Abstract
Physical activity (PA) has documented health benefits, but older Latinos are less likely to engage in leisure time PA than older non-Latino whites. Dance holds promise as a culturally appropriate form of PA that challenges individuals physically and cognitively. This paper describes a randomized controlled trial that will test the efficacy of BAILAMOS©, a 4-month Latin dance program followed by a 4-month maintenance program, for improving lifestyle PA and health outcomes. Older adults (n = 332), aged 55+, Latino/Hispanic, Spanish speaking, with low PA levels, and at risk for disability will be randomized to one of two programs, a dance program or health education control group. BAILAMOS© is a 4-month program that meets two times per week for one hour per session. Dance sessions focus on instruction, including four styles of dance, and couples dancing. Bi-monthly “Fiestas de Baile” (dance parties) are also included, in which participants dance and practice what they have learned.. Monthly 1-hour discussion sessions utilize a Social Cognitive framework and focus on knowledge, social support, and self-efficacy to increase lifestyle PA. The health education control group will meet one time per week for two hours per session. Primary outcomes including PA changes and secondary outcomes including self-efficacy, physical function, cognitive function, and disability will be assessed at baseline, 4, and 8 months. It is hypothesized that PA, self-efficacy, physical function, cognitive function, and functional limitations and disability scores will be significantly better in the BAILAMOS© group at 4 and 8 months compared to the control group.
Keywords: Physical activity, Latin Dance, Latino, Aging, Older adults
1. Introduction and background
By 2050, 20% of the older population in the U.S. will be comprised of Latinos [1]. Unfortunately, the health of many older Latinos is poor, as Latinos have a high prevalence of chronic diseases including diabetes [2]. Latinos also have twice the incidence of Alzheimer’s disease (AD) [3] compared to non-Latino whites; and are more likely than non-Latino whites to use an assistive device [4]. Participation in regular physical activity (PA) is one means to mitigate risks for these outcomes [5]. However, Latinos have the lowest leisure time PA rates among ethnic/racial groups [6–8]; and many older Latinos do not have a history of engaging in traditional exercise like jogging or going to a gym to run on treadmill, to lift weights, etc. [9].
Although evidence demonstrates that PA has a protective effect against disability [10], PA in the form of structured exercise is not considered age-appropriate by many older Latinos, who believe exercising is for young people [11]. Dancing and walking have been cited as the only age-appropriate PA for older Latina women [9]; and they have been the most commonly reported forms of PA among older Latinos [12]. Older Latinos value functional independence, and relate physical fitness to feeling healthy and being able to perform activities with ease [11]. However, this understanding has not led to their adoption and maintenance of PA. Thus, testing innovative methods that can increase PA adoption and maintenance along with their attendant physical and cognitive outcomes remains a pressing issue.
Dance is an important form of socialization and leisure in Latin cultures [13, 14] that challenges individuals both physically and cognitively. The limited literature on the health effects of dance for older adults indicates that dance can significantly improve lower extremity function, including mobility and balance [15]. Dance also requires individuals to plan, monitor, and execute a sequence of goal-directed complex actions, potentially making it ideal for preventing cognitive decline in executive function. Moreover, dance is enjoyable [16], a feature that could lead to increased maintenance [17]. It is currently unknown whether PA in the form of dance that integrates balance, endurance, and weight-shift transitions is effective at minimizing disability [18].
This study will make a significant contribution to knowledge about methods to reduce health disparities among older Latinos. To date, PA interventions with older Latinos have: (1) primarily focused on diabetes or chronic disease management [19, 20] but not other significant health conditions; (2) largely included Latinos of Puerto Rican ethnicity [20] but not other subgroups of Latinos; (3) not reported PA data [21]; and/or (4) been delivered in English but not Spanish, the primary language of older Latinos. Studies of dance interventions for older adults have: (1) had small sample sizes, (2) largely been conducted outside the U.S. and lacked control groups, and (3) not been conducted with older Latinos. These limitations are unfortunate because language- and culture-specific PA programs have the potential to reduce racial/ethnic disparities with respect to disability [22]. We will also be able to address the role of self-efficacy on health outcomes. Keysor (2003) has posited that self-efficacy (confidence in one’s capabilities to successfully carry out courses of action [23]) is an important underlying mechanism in the PA-disability relationship. Self-efficacy is a variable from Social Cognitive Theory that has been shown to influence physical function performance [24, 25] and many health behaviors [23, 26]. Thus, the “B.A.I.L.A.: Being Active, Increasing Latinos’ healthy Aging” study addresses limitations of prior PA and dance interventions by including participants of many Latino subgroups (e.g., Mexican, Puerto Rican, Guatemalan, Ecuadorian) and will test the efficacy of a dance program relative to a control group on the health behaviors and outcomes of PA, self-efficacy, physical function, cognitive function, and self-reported functional limitations and disability.
2. Specific Aims
The specific aims of this trial are to:
-
Test the impact of the BAILAMOS© program on lifestyle PA (i.e., accumulation of leisure time, household, occupational, and transportation PA over the entire day) [27] at 4 months and the impact of BAILAMOS© maintenance activities on lifestyle PA maintenance at 8 months.
Hypothesis 1: Lifestyle PA (self-reported and accelerometer-assessed) will be significantly higher in the BAILAMOS© group at 4 and 8 months compared to the control group.
-
Test the impact of the BAILAMOS© program at 4 months, and BAILAMOS© maintenance activities at 8 months, on self-efficacy (mediator) and on health outcomes (physical function, cognitive function, and self-reported functional limitations and disability).
Hypothesis 2a: Self-efficacy for PA, Balance, and Gait will be significantly higher in the BAILAMOS© group at 4 and 8 months compared to the control group. Moreover, self-efficacy for PA, Balance, and Gait will mediate the effect of the BAILAMOS© program on lifestyle PA and health outcomes.
Hypothesis 2b: Physical function (i.e., mobility, gait speed, balance, and lower body strength and endurance), cognitive function (i.e., executive function, working memory, perceptual speed, verbal episodic memory) and self-reported functional limitations and disability scores (subscales of the Abbreviated Late Life Function and Disability Instrument (LL-FDI) [28] and self-reported use of an assistive device for walking) will be significantly better in the BAILAMOS© group at 4 and 8 months compared to the control group.
3. Methods
3.1. Overview and study design
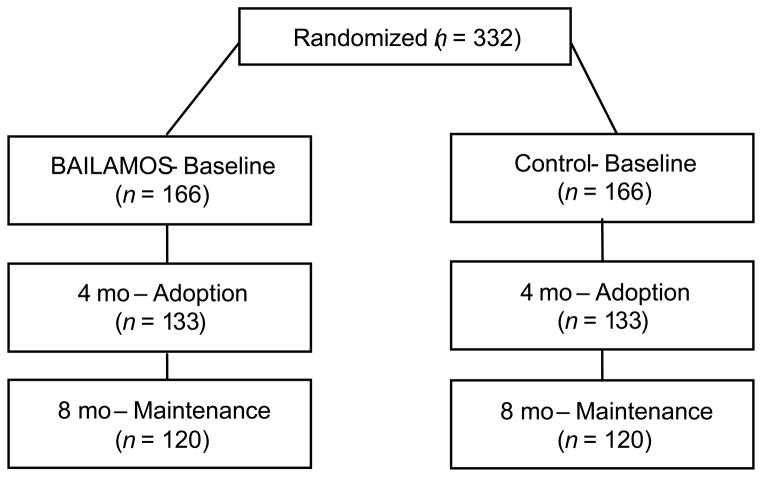
Study approval was obtained from the Institutional Review Boards (IRB) at the University of Illinois at Chicago (UIC), Rush University Medical Center, and University of Illinois at Urbana-Champaign. This study will use a two-group randomized controlled trial (RCT) with randomization at the level of the individual (N=166 Treatment, 166 Control) (see Figure 1) to the BAILAMOS© condition or to a health education control group. We will examine the short-term adoption and impact (months 1–4) of BAILAMOS©, a 4-month group-based intervention; and the short-term maintenance and impact of the BAILAMOS© maintenance activities (months 5–8). We propose to recruit 332 older Latinos across 9–10 sites over four years. Sites will include senior centers and community centers. Recruitment is expected to last 5 weeks at each site, and testing is expected to last 2–3 weeks at each timepoint. We will attempt to enroll approximately 40 individuals (20 treatment, 20 control) at each site. Sites will be staggered so that recruitment begins 5–10 weeks after recruitment has completed at the previous site. There will not be more than 2 sites at any one time offering the 4-month BAILAMOS© dance program (see Figure 2 for snapshot).
Figure 1.
Proposed flowchart of participation
Figure 2.
