Abstract
Objective
To evaluate a 12-session home and community-based health promotion/obesity prevention program (Challenge!) on changes in BMI, body composition, physical activity (PA), and diet.
Methods
235 African-American adolescents (11–16 yrs, 38% overweight/obese) were recruited from low-income urban communities. Baseline measures included weight, height, body composition (dual-energy x-ray absorptiometry (DEXA) and bioelectrical impedance), physical activity (PA) (accelerometry), and diet (food frequency). PA was measured by time in play-equivalent physical activity (PEPA≥1800 activity counts/min). Participants were randomized into a home- and community-based health promotion/obesity prevention controlled trial, anchored in social cognitive theory and involving motivational interviewing techniques, and delivered by college-enrolled, African-American mentors. Control adolescents did not receive the intervention or a mentor. Post-intervention (10 mos) and delayed follow-up (24 mos) evaluations were conducted. Longitudinal analyses using random mixed effects models and generalized estimating equations (GEE) examined direct and moderated effects of time, gender, and baseline BMI category on changes at both follow-ups.
Results
Retention was 76% (178/235) over 2 years; overweight/obese status declined 5.3% among intervention adolescents and increased 11.3% among control adolescents (χ2=5.8, p=0.02, GEE). Among males, but not females, fat free mass was significantly higher among intervention members at both follow-up evaluations. PA effects were moderated by baseline BMI category; among adolescents ≥ 85th percentile, control adolescents averaged 25.5 min less daily activity than intervention adolescents (p=0.018) at the 10-mo, but not the 24-mo follow-up. Intervention adolescents declined significantly more in snack and dessert consumption than control adolescents (p=0.045).
Conclusion
A 12-session, home-and community-based intervention, based on social cognitive theory and delivered by college-enrolled mentors, had sustained effects over 24 months in preventing an increase in BMI category, in enhancing fat free mass among males, and in reducing snack and dessert intake. The intervention prevented PA declines among the heaviest adolescents, but effects were not sustained.
Keywords: adolescent obesity prevention, adolescence, overweight, intervention, randomized controlled trial, mentor, African American, physical activity, diet
Pediatric obesity1 has increased threefold over the past three decades, particularly among minority children from low-income families (1–5). As a defining health issue of the 21st century, pediatric obesity is associated with immediate and long-term health problems, including hypertension, asthma, musculoskeletal problems, obstructive sleep disorders, Type 2 diabetes, depression, and social stigmatization (6–9).
Although multiple programs have attempted to reduce the prevalence of pediatric obesity, reviews (17) and meta-analyses (18) find limited impact on BMI. Our study was designed to address a common criticism, the lack of attention to home and community activities {19, 20, Gittelsohn, 2007}. We focused on adolescents because not only are adolescents are risk for weight gain (21) which is likely to be sustained into adulthood (10–13), but with increasing independence and access to their local community, they make decisions related to diet and physical activity (PA) (23).
We conducted a randomized, controlled trial of a home- and community-based health promotion/obesity prevention program for urban African American adolescents, anchored in social cognitive theory and involving motivational interviewing techniques, and delivered by specially trained, college-enrolled, African American mentors. Our primary outcome was the accretion of body mass and body fat at10-mo and 24-mo follow-ups. Our secondary outcomes were changes in PA and eating habits.
Methods
Participants
The trial was based at a mid-Atlantic, urban, university medical center with two samples of adolescents. The first (N=84) participated in a longitudinal investigation of growth and development. Approximately 17.9% experienced growth faltering by age 2y, but by age 6y, their growth had recovered (24). The second (N=151) was recruited from middle-schools. Eligibility criteria for both samples included age (11 to 16y) and residence in the low-income communities surrounding the medical center. Eligibility was not based on body weight, nor was body weight mentioned in recruitment materials.
Procedure
The protocol was approved by the University of Maryland Baltimore Institutional Review Board. Written informed assent and consent were obtained and participants were compensated for evaluations.
Adolescents and caregivers participated in a baseline evaluation between 7/2002 and 5/2004, including anthropometrics and questionnaires on demographics, diet, and PA. Questionnaires were self-administered on a laptop computer using voice-generating software and mouse responses.
Randomization was stratified by growth history, overweight/obese status, gender, and age. Intervention adolescents were paired with a race and gender-matched (>90%) college-enrolled (age 19–25 y) mentor. Mentors received approximately 40 hours of training, including motivational interviewing (26), and had weekly supervision during the intervention. They delivered the intervention in the adolescents’ homes and accompanied them on field trips to community sites (e.g. convenience stores).
The manualized 12-session intervention, “Challenge,” was based on social cognitive theory (25), developed with an advisory board of African American adolescents, and included a rap music video promoting healthy eating and PA. Principles of mentorship (role modeling and support), participatory learning, and goal setting were central to the intervention. In addition to setting dietary and PA goals, tracking and evaluating progress, and revising goals as necessary, intervention adolescents made and tasted healthy snacks and engaged in PA. Control adolescents did not receive a mentor or any contact between baseline and follow-up evaluations.
Two follow-up evaluations were conducted: post-intervention at approximately 10 months and delayed follow-up at approximately 24 months. Adolescents and caregivers returned to the medical center and repeated the baseline evaluations. Research assistants were unaware of participants’ intervention status or baseline findings.
Measures
Adolescents and caregivers reported basic demographic information, including age, gender, race/ethnicity, highest grade completed, family size, and family income.
Anthropometry
Research assistants collected anthropometrics for adolescents and caregivers. Height was measured (0.1 cm) with a wall-mounted standiometer and weight was measured (0.5 pounds) with a digital scale (Tanita Co. Tokyo, Japan). Adolescents’ BMI was calculated (kg/m2), converted to z-scores and percentiles (28), and used to form categories: normal (<85th percentile), overweight (>85th percentile and <95thpercentile), and obese (≥95th percentile). (1) Caregivers’ BMI was used to form categories: normal (BMI<25 kg/m2), overweight (BMI≥25 kg/m2 and <30 kg/m2), and obese (BMI≥30 kg/m2).
Body Composition
Participants were measured by the body impedance analysis (BIA) method, using a TANITA 300GS instrument (Tanita Corp., Tokyo, Japan). Body fat percentage was calculated using the instrument’s software. Dual energy X-ray absorptiometry (DEXA) scan was included for the final 75% of participants enrolled. The DEXA scan was performed using a QDR 4500 W scanner (Hologic, Inc; Bedfod, MA) in whole-body mode. Percentage body fat, fat mass (kg), and fat free mass (kg) were calculated using manufacturer-provided software. Because the accuracy of DEXA is superior to that of BIA (ref), we performed analyses pertaining to body composition using the DEXA subset data only.
