Abstract
Background
Mindfulness has been identified as a promising strategy for managing cravings for alcohol and other drugs, but little controlled experimental research has directly studied whether this approach is effective. The current study systematically examined the effects of an acute mindfulness manipulation on craving for alcohol during prolonged exposure to alcohol cues.
Method
Heavy drinkers (N = 84; 50% male) underwent a prolonged alcohol cue exposure paradigm in a simulated bar environment and received either a mindfulness-based strategy, a distraction-based strategy (active control), or no strategy (passive control) to cope with alcohol cravings and discomfort associated with craving.
Results
No baseline differences were present between conditions, manipulation checks revealed that participants in the two active conditions reported employing the recommended strategies, and the initial exposure to alcohol cues was associated with significant increases in craving, urge distress, and heart rate. Mixed ANOVAs on these indices following the experimental manipulation revealed significant differences based on condition over the course of the bar laboratory protocol. The distraction strategy was significantly more effective at acutely reducing craving and urge distress than the other two conditions, which did not significantly differ from each other.
Conclusions
Contrary to our prediction, these findings suggest that an acute distraction strategy is beneficial for coping with alcohol cravings. The potential importance of protracted mindfulness training to detect significant effects on in vivo craving, additional implications, and methodological considerations are discussed.
Keywords: alcohol, mindfulness, craving, cue exposure, extinction
Introduction
Alcohol use disorders (AUDs) remain a major public health problem. Recent estimates suggest that 30% of adults in the United States will meet criteria for an AUD during their lifetimes (Hasin et al., 2007). For many individuals struggling with AUDs, craving, or a persistent desire for alcohol, is a common phenomenon (Chakravorty et al., 2010; Yoon et al., 2006). Cravings are theorized to maintain problematic drinking and this has been supported by numerous empirical studies (Bottlender and Soyka, 2004; Flannery et al., 1999; Oslin et al., 2009).
One technique thought to help individuals endure craving and other intense experiential states is mindfulness. Mindfulness is described as a “non-judgmental observation of the ongoing stream of internal and external stimuli as they arise” (Baer, 2003, p. 125). Two key components of mindfulness involve regulating attention by fostering awareness of sensations, thoughts, and feelings, and choosing to adopt an orientation of openness and acceptance towards these experiences (Keng et al., 2011; Bishop et al., 2004). Interventions featuring a mindfulness component have become increasingly more common in psychological treatment (for reviews, see Keng et al., 2011; Zgierska et al., 2009). Although numerous differences between mindfulness interventions exist, the underlying goal often involves helping individuals frame experiential states in a more objective and less distressing way.
In reference to AUDs and other addictive disorders, individuals can be taught to use mindfulness skills in order to increase awareness and tolerability of craving and to decrease automatic habitual responses (Witkiewitz et al., 2005). The idea of objectively experiencing urges without acting on them has given rise to the phrase “urge surfing,” in which cravings are conceptualized like waves in the ocean and individuals are encouraged to “surf the urge by allowing it to pass without being wiped out by giving into it” (Marlatt, 2002, p. 47). An emphasis is placed on developing new and more accepting attitudes towards craving and learning to view it as a mental event instead of an attribute of the self. The ability to monitoring one's experiences in a detached way is thought to decrease reactive behavior, thereby allowing craving that is not reflexively followed by alcohol use.
A growing number of studies have investigated the relationship between alcohol misuse, mindfulness, treatment, and recovery. Several survey-based studies using nonclinical samples have suggested that higher levels of mindfulness are associated with lower levels of adverse alcohol-related consequences such as blackouts and alcohol-related injuries (Murphy and MacKillop, 2012; Fernandez et al., 2010). Clinical research has investigated the effects of various mindfulness-based treatments with mixed findings. Several studies have found positive treatment effects of mindfulness interventions including reduced quantity and frequency of drinking and drug use (Bowen et al., 2006), increased acceptance and acting with awareness and decreasing craving and alcohol use (Bowen et al., 2009), and decreased dysregulated behavioral tendencies such as drinking and acting aggressively (Wupperman et al., 2012). In contrast to these findings, a number of studies have not reported significant positive effects of mindfulness interventions including no significant decrease in craving for alcohol or abstention (Garland at al., 2010; Zgierska et al., 2008), no significant decrease in substance use (Bootzin and Stevens, 2005), and a lack of enhanced treatment outcomes for substance abuse patients (Alterman et al., 2004).
Taken together, although a mindfulness-based approach may have promise in the treatment of addictive disorders, to date, the findings have been mixed and there is considerable ambiguity in the literature. Laboratory research is critical for clarifying in vivo effects and mechanisms of an intervention under controlled conditions, both to establish those effects and to optimize the intervention's use in clinical research and practice. In the context of mindfulness interventions for addictive disorders, several relevant functional variables may be affected by the use of acute mindfulness-based coping skills including craving, distress associated with urges to drink, and overall mood. There is evidence that negative mood generally accompanies acute craving (MacKillop, 2006; Rohsenow et al., 1992) and, since mindfulness interventions emphasize an orientation of openness and acceptance towards what is experienced, it may be that adopting such a perspective allows craving to be perceived as less unpleasant and/or distressing (Witkiewitz et al., 2005; Bishop et al., 2004).
The goal of the current study was to conduct a laboratory investigation of the effects of a mindfulness strategy on acute craving for alcohol to examine its ability to acutely reduce craving, and to elucidate the domains in which the intervention was primarily exerting its effects. Specifically, the effects of mindfulness on craving were examined in the context of established alcohol cue reactivity and extinction paradigms. Exposure to personalized alcohol cues is very well established to elicit an acute increase in craving for alcohol that gradually dissipates over time (Carter and Tiffany, 1999; MacKillop and Lisman, 2007, 2008; Staiger and White, 1991). Therefore, this study attempted to use this paradigm to evoke craving for alcohol and then test the use of acute mindfulness-based coping skills in individuals with a demonstrable urge to drink. To control for the various aspects of the mindfulness strategy (MND), two control conditions were used. The first was an active control condition that included parallel procedural elements of the MND condition but utilized an antithetical distraction strategy (DST) of diverting one's attention when experiencing a craving. The second was a passive control condition (CTL) that included an identical protocol but with no explicit strategy to use to cope with cravings. The study had two primary hypotheses. First, the MND condition was predicted to augment the decay in craving over the extinction period compared to both control groups. Second, the MND condition was predicted to facilitate a reduction in craving-related distress (i.e., urge distress) over the extinction period compared to both control groups. A secondary goal was to conduct exploratory analyses in order to examine possible effects on mood and psychophysiological arousal.