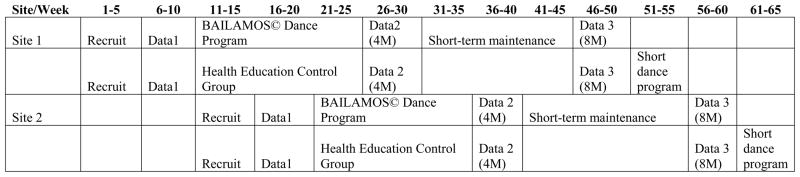
Snapshot of Intervention Design
Notes: Data1 = Baseline data collection; Data2 = Four-month data collection; Data3 = Eight-month data collection; 4M = 4 months; 8M = 8 months
We have chosen to randomize participants within sites, rather than randomizing sites, and include attempts to minimize contamination. Acculturation refers to an adaptation or assimilation process by an ethnic/racial group to a host culture [29], and acculturation levels of Latinos residing in Chicago neighborhoods can differ substantially; thus, randomizing participants within sites will reduce concerns about the probability of systematic differences between Latinos at different sites. This strategy will also ensure that all sites have the opportunity to offer a dance program, which is important for continuing positive relationships with community centers that serve older adults.
3.2. Participants
Chicago is home to more than 86,500 Latinos aged 55 years and older [30]. Inclusion criteria (self-reported) are: (1) aged ≥ 55 years old; (2) self-identification as Latino/Hispanic; (3) ability to speak Spanish; (4) participation in ≤2 days/week of aerobic exercise; (5) at risk for disability (see below); (6) adequate cognitive status as assessed by the Mini Mental State Examination (>14/21) [31]; (7) danced < 2 times/month over the past 12 months; (8) willingness to be randomly assigned to treatment or control group; (9) no current plans to leave the country for more than two consecutive weeks over the next year.
Exclusion criteria (self-reported) include: (1) presence of uncontrolled cardiovascular disease or uncontrolled diabetes mellitus, (2) pacemaker in situ, (3) stroke within the past 12 months, (4) severe chronic obstructive pulmonary disease (COPD), (5) recent healing or unhealed fracture(s) [32], (6) use of an assistive device to walk (cane, walker, or wheelchair) since such individuals are already considered mobility disabled [33, 34].
At risk for disability is operationally defined as one of the following: (1) Presence of diabetes [35, 36]; (2) Underweight (BMI lower than 18.5) [37]; (3) Overweight or obese (BMI greater than 25.0) [37, 38]; or (4) Difficulty or change with any one of the following four tasks: (a) walking a long distance (4 blocks or ½ mile), (b) climbing 10 steps, (c) transferring from a bed or chair, (d) walking a short distance on a flat surface. Two questions will be asked for each task: “Have you had difficulty (task)” and “Have you changed the way you (task) or how often you do this, due to a health or physical condition?” Older adults with difficulty or change with any one of the four tasks will be eligible for the study, similar to methods used by Weiss et al. [34] and those used in our BAILAMOS© pilot study.
We will use the Exercise Assessment and Screening for You (EASY) questionnaire to detect presence of conditions that could preclude study participation [39, 40]. Current PA screening guidelines from a consensus group from the American Heart Association and the American College of Cardiology [41, 42] no longer recommend routine stress testing for those initiating a PA program. Among sedentary older adults who are asymptomatic, moderate intensity PA can be safely initiated regardless of whether the person has had a recent medical evaluation [43, 44]. The EASY has clear recommendations for when evaluation by a physician is needed before beginning a PA program (e.g., when the individual reports new-onset shortness of breath, pain, or dizziness that has not been previously evaluated by a health care provider), and we will follow these recommendations.
3.3. Recruitment procedures
Participants will be recruited using established relationships developed by Dr. Marquez (PI), who has been working with Latino communities in Chicago since 2007. The Community Engagement Advisory Board (CEAB) of the Center for Clinical and Translational Science (CCTS) at UIC will provide assistance. Recruitment will be done through presentations at study sites, churches, parks, and coalition meetings; health centers and clinics, word of mouth, flyers in mailboxes of senior housing facilities, presence at supermarkets, senior fairs and health fairs, and articles and ads in neighborhood and city-wide newspapers and websites. Recruitment will begin in Year 1 and continue until all participants for the last site are recruited, with recruitment focused at the different sites during appropriate years.
3.4. Intervention arm: BAILAMOS©
3.4.1. The BAILAMOS© dances and dance manual
BAILAMOS© includes a 4-month, twice-weekly adoption phase and a 4-month, twice-weekly maintenance phase. BAILAMOS© encompasses four dance styles: Merengue, Cha Cha Cha, Bachata, and Salsa. These four styles of Latin dance can be considered among the most popular in terms of recognition and preference. According to Ainsworth’s Compendium [45], these styles of dance are of moderate intensity, about 4.5 METS. The sequencing of dance styles was determined by level of difficulty, with the simplest style introduced first (i.e., Merengue) and the most difficult style last (i.e., Salsa) to enhance self-efficacy through mastery and accomplishment. Self-efficacy will also be increased through participants’ having vicarious experiences via social modeling [23]. Consistent verbal encouragement will also contribute to increased self-efficacy [23].
The PI and a bilingual professional dance instructor co-developed the extensive BAILAMOS© Dance Manual and a detailed class-by-class schedule. The instructor has been teaching dance classes since 1993 and in 2002 he founded the first professional Salsa dance school in Chicago. He has extensive dance experience, has taught older adults, and has the capacity to teach persons with different skill and experience levels. The dance moves were developed so that participants can perform them safely and at their own pace. The manual, meant for use by instructors of the program, includes an introduction describing the goals of the program and descriptions of the various styles of dance. The manual also has photos and descriptions of every dance broken down into each dance step.
3.4.2. BAILAMOS© session components
3.4.2.1. Format
See Table 1 for the BAILAMOS© format. The first day of week 1 for each style of dance will be 2 hours, with the first hour devoted to discussion of strategies to increase lifestyle PA, followed by one hour of active dance instruction. Participants will receive a dose of leisure time PA via the dance program, and will be encouraged to add more leisure time PA to their lives. Emphasis will be placed on increasing household and transportation PA, as older Latinos can encounter personal, cultural, and environmental barriers that prevent leisure time PA participation. The second day of weeks 1 and 3 for each dance style, and the first day of weeks 2, 3, and 4 for each dance style, will include 1 hour of dance instruction. The second day of weeks 2 and 4 for each dance style will be devoted to “Fiestas de Baile,” “Dance Parties” in which participants spend time dancing and practicing what they have learned. Participants will be encouraged to sign up to bring food and/or drink to share during the Fiestas de Baile.
Table 1.
BAILAMOS© Dance design
| Tuesday | Thursday | |
|---|---|---|
| Week 1 | Discussion + Instruction | Instruction |
| Week 2 | Instruction | Fiesta de Baile |
| Week 3 | Instruction | Instruction |
| Week 4 | Instruction | Fiesta de Baile |
The 4-week plan above is repeated for each of the 4 styles of dance.
3.4.2.2. Content
A staff research assistant will lead the four 1-hour discussion sessions over the 4 months of adoption. Discussion sessions will utilize a Social Cognitive Framework [23], and focus on increasing knowledge, outcome expectations, social support, and self-efficacy in order to increase lifestyle PA. Session one of the first week involves a “Meet and Greet,” a review of program expectations and program logistics (e.g., how to complete a dance log). Participants will also pair up with another participant from class, a “compadre/comadre” or “exercise buddy” intervention partner who will call the partner in case class is missed [46]. We will also cover the 2008 PA Guidelines for Americans to reinforce the need to do PA outside of the dance program, and discuss PA safety. Session one of the fifth week will cover the benefits of PA, and participants’ PA interests and motivation. Session one of the ninth week will be a discussion of perceived barriers to PA and how to overcome those barriers, along with formulation of a PA plan and goal-setting. Session one of the thirteenth week will discuss the BAILAMOS© maintenance activities, and overcoming relapses.
3.4.2.3. Dance
Each session will begin with 2–3 minutes of stepping in place as warm-up, followed by stretching including movements of the neck, trunk, and extremity range of motion exercises. Instruction begins with the basics of the respective styles of dance, followed by advanced steps for singles and couples dancing. For couples dancing participants will learn the roles of both leaders and followers, and will continually rotate partners. Over each month, activity will increase and progress in terms of movement, specificity of dance moves, and complexity. Basic principles will be targeted, such as partnership, timing, footwork, and movement quality [47]. Each session will end with a 5 minute cool-down. Logs will be completed, and participants will be reminded to increase their lifestyle PA outside of the program.
3.4.3. Maintenance program
To enhance maintenance of PA after the 4-month program, we will use the BAILAMOS© maintenance activities manual and a detailed class-by-class schedule. During the maintenance phase (months 5–8), 2–3 indigenous leader(s) (i.e., participants from the initial 4-month dance condition from each site who are especially proficient at dancing, regularly attend the program, and are sociable) will be asked by the dance instructor about their interest and willingness to become “dance instructors.” In a “train the trainer” model, indigenous leaders will be trained to teach the BAILAMOS© program, including new dance moves that have been choreographed by the professional dance instructor. Thus, treatment group participants will have the opportunity to continue dancing in months 5–8. Indigenous leaders will take attendance and lead dance classes for treatment group participants. Also, each participant will be given the opportunity to invite one person to the dance classes. Class material will include review of the previous dance moves; four additional dance moves added to previous moves learned; practice of all moves learned; with the final four weeks consisting of open dance and practice. After the research ends, these indigenous leaders can direct the BAILAMOS© dance program for their community.