PA
We placed a uniaxial accelerometer (Actiwatch; Respironics, Inc.; Bend, OR) on each adolescent’s right ankle with a non-removable, reinforced hospital band. Adolescents wore the accelerometer for ≥9 days next to the skin, under socks. Actiwatch software was used to reduce the data, based on days with complete data (24 hours with average ≥100 counts/min). Adolescents had an average of 6.16 complete days (SD=0.80).
Time in sleep was excluded by eliminating 1-hour blocks of time with average activity <55 counts/min, resulting in average sleep time of 8.05 hours/night (SD=0.98). Two summary scores were created: average daily PA counts/minutes and minutes/day in play-equivalent physical activity (PEPA).
PEPA was defined based on a methodological substudy in a similar population of adolescents (8). The adolescents wore Actiwatch accelerometers on the right knee and ankle during a 20-minute free-play session in a gymnasium furnished with age-appropriate equipment. Knee placement of the Actiwatch has been correlated with energy expenditure, (29) but ankle placement was preferred by participants. Ankle and knee placement counts were highly correlated (r=0.94, p<0.001). We selected periods with >1800 counts/min as a threshold for PEPA. Both average daily activity counts/min and PEPA were logarithmically transformed to approximate a normal distribution.
Yan comments: Hi, based on the original table, only average daily activity counts/min is log transformed, PEPA was not log transformed----I do not change this table since it is where we found significant findings (preventive effect for the overweight or obese youth). Please feel free to let me know if you would like to log transform this variable.
Diet
Dietary patterns were measured with the Youth Adolescent Food Frequency Questionnaire (YAQ), a 131-item instrument developed and validated for adolescents. (30, 31) The YAQ was self-administered and adolescents reported on foods consumed over the past 12 months. Responses were analyzed by Epidemiology Center for Cancer Prevention, Channing Laboratory, Harvard University. We analyzed total energy intake (kcal), total dietary fat, saturated fat, fiber, calcium, fruits (servings/day), vegetables (servings/day), snacks and desserts (servings/day), milk (servings/day), non-diet soda (servings/day), fried foods (servings/day). Adolescents whose energy intake were beyond 3 standard deviations from the means were considered as outliers and were excluded from the analyses on the total energy intake (n=4 for baseline, n=3 for post-intervention, and n=3 for delayed follow-up). There were no differences in results of analyses conducted with and without these adolescents for other variables; therefore all data were retained for analyses on other variables.
Analysis Plan
Intention-to-treat analyses were conducted. Data were checked for skewness, kurtosis, and extreme outliers. Preliminary analyses were conducted to examine baseline differences between intervention and control group with T tests for the continuous variables and Chi-square analyses for categorical variables. Figures were used to illustrate the change of outcome variables across time by intervention.
Multilevel modeling with random intercept was used for the continuous outcome variables to account for the clustering of outcome measures over time within individuals (32, 33). Main effects of intervention, time after baseline assessment (in yr), and interaction between intervention and time were assessed after controlling for the baseline age and gender with the “proc mixed” command of SAS software package (SAS version 9.1; SAS Institute Inc., Cary, NC), (Mujahid, (35). Generalized estimating equations (GEE) was used for the categorical variable “Overweight/Obese”. Similarly the main effects of intervention, time after baseline assessment and interaction between intervention and time were assessed after controlling for the baseline age and gender of the youth (PROC GENMOD SAS version 9.1; SAS Institute Inc., Cary, NC, Liang and Zeger, 1986). The significant interaction between time and intervention suggests significant intervention effect {Fitzmaurice} on the change of the outcome variables.
To explore whether gender or overweight/obese status modified the relationship between intervention and time, we conducted stratified analyses by gender or by overweight/obese status instead of three-way interaction due to concern on the statistical power related to the limited sample size in this study.
Results
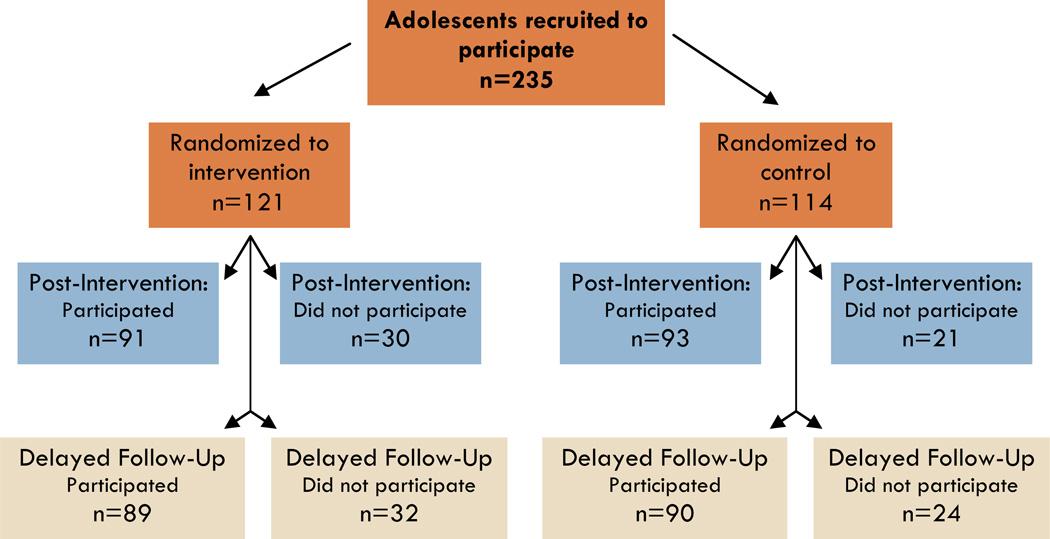
A total of 235 adolescents were recruited (Figure 1, Table 1). The mean age was 13.3 years (SD=1.0); 49% female, 97% African American, 12% overweight, and 26% obese. A total of 121 (52%) were randomized to intervention and 114 (48%) to control. Forty-two adolescents experienced growth deficiency early in life, and were evenly divided by intervention status. The intervention and control adolescents did not differ significantly on any baseline parameter other than overweight status. However, there is no significant difference between intervention and control with regard to the z-sccore of the BMI. Within the intervention, 52% (62/121) attended at least 10 of 12 sessions, 15% (18/121) attended none, and 33% (41/121) attended an average of 4.6 sessions (SD=2.7).
Figure 1.
Flow of participants recruited, randomized, and followed
Table 1.