Materials and Methods
Participants
Sample size was determined via an a priori power analysis with an estimated effect size of f = 0.35 using conventional power parameters (α = 0.05, β = 0.80). Participants (N = 84, 50% male) were recruited from the community via advertisements soliciting drinkers for a research study. Eligibility criteria included being an at-risk heavy drinker, defined as consuming >14/7 drinks/week for men/women (NIAAA, 2010) and scoring ≥8 on the Alcohol Use Disorders Identification Test (AUDIT; Babor et al., 1992); and being between 21-29 years of age. This age range was selected to minimize heterogeneity and to reflect those of legal drinking age who are most likely to be diagnosed with an AUD (Grant et al., 2004). Participants were primarily white (85%; Black, 6%; Asian, 6%, Pacific Islander 1%, Mixed Race 2%) and were, on average, 22.43 years-old (SD = 1.76), with 15.30 (SD = 1.56) years of education, and a median annual family income of $45,000-$60,000. Participants drank, on average, 24.59 (SD = 12.72) drinks/week and had a mean AUDIT score of 15.85 (SD=6.27). A criterion score of 8 has been validated as a cut-off, with 92% of individuals with hazardous or harmful alcohol use and 94% of those without falling above and below this criterion, respectively (Saunders et al., 1993). Thus, this sample reflects a group of individuals whose typical drinking patterns far exceed the suggested cut-off used to detect harmful and hazardous alcohol use.
Procedures
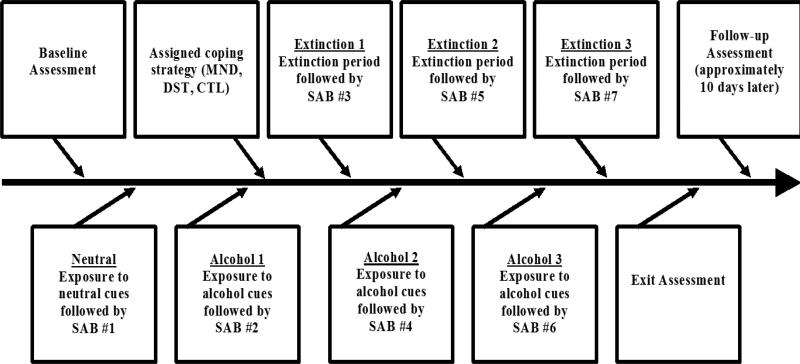
All procedures were approved by the affiliated university Institutional Review Board. Following a positive telephone screen, individuals attended an individual in-person session lasting 2.5 hours (Figure 1). After sobriety was confirmed via breathalyzer, participants underwent informed consent during which they were informed that the purpose of the study was to assess effects of different methods for coping with alcohol cravings. Following that, participants completed a 35- to 45-minute baseline assessment of descriptive and control variables. Participants then began the cue reactivity procedures, implemented via audio recordings and facilitated by research assistants blinded to condition. In each case, research assistants poured a beverage for participants and then asked them to listen to standardized audio recordings designed to utilize auditory, visual, olfactory, proprioceptive, and tactile cues (e.g., “pick up the drink...notice how the glass feels in your hand and the color of the beverage... take five deeps breaths, inhaling the smell of the drink with each breath”). Participants first were exposed to a neutral beverage (i.e., water) while listening to the cue exposure recording followed by the state assessment battery (SAB). Afterward, the participants were escorted to a simulated bar environment where this procedure was repeated using the individual's preferred alcoholic beverage. Subsequently, participants were block randomized by sex into the mindfulness strategy (MND), distraction strategy (DST), and control/no-strategy (CTL) groups.
Figure 1.
Study schematic of experimental procedure. SAB, State Battery Assessment.
While the cue exposure protocol was the same for both groups, each group was given unique instructions regarding how to address any cravings they experienced. The MND instruction set was adapted from a mindfulness-based smoking intervention (Bowen and Marlatt, 2009) and core mindfulness skills training in Dialectical Behavior Therapy (Linehan, 1993). Participants were asked to attend to their moment-to-moment experience, including any cravings that occurred, in an accepting and nonjudgmental fashion (e.g., “please pay close attention to whatever thoughts, sensations, or urges to drink you experience...you don't need to try to take your mind off of them or get rid of them...imagine that your mind is a conveyor belt and that thoughts and feelings are coming down the belt... relax and notice as they come and go”). Participants in the DST group were told that it was important that they tried to distract themselves from any thoughts about drinking and/or temptations to drink they might be experiencing. They were instructed to try to occupy their minds enough to be distracted from their urges and to focus their attention and interest on something else. Participants in the CTL group were informed that they would not be given specific recommendations on how to handle the cravings they experienced. They were told that they were free to use whatever strategy they wanted to address their cravings over the course of the session. Once the instructional strategy recordings finished, a four-minute extinction period in the bar environment began for all groups. During this time, participants sat alone at the bar with their alcoholic beverage, using their assigned coping strategies. After this interval, participants were asked to complete the SAB. This completed the first of three alcohol exposure-extinction intervals (Figure 1). In each instance, an alcohol beverage was poured for the participants. They listened to the cue exposure recording in order to elicit craving and were given suggestions for coping with alcohol-related thoughts, cravings, and urges they experienced according to group. Each time, an extinction period followed for participants to employ the strategy described as a means of managing acute cravings. Following each cue exposure and each extinction period, participants completed the SAB, completing it seven times in total (Figure 1). The procedure was repeated to ensure participants achieved full within-session extinction and to permit the observation of manipulation effects beyond only a single extinction period. The protocol in the simulated bar environment lasted approximately 45 minutes.