3.4.4. Sample retention
Retention strategies will include: (1) clearly communicating the intervention schedule and data-collection times so that participants know what to expect; (2) scheduling convenient appointments for data collection; (3) providing reminder calls for data-collection appointments; (4) requesting designation of family members or friends who can be called when participants cannot be reached; (5) providing compensation for participation in testing; and (6) making telephone calls to participants who miss class sessions. Study staff will primarily be the same ethnicity as participants. Separate $50 lotteries will be conducted every four weeks for intervention and control group participants, respectively, who have attended 75% of classes over the previous four weeks. If we determine that a participant has withdrawn from the program, a staff member will call to obtain reasons for dropout, including factors related to program components and barriers to participation.
3.4.5. Adverse events
All adverse events or unanticipated problems will be reported in writing to the University Institutional Review Board within 5 days of the discovery. Serious or unexpected adverse events will be verbally reported within 24 to 48 hours.
3.5. Control group
Previous dance interventions with older adults have lacked control groups [32, 48–50], or employed no-treatment control groups (i.e., participants were asked to continue with normal daily activities) [51–54]. In the current study sedentary older Latinos randomly assigned to the health education control group will participate in classes developed for older adults and offered by the University of Illinois Extension. All classes will be conducted in Spanish by Extension staff using Spanish-language materials. The curriculum covers topics such as stress, My Pyramid, food labels, diabetes, cancer, osteoporosis, immunizations, building a better memory, and making the most of medical appointments. Classes will meet one day per week for two hours, to provide social contact equivalent to that in the treatment group. After the completion of 8-Month testing, control group participants will have the opportunity to participate in a short dance program (4 classes, 1 class of each style of dance).
3.6. Measures
Most measures have been used previously by our research team in Spanish and English, and measures that are not available in Spanish will be translated using a “modified” committee approach [55]. Assessments will be administered by a research assistant in Spanish or English to reduce participant burden and literacy concerns. Answers will be collected using forms from the Pendragon Software Corporation on an iPad tablet.
3.6.1. Antecedent variables
3.6.1.1. Demographics
Information about age, gender, education, income, marital status, country of origin, race, ethnicity, preferred language, and number of children will be gathered.
3.6.1.2. Body composition
Staff of the UIC Clinical Research Center (CRC) will assess current height and weight in stocking feet, and body mass index (BMI)(kg/m2) will provide a measure of overall size.
3.6.1.3. Acculturation/Cultural values
The measure used in the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) [2] that assesses acculturation, familism, ethnic identity, religious behaviors, and perceived discrimination will be used.
3.6.1.4. Health history/status
A brief survey will elicit information about participants’ health history. Current health will be measured with the single-item global self-reported health question from the Behavioral Risk Factor Surveillance System (BRFSS), the world’s largest, on-going telephone health survey system [56].
3.6.2. Intervention variables
3.6.2.1. Intervention adherence
Attendance at each session will be recorded. Adherence will be the number of classes attended divided by number of classes conducted (32).
3.6.2.2. Intervention engagement
Individual participant dance logs, completed by the participant (with assistance from staff if needed), will include number of minutes danced (the instructor will tell the class the number of minutes danced), Ratings of Perceived Exertion [57], Feeling Scale [58], and perceived enjoyment of the session on a 1–7 Likert scale.
3.6.3. Primary Outcome
3.6.3.1. Lifestyle PA
3.6.3.1.1. Self-Report PA
The Community Healthy Activities Model Program For Seniors (CHAMPS) Physical Activity Questionnaire for Older Adults [59] is a change-sensitive PA scale that assesses weekly frequency and duration of lifestyle PA (leisure time, household, occupational, and transportation PA) typically undertaken by older adults. The CHAMPS has been translated into Spanish and employed with older Latino adults [60], and has established validity and reliability [59].
3.6.3.1.2. Objective PA
ActiGraph Model GT3-Plus accelerometers (The Actigraph, Pensacola, FL) are small and lightweight triaxial accelerometers that measure accelerations in three planes. ActiGraph accelerometers provide valid assessments of lifestyle PA in men and women [61, 62]. Accelerometers will be worn on the wrist, and data will be included in analysis if the accelerometer displays at least 10 hours of data (> 0 count values for each hour) in a 24-hour period on at least 3 days [63–65].
3.6.4. Secondary Outcomes
3.6.4.1. Physical Function Performance
3.6.4.1.1. Mobility
The 400M Walk is used for assessing mobility [66]. Participants will walk in a long hospital hallway or the perimeter of a community room and will be instructed to walk “at a steady and, if possible, constant pace” [67]. We will record actual time to finish the walk.
3.6.4.1.2. Lower extremity function
The Short Physical Performance Battery (SPPB) [68] tests balance (tandem, semi-tandem, and side-by-side stands), gait (time to walk 8 feet), and lower body strength and endurance (time to rise from a chair and return to the seated position 5 times). Scores range from 0–12, the SPPB is widely used with older adults [69].
3.6.4.2. Cognitive Function
In 2009 the official Spanish version of measures in the Uniform Data Set (UDS) of the National Institute on Aging Alzheimer’s Disease Center Program was released [70]. We will use a subsample of these tests that assess functions that have been found to decrease with age but also be influenced by regular PA (i.e., executive function, working memory, perceptual speed, verbal episodic memory) [71].
3.6.4.2.1. Executive Function
3.6.4.2.1.1
The Trail Making Test (TMT; Parts A & B) [72] consists of two parts. It requires an individual to draw lines sequentially connecting 25 encircled numbers randomly distributed on a page (Part A) and encircled numbers and letters in alternating order (Part B). The score is the time required to complete each task.
3.6.4.2.1.2
In the Color task of the short form [73] of the Stroop Neuropsychological Screening Test [74] the participant is shown the names of colors printed in conflicting ink colors and is asked to name the words. The second task is the Color–Word task in which the participant is shown the names of colors printed in conflicting ink colors (e.g., the word “blue” in red ink) and is asked to name the color of the ink rather than the word. The scores are the number of words named correctly in 30 seconds minus the number of errors; and the number of colors named correctly in 30 seconds minus the number of errors [73].
3.6.4.2.1.3
Word fluency [75] asks participants to generate as many examples as possible from two semantic categories (animals; fruits and vegetables) in separate 60-second trials. A word fluency score will be arrived at by summing the number of animals generated with the number of fruits and vegetables generated.
3.6.4.2.2. Working Memory
3.6.4.2.2.1
The Digit Span test [76] has two parts. Digit strings of increasing length are read and the participant is asked to repeat each string forward (Digit Span Forward) or backward (Digit Span Backward). The score is the number of correctly retrieved strings in each part [76].
3.6.4.2.2.2
In Digit Ordering [73, 77] digit strings of increasing length are read and the participant is asked to reorder the digits and say them in ascending order. The score is the number of correctly reordered strings [73].
3.6.4.2.3. Perceptual Speed
3.6.4.2.3.1
In the Symbol Digit Modalities Test [78], the participant is asked to identify and name the digits which belong with consecutively presented symbols. The score is the number of digits correctly paired with symbols in 90 seconds
3.6.4.2.4. Verbal Episodic Memory
3.6.4.2.4.1
Logical Memory I and II [76] has two parts. A brief story is read to the participant who is then asked to retell it immediately (I) and after a 5-minute delay filled with other activities (II). The score is the number of the 25 story units recalled immediately (I) and after the delay (II).
3.6.4.3. Self-Reported Functional Limitations
3.6.4.3.1
The basic and advanced lower extremity function subscales of the Abbreviated Late Life Function and Disability Instrument (LL-FDI) [28] will be used to assess functional limitations. Each subscale is composed of five items reflecting the degree to which participants are limited in their performance of each activity. Higher scores reflect less limitation in performing tasks. This measure has adequate validity and reliability [28].
3.6.4.4. Friendship Network Measurement
At months 4 and 8 post-testing we will collect data on the friendship networks of the participants. They will be shown a roster that includes the names of all the other participants in their study group (i.e., dance group or health education). Following standard procedure for social network data collection [79], participants will be asked to nominate who they knew before the program started; who they were friends with before the program started; and who they are friends with now (at the respective timepoint).
3.6.5. Mediator Variables
3.6.5.1. Lifestyle Self-Efficacy
The Lifestyle Self-Efficacy Scale [80] assesses participants’ beliefs in their ability to be physically active five or more days per week for at least 30 minutes of accumulated PA per day over incremental month periods for 6 months. This measure has established validity and reliability [80][81]. Only participants in the dance condition will complete this measure.
3.6.5.2. Exercise Barriers Self-Efficacy
The Barriers Self-Efficacy Scale [82] assesses perceived capabilities to exercise four times per week over the next three months in the face of commonly identified barriers to participation. This measure has established validity and reliability [83]. We revised this measure to assess perceived capabilities to attend dance classes two times per week over the next three months in the face of commonly identified barriers to participation. Only participants in the dance condition will complete this measure.
3.6.5.3. Gait Self-Efficacy
The Gait Efficacy Scale [84] assesses individuals’ beliefs in their capability to negotiate stairs and objects in their path. This measure has established validity and reliability [84].