Baseline demographics of the participants by intervention status
| Intervention Mean (SD) or n(%) |
Control Mean (SD) or n(%) |
P value | |
|---|---|---|---|
| n=121 | n=114 | ||
| Adolescent Demographics | |||
| Age (years) | 13.3(1.0) | 13.3(1.0) | 0.791 a |
| Education (years) | 7.2(1.3) | 7.2(1.2) | 0.941 a |
| Female(%) | 62(51.2%) | 54(47.4%) | 0.553 b |
| Non-Hispanic Black (%) | 118(97.5%) | 110(96.5%) | 0.585 b |
| BMI Z score | 0.76 (1.2) | 0.59 (1.1) | 0.287 a |
| Overweight or obese (%) c | 54(44.6%) | 36(31.6%) | 0.040 b |
| Caregiver Demographics | |||
| Age (years) | 39.4 (8.5) | 40.7 (9.5) | 0.283 a |
| Female(%) | 113(94.2%) | 105(92.9%) | 0.699 b |
| Biological mothers(%) | 104(86.0%) | 91(79.8%) | 0.212 b |
| Overweight or obese(%) c (BMI ≥ 25kg/m2) | 92(76.7%) | 86(76.1%) | 0.920 b |
| Living below the federal poverty line(%) | 65(59.1%) | 55(52.9%) | 0.361 b |
| With high school diploma or GED(%) | 90(74.4%) | 86(75.4%) | 0.852 b |
| Female-led single parent household(%) | 72(60.0%) | 70(61.4%) | 0.826 b |
T-tests for the continuous variales
Chi-square tests for the categorical variables.
“Overweight or obese” is defined as greater than 85 percentile for the youth, and the BMI is greater or equal to 25kg/m2 for caregivers.
“Female-led single parent household” is defined as no male adult present in the household.
Post-intervention and delayed follow-up evaluations occurred an average of 10.9 (SD=4.70) and 24.1 (SD=5.43) months following baseline. Data were available for 184/235 (78%) adolescents at post-intervention and 179/235 (76%) adolescents at delayed follow-up. There were no differences in retention by group assignment, baseline overweight/obese status, PA, or dietary intake.
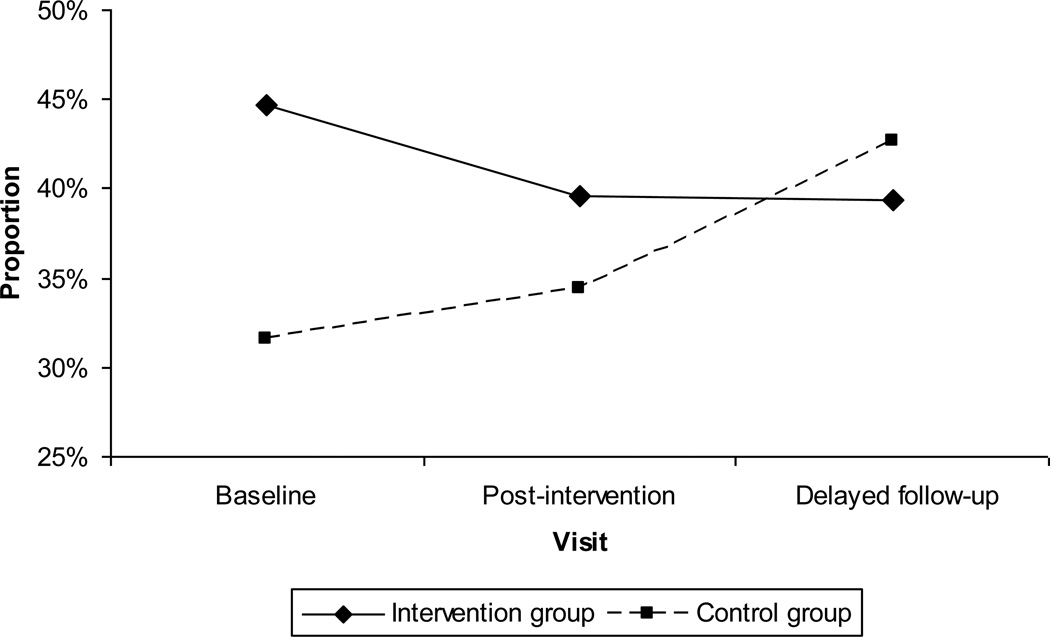
Overweight/Obese status
As shown in Table 2, the percentage of being overweight/obese adolescents declined from 54% to 36% while the percentage declined from 36% to 32% among the control group at post-intervention; The percentage of being overweight/obese further declined to 35%, but increased to 38% among the control group at delayed follow-up. GEE modeling with the exchangeable correlation structure, the auto-regressive correlation structure and unstructured correlation structure did not show much variation in the estimates of coefficients and standard errors. Therefore, we used the exchangeable correlation structure. In the GEE modeling, there was a significant interaction between time and intervention (β = −0.25, SE=0.09, p=0.006) in the delayed follow-up, but not in the post-intervention.
Table 2.
Anthropometry and DEXA-measured body composition scores by intervention status for baseline and two post-intervention follow-up evaluations
| Baseline | Post-intervention | Intervention*time interaction across post- intervention |
Delayed follow-up | Intervention*time interaction across delayed follow-up |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention N=121 |
Control N=114 |
Intervention N=91 |
Control N=93 |
Coeff. (S.E.) |
p- value*** |
Intervention N=89 |
Control N=90 |
Coeff. (S.E.) |
p- value*** |
|
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||||
| Anthropometry | ||||||||||
| BMI z-score | 0.76 (1.23) | 0.59 (1.11) | 0.73 (1.16) | 0.61 (1.14) | −0.03 (0.06) | 0.574 | 0.77 (1.14) | 0.65 (1.14) | −0.03 (0.03) | 0.341 |
| Overweight or obese (vs. normal weight) | 54 (44.63)* | 36 (31.58)* | 36 (39.56) | 32 (34.41) | −0.17 (0.17) | 0.327 | 35 (39.33) | 38 (42.70) | −0.25 (0.09) | 0.006 |
| Body Composition (DEXA) | ||||||||||
| Total percent body fat | 27.20 (10.18) | 24.47 (11.08) | 25.76 (11.36) | 24.20 (11.07) | 0.76 (0.59) | 0.201 | 25.00 (10.97) | 25.62 (12.07) | −0.39 (0.30) | 0.200 |
| Fat mass (kg) | 17.92 (10.47) | 15.37 (1.18) | 17.93 (12.01) | 16.05 (11.94) | 0.14 (0.56) | 0.795 | 18.18 (12.08) | 18.08 (12.78) | −0.46 (0.29) | 0.108 |
| Fat free mass (kg) | 431.75 (9.30) | 41.79 (10.64) | 45.79 (9.78) | 42.87 (8.37) | −1.22 (0.73) | 0.096 | 48.85 (10.55) | 46.56 (8.92) | 0.10 (0.37) | 0.799 |
Time is assessed in years after the intervention.
