Abstract
Objective
Limited data exist on the impact of regurgitation on health-related quality of life (HRQOL) in gastro-oesophageal reflux disease (GORD). We assessed the relationship between regurgitation frequency and HRQOL before and after acid suppression therapy in GORD.
Method
We used data from two randomised trials of AZD0865 25–75 mg/day vs. esomeprazole 20 or 40 mg/day in non-erosive reflux disease (NERD) (n=1415) or reflux oesophagitis (RO) (n=1460). The Reflux Disease Questionnaire was used to select patients with frequent and intense heartburn for inclusion and to assess treatment response. The Quality of Life in Reflux and Dyspepsia (QOLRAD) questionnaire was used to assess HRQOL.
Results
At baseline, 93% of patients in both the NERD and RO groups experienced regurgitation. Mean QOLRAD scores were similar for NERD and RO at baseline and at week 4 and disclosed decremental HRQOL with increasing frequency of regurgitation; a clinically relevant difference of >0.5 in mean QOLRAD scores was seen with regurgitation ≥4 days/week vs. <4 days/week. The prevalence of frequent, persistent regurgitation (≥4 days/week) at week 4 among heartburn responders (≤1 day/week of mild heartburn) was 28% in NERD and 23% in RO. QOLRAD scores were higher amongst heartburn responders. There was a similar pattern of impact related to regurgitation frequency in heartburn responders as in the group as a whole.
Conclusion
Frequent regurgitation was associated with a clinically relevant, incremental decline in HRQOL beyond that associated with heartburn before and after potent acid suppression, in both NERD and RO.
Clinical trial numbers NCT00206284 and NCT00206245.
INTRODUCTION
Although many patients with gastro-oesophageal reflux disease (GORD) respond to acid suppression,[1] some exhibit only a partial response and have persistent reflux symptoms.[2] Furthermore, ‘partial response’ may pertain to heartburn, regurgitation, or less typical symptoms such as chest pain. This complexity has been ignored in treatment trials that have largely focused on the resolution of heartburn as the outcome of most interest.[1, 3] However, a recent systematic review [4] and a retrospective analysis of data from two large GORD clinical trials (conducted using the same dataset as this study)[5] suggest that regurgitation typically responds less well than heartburn to acid suppression. These two GORD trials used the reflux disease questionnaire (RDQ) to characterise upper GI symptoms and found that the average study subject endorsed four of the six RDQ items with some severity and that the response of heartburn (substernal burning behind the breastbone) was diminished by the presence of concomitant symptoms (particularly dyspepsia) at the start of treatment.[6] Another limitation of existing clinical data pertains to the impact of persistent symptoms. Existing health-related quality of life (HRQOL) analyses have focused on the threshold severity at which heartburn has negative impact.[7] Consequently, little is known about whether (or to what extent) regurgitation negatively affects HRQOL in patients with GORD.
The aim of this study was to evaluate the impact of regurgitation on HRQOL before and after potent acid suppression in GORD patients with and without reflux oesophagitis (RO). We used clinical trial data obtained from GORD patients who all had concomitant frequent and intense heartburn at baseline. The second aim was to investigate the prevalence and impact on HRQOL of frequent, persistent regurgitation in patients who exhibited a favourable therapeutic response to heartburn.
METHODS
Data from two parallel-group, double-blind, randomised trials were retrospectively reviewed: 1) AZD0865 (a potassium-competitive acid blocker) 25, 50 or 75 mg/day vs. esomeprazole 20 mg/day (present as 22.3mg/day esomeprazole magnesium trihydrate) for the treatment of NERD (n=1460)[8] (clinicaltrials.gov identifier: NCT00206284), and 2) AZD0865 25, 50 or 75 mg/day vs. esomeprazole 40 mg/day (present as 44.5mg/day esomeprazole magnesium trihydrate) for RO (n=1514)[9] (clinicaltrials.gov identifier: NCT00206245). After cleaning of data with regard to incorrect randomisation and inconsistencies in symptom data entry at baseline with respect to heartburn and dyspepsia inclusion/exclusion criteria (e.g. recording the symptom on 7 days/week but at no intensity), the number of patients included in our analysis for NERD was n=1415 and n =1460 for RO. With respect to the regurgitation domain (defined as the presence of an acid taste in the mouth and/or unpleasant movement of material upwards from the stomach), due to some incomplete reporting, there were n= 1359 evaluable patients with NERD and n=1398 with RO. QOLRAD scores with corresponding RDQ regurgitation data were available for slightly fewer patients (n = 1335 for NERD and n = 1368 for RO) than that available for the RDQ alone, owing to some missing QOLRAD data. Finally, patients with RO whose oesophagitis healed after 2 weeks of therapy did not continue in the study and therefore there were fewer evaluable RO patients at 4 weeks than there were NERD patients (n=849 vs. n=1191).
The relief of heartburn was an important outcome in each study. Both trials used the RDQ to identify patients for enrolment based on 7-day patient recall, and to assess the therapeutic effect of 4 weeks of potent acid suppression, by using an electronic diary twice daily; patients rated RDQ symptom intensity on a 4-point Likert scale of ‘none’ to ‘severe’. The RDQ is a psychometrically validated questionnaire [10, 11] that uses six patient-reported items to evaluate the frequency and intensity of heartburn, regurgitation and dyspeptic symptoms. An inclusion criterion common to both trials was that patients must have been experiencing heartburn (defined as ‘burning feeling behind the breastbone’ on the RDQ, abbreviated here to ‘substernal burning’) for at least 6 months, and also to recall having at least moderate intensity ‘substernal burning’ (sufficient to cause interference with normal activities) on ≥4 days in the week before randomisation. Regurgitation was defined as ‘unpleasant movement of material upwards from the stomach’ (abbreviated here to Regurgitation–movement) and/or ‘an acid taste in the mouth’ (abbreviated here to Regurgitation–taste). No specific inclusion or exclusion criteria were applied with regard to regurgitation symptoms. Patients with pain or burning in the centre of the upper stomach as their dominant RDQ symptom were excluded from the trials.