3.6.5.4. Balance Self-Efficacy
The Activities-specific Balance Scale [85] measures confidence in ability to perform various activities of daily living (ADLs) without compromising balance. This measure has established validity and reliability [85].
3.6.6. Distal Outcomes
3.6.6.1. Disability
3.6.6.1.1
The eight-item disability limitations subscale of the Abbreviated Late Life Function and Disability Instrument (LL-FDI) [28] assesses both the frequency of performing social and personal role activities, and limitation in capability of performing instrumental and management role activities. Higher scores on the disability component reflect less disability. This measure has adequate validity and reliability [28].
3.6.6.1.2
If a person reports using an assistive device for walking they will be considered mobility disabled.
3.7. Procedures
3.7.1. Randomization
Older Latinos who qualify for the study and complete baseline testing will be randomly assigned to the dance treatment or to the health education control group using randomization offered in the Study360™ software (Almedtrac, Inc.). Randomization will be stratified based on sex, as it is likely that fewer men than women will participate and randomization will help to ensure that approximately the same number of men are in each study condition.
3.7.2. Enrollment
Potential participants can consent to be screened in a number of different ways, including learning about the study and signing a sheet agreeing to be called by a research member at a later time; and learning about the study another way and calling our office to be screened. Bilingual study staff will screen all interested individuals for eligibility based on inclusion and exclusion criteria using REDCap™, a secure, web-based application for building and managing online surveys and databases.
3.7.3. Testing
We will use Study 360 software (Almedtrac, Inc.) for project monitoring and daily research protocol management, including automatic reminders and tracking. Testing is expected to last 1–2 hours and will primarily take place at the UIC Clinical Research Center (CRC) of the Center for Clinical and Translational Science. Participants will be offered complementary rides from a taxi service (using an established contract of the PI with the taxi service), which will transport participants from their homes to the UIC CRC and vice versa. For those participants who will not come to the university for testing at Months 4 and 8 we will offer to conduct testing at the study site (i.e., the senior center). Data collection research staff will not be informed as to which study condition participants are in. After participants are deemed eligible they will be scheduled for a baseline assessment. At the assessment a staff member will explain the study and read the Informed Consent to the participant. After participants agree to participate, they will sign the Informed Consent. Questionnaires and tests (available in Spanish or English) will then be administered. Participants must be able to speak/understand Spanish to be eligible for the study; however, some participants will likely prefer to do questionnaires in English. Participants will be compensated with $10 for their participation. At 4-months, post-intervention testing will occur. Questionnaires and tests will be administered in the same order as baseline testing. Participants will be paid $10 as compensation for completing the post-intervention testing. Participants will be tested again at 8-months following the conclusion of the maintenance phase of the program using the same battery of tests with the same compensation. Participants in both study groups will be assessed at all timepoints (i.e., Baseline, 4- and 8-months).
Accelerometers
Prior to the trial and during the last week, Week 16 of the 4-month program, participants will be asked to wear an accelerometer on their wrist for 7 consecutive days to assess baseline and post-intervention levels of participation in lifestyle PA. Accelerometer assessment will also take place at 8-months as a measure of short-term maintenance of PA. Participants will be compensated $10 at each timepoint.
3.7.4. Study Fidelity
The Behavior Change Consortium’s (BCC) model of treatment fidelity will be used to monitor the reliability and validity of the intervention [86] (components of the BCC model are described below).
3.7.4.1. Staff and Training
The bilingual and bicultural Project Director, data collectors, and research assistants will be trained on study procedures prior to the start of data collection. This training will include general orientation to the design and purpose of the study, and research responsibilities including recruiting and screening participants. Data collectors will also be trained in administering questionnaires in Spanish and English, including item-by-item reviews of the questionnaires, and practice interviews; and in using accelerometers (initialization and downloading of data), and conducting physical and cognitive testing.
The dance instructor, who co-developed BAILAMOS©, will review the program before teaching. Backup instructors will be dance instructors familiar with the dances, who will be further trained using our manual. Following initial program completion, the indigenous leaders at each site will be trained to teach BAILAMOS© and the additional moves, using the BAILAMOS© maintenance activities manual along with a DVD of the dance moves. Health educators for the control group will be trained on taking attendance and on the importance of allowing only control group participants into the sessions.
3.7.4.2. Delivery of the intervention
During Months 1–4, we will conduct site visits to observe the dance instructor during the second week of each style of dance. The detailed class-by-class schedule will help to ensure that iterations of the program across sites cover the same material at the same timepoint of the intervention. Site visit members will use a revised version of an Implementation Checklist developed and tested for Fit and Strong! [87]. The visits will enable us to provide feedback to instructors about program implementation and to provide technical assistance as needed. The visits will also enable us to collect valuable information about adaptations that are made to enhance delivery of the program in the field. We will conduct these same site visits during Months 5–8 to ensure that indigenous leaders are properly administering the program, and contamination is not occurring.
3.7.4.3. Receipt of intervention
A checklist to evaluate the extent to which participants receive and perform the dance treatment (i.e., extent to which participants can successfully execute the dance moves taught) will be used on the last day of each style of dance. Additionally, participants will complete a program evaluation survey. This survey includes items on satisfaction with the instructor, the timing and location of the class, and overall satisfaction with the dance program. It will be administered on the last day of class. Quantification of the number of sessions attended will also be assessed as a measure of receipt of intervention [88].
3.7.4.4. Enactment
“Enactment of treatment skills” will monitor if the individual performs skills in relevant real-life settings as intended. To assess this, participants will log their use of the maintenance period dance sessions in Months 5–8 after the formal 4-month program is completed. Overall lifestyle PA will be assessed with the CHAMPS Physical Activity Questionnaire for Older Adults [59].
3.8. Data analytic plan
3.8.1. Data management
Data will be entered onto iPad tablets which have Pendragon software, and the data will be downloaded to a password-protected server. Using SPSS Statistics 22 software (SPSS, Inc.) we will run standard checks for outliers, duplicates, and other types of errors which may occur within a complex data file. All missing data will be flagged and coded accordingly. Procedures will be developed for collection of missing data and for imputations of missing data where the proportion of missing data is small. More complex imputation strategies will be developed if warranted.
3.8.2. Power analysis and sample size
From a clinical standpoint, changes in physical function such as mobility can be considered the most meaningful outcomes for older adults. Since some researchers consider the 400M walk the gold standard for mobility [89], our power analysis was based upon this test. Our pilot test of BAILAMOS© showed a moderate effect size of −0.56 for the 400M walk test (i.e., a decrease in the time needed to complete the test). Using the method of Rochon [90] to calculate statistical power available to test the hypothesis that there is greater improvement in the Treatment group than the Control group on the 400M walk over the 8-month period yields the following: To detect a medium interaction effect size of ES = 0.50 with two-sided Type I error alpha = 0.05; power = 0.80; using Rochon’s usual null hypothesis “H3,” compound symmetry with cross-time residual correlation rho = 0.50; with cluster ICC=0.02; and an R2 = 0.15 requires 240 participants (120 Treatment, 120 Control) at 8-months.
Our proposed RCT employs a two-group repeated measures design. Treatment and Control groups will enroll approximately 166 participants each (332 total). With ~40 participants at each site, 8–9 sites are needed. A 12-week dance program for older adults by Hui et al. (2008) [32] reported an 85% retention rate, and our pilot test resulted in a 75% retention rate. Assuming 80% retention, we anticipate that 266 participants (133 Treatment, 133 Control) will complete assessments at the end of the 4-month program. Assuming most participants will drop out of the study during those initial four months, we anticipate a 90% retention rate of those that participated at 4-months, resulting in 240 participants (120 Treatment, 120 Control) who will complete assessments at the end of the 8-months.
3.8.3. Hypothesis testing
3.8.3.1. Aim 1 Hypothesis
Lifestyle PA (self-reported and accelerometer-assessed) will be significantly higher in the BAILAMOS© group at 4 and 8 months compared to the control group.
The proposed study uses a repeated measures design with two groups and individual covariates. Initially, descriptive statistics will be obtained (e.g., for continuous variables we will examine means and standard deviations).
Using t-tests and chi-square tests, whose p-values will have been adjusted by the Bonferroni method for multiple testing, we will examine all baseline outcomes and covariates to determine whether randomization has produced equivalent groups. Variables exhibiting differences will be added as covariates to analyses. Transformations to achieve normality of residuals will be applied as needed; and residuals from analysis will be examined to detect multivariate outliers. Data will be examined for differential dropout but dropout is expected to be missing at random (MAR) [91] and will thus not be imputed unless necessary.
Analysis will be carried out using standard mixed model analysis of variance and covariance using the SAS program (i.e., PROC MIXED) [92–96], controlling for antecedent factors measured at baseline including demographics, body composition, acculturation, and health status. For Aim 1 the Group x Time interaction term will test whether there is greater improvement in self-reported and accelerometer-assessed lifestyle PA at 4 and 8 months in the treatment group compared to the control group.