Intervention is categorized as “1” for intervention and “0” for control.
P value for BMI>85th percentile are based on Z test of SAS proc mixed model; other p values are based on t tests of SAS Proc Genmod model. All the models were controlled for age and gender at baseline.
In addition, when the analyses were stratified by gender or overweight/obese status, interaction between intervention and time was significant for both normal weight youth (β =−2.46 se=099 p=0.0130) and overweight/obese youth (β =1.89 se=0.90 p=0.036) at post-intervention. Interaction between intervention and time is significant (β =−0.41 se=0.14 p=0.0045) for males at the delayed follow-up, but not significant for females.
DEXA Body Composition
There were no statistically significant interactions between intervention and time in either post-intevention or delayed follow-up for total percent body fat, fat mass or fat free mass in the multi-level modeling with the whole sample. However, when the analyses were stratified by overweight/obese status, the intervention was effective in reducing fat percentile (β =−1.54 se=0.51, p=0.003) and fat mass (β =−1.31 se=0.57, p=0.025) and increasing the fat free mass (β =1.41 se=0.60 p=0.0205) in the overweight/obese youth in the delayed follow-up, but not for the normal weight youth.
Yan’ s question: Do we need to include this stratified results by gender? I included the information below any way in case the information is needed.
In addition, when the analyses were stratified by gender, the intervention was marginally effective for the females (β =−0.76 se=0.39, p=0.055), but not for the males with regard to fat mass in the delayed follow-up.
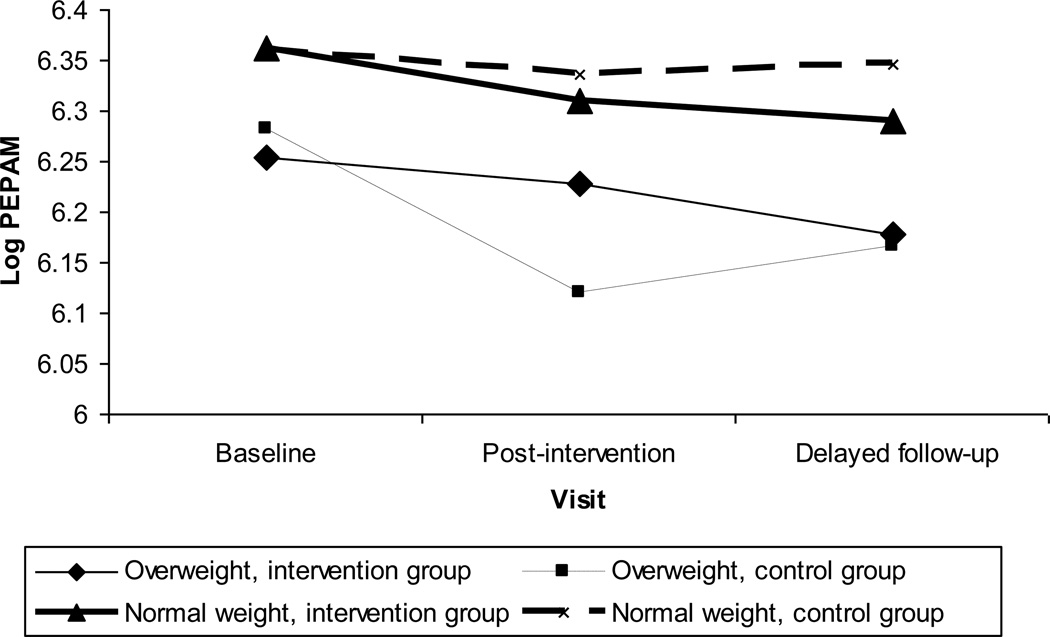
PA
There were no significant interaction between intervention and time with regard to log transformed daily activity counts or PEPA at post-intervention or delayed follow-up in the overall analytic sample (Table 3).
Table 3.
Physical activity (assessed via accelerometry) by intervention status for baseline, post-intervention, and delayed follow-up evaluations
| Baseline | Post-intervention | Intervention*time interaction across post- intervention |
Delayed follow-up | Intervention*time interaction across delayed follow-up |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention N=121 |
Control N=114 |
Intervention N=91 |
Control N=93 |
Coeff. (S.E.) |
p*** | Intervention N=89 |
Control N=90 |
Coeff. (S.E.) |
p*** | |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||||
| Physical activity | ||||||||||
| Log average total physical activity counts |
6.31 (0.26) |
6.34 (0.27) |
6.27 (0.31) |
6.26 (0.35) |
0.08 (0.05) |
0.133 | 6.24 (0.34) |
6.28 (0.30) |
0.01 (0.02) |
0.774 |
| Minutes per day of play equivalent physical activity (PEPA) |
90.93 (38.31) |
95.20 (43.77) |
87.77 (45.96) |
88.93 (50.19) |
10.76 (7.53) |
0.155 | 89.19 (47.99) |
92.32 (44.99) |
2.44 (3.71) |
0.512 |
| Overweight or obese subsample |
81.84 (32.62) n=50 |
86.50 (38.94) n=34 |
84.59 (48.68) n=35 |
66.19 (39.30) n=29 |
29.22 (10.87) |
0.009 | 82.08 (49.08) n=31 |
75.03 (31.77) n=29 |
8.80 (5.70) |
0.125 |
| Normal weight subsample |
98.26 (41.15) n=62 |
99.20 (45.51) n=74 |
90.36 (44.04) n=43 |
100.91 (51.45) n=55 |
−1.78 (10.35) |
0.864 | 94.09 (47.15) n=45 |
101.96 (48.54) n=52 |
−1.46 (4.88) |
0.766 |
Time is assessed in years after the intervention.
Intervention is categorized as “1” for intervention and “0” for control.
P values for interactions are based on z tests of SAS proc mixed models, which controlled for age and gender at baseline.
However, stratified analyses suggested that the effect of intervention on the change of PEPA might be moderated by baseline BMI category. As illustrated in Figure 3, among overweight/obese youth, the average PEPA for adolescents in the control group declined by 20.31 from 86.50 to 66.19 minutes per day while the average PEPA for adolescents in the intervention group increased by 2.75 from 81.84 to 84.59 in post-intervention. Multi-level modeling shows a significant interaction between intervention and time for the overweight/obese youth (β=29.22 se=10.87, p=0.009), but not in the normal weight youth in the post intervention (β=−1.78 se=10.35, p=0.864). No significant intervention effect was found for either overweight/obese group or normal-weight group in the delayed follow-up. Analyses stratified by gender did not found significant findings for post-intervention or delayed follow-up for either PEPA or the log transformed average daily activity.