The Quality of Life in Reflux and Dyspepsia (QOLRAD) questionnaire [12] was used at baseline and at the end of the fourth week of therapy to assess the impact of heartburn and regurgitation on HRQOL. QOLRAD is a patient-completed psychometrically validated 25-item questionnaire that evaluates five dimensions: emotional distress, food/drink problems, sleep disturbance, physical/social functioning and vitality. Mean scores for each dimension were calculated from the 1–7 graded Likert scale used to assess how much or how often the GORD symptoms impacted on patient HRQOL (from “a great deal” or “all of the time” at 1 point to “not at all” or “none of the time” at 7 points). Thus, higher QOLRAD scores indicated better HRQOL. A difference of 0.5 points or more on the 1–7 graded Likert scale has been previously demonstrated to represent a clinically relevant change.[13]
We used pooled data for all treatment arms of each original study [8, 9] in our analysis because neither trial showed a significant difference (or even trend) in the major efficacy outcomes (relief of ‘substernal burning’ and healing of RO) achieved with esomeprazole or AZD0865 therapy, nor were differences seen across the dose range of AZD0865 (25–75 mg).
Statistical analysis
At baseline and week 4, the prevalence of RDQ symptoms were assessed. QOLRAD was analysed as mean score per dimension with 95% confidence intervals [CIs][14]. Descriptive statistics for mean QOLRAD scores were stratified by RDQ symptom frequency to analyse the impact of symptoms on HRQOL. All analyses were conducted for NERD and RO separately. SAS 8.2 (SAS Institute Inc., Cary, North Carolina, USA) was used for statistical analysis.
RESULTS
Prevalence of regurgitation at baseline
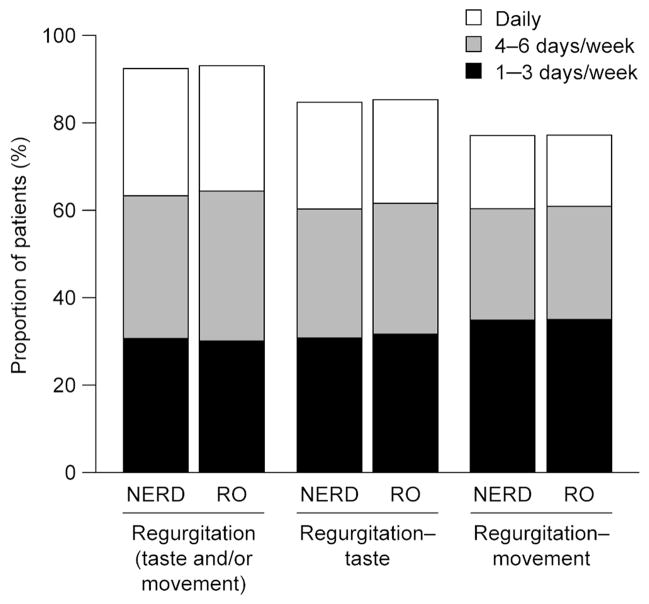
At baseline,1260 /1359 (93%) patients with NERD reported regurgitation (‘regurgitation–taste’, ‘regurgitation–movement’ or both), 1137/1338 (85%) reported ‘regurgitation–taste’ and 993/1284 (77%) reported ‘regurgitation–movement’ (Figure 1). For patients with RO, the corresponding baseline values were 1305/1398 (93%), 1190/1391 (86%) and 1038/1341 (77%) (Figure 1).
Figure 1.
The proportion of patients with regurgitation at baseline.
NERD, non-erosive reflux disease; regurgitation–movement, unpleasant movement of material upwards from the stomach; regurgitation–taste, an acid taste in the mouth; regurgitation, the presence of an acid taste in the mouth and/or unpleasant movement of material upwards from the stomach; RO, reflux oesophagitis.