As we have two correlated dependent variables, both of which are continuous, self-report PA and accelerometer-assessed PA, in addition to the foregoing analysis we will also report the multivariate test of a difference in centroids (multivariate mean points) between groups (e.g., Pillai trace, usually presented in an F-test format); and follow up with step-down F-tests to check which separate responses (self-report, accelerometer) exhibit group differences [97].
3.8.3.2. Aim 2a Hypotheses
Self-efficacy for PA, Balance, and Gait will be significantly higher in the BAILAMOS© group at 4 and 8 months compared to the control group.
The same analysis strategy in Aim 1 will be applied for Aim 2 Hypotheses. The Group x Time interaction term will test whether there is greater improvement in self-efficacy at 4 and 8 months in the treatment group compared to the control group. And we will also report the multivariate test of a difference in centroids between groups; and follow up with step-down F-tests to check which separate responses exhibit group differences.
In connection with Aim 2, Hypothesis 2a, we will conduct mediation analysis following testing procedures recommended by MacKinnon [98]. We will examine whether self-efficacy is a necessary intervening variable to produce the PA and health outcome differences. We will use methods provided in the MPlus statistical package, which offers special facilities for estimating standard errors of mediation terms.
3.8.3.3. Aim 2b Hypothesis
Physical function, cognitive function, and self-reported functional limitations and disability scores will be significantly better in the BAILAMOS© group at 4 and 8 months compared to the control group.
Analysis will be the same as that described for the previous aims. The Group x Time interaction term will test whether there is greater improvement in physical function, cognitive function, and self-reported functional limitations and disability scores at 4 and 8 months in the treatment group compared to the control group. And we will also report the multivariate test of a difference in centroids between groups; and follow up with step-down F-tests to check which separate responses exhibit group differences.
4. Limitations and Challenges
Although this study has the potential to advance science in many ways, the study also has limitations. First, the study will only be recruiting older Latinos from the Chicago area. It is possible that Latinos in various parts of the U.S. differ from Latinos in Chicago. A multi-site effectiveness trial in urban areas around the U.S. should be conducted in the future. Second, we do not have an assessment-only control based on prior trials showing that control groups without a PA intervention do not experience any benefit in PA by participating in the trial[99]. We also believe that with community-based research it is potentially unethical to recruit participants for whom there would be no perceived benefits. Third, by randomizing within sites, contamination is possible. However, as in the BAILAMOS© pilot, the dance instructor will not allow non-treatment group participants into the dance classes. The same will hold for the health educators and their classes. Study staff will monitor implementation of both conditions closely and intervene immediately if any crossover is detected. Moreover, during the maintenance period the indigenous leaders will be taught to only allow treatment group participants into dance sessions. Furthermore, we have a treatment fidelity plan in place for both months 1–4 of intervention, and the 5–8 month maintenance period. Fourth, it is possible that recruiting and retaining over 300 older Latinos will be challenging. However, there are tens-of-thousands of Latinos age 55 years and older living in Chicago [30]. To meet our recruitment goals we will network with Latino service providers and other organizations that we have worked with for years in Latino communities in Chicago, and use multiple strategies that have worked in previous trials for our research team. We will also incorporate retention strategies that have been successful in previous trials for our research team (e.g., lotteries). Finally, it is possible that our dance classes that meet two times per week (less than 120 minutes of PA) do not meet recommended PA guidelines and, as such, the intervention may be under-dosed to achieve meaningful changes in cognitive and physical function.
5. Discussion
The clinical trial that we have described is an essential step in the development of an evidence-based, disseminable community-based dance intervention for older Latinos at risk for disability. Older Latinos are a rapidly growing segment of the older adult population [1]. PA can prevent potential declines in important health outcomes of physical and cognitive function that lead to functional limitations. At present, Latinos aged 65–74 are 46% less likely to engage in leisure time PA than older non-Latino whites [7] and little is known about PA maintenance among ethnic minorities compared to non-Latino whites [100]. In part due to low levels of PA, the physical and cognitive function of older Latinos is poor relative to older non-Latino whites. For example, the number of Latinos in the U.S. with Alzheimer’s disease (AD) is projected to increase by 600% in the next 50 years [101] and AD symptoms may begin seven years earlier in Latinos than in non-Latino whites [102].
Participation in PA has substantial potential to help older Latinos maintain both physical and cognitive function as they age. Walking and dancing are the two most commonly reported forms of PA among older Latinos [103–106]. However, urban older Latinos cite unsafe neighborhoods and extreme weather conditions as significant barriers to walking. Dance is a widely popular form of PA among Latinos of all ages [13, 14] and holds considerable promise as a culturally appropriate form of PA that challenges individuals both physically and cognitively.
The impact of aerobic PA on cognition is well-established [107, 108], and positive gains in cognition have been reported in short-term PA interventions of only three months’ duration [107]. The effects of PA/fitness appear to be largest for cognitive tasks that involve executive function [107], the cognitive skills necessary to plan, monitor, and execute a sequence of goal-directed complex actions [109]. However, what we know about the PA-cognition relationship is based upon studies using aerobic forms of PA and studies with non-Latino whites; thus, the need to test PA interventions that have the potential to reduce the loss of cognitive function among older Latinos is of high public health importance [110].
To date, very few PA programs have been designed for older Latinos. BAILAMOS© is an innovative dance program that has been developed based on focus group input from older community-dwelling Latinos and in collaboration with an accomplished Latin dance instructor. A single group, pre-post 3-month pilot of BAILAMOS© demonstrated substantial program feasibility (9 of 12 participants completed the program, and participants attended 85% of the 24 sessions). Effect sizes (Cohen’s d) indicated greater self-reported lifestyle PA (d=1.38) and greater enjoyment of PA (d=.61) following the intervention. Improvements in physical function (mobility, d=−.56; usual gait speed, d=−.10) and cognitive function (ds=.11–.12) were also seen. Now, an adequately powered efficacy trial conducted over a longer time period is necessary to examine intervention efficacy.
In summary, this paper describes an RCT that will be conducted that will enable us to examine the adoption and adherence of PA in the form of dance and its impact on health outcomes at 4 months, along with impact on short-term maintenance of PA and associated health outcomes (8 months) among older, Spanish-speaking Latinos. This efficacy trial is unique in that it addresses the impact of this new program on both physical and cognitive health outcomes and the role of self-efficacy as a mediator of study outcomes. We believe that aspects of an individual’s profile (i.e., demographics, body composition, level of acculturation, perceived health status) are antecedents that need to be considered and controlled in multivariate analyses. These antecedent variables could predispose certain individuals to be more responsive to PA interventions, and also influence lifestyle PA and health outcomes. Individuals will participate in the BAILAMOS© dance intervention, which is expected to directly affect self-efficacy for PA, gait, and balance; as well as participation in lifestyle PA. Both the intervention and the self-efficacy mediators should improve the outcome of lifestyle PA, which in turn should positively influences physical function, cognitive function, and self-reported functional limitations. These reductions are hypothesized to impact the distal outcome of disability. If successful, an effectiveness study can be proposed following the current efficacy RCT to attempt to extend and adapt BAILAMOS© for broader populations and settings. The effectiveness study can establish the replicability of the BAILAMOS© dance program; its cost-effectiveness; and how to make the program less costly, while expanding program reach.
Poor health and low leisure time PA levels affect older Latinos for many reasons, and culturally appropriate PA that will be adopted and adhered to are essential to promote physical and cognitive health in this population. The potential for this trial to help fill the gap on evidence-based, culturally-appropriate PA programs for older Latinos is substantial as is its potential to add to the literature on the impact of PA on physical and cognitive health for older minority adults.
Acknowledgments
Research reported in this publication was supported by the National Institute of Nursing Research of the National Institutes of Health under Award Number R01NR013151. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
This project was supported by the University of Illinois at Chicago (UIC) Center for Clinical and Translational Science (CCTS), Award Number UL1TR000050 from the National Center for Advancing Translational Sciences, National Institutes of Health. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Advancing Translational Sciences or the National Institutes of Health.
We acknowledge the contributions of Susan Aguinaga, Maria Caceres, Sarah Janicek, Natalie Manbeck, Rosa Patino, Charles Spanbauer, Priscilla Vasquez, and undergraduate research assistants.