Figure 3.
Log of mean minutes of Play Equivalent Physical Activity (PEPA) per day by intervention and overweight status across time.
Diet
Both intervention and control adolescents reported decreases in intake of total calories, fat, and fiber over time. As shown in Table 4, the adolescents in the intervention group, in general, reported a greater degree of decrease in average assumption per day than the adolescents in the control group for each item in post-intervention or delayed follow up except for milk at the post-intervention. The intervention effect reached significance on reducing consumption of snacks and desserts at both the post-intervention (β=−2.21 se=0.66 p=0.001) and the delayed follow-up (β=−0.69 se=0.31 p=0.026) and on reducing the consumption of fiber (β =−4.37 se=2.07 p=0.036) and fruit (β =−0.41 se=0.18 p=0.021) at the post-intervention. The intervention effect was marginally significant in reducing the consumption of total energy (β =−459.73 se=235.37 p=0.053) and total dietary fat (β =−17.01 se=9.28, p=0.069) in the post-intervention and fried food (β =−0.07 se=0.04 p=0.062), fiber (β =−1.76 se=0.99 p=0.077) and fruit (β =−0.15 se=0.09 p=0.089) in the delayed follow-up.
Table 4.
Food frequency daily intakes by intervention status for baseline, post-intervention, and delayed follow-up
| Baseline | Post-intervention | Intervention*time interaction across post- intervention |
Delayed follow-up | Intervention*time interaction across delayed follow-up |
||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Intervention N=121 |
Control N=114 |
Intervention N=91 |
Control N=93 |
Coeff. (S.E.) |
p-value*** | Intervention N=89 |
Control N=90 |
Coeff. (S.E.) |
p-value*** | |
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | |||||
| Total energy (kcal)* | 3058.5 (1703.4) |
2906.9 (1551.7) |
2461.0 (1398.4) |
2700.8 (1642.3) |
−459.73 (235.37) |
0.053 | 2216.6 (1368.2) |
2419.9 (1486.8) |
−167.57 (110.75) |
0.131 |
| Total dietary fat (g) | 111.0 (65.1) | 106.6 (61.3) | 90.3 (57.8) | 99.6 (70.5) | −17.01 (9.28) |
0.069 | 81.6 (51.1) | 89.2 (61.6) | −5.27 (4.29) |
0.221 |
| Saturated fat (g) | 38.4(22.9) | 37.0 (21.6) | 31.6 (20.7) | 34.2 (24.7) | −5.54 (3.37) |
0.102 | 28.5 (17.9) | 31.0 (21.0) | −1.79 (1.54) |
0.247 |
| Fiber (g)* | 23.0 (14.6) | 21.0 (15.2) | 18.8 (13.2) | 20.9 (16.5) | −4.37 (2.07) |
0.036 | 16.7 (11.6) | 18.4 (16.0) | −1.76 (0.99) |
0.077 |
| Calcium (mg) | 1333 (863) | 1263(825) | 1081 (705) | 1073 (817) | −127.65 (127.67) |
0.319 | 952 (640) | 1023 (820) | −73.06 (57.72) |
0.207 |
| Fruits (servings/day) | 1.6 (1.3) | 1.3 (1.3) | 1.2 (1.2) | 1.4 (1.4) | −0.41 (0.18) |
0.021 | 1.1 (0.9) | 1.1 (1.2) | −0.15 (0.09) |
0.089 |
| Vegetables (servings/day) |
2.4 (2.0) | 2.1(2.2) | 2.0(2.0) | 1.9 (2.3) | −0.18 (0.31) |
0.559 | 1.9 (1.9) | 2.0 (2.4) | −0.20 (0.16) |
0.204 |
| Snacks and desserts (servings/day)& |
5.7 (4.7) | 4.9 (4.1) | 4.0 (3.5) | 5.4 (5.2) | −2.21 (0.66) |
0.001 | 3.6 (3.7) | 4.3 (4.0) | −0.69 (0.31) |
0.026 |
| Milk (servings/day) | 1.0 (1.2) | 1.0 (1.2) | 1.0 (1.1) | 0.8 (1.0) | 0.13 (0.22) |
0.556 | 0.7(1.0) | 0.9(1.1) | −0.08 (0.10) |
0.448 |
| Non-diet soda (servings/day) |
0.8 (0.7) | 0.8 (0.7) | 0.6 (0.7) | 0.7 (0.7) | −0.04 (0.13) |
0.745 | 0.5 (0.6) | 0.7 (0.7) | −0.08 (0.06) |
0.163 |
| Fried foods (servings/day) |
0.8 (0.4) | 0.4 (0.3) | 0.6 (0.4) | 0.7 (0.5) | −0.08 (0.09) |
0.375 | 0.6 (0.4) | 0.8 (0.5) | −0.07 (0.04) |
0.062 |
Time is assessed in years after the intervention.
Intervention is categorized as “1” for intervention and “0” for control.
P values for interactions are based on z tests of SAS proc mixed models, which controlled for age and gender at baseline.
Although stratified analyses showed significances of the interaction between intervention and time for several diet variables by overweight/obese status or by gender, the directions of the interaction are, in general, remains the same across the subgroups by overweight/obese or gender. Therefore, the results of the stratified analyses were not detailed here and are available upon request from the corresponding author.
Details for the stratified analyses are listed below. I think they are not very informative, so I summarized the findings and wrote it above. If you need detailes, please see the following two paragraphs. If you do not need, please feel free to delete them.
Stratified analyses by overweight/obese status showed that the interaction between intervention and time for daily energy was significant for the normal weight youth (β=−740.96 se=335.82 p=0.030), but not significant for the overweight/obese youth (β=−112.85 se=326.23 p=0.731); the interaction for regular soda was marginally significant for the overweight/obese youth (β=−0.19 se=0.10 p=0.051), but did not reach significance for the normal weight youth (β=−0.02 se=0.08 p=0.824) in the delayed follow-up; the interaction for fiber was significant for the normal weight youth at the post-intervention (β=−7.96 se=2.88 p=0.007) and marginally significant in the delayed follow-up(β=−2.33 se=1.31 p=0.077), but was not significant for the overweight/obese youth in the post-intervention(β=0.36 se=3.00 p=0.905) or delayed follow-up(β=−1.11 se=1.54 p=0.471); the interaction for fruit was significant for the normal weight youth in the post-intervention (β=−0.73 se=0.24 p=0.003) and the delayed follow-up(β=−0.29 se=0.12 p=0.012), but was not significant for the overweight/obese youth in the post-intervention or the delayed follow-up; the interaction for snack was marginally significant for the overweight/obese youth in the post-intervention (β=−1.68 se=0.90 p=0.067) and in the delayed follow-up (β=−0.82 se=0.42 p=0.054) and was significant for the normal weight youth in the post-intervention (β=−2.62 se=0.95 p=0.007).