Impact on HRQOL of regurgitation at baseline
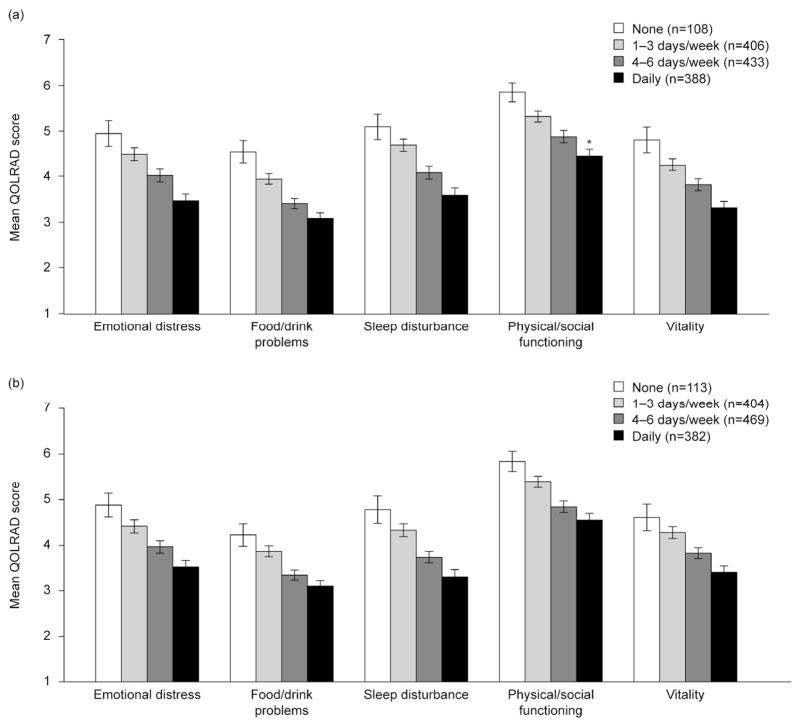
At baseline, there was an inverse association between the frequency of regurgitation and the mean QOLRAD scores in all five dimensions (Figure 2). As all patients had frequent and intense ‘substernal burning’ at baseline, this incremental decrease in HRQOL with regurgitation was in addition to the effects of heartburn. The HRQOL data for NERD and RO patients were similar, with the exception of sleep disturbance, which was slightly more negatively affected in patients with RO than in those with NERD. In patients with NERD, the baseline mean QOLRAD score for sleep disturbance ranged from 3.59 (95% CI 3.44 to 3.75) for those with daily regurgitation to 5.10 (95% CI 4.82 to 5.37) in those with no regurgitation, compared with 3.30 (95% CI 3.15 to 3.46) to 4.78 (95% CI 4.48 to 5.08) in patients with RO. Thus, the difference between the corresponding NERD and RO mean QOLRAD scores did not reach the level of clinical relevance (≥0.5 points) for any dimension. The data were similar for ‘regurgitation–taste’ and ‘regurgitation–movement’ when considered as separate items as it was for the regurgitation domain as a whole. The same pattern of decreasing QOLRAD score with increasing frequency of regurgitation was also observed (data not shown).
Figure 2.
Mean QOLRAD scores (error bars represent 95% confidence intervals) according to the presence and frequency of regurgitation at baseline for patients with (A) NERD (B) RO. *The number of patients with daily regurgitation in the physical/social functioning dimension was 387, rather than 388 as in the other dimensions (missing data).
NERD, non-erosive reflux disease; QOLRAD, The Quality of Life in Reflux and Dyspepsia; regurgitation, the presence of an acid taste in the mouth and/or unpleasant movement of material upwards from the stomach; RO, reflux oesophagitis.
The separation of the 95% CIs for all the mean QOLRAD scores at baseline supported a statistically significant difference between patients with 4–6 days/week of regurgitation vs. no regurgitation. Furthermore, the difference in mean QOLRAD scores between patients with 4–6 days/week of regurgitation vs. no regurgitation was considered clinically relevant since it exceeded 0.5 points (Figure 2). As expected, this difference was even more pronounced when comparing patients with no regurgitation vs. daily regurgitation. When the QOLRAD scores for ≥4 days/week and <4 days/week of regurgitation were compared (Table 1), this pattern of the difference between mean QOLRAD scores of >0.5 points without overlapping CIs was confirmed, suggesting that 4 days/week of regurgitation is a useful threshold for a clinically meaningful negative impact on HRQOL.
Table 1.
Mean QOLRAD scores with 95% confidence intervals for patients with non-erosive reflux disease or reflux esophagitis and <4 days/week vs.≥4 days/week of regurgitation at baseline.
| QOLRAD dimension | GORD group | Mean (95% CI) | |
|---|---|---|---|
| ≥4 days/week regurgitation | <4 days/week regurgitation | ||
| Emotional distress | NERD | 3.76 (3.66 to 3.87) | 4.60 (4.47 to 4.72) |
| RO | 3.77 (3.67 to 3.87) | 4.52 (4.39 to 4.65) | |
| Food/drink problems | NERD | 3.26 (3.18 to 3.34) | 4.07 (3.87 to 4.18) |
| RO | 3.23 (3.15 to 3.31) | 3.95 (3.84 to 4.06) | |
| Sleep disturbance | NERD | 3.85 (3.74 to 3.96) | 4.78 (4.66 to 4.90) |
| RO | 3.55 (3.45 to 3.65) | 4.43 (4.30 to 4.56) | |
| Physical/social functioning | NERD | 4.68 (4.58 to 4.78) | 5.43 (5.33 to 5.54) |
| RO | 4.71 (4.61 to 4.81) | 5.49 (5.38 to 5.60) | |
| Vitality | NERD | 3.59 (3.49 to 3.68) | 4.38 (4.26 to 4.50) |
| RO | 3.64 (3.54 to 3.73) | 4.35 (4.23 to 4.47) | |
GORD, gastro-oesophageal reflux disease; NERD, non-erosive reflux disease; RO, reflux oesophagitis
Prevalence of persistent regurgitation at week 4 of potent acid suppression
At 4 weeks, 791/1191 (66%) patients with NERD reported persistent regurgitation (‘regurgitation–taste’, ‘regurgitation–movement’ or both), 634/1191(53%) reported ‘regurgitation–taste’ and 674/1191 (57%) reported ‘regurgitation–movement’. For patients with RO, the corresponding week 4 values were 529/849 (62%), 401/849 (47%) and 455/849 (54%).
