
Tedizolid phosphate also does not seem to have meaningful effects on blood pressure when coadministered with pseudoephedrine.20 However, as the data are still scarce, further studies are needed to determine tedizolid phosphate’s potential for other adrenergic and serotonergic interactions observed with linezolid.
COST AND AVAILABILITY
Tedizolid phosphate is available as 200-mg tablets in a unit dose blister pack of six tablets or a bottle of 30 tablets. It is also available as a 200-mg single-use vial for injection. The average wholesale prices for six days of oral versus IV therapy are $2,212 and $1,692, respectively.21
P&T COMMITTEE CONSIDERATIONS
Tedizolid phosphate has demonstrated good activity against clinically relevant gram-positive organisms such as MRSA. Potential advantages with the available data include enhanced potency, longer half-life, weak and reversible inhibition of MAO enzymes, and an improved safety profile when compared to linezolid. Although several agents with a similar spectrum of activity are currently available (Table 2), tedizolid phosphate may have a role in treating infections involving antimicrobial resistance. Additional efficacy and safety data are needed before P&T committees can delineate its specific role in clinical practice and make a formulary decision.
CONCLUSION
Tedizolid phosphate is a novel second-generation oxazolidinone with activity against clinically relevant gram-positive organisms. It has recently been approved for the management of ABSSSIs in adults. Additional data are needed on the safety of this therapy when used in the setting of neutropenia and on coadministration with serotonergic agents. As studies continue, it will also be interesting to see the effectiveness of tedizolid phosphate in other indications such as nosocomial pneumonias (NCT02019420).22
REFERENCES
- 1.McCaig LF, McDonald LC, Mandal S, Jernigan DB. Staphylococcus aureus-associated skin and soft tissue infections in ambulatory care. Emerg Infect Dis. 2006;12(11):1715–1723. doi: 10.3201/eid1211.060190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Food and Drug Administration, Center for Drug Evaluation and Research Guidance for Industry: Acute Bacterial Skin and Skin Structure Infections: Developing Drugs for Treatment. Available at: http://www.fda.gov/downloads/Drugs/.../Guidances/ucm071185.pdf. Accessed February 4, 2014. [Google Scholar]
- 3.Itani KM, Shorr AF. FDA guidance for ABSSSI trials: implications for conducting and interpreting clinical trials. Clin Infect Dis. 2014;58(S1):S4–9. doi: 10.1093/cid/cit612. [DOI] [PubMed] [Google Scholar]
- 4.Corey GR, Stryjewski ME. New rules for clinical trials of patients with acute bacterial skin and skin-structure infections: do not let the perfect be the enemy of the good. Clin Infect Dis. 2011;52(S7):S469–S476. doi: 10.1093/cid/cir162. [DOI] [PubMed] [Google Scholar]
- 5.Stevens DL, Bisno AL, Chambers HF, et al. Practice guidelines for the diagnosis and management of skin and soft-tissue infections. Clin Infect Dis. 2005;41:1373–1406. doi: 10.1086/497143. [DOI] [PubMed] [Google Scholar]
- 6.Zyvox (linezolid) prescribing information. New York, New York: Pharmacia & Upjohn Co.; 2013. Available at: http://labeling.pfizer.com/showlabeling.aspx?id=649. Accessed February 4, 2014. [Google Scholar]
- 7.Toh S-M, Xiong L, Arias CA, et al. Acquisition of a natural resistance gene renders a clinical strain of methicillin-resistant Staphylococcus aureus resistant to the synthetic antibiotic linezolid. Mol Microbiol. 2007;64(6):1506–1514. doi: 10.1111/j.1365-2958.2007.05744.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Morales G, Picazo JJ, Baos E, et al. Resistance to linezolid is mediated by the cfr gene in the first report of an outbreak of linezolid-resistant Staphylococcus aureus. Clin Infect Dis. 2010;50(6):821–825. doi: 10.1086/650574. [DOI] [PubMed] [Google Scholar]