The interaction for total fat was marginally significant for the females were marginally significant in the delayed follow-up (β =−10.23 se=5.23 p=0.052), but not for the males; the interaction for the calcium was significant for females (β =−150.36 se=67.08 p=0.026),, but not for males in the delayed follow-up; the interaction for the regular soda was significant for females (β =−0.17 se=0.18 p=0.038), but not for males in the delayed follow-up; the interaction for the saturated fat was significant for females (β =−3.66 se=1.85 p=0.0498) in the delayed follow-up, but not for males in the delayed follow-up; the interaction for the fiber was significant for males (β =−8.06 se=3.43 p=0.021) in the post-intervention, but not for males in the post-intervention; the interaction for the fruit was significant for males, but not for females in the post-intervention (β =−0.74 se=0.28 p=0.009); the interaction for the snack was significant was marginally significant (β =−1.53 se=0.78 p=0.054) for the post-intervention and significant (β =−1.03 se=0.38 p=0.008) for the delayed follow-up among females, and was significant in the post-intervention (β =−3.29 se=1.10 p=0.004), but not significant in the delayed follow-up for the males.
Discussion
Challenge! was designed to overcome many barriers that interfered with the success of previous adolescent obesity prevention trials.(14) The 12-session intervention was implemented in adolescents’ homes with college students as mentors who accompanied the adolescents to neighborhood convenience stores and playgrounds to promote healthy dietary choices and PA. Using the principles of social cognitive theory and motivational interviewing, the mentors helped the adolescents identify personal challenges and goals related to diet and PA. These implementation strategies were effective in promoting positive changes related to weight status, percent body fat, PA, and diet.
Weight Status
The intervention adolescents did not advance in BMI category during the 2-year study period. In contrast, control adolescents advanced in BMI category over time, following a pattern of adolescent weight gain that has been well-described.(2) The effects of the intervention were not significant until the delayed follow-up, conducted more than one year after the intervention ended. This pattern suggests that a behavior change in either diet or PA preceded the change in weight gain. Moreover, the sustained effects in BMI category suggest that the intervention adolescents made long-lasting behavioral changes.
The absence of a significant change in z-BMI score may be partially explained by the inclusion of adolescents across a wide BMI range. Although changes in z-BMI within the normal weight category are of limited health consequence, we focused on youth regardless of their weight status to emphasize the normative aspects of consuming a healthy diet and engaging in PA and to reduce the stigma that may have resulted from targeting the overweight/obese adolescents. Our reasoning was that the adolescents’ low-income, minority status; high snack and dessert consumption; low PA; and high rate of maternal overweight/obesity placed all of them at risk (20, 47).
Percent Body Fat
Although percent body fat (measured by DEXA) declined among intervention adolescents and increased among control adolescents, the overall group difference over time was marginal. The pattern observed for control adolescents follows the expected trend (1–3). Among intervention adolescents, percent fat decreased over time while BMI category remained constant, suggesting that intervention adolescents were protected against becoming overweight/obese through exposure to the intervention and also experienced a slight, although non-significant decline in adiposity.
The gender differences in fat free mass related to the intervention suggest that males in the intervention experienced an increase in body tissues not containing fat, such as skeletal muscle. Although there were no gender-related differences in PA measured by accelerometry, adolescent males are more likely than females to form muscle in response to interventions. One possibility is that intervention males engaged in weight bearing activities that increased fat free mass, but were not detected by accelerometry.
PA
At the post-intervention follow-up, the intervention protected the heaviest adolescents from the decline in PA experienced by the control adolescents. During the following year, the differences between the intervention and control adolescents declined, suggesting that the intervention effects were not sustained. Adolescents may require more sustained intervention to continue to achieve changes in PA.
The decline in PA among control adolescents is consistent with national findings that rates of PA decline during adolescence (40, 41). Although at the post-intervention evaluation, we found significant differences in efficacy favoring the heaviest youth within the intervention, the intervention effects represented maintenance of the status quo, not an increase in PA. An inverse relation between body size and PA has been well documented among adolescents. (42) One possibility is that the heaviest adolescents, those most likely to experience a decline in PA, benefited from the individualized support of the mentored intervention and were able to sustain their prior levels of PA.
A strength of the current investigation is the reliance on accelerometry to measure PA. Many previous studies have relied on self-report recall to measure PA. However, self-reported PA is notoriously unreliable (14).
Snacks and Desserts
By the delayed follow-up, snack and dessert consumption decreased significantly more among intervention adolescents than control adolescents. Not only do adolescents tend to snack frequently (44), but snacks are often high in energy density and fat. Although we did not find other intervention effects related to diet, the overall sample reported declines in calories, fat, and fibers. However, caution is warranted because children may underreport dietary intake. (47).
Home Environment
Conducting the intervention in homes and communities enabled mentors to help adolescents build skills in their personal environments. Adherence to the intervention was positive; over half of the intervention adolescents participated in at least 10/12 sessions.
Methodological Considerations
There are several methodological considerations. First, generalizability is limited to similar populations. Second, although accelerometry provides an objective measure of movement, it does not capture weight-bearing activities or yield information on the type of PA. Third, although analyses of changes in BMI category and PA suggest that the beneficial effects of the intervention were concentrated among the heaviest adolescents, our power to conduct stratified analyses was limited. Finally, in spite of efforts to promote adherence by delivering the intervention at home, there was variability in the adolescents’ participation.
Conclusions
A one-on-one, 12-week health promotion, obesity prevention program delivered to low-income, urban adolescents in their homes and communities by college mentors was effective in preventing an increase in BMI category, in preventing a decline in PA among the heaviest adolescents, in enhancing fat free mass among males, and in reducing the intake of snacks and desserts. With the exception of the changes related to PA, the effects of the intervention were retained for one year after implementation of the intervention, illustrating that the effects of obesity prevention trials may not be detected at the close of the intervention and that behavioral interventions can lead to sustainable changes. One possibility is that the cultural sensitivity of the intervention delivered by college-enrolled mentors successfully altered the adolescents’ social norms around diet and PA.