Footnotes
Trial Registration: ClinicalTrials.gov: NCT01988233
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Federal Interagency Forum on Aging-Related Statistics. Older Americans 2010: Key Indicators of Well-Being. Washington, DC: Federal Interagency Forum on Aging-Related Statistics; Jul, 2010. [Google Scholar]
- 2.Daviglus ML, Talavera GA, Aviles-Santa ML, Allison M, Cai J, Criqui MH, et al. Prevalence of major cardiovascular risk factors and cardiovascular diseases among Hispanic/Latino individuals of diverse backgrounds in the United States. Jama. 2012;308:1775–84. doi: 10.1001/jama.2012.14517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Tang MX, Cross P, Andrews H, Jacobs DM, Small S, Bell K, et al. Incidence of AD in African-Americans, Caribbean Hispanics, and Caucasians in northern Manhattan. Neur. 2001;56:49–56. doi: 10.1212/WNL.56.1.49. [DOI] [PubMed] [Google Scholar]
- 4.Cornman JC, Freedman VA. Racial and ethnic disparities in mobility device use in late life. J Gerontol B Psychol Sci Soc Sci. 2008;63:S34–41. doi: 10.1093/geronb/63.1.s34. [DOI] [PubMed] [Google Scholar]
- 5.Chodzko-Zajko WJ, Proctor DN, Fiatarone Singh MA, Minson CT, Nigg CR, Salem GJ, et al. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc. 2009;41:1510–30. doi: 10.1249/MSS.0b013e3181a0c95c. [DOI] [PubMed] [Google Scholar]
- 6.Ham SA, Yore MM, Kruger J, Heath GW, Moeti R. Physical activity patterns among Latinos in the United States: putting the pieces together. Preventing chronic disease. 2007;4:A92. [PMC free article] [PubMed] [Google Scholar]
- 7.Marquez DX, Neighbors CJ, Bustamante EE. Leisure time and occupational physical activity among racial or ethnic minorities. Med Sci Sports Exerc. 2010;42:1086–93. doi: 10.1249/MSS.0b013e3181c5ec05. [DOI] [PubMed] [Google Scholar]
- 8.Marshall SJ, Jones DA, Ainsworth BE, Reis JP, Levy SS, Macera CA. Race/Ethnicity, Social Class, and Leisure-Time Physical Inactivity. Med Sci Sports Exerc. 2007;39:44–51. doi: 10.1249/01.mss.0000239401.16381.37. [DOI] [PubMed] [Google Scholar]
- 9.Cromwell SL, Berg JA. Lifelong physical activity patterns of sedentary Mexican American women. Geriatr nurs New York, NY. 2006;27:209–13. doi: 10.1016/j.gerinurse.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 10.Vincent HK, Raiser SN, Vincent KR. The aging musculoskeletal system and obesity-related considerations with exercise. Ageing res rev. 2012;11:361–73. doi: 10.1016/j.arr.2012.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Melillo KD, Williamson E, Houde SC, Futrell M, Read CY, Campasano M. Perceptions of older Latino adults regarding physical fitness, physical activity, and exercise. J Gerontol Nurs. 2001;27:38–46. doi: 10.3928/0098-9134-20010901-08. [DOI] [PubMed] [Google Scholar]
- 12.Marquez DX, Hoyem R, Fogg L, Bustamante EE, Staffileno B, Wilbur J. Physical activity of urban community-dwelling older Latino adults. J phys act & health. 2011;8 (Suppl 2):S161–70. [PubMed] [Google Scholar]
- 13.Delgado CF, Munoz JE. Everynight Life: Culture and Dance in Latin/o America. Durham, NC: Duke University Press; 1997. [Google Scholar]
- 14.Lewis D. Introduction: Dance in Hispanic Cultures. Choreography and Dance. 1994;3:1–5. [Google Scholar]
- 15.Keogh JWL, Kilding A, Pidgeon P, Ashley L, Gillis D. Physical benefits of dancing for healthy older adults: A review. J Aging Phys Act. 2009;17:479–500. doi: 10.1123/japa.17.4.479. [DOI] [PubMed] [Google Scholar]
- 16.Judge JO. Balance training to maintain mobility and prevent disability. Am J Prev Med. 2003;25:150–6. doi: 10.1016/S0749-3797(03)00178-8. [DOI] [PubMed] [Google Scholar]
- 17.Robinson TN, Killen JD, Kraemer HC, Wilson DM, Matheson DM, Haskell WL, et al. Dance and reducing television viewing to prevent weight gain in African-American girls: the Stanford GEMS pilot study. Ethn Dis. 2003;13:S65–77. [PubMed] [Google Scholar]
- 18.Keysor JJ. Does late-life physical activity or exercise prevent or minimize disablement? A critical review of the scientific evidence. Am J Prev Med. 2003;25:129–36. doi: 10.1016/S0749-3797(03)00176-4. [DOI] [PubMed] [Google Scholar]
- 19.Lorig KR, Ritter PL, Jacquez A. Outcomes of border health Spanish/English chronic disease self-management programs. Diabetes Educ. 2005;31:401–9. doi: 10.1177/0145721705276574. [DOI] [PubMed] [Google Scholar]
- 20.Rosal MC, Olendzki B, Reed GW, Gumieniak O, Scavron J, Ockene I. Diabetes self-management among low-income Spanish-speaking patients: a pilot study. Ann Behav Med. 2005;29:225–35. doi: 10.1207/s15324796abm2903_9. [DOI] [PubMed] [Google Scholar]
- 21.Keller CS, Cantue A. Camina por Salud: walking in Mexican-American women. Applied nursing research: ANR. 2008;21:110–3. doi: 10.1016/j.apnr.2006.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dunlop DD, Song J, Manheim LM, Daviglus ML, Chang RW. Racial/ethnic differences in the development of disability among older adults. Am J Public Health. 2007;97:2209–15. doi: 10.2105/AJPH.2006.106047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bandura A. Self-Efficacy: The Exercise of Control. New York: W.H. Freeman and Company; 1997. [Google Scholar]
- 24.Li F, Harmer P, McAuley E, Fisher KJ, Duncan TE, Duncan SC. Tai Chi, self-efficacy, and physical function in the elderly. Prev Sci. 2001;2:229–39. doi: 10.1023/a:1013614200329. [DOI] [PubMed] [Google Scholar]
- 25.Rejeski WJ, Ettinger WH, Jr, Martin K, Morgan T. Treating disability in knee osteoarthritis with exercise therapy: a central role for self-efficacy and pain. Arthritis Care Res. 1998;11:94–101. doi: 10.1002/art.1790110205. [DOI] [PubMed] [Google Scholar]
- 26.McAuley E, Blissmer B. Self-efficacy determinants and consequences of physical activity. Exerc and Sport Sci Rev. 2000;28:85–8. [PubMed] [Google Scholar]
- 27.Dunn AL, Andersen RE, Jakicic JM. Lifestyle physical activity interventions. History, short- and long- term effects, and recommendations. Am J Prev Med. 1998;15:398–412. doi: 10.1016/S0749-3797(98)00084-1. [DOI] [PubMed] [Google Scholar]
- 28.McAuley E, Konopack JF, Motl RW, Rosengren K, Morris KS. Measuring disability and function in older women: psychometric properties of the late-life function and disability instrument. J Gerontol A Biol Sci Med Sci. 2005;60:901–9. doi: 10.1093/gerona/60.7.901. [DOI] [PubMed] [Google Scholar]
- 29.Berry JW. Psychology of acculturation. Nebraska Symposium on Motivation. 1989;39:201–34. [PubMed] [Google Scholar]
- 30.U.S. Census Bureau. 2006–2008 American Community Survey, Selected Population Profile in the United States: Hispanic or Latino (of any race) in Chicago. 2010. [Google Scholar]
- 31.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J psych research. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 32.Hui E, Chui BT, Woo J. Effects of dance on physical and psychological well-being in older persons. Arch gerontol geriatr. 2008 doi: 10.1016/j.archger.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 33.Simonsick EM, Newman AB, Visser M, Goodpaster B, Kritchevsky SB, Rubin S, et al. Mobility Limitation in Self-Described Well-Functioning Older Adults: Importance of Endurance Walk Testing. J Gerontol A Biol Sci Med Sci. 2008;63:841–7. doi: 10.1093/gerona/63.8.841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Weiss CO, Fried LP, Bandeen-Roche K. Exploring the hierarchy of mobility performance in high-functioning older women. J Gerontol A Biol Sci Med Sci. 2007;62:167–73. doi: 10.1093/gerona/62.2.167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Al Snih S, Fisher MN, Raji MA, Markides KS, Ostir GV, Goodwin JS. Diabetes mellitus and incidence of lower body disability among older Mexican Americans. J Gerontol A Biol Sci Med Sci. 2005;60:1152–6. doi: 10.1093/gerona/60.9.1152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Blaum CS, West NA, Haan MN. Is the metabolic syndrome, with or without diabetes, associated with progressive disability in older Mexican Americans? J Gerontol A Biol Sci Med Sci. 2007;62:766–73. doi: 10.1093/gerona/62.7.766. [DOI] [PubMed] [Google Scholar]