Once the bar lab protocol was complete, participants were escorted back to a neutral laboratory room and asked to fill out a brief exit assessment battery which included manipulation check questions and the DRSEQ. Afterward, they were debriefed and compensated for their time. During the debriefing, the exposure-extinction portion of the study was framed as intending to illustrate that an individual can refrain from drinking despite having an urge. Additionally, taking one's mind off wanting to drink (DST), allowing oneself to experience urges mindfully cognizant of the fact that they will naturally wax and wane (MND), and realizing that cravings extinguish with time (CTL) were highlighted according to group. Participants were encouraged to use this information to their advantage if they experienced any unwanted cravings for alcohol in their future. One week following the study, participants were contacted by telephone for a brief telephone assessment in which cravings for alcohol (PACS) and alcohol consumption (DDQ) during the interim period was assessed. The purpose of this assessment was to test whether learned coping strategies impacted cravings and, by extension, alcohol consumption outside of the laboratory context.
Measures
Descriptive and Control Variables
Demographics, individual characteristics, and alcohol involvement were assessed via questionnaires to establish baseline group equivalence. This included assessing weekly alcohol consumption using the Daily Drinking Questionnaire (DDQ; Collins et al., 1985), alcohol misuse using the Alcohol Use Disorders Identification Test (AUDIT; Babor et al., 1992), typical alcohol craving using the Penn Alcohol Craving Scale (PACS; Flannery et al., 1999), perceived capacity to resist drinking using the Drinking Refusal Self-Efficacy Questionnaire (DRSEQ-RA; Young et al., 2007), and mindfulness traits using the Five-Facet Mindfulness Questionnaire (FFMQ; Baer et al., 2006). As noted above, participants were asked to complete the PACS, DDQ, and DRSEQ on two occasions to assess potential changes in these variables.
State Assessment Battery (SAB)
Participants were asked to answer a series of self-report questions pertaining to the present moment. Craving for alcohol was assessed using an established 4-item 11-point (0-10) Likert-type state measure (Stasiewicz et al., 2007; Klein et al., 2007) which demonstrated excellent internal reliability at all assessments (αs = .98-.99). Associated distress from craving for alcohol (henceforth, urge distress) was assessed using a 3-item measure using the same scale and also demonstrating excellent internal consistency (αs = .93-.96). Items asked how annoying is not being able to drink, how much is your desire to drink bothering you, and how uncomfortable is your craving to drink. Mood was measured using an 8-item, 11-point questionnaire based on the affect circumplex (Posner et al., 2005), with four items assessing both positive (PA; happy, calm, excited, relaxed) and negative (NA: bored, sad, stressed, tense) affect. Two items (“excited,” “bored”) were dropped based on improved internal consistency following their exclusion; resulting PA αs =.63-.79, and resulting NA αs =.75-.83. Psychophysiological arousal was assessed as heart rate (HR) beats per minute using a commercially-available self-inflating wrist cuff (LifeSource©). HR was assessed immediately after participants completed self-report questionnaires with one sample taken during each SAB.
Manipulation checks
Two separate manipulation checks were used. During the SAB participants were asked the extent to which they were distracting themselves from their cravings and the extent to which they were observing and accepting their cravings using an 11-point Likert-type scale. Similarly, during the exit assessment, participants were asked questions assessing the extent to which they understood and followed the instructions including true/false (e.g., “the recording...asked me to accept my thoughts without judging them”) and Likert-scale (e.g., “I intentionally tried to distract myself from wanting to drink and was able to”) questions measured from 1 (strongly disagree) to 5 (strongly agree).
Data Analysis
Initial tests for outliers (Z>3.00) and normality distributions were conducted to ensure that all values were within the acceptable range. One outlier was detected for drinks/week and was recoded as one unit higher than the greatest non-outlying value to reduce leverage (Tabachnick and Fidell, 2006). One-way analyses of variance (ANOVAs) were conducted to establish group equivalence at baseline on drinks per week, craving, drink refusal self-efficacy, and mindfulness. One-way ANOVAs were also conducted to compare responses on manipulation check questions. Mixed ANOVAs were used to compare the groups on initial reactivity to alcohol cues to ensure equal responsiveness. Omnibus 2 × 3 mixed ANOVAs were used to compare the SAB following the initial alcohol exposure (alcohol exposure #1) to the final SAB (extinction #3), reflecting differences during the full period during which the different strategies were putatively operative. To minimize Type I error rate inflation, follow-up 2 × 3 mixed ANOVAs were conducted between adjacent time points only when differential responding by condition was evident in omnibus analyses. In addition to these primary analyses, a 2 (time) × 3 (group) mixed ANOVA was used to examine changes in drink-refusal self-efficacy (DRSE) over the course of the session. Finally, 2 × 3 mixed ANOVAs were conducted to compare baseline and follow-up levels craving and alcohol consumption. In each case, follow-up pairwise comparisons were conducted as necessary to clarify the nature of the significant effect.
Results
Preliminary Analyses
Baseline group comparisons revealed no significant differences between groups on age, education, drinks/week (DDQ), craving (PACS), trait-level mindfulness (FFMQ), and drink refusal self-efficacy (DRSEQ), all ps>0.05). Manipulation checks confirmed strategy understanding and adherence in the MND and DST groups (Table 1). Mixed ANOVAs comparing the three groups on initial reactivity to alcohol cues on the two primary dependent variables (craving and urge distress) and the three secondary dependent variables (PA, NA, HR) revealed significant effects of cues on craving, urge distress, and HR and no group × time interactions (Table 2).
Table 1.