Figure 2.
Proportion of adolescents with a BMI ≥85th percentile by intervention across time.
Acknowledgments
Funding: This research was supported by grant R40MC00241 from the Maternal and Child Health Research Program, US Department of Health and Human Services to Maureen Black, Ph.D., and the University of Maryland General Clinical Research Center grant M01 RR16500, General Clinical Research Centers Program, National Center for Research Resources (NCRR), NIH.
Abbreviations
- BMI
body mass index
- z-BMI
BMI z-score
- PA
physical activity
- PEPA
play equivalent physical activity
- DEXA
dual-energy x-ray absorptiometry
- BIA
bioelectrical impedance analysis
- kg
kilograms
- m
meters
- GEE
generalized estimating equation
- y
years
- SD
standard deviation
- YAQ
Youth Adolescent Food Frequency Questionnaire
- SES
socioeconomic status
Footnotes
Conflict of Interest: None of the authors has a conflict of interest.
Based on body mass index (BMI) weight in kg/height in m2. Overweight=BMI≥85th percentile and <95th percentile; obesity=BM≥95th percentile.
References
- 1.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007;120(Suppl 4):S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 2.Hedley AA, Ogden CL, Johnson CL, Carroll MD, Curtin LR, Flegal KM. Prevalence of overweight and obesity among US children, adolescents, and adults, 1999–2002. Jama. 2004;291(23):2847–2850. doi: 10.1001/jama.291.23.2847. [DOI] [PubMed] [Google Scholar]
- 3.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299(20):2401–2405. doi: 10.1001/jama.299.20.2401. [DOI] [PubMed] [Google Scholar]
- 4.IOM IoM. Preventing Childhood Obesity: Health in the Balance. Washington, DC: National Academies Press; 2005. [PubMed] [Google Scholar]
- 5.Shrewsbury V, Wardle J. Socioeconomic status and adiposity in childhood: a systematic review of cross-sectional studies 1990–2005. Obesity (Silver Spring) 2008;16(2):275–284. doi: 10.1038/oby.2007.35. [DOI] [PubMed] [Google Scholar]
- 6.Kiess W, Galler A, Reich A, Muller G, Kapellen T, Deutscher J, et al. Clinical aspects of obesity in childhood and adolescence. Obes Rev. 2001;2(1):29–36. doi: 10.1046/j.1467-789x.2001.00017.x. [DOI] [PubMed] [Google Scholar]
- 7.Clinton-Smith J. The current epidemic of childhood obesity and its implications for future coronary heart disease. Pediatr Clin North Am. 2004;51(6):1679–1695. doi: 10.1016/j.pcl.2004.07.005. [DOI] [PubMed] [Google Scholar]
- 8.Snitker S, Le KY, Hager E, Caballero B, Black MM. Association of physical activity and body composition with insulin sensitivity in a community sample of adolescents. Arch Pediatr Adolesc Med. 2007;161(7):677–683. doi: 10.1001/archpedi.161.7.677. [DOI] [PubMed] [Google Scholar]
- 9.Spector A, Scheid S, Hassink S, Deutsch ES, Reilly JS, Cook SP. Adenotonsillectomy in the morbidly obese child. International Journal of Pediatric Otorhinolaryngology. 2003;67(4):359–364. doi: 10.1016/s0165-5876(02)00401-9. [DOI] [PubMed] [Google Scholar]
- 10.Guo SS, Huang C, Maynard LM, Demerath E, Towne B, Chumlea WC, et al. Body mass index during childhood, adolescence and young adulthood in relation to adult overweight and adiposity: the Fels Longitudinal Study. Int J Obes Relat Metab Disord. 2000;24(12):1628–1635. doi: 10.1038/sj.ijo.0801461. [DOI] [PubMed] [Google Scholar]
- 11.Engeland A, Bjorge T, Tverdal A, Sogaard AJ. Obesity in adolescence and adulthood and the risk of adult mortality. Epidemiology. 2004;15(1):79–85. doi: 10.1097/01.ede.0000100148.40711.59. [DOI] [PubMed] [Google Scholar]
- 12.Kvaavik E, Tell GS, Klepp KI. Predictors and tracking of body mass index from adolescence into adulthood: follow-up of 18 to 20 years in the Oslo Youth Study. Arch Pediatr Adolesc Med. 2003;157(12):1212–1218. doi: 10.1001/archpedi.157.12.1212. [DOI] [PubMed] [Google Scholar]
- 13.Whitaker RC, Wright JA, Pepe MS, Seidel KD, Dietz WH. Predicting obesity in young adulthood from childhood and parental obesity. N Engl J Med. 1997;337(13):869–873. doi: 10.1056/NEJM199709253371301. [DOI] [PubMed] [Google Scholar]
- 14.Davis MM, Gance-Cleveland B, Hassink S, Johnson R, Paradis G, Resnicow K. Recommendations for prevention of childhood obesity. Pediatrics. 2007;120(Suppl 4):S229–S253. doi: 10.1542/peds.2007-2329E. [DOI] [PubMed] [Google Scholar]
- 15.Hill AJ, Franklin JA. Mothers, daughters and dieting: investigating the transmission of weight control. Br J Clin Psychol. 1998;37(Pt 1):3–13. doi: 10.1111/j.2044-8260.1998.tb01275.x. [DOI] [PubMed] [Google Scholar]
- 16.Troiano RP, Flegal KM. Overweight children and adolescents: description, epidemiology, and demographics. Pediatrics. 1998;101(3 Pt 2):497–504. [PubMed] [Google Scholar]
- 17.Summerbell CD, Chinnock P, O'Malley C, van Binsbergen JJ. The Cochrane Library: more systematic reviews on nutrition needed. Eur J Clin Nutr. 2005;59(Suppl 1):S172–S178. doi: 10.1038/sj.ejcn.1602193. discussion S195–6. [DOI] [PubMed] [Google Scholar]
- 18.Stice E, Shaw H, Marti CN. A Meta-analytic review of obesity prevention programs for children and adolescents: The skinny of interventions that work. American Psychological Association. 2006;132(5):667–691. doi: 10.1037/0033-2909.132.5.667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Davison KK, Birch LL. Weight status, parent reaction, and self-concept in five-year-old girls. Pediatrics. 2001;107(1):46–53. doi: 10.1542/peds.107.1.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Fulkerson JA, Strauss J, Neumark-Sztainer D, Story M, Boutelle K. Correlates of psychosocial well-being among overweight adolescents: the role of the family. J Consult Clin Psychol. 2007;75(1):181–186. doi: 10.1037/0022-006X.75.1.181. [DOI] [PubMed] [Google Scholar]