- 37.Al Snih S, Ottenbacher KJ, Markides KS, Kuo YF, Eschbach K, Goodwin JS. The effect of obesity on disability vs mortality in older Americans. Arch Intern Med. 2007;167:774–80. doi: 10.1001/archinte.167.8.774. [DOI] [PubMed] [Google Scholar]
- 38.Chen H, Bermudez OI, Tucker KL. Waist circumference and weight change are associated with disability among elderly hispanics. J Gerontol A Biol Sci Med Sci. 2002;57:M19–25. doi: 10.1093/gerona/57.1.m19. [DOI] [PubMed] [Google Scholar]
- 39.Resnick B, Ory M, Hora K, Rogers M, Page P, Chodzko-Zajko W, et al. The Exercise Assessment and Screening for You (EASY) Tool: Application in the oldest old population. Am J Lifestyle Med. 2008;2:432–40. [Google Scholar]
- 40.Resnick B, Ory MG, Hora K, Rogers ME, Page P, Bolin JN, et al. A proposal for a new screening paradigm and tool called Exercise Assessment and Screening for You (EASY) J Aging Phys Act. 2008;16:215–33. doi: 10.1123/japa.16.2.215. [DOI] [PubMed] [Google Scholar]
- 41.Gibbons RJ, Balady GJ, Beasley JW, Bricker JT, Duvernoy WF, Froelicher VF, et al. ACC/AHA guidelines for exercise testing: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Exercise Testing) Circulation. 1997;96:345–54. doi: 10.1161/01.CIR.96.1.345. [DOI] [PubMed] [Google Scholar]
- 42.US Preventive Services Task Force. Screening for coronary heart disease: recommendation statement. Ann Intern Med. 2004;140:569–72. doi: 10.7326/0003-4819-140-7-200404060-00001. [DOI] [PubMed] [Google Scholar]
- 43.Cress ME, Buchner DM, Prohaska T, Rimmer J, Brown M, Macera C, et al. Best practices for physical activity programs and behavior counseling in older adult populations. J Aging Phys Act. 2005;13:61–74. doi: 10.1007/s11556-006-0003-9. [DOI] [PubMed] [Google Scholar]
- 44.Pescatello L, DiPietro L, Fargo A, Ostfeld A, Nadel E. The impact of physical activity and physical fitness on health indicators among older adults. J Aging Phys Act. 1994;2:2–13. [Google Scholar]
- 45.Ainsworth BE, Haskell WL, Whitt MC, Irwin ML, Swartz AM, Strath SJ, et al. Compendium of physical activities: An update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32:S498–504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 46.Hovell MF, Mulvihill MM, Buono MJ, Liles S, Schade DH, Washington TA, et al. Culturally tailored aerobic exercise intervention for low-income Latinas. Am J Health Promot. 2008;22:155–63. doi: 10.4278/ajhp.22.3.155. [DOI] [PubMed] [Google Scholar]
- 47.Hackney ME, Kantorovich S, Earhart GM. A study on the effects of Argentine Tango as a form of partnered dance for those with Parkinson Disease and the healthy elderly. Am J Dance Ther. 2007;29:109–27. doi: 10.1007/s10465-007-9039-2. [DOI] [Google Scholar]
- 48.Alpert PT, Miller SK, Wallmann H, Havey R, Cross C, Chevalia T, et al. The effect of modified jazz dance on balance, cognition, and mood in older adults. J Am Acad Nurse Practitioners. 2009;21:108–15. doi: 10.1111/j.1745-7599.2008.00392.x. [DOI] [PubMed] [Google Scholar]
- 49.Lima MMS, Vieria AP. Ballroom Dance as Therapy for the Elderly in Brazil. American J Dance Ther. 2007;29:129–42. [Google Scholar]
- 50.Moffet H, Noreau L, Parent E, Drolet M. Feasibility of an eight-week dance-based exercise program and its effects on locomotor ability of persons with functional class III rheumatoid arthritis. Arthritis Care Res. 2000;13:100–11. doi: 10.1002/1529-0131(200004)13:2<100::AID-ANR4>3.0.CO;2-V. [DOI] [PubMed] [Google Scholar]
- 51.Eyigor S, Karapolat H, Durmaz B, Ibisoglu U, Cakir S. A randomized controlled trial of Turkish folklore dance on the physical performance, balance, depression and quality of life in older women. Arch gerontol geriatr. 2009;48:84–8. doi: 10.1016/j.archger.2007.10.008. [DOI] [PubMed] [Google Scholar]
- 52.Hopkins DR, Murrah B, Hoeger WW, Rhodes RC. Effect of low-impact aerobic dance on the functional fitness of elderly women. Gerontol. 1990;30:189–92. doi: 10.1093/geront/30.2.189. [DOI] [PubMed] [Google Scholar]
- 53.Shigematsu R, Chang M, Yabushita N, Sakai T, Nakagaichi M, Nho H, et al. Dance-based aerobic exercise may improve indices of falling risk in older women. Age Ageing. 2002;31:261–6. doi: 10.1093/ageing/31.4.261. [DOI] [PubMed] [Google Scholar]
- 54.Sofianidis G, Hatzitaki V, Douka S, Grouios G. Effect of a 10-week traditional dance program on static and dynamic balance control in elderly adults. J Aging Phys Act. 2009;17:167–80. doi: 10.1123/japa.17.2.167. [DOI] [PubMed] [Google Scholar]
- 55.Schoua-Glusberg A. Report on the Translation of the Questionnaire for the National Treatment Improvement Evaluation Study. Chicago: National Opinion Research Center; 1992. [Google Scholar]
- 56.Hennessy CH, Moriarty DG, Zack MM, Scherr PA, Brackbill R. Measuring health-related quality of life for public health surveillance. Public Health Rep. 1994;109:665–72. [PMC free article] [PubMed] [Google Scholar]
- 57.Borg G. An Introduction to Borg’s RPE-Scale. Ithaca, NY: Mouvement; 1985. [Google Scholar]
- 58.Hardy CJ, Rejeski WJ. Not what, but how one feels: the measurement of affect during exercise. J Sport Exerc Psychol. 1989;11:304–17. [Google Scholar]
- 59.Stewart AL, Mills KM, King AC, Haskell WL, Gillis D, Ritter PL. CHAMPS physical activity questionnaire for older adults: outcomes for interventions. Med Sci Sports Exerc. 2001;33:1126–41. doi: 10.1097/00005768-200107000-00010. [DOI] [PubMed] [Google Scholar]
- 60.Rosario MG, Vazquez JM, Cruz WI, Ortiz A. Internal consistency of the CHAMPS physical activity questionnaire for Spanish speaking older adults. Puerto Rico health sciences journal. 2008;27:224–8. doi: 10.1249/01.mss.0000273699.00091.93. [DOI] [PubMed] [Google Scholar]
- 61.Ainsworth BE, Bassett DR, Jr, Strath SJ, Swartz AM, O’Brien WL, Thompson RW, et al. Comparison of three methods for measuring the time spent in physical activity. Med Sci Sports Exerc. 2000;32:S457–64. doi: 10.1097/00005768-200009001-00004. [DOI] [PubMed] [Google Scholar]
- 62.Hendelman D, Miller K, Baggett C, Debold E, Freedson P. Validity of accelerometry for the assessment of moderate intensity physical activity in the field. Med Sci Sports Exerc. 2000;32:S442–9. doi: 10.1097/00005768-200009001-00002. [DOI] [PubMed] [Google Scholar]
- 63.Matthews CE, Ainsworth BE, Thompson RW, Bassett DR., Jr Sources of variance in daily physical activity levels as measured by an accelerometer. Med Sci Sports Exerc. 2002;34:1376–81. doi: 10.1097/00005768-200208000-00021. [DOI] [PubMed] [Google Scholar]
- 64.Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Med Sci Sports Exerc. 2005;37:S531–43. doi: 10.1249/01.mss.0000185657.86065.98. [DOI] [PubMed] [Google Scholar]
- 65.Ward DS, Evenson KR, Vaughn A, Rodgers AB, Troiano RP. Accelerometer use in physical activity: best practices and research recommendations. Med Sci Sports Exerc. 2005;37:S582–8. doi: 10.1249/01.mss.0000185292.71933.91. [DOI] [PubMed] [Google Scholar]
- 66.Buchner DM. One lap around the track: the standard for mobility disability? J Gerontol A Biol Sci Med Sci. 2008;63:586–7. doi: 10.1093/gerona/63.6.586. [DOI] [PubMed] [Google Scholar]
- 67.Marsh AP, Miller ME, Saikin AM, Rejeski WJ, Hu N, Lauretani F, et al. Lower extremity strength and power are associated with 400-meter walk time in older adults: The InCHIANTI study. J Gerontol A Biol Sci Med Sci. 2006;61:1186–93. doi: 10.1093/gerona/61.11.1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–94. doi: 10.1093/geronj/49.2.M85. [DOI] [PubMed] [Google Scholar]
- 69.Sherrington C, Lord SR, Vogler CM, Close JC, Howard K, Dean CM, et al. Minimising disability and falls in older people through a post-hospital exercise program: a protocol for a randomised controlled trial and economic evaluation. BMC geriatr. 2009;9:8. doi: 10.1186/1471-2318-9-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Acevedo A, Krueger KR, Navarro E, Ortiz F, Manly JJ, Padilla-Velez MM, et al. The Spanish translation and adaptation of the Uniform Data Set of the National Institute on Aging Alzheimer’s Disease Centers. Alzheimer disease and associated disorders. 2009;23:102–9. doi: 10.1097/WAD.0b013e318193e376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Kramer AF, Erickson KI, Colcombe SJ. Exercise, cognition, and the aging brain. J Appl Physiol. 2006;101:1237–42. doi: 10.1152/japplphysiol.00500.2006. [DOI] [PubMed] [Google Scholar]