- 9.Kanafani Z, Corey GR. Tedizolid (TR-701): a new oxazolidinone with enhanced potency. Expert Opin Investig Drugs. 2012;21(4):515–522. doi: 10.1517/13543784.2012.660250. [DOI] [PubMed] [Google Scholar]
- 10.Prokocimer P, Bien P, Surber J, et al. Phase 2, randomized, double-blind, dose-ranging study evaluating the safety, tolerability, population pharmacokinetics, and efficacy of oral torezolid phosphate in patients with complicated skin and skin structure infections. Antimicrob Agents Chemother. 2011;55(2):583–592. doi: 10.1128/AAC.00076-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sivextro (tedizolid phosphate) prescribing information. Lexington, Massachusetts: Cubist Pharmaceuticals U.S.; 2014. Available at: http://sivextro.com/pdf/PrescribingInformation.pdf. Accessed July 9, 2014. [Google Scholar]
- 12.Prokocimer P, De Anda C, Fang E, et al. Tedizolid phosphate vs. linezolid for treatment of acute bacterial skin and skin structure infections: the ESTABLISH-1 randomized trial. JAMA. 2013;306(6):559–569. doi: 10.1001/jama.2013.241. [DOI] [PubMed] [Google Scholar]
- 13.Rodriguez-Avial I, Culebras E, Betriu C, et al. In vitro activity of tedizolid (TR-700) against linezolid-resistant staphylococci. J Antimicrob Chemother. 2012;67(1):167–169. doi: 10.1093/jac/dkr403. [DOI] [PubMed] [Google Scholar]
- 14.Choi S, Im W, Bartizal K. Activity of tedizolid phosphate (TR-701) in murine models of infection with penicillin-resistant and penicillin-sensitive Streptococcus pneumoniae. Antimicrob Agents Chemother. 2012;56(9):4713–4717. doi: 10.1128/AAC.00346-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lepak AJ, Marchillo K, Pichereau S, et al. Comparative pharmacodynamics of the new oxazolidinone tedizolid phosphate and linezolid in a neutropenic murine Staphylococcus aureus pneumonia model. Antimicrob Agents Chemother. 2012;56(11):5916–5922. doi: 10.1128/AAC.01303-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Keel RA, Tessier PR, Crandon JL, Nicolau DP. Comparative efficacies of human simulated exposures of tedizolid and linezolid against Staphylococcus aureus in the murine thigh infection model. Antimicrob Agents Chemother. 2012;56(8):4403–4407. doi: 10.1128/AAC.00122-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Housman ST, Pope JS, Russomanno J, et al. Pulmonary disposition of tedizolid following administration of once-daily oral 200-milligram tedizolid phosphate in healthy adult volunteers. Antimicrob Agents Chemother. 2012;56(5):2627–2634. doi: 10.1128/AAC.05354-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sahre M, Sabarinath S, Grant M, et al. Skin and soft tissue concentrations of tedizolid (formerly torezolid), a novel oxazolidinone, following a single oral dose in healthy volunteers. Int J Antimicrob Agents. 2012;40(1):51–54. doi: 10.1016/j.ijantimicag.2012.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Moran GJ, Fang E, Corey GR, et al. Tedizolid for 6 days versus linezolid for 10 days for acute bacterial skin and skin-structure infections (ESTABLISH-2): a randomized, double-blind, phase 3, non-inferiority trial. Lancet Infect Dis. 2014 doi: 10.1016/S1473-3099(14)70737-6. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 20.Flanagan S, Bartizal K, Minassian SL, et al. In vitro, in vivo, and clinical studies of tedizolid to assess the potential for peripheral or central monoamine oxidase interactions. Antimicrob Agents Chemother. 2013;57(7):3060–3066. doi: 10.1128/AAC.00431-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Red book Online. Ann Arbor, Michigan: Truven Health Analytics; Accessed July 14, 2014. [Google Scholar]
- 22. ClinicalTrials.gov. TR-701 FA vs linezolid for the treatment of nosocomial pneumonia [July 13, 2014]. Available at: http://clinicaltrials.gov/ct2/show/NCT02019420?term=tr-701&rank=7. Accessed July 14, 2014.