Impact of persistent regurgitation at week 4 of potent acid suppression
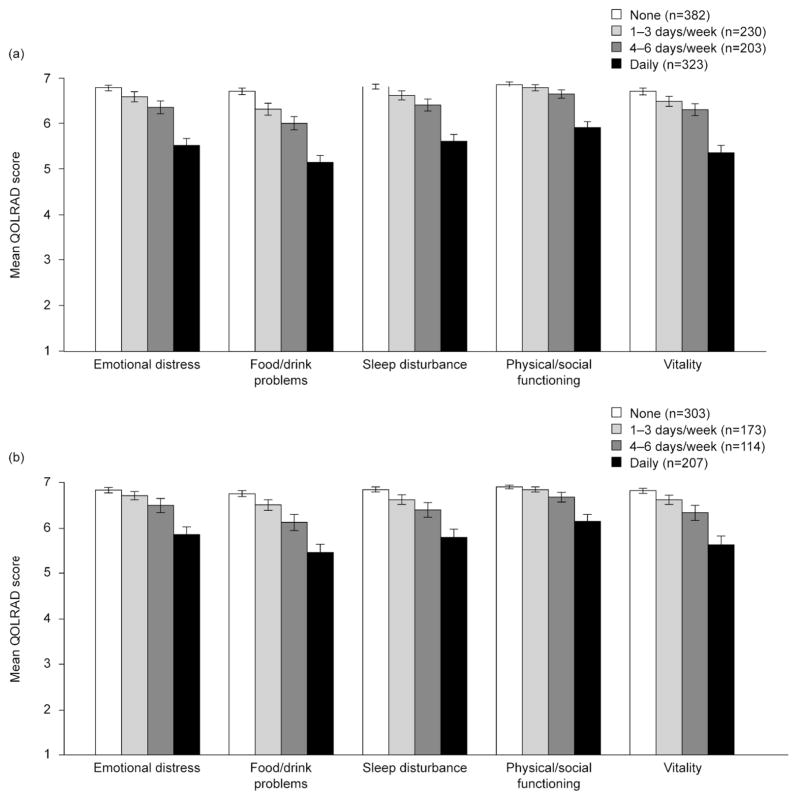
At week 4 of acid suppressive treatment, the mean QOLRAD scores for regurgitation increased from baseline by approximately 2 to 3 points, indicating a positive, clinically important therapeutic response. This general improvement was mainly owing to the response of ‘substernal burning’ with 4 weeks of treatment, irrespective of whether or not regurgitation was present. As seen at baseline, an incremental decrease in HRQOL was observed with higher frequencies of persistent regurgitation following 4 weeks of acid suppression (Figure 3). This was also the case for regurgitation–taste and regurgitation–movement as separate dimensions (data not shown). When the same comparison used at baseline was performed (≥4 days/week vs.<4 days/week of persistent regurgitation), there was still a clinically relevant difference between the groups (Table 2). At 4 weeks, however, the negative incremental impact on HRQOL seemed to be driven by those patients who had persistent daily regurgitation (Figure 3).
Figure 3.
Mean QOLRAD scores (error bars represent 95% confidence intervals) according to the presence and frequency of persistent regurgitation at week 4 for patients with (A) NERD and (B) RO.
NERD, non-erosive reflux disease; QOLRAD, The Quality of Life in Reflux and Dyspepsia; regurgitation, the presence of an acid taste in the mouth and/or unpleasant movement of material upwards from the stomach; RO, reflux oesophagitis.
Table 2.
Mean QOLRAD scores with 95% confidence intervals for patients with non-erosive reflux disease or reflux esophagitis and ≥4 days/week vs. <4 days/week of regurgitation at week 4 of therapy.
| QOLRAD dimension | GORD group | Mean (95% CI) | |
|---|---|---|---|
| ≥4 days/week regurgitation | <4 days/week regurgitation | ||
| Emotional distress | NERD | 5.84 (5.72 to 5.95) | 6.71 (6.65 to 6.76) |
| RO | 6.10 (5.97 to 6.22) | 6.80 (6.75 to 6.85) | |
| Food/drink problems | NERD | 5.48 (5.36 to 5.59) | 6.55 (6.49 to 6.62) |
| RO | 5.71 (5.58 to 5.85) | 6.68 (6.62 to 6.74) | |
| Sleep disturbance | NERD | 5.91 (5.80 to 6.02) | 6.74 (6.68 to 6.79) |
| RO | 6.02 (5.90 to 6.15) | 6.77 (6.72 to 6.83) | |
| Physical/social functioning | NERD | 6.19 (6.09 to 6.29) | 6.83 (6.79 to 6.88) |
| RO | 6.35 (6.24 to 6.46) | 6.89 (6.86 to 6.92) | |
| Vitality | NERD | 5.73 (5.61 to 5.84) | 6.61 (6.55 to 6.68) |
| RO | 5.90 (5.76 to 6.04) | 6.75 (6.70 to 6.81) | |
GORD, gastro-oesophageal reflux disease; NERD, non-erosive reflux disease; RO, reflux oesophagitis
Prevalence of persistent regurgitation at week 4 in patients whose heartburn responded to potent acid suppression
At week 4, ‘substernal burning’ had responded to treatment (defined as having ≤1 day/week of persistent ‘substernal burning’ of mild intensity) in 667/1191(56%) evaluable patients with NERD and 533/849 (63%) with RO. The prevalence of frequent, persistent regurgitation (defined as ≥4 days/week) among heartburn responders in NERD was 186/667 (28%) for regurgitation, 96/667 (14%) for ‘regurgitation–taste’ and 137/667 (21%) for ‘regurgitation–movement’; in RO, the values were 120/533 (23%), 69/533 (13%) and 84/533 (16%) respectively.