One-way ANOVAs of Manipulation Check Questions
| M | D | C | F | p | |
|---|---|---|---|---|---|
| State Assessment Battery Questions | (0=Min/10=Max) | ||||
| How much are you noticing and accepting your urges to drink? | 7.4* | 4.0 | 5.3 | 11.8 | <.01 |
| How much are you distracting yourself from your urges to drink? | 2.3 | 6.2* | 4.1 | 15.7 | <.01 |
| Exit Assessment Questions - Understanding of Strategy | |||||
| During today's study I was asked... | (1=True/2=False) | ||||
| ...to pick up the drink in front of me | 1.0 | 1.0 | 1.0 | 1.0 | 0.37 |
| ...to notice how the glass feels in my hand and the color of the beverage | 1.0 | 1.0 | 1.0 | -- | -- |
| ...to inhale the smell of the drink | 1.0 | 1.0 | 1.0 | -- | -- |
| ...not to label or evaluate my thoughts as good or bad | 1.0* | 1.9 | 2.0 | 179.7 | <.01 |
| ...to accept my thoughts without judging them | 1.0* | 1.9 | 2.0 | 144.2 | <.01 |
| ...to allow craving, frustration, and discomfort to be present | 1.0* | 1.8 | 1.9 | 77.5 | <.01 |
| ...to distract myself in order to take my mind off drinking | 2.0 | 1.0* | 1.7 | 85.0 | <.01 |
| ...to try to make my urges to drink go away | 2.0 | 1.1* | 1.7 | 47.3 | <.01 |
| ...to find ways to distract myself | 2.0 | 1.0* | 1.6 | 68.2 | <.01 |
| Exit Assessment Questions - Strategy Adherence and Evaluation | (0=Min/10=Max) | ||||
| How difficult was the coping strategy described to you? | 4.4 | 3.0 | 2.4 | 3.5 | .04 |
| How useful was the coping strategy described to you? | 6.3 | 7.8* | 6.3 | 3.3 | .04 |
| Rate how much you agree with the following... | (1=Strongly Disagree/5=Strongly Agree) | ||||
| ...I was given a specific strategy to use to cope with cravings [today] | 4.4 | 3.9 | 1.3* | 95.3 | <.01 |
| ...Iused the strategy I was instructed to in order to cope with cravings | 4.2 | 4.3 | 2.8* | 17.1 | <.01 |
| ...Iintentionally tried to accept wanting to drink without [judgment]...and was able to | 4.3* | 3.5 | 3.0 | 13.3 | <.01 |
| ...I intentionally tried to distract myself from wanting to drink and was able to | 1.9 | 4.5* | 3.8 | 62.0 | <.01 |
| ...Based [on today], I think this strategy would be helpful to deal with [alcohol cravings] | 3.4 | 4.2* | 3.3 | 7.9 | <.01 |
Note. M = Mindfulness Group mean. D = Distraction Group mean. C =Control Group mean.
Follow-up tests indicate that group mean is significantly different than mean of both other groups.
Table 2.
Comparisons of Responses to Alcohol Cues Using 3 (Condition) × 2 (Time) Mixed ANOVAs
| Initial Reactivity to Alcohol Cues | ||||||
|---|---|---|---|---|---|---|
| Variable | Condition (C) | Time (T) | C × T | |||
| F | η 2 p | F | η 2 p | F | η 2 p | |
| Craving | 1.85 | .04 | 109.32*** | .57 | 1.40 | .03 |
| Urge Distress | .93 | .02 | 100.13*** | .55 | .84 | .02 |
| Heart Rate | .31 | .01 | 40.81** | .34 | .45 | .01 |
| Positive Affect | 2.16 | .05 | 2.46 | .03 | .34 | .01 |
| Negative Affect | 1.08 | .03 | 2.28 | .03 | 1.51 | .04 |
| Changes Across the Bar Lab Protocol | ||||||
|---|---|---|---|---|---|---|
| Variable | Condition (C) | Time (T) | C × T | |||
| F | η 2 p | F | η 2 p | F | η 2 p | |
| Craving | 6.52** | .14 | 38.84*** | .32 | 10.62*** | .21 |
| Urge Distress | 1.95 | .05 | 34.50*** | .30 | 6.51** | .14 |
| Heart Rate | .24 | .01 | 11.47** | .12 | .15 | .00 |
Note.
* = p ≤ 0.05
= p ≤ 0.01
= p ≤ 0.001
Strategy Effects on Acute Motivation for Alcohol
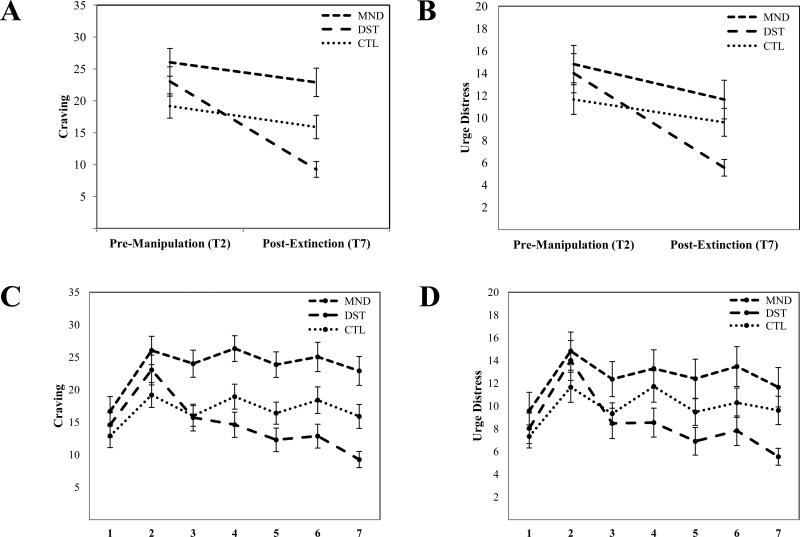
Mixed ANOVAs for dependent variables significantly affected by alcohol cues in preliminary analyses (i.e., craving, urge distress, and HR) are presented in Table 2. Means and standard errors across the omnibus comparisons are presented in Figure 2 (Panels A and B). A significant group × time interaction was present for craving in omnibus analyses indicating differential responding by condition. Follow-up mixed ANOVAs of adjacent time points (Table 3) on craving revealed significant condition × time interaction effects during two time points (Figure 2 Panel C). Following the first extinction period, there was a significant interaction in which the DST group had a greater decrease in craving than the other groups. There was also a significant interaction during the subsequent cue exposure, in which only the DST did not report a significant increase in craving. For the remaining cue exposure and extinction periods, significant interactions were not present. When considering urge distress, a similar pattern was evident. A significant group × time interaction was present in the omnibus ANOVA (Table 2) with the DST group demonstrating a steeper decrease in urge distress over the course of the protocol (Figure 2 Panel B). Follow-up examinations of adjacent time-points revealed that the DST had a greater decrease in urge distress during the initial extinction period when compared to the other groups as well as a trend toward a condition × time interaction (p = .06) following the second presentation of alcohol cues. For the remaining cue exposure and extinction periods, significant interactions were not present. A significant effect of time was present for HR, reflecting a decrease in heart rate over the course of the bar lab protocol (HR following alcohol exposure #1: M = 75.61 [SEM = 1.40]; HR following extinction #3: M = 72. 94 [SEM = 1.25]), but no condition × time interaction was present in the omnibus analysis.