- 72.Adjutant General’s Office. Army Individual Test Battery: Manual of Directions and Scoring. Washington, DC: War Department, Adjutant General’s Office; 1944. [Google Scholar]
- 73.Wilson RS, Barnes LL, Krueger KR, Hoganson G, Bienias JL, Bennett DA. Early and late life cognitive activity and cognitive systems in old age. J Int Neuropsych Society: JINS. 2005;11:400–7. doi: 10.1017/S1355617705050459. [DOI] [PubMed] [Google Scholar]
- 74.Trenerry M, Crosson B, DeBoe J, Leber W. Stroop Neuropsychological Screening Test manual. Adessa, FL: Psychological Assessment Resources (PAR); 1989. [Google Scholar]
- 75.Welsh KA, Butters N, Mohs RC, Beekly D, Edland S, Fillenbaum G, et al. The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD) Part V. A normative study of the neuropsychological battery. Neurology. 1994;44:609–14. doi: 10.1212/wnl.44.4.609. [DOI] [PubMed] [Google Scholar]
- 76.Wechsler D. The Wechsler Memory Scale-Revised. San Antonio, TX: Psychological Corporation; 1987. [Google Scholar]
- 77.Cooper JA, Sagar HJ, Jordan N, Harvey NS, Sullivan EV. Cognitive impairment in early, untreated Parkinson’s disease and its relationship to motor disability. Brain: a journal of neurology. 1991;114 (Pt 5):2095–122. doi: 10.1093/brain/114.5.2095. [DOI] [PubMed] [Google Scholar]
- 78.Smith A. Symbol Digit Modalities Test manual-revised. Los Angeles: Western Psychological Services; 1982. [Google Scholar]
- 79.Borgatti SP, Everett MG, Johnson JC. Analyzing Social Networks. SAGE Publications Limited; 2013. [Google Scholar]
- 80.McAuley E, Hall KS, Motl RW, White SM, Wojcicki TR, Hu L, et al. Trajectory of declines in physical activity in community-dwelling older women: social cognitive influences. J Gerontol B Psychol Sci Soc Sci. 2009;64:543–50. doi: 10.1093/geronb/gbp049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.McAuley E, Konopack JF, Morris KS, Motl RW, Hu L, Doerksen SE, et al. Physical activity and functional limitations in older women: influence of self-efficacy. J Gerontol B Psychol Sci Soc Sci. 2006;61:270–7. doi: 10.1093/geronb/61.5.P270. [DOI] [PubMed] [Google Scholar]
- 82.McAuley E. The role of efficacy cognitions in the prediction of exercise behavior in middle-aged adults. J Behav Med. 1992;15:65–88. doi: 10.1007/BF00848378. [DOI] [PubMed] [Google Scholar]
- 83.Marquez DX, McAuley E. Social cognitive correlates of leisure time physical activity among Latinos. J Behav Med. 2006;29:281–9. doi: 10.1007/s10865-006-9055-6. [DOI] [PubMed] [Google Scholar]
- 84.McAuley E, Mihalko SL, Rosengren K. Self-efficacy and balance correlates of fear of falling in the elderly. J Aging Phys Act. 1997;5:329–40. [Google Scholar]
- 85.Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1995;50A:M28–34. doi: 10.1093/gerona/50A.1.M28. [DOI] [PubMed] [Google Scholar]
- 86.Resnick B, Bellg AJ, Borrelli B, Defrancesco C, Breger R, Hecht J, et al. Examples of implementation and evaluation of treatment fidelity in the BCC studies: where we are and where we need to go. Ann Behav Med. 2005;29 (Suppl):46–54. doi: 10.1207/s15324796abm2902s_8. [DOI] [PubMed] [Google Scholar]
- 87.Hughes SL, Seymour RB, Campbell RT, Huber G, Pollak N, Sharma L, et al. Long-term impact of Fit and Strong! on older adults with osteoarthritis. Gerontologist. 2006;46:801–14. doi: 10.1093/geront/46.6.801. [DOI] [PubMed] [Google Scholar]
- 88.Moe EL, Elliot DL, Goldberg L, Kuehl KS, Stevens VJ, Breger RK, et al. Promoting Healthy Lifestyles: Alternative Models’ Effects (PHLAME) Health Educ Res. 2002;17:586–96. doi: 10.1093/her/17.5.586. [DOI] [PubMed] [Google Scholar]
- 89.Espeland MA, Gill TM, Guralnik J, Miller ME, Fielding R, Newman AB, et al. Designing Clinical Trials of Interventions for Mobility Disability: Results From the Lifestyle Interventions and Independence for Elders Pilot (LIFE-P) Trial. J Gerontol A Biol Sci Med Sci. 2007;62:1237–43. doi: 10.1093/gerona/62.11.1237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Rochon J. Sample size calculations for two-group repeated-measures experiments. Biometrics. 1991;47:1383–98. [Google Scholar]
- 91.Little RJA, Rubin DB. Statistical analysis with missing data. 2. Hoboken, NJ: John Wiley & Sons; 2002. [Google Scholar]
- 92.Fitzmaurice GM, Laird NM, Ware JH. Applied longitudinal analysis. Hoboken, NJ: John Wiley & Sons; 2004. [Google Scholar]
- 93.Hedeker D, Gibbons RD. Longitudinal data analysis. Hoboken, NJ: John Wiley & Sons; 2006. [Google Scholar]
- 94.Littell RC, Milliken GA, Stroup WW, Wolfinger RD, Schabenberger O. SAS for mixed models. 2. Cary, NC: SAS Institute, Inc; 2006. [Google Scholar]
- 95.Molenberghs G, Verbeke G. Models for discrete longitudinal data. New York: Springer-Verlag; 2005. [Google Scholar]
- 96.Verbeke G, Molenberghs G. Linear mixed models for longitudinal data. New York: Springer-Verlag; 2000. [Google Scholar]
- 97.Tabachnick BG, Fidell LS. Using Multivariate Statistics. 6. Pearson; 2012. [Google Scholar]
- 98.MacKinnon D. Introduction to Statistical Mediation Analysis. New York: Erlbaum Psych Press; 2008. [Google Scholar]
- 99.Conn VS, Phillips LJ, Ruppar TM, Chase JA. Physical activity interventions with healthy minority adults: meta-analysis of behavior and health outcomes. J health care poor underserved. 2012;23:59–80. doi: 10.1353/hpu.2012.0032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Dornelas EA, Stepnowski RR, Fischer EH, Thompson PD. Urban ethnic minority women’s attendance at health clinic vs. church based exercise programs. J cross-cultural gerontol. 2007;22:129–36. doi: 10.1007/s10823-006-9023-1. [DOI] [PubMed] [Google Scholar]
- 101.Novak K, Riggs J. Hispanics/Latinos and Alzheimer’s Disease. Alzheimer’s Association; 2010. [Google Scholar]
- 102.Clark CM, DeCarli C, Mungas D, Chui HI, Higdon R, Nunez J, et al. Earlier onset of Alzheimer disease symptoms in latino individuals compared with anglo individuals. Arch neurology. 2005;62:774–8. doi: 10.1001/archneur.62.5.774. [DOI] [PubMed] [Google Scholar]
- 103.Crespo CJ, Keteyian SJ, Heath GW, Sempos CT. Leisure-time physical activity among US adults. Results from the Third National Health and Nutrition Examination Survey. Arch Int Med. 1996;156:93–8. doi: 10.1001/archinte.1996.00440010113015. [DOI] [PubMed] [Google Scholar]
- 104.King AC. Interventions to promote physical activity by older adults. J Gerontol A Biol Sci Med Sci. 2001;56(Spec No 2):36–46. doi: 10.1093/gerona/56.suppl_2.36. [DOI] [PubMed] [Google Scholar]
- 105.Ramirez AG, Chalela P, Gallion K, Velez LF. Energy balance feasibility study for Latinas in Texas: a qualitative assessment. Preventing chronic disease. 2007;4:A98. [PMC free article] [PubMed] [Google Scholar]
- 106.Wood FG. Leisure time activity of Mexican Americans with diabetes. J Adv Nurs. 2004;45:190–6. doi: 10.1046/j.1365-2648.2003.02880.x. [DOI] [PubMed] [Google Scholar]
- 107.Colcombe S, Kramer AF. Fitness effects on the cognitive function of older adults: a meta-analytic study. Psychol Sci. 2003;14:125–30. doi: 10.1111/1467-9280.t01-1-01430. [DOI] [PubMed] [Google Scholar]
- 108.Kramer AF, Colcombe S, McAuley E, Erickson K, Scalf P, Jerome GJ, et al. Enhancing brain and cognitive function of older adults through fitness training. J Molec Neuro. 2003;20:213–22. doi: 10.1385/JMN:20:3:213. [DOI] [PubMed] [Google Scholar]
- 109.Lezak M, Howieson D, Loring D, Hannay H, Fischer J. Neuropsychological Assessment. Oxford University Press; 2004. [Google Scholar]
- 110.Williamson JD, Espeland M, Kritchevsky SB, Newman AB, King AC, Pahor M, et al. Changes in Cognitive Function in a Randomized Trial of Physical Activity: Results of the Lifestyle Interventions and Independence for Elders Pilot Study. J Gerontol A Biol Sci Med Sci. 2009 doi: 10.1093/gerona/glp014. [DOI] [PMC free article] [PubMed] [Google Scholar]