Impact on HRQOL of persistent regurgitation at week 4 in patients whose heartburn responded to potent acid suppression
At week 4, a decrease in HRQOL was observed with greater frequencies (≥4 days/week) of persistent regurgitation in patients whose ‘substernal burning’ responded (who had at most 1 day/week of mild heartburn) to acid suppression. Thus, the pattern was the same in the subset of patients who had ‘substernal burning’ relief at week 4 as in the whole patient population at week 4 (data not shown). This is an important finding because although the detrimental impact of regurgitation is less substantial in the patients with heartburn relief, it is still measurable and relevant given that heartburn is no longer a confounding influence. However, although there was a lack of overlap between the 95% CIs for patients with 4–6 days/week of regurgitation vs. no persistent regurgitation, an absolute difference in QOLRAD scores of >0.5 points was only found in one of the five QOLRAD dimensions (food/drink problems) in the NERD cohort. Thus, 4 days/week of persistent regurgitation remained a threshold for clinical relevance in only this dimension for those NERD patients with relieved ‘substernal burning’ at week 4. In the RO cohort, no absolute differences of >0.5 points were observed in any of the QOLRAD dimensions for all aspects of regurgitation (data not shown) and there was no clear threshold for the RO subset with resolved ‘substernal burning’, although an absolute difference in QOLRAD scores of >0.5 points was seen for those with daily regurgitation compared with those with none.
Evidence for the negative impact of regurgitation on HRQOL beyond that of Heartburn
In patients without regurgitation at baseline, frequent ‘substernal burning’ was associated with a clinically relevant reduction in mean QOLRAD scores of approximately 1–3 points from the maximum of 7 points. In patients with concomitant regurgitation at baseline, mean QOLRAD scores were incrementally further reduced by approximately 1–1.5 points (Figure 2). A clinically relevant difference (>1 point) in mean QOLRAD scores was observed between patients with daily vs. no regurgitation at baseline, all of whom had frequent and intense ‘substernal burning’ (Table 3).
Table 3.
Mean QOLRAD scores with 95% confidence intervals for patients with non-erosive reflux disease or reflux esophagitis and daily vs. no regurgitation at baseline and at week 4.
| QOLRAD dimension | GORD group | Mean (95% CI) | |||
|---|---|---|---|---|---|
| Patients with frequent and intense heartburn and daily regurgitation at baseline (NERD, n = 388*; RO, n = 382) | Patients with frequent and intense heartburn and no regurgitation at baseline (NERD, n = 108; RO, n = 113) | Patients with no or greatly improved heartburn at week 4 and daily regurgitation (NERD, n = 78; RO, n = 60) | Patients with no or greatly improved heartburn at week 4 and no regurgitation (NERD, n = 324; RO, n = 264) | ||
| Emotional distress | NERD | 3.47 (3.33 to 3.62) | 4.95 (4.67 to 5.23) | 6.13 (5.86 to 6.40) | 6.87 (6.82 to 6.92) |
| RO | 3.52 (3.38 to 3.67) | 4.88 (4.62 to 5.14) | 6.38 (6.13 to 6.63) | 6.88 (6.83 to 6.93) | |
| Food/drink problems | NERD | 3.09 (2.97 to 3.21) | 4.55 (4.31 to 4.80) | 5.87 (5.59 to 6.14) | 6.80 (6.74 to 6.86) |
| RO | 3.10 (2.98 to 3.22) | 4.23 (3.98 to 4.47) | 6.13 (5.85 to 6.41) | 6.84 (6.79 to 6.90) | |
| Sleep disturbance | NERD | 3.59 (3.44 to 3.75) | 5.10 (4.82 to 5.37) | 6.32 (6.10 to 6.55) | 6.90 (6.85 to 6.94) |
| RO | 3.30 (3.15 to 3.46) | 4.78 (4.48 to 5.08) | 6.27 (5.97 to 6.58) | 6.90 (6.85 to 6.95) | |
| Physical/social functioning | NERD | 4.46 (4.31 to 4.61) | 5.85 (5.64 to 6.06) | 6.45 (6.27 to 6.64) | 6.92 (6.88 to 6.97) |
| RO | 4.55 (4.40 to 4.70) | 5.84 (5.62 to 6.06) | 6.49 (6.24 to 6.75) | 6.94 (6.91 to 6.97) | |
| Vitality | NERD | 3.32 (3.19 to 3.46) | 4.81 (4.53 to 5.09) | 6.06 (5.81 to 6.31) | 6.83 (6.77 to 6.88) |
| RO | 3.40 (3.26 to 3.54) | 4.61 (4.32 to 4.90) | 6.20 (5.89 to 6.51) | 6.88 (6.82 to 6.93) | |
Physical/social functioning n = 387.
GORD, gastro-oesophageal reflux disease; NERD, non-erosive reflux disease; RO, reflux oesophagitis
Although the increase of 2 to 3 points in QOLRAD scores with treatment at week 4 was driven by heartburn improvement (Figure 3), a smaller, but still clinically relevant difference (>0.5 points) was observed between patients with daily vs. no regurgitation, all of whom had no or greatly improved ‘substernal burning’ (≤1 day/week of mild heartburn) (Table 3).
This suggests that the presence of frequent regurgitation had an additional negative impact on HRQOL to that of ‘substernal burning’ at baseline as well as after 4 weeks of potent acid suppression.