Figure 2.
Effects of mindfulness, distraction, and no strategy on subjective craving for alcohol and urge distress. Panels A and B depict the omnibus 3 (condition: MND, DST, CTL) 9 2 (time: prior tomanipulation of coping strategy and at the end of the experimental period). Panels C and D show full-resolution depictions of each group at all time points across the protocol (statistical significance for changes presented in Tables 1 and 2). Neutral cues were presented at time point 1, alcohol cues were acutely presented at time points 2, 4, and 6, and unreinforced exposure to alcohol cues (extinction) took place at time points 3, 5, and 7.MND, mindfulness group; DST, distraction group; CTL, control group; T, time point.
Table 3.
Mixed ANOVAs for Primary Dependent Variables Using 3 (group) × 2 (time) Mixed ANOVAs of Adjacent Time Points
| Period | Time points (Figure 2) | Condition | Time | C × T | |||
|---|---|---|---|---|---|---|---|
| F | η 2 p | F | η 2 p | F | η 2 p | ||
| Craving | |||||||
| EXT #1 | 2 vs. 3 | 4.02* | .09 | 35.16*** | .30 | 5.14** | .11 |
| CUES#2 | 3 vs. 4 | 7.83*** | .16 | 5.95* | .07 | .90** | .11 |
| EXT#2 | 4 vs. 5 | 10.22*** | .20 | 25.30*** | .24 | .02 | .00 |
| CUES #3 | 5 vs. 6 | 9.88*** | .20 | 6.64* | .08 | .73 | .02 |
| EXT#3 | 6 vs. 7 | 12.29*** | .23 | 15.80*** | .16 | .41 | .01 |
| Urge Distress | |||||||
|---|---|---|---|---|---|---|---|
| EXT #1 | 2 vs. 3 | 1.38 | .03 | 41.05*** | .34 | 3.81* | .09 |
| CUES #2 | 3 vs. 4 | 2.65 | .06 | 8.16** | .09 | 2.93 | .07 |
| EXT#2 | 4 vs. 5 | 3.42* | .08 | 24.94*** | .24 | 1.51 | .04 |
| CUES #3 | 5 vs. 6 | 3.98* | .09 | 8.38** | .09 | .05 | .00 |
| EXT#3 | 6 vs. 7 | 4.96** | .11 | 10.97** | .12 | .98 | .02 |
Note. EXT = extinction period, CUES = alcohol cue exposure period
= p ≤ 0.05
= p ≤ 0.01
= p ≤ 0.001
Exit and Follow-up Analyses
During the exit assessment, individuals were asked several questions regarding their perceptions of the various coping strategies employed (Table 1). Although results of the one-way ANOVA indicated a significant difference in perceived difficulty of the strategies, pairwise comparisons revealed that this reflected low levels of difficulty reported by individuals in the CTL group who had not been given any explicit strategy, with the means of MND and DST groups not being significantly different t(54) = 1.81, p = .08. When participants were asked how useful the coping strategies described to them were, results of one-way ANOVA again revealed significant differences (Table 1) and pairwise comparisons suggested individuals in the DST group found their strategy to be more beneficial during the session than did individuals in the MND group, t(54) = −3.08, p < .01. Correspondingly, significant group differences were detected when individuals were asked whether they thought the strategy employed would be a helpful tool to manage cravings (Table 1). Again, individuals in the DST group reported stronger support for their strategy than was reported in the mindfulness condition, t(54) = −3.30, p < .01.
Also during the exit assessment, individuals were assess to explore whether aspects of the experimental manipulation (i.e., experiencing a craving while in the presence of alcohol cues but using a given technique rather than drinking) had influenced their perceived ability to resist drinking in various situations (e.g., when offered a drink, when frustrated). A mixed ANOVA comparing baseline and exit DRSEQ scores, showed a significant increase in drink refusal self-efficacy for all groups over the course of the session, F (2, 81) = 4.63, p = .03, but there was not a significant group × time interaction.
The follow-up telephone assessment was completed by a majority of participants (81%, n = 68) with no significant completion differences by group, χ2 (2) = 1.08, p = .59. Comparing baseline levels of craving and number of drinks/week to those reported during the telephone follow-up revealed a significant effect of time with participants reporting lower levels of craving, F (1, 65) = 6.82, p = .01, and fewer drinks/week, F (1, 65) = 25.63, p < .01, than initially reported. This was the case across conditions and group × time interactions were not present.
Discussion
The goal of the current study was to conduct a laboratory investigation of the effects of a mindfulness strategy on acute craving for alcohol. A comparative design was employed in which a mindfulness strategy was predicted to be superior to both an alternate strategy and no strategy at reducing acute desire to drink and associated urge-related distress. Contrary to predictions, however, the MND strategy was not significantly better at reducing desire to drink or distress caused by urges. Instead, individuals in the DST group exhibited significantly more successful craving management compared to both the MND and CTL groups. Over the course of the session, the DST group reported decreases in desire to drink and distress from urges that were nearly triple what was reported in the MND or CTL groups. These differences were most pronounced early in the session with the DST group demonstrating greater extinction to the effects of alcohol cues as well as decreased reactivity to them. The similar pattern of findings across craving and urge distress provide greater confidence in the differences in strategy effects.
Although the experimental procedures were found to influence experiential craving and resulting distress, similar effects were not demonstrated when considering physiological arousal and mood. Overall levels of positive and negative affect did not fluctuate considerably during the session and there was not a significant change in PA or NA in response to alcohol cues. Although participants reported fluctuations in how annoying and uncomfortable their desire to drink was, as measured by urge distress, this appeared to be largely independent of global mood states. In other words, participants endorsed that their cravings made them feel increasingly uncomfortable without a commensurate change in general happiness or sadness. Accordingly, this study provides support for urge distress as a novel index of motivation for alcohol and suggests that mood-ratings may not fully capture the extent to which urges to drink are experienced as unpleasant and distressing. Unlike PA and NA, there was a significant elevation in HR in response to alcohol cues. Nonetheless, assigned coping strategies did not differentially impact psychophysiological arousal over the course of the session. Instead, HR quickly returned to levels experienced prior to exposure to alcohol cues. This decrease likely reflected an adaptive, physiological response following the presentation of a novel stimulus that was facilitated by coping techniques, regardless of type.