- 21.Dietz WH. Critical periods in childhood for the development of obesity. Am J Clin Nutr. 1994;59(5):955–959. doi: 10.1093/ajcn/59.5.955. [DOI] [PubMed] [Google Scholar]
- 22.Smolak L. Body image in children and adolescents: where do we go from here? Body Image. 2004;1(1):15–28. doi: 10.1016/S1740-1445(03)00008-1. [DOI] [PubMed] [Google Scholar]
- 23.Langevin DD, Kwiatkowski C, McKay MG, Maillet JO, Touger-Decker R, Smith JK, et al. Evaluation of diet quality and weight status of children from a low socioeconomic urban environment supports "at risk" classification. J Am Diet Assoc. 2007;107(11):1973–1977. doi: 10.1016/j.jada.2007.08.008. [DOI] [PubMed] [Google Scholar]
- 24.Black MM, Krishnakumar A. Predicting longitudinal growth curves of height and weight using ecological factors for children with and without early growth deficiency. J Nutr. 1999;129(2S Suppl):539S–543S. doi: 10.1093/jn/129.2.539S. [DOI] [PubMed] [Google Scholar]
- 25.Bandura A. Social foundations of thought and action: A social cognitive theory. New Jersey: Prentice-Hall, Inc.; 1986. [Google Scholar]
- 26.Resnicow K, Jackson A, Wang T, De AK, McCarty F, Dudley WN, et al. A motivational interviewing intervention to increase fruit and vegetable intake through Black churches: results of the Eat for Life trial. Am J Public Health. 2001;91(10):1686–1693. doi: 10.2105/ajph.91.10.1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.U.S. Census Bureau. 2004 In. [Google Scholar]
- 28.CDCP. CDC Growth Charts: United States. 2000 http://www.cdc.gov/growthcharts. [PubMed]
- 29.Puyau MR, Adolph AL, Vohra FA, Butte NF. Validation and calibration of physical activity monitors in children. Obes Res. 2002;10(3):150–157. doi: 10.1038/oby.2002.24. [DOI] [PubMed] [Google Scholar]
- 30.Rockett HR, Breitenbach M, Frazier AL, Witschi J, Wolf AM, Field AE, et al. Validation of a youth/adolescent food frequency questionnaire. Prev Med. 1997;26(6):808–816. doi: 10.1006/pmed.1997.0200. [DOI] [PubMed] [Google Scholar]
- 31.Rockett HR, Berkey CS, Field AE, Colditz GA. Cross-sectional measurement of nutrient intake among adolescents in 1996. Prev Med. 2001;33(1):27–37. doi: 10.1006/pmed.2001.0850. [DOI] [PubMed] [Google Scholar]
- 32.Snijders T, Bosker R. Multilevel analysis: an introduction to basic and advanced multilevel modeling. London, United Kingdom: Sage; 1999. [Google Scholar]
- 33.Diez-Roux AV. Multilevel analysis in public health research. Annu Rev Public Health. 2000;21:171–192. doi: 10.1146/annurev.publhealth.21.1.171. [DOI] [PubMed] [Google Scholar]
- 34.Fitzmaurice G, Laird N, Ware J. Applied Longitudinal Analysis. Hoboken, NJ: John Wiley & Sons, Inc.; 2004. [Google Scholar]
- 35.Mujahid MS, Diez Roux AV, Borrell LN, Nieto FJ. Cross-sectional and longitudinal associations of BMI with socioeconomic characteristics. Obes Res. 2005;13(8):1412–1421. doi: 10.1038/oby.2005.171. [DOI] [PubMed] [Google Scholar]
- 36.Botton J, Heude B, Maccario J, Ducimetiere P, Chares M, Group FS. Postnatal weight and height growth velocities at different ages between birth and 5 years and body composition in adolescent boys and girls. Am J Clin Nutr. 2008;87(6):1760–1768. doi: 10.1093/ajcn/87.6.1760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Aiken L, West S. Multiple Regression: Testing and Interpreting Interactions. Newbury Park, CA: Sage; 1991. [Google Scholar]
- 38.Sweeting HN. Gendered dimensions of obesity in childhood and adolescence. Nutr J. 2008;7:1. doi: 10.1186/1475-2891-7-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Doak CM, Visscher TL, Renders CM, Seidell JC. The prevention of overweight and obesity in children and adolescents: a review of interventions and programmes. Obes Rev. 2006;7(1):111–136. doi: 10.1111/j.1467-789X.2006.00234.x. [DOI] [PubMed] [Google Scholar]
- 40.Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc. 2000;32(5):963–975. doi: 10.1097/00005768-200005000-00014. [DOI] [PubMed] [Google Scholar]
- 41.Webber LS, Catellier DJ, Lytle LA, Murray DM, Pratt CA, Young DR, et al. Promoting physical activity in middle school girls: Trial of Activity for Adolescent Girls. Am J Prev Med. 2008;34(3):173–184. doi: 10.1016/j.amepre.2007.11.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McMurray R, Harrell J, Creighton D, Wand Z, Bangdiwala S. Influence of physical activity on change in weight status as children become adolescents. Int J Pediatr Obes. 2008;3(2):69–77. doi: 10.1080/17477160701789794. [DOI] [PubMed] [Google Scholar]
- 43.Surgeon G. Physical Activity and Health: A Report of the Surgeon General. Atlanta, GA: 1996. [Google Scholar]
- 44.Lewis-Moss RK, Paschal A, Redmond M, Green BL, Carmack C. Health Attitudes and Behaviors of African-American Adolescents. J Community Health. 2008 doi: 10.1007/s10900-008-9101-0. [DOI] [PubMed] [Google Scholar]
- 45.Baranowski T, Cullen KW, Nicklas T, Thompson D, Baranowski J. Are current health behavioral change models helpful in guiding prevention of weight gain efforts? Obesity Research. 2003;11(Suppl):23S–43S. doi: 10.1038/oby.2003.222. [DOI] [PubMed] [Google Scholar]
- 46.Johnson R. Dietary intake: How do we measure what people are really eating. Obesity Research. 2002;10(1):63S–68S. doi: 10.1038/oby.2002.192. [DOI] [PubMed] [Google Scholar]
- 47.Campbell K, Crawford D, Salmon J, Carver A, Garnett S, Baur L. Associations between the home food environment and obesity-promoting eating behaviors in adolescence. Obesity (Silver Spring) 2007;15(3):719–730. doi: 10.1038/oby.2007.553. [DOI] [PubMed] [Google Scholar]
- Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73:13–22. [Google Scholar]