DISCUSSION
The impact of regurgitation on HRQOL in patients with GORD has not previously been extensively studied. In the analysis reported here, data from two large, randomised clinical trials with well-defined NERD and RO populations were used to assess the relationship between patient-reported regurgitation and HRQOL. The major finding was that frequent regurgitation (≥4 days/week) was associated with a consistent clinically relevant reduction in the HRQOL of GORD patients, which was incremental to that associated with heartburn. Indeed, the frequency dependent pattern with which regurgitation reduced HRQOL was observed both at baseline (when all patients had frequent and intense heartburn) and after 4 weeks of potent acid suppression in a mix of patients with and without complete resolution of ‘substernal burning’, in both NERD and RO. The similarity of the data for NERD and RO patients suggests that the association between the increasing frequency of regurgitation and decreasing HRQOL is independent of the presence of RO.
The overarching definition of GORD devised by the Montreal consensus is ‘a condition which develops when the reflux of stomach contents causes troublesome symptoms and/or complications.’[7] That consensus document went on to review HRQOL data pertinent to the cardinal GORD symptoms, heartburn and regurgitation. In the case of heartburn, the threshold at which the symptom becomes ‘troublesome’ as evident by a clinically relevant decrement in HRQOL was ≥2 days/week of mild symptoms or ≥1 day/week of ≥moderate symptoms. No thresholds were proposed for other GORD symptoms because no relevant data could be found in the literature. Data provided in this analysis suggest that for the other cardinal GORD symptom, regurgitation, patients reporting ‘regurgitation–taste’ and/or ‘regurgitation–movement’ of at least mild intensity on ≥4 days/week in addition to frequent and intense ‘substernal burning’ (at baseline) or in the whole patient group at 4 weeks, had a clinically meaningful reduction in HRQOL compared with those with a lesser frequency (or no) regurgitation. Hence, based on our data, a reasonable definition of ‘troublesome’ or problematic regurgitation seems to be regurgitation occurring ≥4 days per week. At this frequency threshold, regurgitation negatively affects HRQOL, even in patients with good control of heartburn. We focused our analysis on the frequency of regurgitation rather than the intensity of regurgitation because frequency was considered the more objective and robust measurement for this essentially dichotomous symptom. Furthermore, previous analysis found that there was a reasonable correlation between frequency and intensity of GORD symptoms.[15]
Frequent, persistent regurgitation was relatively common in patients with NERD (28%) and RO (23%) despite a good response of ‘substernal burning’ to 4 weeks of potent acid suppression. However, in the subset of NERD patients who had relieved ‘substernal burning’ at week 4, a threshold of ≥4 days/week of persistent regurgitation remained a reliable discriminator of clinically relevant problematic regurgitation in only the ‘food/drink problems’ dimension.
This study was strengthened by the use of a large prospective dataset with precise definitions of regurgitation. Furthermore, symptoms were patient-reported, a more appropriate and valid method of data collection than clinician assessment when measuring a concept best known by the patient.[16] A limitation of this analysis was that the prevalence and response of regurgitation to therapy was not a primary outcome in the original studies. The primary outcome measure was the time to sustained absence of heartburn in the NERD trial [8] and the comparative healing of oesophagitis in the RO trial.[9] In addition, all the included patients had concomitant frequent and intense heartburn at baseline, suggesting that further study would be required to confirm whether the frequency threshold for the negative impact of regurgitation on HRQOL proposed here (≥4 days per week) is applicable in GORD populations with less severe heartburn at baseline.
To date, treatment success in RO has mainly been assessed based on the objective endpoint of healing of oesophagitis. Since the mean QOLRAD scores were so similar for patients with NERD and for those with RO, the data suggest that symptoms, rather than the presence of oesophagitis, have the greatest impact on HRQOL. With respect to symptoms, both RO and NERD trials have mainly evaluated the relief or resolution of heartburn. However, this study demonstrated approximately one-quarter of patients with GORD still had frequent regurgitation, despite heartburn relief. This is in line with the findings of two other studies derived from this dataset,[5, 6] reporting that the responsiveness of individual GORD symptoms was not equivalent and that regurgitation was not as responsive as heartburn to potent acid suppression. These data suggest that persistent regurgitation may be a relatively common characteristic of patients with GORD who do not respond fully to therapy. Thus, evaluation of treatment response of GORD requires a more comprehensive symptom assessment than simply quantifying heartburn. Specifically, since regurgitation seems to be present before treatment in most patients with heartburn and persistent regurgitation is a frequent phenotype of incomplete treatment response, trials should consider regurgitation as both an entry criterion and a primary outcome. This could lead to a more thoughtful approach to therapy, targeting specific troublesome symptoms rather than using a ‘one size fits all’ approach. Patients with predominant heartburn are likely to respond to potent acid suppression, whereas those with predominant regurgitation may require alternative or adjunctive treatment, such as reflux inhibitors or surgical interventions, although this can only be recommended if the response to these therapies has been compared to the current gold standard (PPIs) in well-designed trials.
The differing response of heartburn and regurgitation to acid suppression may be at least in part attributable to the contribution of mechanical stimuli, as opposed to chemical stimuli, in the perception of regurgitation, whilst the burning feeling of heartburn is dominated by chemical stimuli, specifically the pH of the refluxate.[17] PPI and AZD0865 therapy reduces gastric acid secretion, although they have distinct mechanisms of action to do so.[9] Hence, on acid suppression, there is less potential for acid to enter the oesophagus, mouth, or hypopharynx and the chemical stimulation for the perception of heartburn is substantially reduced. Reduced acid secretion also has the secondary effect of reducing the volume of fluid in the stomach available to reflux into the oesophagus.[18] The volume of reflux, irrespective of its acidity, influences its intraluminal distribution and the degree of resultant oesophageal distension.[17] Smaller volumes of refluxate will result in less oesophageal distension and therefore the mechanical stimulation of the oesophageal nociceptors for the perception of regurgitation maybe reduced. However, a multitude of other factors including the rate of gastric emptying, the volume of the meal consumed, the presence of hiatus hernia, and the degree of oesophagogastric junction incompetence could also influence the volume of refluxate and these factors will not be significantly affected by acid suppression therapy. Hence, one might anticipate a lesser therapeutic response with acid suppression for regurgitation than for heartburn.