In addition to the effects on primary and secondary dependent variables, there were several additional effects of note. Following the alcohol extinction protocol, individuals reported greater confidence in their ability to resist having a drink in a variety of high-risk situations. This finding was independent of group assignment. Thus, deliberately refraining from drinking despite active cravings appears to have fostered participants’ insight into their ability to do so, resulting in increased drink refusal self-efficacy. Similarly, when contacted one week after participation in the laboratory session, participants reported lower levels of craving and reduced alcohol consumption. This was also regardless of group status, suggesting that participating in the extended cue exposure and extinction session had a positive impact on subsequent alcohol craving and consumption irrespective of strategy.
Although interest in using mindfulness in the treatment of addictive behavior has burgeoned, the results of this study did not indicate that applying mindfulness techniques to acute cravings was effective at reducing craving or in changing the way in which craving is experienced. This converges with research demonstrating that mindfulness and acceptance-based strategies to reduce acute craving for cigarettes were not superior to a control condition (Bowen and Marlatt, 2009), to a strategy involving ignoring thoughts (Rogojanski et al., 2011), or to a strategy involving suppressing thoughts of smoking (Litvin et al., 2012). Thus, results of the present study seem to replicate similar recent findings that suggest acute mindfulness-based strategies may not be particularly effective at reducing acute drug cravings. Rather than MND strategy being the most effective of those employed in the present study, the DST strategy, which consisted of recommendations that were behavioral (e.g., do something else) and cognitive (e.g., think about something else) in nature, was found to be superior. Although the DST condition was selected to serve as an active control condition for the purposes of the current study, the positive DST findings converge with previous research suggesting that diverting attention and distracting oneself are likely to facilitate the ability to withstand temptation (Peake et al., 2002). Furthermore, these findings are consistent with two studies on smoking using active behavioral strategies to reduce substance consumption. One study demonstrated that “keeping busy” was a strategy frequently endorsed by individuals who had successful stopped smoking cigarettes (Richter et al., 2002). In another study, cigarette smokers who practiced a distracting activity (i.e., seated isometric exercises such as fist clenching) while experiencing a desire to smoke had statistically significant reductions in craving immediately following an experimental manipulation and after a delay (Ussher et al., 2006). Applying this approach for managing alcohol cravings is a promising future direction to verify extend the current findings and research modifying parametric aspects of the distraction condition (e.g., having participants complete particular distraction tasks) may be beneficial to this end.
As this is one of the first laboratory studies to examine the effects of a mindfulness-based coping strategy on acute cravings for alcohol, the current findings should be considered in the context of the study's strengths and limitations. Among the strengths, this study was appropriately powered to detect effects, the manipulation checks supported the internal validity of the independent variables, and acute motivation for alcohol was assessed using a multidimensional approach. There were also several limitations. First, this study did not involve an alcohol self-administration component. As such, it is unclear whether the changes in craving and distress from craving reported would have translated into actual differences in consumption. Second, the modality used to collect data during the follow-up telephone assessment (i.e., interview) was different than the one used during the laboratory session (i.e., self-report questionnaire) and it is possible that differences in assessment modality may have influenced responding. Finally, the coping strategy manipulations in this study were acute in nature and did not involve extensive practice, which may be required for successfully using mindfulness to cope with cravings. Although the MND strategy was not reported to be more difficult than the DST strategy, like many skills, mastery of mindfulness techniques may require repetition and practice in order to yield skillful and effective implementation. This is, however, an empirical question and one that will be important to address in future studies.
In addition to these limitations, several other considerations deserve mentioning. First, this study used alcohol cues as a way to elicit the cravings to which coping strategies were subsequently applied. It is possible that results may vary given different study parameters such as applying given techniques to other types of craving (e.g., stress-elicited, withdrawal-elicited). Second, it is important to acknowledge the possibility of demand characteristics influencing participants’ responding. Although the groups were given different strategies regarding how they were to interact with any cravings that they experienced, all participants were instructed that the study was investigating how well “different strategies work to handle cravings for alcohol.” Therefore, all participants had identical information regarding what was expected of them with regard to study aims and objectives. In addition, neither participants nor experimenters had knowledge of specific hypotheses (e.g., the superiority of one strategy over another). Therefore, differences reported during the experimental manipulation (e.g., significantly lower levels of craving and urge distress reported by individuals in the DST group) and during the exit assessment (e.g., significantly higher levels of support for the usefulness of the given strategy and its ability to be a helpful tool to manage cravings reported by individuals in the DST group) are unlikely to be the result of participant's having different perceptions of what was expected of them. Another consideration is the nature of the sample. Even though participants were at-risk heavy drinkers, they were not actively seeking treatment, so caution should be taken when generalizing these findings to treatment-seeking populations. It is important not to overgeneralize these findings, but this study echoes concerns that empirical research has not provided unequivocal support for the effectiveness of mindfulness for substance abuse (Appel and Kim-Appel, 2009). Methodologically rigorous research continues to be needed to understand what components of mindfulness, if any, effectively aid the management of acute cravings for alcohol and other addictive drugs.
Acknowledgments
We are grateful to several members of the Experimental and Clinical Psychology Laboratory who assisted in conducting experimental sessions including Jared Bollinger, Evelyn French, Griffin Sheats, Alex Rothbaum, Melanie Nembhard, Christy Hall, and Shannon Ritter. This work was partially supported by a grant from the National Institutes of Health (K23 AA016936; JM)
Contributor Information
Cara M. Murphy, Department of Psychology, University of Georgia
James MacKillop, Department of Psychology, University of Georgia; Department of Behavioral and Social Sciences, Brown University.
Reference List
- Alterman AI, Koppenhaver JM, Mulholland E, Ladden LJ, Baime MJ. Pilot trial of effectiveness of mindfulness meditation for substance abuse patients. Journal of Substance Use. 2004;9(6):259–268. doi:10.1080/14659890410001711698. [Google Scholar]
- Appel J, Kim-Appel D. Mindfulness: Implications for substance abuse and addiction. International Journal of Mental Health and Addiction. 2009;7(4):506–512. doi:10.1007/s11469-009-9199-z. [Google Scholar]
- Babor TF, De La Fuente JR, Saunders J, Grant M. The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Health Care. World Health Organization; Geneva, Switzerland: 1992. [Google Scholar]
- Baer RA. Mindfulness training as a clinical intervention: A conceptual and empirical review. Clinical Psychology-Science and Practice. 2003;10(2):125–143. doi:10.1093/clipsy.bpg015. [Google Scholar]
- Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. doi:10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- Bishop SR, Lau M, Shapiro S, Carlson L, Anderson ND, Carmody J, Zindel ZV, Abbey S, Speca M, Velting D, Gerald D. Mindfulness: A proposed operational definition. Clinical Psychology-Science and Practice. 2004;11(3):230–241. doi:10.1093/clipsy.bph077. [Google Scholar]
- Bootzin RR, Stevens SJ. Adolescents, substance abuse, and the treatment of insomnia and daytime sleepiness. Clinical Psychology Review. 2005;25:629–644. doi: 10.1016/j.cpr.2005.04.007. doi:10.1016/j.cpr.2005.04.007. [DOI] [PubMed] [Google Scholar]
- Bottlender M, Soyka M. Impact of craving on alcohol relapse during, and 12 months following, outpatient treatment. Alcohol and Alcoholism. 2004;39:357–361. doi: 10.1093/alcalc/agh073. doi:10.1093/alcalc/agh073. [DOI] [PubMed] [Google Scholar]
- Bowen S, Chawla N, Collins SE, Witkiewitz K, Hsu S, Grow J, Clifasefi S, Garner M, Douglass A, Larimer ME, Marlatt A. Mindfulness-based relapse prevention for substance use disorders: A pilot efficacy trial. Substance Abuse. 2009;30(4):295–305. doi: 10.1080/08897070903250084. doi:10.1080/08897070903250084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowen S, Marlatt A. Surfing the urge: Brief mindfulness-based intervention for college student smokers. Psychology of Addictive Behaviors. 2009;23(4):666–671. doi: 10.1037/a0017127. doi:10.1037/a0017127. [DOI] [PubMed] [Google Scholar]
- Bowen S, Witkiewitz K, Dillworth TM, Chawla N, Simpson TL, Ostafin BD, Larimer ME, Blume AW, Parks GA, Marlatt GA. Mindfulness meditation and substance use in an incarcerated population. Psychology of Addictive Behaviors. 2006;20(3):343–347. doi: 10.1037/0893-164X.20.3.343. doi:10.1037/0893-164X.20.3.343. [DOI] [PubMed] [Google Scholar]
- Carter BL, Tiffany ST. Meta-analysis of cue-reactivity in addiction research. Addiction. 1999;94(3):327–340. doi:10.1046/j.1360-0443.1999.9433273.x. [PubMed] [Google Scholar]
- Chakravorty S, Kuna ST, Zaharakis N, O'Brien CP, Kampman KM, Oslin D. Covariates of craving in actively drinking alcoholics. American Journal on Addictions. 2010;19(5):450–457. doi: 10.1111/j.1521-0391.2010.00067.x. doi:10.1111/j.1521-0391.2010.00067.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collins RL, Parks GA, Marlatt GA. Social determinants of alcohol consumption: The effects of social interaction and model status on the self-administration of alcohol. Journal of Consulting and Clinical Psychology. 1985;53(2):189–200. doi: 10.1037//0022-006x.53.2.189. doi:10.1037/0022-006X.53.2.189. [DOI] [PubMed] [Google Scholar]
- Fernandez AC, Wood MD, Stein LR, Rossi JS. Measuring mindfulness and examining its relationship with alcohol use and negative consequences. Psychology of Addictive Behaviors. 2010;24(4):608–616. doi: 10.1037/a0021742. doi:10.1037/a0021742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flannery BA, Volpicelli JR, Pettinati HM. Psychometric properties of the Penn Alcohol Craving Scale. Alcoholism: Clinical and Experimental Research. 1999;23(8):1289–1295. doi:10.1111/j.1530-0277.1999.tb04349.x. [PubMed] [Google Scholar]
- Garland EL, Gaylord SA, Boettiger CA, Howard MO. Mindfulness training modifies cognitive, affective, and physiological mechanisms implicated in alcohol dependence: Results of a randomized controlled pilot trial. Journal of Psychoactive Drugs. 2010;42(2):177–192. doi: 10.1080/02791072.2010.10400690. doi:10.1080/02791072.2010.10400690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug and Alcohol Dependence. 2004;74(3):223–234. doi: 10.1016/j.drugalcdep.2004.02.004. doi:10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Stinson FS, Ogburn E, Grant BF. Prevalence, correlates, disability, and comorbidity of DSM-IV alcohol abuse and dependence in the United States - Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Archives of General Psychiatry. 2007;64(7):830–842. doi: 10.1001/archpsyc.64.7.830. doi:10.1001/archpsyc.64.7.830. [DOI] [PubMed] [Google Scholar]
- Keng SL, Smoski MJ, Robins CJ. Effects of mindfulness on psychological health: A review of empirical studies. Clinical Psychology Review. 2011;31(6):1041–1056. doi: 10.1016/j.cpr.2011.04.006. doi:10.1016/j.cpr.2011.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klein AA, Stasiewicz PR, Koutsky JR, Bradizza CM, Coffey SF. A psychometric evaluation of the Approach and Avoidance of Alcohol Questionnaire (AAAQ) in alcohol dependent outpatients. Journal of Psychopathology and Behavioral Assessment. 2007;29(4):231–240. doi:10.1007/s10862-007-9044-2. [Google Scholar]
- Linehan MM. Skills training manual for treating borderline personality disorder. Guilford Press; New York, NY US: 1993. [Google Scholar]
- Litvin EB, Kovacs MA, Hayes PL, Brandon TH. Responding to tobacco craving: Experimental test of acceptance versus suppression. Psychology of Addictive Behaviors. 2012;26(4):830–837. doi: 10.1037/a0030351. doi:10.1037/a0030351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacKillop J. Factor structure of the alcohol urge questionnaire under neutral conditions and during a cue-elicited urge state. Alcoholism: Clinical and Experimental Research. 2006;30(8):1315–1321. doi: 10.1111/j.1530-0277.2006.00159.x. doi:10.1111/j.1530-0277.2006.00159.x. [DOI] [PubMed] [Google Scholar]