In conclusion, we retrospectively evaluated a robust dataset from two large GORD trials, one of patients with NERD and one of RO to ascertain the impact of regurgitation on HRQOL. We found that the frequency of regurgitation, reported as ‘regurgitation–taste’ and/or ‘regurgitation–movement’, had an incremental negative impact on HRQOL over that associated with heartburn in GORD patients particularly before but also after 4 weeks of potent acid suppression. Importantly, regurgitation still had a detrimental effect on HRQOL in patients whose heartburn was relieved by potent acid suppression therapy. The threshold frequency at which regurgitation became ‘troublesome’ evident by a clinically meaningful reduction in HRQOL was ≥4 days/week. This association was independent of the presence of RO. We conclude that persistent regurgitation is a frequent phenotype of incomplete response to PPIs and that GORD treatment trials should incorporate regurgitation into patient assessment to more completely capture the impact of GORD on HRQOL.
SIGNIFICANCE OF THIS STUDY.
What is already known about this subject?
Recent publications suggest that regurgitation typically responds less well than heartburn to acid suppression.
Studies on the negative impact of gastro-oesophageal reflux disease (GORD) symptoms on health-related quality of life (HRQOL) have tended to focus on the effect of heartburn and little is known about the impact of regurgitation.
What are the new findings?
At baseline, all patients had frequent and intense heartburn and most also had regurgitation. A quarter of patients whose heartburn responded to acid suppression therapy still had frequent regurgitation.
The frequency of regurgitation was negatively associated with HRQOL, both before and after therapy. This association was incremental to that attributable to concomitant heartburn and was irrespective of the presence of reflux oesophagitis.
Regurgitation on ≥4 days/week is suggested as a clinically relevant threshold for the negative impact on HRQOL.
How might it impact on clinical practice in the foreseeable future?
The evaluation of treatment response in GORD requires a more comprehensive symptom assessment than simply quantifying heartburn.
A more differentiated approach to therapy in patients with GORD, specifically targeting troublesome symptoms, is needed in clinical practice.
Acknowledgments
Funding This study was supported by AstraZeneca R&D, Mölndal, Sweden.
Study approval: This was a post hoc analysis of existing clinical trial data (clinicaltrials.gov identifiers: NCT00206284 and NCT00206245), and therefore did not require approval. Local ethics committee approval was obtained in the participating countries and written informed consent was required from all participants before study enrolment in the original clinical trials.
Footnotes
Guarantor of the article
Peter Kahrilas accepts full responsibility for the conduct of the study.
Contributors
Peter Kahrilas took a lead in determining the study concept and design, analysing and interpreting the data, as well as drafting and critically reviewing the manuscript for important clinical and intellectual content. Andreas Jonsson had a role in data acquisition, performed the statistical analysis and critically reviewed the manuscript drafts. Hans Denison had a role in determining the study concept and design, analysing and interpreting the data, as well as drafting and critically reviewing the manuscript for important clinical and intellectual content. Börje Wernersson had a role in determining the study concept and design, analysing and interpreting the data, as well as drafting and critically reviewing the manuscript. Nesta Hughes had a role in analysing and interpreting the data, as well as drafting and critically reviewing the manuscript. Colin W. Howden had a major role in determining the study concept and design, analysing and interpreting the data, as well as drafting and critically reviewing the manuscript for important clinical and intellectual content. All authors have approved the final draft of the manuscript.
Copyright licence
“The Corresponding Author has the right to grant on behalf of all authors and does grant on behalf of all authors, an exclusive licence (or non-exclusive for government employees) on a worldwide basis to the BMJ Group and co-owners or contracting owning societies (where published by the BMJ Group on their behalf), and its Licensees to permit this article (if accepted) to be published in Gut and any other BMJ Group products and to exploit all subsidiary rights, as set out in our licence.”
Competing interests: Peter Kahrilas has acted as a consultant for AstraZeneca, Eisai, EndoGastric Solutions, Ironwood, Novartis, and XenoPort. Andreas Jonsson, Hans Denison and Börje Wernersson are employees of AstraZeneca R&D, Mölndal, Sweden. Nesta Hughes is an employee of Oxford PharmaGenesis™ Ltd, Oxford, UK, which has received funding from AstraZeneca R&D, Mölndal, Sweden. Colin Howden has acted as a consultant for Boehringer Ingelheim, Novartis Consumer Health, Novartis Oncology, Otsuka, Takeda, Perrigo and XenoPort, and as a speaker for Novartis, Otsuka, Ironwood, Forest Laboratories, Takeda and GlaxoSmithKline.
References
- 1.van Pinxteren B, Sigterman KE, Bonis P, et al. Short-term treatment with proton pump inhibitors, H2-receptor antagonists and prokinetics for gastro-oesophageal reflux disease-like symptoms and endoscopy negative reflux disease. Cochrane Database Syst Rev. 2010:CD002095. doi: 10.1002/14651858.CD002095.pub4. [DOI] [PubMed] [Google Scholar]
- 2.El-Serag H, Becher A, Jones R. Systematic review: persistent reflux symptoms on proton pump inhibitor therapy in primary care and community studies. Aliment Pharmacol Ther. 2010;32:720–37. doi: 10.1111/j.1365-2036.2010.04406.x. [DOI] [PubMed] [Google Scholar]
- 3.Donnellan C, Sharma N, Preston C, et al. Medical treatments for the maintenance therapy of reflux oesophagitis and endoscopic negative reflux disease. Cochrane Database Syst Rev. 2005;2:CD003245. doi: 10.1002/14651858.CD003245.pub2. [DOI] [PubMed] [Google Scholar]
- 4.Kahrilas PJ, Howden CW, Hughes N. Response of regurgitation to proton pump inhibitor therapy in clinical trials of gastroesophageal reflux disease. Am J Gastroenterol. 2011;106:1419–25. doi: 10.1038/ajg.2011.146. [DOI] [PubMed] [Google Scholar]
- 5.Kahrilas PJ, Jonsson A, Denison H, et al. Regurgitation is less responsive to acid suppression than heartburn in patients with gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2012;10:612–9. doi: 10.1016/j.cgh.2012.01.022. [DOI] [PubMed] [Google Scholar]
- 6.Kahrilas PJ, Jonsson A, Denison H, et al. Concomitant symptoms itemized in the Reflux Disease Questionnaire are associated with attenuated heartburn response to acid suppression. Am J Gastroenterol. 2012;107:1354–60. doi: 10.1038/ajg.2012.197. [DOI] [PubMed] [Google Scholar]
- 7.Vakil N, Veldhuyzen van Zanten S, Kahrilas P, et al. The Montreal definition and classification of gastro-esophageal reflux disease (GERD) – a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–20. doi: 10.1111/j.1572-0241.2006.00630.x. [DOI] [PubMed] [Google Scholar]
- 8.Dent J, Kahrilas PJ, Hatlebakk J, et al. A randomized, comparative trial of a potassium-competitive acid blocker (AZD0865) and esomeprazole for the treatment of patients with nonerosive reflux disease. Am J Gastroenterol. 2008;103:20–6. doi: 10.1111/j.1572-0241.2007.01544.x. [DOI] [PubMed] [Google Scholar]
- 9.Kahrilas PJ, Dent J, Lauritsen K, et al. A randomized, comparative study of three doses of AZD0865 and esomeprazole for healing of reflux esophagitis. Clin Gastroenterol Hepatol. 2007;5:1385–91. doi: 10.1016/j.cgh.2007.08.014. [DOI] [PubMed] [Google Scholar]
- 10.Shaw MJ, Talley NJ, Beebe TJ, et al. Initial validation of a diagnostic questionnaire for gastroesophageal reflux disease. Am J Gastroenterol. 2001;96:52–7. doi: 10.1111/j.1572-0241.2001.03451.x. [DOI] [PubMed] [Google Scholar]
- 11.Dent J, Vakil N, Jones R, et al. Accuracy of the diagnosis of GORD by questionnaire, physicians and a trial of proton pump inhibitor treatment: the Diamond Study. Gut. 2010;59:714–21. doi: 10.1136/gut.2009.200063. [DOI] [PubMed] [Google Scholar]
- 12.Wiklund IK, Junghard O, Grace E, et al. Quality of life in reflux and dyspepsia patients. psychometric documentation of a new disease-specific questionnaire (QOLRAD) Eur J Surg Suppl. 1998;583:41–9. [PubMed] [Google Scholar]
- 13.Talley NJ, Fullerton S, Junghard O, et al. Quality of life in patients with endoscopy-negative heartburn: reliability and sensitivity of disease-specific instruments. Am J Gastroenterol. 2001;96:1998–2004. doi: 10.1111/j.1572-0241.2001.03932.x. [DOI] [PubMed] [Google Scholar]
- 14.Engels LGJB, Klinkenberg-Knol EC, Carlsson J, et al. Psychometric validation of the Dutch translation of the quality of life in reflux and dyspepsia (QOLRAD) questionnaire in patients with gastroesophageal reflux disease. Health Qual Life Outcomes. 2010;8:85. doi: 10.1186/1477-7525-8-85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Jones R, Junghard O, Dent J, et al. Development of the GerdQ, a tool for the diagnosis and management of gastro-oesophageal reflux disease in primary care. Aliment Pharmacol Ther. 2009;30:1030–8. doi: 10.1111/j.1365-2036.2009.04142.x. [DOI] [PubMed] [Google Scholar]
- 16.Food and Drug Administration. Patient-reported outcome measures: use in medical product development to support labeling claims. Rockville, USA: Food and Drug Administration; Dec 8, 2009. [Accessed 29 January 2013]. Available: http://www.fda.gov/downloads/Drugs/GuidanceComplianceRegulatoryInformation/Guidances/UCM193282.pdf. [Google Scholar]
- 17.Sifrim D, Mittal R, Fass R, et al. Review article: Acidity and volume of the refluxate in the genesis of gastro-oesophageal reflux disease symptoms. Aliment Pharmacol Ther. 2007;25:1003–15. doi: 10.1111/j.1365-2036.2007.03281.x. [DOI] [PubMed] [Google Scholar]
- 18.Howden CW, Forrest JA, Reid JL. Effects of single and repeated doses of omeprazole on gastric acid and pepsin secretion in man. Gut. 1984;25:707–10. doi: 10.1136/gut.25.7.707. [DOI] [PMC free article] [PubMed] [Google Scholar]