- MacKillop J, Lisman SA. Examining the effect of perceived availability on craving for alcohol: A quasi-experimental approach. Addiction Research & Theory. 2007;15(3):231–245. doi:10.1080/16066350701407104. [Google Scholar]
- MacKillop J, Lisman SA. Effects of a context shift and multiple context extinction on reactivity to alcohol cues. Experimental and Clinical Psychopharmacology. 2008;16(4):322–331. doi: 10.1037/a0012686. doi:10.1037/a0012686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marlatt GA. Buddhist philosophy and the treatment of addictive behavior. Cognitive and Behavioral Practice. 2002;9(1):44–49. doi:10.1016/S1077-7229(02)80039-6. [Google Scholar]
- Murphy CM, MacKillop J. Living in the here and now: Interrelationships between impulsivity, mindfulness, and alcohol misuse. Psychopharmacology. 2012;219(2):527–536. doi: 10.1007/s00213-011-2573-0. doi:10.1007/s00213-011-2573-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA), National Institutes of Health (NIH). U.S. Department of Health and Human Services Rethinking drinking: Alcohol and your health. 2010 (NIH Publication No. 10-3770) [Google Scholar]
- Oslin DW, Cary M, Slaymaker V, Colleran C, Blow FC. Daily ratings measures of alcohol craving during an inpatient stay define subtypes of alcohol addiction that predict subsequent risk for resumption of drinking. Drug and Alcohol Dependence. 2009;103(3):131–136. doi: 10.1016/j.drugalcdep.2009.03.009. doi:10.1016/j.drugalcdep.2009.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peake PK, Hebl M, Mischel W. Strategic attention deployment for delay of gratification in working and waiting situations. Developmental Psychology. 2002;38(2):313–326. doi: 10.1037//0012-1649.38.2.313. doi:10.1037/0012-1649.38.2.313. [DOI] [PubMed] [Google Scholar]
- Posner J, Russell JA, Peterson BS. The circumplex model of affect: An integrative approach to affective neuroscience, cognitive development, and psychopathology. Development and Psychopathology. 2005;17(3):715–734. doi: 10.1017/S0954579405050340. doi:10.1017/S0954579405050340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Richter K, McCool RM, Okuyemi KS, Mayo MS, Ahluwalia JS. Patients’ views on smoking cessation and tobacco harm reduction during drug treatment. Nicotine & Tobacco Research. 2002;4(Suppl. 2):S175–S182. doi: 10.1080/1462220021000032735. doi:10.1080/1462220021000032735. [DOI] [PubMed] [Google Scholar]
- Rogojanski J, Vettese LC, Antony MM. Coping with cigarette cravings: Comparison of suppression versus mindfulness-based strategies. Mindfulness. 2011;2(1):14–26. doi:10.1007/s12671-010-0038-x. [Google Scholar]
- Rohsenow DJ, Monti PM, Abrams DB, Rubonis AV. Cue elicited urge to drink and salivation in alcoholics: Relationship to individual differences. Advances in Behaviour Research & Therapy. 1992;14(3):195–210. doi:10.1016/0146-6402(92)90008-C. [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption: II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. doi:10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Staiger PK, White JM. Cue reactivity in alcohol abusers: Stimulus specificity and extinction of the responses. Addictive Behaviors. 1991;16(5):211–221. doi: 10.1016/0306-4603(91)90014-9. doi:10.1016/0306-4603(91)90014-9. [DOI] [PubMed] [Google Scholar]
- Stasiewicz PR, Brandon TH, Bradizza CM. Effects of extinction context and retrieval cues on renewal of alcohol-cue reactivity among alcohol-dependent outpatients. Psychology of Addictive Behaviors. 2007;21(2):244–248. doi: 10.1037/0893-164X.21.2.244. doi:10.1037/0893-164X.21.2.244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using Multivariate Statistics. 5th ed. Allyn & Bacon; Needham Heights, MA.: 2006. [Google Scholar]
- Ussher M, Cropley M, Playle SL, Mohidin R, West R. Effects of isometric exercise and body scanning on cigarette cravings and withdrawal symptoms. Addiction. 2009;104:1251–1257. doi: 10.1111/j.1360-0443.2009.02605.x. doi:10.1111/j.1360-0443.2009.02605.x. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA, Walker D. Mindfulness-Based Relapse Prevention for alcohol and substance use disorders. Journal of Cognitive Psychotherapy. 2005;19(3):211–228. doi:10.1891/jcop.2005.19.3.211. [Google Scholar]
- Wupperman P, Marlatt GA, Cunningham A, Bowen S, Berking M, Mulvihill-Rivera N, Easton C. Mindfulness and modification therapy for behavioral dysregulation: Results from a pilot study targeting alcohol use and aggression in women. Journal of Clinical Psychology. 2012;68(1):50–66. doi: 10.1002/jclp.20830. doi:10.1002/jclp.20830. [DOI] [PubMed] [Google Scholar]
- Yoon G, Kim SW, Thuras P, Grant JE, Westermeyer J. Alcohol craving in outpatients with alcohol dependence: rate and clinical correlates. Journal of Studies on Alcohol. 2006;67:770–777. doi: 10.15288/jsa.2006.67.770. [DOI] [PubMed] [Google Scholar]
- Young RM, Hasking P, Oeie TPS, Loveday W. Validation of the Drinking Refusal Self-Efficacy Questionnaire -- Revised in an adolescent sample (DRSEQ-RA). Addictive Behaviors. 2007;32(4):862–868. doi: 10.1016/j.addbeh.2006.07.001. doi:10.1016/j.addbeh.2006.07.001. [DOI] [PubMed] [Google Scholar]
- Zgierska A, Rabago D, Chawla N, Kushner K, Koehler R, Marlatt GA. Mindfulness meditation for substance use disorders: A systematic review. Substance Abuse. 2009;30:266–294. doi: 10.1080/08897070903250019. doi:10.1080/08897070903250019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zgierska A, Rabago D, Zuelsdorff M, Coe C, Miller M, Fleming M. Mindfulness meditation for alcohol relapse prevention: A feasibility pilot study. Journal of Addiction Medicine. 2008;2(3):165–173. doi: 10.1097/ADM.0b013e31816f8546. doi:10.1097/ADM.0b013e31816f8546. [DOI] [PMC free article] [PubMed] [Google Scholar]